#antibiotic resistance
Link
A groundbreaking study conducted by scientists from MIT and McMaster University has unveiled a revolutionary artificial intelligence-based antibiotic that effectively eliminates a specific strain of bacteria often associated with drug-resistant infections. If it receives approval for patient usage, the newly developed antibiotic has the potential to significantly contribute to the battle against Acinetobacter baumannii, a bacterial strain frequently encountered within healthcare facilities.
Acinetobacter baumannii is known for its ability to induce serious infections like pneumonia and meningitis, making it a formidable adversary. Furthermore, it is noteworthy to mention that this microbe also contributes significantly to infections among injured soldiers in Iraq and Afghanistan. This article examines how cutting-edge research and AI algorithms are transforming drug discovery and providing encouragement in the fight against antibiotic resistance.
As bacteria evolve and develop strategies to dodge the effects of existing medicines, the growth of antibiotic resistance has become a global health concern. Regrettably, new antibiotic development has not kept pace with the growth of resistant bacteria. Recognizing this urgent need, the research team at MIT and McMaster University sought to leverage AI technology to expedite the discovery of novel antibiotics.
Continue Reading
85 notes
·
View notes
Text
alright it's time to find smth out
please note that with labels like flexitarian especially it's not about 'oh i never eat these things'; it's a sliding label with things like vegan and vegetarian and pescatarian where you can identify however you feel comfortable. some people just eat meat etc on special occasions or when they go out or when they don't have time/spoons to cook something nutritious, and that's perfectly valid!! whatever you're able to do has an impact that's felt and there's no pressure to do it to whatever standard we have of 'perfect' in our heads <3
#bringing gender labels to vegetarianism#kind of. we need a lot more validation in these spaces#again want to stress so much. literally no judgement based on what you choose. the important part is if we can we do smth#and if you can't then i believe you and you don't need to worry bc those of us who can are doing what we can#vegan#vegetarian#pescatarian#flexitarian#climate action#climate justice#food security#antibiotic resistance#bird flu#biosecurity#public health#human rights#feminism#biodiversity collapse
16 notes
·
View notes
Text
“And, if you find scary bacteria, send them to [other doctor]. I’m too old to deal with that crap.”
Head of the Infectology department.
#medicine#med school#medblr#infectology#bacteria#antibiotic safety#antibiotics#antibiotic resistance#pinned
102 notes
·
View notes
Text

From Regenesis: Feeding the World Without Devouring the Planet by George Monbiot
18 notes
·
View notes
Text
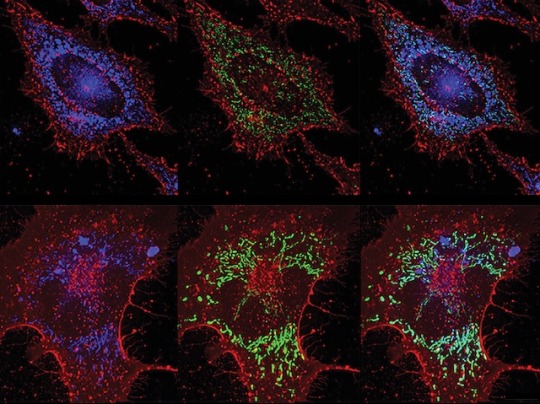
ROS vs Bacteria
Inducing lung lining cells to produce bacteria-killing reactive oxygen species (highly reactive chemicals that can cause oxidative damage) protects against pneumonia without reliance on antibiotics
Read the published research paper here
Image from work by Yongxing Wang and colleagues
Department of Pulmonary Medicine, University of Texas MD Anderson Cancer Center, Houston, TX, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in PLOS Pathogens, September 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#reactive oxygen species#ROS#sci art#pulmonary#lungs#pneumonia#antibiotics#antibiotic resistance
10 notes
·
View notes
Text
My breathing is getting worse again. This will be the fifth antibiotic resistance I've had. It's by far worse than any bronchitis I've ever heard of. They said I don't have pneumonia anymore but almost all my symptoms are the same severity, and it's in both lungs now.
I can't sleep because I can't stop coughing and internally it sounds like a Geiger counter. I'm just really scared. I'm on 10+ prescriptions. I'm sure all of this is related to having covid in September because I have never before been a fraction of this ill ever in my life. I wear a mask virtually everywhere but finally caught covid doing odd jobs and errands for a wealthy person who did not wear a mask. I've felt weaker ever since that happened but really could not afford to slow down or take a break to get better. I couldn't even rest enough while actually having covid because I was living with a denier and my spouse would not let me come to our house during that time. I did at least get to take paxlovid but was pretty much forced to be active during that time and immediately go back to work after.
Then, a month later, I got extremely ill from a cold my coworker had. I went to urgent care for high fever but because I went during one of the only breaks in the actual fever, I was given nothing for it and it kept coming back until I had pneumonia.
Then, I went to a university hospital where I feel more mistakes were made, like giving me something too weak for too short a time, giving me antibiotics through a bad iv, and not releasing me with any oral antibiotic. They also would not let me have my blood pressure medication so I had extremely high blood pressure the whole time I was there (also a problem I did not have before covid).
Now I have two inhalers and a home nebulizer. Sometimes I feel like I just pass out from not having enough oxygen. It feels like physically moving my lungs to breathe is difficult, even beyond oxygen saturation. I have been to a marginally better hospital, but it takes longer to get to and I know if the ER were busy it would probably be as bad as the university one. I have an appointment with a specialist on boxing day, which was the soonest I could get since this started, even after being admitted (the university hospital made me an appointment for the end of January and I've been back in the ER twice since then). I don't know if I can even wait for five more days. Since the first time I went to the ER I haven't been out of the hospital for as long as a week without then feeling worse and needing to go back even more urgently. Based on all of this, I will probably have to go back by Saturday.
I know there are lots of stories like mine but I just wanted to make a longer post about it in case I feel too badly to do it later.
Cautionary advice:
wear your mask; only take it off if you are specifically willing to get sick from the environment/activity you're engaging in.
If you have persistent high fever, do not lie on your side if you are crying, laughing, or congested; this can easily cause an infection to spread to the lung on the side you're lying on. Also, if you already have an infection of that severity, don't even lean to one side while laughing or crying because that can make it suddenly worse and further spread the infection. I just feel like I need to include this because it can happen so easily.
Everyone probably knows this but if you have a busted vein, do not use an iv on the same vein, even if medical staff say it doesn't matter. It does matter, and getting an infusion that just leaks out of a busted vein instead of actually circulating intravenously will not have the same effect and will cause complications.
If you have antibiotic resistance and you get iv antibiotics and then leave the facility before you're in good health, you need to go home with oral antibiotics. Really this is probably a good idea even without prior antibiotic resistance since an incomplete course just makes resistance more likely.
#Long post#Personal#Cautionary#Covid#Pneumonia#Bronchitis#Antibiotic resistance#Hospital#Just want to share so maybe someone else can avoid a similar situation#I am so tired of this but it's not going anywhere
6 notes
·
View notes
Text
Tldr (or just don't like scientific journals)? Read this:
#science#science communication#scicomm#stem#science education#science blog#biology#environmental science#climate change#climate emergency#climate and environment#environmental issues#environmental impact#antibiotic resistance#microbiology
13 notes
·
View notes
Text
Did you know that the US allows use of an antibiotic as a pesticide????
There are farmers out there, spraying an antibiotic on their crops. And on the soil. And bugs. And everything else nearby and I guarantee it collects in stormwater runoff.
And it's used on a scale of 100,000+ lbs. Sprayed. Into the environment.
#pesticides#antibiotic resistance#but a us reglatory agency said it's fiiiiiiine so its totally okay right guys??#I am viscerally Uncomfortable.
2 notes
·
View notes
Text
Watching a young patient with severe bacterial infection and no way to save them because the bacteria is resistant to every know antibiotic that should be effective against it hits really fucking hard.
We should be able to treat this, we have the means, and yet... We don't. It's terrifying.
#medblr#antibiotic resistance#i long ago gave up the dream that we could save everyone#but this is a new level#when we used to be able to fight this#but now we just watch#and pray that this specific bacteria doesn't get out of containment#tw death#because that's where this story will end
22 notes
·
View notes
Text
USAmerican problems in providing healthcare are resulting in the spread of antibacterial-resistant strains.
On top of the overuse of antibiotics contributing to the development of antibacterial-resistant bacteria, people who leave their entire country to access affordable medical care are at a very high risk of spreading resistant bacteria around. This study, for example, found that 30% of international travellers returned with a antimicrobial resistant bacterium. Now consider that that is among completely healthy travellers, and that hospitals tend to be hotbeds for antibiotic and antimicrobial resistant strains of bacteria.
Not only is it dangerous for the individual to leave the country for healthcare (what if you don’t speak the language? Do you have a place to safely recover there? What if you have a complication but you’ve already arrived back at your home country?), not only is it absolutely ludicrous and dystopian that someone in a country with the ability to have good quality medical care would have to LEAVE to actually get such care, it’s also contributing to one of the biggest problems in medical science today.
Universal healthcare is a necessity.
(Additional sources below the cut)
http://www.jstor.org/stable/26690839
#medical tourism#healthcare#antibiotics#antibiotic resistance#medical science#medical microbiology#universal healthcare
3 notes
·
View notes
Link
Scientists from Barcelona have discovered a new hexameric protein structure for the RepB protein, which is involved in catalyzing replication initiation in Streptococcal plasmid pMV158, conferring antibiotic resistance to tetracycline. The new hexameric structure, obtained using biochemical methods and X-ray crystallography, is found to render flexibility, which attributes to the dual functionality of the protein, viz., binding to two distinct sites of the plasmid and separating one of the DNA strands by cutting it off, resulting in the initiation of DNA replication. The new structural information now available will aid in designing new antibiotics for therapeutics as well as in a better understanding of antibiotic resistance in the laboratory.
The story of antibiotic resistance and DNA replication featuring RepB protein
Antibiotic resistance results when the disease-causing bacterium or other pathogens acquire genetic mutations to adapt against the drugs designed to nullify them. These mutations, under selective pressure to adapt to the toxic environment, as generated by the drugs, result in drug-resistant variants. These acquired mutations are often not vertically obtained from previous generations but rather are acquired horizontally through horizontal gene transfer (HGT). This lateral transfer of mutations is across species in the tree of life and is quite prevalent in prokaryotes like bacteria and some eukaryotes like yeast. Antibiotic resistance genes in bacteria are mostly acquired by HGT.
Continue Reading
72 notes
·
View notes
Text
british culture btw
#im going insane in de membrane#i think ive used that tag before huh#jessjamie shitposts#just me and school mates on disc at 11:30 at night when we could be revising for our alevels#horrible histories#british memes#british culture#british#antibiotic resistance#wonderwall#park life#blur#oasis#kings and queens
64 notes
·
View notes
Text
*accidentally drops a snack in the hospital*
Student: Great, now it has carbapenemases.
21 notes
·
View notes
Text

Our Health Secretary, a good friend of antibiotic resistant bacteria.
19 notes
·
View notes
Photo
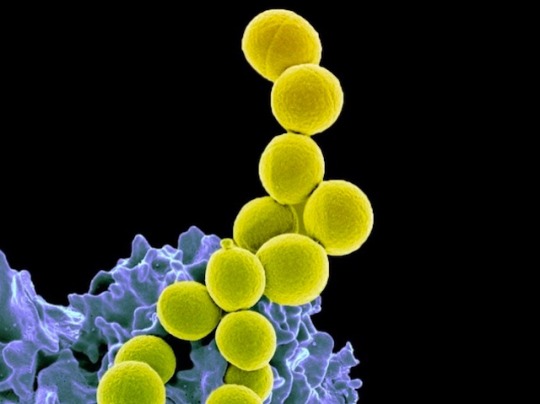
Potential Pathogen
These yellow spheres are Staphylococcus aureus bacteria on the surface of a human immune cell (blue). They are found in, and on, about a third of the human population and are generally harmless except, that is, for when they’re not. S. aureus can cause severe and potentially fatal infections of the skin, soft tissues, bone and blood, and especially dangerous are the drug-resistant strains – so called, methicillin-resistant S. aureus (MRSA). The bacteria were thought to mainly inhabit the skin and nose, but recent research shows they are most abundant in the gut. This discovery led researchers to test whether probiotics – oral doses of friendly bacteria – could suppress S. aureus colonisation. And they could – by around ninety-five percent. Probiotics work more slowly than traditional antibiotics for tackling infections, but they can be taken for much longer without harm, and will likely be able to tackle MRSA strains when regular drugs cannot.
Written by Ruth Williams
Image from the NIH, National Institute of Allergy and Infectious Diseases (NIAID), Bethesda MD, USA
Research by Pipat Piewngam & Sunisa Khongthong, et al, NIAID and Rajamangala University of Technology Srivijaya, Thailand
Image in the Public Domain
Research published in Lancet Microbe, January 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#staphlococcus aureus#staph aureus#bacterial infections#mrsa#antibiotic resistance#probiotics#electron microscopy
33 notes
·
View notes
Text
Unusual antibiotic killing mechanism we just published in Nature
Our study about the unusual molecular mechanism behind the antibiotic activity of teixobactin can be read open access here:
https://www.nature.com/articles/s41586-022-05019-y
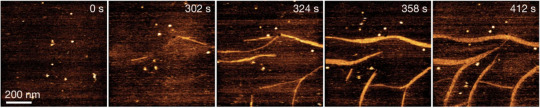
Figure: The target of teixobactin are bacteria-specific molecules (e.g. they do not exist in human cells) in outer membranes of bacteria. Teixobactin sits on the membrane and aggregates into fibrils, damaging the bacterial membrane and hindering its functions. We got these images by atomic force microscopy that has nanometer resolution. We can see individual teixobactin molecules coming to the bacterial membrane and forming the aggregate.
This is the first star from my research on antibiotics that I started at my postdoc in the Netherlands. More are coming out soon! The very first star was published in Nature, the most read journal in life sciences. I am in scientific heaven!
#science#research#publishing#nature journal#achievement#antibiotic#biophysics#stem#women in science#scientific article#scientific discovery#antibiotic resistance#original content
29 notes
·
View notes