#md/mph
Text
I am one month into residency. Here are a few things I've learned (mostly about myself):
1) I am, indeed, a textbook person. I always thought I was an uptodate person, but it's just not always the best resource for peds. I have looked things up in Red Book, Lange Neonatology, Bright Futures, and AAP Peds in Review multiple times this month already. They just seem to work better for me when I have the time. Uptodate is my second choice for on-the-go reading (like when walking to morning conference)
2) organization is key. I'm not sure what system works best for me on rounds since the handoff sheet we get is completely different from what we used at my med school. (Same info, just formatted differently on the page). But, I have found having a succinct cover sheet with all of my patients only and their to-do items for the day to be way more efficient than flipping back and forth in a big packet. I'm still working out how to make the handoff page work best for me during rounds though. One thing is clear though, if you're not organized, something will be forgotten. For me, keeping lists and check boxes is key.
3) if I don't write it down, it doesn't exist. How do people remember *everything*?? If I don't write it down within 5 minutes of doing it/hearing about it/being told to do it, it's forgotten in the abyss.
4) good sleep hygiene is my BFF. I probably have co-residents with wacky schedules, but I like my routine and I have noticed I do better when I'm well rested. I typically get 6-8 hours, but in order to ensure that happens, I have a pretty consistent routine in the evenings after work and the mornings before work (especially since I don't have a yard and have to walk my dog both times). I also like feeling well rested in the morning. I'm in a better mood, less stressed, and make fewer mistakes. (Maybe this one matters more since I don't drink coffee or soda so I don't get an extra boost from the caffeine?? I've debated energy shots, but I get heart palpitations with anxiety and they freak me out. I can only imagine what extra caffeine would do)
5) I 100000% prefer to work as a team than work alone. My last block was very team oriented and I felt like I thrived. We were always asking each other how we could help and getting lunch or snacks for each other when we couldn't go together as a group. It was very much a "we all lift each other up" kind of environment. I hope that carries into my other blocks, too. I'm going to do my best to continue to be a team player and help everyone with their workload.
6) I still feel pretty dumb and unsure of myself, but the imposter syndrome is WAY less than before. Idk if it's the new environment or what, but I just don't feel that same fear of being too dumb and undeserving and being the weak link like I did during med school. Sure, I have a lot to learn and I do sometimes forget things or freeze up (for instance, I completely forgot what DI was today during rounds. Literally could not have even told my fellow my name if she had asked.lol) and while I fell a little embarrassed, it's not the same as it was before. Maybe I'm in a better mental place for now?
7) Im somehow less stressed. Like, I work hard at work and sometimes I get frustrated or get stuck, but it's not the same as being a student. I read articles and do practice questions at home but it's much more leisurely. Despite the long hours, I find this WAY more enjoyable than med school. I don't feel guilty for taking time off or enjoying my hobbies and I actually enjoy studying and looking up stuff about my patients. Residency is hard, but I am so much happier than I was before. I hope it stays this way.
8) my dog is still one of the absolutely best part of my day. She's happy when we get up in the morning and happy when I get home in the evening. She will forever be the bright, sunny spot in my day. Its a lot of work having a dog while living alone, but holy crap is she worth it❤
#residency#resident#doctor#md#md/mph#pgy1#intern#internship#intern year#medical#medicine#physician#studyblr#study blog#medical blog#medblr
18 notes
·
View notes
Text
rewatching house and i'm on season 4 rn and every time kutner appears on my screen i get cuteness aggression. i need to squish him like a stress ball. i fucking love him hey why the fuck is a cop car pulling up to my high school lights and sirens rn
#got distracted mid post mb#APPARENTLY SOMEONE WAS DRIVING 95 MPH OUT HERE??? HELLO 😭#where the fuck could u have possibly managed to do that.....#anyways#house md#lawrence kutner#kutner#dr kutner#thanks obama
68 notes
·
View notes
Text
Have said it before, will say it again: I'm no great person. Neither morally nor intellectually. When I rag on all sorts of experts and degree-holders, it's not because I think so much of myself as to imagine I'm omnicompetent, but because I think so very little of them.
So here's my latest bit of ragging on high places:
Opinion: Trust in science is declining. Here’s how we can regain it
Megan L. Ranney, MD MPH, is an emergency physician and dean of Yale School of Public Health. Katelyn Jetelina, MPH PhD, is an epidemiologist, advisor to the US Centers for Disease Control and Prevention
These two Masters of Public Health have correctly noticed a lack of trust. Their proposed patch boils down to: tell people to have more trust, loudly, frequently, and on more channels.
There is no mention of apologizing for mistakes in general, nor acknowledging any specific mistakes made. Nothing about improvements to be made among scientists, neither self-policing nor the lack thereof, nor the replication crisis, et cetera. There is only a lengthy call to communicate better, leading to this amazingly awful sentence:
At the end of the day, if the United States is going to improve our trust in science, we have to ensure that we are all public health communicators.
Problem 1: you take your own perfection for granted, not considering anything you might do to earn trust.
Problem 2: you treat "trust" as a goal in itself, rather than something that should correspond to your trustworthiness.
Problem 3: you equivocate between science and public health.
Problem 4: you call on everyone else in "we" to fix your bad rep.
THESE ARE BAD PEOPLE. DON'T TRUST THEM.
Social media can play a part, too. Work by the National Academy of Medicine, in collaboration with the Council for Medical Specialty Societies and the World Health Organization (with which Dr. Ranney was involved), outlined ways for social media companies to identify and amplify “credible health messengers” — both the professionals and the everyday folks who are volunteering their time to create content. We applaud companies like YouTube that have made this work a priority, and hope that more companies will follow.
A cynical person might describe this in terms of selective reporting and suppressing dissent. The use of "credible" as opposed to "honest" sounds like a spin doctor wanting to make problems go away by rhetoric instead of work. It's not clear how much of the MPH's focus on health, vaccination, the WHO and so forth is déformation professionelle, and how much is a MPH trying to spend down the credit of "science" at large for the benefit of her personal narrow slice of it.
CNN Opinion selects for the kind of people who want to be on CNN, and the kind of people CNN wants to have on, so Ranney and Jetelina are probably not representative of public health, or so I hope. They're still awful people. Their entire opinion piece is a demonstration of why "trust in science" should be low: there is a serial conflation of trust in scientists and trust in experts and trust in credential-holders like Ranney and Jetelina who in turn treat trust as a kind of compliance to be acquired by badgering people.
46 notes
·
View notes
Text
i am one of only two people on this symposium agenda that does not have a PhD, MD or MPH
#theres just me and another man who have Only our names next to our presentation#everyone else has all their Qualifications next to them#i have. a bachelor's degree lmao
8 notes
·
View notes
Note
hi legend😍 miss you 😔 dont take that corporate job too seriously 👍 live laugh love
makoshark x charlesbeckendorf linkup once you’re a bs phd mph md ba etc etc will be legendary
7 notes
·
View notes
Video
Matt: Male gametes. That’s what makes me male.
Michelle: No. No, your sperm don’t make you male.
Matt: Then what does?
Michelle: It’s a constellation.
Matt: In reality. In truth.
Michelle (confused): Whose truth are we talking about?
Matt: The same truth that says we’re sitting in this room right now, you and I.
Michelle: No. You’re not listening.
Matt: If I see a chicken laying eggs and I say that’s a female chicken laying eggs, did I assign female or am I just observing a physical reality that’s happening in the world?
Michelle: Does a chicken have gender identity? Does a chicken cry? Does a chicken commit suicide? Let’s frame it...
Matt: What’s that have to do with...
Michelle: Because you’re talking, you’re trying...
Matt: A chicken has sex, like any biological organism.
Michelle: A chicken has an assigned gender. But a chicken doesn’t have a gender identity.
Matt: So we “assign” female to chickens when they lay eggs? That’s a...
Michelle: We assume they’re female if they lay eggs.
==
It wasn’t so long ago that we were being told “NoBoDyS SaYiNg bIoLoGiCaL SeX IsNt rEaL”. Now they’re saying so out loud.
A licensed medical doctor and professor of pediatrics at Brown University who doesn’t think biological sex is observed or even real. Yet is allowed to advise, prescribe drugs to, and transition children based on the mental virus of postmodern social constructivism, and teach others the same.
https://vivo.brown.edu/display/mforcier
Michelle Forcier, MD, MPH has been in Rhode Island and at Hasbro Children’s Hospital since 2009. She is a Professor of Pediatrics, Assistant Dean of Medicine (Admissions) at The Warren Alpert Medical School of Brown University.
#Matt Walsh#Michelle Forcier#What is a Woman#What is a Woman?#social constructivism#social construct#gender ideology#queer theory#gender pseudoscience#gender phrenology#medical malpractice#biological dimorphism#dimorphism#human biology#evolution denial#evolution deniers#insane people#unethical#deranged people#religion is a mental illness
274 notes
·
View notes
Link
FDA explicitly recognizes that doctors do have the authority to prescribe ivermectin to treat COVIDDepartment of Justice lawyer representing the FDACircuit J...
21 notes
·
View notes
Text
Of course it would be a who MAN would try to amend a bill the Child-Parent Security Act (CPSA) to: (1) deny a surrogate child's fundamental human right to know the identity of his or her birth mother; (2) allow the possible removal of the surrogate mother's identity on the child's birth certificate; (3) weaken the CPSA's residency requirements of the surrogate and the intending parent(s); (4) increase highly coercive contract remedies; (5) eliminate certain legal fees coverage for the surrogate in the event of a litigated dispute with the intending parent(s); (6) suggest that gamete providers have parental rights they must relinquish; and (7) loosen the requirements that surrogates must be administered informed consent procedures.
NEW YORK, May 25, 2023 /PRNewswire/ -- Dozens (and counting) of New York children's and women's rights advocates, including the Coalition Against Trafficking in Women, author and feminist activist Gloria Steinem, medical and public health professionals, surrogate survivors, and members of the LGBTQI+ community signed a letter to the New York State Senate and Assembly leadership detailing their concerns regarding Bill S.5107 introduced by Senator Brad Hoylman-Sigal.
The bill significantly amends the Child-Parent Security Act (CPSA) that legalized reproductive commercial surrogacy in New York. The CPSA was enacted by former Governor Andrew Cuomo in April 2020 as a line item in the 400-page state budget at the height of the COVID-19 emergency in New York. It was never afforded the opportunity of critical public discussions or deliberations.
Although Bill S.5107 is presented to the NYS Senate as a merely technical, "clean up" intervention, it in fact introduces substantive changes that far worsen the positions of children born of surrogacy arrangements, persons providing gametes, and surrogates.
The extensive amendments to the CPSA offered by Bill S.5107 propose to: (1) deny a surrogate child's fundamental human right to know the identity of his or her birth mother; (2) allow the possible removal of the surrogate mother's identity on the child's birth certificate; (3) weaken the CPSA's residency requirements of the surrogate and the intending parent(s); (4) increase highly coercive contract remedies; (5) eliminate certain legal fees coverage for the surrogate in the event of a litigated dispute with the intending parent(s); (6) suggest that gamete providers have parental rights they must relinquish; and (7) loosen the requirements that surrogates must be administered informed consent procedures.
The speed with which the proposed amendment appears to be moving through the New State Senate approval process just a few days before the end of the legislative session is extremely troubling. The signatories of the letter call for open and fair deliberations and discussion on Bill S.5107.
For more information, contact:
Wendy Chavkin, MD, MPH
[email protected]
Yasmine Ergas, JD
[email protected]
Taina Bien-Aimé, Coalition Against Trafficking in Women
[email protected]

View original content:https://www.prnewswire.com/news-releases/gloria-steinem-and-dozens-of-new-york-womens-rights-civil-and-human-rights-advocates-express-deep-concern-about-proposed-new-york-senate-bill-on-reproductive-commercial-surrogacy-and-call-for-public-deliberations-301835077.html
SOURCE The Coalition Against Trafficking in Women (CATW)
#anti surrogacy sunday#USA#New York#anti exploiting women#babies are not commodities#Coalition Against Trafficking in Women#Gloria Steinem#Bill S.5107#Senator Brad Hoylman-Sigal#Child-Parent Security Act (CPSA)
32 notes
·
View notes
Text
So, I've been checking off as much as possible on my pre-residency to-do list before I move.
I've officially been everywhere on my med school city bucket list except for one place that I just can't make happen before I move. Overall, not bad.
All of my pre-orientation items are done except for signing up for parking, which I can't do until mid June anyway.
I've been reviewing the NRP book periodically. I start in the newborn nursery, so it feels nice to be reading something helpful. It had made me feel a little more prepared and (a little) less nervous. I'm definitely not trying to seriously study before starting residency, but since it's going to be well over 100°F here every day this week, I needed something to mull over in the midday heat -- especially since everything else is packed up already.
Seriously, it's so hot my dog even voluntarily declined an evening walk today. She's never done that before.
#medblr#medical school#medical student#future doctor#studyblr#med student#md/mph#med school#medicine#personal#pgy1#resident#medical resident#thoughts#medical blog#studygram#study blog
4 notes
·
View notes
Text
youtube
Mammography - Does it save lives? | The USPSTF is incorrect | I review ALL the data
Vinay Prasad, MD MPH; Physician & Professor Hematologist/ Oncologist Professor of Epidemiology, Biostatistics and Medicine
4 notes
·
View notes
Photo

岸田直樹【総合内科/感染症コンサルタント】MD,MPH,PhD,CEO, 三児父,キッシーさんはTwitterを使っています:「この3た論法 が大切です これを知っているだけでも、ものの見方を 歪みなくとらえることができます」
46 notes
·
View notes
Text
all people have is the audacity...had a woman in my class say that the doctor with an MD and MPH doesn't seem like an expert??? because she says um????

2 notes
·
View notes
Text
“Donna Roe” 19 (USA 1973)
The unidentified teenager known only as “Donna Roe” was 19 years old and pregnant for the first time when she underwent a legal abortion. She didn’t know that Roe v. Wade was no guarantee of her safety.
Donna had no noted pre-existing health problems, although a doctor had an unconfirmed suspicion that she may have been an IV drug user. If this was correct, it’s possible that she may have had the abortion out of fear of what the drugs had done to her child.
At 17 weeks pregnant, Donna underwent a vaginally-administered prostaglandin abortion. Approximately two hours after passing her dead baby, Donna went into cardiac arrest. All attempts to save her life failed and she was soon declared dead.
Donna’s autopsy revealed what the prostaglandin had done to her body. She had an electrolyte imbalance and microscopic pulmonary embolism. Either of these alone could have sent her into cardiac arrest.
Fatal Pulmonary Embolism During Legal Induced Abortion in the United States from 1972-1985, Lawson, Herschel W., MD, Atrash, Hani K., MD, MPH, Franks, Adele L., MD, American Journal of Obstetrics and Gynecology, Vol. 162, No. 4, April 1990, p. 986-990
Deaths caused by pulmonary thromboembolism after legally induced abortion, Kimball, Hallum, Cates, American Journal of Obstetrics and Gynecology, Sept. 15, 1978, 132:2, 169-74
#tw abortion#pro life#unsafe yet legal#tw ab*rtion#tw murder#abortion#abortion debate#death from legal abortion
3 notes
·
View notes
Text
@ that nazi anon - thinking you're a doctor does NOT make you a doctor.
I'm not posting your little tantrum.
on the off chance you can read, here's some basic biology and statistics for you. If this is too wordy, maybe just take the entire world's health professionals at their word that trans health care is lifesaving. Thx!
Mental Health Outcomes and Receipt of Gender-affirming Care -David J. Inwards-Breland, MD, MPH; Diana M. Tordoff, MPH; Jonathon Wanta, MD; Cesalie Stepney, Ph.d - Pediatrics (2022) 149 (1 Meeting Abstracts February 2022): 590.
#tw transphobia#lgbtq#transgender#trans#trans healthcare#transrights#antifa#trans genocide#queer#lgbt#lgbtq+#transphobia#fascisim#trans health#trans rights
15 notes
·
View notes
Text

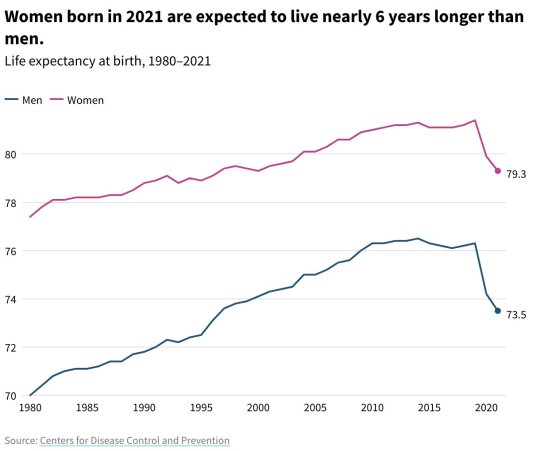
By: Brandon W. Yan, MD, MPH1,2; Elizabeth Arias, PhD3; Alan C. Geller, MPH, RN2; et al
Published: Nov 13, 2023
As life expectancy at birth in the US decreased for the second consecutive year, from 78.8 years (2019) to 77.0 years (2020) and 76.1 years (2021), the gap between women and men widened to 5.8 years, its largest since 1996 and an increase from a low of 4.8 years in 2010.1,2 For more than a century, US women have outlived US men, attributable to lower cardiovascular and lung cancer death rates related largely to differences in smoking behavior.1,2 This study systematically examines the contributions of COVID-19 and other underlying causes of death to the widened gender life expectancy gap from 2010 to 2021.
Methods
Analyses were performed from March to July 2023 using Stata, version 17.0 (StataCorp LLC) and Office Excel (Microsoft). Using mortality data from the National Center for Health Statistics, this cross-sectional study examines the association of changes in cause-specific mortality with changes in the gap in life expectancy at birth between men and women from 2010 to 2021, divided by pre– and post–COVID-19 years. We used a decomposition technique to partition changes in the life expectancy gap between men and women into component additive parts that identify the causes of death having the greatest assocation, positive or negative, with changes in life expectancy.3 Cause of death categories are based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. For further specificity, we partitioned changes in unintentional injuries into select components (unintentional poisoning [mostly drug overdose], unintentional transport-related injuries, and all other injuries). We estimated the differences between men and women in the age-adjusted death rates for the top causes of death associated with changes in the life expectancy gender gap. This study was exempt from review from the Harvard Longwood Campus institutional review board, and informed consent was not required because this study used deidentified data. This study followed the STROBE reporting guideline.
Results
The gender life expectancy gap increased 0.23 years from 2010 to 2019 and 0.70 years from 2019 to 2021. Prior to COVID-19 in 2020, the largest contributors to worsening life expectancy for men vs women were unintentional injuries (−0.23 years [−0.23246/−0.5116 = 45.4%]), diabetes (−0.05 years [10.1%]), suicide (−0.04 years [7.8%]), homicide (−0.03 years [5.3%]), and heart disease (−0.03 years [4.9%]) (Figure, A). This was offset by differential improvement for men vs women in mortality from cancer (0.12 years [43.1%]), Alzheimer disease (0.06 years [20.5%]), and chronic lower respiratory disease (0.04 years [12.3%]), among others.
From 2019 to 2021, COVID-19 became the leading contributor to the widening gender life expectancy gap (−0.33 years [39.8%]) followed by unintentional injuries (−0.27 years [32.5%]) (Figure, B). The increasing maternal deaths among women and the relative reductions in cancer and perinatal conditions among men partially mitigated the increasing gap (Figure, B). From 2010 to 2021, unintentional poisonings (mostly drug overdoses) and unintentional transport-related injuries contributed 0.44 (86.3%) and 0.06 (11.8%) of the 0.51-year decrease in life expectancy from unintentional injuries. The absolute difference in age-adjusted death rates between men and women increased from 252 to 315 per 100 000 between 2010 and 2021, with a persistent gap for heart disease and widening gaps for COVID-19, unintentional injuries, and several other causes (Table).

Discussion
This analysis finds that COVID-19 and the drug-overdose epidemic were major contributors to the widening gender gap in life expectancy in recent years. Men experienced higher COVID-19 death rates for likely multifactorial reasons, including higher burden of comorbidities and differences in health behaviors and socioeconomic factors, such as labor force participation, incarceration, and homelessness.4,5 Differentially worsening mortality from diabetes, heart disease, homicide, and suicide suggest that chronic metabolic disease and mental illness may also contribute. The increase in overdose deaths, homicide, and suicide underscore twin crises of deaths from despair and firearm violence.6 Limitations include binary gender classification and unexplored heterogeneity within disease classifications and across geographic and demographic subgroups. Future analyses could explore whether these trends changed after 2021, especially as the pandemic recedes, with further detail on specific causes.
==
Look at that COVID differential. Nobody talked about how the two greatest contributing factors to COVID death where obesity and being male.
Life is the greatest privilege of all.
Followed by the privilege of anyone caring about your wellbeing.
#men's health#life expectancy#suicide#COVID#drug overdose#heart disease#gender gap#female privilege#health#homelessness#homeless men#homeless#science#religion is a mental illness
9 notes
·
View notes
Text
Are European Baby Formulas *Really* Better Than Ones Made in the US?
I live my life by the Reddit Click Theory (something I just now invented on the spot), which states: the number of clicks it takes to get to a piece of information on Reddit is directly correlated with its status as a conspiracy theory. One click? You're probably safe. Five clicks? You're in anti-vaxxer territory. Anyway, as I Googled "best baby formula" to feed my twin boys, Reddit threads professing the life-altering magic of HiPP, Holle, Kendamil, and other European baby formulas kept rising to the top. Upon further research, it became clear that there is a fairly sizable faction of parents who prefer the standards of European Union baby formulas to American recipes.
"We dug into this trend in 2019, prior to the infant formula shortage," says Dina DiMaggio, MD, FAAP, medical research director at Bobbie Labs, an offshoot of the organic formula brand that supports research on infant feeding. "Our research, which focused on New York City-based parents, found that 20 percent of families were using illegally imported European infant formulas [bought through unregulated third-party websites]."
Parents who utilize EU formulas regularly cite that the EU has stricter standards for baby formulas than in the United States, with non-GMO, grass-fed dairy, and organic ingredients being frequently thrown around. If you look at third-party sites, this is echoed in the reviews, which bemoan the use of corn syrup, pesticides, and sugar levels in American formulas.
"The rise in this trend came while consumers were beginning to understand the difference between EU and US regulations in other product categories," says Dr. DiMaggio. "Just as people were taking a closer look at what was in the products they were purchasing for themselves, it's natural that they started to do the same for their babies."
What Are the Main Differences Between EU and US Formulas?
In scrutinizing labels, I found that both EU and US formulas contain the same key ingredients: a milk source (usually from cows; though sometimes sensitive formulas are made from goat's milk), lactose, vegetable oils, and whey protein. As with labels for personal care products, ingredients for baby formulas are listed with the ingredient that's in the largest quantity in the formula at the front of the label.
Related:
The Best Baby Formula of 2023, According to Reviewers
Largely, the differences between formulas can be attributed to requirements that the Food and Drug Administration - which regulates baby formula in the United States - sets for brands to meet versus what the EU requires its formulas to meet. "Both the FDA and European Union have specific and strict standards for infant formula with nutrient requirements and labeling laws," says Anthony Porto, MD, FAAP, MPH, Chief Medical Director at Bobbie Labs.
Let's take a closer look at where the regulating bodies' standards differ, shall we?
1. DHA
The EU requires DHA - an omega-3 fatty acid that plays an important structural role for brain, skin, and eye development - to be between 20 to 50 milligrams per 100 calories; however, the FDA and US formulas have no DHA requirement. Though, importantly, many formula companies in the U.S. still enhance their formulas with DHA.
2. Carb Sources
There are also differences in sugar in the varying formulas. "The EU also has a limit on how much of the carb source can come from an alternative sugar source other than lactose, which is the sugar found in breastmilk," says Dr. Porto.
3. Iron
Most US formulas include more iron than formulas made in Europe.This is because the FDA requires US formulas to meet certain requirements for the level of 30 nutrients, one of them being iron. Formulas in the US are fortified with iron at 12 mg/dL.
Okay, So What Should I Buy?
Which formula to buy for your babe is a deeply personal decision. "It's important to remember that both US and European formulas provide safe and healthy nutrition for… https://www.popsugar.com/family/european-vs-american-formula-49314493?utm_source=dlvr.it&utm_medium=tumblr
3 notes
·
View notes