Text

[Image Source]
2024 Responsible Breeding in Feline Medicine Position Statement
Shared from the American Association of Feline Practioners.
The AAFP supports the health and welfare of cats, placing overall wellbeing at the forefront of veterinary healthcare for every cat. In regard to the breeding of cats, the veterinarian has the ethical and moral responsibility to advocate for the welfare and comfort of the cat, independent of the breeder/caregiver’s desire for certain breed practices and standards or characteristics. The cat’s health, behavioral, and environmental needs are to be considered for the welfare and comfort of the cat.
As a consequence of selective breeding for appearance or other traits considered desirable, certain breeds of cats are at increased risk of pathology and poor wellbeing. The AAFP does not support the breeding of cats in which welfare is compromised or negatively impacted. Veterinarians should implement preventive genetic and health testing (eg, echocardiography screening for hypertrophic cardiomyopathy) as part of diagnostics to provide state-of-the-art healthcare. Genetic tests are widely available for certain diseases, as well as coat length, colors, and other traits in various cat breeds. With the help of genetic and other health screening, many inherited disorders in cats can be prevented and eradicated, and support precise and individualized veterinary healthcare.
The AAFP does not support breeding based solely on appearance when health concerns and feline welfare are not prioritized. While veterinarians will continue to provide appropriate healthcare for all cats, the AAFP does not condone the breeding of cats with inherent malformations, such as Scottish Folds and Manx, and any breed with severe brachycephaly or other compromised conformation. The AAFP encourages increased awareness of, and further research into, these breeds and their associated health issues to garner a better appreciation and understanding of the welfare impacts on these cats.
The AAFP strongly supports the Convention on International Trade in Endangered Species of Wild Fauna and Flora (CITES) and condemns the illegal importation of all wild felids. The AAFP opposes the breeding of wild felids (non-domestic cats) with domestic cats and discourages ownership of early-generation hybrid cats on the grounds of both animal welfare and public safety concerns.
[Read @ Source]
15 notes
·
View notes
Text

[Image Source]
Do I Need to Bathe My Cat?
Shared from Zoetis.
Dogs, people, and even birds get baths. Does that mean you should be bathing your cat, too? Not exactly. Read on to learn why most cats don't need the same grooming and bathing as other animals, when there are exceptions to that rule, and how you should approach bathing your cat when it's necessary.
Do Cats Really Need Baths?
In most cases, no, you really don't need to give your cat a bath. Cats do an extremely good job of keeping themselves clean and their coat and skin benefit from natural oils you don't want to wash away. However, there are times when it may be helpful or even necessary to bathe your cat.
As cats get older, or if they have physical limitations, they may be less able to self-groom.
Some longhair breeds may need bathing to keep fur from matting, like Persians, Himalayans, and Ragdolls.
Cats with specific skin conditions may need baths to soothe or treat the skin.
If your cat gets into something they shouldn't ingest, you'll want to bathe them for safety reasons to remove any residue from their coats.
If your cat picks up bugs in their fur (like fleas, ticks, mites, or lice) bathing — and medical treatment — may help prevent irritation, infection, and disease.
There may be litter box incidents or other messy situations that need a little clean-up.
Even if your cat needs a bath, it's important to remember that a cat's scent is extremely important. Bathing not only diminishes it but may even cloud it with the scent of the bath products you use (which can be stressful for your cat). Use unscented shampoo — if you can smell it, your cat can really smell it!
Can You Teach a Cat to Like Being Bathed?
Sure, it's possible (it’s not a bad idea to try and get them comfortable with water, even if you don't ever plan on bathing them, as you never know when a water situation may come up that you can't avoid). Forcing a cat into water against their will can be traumatizing to them and dangerous for you, so they need to be desensitized to the process very slowly.
Start with a very small amount of lukewarm water — maybe just half an inch at the front of the tub. You might even start with a slow drizzle of water in the sink and work up to the bathtub over time.
Make sure they have something stable to stand on (like a rubber mat) so they aren't sliding around.
Have their favorite treats handy.
Use tiny steps to take them from being near the water, to dipping a paw in, to standing in the water, to letting you sprinkle water over them, and so on until you can bathe them properly.
Use toys and treats to lure and guide them throughout the process (and take your time).
Giving treats will help build positive associations and give them a reason to stick around.
The key is giving the cat control over the situation. Anytime a cat is forced to do something, they automatically go into defensive mode. They aren't choosing what's happening and, therefore, don't know if it's safe.
How to Bathe a Cat
When your cat is comfortable with water (by following the steps above), you can bathe them as needed.
Plan ahead and have your tools ready to go so you can move quickly through the process. You'll need:
A bathtub, sink, or large bin to hold water
A non-slip surface to set in the water (like a rubber mat)
Cat shampoo (unscented and hypoallergenic if possible)
A towel
A pet-specific air dryer or human hair dryer on low heat, low airflow (only if you've carefully desensitized your cat to drying)
Lots of treats
To bathe your cat, you'll use the same process you did to get them used to the water.
Add a couple of inches of water to the tub or basin.
If possible, use your treats or toys to lure them onto the non-slip surface.
Gently get their fur wet using your hands, a cup, or a pet water wand if they've been desensitized to it.
Add a small amount of shampoo to the body.
Be careful around eyes that may be sensitive and ears to avoid trapping water that could cause an ear infection or discomfort. If you get shampoo in your cat’s eyes, rinse them out with cool water or saline eyewash. Keep a cat-appropriate ear cleaner on hand to rinse out any water that gets in their ears.
Thoroughly rinse your cat using the same method you did to wet their fur.
Make sure all shampoo is removed.
If you're using a conditioner, follow the manufacturer's instructions.
iDry your cat as well as possible with a towel.
You can use an air dryer only on the lowest possible setting and if they’ve been slowly desensitized to it.
Throughout the process, especially at the end, give your cat lots of treats and verbal praise.
Alternatives to Bathing Your Cat
A cat bath doesn't have to mean they're fully submerged in water — a wet cloth may be all you need for some situations. There are also cat-specific cleansing cloths on the market, which are great for dirty spots like feet or the backend, as well as a light all-over wipe down after a roll in the dirt. Cat-appropriate waterless shampoo can also be helpful to break up fur soiling before wiping. Make sure any product you’re using is designed specifically for cats, as human products should not be used unless directed by your veterinarian.
[Read Article @ Source]
26 notes
·
View notes
Text
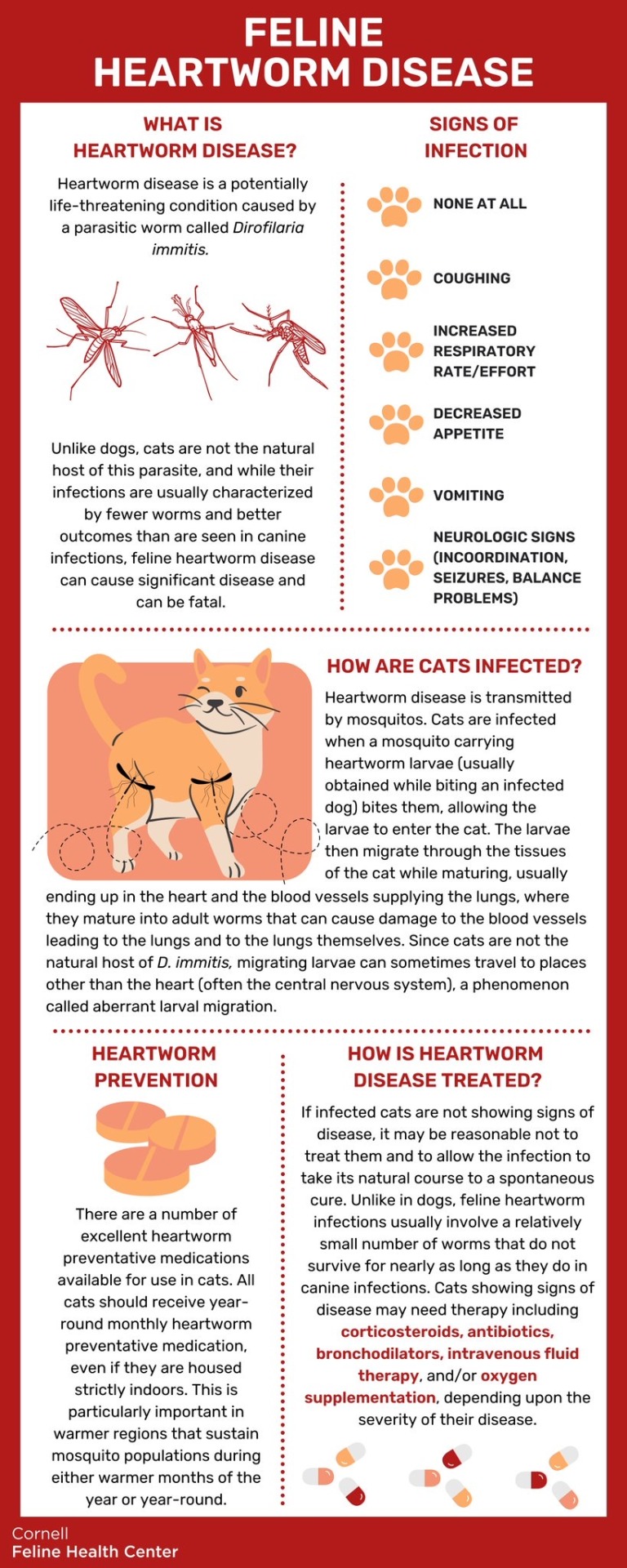
Heartworm in Cats
Shared from Cornell Feline Health Center.
Among all of the various disorders that can endanger a cat’s physical well-being and perhaps threaten its life, few are more insidious than feline heartworm disease, a potentially life-threatening condition that occurs when a parasitic worm called Dirofilaria immitis gets into an animal’s system. And the only way in which this worm can enter your cat’s body is through a mosquito bite.
The infection occurs when a mosquito pierces a cat’s skin and, in so doing, allows entry of heartworm larvae that it has picked up from another animal, most commonly an infected dog, into the victim’s bloodstream. Over time (typically about eight months) these larvae thrive and develop in the bitten cat’s body, initially in the subcutaneous tissues directly beneath the skin, then in the muscle tissues and eventually in the right ventricle of the animal’s heart, in its lungs and in the arteries associated with those vital organs.
But the worms can cause problems before they are fully grown, says Dwight Bowman, DVM, PhD, a professor of parasitology at Cornell University’s College of Veterinary Medicine. “Between 60 and 100 days after the initial infection,” he says, “you can start to see signs of pathology in an affected animal’s body, even though the parasite has not yet reached maturity.” The immature worms’ arrival into the small arteries in the lungs initiates a severe inflammatory response that damages not only the arteries, but also the bronchioles (small airways) and alveoli (air sacs where gas exchange in the lungs takes place).
Furthermore, he points out, although the name of the disease suggests that the disorder mainly affects the heart, the mature parasite eventually resides, for the most part, not in the heart, but in the pulmonary arteries, which carry blood from the heart to the lungs. And in the cat, the disease primarily affects the lungs, not just the heart. Veterinary scientists have coined a new term—heartworm associated respiratory disease, or HARD—to describe the lung disease that heartworms cause. For additional information about HARD and feline heartworm disease, see Know Heartworms' website.
Severe Damage
The various disorders brought about by heartworm infection are in part attributable to the impressive size of the parasite—white, spaghetti-like creatures that can grow to be nearly a foot long—and to the inflammatory response that immature and dying adult worms induce. In an advanced infection, especially in dogs, the worms damage the walls of the pulmonary arteries and impede the passage of blood through them, which results in excessive strain on the heart as it attempts to pump blood through those packed vessels.
In some cats, a heartworm infection may disappear spontaneously, possibly because an animal has developed an immune response that is sufficiently strong to kill the parasite. The immune response itself, though, is believed to cause many of the signs commonly seen in feline heartworm disease. In most cases, the infection will progress steadily, with nonspecific clinical signs that may mimic the indications of many other feline diseases.
Signs of Infection
The most common clinical signs of heartworm infection include: intermittent vomiting (sometimes of blood as well as of food); diarrhea; rapid and difficult breathing, coughing and gagging, all of which may be confused with feline asthma or some other bronchial disease; loss of appetite; lethargy and weight loss. In some cases, a cat may survive a heartworm infection for an extended period of time before succumbing to another feline disorder. In an acute case of the disease, a cat may die suddenly. “In any case,” says Dr. Bowman, “the prognosis is not good. Heartworm disease is not something that you want your cat to get.”
Diagnosing feline heartworm disease will typically involve a complete blood count and blood chemistry profile, chest X-rays, a test to determine whether the patient’s blood contains antibodies to the parasite and a test to see whether adult heartworm proteins are present in the blood. In addition, ultrasound imaging may be able to visually reveal the presence of heartworms in the heart or pulmonary vessels.
Unfortunately, says Dr. Bowman, heartworm disease in cats—unlike the condition in dogs—is untreatable. The powerful substances that are regularly used to rid a dog of the infection, he explains, can be fatal to a cat.
Treatment Options
Most cats that are diagnosed with heartworm infection but are not showing severe clinical signs will be monitored to see whether the condition might resolve itself spontaneously.
Cases where there is evidence of disease in the lungs and associated blood vessels can be monitored with periodic chest X-rays. Supportive therapy with small, gradually decreasing doses of prednisone is recommended for cats with clinically confirmed evidence of lung disease.
Cats with clearly apparent signs of heartworm disease may require additional supportive treatment in the form of intravenous fluids, oxygen therapy, cardiovascular drugs and antibiotics.
Protective Measures
The key to providing year-round protection against feline heartworm disease—especially in the warm, muggy sections of the U.S. where mosquitoes proliferate—is the routine administration of such preventive medications as selamectin, milbemycin and ivermectin to all cats in a household. “With the approval of their veterinarians,” says Dr. Bowman, “all cats should definitely be given these medications.”
Cat owners can obtain additional information regarding this all-too-common feline disease by contacting the American Heartworm Society.
[Read Article @ Source]
30 notes
·
View notes
Note
Do you consider brachycephalism in cats as serious as in dogs? I'm in veterinary medicine but I don't encounter many brachy kitties and would love to hear your thoughts on it.
Brachycephaly is a problem.
Schlueter et al (2009) categorized brachycephalic head shapes into four categories randing from mild to severe.
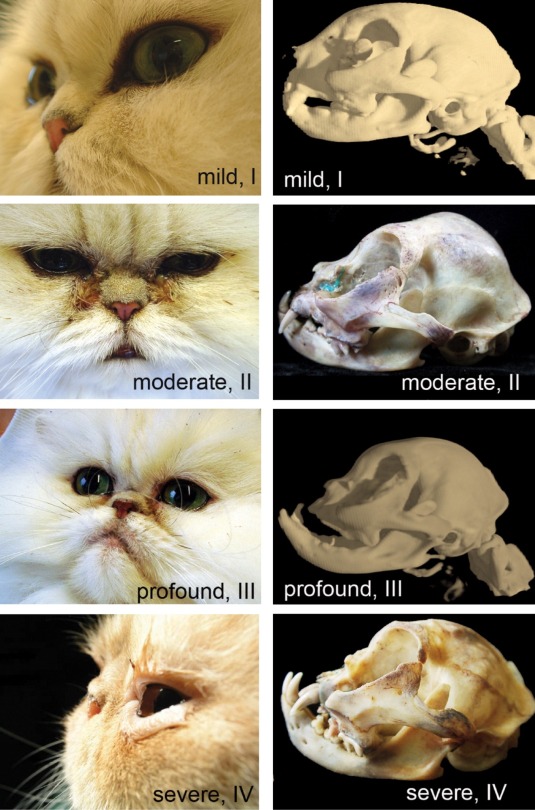
Moderate brachycephaly is where we begin to really see problems and profound or severe brachycephalic cats are going to have a real issue.


The British Shorthair (left) is a breed where mild brachycephaly is part of the standard compared to an Exotic Shorthair (right) where profound - severe brachycephaly is desireable.



On the left with have a British Shorthair, in the center an Exotic Shorthair and on the right a Persian.
One of the problems we see with brachycephalic breeds is stenotic nares, which are narrow nostrils. You can’t even make out the nares on the Persian shown above and, as one may expect, this affects how much air they move through them.
We can see similar obstructive effects in cats with nasopharyngeal polyps, masses or reconstruction due to scarring from chronic rhinosinusitis problems.
Due to their inability to breath normally through their nose these cats tend to be heat and exercise intolerant and can run into trouble more quickly during high stress events.
Stenotic nares can be surgically corrected but I don’t think this is as common in cats as it is in dogs, at least I haven’t encountered many cats who’ve undergone the procedure. I don’t know if it’s not as necessary, if cats don’t respond as well or if cat owners are less likely to seek treatment.
Or maybe it is as common and my lack of experience is the outlier.
Brachycephaly is also associated with malocclusion and dental disease, chronic epiphora, facial dermatitis related to the chronic tearing and ocular issues such as conreal sequestrum or entropion related to the protruding eye structure.
I know globe proptopsis is a problem in some brachycephalic dog breeds like pugs but I haven’t heard of this specifically happening in brachycephalic cat breeds.
Exotics and Persians are obviously the worst when it comes to brachycephaly in cats but the Bombay and (American) Burmese are also offenders.
There are other breeds which don’t call for a brachycephalic head shape (or even default it) or call for only a mild version but certain breeders are selecting for extreme typeing anyways because even though their cats might not win any shows they can sell them as designer variants for more.


On the left we have a Sphynx and in the right we have a Devon Rex both with an extreme head type contradictory to the breed standard.
So yes, unfortunately the brachycephalic head type is a problem in cats. Some try to argue that brachycephalic animals often live long lives which means the abnormal structure isn’t a problem… but longevity is only one measure of a breeds ethical soundness, quality of life and history are also important in my opinon.
2K notes
·
View notes
Text

[Image Source]
Crisfield Raccoon Tests Positive for Rabies After Fighting with Dog [WBOC]
The Somerset County Health Department says a raccoon has tested positive in Crisfield after the animal was collected following a fight with a dog.
According to the Health Department, the raccoon was taken for testing on Friday, April 12th after the incident with the dog. A positive rabies result was received on Monday, April 15th.
Rabies is 100% fatal if left untreated, the Health Department says, and neighbors are advised to take the following precautions to avoid exposure to the virus:
Report any sick or strange acting wildlife.
Vaccinate pets and livestock. Maryland law requires that all dogs, cats and ferrets be vaccinated against rabies by four months of age. Vaccinating your domestic animal not only provides protection for the animal, but vaccinated pets act as a barrier to keep the rabies virus from spreading between wild animals and people.
Do not feed wildlife or stray animals and discourage them from seeking food near your home.
Do not approach an unknown animal, either wild or domestic, especially if it is acting in a strange or unusual manner.
Keep garbage cans tightly covered and avoid storing any food outside.
Instruct children to tell an adult immediately if they were bitten or scratched by any animal.
If an unvaccinated pet comes in contact with rabid or suspected rabies the pet must be quarantined for four months.
Vaccinated pets that come in contact with rabid or suspected rabid animals must be given a booster rabies vaccination within five days of the contact.
[Read Article @ Source]
31 notes
·
View notes
Text

Do You Know Which Flowers and Plants are Toxic to Pets? Our Experts Explain!
Shared from the ASPCA.
Toxic Plants:
Lilies: Lilies from the Lilium or Hemerocallis species can be lethal to cats. To avoid injury or illness, keep these flowers out of your home and carefully research any bouquets that may have lilies hiding in the assortments. Even small exposures to pollen from these flowers can cause kidney failure or even death in cats.
The following are a few common and botanical names of toxic lily plants:
Easter Lily (Lilium longiflorum)
Japanese Lily (Lillium speciosum)
Oriental Lily Hybrids (Lilium spp.)
Stargazer Lily (Lilium orientalis ‘Stargazer’)
Casa Blanca Lily (Lilium orientalis ‘Casa Blanca’)
Tiger Lily (Lilium lancifolium)
Daylilies (Hemerocallis spp.)
Sago Palms (Cycas revoluta): Sago palms are common household and landscaping plants that unfortunately carry very serious consequences to dogs and cats with even small exposures. Primary concerns with ingestion include severe stomach upset, liver damage, low blood sugar and bleeding issues, which can progress to seizures and death. All parts of the plant are toxic, with the seeds being most concentrated and dangerous.
Tulips (Tulipa spp.): Tulips and tulip bulbs are toxic to dogs, cats and horses. They can cause significant stomach upset, depression and possible intestinal obstructions if large bulbs are ingested.
Oleander (Nerium oleander): Oleander are beautiful flowering shrubs often used in landscaping, but for dogs, cats and horses, they carry the risk of causing serious heart problems — including arrythmias and low blood pressure — when ingested, which can be life threatening. Symptoms can be delayed after exposure and stomach upset – including vomiting, diarrhea and pain – is often seen prior to abnormalities with heart function.
Autumn Crocus (Colchicum autumnale): Autumn crocuses are often mistaken as other types of crocuses, but the autumn crocus is important to differentiate as it’s extremely toxic to dogs, cats and horses with even small ingestions. Toxicity from the autumn crocus can cause severe stomach upset, heart problems (arrythmias, low blood pressure), liver failure, kidney failure and issues with abnormal bleeding and bone marrow function.
Non-Toxic Flowers and Plants:
Flowers
Roses – Rosa spp.
Sunflowers – Helianthus spp.
Zinnia – Zinnia elegans
Gerber Daisy – Gerbera spp.
Snapdragons – Antirrhinum spp.
Orchids – Orchidaceae
Asters – Symphyotrichum spp.
Statice – Limonium spp.
Freesia – Freesia spp.
Wax Flower – Chamelaucium spp.
Safe Plants
Petunia – Petunia spp.
African Violet – Streptocarpus sect. Saintpaulia
Easter Cactus - Rhipsalidopsis gaertneri
Hens and Chicks - Sempervivum tectorum
Friendship Plant - Pilea involucrata
Boston Fern - Nephrolepis exaltata
Spider Plant - Chlorophytum comosum
Zebra Haworthia - Haworthiopsis attenuate
For more information and resources on toxic and non-toxic plants, see the ASPCA Animal Poison Control Center’s full list of poisonous plants.
If you have any reason to suspect your pet has ingested something toxic, please contact your veterinarian or the ASPCA Animal Poison Control Center’s 24-hour hotline at (888) 426-4435.
[Read Article @ Source]
41 notes
·
View notes
Text

[Image Source]
Orally Administered Gabapentin and Alprazolam Induce Comparable Levels of Anxiolysis and Sedation in Cats
Objective
To assess the level of anxiolysis achieved by alprazolam and gabapentin in hospitalized cats prior to elective ovariohysterectomy and to evaluate the sedative effects of these agents.
Animals
60 client-owned female cats classified as American Society of Anesthesiologists physical status 1, admitted for elective ovariohysterectomy at a veterinary teaching hospital.
Methods
The cats were prospectively and randomly allocated into 3 groups. Ninety minutes before evaluation, group G received gabapentin (100 mg/cat), group A received alprazolam (0.125 mg/cat), and group P received no medication (placebo). Stress, enclosure activity, and sedation scores were blindly evaluated.
Results
Stress scores were similar in cats treated with gabapentin and alprazolam and gabapentin-treated cats had significantly lower stress score than those of the placebo group. Enclosure activity levels did not differ among the groups. Additionally, gabapentin and alprazolam resulted in similar sedation levels 90 minutes after treatment, which differed significantly compared to placebo.
Clinical Relevance
The results of this study suggest that gabapentin provides similar anxiolysis in cats to that of alprazolam when evaluated 90 minutes after administration. Although no difference was noted in sedation levels between gabapentin and alprazolam, both induced deeper sedation than placebo.
[Read Full Study]
8 notes
·
View notes
Text
Things are heating up in the feral cat fandom 👀
By which I mean the local TNR scene. It’s absolutely insane so of course I’m gonna share the tea here for you all.
Discussion of animal death and such below cut.
So Person A is very well known in the rescue community, A is a major TNR advocate and does a lot of work with rescue and transport and whatnot. A has a major social media following, I’m talking double digit thousands, with enough influence that they’ve effected local legislation.
Then there’s Person B who is also involved in the rescue community but in a less hands on way, B moderates a huge amount of groups and pages pertaining to missing pets, rescue and the sort.
For whatever reason B has beef with A, and truthfully there are a lot of reasons that could be. If you haven’t figured it out A is a very beefable person.
As is B’s right to curate their online space and experience B has A blocked, meaning A is unable to view or interact with B’s groups or receiving notifications of people pinging them in B’s groups even if they’re public.
Person C posted in one of B’s groups about a very ill cat who they weren’t able to take for one reason or another. This cat was in bad shape, honestly I expect this cat was beyond help aside from helping them to pass peacefully. It was clear from the images and videos shared that this cat was done, on the cusp of dying if not actively doing so.
This cat wound up passing away before anyone could get to them.
Person A made a post on their page with many, many followers labeling B as a cat killer for blocking A from their groups, because if B hadn’t blocked A then A could have seen the post about the sick/dying cat and could have helped.
Because of the disingenuous wording on A’s post people are thinking B is directly involved with the cats death in one way or another - actively maimed or killed the cat, deliberately blocked help attempts, neglect, whatever. Everyone seems to be drawing their own conclusions which A isn’t correcting.
People are calling for B to be reported, to be arrested. People are spamming B’s pages, sending B nasty messages, etc.
As if this isn’t nonsense enough…
People were trying to help the cat.
People far more local than A. Person C wasn’t answering or giving clear directions so the multiple people who offered help were left floundering until the cat had passed on their own, at which point they were able to locate the body.
These people are fucking nuts. Thought you’d all want to cringe at this with me.
39 notes
·
View notes
Text

Shared from Cat Friendly Homes
⚠️ Emergencies happen when you least expect it ⚠️
If your cat has been injured or is experiencing a medical emergency, call your veterinarian before you attempt any type of first aid. Always make sure to speak with your veterinarian and/or with a poison control specialist before starting any therapies at home. Never administer any over-the-counter human medications to cats without speaking to a veterinary professional first.
Assembling a Pet First Aid Kit
Here are some basic things you should have prepared in case of an emergency with your cat.
Emergency Contact Information
Create a notebook or index card with important phone numbers and addresses. Store it in sealable sandwich bag to keep dry.
Make sure to include the following information:
Primary veterinary clinic
Closest emergency-veterinary clinic (include directions)
Pet Poison Helpline: petpoisonhelpline.com (1-800-213-6680)
Microchip ID number and company phone number
First aid book
Current vaccination records, especially proof of rabies vaccination
Current list of medications; include name, dosage, and frequency
Current medical records including any conditions or diseases, as well as treatment plans
List of temporary evacuation centers/shelters that are pet friendly
First Aid Kit
Use a sealable waterproof container like a toolbox or hard covered lunch box to contain all of your first aid supplies.
The First Aid Kit Should Contain:
Non-latex gloves
Gauze or other absorbent material and an outer protective bandage layer
Artificial tears or other sterile ophthalmic drops
Non-adherent pads such as Telfa pads
Adhesive tape for the bandages
Bandage scissors
Antibiotic ointment
Water-based lubricant, such as K-Y jelly, to protect open wounds
Eyedropper or syringe without a needle to clean wounds
Cotton balls or cotton swabs
Tweezers
Magnifying glass
Flashlight
Cold pack/chemical hot pack
Liquid dishwashing detergent for oil or another contaminant exposure
Muzzle or other method of protecting caregivers from bite risk when a cat is in pain or frightened by accident
Basic Transportation Supplies
Items You Should Have So You Can Safely Transport Your Cat in An Emergency Situation:
Secure carrier (we recommend you choose a hard-sided carrier that opens from the top and front)
Collar with tags
Leash (if your cat has been trained and is comfortable with it)
Large towel/blanket to assist in moving an injured or sick pet, or to cover a frightened or anxious animal
Bedding for carrier
For more suggestions about how to create a pet first aid kit, visit the Pet Poison Helpline resources.
[Read Article @ Source]
40 notes
·
View notes
Text
On a less grim note everytime I hear the word “community cat” I vomit in my mouth a little.
#like not even related to how i feel about tnr#im trying to figure out how to word this#it sanitizes the issue and reduces urgency in dealing with it#and it rarely reflects the feelings of the community at large#just call them a colony cat or a feral cat
46 notes
·
View notes
Text

[Image Source]
Prevalence of Otitis Externa in Stray Cats in Northern Italy
Feline otitis externa is a dermatological disorder that has not been evaluated much in stray cats. One hundred and eighty-seven stray cats were randomly selected during a trap–neuter–release programme to investigate the prevalence of otitis externa in stray cat colonies in northern Italy. Swabs for cytological examination were obtained from the external ear canal of each cat. A direct otoscopic assessment of the external ear canal was made in 86/187 cats. Cytological evidence of otitis externa was present in 55.1% of cats. The influence on otitis of age, gender, habitat and season of sampling was tested, but no risk factors were found. Otodectes cynotis (as a sole agent or in combination) was the primary cause of otitis in 53.3% of cats. Cocci and rods, either alone or in combination with other agents, were perpetuating factors in 71.8% and 29.1% of cats, respectively. Pregnancy status was a risk factor for otitis caused by coccal infections. Malassezia species, alone or in combination, was the perpetuating factor in 50.5% of cats with otitis. Urban habitat and winter season were risk factors for otitis associated with Malassezia species. Demodex cati was identified as an incidental finding in two cats. There was good agreement between otoscopy and cytology with regard to the diagnosis of otitis externa. The results of this study show a high prevalence of otitis externa in stray colony cats and provide information on causal factors for feline otitis externa.
[Read Full Study]
4 notes
·
View notes
Text
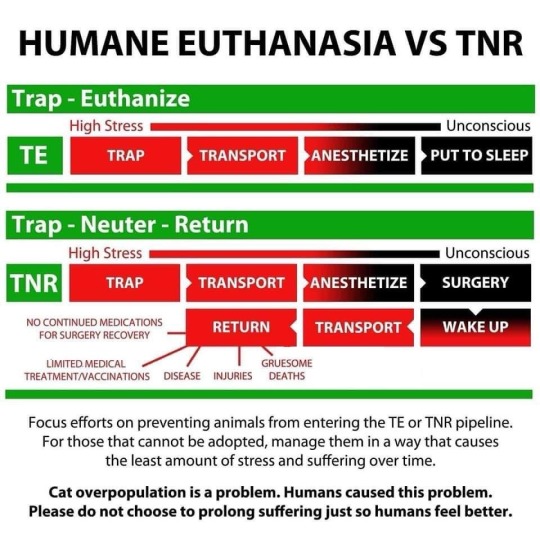
I wish I could say my opposition to TNR stems from my concern for the environment. I wish I could say I set aside my love for cats to see the bigger picture of the ecological damage they cause and made the difficult decision to no longer support an insufficient system of management.
And of course this is a factor, of course the environment and the impact feral and outdoor cats have on it is of great concern to me…
But it would be a lie to claim that as my primary, driving factor. The main reason I don’t support TNR is because I hate to see cats suffer. The things that these poor animals endure and so pointlessly, so preventably…
A cat is found with a flacid tail and dragging a knuckled over paw.
A cat is found with grievous injuries to the back and tail from a dog or other animal attack. The cat self-amputates the tail. Tail injuries that involve degloving and amputation are pretty common.
A cat is struck by a car, not only amputating the tail and lower portion of a limb but fully degloving the remaining portion of the leg. The cat is alive when found in this state.
A cat is found with a wound on the neck consistent with a ruptured abscess. Either unnoticed or unable to treat in a timely manner it becomes infected and then necrotic. Ruptured abscesses resulting in full thickness wounds exposing muscle are not uncommon.
A cat is struck by a car resulting in a fracture to the hard palate, skull and jaw as well as both eyes popped out. The cat is alive when found in this state. This kind of injury is common in hit by car cases, although most don’t survive - most of the cats I peel off the road present similarly.
A cat is found with the flesh and meat fully removed from the lower portion of a hind limb, having become necrotic and the decaying flesh feasted on by maggots. The skeletal remains of the paw are still attached. I would not say this is “common” but the frequency that I see this is alarming.
A cat is found functionally scalped, exposing portions of the skull. Perhaps due to an animal attack or perhaps due to being hit by a car. I’ve actually seen reports of this happen on at least two seperate occasions? As with other cases the cats were found alive in that condition.
A cat is noticed to be very ill. The cat has previously been trapped as part of a TNR program and is now trapped savvy and cautious of usual means. When the cat is finally captured their condition has deteriorated to the point where they passed away shortly after.
These are all examples I have personally encountered or have seen shared by the various rescue groups I follow on Facebook and Instagram. Often accompanied by gruesome pictures which I’m choosing not to include in this post.
As stated a lot of these aren’t isolated incidents. I see rescues from all over share similar cases entirely unrelated to each other, likely unaware of the matching case(s) experienced in rescues across the country or in other countries.
And I just can’t see this as humane.
These cats are not socialized, they are afraid of humans and handling them is incredibly stressful. Oftentimes euthanasia is the only option because these cats cannot realistically be handled for ongoing treatment.
The end result of euthanasia is the same, the only difference is the amount of pain and suffering endured between first trapping and eventual euthanasia.
And the cat doesn’t know you’re trying to help them, all they know is that they’re already hurting and that they’re vulnerable because of their injury or illness and now this giant creature who may or may not want to eat them has them trapped and is dragging them to strange, bad smelling places to be poked and prodded by more creatures.
It makes me sick to think about. I get so worked up because it isn’t like the worst case scenario is a scrape or stubbed toe, these are massive and grievous injuries that must be extremely painful… and there is no reason to allow them to occur. There is no reason for suffering to predate peace just so people can pat themselves on the back and feel like they did something.
57 notes
·
View notes
Text

[Image Source]
Physical Examination and CT to Assess Thoracic Injury in 137 Cats Presented to UK Referral Hospitals After Trauma
Results
In total, 137 cats were included. Road traffic accidents (RTAs) were the most frequently reported cause of trauma (69%). Tachypnoea (32%), pale mucous membranes (22%) and dyspnoea (20%) were the most common abnormal findings on thoracic examination. The most frequently identified thoracic pathologies on TCT were atelectasis (34%), pulmonary contusions (33%), pneumothorax (29%) and pleural effusion (20%). Thoracocentesis was the most commonly performed intervention (12%), followed by chest drain placement (7%). A total of 45 (33%) cats had no physical examination abnormalities but did have abnormalities detected on TCT; six of these cats required interventions. Increasing numbers of thoracic abnormalities on clinical examination were associated with increasing likelihood of having abnormal findings on TCT (odds ratio [OR] 2.04, 95% confidence interval [CI] 1.21–3.44, P = 0.008) and of requiring an intervention (OR 1.82, 95% CI 1.32–2.51, P <0.001).
Conclusions and Relevance
RTAs were the most common reported cause of blunt trauma. Atelectasis, pulmonary contusions and pneumothorax were the most common abnormalities identified on TCT, and thoracic drainage was the most utilised intervention. TCT may be useful in identifying cats with normal thoracic physical examination findings that have significant thoracic pathology, and a high number of abnormal findings on thoracic examination should raise suspicion for both minor and major thoracic pathology. The results of this study can be used to assist in selecting appropriate cases for TCT after blunt trauma.
[Read Full Study]
8 notes
·
View notes
Text

[Image Source]
Stray Cat in Watertown Tests Positive for Rabies [NCPR]
A stray cat in Watertown has tested positive for rabies.
The Jefferson County Public Health Service said a member of the public took in a stray that had a visible wound. They took the cat to the vet and then brought it home. It developed symptoms of rabies, went back to the vet's office and died.
The county says there aren’t any known pet exposures. But three people are known to have been exposed to the rabies infection.
Rabies is a fatal disease that attacks the brain and spinal cord. Symptoms can take weeks or months to appear. Any mammal can contract rabies, but it’s most often seen in bats, raccoons, skunks and foxes. Early treatment for humans who are exposed can prevent the disease.
"Animals do not have to be aggressive or behave erratically to have rabies. Changes in any animal’s normal behavior can be early signs of rabies," reads a press release from Jefferson County's public health department.
Health officials say there have been rabies cases across Jefferson County and to avoid contact with any unfamiliar animals.
Officials say to remove pet food from outside your home that would attract wild animals and to keep your own pet’s vaccinations up to date.
Jefferson County Public Health is hosting a rabies vaccination clinic on March 21 at the county's dog control.
[Read Article @ Source]
51 notes
·
View notes
Text

How Do I Know If My Cat Is In Pain?
Shared from Cat Friendly Homes
Behavior changes in your cat are the primary indicator of pain. As the person who knows your cat best, you are an important member of their healthcare team and key in helping to detect the signs of pain as soon as possible. The signs of pain may be subtle because cats hide signs of discomfort and illness which could make them appear vulnerable to their enemies. This trait comes from their wild ancestors who needed to avoid becoming another animal’s prey. This can make it difficult to recognize if your cat is sick or in pain. Veterinary professionals have been trained to evaluate these subtle behaviors and physical health changes.
Categories of Pain
Acute Pain
This type of pain occurs in conjunction with inflammation and healing after an injury and can last for up to 3 months. It can be caused by injury, trauma, surgery, and acute medical conditions and diseases. Acute pain generally begins suddenly and usually doesn’t last long.
Chronic Pain
This is usually described as either pain that lasts beyond the normal healing time or pain that lasts in conditions where healing has not or will not occur. Degenerative joint disease (DJD), also known as feline arthritis, is an extremely common, chronic, painful disease in cats, with as many as 92% of all cats showing some signs of this disease. It is also one of the most significant and under-diagnosed diseases in cats.
Persistent Pain
Cats with persistent pain may need palliative care. Palliative care is the all-encompassing approach that provides cats, who have a disease that is not responsive to curative treatment, with a plan to provide an improved quality of life with pain control being the principal feature.
During regular checkups, your veterinarian talks with you about your cat and obtains a patient history. Regular checkups should occur a minimum of once yearly, and more frequently for senior cats and those with chronic conditions. So, when you notice changes in how your cat is behaving, interacting, or his daily routine, contact your veterinarian.
Signs and Symptoms
It is important for you to know your cat’s normal temperament and behavior. Just the slightest change could be a sign that your cat is sick or in pain. Since your cat is nonverbal and can’t tell you he is in pain, your veterinarian relies on you to determine if there are any abnormal behavior patterns that may be pain-related. If your cat displays any of the following changes, contact your veterinarian immediately.
Decreased appetite or no interest in food
Withdrawn or hiding
Reduced movement or mobility, or hesitation to climb steps or jump
Diminished exercise tolerance and general activity
Difficulty getting up, standing, or walking
Decreased grooming
Changes in urination or defecation habits
Squinting
Hunched or tucked-up position instead of curled-up when sleeping
Sensitivity or vocalization to petting or touch
Temperament or other substantial behavior changes for your cat (e.g., seeking solitude, aggression, loss of appetite)
Management of Your Cat’s Pain
Your cat’s pain management plan that you develop with your veterinarian may include:
Medication
Physical Therapy
Environmental changes such as using special bedding or ramps
Your veterinarian is committed to developing a strategy with you that provides your cat with compassionate care; optimum recovery from illness, injury, or surgery; and enhanced quality of life.
Monitoring
Once a veterinary plan has been developed, you may be asked to monitor your cat at home. It is important that you receive verbal instructions, written instructions, and ask for a hands-on demonstration of how to administer medications and handle your cat at home.
When you are monitoring your cat at home, we recommend that you:
Use a notebook to record your observations.
Include any changes in behavior, activities, or routine even if they seem minor.
Schedule follow-up appointments with your veterinarian to share your observations.
Alert your veterinary practice right away if there are changes, you have questions, or you notice early signs of adverse reactions.
Continuous management is required for chronically painful conditions, and for acute conditions until the pain is resolved. When pain is not recognized or managed, it can result in what may be considered unfavorable behavior changes.
Please remember – cats do not act out of spite, and any behavior change can be a sign of pain or another health problem. Being able to recognize and manage your cat’s pain can be as life-preserving as any other veterinary medical treatment.
[Read Article @ Source]
39 notes
·
View notes
Text

[Image Source]
Mercury Mystery: Poisonous Element Persists in Tuna [BBC]
Levels of mercury persist in tuna, decades after pollution controls were introduced to limit emissions, scientists say.
The poisonous element is released by mining and burning coal and ends up in the ocean, where it builds up in fish.
Levels have fallen dramatically in the atmosphere - but remained stable in tuna since 1971.
Very old mercury lurks deep in the ocean and wells up into the waters where the tuna swim, experts say.
Mercury entering marine ecosystems is converted into methylmercury, the most dangerous form of the chemical.
It builds up in tuna when they consume contaminated prey.
And humans are then exposed to the element when they eat the fish, one of the most widely consumed around the world.
Mercury poses a particular threat to unborn babies and small children but has also been linked to cardiovascular disease in adults.
Concerns over exposure to mercury have seen governments the world over try to reduce activities that released the chemical into the atmosphere.
The major sources include:
Coal and Gold Mining
Coal Burning
Industry
Waste Processing
Even the cremation of human bodies with amalgam fillings adds to the total in the air.
Restrictions on many of these activities have seen emissions levels in the atmosphere fall by about 90% since 1990.
And to see if these actions had had an impact on mercury levels in tuna, researchers examined data from nearly 3,000 tuna muscle samples, from fish captured in the Pacific, Atlantic and Indian Oceans, including skipjack, bigeye and yellowfin, which together account for 94% of global tuna catches.
The new work contrasts with other research showing levels of mercury declining in some tuna species.
"We have much more data, more sampling years, and also a broader range of fish sizes," lead author Anaïs Médieu, from the French National Research Institute for Sustainable Development, said.
"This is very important because mercury bio-accumulates during the [lifespan] of the animal. So having a broad range of fish sizes is really important."
Mercury levels in tuna had remained constant between 1971 and 2022, the scientists found, apart from an increase in the north-western Pacific, in the late 1990s, linked to growing mercury emissions in Asia, sparked by rising coal consumption for energy.
The constant levels may be caused by emissions many decades or centuries ago, the researchers said.
"You have this huge amount of legacy mercury that is in the deeper subsurface ocean," Ms Médieu said.
"This mixes with the surface ocean, where the tuna swim when they feed.
"That's why you have a continuous supply of this historic mercury that was emitted decades or centuries ago."
'Stabilise Slowly'
Co-author Anne Lorrain, also from from the French National Research Institute for Sustainable Development, told BBC News: "Our study suggests that we will need massive mercury emissions reductions to see a decrease in tuna mercury levels.
"Even with massive reduction in mercury emissions, our results show that we will have to be patient before seeing a change in tuna mercury levels.
"Overall, it is similar to CO2 [carbon-dioxide] emissions - if we stop emitting drastically, CO2 in the atmosphere will stabilise slowly and finally start to decline. "
The study has been published in the journal Environmental Science & Technology Letters.
[Read Article @ Source]
25 notes
·
View notes