Text
So it’s been a hot few minutes months since I posted and now a double update on my recent chaos-filled escapades is probably in order (since I’ve done 2x placements without update, including my beloved O&G). But since I am shattered today from a ludicrously long op, until then I wanted to highlight the pure gold that is Geeky Medics’ Theatre Etiquette:

(There is a fourth historical reason, which is fear of static discharge igniting oxygen or other explosive/volatile substances in use. These substances have largely been phased out of theatre use as well as additional anti-static precautions in flooring design, but still relevant in less updated settings.)

(Seeing consultants scrubbing with plain rings on while having vivid memories of other students being yelled at for wearing them on the bare-below-elbows wards definitely messed with my head a bit.)
(In my particular hospital this is also a typical calling card of the anaesthetist, who is most likely to be drifting between theatre areas. They do look super cool though. Then again, anaesthetists usually do anyway.)

(I have never in my life heard anyone ever offer “a hug”, only ever a huddle, presumably to avoid precisely this confusion.)

(On the topic of surgical lights: also be wary of banging your head on them if you’re shorter than the surgeon. I’ve forced the replacement of more than a few sterile handle covers by bumping them!)
(Guilty as charged, but untrue in my case: not to brag too much, but I’ve been one of the more popular singers.)
9 notes
·
View notes
Note
Everyday I feel guilty that I may have not done enough for my patients. As a newly minted doctor, I still wonder whether I should be given this responsibility to practice medicine but then a patient tells me I was the only doctor who tried to explain their condition to them, the doctor they enjoyed talking to, the doctor they can trust, the doctor they're thankful they got and I think maybe I am meant to be one? Maybe this is what I'm supposed to do after all?
Anyway, hang in there! It never gets easier, you just get better is what I always tell myself.
Awww, that's such a fantastic experience! Every now and then we need little reassurances and reminders that we're in the right place and doing the right thing, so I'm glad you got it when you needed it. :)
#qna#sorry for the long delay#this has been sitting in my inbox for a time#I've just been... so... swamped
4 notes
·
View notes
Note
Where art thou? No updates
Oh hi, thank you for asking! Really wasn't sure anyone read deep enough into my About page to reach the "remind me to get my rear in gear" part!
I am alive! And quite well actually! Just been very, very busy recently, long overdue for an update but one had to come sooner or later. Been on my GP placement for a good few weeks, and sad to be nearing the end of it, been such an amazing experience compared to previous blocks.
Definitely a jump in the deep end (from day 1 it was "here's a room for you, here's your patient list, good luck!"). But it's been incredible how obvious to me the growth and jump in my confidence, independence and familiarity have been. Like, the imposter syndrome has been inverted: hard to feel like I don't belong when I'm giving medical advice which is as good if not better than the practice GPs (no judgment to them, everyone has knowledge gaps, and I have my little niches of expertise).
A whole range of meaningful patient interactions some wholesome and sweet (the wonderful compliment mentioned in my last post for example), some considerably more difficult and emotionally-charged, but tbh I've gotten so many learning points from all of them that I couldn't begin to explain. And the practice itself was very sweet too, great relationship with all the GPs, nurses, receptionists and admins, definitely made it easy to become part of the whole team.
Sadly enough I'll be leaving soon like I said, but next I'm rotating onto my longtime love (obstetrics & gynaecology), so hopefully more good things in the future?
6 notes
·
View notes
Text
“Thank you, Dr Hopefully, for being so thorough.”
“Well, not quite a doctor yet, but you’re--”
“Then hurry up, we need more good ones.”
#dnh(h)#personal#some days are good ones actually :')#medblr#medical student#less than a year until finals and the imposter syndrome is slowwwwly fading
38 notes
·
View notes
Text
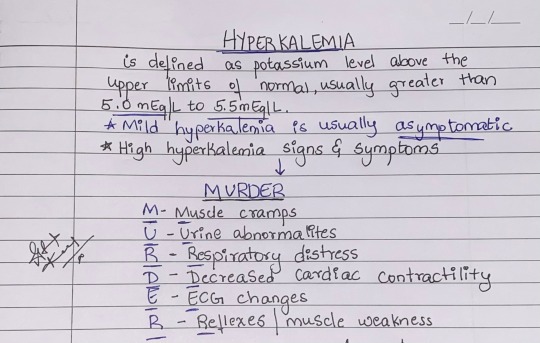
Hyperkalemia intro with mnemonic!
159 notes
·
View notes
Text
For Year 2 medical students/ medical professions. Insulin analogs mnemonics.
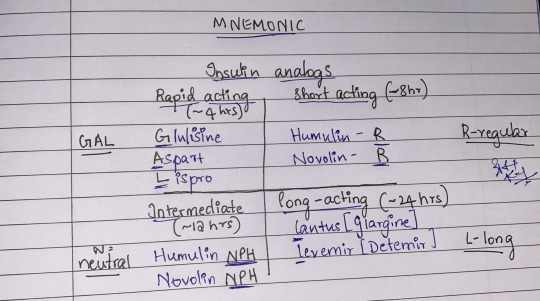
119 notes
·
View notes
Text
Hypoglycemia introduction summary!
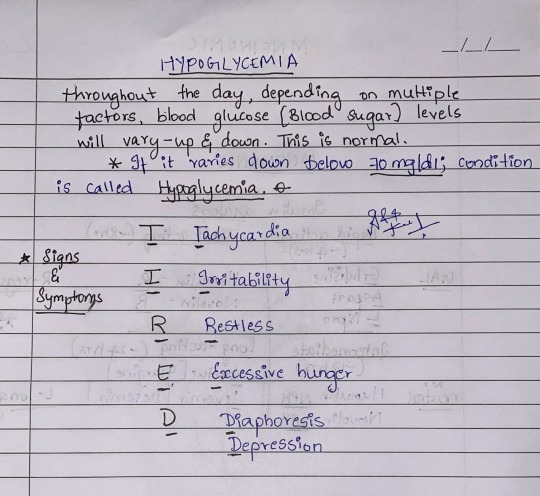
125 notes
·
View notes
Text
(In a tutorial looking at radiographs of fractures)
Teaching Fellow: Anyone want to shout out what you see in this radiograph? Other than the interesting artifact ideally?
Me (barely contained laughter): Is this seriously an example of a Throckmorton’s sign?
Teaching Fellow: Is this a what.
(Turns out, yes, they were referring to the penis as the “interesting artifact” but had not heard of Throckmorton’s sign before. Score: Tumblr 01, Teaching Fellow 00)
#dnh(h)#personal#important note: Throckmorton's sign is NOT clinically useful and is prone to false +ve#but it is very fun when you do see it and it actually helps identifying a fracture
4 notes
·
View notes
Text
Okay. You people. Here are the final results:
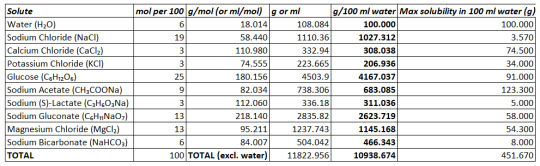
Let's just take note of why I included max solubility (at 20°C wherever possible): y'all tried to dissolve nearly 12kg of solutes in 108mL of water.
Any one solute would have surpassed saturation in this solution. This "hydration fluid" is literally a pile of salts sitting in a tiny drenching of water. I mean, there's no way in hell you could get this through an IV without clogging it up, but words cannot describe the carnage if you did.
Let's look at fan favourite glucose alone - easily the Medblr equivalent of vanilla extract with 25% vote share - giving us ~4,167g/100mL. Put that into a standard 500mL over 15min bolus for initiating fluid resuscitation, and that means 20,835g of glucose. Let's generously assume we're putting that into a person with a healthy blood volume, 5,700mL, and at the lower tolerable end of fasting blood glucose levels at 700mg/L blood or 3990mg (3.99g) overall.
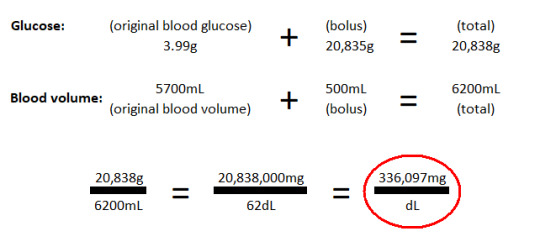
For context:
Normal Fasting Blood Glucose: 70-99 mg/dL
Prediabetic Fasting Blood Glucose: 100-125 mg/dL
Diabetic Fasting Blood Glucose: 126+ mg/dL
Typical DKA Blood Glucose: 250+ mg/dL
Typical HHS Blood Glucose 600+ mg/dL
Highest Recorded Survivable Blood Glucose: 2,656 mg/dL
Your result has given our fictional patient a blood glucose 126x the highest known survivable level. A hyperosmolar hyperglycaemic state to end all hyperosmolar hyperglycaemic states. Good job Medblr, you've officially created the stuff of nightmares that will finally bring something all the specialists can agree on.
In the search for Medblr's equivalent of vanilla extract, I now present my horror show:
Please note: this is just for fun and is in fact a terrible idea. I will not be making this solution or putting it into patients, and I highly suggest you follow my example.
The only point of this is to create a sequel to Hartmann's solution so abominable that anaesthetists, nephrologists, ED doctors and other clinicians can all unite in their shared hatred of it.
The rules: poll will be open for 1 week, all percentages will be taken as relative amount, in mol or mmol, compared to each other (for context: 1L of normal saline contains 0.154 moles of sodium chloride in 55.5mol water).
18 notes
·
View notes
Text
In the search for Medblr's equivalent of vanilla extract, I now present my horror show:
Please note: this is just for fun and is in fact a terrible idea. I will not be making this solution or putting it into patients, and I highly suggest you follow my example.
The only point of this is to create a sequel to Hartmann's solution so abominable that anaesthetists, nephrologists, ED doctors and other clinicians can all unite in their shared hatred of it.
The rules: poll will be open for 1 week, all percentages will be taken as relative amount, in mol or mmol, compared to each other (for context: 1L of normal saline contains 0.154 moles of sodium chloride in 55.5mol water).
18 notes
·
View notes
Text
Week 1 in ED done
Oh look, an update from me without any particular purpose, been a while since one of those! I’m pretty shattered and there’ve been a few meh spots throughout the week (mix of hospital time and teaching time), but mostly, and especially my time in ED itself, it’s been a good one.
Put more cannulas in in one week than I have in all the years prior, played an active role in an arrest team in an ALS setting, so many blood gases I’ve had day-nightmares about the machines demanding 15+min to run a sample, been left unofficially in charge* of management for more than a few patients (*with a supervisor always next cubicle over), briefly followed a patient into interventional radiology for a percutaneous embolisation... and perhaps most delightful of all to me, felt useful in both my knowledge and actions for one of the few times in my medical degree.
Like, I’m fond of obstetrics & gynaecology and am still very strongly leaning towards it, but I gotta say: I like Emergency Department. A lot.
3 notes
·
View notes
Text
Pet peeve: algorithms being appropriated for things they were never validated for
So I had a simulation day recently, which was actually a really useful experience (first time even practicing being the lead on an acute patient’s management), but one of my incidents bugged me. Sim patient comes in with a history of COPD and a very clear ongoing exacerbation.
A to E goes fine and dandy, oxygen titred to hold at around 92% sats for a known retainer, salbutamol back-to-back, ipratropium, steroids as required, bloods incl. cultures taken, regular ABGs and CXR pending because the fictional portable machine is busy. And then I dawdle ‘cos I’m not sure whether to also prescribe Abx for a potential infectious exacerbation via pneumonia. Temperature is normal, not able to bring up any sputum, so fellow med student suggests I look at CURB-65 score.
Instant regret. He’s already scoring a minimum 2 due to age (83) and resp rate (32), but urea won’t be back for hours bc there’s a delay in labwork which appears in the scenario just as I’d suspect in real life (plus a delay in the CXR and an ambiguity in interpreting it - turns out, the whisps and opacification around the hilum were nothing more than an unusually prominent hilum). I cave and back out on following the CAP algorithm and just left it at my present management while waiting on NIV.
Good news is, the scenario was written as a non-infective exacerbation, but ambiguous enough that I could’ve justified giving Abx anyway until review by a senior; my performance is exactly what would be expected of an FY1. It’s only afterwards in the debrief that I’m reminded of the facepalm point. The main issue is that CURB-65 was never designed for diagnosing pneumonia, despite so many hospital trusts co-opting it for that. It was only ever meant for assessing severity of already confirmed or suspected community-acquired pneumonia to decide when to admit. CURB-65 being used by some trusts as a diagnostic tool, without validation, had thrown a massive wrench into the gears of what should’ve been based on clinical judgment.
And it’s far from the only one. Glasgow Coma Score was only ever intended for traumatic brain injury, and even then its inter-rater validity has been questioned. The WHO pain ladder was only created for cancer pain management, and even though it’s shown usefulness in other contexts its use is still unvalidated and possibly incorrect in most of them.
This, friends, is why we go back and read the original studies. Because just because someone in a position of authority says a certain tool is clinically useful for a given purpose doesn’t mean it is.
#dnh(h)#personal#fictional patient - no one's medical confidentiality is being broken here!#ftr the other big criticism was 'You didn't do anything wrong but you seemed the most unconfident of any of the students today#chill out you're doing fine and you know what you're doing'
5 notes
·
View notes
Photo

For the first time in a while, I’ve signed up to do some peer teaching for 1st years over a revision special event, and one of those sessions is a cardiac exam, so I threw this together to help with remembering the examination and signs of stenosis and regurgitation of the aortic and mitral valves.
I’ve always loved the symmetry of this diagram, and it’s genuinely helped me to easily recall the cardiac cycle stage and manoeuvres needed to identify all of these murmurs.
120 notes
·
View notes
Text
Oh hi, it’s been a hot minute since I was last active here. Needless to say it’s been a wild ride and a retrospective is overdue (for context: on this day last year I was diagnosed with Covid, forcing me to quarantine alone in my flat for 10 days just after learning I’d have to repeat 2nd year), but needless to say I’m in a much better place than I was.
But no, this isn’t that retrospective. Not yet. Instead this is a rant about an offhand comment of advice to medical students given by a lecturer I otherwise and quite fond of and am glad is overseeing my first proper placement of 3rd year. The context? Advice on how to make the most of the placement. The controversial comment that set me on edge?:
“You get out of it what you put into it.”
To explain how and why I loathe this statement and this idea, let’s give some story time about my relationship with obstetrics & gynaecology.
My involvement with O&G has grown a lot from a passing interest before starting med school to my default answer of my probable-but-not-confirmed future career path. By beginning of year 2, take 1, I was already deeply invested from all biospychosocial angles, on my way to my first publication in a related research field, and rearing to go get some clinical experience.
Now, the second year curriculum in my course is pretty irregular, and O&G only fitted into a single composite placement of around 8 weeks which it shared with about 7 other specialties which received much more attention. Our scheduled time on labour ward consisted of 1.5 days total.
I on the other hand went 5 times in that 8wk period, in my own spare time while juggling the mess of other specialties I had simultaneously. I was so hyper-aware that there were clinical competencies and presentations for the curriculum I needed to be comfortable with, so desperate to put myself more at ease in a setting that I could very likely end up working in, and so nervous that I needed all the opportunities I could get despite people being nervous about having me observing them looking exactly like my cis male birth gender (and tbh, I doubt that even having a “they/them” pronouns badge would’ve helped there).
And what did I get out of all that, of putting more than twice as much time and energy into it as I was expected to? Other than sitting, waiting and reading the textbook cover to cover, in between acting as an unofficial porter for rooms I wasn’t allowed into: one NIPE and one observed normal vaginal delivery, both on the final day. Because the midwives assumed that the mothers-to-be under their care wouldn’t want someone like me observing them (which would be valid... if they even asked). Because of “shortages” of clinicians to teach me, even though that ward was virtually the only one in the hospital not to have staff missing with Covid, and surprisingly few on their arranged annual leave. Because there were always student midwives and nurses who the ward staff thought needed the experience more than I did. Because the rota meant that every time I went back it was somehow always a different team and no-one ever recognised me as someone who’d been coming back time and time again.
Come year 2, take 2, my very first day on labour ward, I’d accompanied and assisted a mother throughout their normal vaginal delivery, followed them into theatre and scrubbed in to assist in their perineal laceration repair along with two caesarean sections, one of which twins.
I wasn’t doing anything different - in fact, my confidence had been severely shaken from the previous year. I certainly hadn’t “put in” any more than I had the year before. I just got lucky to have the right kind of patients who are happy to have me there, the right day when I’m not competing with other healthcare profession students, the right registrar who noticed my enthusiasm and kindly took me under her wing to push me into as many opportunities as she could spot.
And this is why “You get out of it what you put into it” sends me into a quiet rage, because it translates to “If you don’t get sufficient learning opportunities, it must be your own fault for not trying hard enough”. Granted, it probably rings true for people who avoid the learning responsibilities that are expected of them, but it sure as hell does not mean enthusiasm and dedication pays off. And nothing hurts more when your enthusiasm and dedication and extra effort to get those learning experiences don’t pay off due to pure circumstance, and the only response you get is that “you must be to blame for that.”
And I think we can be more emotionally and intellectually honest about that. The people who care abut putting in that much of their heart and soul into it deserve more honesty about that. And if I were asked to give my thoughts on this to a bright-eyed and naive young med student as I was when I started, it would be this:
“Sometimes, you will put far more into it than you will receive. Sometimes you will go the extra mile and yet not find it productive for reasons beyond your control, because the system or circumstance fails you. And when it does, it’s okay to be upset and disappointed. It doesn’t mean you didn’t deserve to be here. It doesn’t mean you don’t have what it takes. It doesn’t mean you won’t be able to catch up later. And it doesn’t mean you should stop trying to get the opportunities to grow and improve as a clinician that you’ve fought for and earned.”
#dnh(h)#personal#medical education#resilience#okay back to our (ir)regular programming soon#sometimes you hear something and think 'LIES LIES LIES' and just need to rant ok
11 notes
·
View notes
Text
So. Retaking the year. That was an experience. Now it’s done and I’m glad it’s over.
Let’s never do it again please.
#if you're wondering if this is my way of saying 'I passed' you'd be right#year 2 x2 should be enough for anyone#dnh(h)#personal
7 notes
·
View notes
Photo

shamelessly stolen from facebook because I haven’t seen it circulating on here yet
89 notes
·
View notes
Text
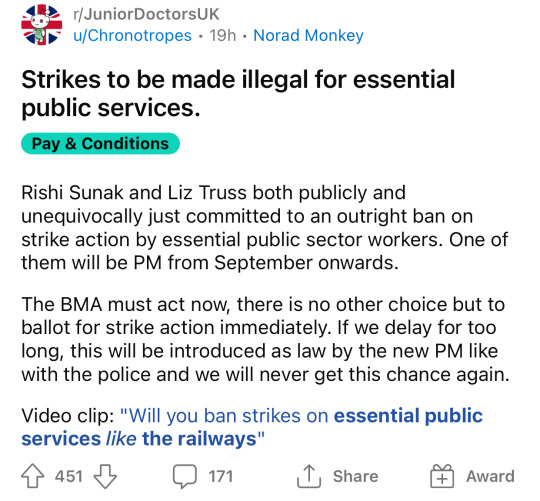
There’s no amount of words of English language to encapsulate the “FUCK YOU” these two deserve. Let’s be clear: this will, by definition, include doctors and other healthcare professionals, not just railway workers (who in any case also deserve the fucking right to strike). And this comes less than a month after the BMA committed to pursuing pay restoration for the 30% RPI drop in doctors’ pay since 2008 and weeks after junior doctors were excluded from the 4.5% pay rise offered to healthcare professionals (already a paltry amount) and given a measly 2% pay rise, still leaving them an effective 9% pay cut since 2008.
If you think this isn’t a declaration of war on UK doctors’ rights to protest and collective negotiation, think again. And while I’m of the opinion the BMA should strike anyway - it’s denial of service whether the doctors are striking or arrested - they’ve shown enough toothlessness before that this might be enough to put industrial action in a coffin.
They’re literally plotting to strip away the democratic rights and freedoms of doctors.
5 notes
·
View notes