Text
It will be Tuesdays at 7pm EST for everyone asking. There will be recording links that come with the price, so you can watch it any time up to a month after the last session.
Thanks!
Announcing MEDLEY: A Medical Primer for Writers (Summer Edition)

Are you a writer?
Do you need to know things about medicine for your fiction works?
Have you considered taking a 100% online class about it?
Starting Tuesday, June 4th and running for 9 weeks is MEDLEY.
Topics include:
WEEK 1: (US) Hospitals and the People Who Work in Them
WEEK 2: The Physical Exam
WEEK 3: Codes and ACLS
WEEK 4: Remote and Improvised Medicine 1
WEEK 5: Remote and Improvised Medicine 2
WEEK 6: Recovery and Aftermath
WEEK 7: Historical Medicine
WEEK 8: Mental Healthcare
WEEK 9: Bonus Episode
This is the second time I'm running this course so hopefully the kinks are nice and ironed out this time.
Price is $36 per person ($4/week).
Two scholarships are available no questions asked.
Contact me at [email protected] for more information/to sign up.
118 notes
·
View notes
Text
Announcing MEDLEY: A Medical Primer for Writers (Summer Edition)

Are you a writer?
Do you need to know things about medicine for your fiction works?
Have you considered taking a 100% online class about it?
Starting Tuesday, June 4th and running for 9 weeks is MEDLEY.
Topics include:
WEEK 1: (US) Hospitals and the People Who Work in Them
WEEK 2: The Physical Exam
WEEK 3: Codes and ACLS
WEEK 4: Remote and Improvised Medicine 1
WEEK 5: Remote and Improvised Medicine 2
WEEK 6: Recovery and Aftermath
WEEK 7: Historical Medicine
WEEK 8: Mental Healthcare
WEEK 9: Bonus Episode
This is the second time I'm running this course so hopefully the kinks are nice and ironed out this time.
Price is $36 per person ($4/week).
Two scholarships are available no questions asked.
Contact me at [email protected] for more information/to sign up.
118 notes
·
View notes
Text
A spring I just found on my property! I’m going to try to make a mini spring house with it.
25 notes
·
View notes
Text
Goals
My wife and I are finally at a pretty stable point in our lives (after a year+ of things being pretty wild). So we're each making a list of goals based on the (original) NerdFitness* Goal Sheet. Here's mine:
Physical
Level of functional fitness I was at at the end of AmeriCorps
Able to use a 2-wheeled tractor all day
Teach WRFA once per month
Mental (interpreting this as mental health for myself as that is what will give me the most at this point in my life)
Get a psychiatrist
Get on a mix of medications that consistently treats all my symptoms
Figure out sustainable backup plan (lifestyle/herbs) that will work if meds become unavailable
Work
Have homesteading be my primary work
Work from home part time for money doing something I love
Publish a book and receive ongoing money from it
Adventure
Do a summer as an AmeriCorps NCCC Team Leader
Get a cow and go through the process of breeding it and getting and preserving milk from it for all or most dairy needs
Acquire and raise a child
Courage
Step in and talk down a public situation
Respond to a car accident (and genuinely help)
Fully commit myself to the life I want to lead
Freedom
Full working homestead
Produce 80% of my own food and build a network to trade for things I can't grow myself
Have a fully climate change resistant house and homestead
Master (interpreting as "mastering a skill" instead of just a major goal)
Basic construction and build a root cellar with materials from my property
Farm animal husbandry
Apothecary
Gratitude
Be stable enough financially and personally to take care of my parents as they age
Give someone a leg up out of poverty by offering shelter or financial assistance
Do a health-related part time AmeriCorps VISTA program in my area
Legacy
Write a home nursing textbook
Raise a happy and knowledgeable kid who can take care of themself through anything
Find a good way to preserve this blog
*Highly recommend if you want to do NerdFitness you use the Wayback Machine on Internet Archive to get you to somewhere in the 2014-2016 sweet spot of this being a non-commercialized site.
23 notes
·
View notes
Note
if a person goes into cardiac arrest and early resuscitation efforts were given but it lasted for 30 minutes until ECMO was initiated and ROSC was achieved, how is brain death determined if therapeutic hypothermia and deep sedation was given?
It's just not something they can determine initially.
The sedation and paralytics are given to prevent the person from shivering when the therapeutic hypothermia is initiated. Therapeutic hypothermia is usually only used for about 24 hours, after which the person is warmed back up to normal temps. At this time, every 24 hours or so the person undergoes a "sedation vacation" where the sedation is withdrawn to see if the person can wake up and breathe on their own. It would be during this time when an EEG or other determinations of brain death, like cold calorics, would be used.
18 notes
·
View notes
Note
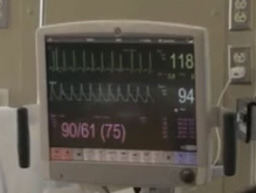
hii! what are the effects of prolonged tachycardia with fluctuating bpm ranging from 140-160 for around 30 minutes to a conscious patient? will it cause any brain damage?
The short answer is basically nothing and no.
Tachycardia is any heart rate above 100 in an adult. There are several different kinds of tachycardia, including sinus tachycardia, paroxysmal supraventricular tachycardia, atrial fibrillation with RVR, and ventricular tachycardia. Whether the tachycardia is bad for a person has to do with what kind of tachycardia it is, what the heart rate is, and how long the person is in that rhythm.
The first one we'll talk about is sinus tachycardia. Sinus tachycardia is a normal physiological response to the body's demand for more oxygen and nutrients. Sinus tach happens when someone has a fever, is dehydrated, has blood loss, is in shock, or is having a strong emotional response.
It's one of those things that doesn't need treated in and of itself, though figuring out and treating the cause is important. Once the cause is treated, the heart rate usually drops back down to normal.
There are also times when you intentionally bring the heart rate up above 100- for example, exercise. This is also considered sinus tachycardia. When you exercise, you want your heart rate to be in a target zone, which depending on age can be anywhere from 75-170bpm (the younger you are, the higher the target heart rate).
In the case of exercise, a heart rate of 140-160bpm for a half hour would be completely reasonable. In the case of dehydration or shock, you'd really need to fix the problem, but the heart rate itself isn't going to hurt anyone under about 60 who is otherwise healthy.
Paroxysmal Supraventricular Tachycardia (PSVT) is a condition in which the heart rate randomly increases into the high 100s-low 200s. This heart rate is so fast that the heart doesn't have time to fill with blood in between beats. Because of this, not as much blood is getting out of the heart to the brain and body, which means the person may feel faint, short of breath, or dizzy or even pass out.
People in PSVT may spontaneously convert back into a normal rhythm, or they may need a drug called adenosine given to change them back to a normal rhythm. Adenosine works kind of like a defibrillator- it briefly stops the heart in order to let it restart normally. If this happens frequently, someone may need an ablation- a procedure in which parts of the heart muscle that are causing the rapid heart rate are burned to permanently prevent future attacks.
In order to understand atrial fibrillation with RVR, you have to understand how the heart initiates beats normally. In the heart there are cells in a place called the SA pacemaker node, which send out small electrical signals that work to coordinate a beat across all the cells in the heart.
In atrial fibrillation, lots of cells outside this node try to initiate beats, which causes the top half of the heart to quiver. If a lot of these "beats" get through to the bottom of the heart, that's called Rapid Ventricular Response, or RVR. Afib RVR causes a rapid, irregular heart rate.
Afib RVR can cause the same problem as PSVT- namely that it causes the heart to beat so fast it can't refill with blood in between beats. Usually the first few times this happens the person converts out to a normal rhythm within about a week (or can be converted out with defibrillation or medications). Later this state can become permanent and has to be managed with medications that reduce the heart rate and blood thinners to prevent strokes and heart attacks, which happen because blood gets stuck and clots in the quivering upper part of the heart.
The last one, ventricular tachycardia, is the most dangerous because if not treated it can either become so fast virtually no blood is coming out of the heart (cardiac arrest) or become another dangerous rhythm called ventricular fibrillation (also cardiac arrest, but even worse).
This one is a life-threatening emergency and needs to be treated immediately with CPR (if the person is unconscious) defibrillation and medications.
This was a lot to answer your question, but all this to say that if your person is running 140s-160s because they're working out for a half hour, they're totally fine. If they're 140s-160s because of PSVT they're not fine but they're probably going to convert out of it with a medication or just time. If they're 140s-160s in RVR they're probably uncomfortable and need medical attention but they'll probably be alright. If they're in ventricular tachycardia, they need emergency care.
Of these, the only one that could really cause brain damage is the ventricular tachycardia, but it would have to be a lot faster than 140-160.
21 notes
·
View notes
Note
I have way too many whump/hospitak questions in my head but I’ll stick with these two for now-
1- Sooo imagine you have a prosthetic arm made of metal that you cannot remove, or you can remove it but it leaves a ring of metal to act as a seal/attachment point to the metal arm. Say that a person with this prosthetic has something happen to them and their heart stops beating so they need CPR/rescue breaths. This brings me to my first question- are there any types of hospital AEDs that can still work normally without hurrying about the metal connecting to the patient themselves?
2- if a patient is drenched [think stuck in a rainstorm and soaked to the bone] and needs to have an AED used on them, are there any types of AED’s that are waterproof or can be safely used in the rain? If not, how much of the patients body do they need to dry off before they are able to safely use the AED on them?
1: Any AED should work fine, even with the metal. We use AEDs on people with metal implants (pacemakers, orthopedic pins and screws, etc...) all the time so I imagine it wouldn't be much of a problem.
2: Generally if you can, you want to get the person out of standing water, get them under some kind of shelter from direct rain, and dry off at least the parts of their chest that would be in contact with the pads. But also the person's heart isn't beating so you have to weigh this against how long it's going to take to do these things.
15 notes
·
View notes
Text

10 notes
·
View notes
Text
23 notes
·
View notes
Text
Controversial opinion: I think we do a serious disservice to new nurses (and their patients!) when we teach them medicine for 3-4 years and then expect them to learn the nursing part on the job.
Nursing is a learned skill. No one is born with the knowledge to do nutrition management for a variety of illnesses. No one is born with the skill to build and maintain an environment conducive to healing while balancing the need to keep someone safe. No one is born with the skill to mediate family conflict or encourage a patient to talk through their problems. No one is born with the basic knowledge to hands-on manage a variety of complex illnesses, let alone the completely different skill of teaching the patient to do the same in a way that works for their needs and lifestyle.
And while I know they touch on these things in nursing school, they're hardly as much of a focus as they were 50 years ago. And I think that needs to change, even if we cut out some of the medicine.
44 notes
·
View notes
Note
I had not, but I went to look it up, and as it turns out it decreases risk of long covid by up to 41%. And the studies are really high quality, appropriately blinded, with lots of participants. It would be really interesting if it also worked on other long-viral syndromes.
What’s the weirdest or most surprising thing that metformin does?
Probably the fact that it treats malaria. That's a weird one no one really expects, even though that's one of the reasons it exists.
62 notes
·
View notes
Note
so i have this character who drowned and was pulled out of water with no pulse, other than doing rescue breaths + CPR can the rescuer used an AED and epinephrine on this character to get their heart beating again?
Yes.
In fact, you're probably going to need at least the AED to get the heart beating again in a normal rhythm.
The epi is a weird one since most people don't carry it in the form necessary to work fast enough to make a difference in a cardiac arrest. Like, could you use an epi pen (or other auto-injector)? Maybe, but the dose in an adult epi pen is less than a third of the dose usually used in a cardiac arrest (0.3ml vs 1ml).
And epi pens deliver their dose into the muscle instead of into a vein, so it takes time to absorb. Even longer if the only circulation is CPR. You'd probably have to do CPR for at least 20-30 minutes before even some of the epi made it to the heart, making it all but useless.
I hear you then saying "but what if I discharged 3 epi pens straight into the heart Pulp Fiction style (or took an epi pen apart to get to the rest of the epi and injected it straight into the heart)?" Well, unfortunately, the needle is not long enough. It's only 16mm, and the average chest wall thickness is close to 40mm.
So TL;DR if your character doesn't have IV access and enough epi, I would probably just stick to the AED and CPR.
34 notes
·
View notes
Note
Is it possible for someone to pass out in mild freezing weather in just pajamas and develop frost bite bad enough to impair their hands and feet? How long would they be unable to walk or use their hands fully?
Probably not.
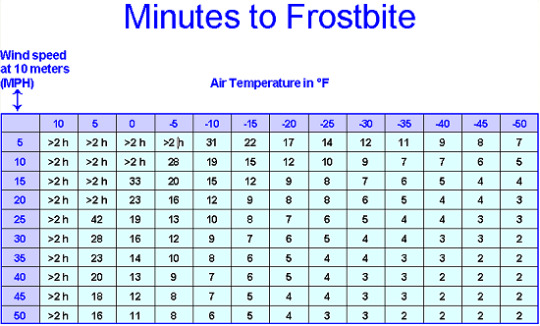
As you can see in this table, even at 10F (-12C) it takes well over 2 hours no matter how much wind there is to get even some frostbite, so mildly freezing temperatures probably wouldn't cut it.
Hypothermia, however, is a lot easier to get. Your character can get that with 40F and a drizzle.
53 notes
·
View notes
Note
So, in PA there is a bill in the senate called the Patient Safety Act that mandates nurse:patient ratios. Obviously, I am a big fan of this bill as it would ease pressure on nurses and improve patient safety outcomes. It is also very bipartisan, with both republicans and democrats being for and against it in similar ratios. The big criticism of the act as it stands is that there are little to no considerations for small, rural hospitals who would find it difficult to meet those ratios without going under (don't have enough nurses, will have to close beds/hospitals). I thought the solution to this was to obviously increase protections for rural hospitals (like making the ratios for them say 1:6 instead of 1:5 for example.) But this has the unintended consequence of making it more difficult for rural hospitals to entice nurses to work for them (who wants to work in a rural hospital with worse ratios when you can make more money with better conditions somewhere else?) It's already difficult for rural hospitals to find staff. Do you have any ideas on solutions to the problem? I was surprised to find out how nuanced this situation really is, and how it isn't just "put in ratios plz" and everything would be fixed.
You're right in that this situation is extremely nuanced, especially when it comes to the fact that we are (as usual*) in a nursing shortage nation wide.
Staffing ratios only work when there are enough nurses to meet demand. A lot of times the goal of staffing ratios is to incentivize hospitals to hire more nurses, but if there are no nurses to hire that doesn't work. So you have to then consider alternatives, like you mentioned- either closing hospitals, or closing beds.
Consider, though, that if hospitals go the route of closing beds to maintain ratios, the acuity (care difficulty/complexity) of those patients the nurses are caring for goes up because lower acuity patients get triaged out.
The "sweet spot" of acuity to number of patients then relies on the number of nurses available to serve a population. That means that populations with a smaller number of nurses have either a higher number of patients per nurse, or a higher acuity patient load than a population with a relatively large number of nurses.
And pretty much everywhere right now, rural areas specifically, there are just too few nurses to make staffing ratios possible at scale.
So. How do you go about providing a high standard of care for patients when there are fundamentally too many patients and too few nurses? The system needs to change. I present a few possibilities below:
Bring LPNs back to the bedside in hospitals: While I don't mind Magnet as an entity and think they do some good things, IMO they royally screwed the pooch by mandating RNs (particularly BSN prepared RNs) only on hospital floors. You can make LPNs a lot faster and cheaper (10-18months, $20,000) than you can make RNs (3 years, $40,000), or BSN-RNs (4-5 years, $80,000). And while you still need an RN license to do things like push IV meds and interpret assessment findings, just about everything else can be done by an LPN. So we need to be using that resource to make more nurses fast.
Institute Team Nursing: You know how you use LPNs efficiently? It's not by giving them a group of patients and having them run around to find an RN every time they need to push an IV med. It's either by having them as a dedicated tasker (doing the time-consuming skilled tasks like wound care, catheter placement, IV placement, etc... for many RNs) or incorporating them into a team. With team nursing, you have an RN, an LPN, and an STNA/Tech all caring for 12-15 patients instead of an RN and an LPN caring for 5 each with a tech helping. The RN does the tasks only an RN can do (assessments, IV meds, plans of care) and communicates with the doctors, the LPN does most of the med pass and skilled tasks, and the STNA does the basic patient care. Since there's 3 people working together instead of separately, it's easier to find someone to help with 2-person tasks like boosting a patient in bed. You would not believe how much time this saves and how much more patient care can actually get done.
Institute Advance Practice Providers (or at least universal contact methods): I'm not saying we have a ton of these either, but you only need about one per floor. See, I can't tell you how much time I used to spend just trying to figure out who to contact about a problem, and how they wanted to be contacted. Because God forbid you text Doctor A instead of paging or page Doctor C instead of calling. Now I work on a floor with an APP and you can just go straight to them and they can either write the order you need themselves or contact the doc who can. Probably a good 15% of my time is back and I'm not even exaggerating.
Change culture around nursing duties: this is a controversial one, but as nurses are spread more thinly than ever and medical acuity has gotten so much higher, the basic care is genuinely getting worse. I have seen this happen over the last 8 years I've been in my job. So. Re-teach families how to care for loved ones in the hospital. Make it culture that if you have a family member in the hospital someone is with them. And when I say with them, I don't mean just visiting. I mean actively caring for the family member. Helping them to the bathroom, helping them dress and eat and clean themselves. Helping them do basics. Entertaining them, distracting them, comforting them. Things we used to be able to do when our patients weren't actively trying to die at all times.
*technically, we have been in a nursing shortage since WWII. But a lot of factors, COVID-19 specifically and a shortage of student slots in RN-level nursing schools, have made things particularly bad in recent years.
36 notes
·
View notes
Note
Years ago I wrote a character who fell into a very cold quarry lake and had a heart attack right after being pulled out-- it was based on some research I did at the time, but for the life of me I didn't understand what was actually going on that causes that kind of reaction to being pulled out of very cold water. Could you explain?
It's cold shock.
When your skin first hits very cold water you enter a temporary state called cold shock. This is not shock in the medical sense, nor is it the same as hypothermia. It's just a situation where you gasp uncontrollably, and heart rate and blood pressure go way, way up as a response to the skin suddenly getting very cold. It ends within a couple of minutes, but while it's happening, it greatly increases the oxygen demand of the heart muscle.
That means, if there are any blockages (clots, plaque) in the arteries supplying the heart muscle with blood, the arteries can't supply the necessary oxygen, and the heart muscle begins to die- a heart attack.
41 notes
·
View notes
Note
suggestion for post topic: list of improvised first aid/medical supplies & uses from things commonly found in a kitchen
The following is, as usual, not medical advice:
What I like to call "Severe" Hot Chocolate: Do you have asthma? COPD? Don't have your inhaler with you? Severe Hot Chocolate might help! In a sauce pan over low heat, combine 1Tb sugar and 3Tb unsweetened cocoa powder with a little water. Once its combined into a sludge, add a cup of milk or milk substitute of choice and stir to combine and heat. Then drink. It will be bitter, but not too bad if you like dark chocolate.
An Entire Head of Lettuce: Need to poop? Wanna do it tomorrow morning? Eat an entire head of iceburg lettuce in one go (with or without dressing).
Lite Salt: Need electrolyte replacement or a cheap sports drink? Dissolve 1/2tsp Lite Salt (half sodium chloride and half potassium chloride) in 2 cups of lemonade or other flavored drink. Sugar actually helps with the absorption of the electrolytes, but if you need a no sugar drink you can do that too.
Plastic Wrap: Stabbed in the chest? Unfortunate. Get a piece of plastic wrap to put over the wound and tape it down snugly. The sucking chest wound will still be there but it will buy time to get to a hospital.
Ice/ziploc bags: While ice doesn't help things heal, it sure makes them feel better. Put some ice in a bag and wrap that bag in a towel and put that on your musculoskeletal injury for pain relief.
Instant Pot: Need to sterilize something made of metal? Don't want to use a chemical? Put it on a shelf in your pressure cooker and add some water to the bottom. 10 mins on high pressure should do it.
Rice (in a sock): Fill a sock with dry white rice. Microwave it for a minute or so. Use it for cramps or back pain.
Fresh Coffee Grounds: This isn't so much a medical thing (though it is frequently used in hospitals) as it is a good-to-know. Coffee grounds absorb biological odors. Just put a little bowl of them in a room with a poop or BO-type smell and it will absorb it.
135 notes
·
View notes