Text
uterus: Guurl, you’re ❌NOT❌ pregnant🎉💃
me hunched over in agony: This… could have been… an email
100K notes
·
View notes
Text
This is SUPER important.
I'm not sure that I really understood the difference until closer to 30. There is a difference and it is a life skill to recognize it to maintain relationships.
one of the most challenging skills i've had to learn as an adult is the art of figuring out whether i'm proportionally annoyed with someone or just tired and overstimulated and looking for reasons to be pissed off
95K notes
·
View notes
Text
This is why we do not utter the following words in my ICU:
Quiet
Slow
Boring
Easy
These words only bring chaos and suffering to any shift.
ICU Resident *evil smile*: Damn, looks like your are having a very quiet shift…
Night shift Med-Surg Resident: NOOO, LAST TIME YOU SAID THAT I HAD TWO PATIENTS BECOME SEPTIC, FUCK YOU
45 notes
·
View notes
Text
From the archives: Shock States
Honestly, probably the best and most useful content I have written on here.
Shock
Time for the learning! A quick breakdown of the 4 types of shock so all you students getting pimped on rounds will be freakin' bosses. In all seriousness, this is vital to understand and if you're thinking of emergency medicine or critical care, it is extremely important to get this down pat. Remember, septic shock and hemorrhagic shock are SUBCATEGORIES, not one of the 4 main types.

When you think about shock, generally think about someone who (usually) has a reversible problem that causes enough hemodynamic instability that they require vasopressors. Essentially, cardiac output is reduced. Depending on the etiology of the shock, the symptoms can very. Before thinking about shock, it's important to understand cardiac output.
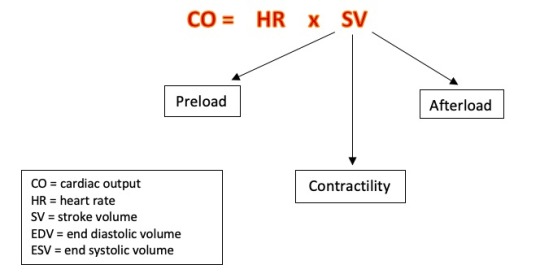
Stroke volume is defined as the volume of blood (in L/min) that exits the left ventricle per heart beat. More specifically, this is EDV-ESV of the left ventricle. You've learned about the Frank Starling Curve - I'm choosing to explain it a little differently without using the curve.
I think of heart rate as being a response to a certain change in stroke volume. Two of the three components of SV are proportional.
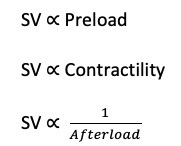
When preload increases, stroke volume increases. When afterload increases, stroke volume decreases.
Preload is referred to as end-diastolic volume, i.e. the amount of blood in the ventricle at the end of diastole and prior to ejection through the aortic valve.
Contractility is the amount of cardiac muscle stretch prior to ejection.
Afterload is the amount of pressure the left ventricle must overcome to eject blood through the aortic valve. You can think of this as systemic vascular resistance.
When thinking about shock, think about what components of stroke volume are possibly being effected.
General symptoms of shock: hypotension, tachycardia, bradycardia, confusion, delirium, LOC, dizziness, lightheadedness, general malaise, febrile, sweating, pallor, shortness of breath
In the treatment sections below, please consider your ABCs first.
Hypovolemic
Main problem: there isn't enough volume in circulation to support normal hemodynamic function. Not enough preload.
Examples: dehydration (vomiting, diarrhea), hemorrhage (loooooong list of etiology), pancreatitis, severe insensible fluid loss (big burns, open abdomens), etc
Subcategory: hemorrhagic shock
Treatment: fluid or product resuscitation, stopping the source of bleeding
Obstructive
Main problem: something is compressing the heart or creating a circulatory blockage which disrupts normal hemodynamics/heart function. Afterload is increased.
Examples: tamponade, tension pneumothorax, PE, severe STEMI.
Treatment: reduce the afterload. Dependent on cause - pericardiocentesis, needle decompression, chest tube insertion, anticoagulation/ thrombectomy, cardiac angio/catheterization.
Distributive
Main problem: something is causing volume to be dispersed in places that it should not via severe vasodilation. Blood vessels are so vasodilated that adequate tissue perfusion doesn't occur. Disruption in preload via reduced afterload (systemic vascular resistance). This type of shock is also referred to as vasodilatory shock.
Examples: bacteremia, large burns, polytraumatic injury (or anything particularly inflammatory like anaphylaxis), spinal cord injury, TBI
Subcategory: septic shock, neurogenic shock, anaphylactic shock, shock due to adrenal crisis.
Treatment: increasing systemic vascular resistance with use of vasoconstricting drugs, +/- treating the infection, reducing inflammation (steroids)
Septic shock is tricky because CO can be maintained for a time. The heart will compensate by increasing the rate, which is why septic patients routinely have HRs well over 120 bpm. But the increased HR is a sign that SOMETHING ISN'T right. If you have a patient with a new, increased HR, do NOT simply treat with a beta blocker (you'll probs code them if they are septic). Think WHY is the HR increased? If you need a vasopressor for a septic patient, norepinephrine is ALWAYS the first choice per Surviving Sepsis Guidelines.
Neurogenic shock presents itself differently because the etiology of the vasodilation is decreased sympathetic tone. Because of this, you'll have a hypotensive patient who is also bradycardic. Seen in patients with new spinal cord injury most commonly and sometimes new TBIs. These patients need MAP goals, usually over >80, with the help of a vasopressor to keep them out of a shock state. Any pressor will do, generally if my patients aren't excessively bradycardic I'll use phenylephrine.
Anaphylactic shock is unique due to it's rapid development and more immediate risk to the airway. Intubating these patients is the first priority. The vasopressor of choice is epinephrine.
Shock due to adrenal crisis should first be treated with high dose hydrocortisone. Any pressor will do (though to be honest, I have never had a patient in adrenal crisis myself, so suggestions welcome). This type of shock has some secondary concerns like sodium and calcium loss that need to be corrected immediately. It's most commonly triggered by dehydration so fluids are a must.
Cardiogenic
Main problem: pathology within the heart is causing disturbed hemodynamics. Increased afterload OR increased preload (think right heart failure). Reduced contractility. It's the one form of shock that is less likely to be reversible, ie. if you have structural heart disease of any kind, that's not reversible.
Examples: chronic heart failure (left or right), cardiomyopathy, severe aortic stenosis, Takasubo's, STEMI, ventriculoseptal defect, ventricular outflow obstruction (LVOT obstruction).
Treatment: depends on etiology but generally involves increasing contractility by adding an inotrope like dobutamine, milirinone, etc. Correcting or improving the underlying issue can improve things. These patients often need vasodilating agents to reduce afterload. If they are too sick for an intervention, they may need ECMO, IABP, or LVAD/RVAD to bridge them to improve enough for a procedure.
Overall Message
When you have a patient with low blood pressure requiring vasopressors, think about the underlying etiology to figure out the differential. Don't look at clinical symptoms separately - there is often a bigger picture at play. Also worth nothing that multiple kinds of shock can exist in the same patient OR treatment for one type causes another.
Good luck!
#medicine#emergency medicine#critical care medicine#critical care#pablr#MD#DO#PA-C#ARNP#DNP#shock#types of shck#medblr#nurblr#pharmblr#cardiogenic shock#distributive shock#hypovolemic shock#obstructive shock#types of shock
30 notes
·
View notes
Text
From the archives: witnessing the source of a patient's injury
I stumbled on this post while updating my FAQs. Honestly, I forgot about this patient story. It happened a couple of months before I started graduate school when I was still working as a CNA in an ICU in 2016. My perspective on it now is a little different. I read this and I still feel righteous indignation for the patient. However, I also read this and consider how hard it would be for the husband to show up to the hospital. How hard it would be for the patient to even let him.
At the time of this story, I was married for not even 2 years. Now I've been married almost 10 years and this just hits differently with experience. I feel much more sad than angry - decent people can do stupidly shitty things when they have poor coping mechanisms. 110% not justifying husband's behavior. But with situations like these, there is always more beneath the surface that we do not see or appreciate.
Third Wheel
I had a patient recently who came in after a suicide attempt. She overdosed on quite a bit of benzos. Apparently she did this after she caught her significant other in the act with the neighbor. She had a history of depression and marital issues. Seeing her was distressing to me. She was so frail, vulnerable; I felt some intense righteous indignation on her part—sisterhood solidarity if you will.

And then the husband showed up to see her.
I don’t believe I can ever describe a situation so tense. They didn’t speak, just cried. It was the first time I had ever seen the source of my patient’s depression so completely manifested. Let me tell you, the tension was off the charts. Seeing him, it made me SO angry. Internally, I was seething. How dare he? How dare he show up and try to comfort someone he traumatized so horrifically that they attempted suicide.

I’m not even sure how to feel. I know how I would feel if it were me. But I suppose, as health care providers, we see so much that we experience in a tertiary sense. We want to intervene but sometimes we have to let things be. The patient agreed to have him come. I think it says a lot about her strength as a person and I truly hope she finds peace with what happened. However, I struggled with the emotion of it all. It got to me. And perhaps that is because I am a fellow depressive and I see myself in her–I’m not sure.
I saw a kind person completely thrown under the bus and forced to live her trauma in front of my eyes. Even if it was her choice, I was still furious about it. The saddest part of it all, I believe, is that there was nothing I could do or say to comfort her. Nothing that would make her feel any better. I haven’t worked with a patient or family in several months with that level of stress and sadness. It reminded me just how humbling working in health care can be and how impotent you can feel when you can’t do a damn thing.
#medicine#critical care#emergency medicine#medblr#pablr#nurblr#pharmblr#MD#DO#PA-C#ARNP#DNP#patient story
11 notes
·
View notes
Text
From the archives: Thermal Burn Management for PCPs.
It's getting warmer and we all know that means outdoor activities and increased possibility of burns! There is a lot that PCPs can manage with the right knowledge. Not comfortable with burns? See this post for the low down on how to advance your practice.
Thermal, Scald, and Contact Burns
This is a quick guide to thermal, scald, and contact burns. I’ll review what YOU can do as a PCP if you get small burns of this nature. For information regarding burns in general or when to refer to a burn center, please see my post about burn center referrals.
Quick facts
Scald and contact burns are some of the most common injuries among children < 5 y/o
Thermal burns include extremely hot air, flame, or steam.
Contact burns include touch a hot surface, molten metal splash back
Scald burns include exposure to a hot liquid of any kind, but more often than not it is water.
Keep reading
#medicine#medblr#pablr#nurblr#pharmblr#burns#burn medicine#family practice#PCP#MD#DO#PA-C#ARNP#DNP#primary care#emergency medicine
120 notes
·
View notes
Text
Hyperbaric Medicine (HBO)
I'm sorry, what is that?

I have a side hustle as a hyperbaric medicine provider and I am here to give you the down and dirty!
Sometimes referred to as HBO (hyperbaric oxygen), hyperbaric or dive medicine is a specialty that utilizes oxygen at high pressure to treat a variety of conditions, primarily things involving wounds. We place a patient in a chamber, deliver 100% oxygen to them, pressurize the chamber, and keep them in there for about 120 minutes. Since oxygen is the number one thing you need to heal a wound, we use a lot of it to try and speed up the process.
The Basics
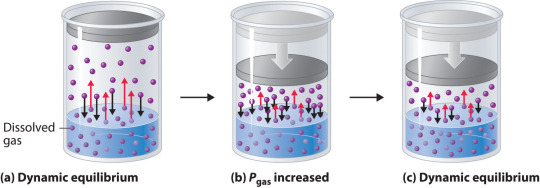
Wait - what? HOW? Try not to have PTSD from your days in chemistry, but remember these?

The treatment physiology of hyperbarics relies on gas laws. Recall that it takes a lot of pressure to dissolve a gas into a liquid.
We use pressure to force oxygen into the blood stream at high rates to facilitate wound healing. For reference, most of your oxygen content is bound to hemoglobin (~98%). You do have dissolved oxygen in your blood, represented by your PaO2/PvO2 in a blood gas. However, this makes up a fraction of O2 content (~2%: if you want a clinical soap box, you should hear me talk about blood gases to students lol). A normal ABG would have a PaO2 of 65-100. An ABG acquired during hyperbaric treatment would be well over 2,000.
As an aside, recall that ambient air is 21% oxygen. Also, as a reminder, we exist at 1.0 ATA of pressure (one atmosphere).
How is it done?
Delivering oxygen this way requires delivery of a lot of pressure. We utilize dive chambers for this purpose. There are two types of chambers:
Monoplace: literally looks like a class coffin. Holds one patient and delivers oxygen at pressure through the entire chamber. These are very popular at wound centers.

Multiplace: literally looks like a submarine. Holds 2+ patients and delivers oxygen at pressure to individual patients hooked up to hoods or masks. These are found at tertiary care/academic medical centers.

Literally, the multiplace hoods make you look like a silly space person.

The reason oxygen is delivered this way in a multiplace chamber is to reduce the risk of fire. Oxygen at pressure can go boom. Having an entire chamber full of O2 is a big risk. So, we deliver the gas individually to each patient.
How did it start?
Dinking around with gases at pressure has been a thing for 400 years. However, it didn't become a more focused endeavor until the first dive suits started to be a thing in the 1870s. The specialty itself is relatively new, developed in the 1930s due to advent of decompression illness with divers. Things really progressed in the 1950s.
One pivotal study was "Life without Blood" in 1959. Dr. Boerema proved that he could keep a pig alive with HBO alone. The ethics of this experiment are questionable but he exsanguinated a pig under hyperbaric conditions (3.0 ATA, 100% FiO2). Plasma was left behind. By doing this, he proved that, at pressure, an organism does not need hemoglobin to live. Kind of a radical thing to prove! Don't worry, the pigs did get their blood back and recovered without issue.
What is treated with HBOT? (hyperbaric oxygen therapy)
Anything related to wound healing can be treated with HBOT. We also treat carbon monoxide poisoning, air gas embolism, and decompression sickness with HBOT. I'll start with those since they are (imo), the most clinically interesting. ;-D
Carbon monoxide poisoning: The physiology of using HBOT to treat CO poisoning is based on the binding affinity of CO to hemoglobin. CO has 200 x the binding affinity for hemoglobin than O2 or CO2 does. Because the binding sites are taken up by CO, hemoglobin cannot pick up O2. It also can't offload whatever O2 is already bound. The goal with HBOT is to bombard the blood with massive amounts of O2 to force CO off.

For reference, it would take about 6 hours for CO to offload on its own from hemoglobin on room air. It would take half as long at 100% FiO2 delivered at standard air pressure (1.0 ATA). CO is rapidly forced off within 30 minutes with HBOT. With very severe CO poisoning, particularly in cases of LOC, this is vital for limitation of hypoxia and neurological sequelae of exposure. Treatment is 1-3 "dives" depending on clinical context. The patient is treated at 2.8 ATA (60 feet of sea water) for about 120 minutes.
Air gas embolism: This occurs when gas is accidentally introduced into circulation. It can either be venous or arterial. The venous system has much more flexibility in tolerance for air bubbles. 15 cc or less of gas introduction is probably not going to result in symptoms. Higher volumes go to the lungs and can result in local lung infarction.
The real danger with this is air introduced into arterial circulation. Depending on where it is introduced, it can go directly to the heart causing an MI, or to the brain causing a stroke. Any volume of air introduced into arterial circulation is bad news bears. Treatment is usually 1 "dive" but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? If we ascend too quickly, the air bubble will reform.
Decompression sickness: This occurs primary with scuba divers who ascended too quickly. Scuba divers generally breath mixed gas, most commonly air (21% O2, ~79% N2) or nitrox (35% O2, ~65% N2). As someone is diving, the nitrogen they breath is also dissolved into their blood since they are at a pressure greater than 1.0 ATA. If a diver ascends too quickly, the nitrogen dissolved in the blood will rapidly reform air bubbles in the blood. We just mentioned how that is problematic.
Since air bubbles can go everywhere in circulation, the symptoms are variable ranging from headache, vertigo, nausea, joint pain, chest pain, stroke symptoms, loss of bowel/bladder function, etc. The treatment for this is to recompress the patient and very slowly ascend in the HBO chamber. Treatment is usually 1 dive but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? Again, if we ascend too quickly, the air bubble will reform.
Wound related conditions: there are roughly 15 approved diagnoses for HBO by Medicare in the USA. This is important to mention because if a condition is not covered, paying out of pocket is extremely cost-prohibitive. Insurance is billed $6,000 per treatment! Some of the most common conditions treated are osteoradionecrosis, soft-tissue radionecrosis, irradiation cystitis with hematuria, and refractory chronic osteomyelitis. Wounds created from radiation exposure have the best evidence to support the use of HBOT. These are considered outpatient conditions so patients come to be treated Monday-Friday. We dive to 2.4 ATA for 120 minutes. At minimum, patients are prescribed 20 dives but most treatment protocols for radiation induced injuries is at least 40 dives.
As you can see, this is a HUGE commitment for the patient. One dive is not enough for these wound related conditions. As a hyperbaric provider, I can say that we have patients with such significant symptom relief from HBO. For example, irradiation cystitis with hematuria is extremely debilitating. Patients are fatigued from chronic blood loss, deal with painful bladder spams and pelvic pain, pain with urination, and increased frequency. The blood can clot and obstruct their urethra or foley catheter. Symptoms like this limit quality of life. HBOT makes a huge difference for them.
Benefits
Anyone who has barriers to wound healing can benefit from HBO. Barriers include vascular disease, CKD, COPD, DM, heart failure, and immunocompromised status. The goal is symptom resolution/improvement or healing of the wound. Some patients get approved for far more treatments than we typically do. Usually the maximum insurance will cover is 60. However, in some situations, the clinical benefit of continued treatments is recognized by insurance and treatment is extended.
As a provider, I get to know these patients pretty well. They show up every day that I am staffing in HBO and it is rewarding to see them improve. Compared to my critical care role, this is a nice change of pace.
Adverse Reactions and Risks
There are risks and side effects to HBO. The most common are barotrauma, pneumothorax, seizure, temporary worsening of cataracts/vision, and abdominal distention.
Barotrauma of the ears and sinuses is by the most common issue we face in HBOT. If patients are not able to clear their ears as they descend ("pop" their ears), they can rupture their ear drums. Patients that cannot descend without extreme pain may need myringotomy tubes (ear tubes) to assist with equalizing pressure.
Seizure is a risk of HBOT and that primarily comes from oxygen reducing the seizure threshold. We mitigate this with "air breaks". These are 5 minutes intervals of the treatment where the patient is receiving air rather than 100% O2. Example, we treat at 100% for 30 minutes, have a 5 minute air break, repeat x 2. Obviously the people at highest risk are those with epilepsy or taking seizure threshold reducing medications.
HBOT can worsen cataracts and vision temporarily. The mechanism of this is poorly understood but we know it is reversible. Distance vision is affected the most.
Contraindications
The only absolute contraindication to HBOT is an untreated pneumothorax. There are many relative contraindications that require a risk benefit analysis. An example of this is pregnancy. HBOT has not been thoroughly studied in pregnancy and is not recommended EXCEPT in cases of CO poisoning where we know that the CO concentration is higher in fetal circulation than maternal. Always treat a pregnant person with CO poisoning.
Other potential contraindications include use of certain chemotherapy agents, COPD with blebs/bullae, severe heart failure, epilepsy, sinus/HEENT disease, claustrophobia, certain implanted devices, or active infection.
With certain chemo agents, they can lower the seizure threshold putting patients at higher risk of seizure in the chamber. People with COPD and blebs are at risk of those blebs popping under pressure and causing acute respiratory distress. People with heart failure can experience flash pulmonary edema after an HBO treatment. If people are claustrophobic, obviously spending time in a monoplace chamber can trigger panic attacks. At my center, we sometimes have people referred to our multiplace chamber for exactly that reason.
Most implanted medical devices are HBOT compliant. Generally, pacers and other devices are tested at 4.0 ATA of pressure. We double check with the manufacturer that the device is compliant. If it isn't, we cannot safely treat and have to deny the consult.
Obviously, if someone is sick, we don't want them in the chamber. Particularly colds, severe allergies, fever, or anything that is affecting HEENT. People with acute sinus infection are unable to clear sufficiently to dive. Even if they can clear, they feel miserable. No need to go through that.
Safety Issues
I mentioned that high O2 environments are at risk for explosion. Safety is the number one concern with any chamber. The goal is to reduce risk of fire by removing fabrics that create static (anything synthetic), removing electronic devices that are not HBOT approved, and going through multiple levels of safety checks for patients and for chamber preparation.
At our chamber, only 100% cotton is allowed in the chamber. All patients have special scrubs that they wear during treatment. No electronic devices can be brought in the chamber which includes phones, tablets, laptops, e-readers, watches, pagers, etc. We do have HBOT approved IV pumps and radio headsets that we use. These have been tested at 4.0 ATA. The radio headsets are for the attendant (staff member) who is in the chamber and this is also for safety purposes. Since we have a mulitplace chamber, a staff member is always in the chamber with the patient(s).
One thing I do want to address is that some people are concerned about putting a patient with active cancer into the chamber. There is concern that the high O2 environment will "feed" the cancer. There is simply not data to support this. Active cancer is not a contraindication to HBOT.
And there you have it! The down and dirty of HBOT! Hopefully you learned something cool. If you think you have a patient who would benefit, find your local HBOT provider. We are always happy to talk with you about the process. If you care about a soapbox of how insurance companies suck, see below. :-D
Soapbox: I will say, I have definitely been frustrated with insurance companies. They are the gatekeepers of this treatment. You can have several providers supporting the use of treatment and an insurance company can still say "no". Very frustrating.
A prime example of this are patients who have avascular necrosis that is steroid or chemotherapy induced. These are often younger patients (late teens, early 20s) who have/had leukemia of some kind. They end up having necrosis at a joint, usually the femoral head, that will likely result in complete joint replacement at a young age. No orthopedic surgeon wants to replace joints on a young person. It comes will all kind of problems and always needs revision later in life.
Insurance companies will say "we only cover radiation induced necrosis" because that is what the literature supports. Yes, they are correct that the vast majority of studies support HBOT for radiation induced injury. However, the pathophysiology of the tissue destruction, while a little different, ends up with the SAME problem. There are studies that support HBOT use in these situation but not nearly as many as radiation induced injury. The result is that patients suffer, get a joint replacement they could have avoided (or postponed until they are fully developed), and generally are shafted.
*end soapbox*
#pablr#medblr#nurblr#pharmblr#physician assistant#physician associate#doctor#physician#hyperbaric medicine#hbot#hbo#medicine#oxygen therapy
6 notes
·
View notes
Text
Five Years as a PA-C
Well, 5 years as a PA-C really snuck up on me. I was at work on Tuesday and while checking my email, my hospital send one of those "Congrats on 5 years! Pick a cool thing from this random website!" To be perfectly frank, I was a little dumb struck.
In many ways, it just doesn't seem like that much time has passed. I work in such a fast paced, stimulating environment, constantly learning new things, that I didn't really FEEL the time. Well, at least the last 3 years. The first 2 were long and arduous.
Looking through my archives, I faithfully did reflections after the first and second years. Somehow skipped the others. Never too late to get back in it.
Lessons Learned
There are people that work in healthcare for a pay check. Let your frustration with that slide away.
Some people are just assholes. Don't overthink that. Again, let that shit go.
Some parts of medical education/residency are completely ridiculous, unfair, and unsafe. Try to change what you can (especially the unsafe).
Stand up for your boundaries. I was offered a chance to "move up" into management. I declined because I knew I would hate my job if I took on admin. Don't apologize for setting this boundary.
Cultivate relationships with your coworkers and hang out with them outside of work. This is so important for our critical care team. I believe it enhances our ability to work well together.
Use your vacation time.
Some families or patients will suck you dry. Prepare yourself for those interactions and have a plan to decompress what you absorb.
Always be excited to learn. Medicine is changing every day. Learning is a foundation of the profession.
The best decision I made was changing specialties. The second best decision I made was to turn down a management opportunity. You can challenge yourself in ways that do not result in more pay, more responsibility, or more stress. I am wanting to get my chest tube placement verification done this year. Would love to add paras to that. I want to expand the teaching I have done with my PA school and possibly guest lecture on other topics. There are a lot of things that advance a career that aren't management. For me, that is desirable.
So what next? Well, some of you know that I have some intense outside of work things going on. For now, I am hanging out where I am. Probably will go to a conference this year. Probably will do more teaching. I'm ok with that. I love critical care and I have no plans to leave it any time soon.
11 notes
·
View notes
Text
From the Archives: Compartmentalizing
I recently admitted a patient where there was literally nothing we could do when the patient got there except keep them alive long enough for family to say goodbye. Awful things happen to all kinds of people. Families wail into the void when they realize they will never talk to their loved one again. It is a completely mentally bankrupting thing to see and experience. Being able to compartmentalize the anguish and pain we see on a daily basis is a big skill for people in health care.
Medicine and Death : The stuff I wasn't prepared for.
These last 4.5 years of med school, have been all about learning anatomy and physiology and cases and drug reactions and clinical features on paper and fancy books..... A heaven and hell of difference from what actually practicing medicine, the reality of it, entails.
Day before yesterday a 6 year old girl died during my shift. She came in with RTA and severe SAH, admitted around 4 pm, received appropriate drugs....... around 8:30 pm I get a call-book (similar to a paging, in Western-speak) from the ward (which was already too late in coming, I realise now) that she's gasping. I was the sole on-call doc in the neurosurgery ward for the night, amidst a 40 hour shift in the general surgery ER. I go in and within 10 seconds I knew she'd already expired.... No carotids, no breaths, no heart sounds, her pupils fixed and dilated in the blank stare of the dead....her skin was still warm under the layers of sheets she was bundled in..... The oxygen pump and mask was still on, uselessly.
I kinda felt numb at that moment, tbh. Never in my life had I been prepared to face that kind of crisis.
I frantically added the emergency drugs, ran to the ward and asked the nurse to administer them stat, called the neurosurgeon visiting (who was off duty), sent him the CT scan photos as a last ditch effort, even though I knew it would be useless.
Then after an hour I had to break the news to the parents. The family belonged to the rural poor, the father was barely able to sign his name in shaky, unpracticed hands, under my written declaration of his little girl's death.
Strangely enough, it was just a matter of half an hour. A very short life ended, without any pomp or rejoice, the last breath drawn before I could even reach there to do anything meaningful.
It was the most horrible fucking experience of my life till now. I still haven't stopped to process everything, my brain went into damage control mode and shut down any and all rewinds of this whole thing, until now.
I instinctively turn to drawing/painting whenever I need to shut down and distance myself from reality. It's something cathartic and meditative for me. It's strange how not all art is born from joy and happiness. The vast seas I painted yesterday (below), well after midnight, because I couldn't fall asleep, was probably the effort of my subconscious to let my heart be free, even if for a little while.


I'm not sure I can keep doing this on and on, over and over. Right now, this whole prospect of taking responsibility for hundreds of lives each day, seems like a surreal, humongous task. Maybe after witnessing 10 or 15 or a hundred more deaths, this incident will feel insignificant, lost amidst all the other chaos. Until then, I'll continue to feel out of balance, skeptical of each and every of my decision : did I do the right thing? Was there something else I could do? What if this happened instead of that? What if....?
#pablr#pa-c#md#do#medblr#medicine#health care#nurblr#pharmblr#physician assistant#physician associate#doctor#physician#critical care#handling patient death#originstory
170 notes
·
View notes
Text
I am sorry you are experiencing this. When I was contemplating what speciality to work in, this was the biggest reason why I avoided ED.
I had a day where I see my future trajectory of burnout in the ED. I had so many argumentative chronic abdominal pain patients today. I’m tired of arguing. I’m known for being extremely nice but in this environment I’ve had to learn to be firm. I’m tired of everyone thinking the ED is a diagnostic center. The purpose is to stabilize and treat life threatening conditions. Not to run hundreds of tests to see what you may or may not have when your life isn’t in immediate danger. And when the extra tests you demanded are normal you are still going home. Thank you and goodbye.
32 notes
·
View notes
Text
Bad at This
I am royally bad at this updating thing. Actually, when I reflect on creating the PAblr community, I recall that as people graduated and practiced, I saw less and less of them. I sort of get it. I am in a different place in practice where I *somehow* have enough confidence that I do not need to reach out here as much. That is both a good and a sad thing.
In my journey to PA school, Tumblr and the PAblr community was a constant rock of support. And I needed it. There were only so many times I could rant to Mr Poppen before he was like "I support you but I can't relate." Y'all relate. I thank you for that.
While this blog transforms as I do, I'll still be around. I am planning some educational ICU content for the sole purpose of utilizing some nervous energy to benefit others.
I guess that's what this has been all along - using anxiety and transforming it into a positive thing.
#pablr#medblr#nurblr#pharmblr#physician assistant#physician associate#pa-s#pa-c#pre-pa#health care careers#medicine
5 notes
·
View notes
Text
This is a great basic description. While I learned to interpret x-rays in school, we were not taught how to interpret CT or MRI, much less HOW they worked. Honestly, if you know HOW they work, interpreting them becomes easier.
Radley's sneaky spicy cheatsheet for imaging modalities!
X-ray
Super quick zappyzap! One-to-three images in the UK, unless you're doing something fancy like stitching scolio spines. Fast, cheap, and very good at looking at bones / basic abdominal organ pathology / size of your heart. You hold still for like, one second. Then - ZOOP! You're done.
CT
X-ray BUT MORE X-RATED! Much, much higher dose, because it's basically taking a ridiculous amount of x-ray images while spinning the gantry (the 'camera', so to speak) around you at very high speed, and then algorithmically compiling those images to create a 3d digital construction of your innards! Very useful for looking at internal organs, especially with contrast media that makes pathology all shiny and pretty. Sometimes slower & always more expensive than X-ray, but much faster & cheaper than MRI. Patients can't move for the duration (unless you're doing cardiac stuff that takes a picture only in the lull between heartbeats - very cool!).
MRI
CT BUT WITH MAGNETS (okay it's not really much like CT except that it creates slices of the body in all three planes). There's no ionising radiation! It produces really, really clear, gorgeous pictures that show off soft tissue beautifully! We like that!! But... it's also really slow, really expensive, and really claustrophobic. A lot of patients don't enjoy it, and who can blame 'em? Who wants to be stuck in a small tube for a half hour while it makes horrid boomy noises at you? And you're not allowed to move at all? (we don't even like you to breathe too fast or too slow!)
Ultrasound
SOUNDWAVES GO BOUNCYBOUNCE. Though it produces a relatively unclear image that you need a lotta extra training to decipher, the tech is super cheap and available, and it's very quick to use! There's no ionising radiation involved! AND you can use it for realtime imaging - so, you can see a foetus move as it happens, rather than this movement messing up your entire image, or having to be carefully planned around!
Fluoroscopy
X RAY BUT VIDEO. This is a constant (and therefore high dose) real-time 'video' taken with X-ray, which can visualise movements within the body. You can watch contrast media (shiny juice) shift around to ensure that systems are functioning correctly! You can watch surgeons push their guide wires/stents/etc. into place, to be sure they hit the right spot! Or you can inject Shiny Juice into the blood vessels and, with angiography, watch it flow around the heart/brain to find blockages!
Nuclear med
WE STICK THE RADIOACTIVE STUFF IN YOU. For instance, we give you a radioactive tracer in a solution with stuff that binds well to bony metastases.... and BOOM we can see all your bony metastases on a PET-CT/MRI because they're glowing red-hot! Or we IV a nuclear tracer into your heart and make you exercise/give you meds that raise your heart rate and BOOM we can see whether your heart has an adequate blood supply during exertion!
42 notes
·
View notes
Text
Bad
I am getting bad at this blogging thing. *Shrugs*
No big changes per se in 2024. My boss left in December and thus we are "boss-less". I suppose I should honored that a bunch of people asked me to apply...and I am. Truly. I just...administration (and its associated bs) isn't for me.
At work a week ago I had a very strange situation where a patient who was floor ready without anything concerning randomly had a respiratory code. They came in initially with a cerebellar hemorrhage and I was afraid they rebled and just shut off their respiratory drive. Or had a saddle PE. Or something. Nope, did not rebleed. Just...stopped breathing.
It was a combination of an airway issue and the location of their stroke which made it "easier" for them to stop breathing. Their respiratory code turned into a cardiac arrest but we got ROSC in 2 minutes after securing the airway. And thankfully the patient follows commands and doesn't appear to have new deficits. They'll get a tracheostomy and be on their way to recovery.
We've been hunkered down with the blizzard that rolled through. Good gawd there is so much snow. I had 2 ft drifts to clear in the driveway. Total bitch. Now it's just dead ass cold.
This time of the year makes me happy I no longer work in burn medicine. Frostbite was (and still is) one of my least favorite things to care for. The data of thrombolytics isn't great and everyone has their own thoughts on how to treat it. It almost always ends up in someone getting amputations in April or May. Plus, the neuropathy is so hard to treat and so functionally devastating for patients.
Things coming up: volunteer orchestra rehearsals will start soon. My other volunteer gig continues and hopefully will end up making a difference. Since getting a Peloton in October, I have made commitment to movement. So far, I average working out 3-4 times a week which is way the hell better than before. Even if those rides are only 15 minutes.
I am slowly becoming a person that wakes up at 04:15 to work out. It's gross but the anxiety that looms over me during the day time goes away if I just get up and do the thing. And YES I do feel more awake (though I don't WANT to admit that.)
Stay warm tumblr buddies
#pablr#pa-c#pa-s#pre-pa#medicine#physician assistant#physician associate#grad school#healthcare#critical care
5 notes
·
View notes
Text
"...but I'm not moving that fast and he is DAWDLING. Disgusting. No work ethic these days."
This post is everything.
A code status is what you want the hospital to do if your heart or breathing stops, and we've got two basic options: full code which means we do EVERYTHING and Do Not Resuscitate or DNR which means we do less than everything. There's like little add-ons like intubated or not intubated, or blood products or no blood products, but that's basic gist of it. Do you want us to try everything we can to save your life or if your heart stops, is that it? And then we take that information and put it in your chart and make it very prominent in case we need to find it quickly in an emergency. Jane Doe, 72 years old, DNR. John Whatsisname, 49 years old, full code. Like that.
Anyway I'd like to propose a third code status that we'll call "DNR!!!" This is when you not only don't want heroic measures to extend your life, you are so excited to die. I thought of this recently when getting report on a patient, and the day nurse talking to me was like, "Alice Smith, 80 years old, DNR and she will tell you that herself." And I was like, "I don't think code status is gonna come up organically," and the nurse was like, "It won't, but she'll tell you anyway." And then I introduced myself to the patient, and like three minutes in as we're talking about pain meds, she goes, "and by the way, when I'm dead, I'm DEAD. Don't be bringing me back! Every woman in my family has lived past 90, and I'm here to break that tradition! NO one needs to live that long, and I certainly don't, and frankly it's indecent for me to have made it this far. God willing the reaper will come for me any day now. I would never take actions to make him come sooner, but I'm not moving that fast and he is DAWDLING. Disgusting. No work ethic these days. And don't bother with a grave, just chuck me out the window and let the birds at me."
And I'm like "so is that a no to the tylenol"
And she was like "oh no, I'd love some tylenol and a warm blanket too. Now look at me. I've done everything I could possibly want to do in this world and quite a few things I didn't want to do, and personally I don't think I should have to keep doing things. I'd also love a cranberry juice."
Anyway. DNR!! I'm sorry to say she made it through the night completely unscathed.
26K notes
·
View notes
Text
Down to the Hour
Long time, no write. I've been on vacation and just...life happens. Work has been mostly ok. For some reason we have had fewer super critically ill people as of late. Obviously this is good for society - it's just less intellectually interesting to me.
Every time I say/think/write that I feel like an ass.
I need to complete my CME for this 2 year period. I had a TON of category 1 credits (>70) but I am still like 10 short. I now have a stack of journal articles on my desk and I am raiding SCCM's online modules. *sigh*
Don't procrastinate, y'all.
I am also getting over a cold. I am in the coughing phase and sleep like shit. It has derailed my efforts with my new Peloton! I can see why people are into it - there is a lot of diversity and is a great workout. I hopped on the bike yesterday after like a week and a half off because of my cold - oof da. It was rough.
Actually, one of the interesting things was that I was on a workout 2 weeks ago and the instructor was like "you probably have to be strong for someone in your life - you deserve 30 minutes to yourself." I thought about this immediately in the context of my job. It was honestly the first time after 5 years of critical care practice that I realized that.
A huge part of my job that I push aside is working with patient families. It is the most stressful part of my job if I am honest. Dying people are not stressful. Bleeding, mangled people are not stressful. But families in pain, that is stressful. And the amount of energy I pour into trying to clearly educate and comfort them is...enormous. I brush it off and I am realizing that I need to not.
#pablr#pa-c#pre-pa#pa-s#physician assistant#physician associate#health care#critical care#life update
9 notes
·
View notes
Text
Me After Getting a Peloton

But seriously, game changer. We got it as a prime day 1/2 thing. Super pumped about the work outs. :-D
1 note
·
View note