#PRMT Inhibitors
Text
Phase 1 study of GSK3368715, a type I PRMT inhibitor, in patients with advanced solid tumors
http://dlvr.it/SphXZs
0 notes
Text
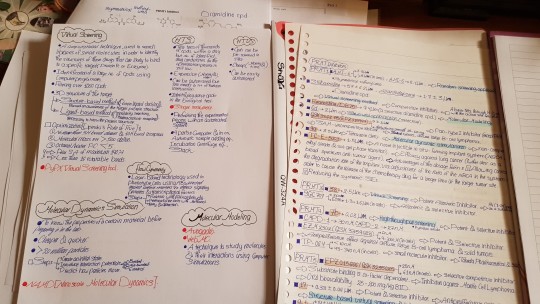



Notes & a summary of my graduation project "A review of PRMT Inhibitors"
#PRMT#PRMT Inhibitors#Drugs#Anticancer#Graduation project#Academic writing#studyblr#university study#Pharmacy#pharmacist#pharm school#pharmacy school#pharmacy student#pharmblr#medstudyblr#notes#summary#writing#studystudystudy#studying#study notes#study inspo#study motivation#studybuzz#studyinstyle#studyquill#studyspiration#studyspo#studygram#my handwriting
15 notes
·
View notes
Text
The asymmetric dimethylarginine-mediated inhibition of nitric oxide in the rostral ventrolateral medulla contributes to regulation of blood pressure in hypertensive rats
Xing Tan, Ji-Kui Li, Jia-Cen Sun, Pei-Lei Jiao, Yang-Kai Wang, Zhao-Tang Wu, Bing Liu, and Wei-Zhong Wang
Nitric oxide (NO) is characterized by its physiological and pathological roles in cardiovascular regulation. The rostral ventrolateral medulla (RVLM) is an important region for maintaining basal blood pressure (BP) and sympathetic tone. NO exerts a sympathoinhibitory effect in the RVLM. Overexpression of inducible NO synthesis (iNOS) in the RVLM increases BP, whereas bilateral microinjection of the iNOS selective inhibitor aminoguanidine into the RVLM reduced BP and heart rate (HR). On cardiac sympathoexcitatory responses NO in the RVLM exerts an excitatory effect.
Asymmetric dimethylarginine (ADMA), an endogenous inhibitor of NOS, is generated by protein arginine methyltransferases (PRMT) and eliminated by dimethylarginine dimethylaminohydrolase (DDAH). ADMA is characterized as a risk marker of cardiovascular disease events. The elevated ADMA level in plasma has been observed in many cardiovascular diseases such as atherosclerosis, coronary artery disease, stroke, and heart failure. Intravenous infusion of ADMA into healthy subjects increases systemic vascular resistance and elevates BP in a dose-related manner. ADMA plays a key role in the development and progression of salt-sensitive hypertension, associating with endothelial dysfunction in vitro and in vivo
Overactivity of the central renin-angiotensin system (RAS) plays a pivotal role in the pathogenesis of hypertension and related cardiovascular disorders. The pathological roles of angiotensin II (Ang II), a main factor of RAS, in neural mechanisms of hypertension are highly diverse. Multiple signaling pathways underlie the deleterious roles of Ang II in the RVLM in neurogenic hypertension. In the cultured endothelial cells, Ang II can increase the level of intracellular ADMA. An important goal of this study was to find out whether ADMA in the RVLM is regulated by Ang II in hypertension. The other aims in the present study were designed to determine: 1) if ADMA in the RVLM has effects on central control of cardiovascular activities; 2) if the ADMA-mediated cardiovascular effect in the RVLM is associated with increased Ang II in hypertension. Sixteen-week-old male Sprague Dawley (SD) rats, Wistar Kyoto (WKY) rats, and spontaneously hypertensive rats (SHRs) were used for this study.
In the present study, three major findings were: 1) Microinjection of ADMA into the RVLM evoked a significant increase in BP, heart rate (HR), and renal sympathetic nerve activity (RSNA), as well as a significant decrease in total NO production in the RVLM. The pressor response to ADMA was significantly blunted by pretreatment with L-arginine; 2) In the central Ang II-induced hypertensive rats and SHR, the ADMA content increased and total NO production decreased in the RVLM, which may be associated with up-regulation of PRMT1 and downregulation of DDAH1; and 3) These alterations in SHR were blunted by central infusion of losartan. This led to the conclusion that ADMA in the RVLM plays a critical role in the regulation of BP in hypertension, which is associated with increased Ang II.
ADMA is said to contribute to central regulation of BP and sympathetic outflow, associated with NO reduction. ADMA in the RVLM was increased by Ang II via upregulation of PRMT1 and downregulation of DDAH1, which inhibited the NOS activity and decreased total NO production and resulted in a high level of sympathetic tone and BP. The increased ADMA along with NO inhibition in the RVLM caused by Ang II plays an important role in the pathogenesis of hypertension. Strategies that decrease ADMA in the central nervous system may be a possible therapeutic targeting for hypertension.
Source: https://www.ncbi.nlm.nih.gov/pubmed/28392446
Raisa Monteiro
0 notes
Text
The arginine methyltransferase PRMT5 and PRMT1 distinctly regulate the degradation of anti-apoptotic protein CFLAR L in human lung cancer cells
Abstract
Background
CFLARL, also known as c-FLIPL, is a critical anti-apoptotic protein that inhibits activation of caspase 8 in mammalian cells. Previous studies have shown that arginine 122 of CFLARL can be mono-methylated. However, the precise role of arginine methyltransferase of CFLARL remains unknown. PRMT5 and PRMT1, which are important members of the PRMT family, catalyze the transfer of methyl groups to the arginine of substrate proteins. PRMT5 can monomethylate or symmetrically dimethylate arginine residues, while PRMT1 can monomethylate or asymmetrically dimethylate arginine residues.
Methods
Lung cancer cells were cultured following the standard protocol and the cell lysates were prepared to detect the given proteins by Western Blot analysis, and the protein interaction was assayed by co-immunoprecipitation (Co-IP) or GST pull-down assay. CFLARL ubiquitination level was evaluated by proteasomal inhibitor treatment combined with HA-Ub transfection and WB assay. PRMT1 and PRMT5 genes were knocked down by siRNA technique.
Results
We show that PRMT5 up-regulated the protein levels of CFLARL by decreasing the ubiquitination and increasing its protein level. Additionally, PRMT1 down-regulated the protein level of CFLARL by increasing the ubiquitination and degradation. The overexpression of PRMT5 can inhibit the interaction between CFLARL and ITCH, which has been identified as an E3 ubiquitin ligase of CFLARL, while overexpressed PRMT1 enhances the interaction between CFLARL and ITCH. Furthermore, we verified that dead mutations of PRMT5 or PRMT1 have the same effects on CFLARL as the wild-type ones have, suggesting it is the physical interaction between CFLAR and PRMT1/5 that regulates CFLARL degradation other than its enzymatic activity. Finally, we showed that PRMT5 and PRMT1 could suppress or facilitate apoptosis induced by doxorubicin or pemetrexed by affecting CFLARL in NSCLC cells.
Conclusions
PRMT5 and PRMT1 mediate the distinct effects on CFLARL degradation by regulating the binding of E3 ligase ITCH in NSCLC cells. This study identifies a cell death mechanism that is fine-tuned by PRMT1/5 that modulate CFLARL degradation in human NSCLC cells.
http://bit.ly/2I3sRTo
0 notes
Text
The asymmetric dimethylarginine-mediated inhibition of nitric oxide in the rostral ventrolateral medulla contributes to regulation of blood pressure in hypertensive rats
Xing Tan, Ji-Kui Li, Jia-Cen Sun, Pei-Lei Jiao, Yang-Kai Wang, Zhao-Tang Wu, Bing Liu, and Wei-Zhong Wang
Nitric oxide (NO) is well characterized for its physiological and pathological roles in cardiovascular regulation. The rostral ventrolateral medulla (RVLM) is a key region for maintaining basal BP and sympathetic tone. The NO precursor L-arginine microinjected into the RVLM elicits hypotension, bradycardia, and reduction in sympathetic vasomotor tone in a spontaneously hypertensive rat (SHR). Microinjection of NG-monomethyl-L-arginine (L-NMMA), a nitric oxide synthesis (NOS) inhibitor, into the RVLM induces a pressor response in hypertensive rats. Overexpression of endothelial nitric oxide synthesis (eNOS) in the RVLM causes a greater sympathoinhibition in hypertensive rats than in normotensive WKY rat. NO in the RVLM exerts a sympathoinhibitory effect. Overexpression of inducible NO synthesis (iNOS) in the RVLM increases BP in WKY rats and SHR, and bilateral microinjection of the iNOS selective inhibitor aminoguanidine into the RVLM reduces BP and heart rate (HR) in SHR. NO in the RVLM exerts an excitatory effect on cardiac sympathoexcitatory responses.
Asymmetric dimethylarginine (ADMA), an endogenous inhibitor of NOS, is generated by protein arginine methyltransferases (PRMT) and eliminated by dimethylarginine dimethylaminohydrolase (DDAH). ADMA is characterized as a risk marker of cardiovascular disease events. The elevated ADMA level in plasma has been observed in many cardiovascular diseases such as atherosclerosis, coronary artery disease, stroke, and heart failure. ADMA plays a key role in the development and progression of salt-sensitive hypertension, associating with endothelial dysfunction in vitro and in vivo.
Overactivity of the central renin-angiotensin system (RAS) plays a pivotal role in the pathogenesis of hypertension and related cardiovascular disorders. The pathological roles of angiotensin II (Ang II), a main factor of RAS, in neural mechanisms of hypertension are highly diverse. Multiple signaling pathways underlie the deleterious roles of Ang II in the RVLM in neurogenic hypertension. The balance between nitric oxide (NO) signaling and reactive oxygen species (ROS) in the RVLM is broken resulting in decreased baroreflex function, which contributes to neurogenic hypertension. The two main aims in the present study were designed to determine: 1) if ADMA in the RVLM has effects on central control of cardiovascular activities; 2) if the ADMA-mediated cardiovascular effect in the RVLM is associated with increased Ang II in hypertension. Sixteen-week-old male Sprague Dawley (SD) rats and WKY rats were used for this study.
The three major findings are that: 1) Microinjection of ADMA into the RVLM evokes a significant increase in BP, HR, and RSNA, as well as a significant decrease in total NO production in the RVLM. Moreover, the pressor response to ADMA is significantly blunted by pretreatment with L-arginine; 2) In the central Ang II-induced hypertensive rats and SHR, the ADMA content is increased and total NO production is decreased in the RVLM, which may be associated with up-regulation of PRMT1 and downregulation of DDAH1; and 3) These alterations in SHR were blunted by central infusion of losartan. ADMA in the RVLM plays a critical role in the regulation of BP in hypertension, which is associated with increased Ang II.
ADMA is confirmed to contribute to central regulation of BP and sympathetic outflow, which might be associated with NO reduction. Ang II increased ADMA in the RVLM via upregulation of PRMT1 and downregulation of DDAH1, which inhibited the NOS activity and decreased total NO production and resulted in a high level of sympathetic tone and BP. The increased ADMA along with NO inhibition in the RVLM caused by Ang II plays an important role in the pathogenesis of hypertension. Strategies that decrease ADMA in the central nervous system may be a possible therapeutic targeting for hypertension.
Source: https://www.ncbi.nlm.nih.gov/pubmed/28392446
Raisa Monteiro
0 notes
Text
Mouse Models of Overexpression Reveal Distinct Oncogenic Roles for Different Type I Protein Arginine Methyltransferases
Protein arginine methyltransferases (PRMT) are generally not mutated in diseased states, but they are overexpressed in a number of cancers, including breast cancer. To address the possible roles of PRMT overexpression in mammary gland tumorigenesis, we generated Cre-activated PRMT1, CARM1, and PRMT6 overexpression mouse models. These three enzymes are the primary type I PRMTs and are responsible for the majority of the asymmetric arginine methylation deposited in the cells. Using either a keratin 5-Cre recombinase (K5-Cre) cross or an MMTV-NIC mouse, we investigated the impact of PRMT overexpression alone or in the context of a HER2-driven model of breast cancer, respectively. The overexpression of all three PRMTs induced hyper-branching of the mammary glands and increased Ki-67 staining. When combined with the MMTV-NIC model, these in vivo experiments provided the first genetic evidence implicating elevated levels of these three PRMTs in mammary gland tumorigenesis, albeit with variable degrees of tumor promotion and latency. In addition, these mouse models provided valuable tools for exploring the biological roles and molecular mechanisms of PRMT overexpression in the mammary gland. For example, transcriptome analysis of purified mammary epithelial cells isolated from bigenic NIC-PRMT1Tg and NIC-PRMT6Tg mice revealed a deregulated PI3K–AKT pathway. In the future, these PRMTTg lines can be leveraged to investigate the roles of arginine methylation in other tissues and tumor model systems using different tissue-specific Cre crosses, and they can also be used for testing the in vivo efficacy of small molecule inhibitors that target these PRMT.Significance:These findings establish Cre-activated mouse models of three different arginine methyltransferases, PRMT1, CARM1, and PRMT6, which are overexpressed in human cancers, providing a valuable tool for the study of PRMT function in tumorigenesis.See related commentary by Watson and Bitler, p. 3
http://bit.ly/2F1epcd
0 notes
Text
Mouse models of overexpression reveal distinct oncogenic roles for different type I protein arginine methyltransferases
Protein arginine methyltransferases (PRMTs) are generally not mutated in diseased states, but they are overexpressed in a number of cancers, including breast cancer. To address the possible roles of PRMT overexpression in mammary gland tumorigenesis, we generated Cre-activated PRMT1, CARM1 and PRMT6 overexpression mouse models. These three enzymes are the primary Type I PRMTs and are responsible for the majority of the asymmetric arginine methylation deposited in the cells. Using either a keratin 5-Cre recombinase (K5-Cre) cross or an MMTV-NIC mouse, we investigated the impact of PRMT overexpression alone or in the context of a HER2-driven model of breast cancer, respectively. The overexpression of all three PRMTs induces hyper-branching of the mammary glands and increased Ki-67 staining. When combined with the MMTV-NIC model, these in vivo experiments provided the first genetic evidence implicating elevated levels of these three PRMT in mammary gland tumorigenesis, albeit with variable degrees of tumor promotion and latency. In addition, these mouse models provided valuable tools for exploring the biological roles and molecular mechanisms of PRMT overexpression in the mammary gland. For example, transcriptome analysis of purified mammary epithelial cells isolated from bigenic NIC-PRMT1Tg and NIC-PRMT6Tg mice revealed a deregulated PI3K/AKT pathway. In the future, these PRMTTg lines can be leveraged to investigate the roles of arginine methylation in other tissues and tumor model systems using different tissue-specific Cre crosses, and they can also be used for testing the in vivo efficacy of small molecule inhibitors that target these PRMT.
https://ift.tt/2CYTZzu
0 notes
Text
CARM1 Is Essential for Myeloid Leukemogenesis but Dispensable for Normal Hematopoiesis
Publication date: 11 June 2018
Source:Cancer Cell, Volume 33, Issue 6
Author(s): Sarah M. Greenblatt, Na Man, Pierre-Jacques Hamard, Takashi Asai, Daniel Karl, Concepcion Martinez, Daniel Bilbao, Vasileios Stathais, Anna McGrew-Jermacowicz, Stephanie Duffort, Madhavi Tadi, Ezra Blumenthal, Samantha Newman, Ly Vu, Ye Xu, Fan Liu, Stephan C. Schurer, Michael T. McCabe, Ryan G. Kruger, Mingjiang Xu, Feng-Chun Yang, Daniel Tenen, Justin Watts, Francisco Vega, Stephen D. Nimer
Chromatin-modifying enzymes, and specifically the protein arginine methyltransferases (PRMTs), have emerged as important targets in cancer. Here, we investigated the role of CARM1 in normal and malignant hematopoiesis. Using conditional knockout mice, we show that loss of CARM1 has little effect on normal hematopoiesis. Strikingly, knockout of Carm1 abrogates both the initiation and maintenance of acute myeloid leukemia (AML) driven by oncogenic transcription factors. We show that CARM1 knockdown impairs cell-cycle progression, promotes myeloid differentiation, and ultimately induces apoptosis. Finally, we utilize a selective, small-molecule inhibitor of CARM1 to validate the efficacy of CARM1 inhibition in leukemia cells in vitro and in vivo. Collectively, this work suggests that targeting CARM1 may be an effective therapeutic strategy for AML.
Graphical abstract
Teaser
Greenblatt et al. show that loss of the protein arginine methyltransfersase CARM1 minimally impacts normal hematopoiesis but strongly impairs leukemogenesis by regulating cell-cycle progression, myeloid differentiation, and apoptosis. Targeting CARM1 reduces AML growth in primary patient samples and mouse models.
https://ift.tt/2JuIaoA
0 notes