#abdominal effusion
Text
guess who forgot the (extended) light criteria at a practical exam... and also said “atelectasia” when it was obviously an effusion in the x-ray.... and discarded pleuroascites bc it was unilateral and with no evident (abdominal) ascites....
what a nice semester, i think i’ll do it again
#i just hope i won’t actually fail this course#and if i do#i hope i don’t lose my scholarship#bc that’s a lot of money i don’t have at the moment
28 notes
·
View notes
Text
Ascites in Dogs

(Source: Mobile Vet Clinic)
Definition
Ascites (also known as Malignant Ascites, Abdominal Effusion or Free Abdominal Fluid) is a condition in which fluid fills up the space of a dog’s abdomen. This condition had the potential to be life threatening, as the buildup of the fluid exerts pressure onto the chest cavity, which causes difficult in breathing and leading to other negative symptoms. Additionally, though the ascites fluid is generally made up of a combination of lipids, bile acids and proteins, closely examining the composition can tell the veterinarian what the underlying cause may be.
Causes
There are various causes of ascites— most of them related to an organ failure —including, but not limited to:
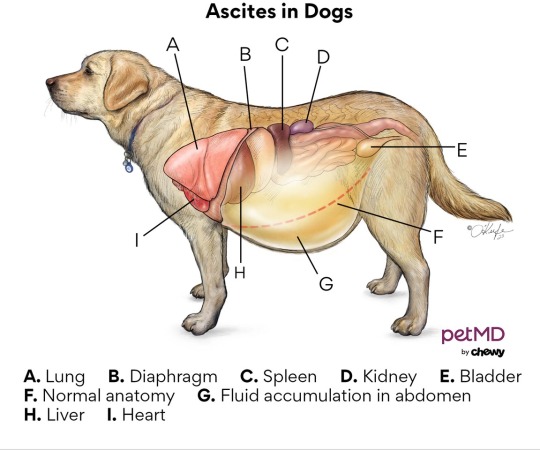
(Source: PetND)
1. Right side heart failure
2. Heartworm disease or dialated cardiomyopathy
3. Liver disease (hepatitis, portal hypertension, etc)
4. Infection in the abdominal lining (Peritonitis)
5. Ingestion of poison or toxins
6. Lack of protein
7. Presence of cancer or tumours
Symptoms
Should a dog display the following symptoms for a concerning amount of time, take it to a veterinarian for an examination.
1. Lethargy/Weakness
2. Decreased appetite
3. Excessive bloating of stomach/abdomen
4. Sudden weight gain
5. Excessive panting or difficulty breathing
6. Pale or discoloured gums
7. Coughing
8. Diarrhea
Examination, Diagnosis & Treatment
During the physical examination, the veterinarian can use ultrasound, x-rays, chemistry panel, CBC (complete blood count), palpating (touch) and urinalysis, along with examining the fluid contents to diagnose and determine the cause of the ascites.
The treatment for ascites has multiple steps. First, the veterinarian drains the fluid to facilitate the dog’s breathing and for its comfort (this is only a temporary solution, as the fluid will build back up). This is done by inserting a needle into the dog’s abdomen and using an attached tube to draw out the fluid.


Then, the vet needs to address the underlying causes. For instance, if the dog has a tumour or damaged organs, a surgery may be required. Or if the problem is that the dog lacks protein, then a transfusion or special diet is recommended.
Unfortunately, there are some cases where the condition cannot be cured. This is especially common for older dogs.
#dogblr#doglover#animals#veterinarian#veterinary#animal facts#vetblr#doggo#veterans#animal medicine#medicine#vet#animal health#dog tips
3 notes
·
View notes
Text
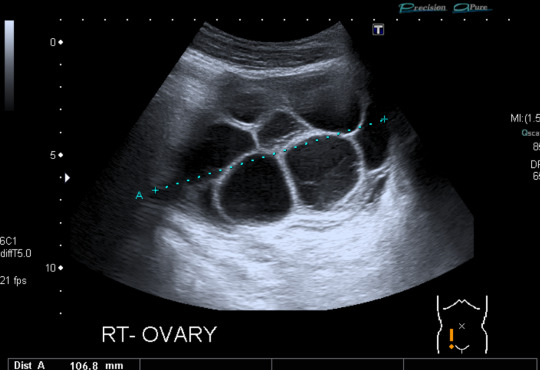

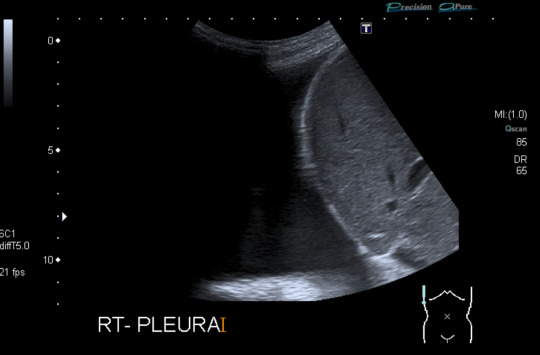
Today's case is a pelvic ultrasound of a 35-year-old woman who presented with abdominal pain and bloating 9 days after initiating controlled ovarian hyperstimulation in preparation for IVF. Ultrasound reveals enlarged ovaries with multiple large follicles, ascites, and pleural effusions. Findings are compatible with ovarian hyperstimulation syndrome (OHSS) which occurs in approximately 5% of women undergoing ovarian stimulation. Fluid shift results in hemoconcentration and oliguria. Treatment is supportive and may include paracentesis or thoracentesis to relive discomfort from accumulated fluid. Severe cases can be fatal, so patient education, prompt recognition and timely intervention are key. Risk factors include PCOS and prior OHSS. Younger age and low body weight are not good predictors of risk, as was previously posited by some papers.
Case courtesy of René Pfleger, Radiopaedia.org, rID: 29070
3 notes
·
View notes
Text
“Belle Roe,” 21 (USA 2009)
“Belle’s” real name is unknown because her case is reported from a medical journal. She has been given the last name Roe after the court decision that led to the deaths of so many pregnant people and babies across America.
Belle was a 21-year-old American with no health problems whatsoever. She should have been able to live a long life, but instead she was sold the abortion pill from a legal facility in 2009 and died 12 days later.
Belle took the lethal pills when she was 7 weeks pregnant. 6 days after beginning the abortion, she suffered from severe abdominal cramping, vomiting and diarrhea. On Day 7 she was brought to the hospital with dangerously low blood pressure, tachycardia, pleural effusions, ascites and massive infection. Oddly enough, she did not have a fever despite the fact that she was dying from infection. This is a phenomenon that has been documented in multiple cases as a result of the RU-486 abortion pill.
Despite emergency surgery and hospitalization, Belle died of severe sepsis, kidney failure and DIC (disseminated intravascular coagulopathy). The organs in her reproductive system were necrotizing. Analysis confirmed the presence of Clostridium sordellii infection. C. sordellii has been known to grow out of control and cause raging infections after use of the abortion pill.
Despite what the abortion industry tells the public, the abortion pill is not safe. Deaths like these are not nearly as rare as abortion corporations claim. Multiple abortion supporters have also pressured abortion pill clients to lie to ER staff and claim they are suffering a miscarriage. Despite what these abortion supporters claim, the symptoms and necessary care are NOT identical for an abortion and a miscarriage. As the study noted, doctors “should be aware of common clinical features, including abdominal pain, hypotension, tachycardia, third-space fluid accumulations, hemoconcentration, and marked leukemoid response, typically without fever. In patients with this presentation, a high index of suspicion for this syndrome and early aggressive treatment are needed.” Further study has shown that misdiagnosis of abortion side effects as miscarriage is a serious risk for medical problems requiring hospitalization. Those whose abortions were miscoded as miscarriages in the ER were more likely to be hospitalized for any reason than women whose abortions were accurately reported. ER patients whose chemical abortions were miscoded further exhibited a pattern of multiple hospitalizations in the 30 days following their abortions – the number of hospital admissions per patient was 78% higher in the miscoded group.
Pregnant people deserve better than the abortion pill, which is unsafe even when it’s legal.
#abortion#pro choice#pro life#tw abortion#tw murder#abortion debate#unsafe yet legal#tw ab*rtion#tw death#unsafe but legal#abortion kills women#kill pill#death from legal abortion#abortion pill#abortion is not healthcare
4 notes
·
View notes
Text
we get some wild referrals...had a cat come in for abdominal effusion recently and the rDVM had given it Lasix and Convenia?
Lasix aka furosemide is a diuretic, so you give it when you're thinking right-sided heart failure, which can cause abdominal effusion. but cats almost never get right-sided heart failure, they get left-sided heart failure, which causes pulmonary edema & pleural effusion. aka they get fluid in their chest, not the abdomen. certainly heart disease is on the rule out list, but it shouldn't be anyone's first assumption.
Convenia is an injectable antibiotic, so I assume they were thinking about infectious disease as a possibility, which again isn't crazy. but Convenia is for, like...skin infections? small wounds and abscesses in cats that refuse to take oral medications? I've never seen anyone use it for anything more serious. certainly not for FIP, lol
but like...honestly, without an acute trauma history, in an indoor-only senior cat with relatively normal blood work, realistically this kind of thing is going to be cancer. carcinoma, sarcoma, IDEK what else, but definitely cancer. tumors were confirmed by ultrasound for this patient, although I don't think they went as far as biopsying anything.
it was just one of those head scratching "what were they thinking?" cases. up there on my list along with the place that once sent us an unblocked cat for hospitalization with his urinary catheter just...open. not attached to a collection set, not even capped off briefly for travel after the bladder was emptied, just...open. dribbling urine and exposing the patient to urinary tract infection. what on earth
3 notes
·
View notes
Text
Assessment of Bones and Soft Tissue on Chest X-Ray - An Article by Prognosys Medical System
Chest X-rays are a commonly performed diagnostic imaging test that provides valuable information about the bones and soft tissues within the chest cavity. This article aims to explore the assessment of bones and soft tissue on chest X-rays and the significance of these findings in clinical practice. Understanding the interpretation of these images is crucial for healthcare professionals involved in the care of patients with chest-related conditions.
Assessing Bones on Chest X-Ray
One of the primary objectives of a chest X-ray is to evaluate the bones within the chest cavity. The ribs, sternum, and clavicles are the main structures assessed in this regard. Abnormalities such as fractures, dislocations, or bony lesions can be visualized on the X-ray images. Fractures may appear as thin lines or breaks in the continuity of the bone. Dislocations can be seen as abnormal alignment or separation of bone ends. Bony lesions, such as tumors or metastases, may manifest as areas of abnormal density or destruction.
Soft Tissue Assessment on Chest X-Ray
In addition to bones, chest X-rays also allow for the assessment of soft tissues within the chest cavity. This includes the evaluation of the lungs, heart, mediastinum, and diaphragm. Abnormalities in these structures can provide important diagnostic clues for various respiratory and cardiovascular conditions.
The lungs are the most prominent soft tissue structures seen on a chest X-ray. They are evaluated for the presence of masses, infiltrates, consolidation, or pleural effusions. Masses can indicate tumors or infections, while infiltrates and consolidation may suggest pneumonia or other lung pathologies. Pleural effusions, which are the accumulation of fluid in the pleural space surrounding the lungs, can be observed as blunting of the costophrenic angles or meniscus-shaped opacities.
The heart and mediastinum are assessed for size, shape, and position on chest X-rays. Cardiac enlargement may be indicative of conditions such as congestive heart failure or cardiomegaly. The mediastinum, which is the central compartment of the thoracic cavity, houses various structures including the thymus, esophagus, and major blood vessels. Any abnormalities in these structures can be identified on the X-ray images.
The diaphragm, a dome-shaped muscle that separates the chest cavity from the abdominal cavity, can also be evaluated on chest X-rays. Its position, shape, and movement can provide important information about the integrity of the diaphragm and its function. Diaphragmatic abnormalities may be observed in conditions such as diaphragmatic hernias or paralysis.
Significance in Clinical Practice:
Assessing bones and soft tissue on chest X-rays is essential in the diagnosis and management of various respiratory, cardiovascular, and musculoskeletal conditions. The findings on these images can guide healthcare professionals in formulating appropriate treatment plans and further diagnostic investigations.
Conclusion:
In conclusion, the assessment of bones and soft tissue on chest X-rays plays a crucial role in the evaluation of patients with chest-related conditions. By carefully analyzing these images, healthcare professionals can identify fractures, dislocations, bony lesions, as well as abnormalities in the lungs, heart, mediastinum, and diaphragm. This enables accurate diagnosis and appropriate management of patients, leading to improved outcomes.
Prognosys Medical Systems has expanded its capabilities from manufacturing X-ray equipment to single detector solutions, dual detector solutions, floor mounted systems, ceiling suspended systems, floor to ceiling systems, mobile system, line powered and battery-operated systems and a range of C arms to offer the most comprehensive design solutions under one roof.
Few of the Diagnostic Imaging (Chest X-Ray) Systems offered by Prognosys Medical Systems:
PRORAD 2FC - Single
PRORAD 2FC - Dual
PRORAD 2FC – Floor to Ceiling – Single
PRORAD 2FC – Floor to Ceiling – Dual
Click the links to Know More about Prognosys Medical Systems Product Range and Request for Quote.
Contact us for more information:
– Content Team
Prognosys Medical Systems
[email protected]
0 notes
Text
Top Uses of Chiba Needles in the Medical Field
Chiba needles, also known as Chiba biopsy needles, are thin and sharp medical instruments commonly used in various procedures within the medical field. These specialized needles have become an essential tool for physicians and healthcare professionals due to their versatility and effectiveness in a wide range of medical applications.
From diagnostic biopsies to therapeutic injections, Chiba needles have revolutionize the way medical procedures are perform, providing accurate and efficient results. In this article, we will discuss the top uses of Chiba needles in the medical field, highlighting their importance and impact on patient care.
What are chiba needles?
Chiba needles are thin, flexible needle that are use in various medical procedures to access specific areas of the body with precision. They are named after the Japanese radiologist who first introduced them, Dr. Chiba. These needles come in different lengths and gauges, making them versatile tools for healthcare professionals.
Top chiba needle applications in the medical field
1.Diagnostic Procedures
One of the primary use of Chiba needle is in diagnostic procedures such as biopsies and aspirations. These needles allow doctors to obtain tissue or fluid samples from deep within the body with minimal trauma to the patient. This is crucial in diagnosing conditions such as cancer or infections.
2.Pain Management
Chiba needle are also use in pain management procedures such as nerve blocks and epidural injections. By delivering medication directly to the source of pain, these needles can provide targeted relief for patients suffering from chronic pain conditions.
3.Biopsy Procedures
When it comes to performing biopsies, Chiba needle are essential tools for obtaining tissue samples from organs such as the liver, kidneys, or lungs. These needles are design to penetrate deep tissues safely and accurately, making them invaluable in the diagnosis of various diseases.
Read More : How to Choose the Right Biopsy Needle for Your Practice
4.Interventional Radiology
In the field of interventional radiology, chiba needle play a crucial role in procedures such as percutaneous drainage or ablation. These needles allow radiologists to access and treat tumors or fluid collections under imaging guidance, offering minimally invasive alternatives to traditional surgery.
5.Drainage Procedures
Chiba needles are commonly employ for various drainage procedures, including thoracentesis (draining fluid from the pleural space), paracentesis (draining fluid from the abdominal cavity), and pericardiocentesis (draining fluid from the pericardial sac). The sharpness and flexibility of Chiba needles facilitate smooth insertion and effective drainage, crucial for managing conditions such as pleural effusion and ascites.
6.Minimally Invasive Surgery
In minimally invasive surgical techniques such as laparoscopy and percutaneous procedures, Chiba needles find application in tasks such as tissue sampling, vessel cannulation, and suture placement. Their slender profile and precise control make them invaluable instruments for surgeons performing complex procedures through small incisions.
Conclusion: The Versatility of Chiba Needles
In conclusion, chiba needle are versatile instruments that have revolutionized the way medical procedures are performed. From diagnostic biopsies to pain management interventions, these needles continue to be indispensable tools in the medical field. So, the next time you hear about Chiba needle, remember their significant impact on patient care and the advancement of medical technology.
Source : Top Uses of Chiba Needles in the Medical Field
#Chiba Needles#Chiba biopsy needles#medical instruments#medical procedures#biopsies injections#Medical Device#Medication#Healthcare#Needle Manufacturers#Needle Suppliers
0 notes
Text
Viruses, Vol. 16, Pages 462: Serologic, Virologic and Pathologic Features of Cats with Naturally Occurring Feline Infectious Peritonitis Enrolled in Antiviral Clinical Trials
Feline infectious peritonitis (FIP) is a multisystemic, generally lethal immuno-inflammatory disease of domestic cats caused by an infection with a genetic variant of feline coronavirus, referred to as the FIP virus (FIPV). We leveraged data from four different antiviral clinical trials performed at the University of California, Davis. Collectively, a total of 60 client-owned domestic cats, each with a confirmed diagnosis of naturally occurring FIP, were treated with a variety of antiviral compounds. The tested therapies included the antiviral compounds GS-441524, remdesivir, molnupiravir and allogeneic feline mesenchymal stem/stroma cell transfusions. Four client-owned cats with FIP did not meet the inclusion criteria for the trials and were not treated with antiviral therapies; these cats were included in the data set as untreated FIP control cats. ELISA and Western blot assays were performed using feline serum/plasma or ascites effusions obtained from a subset of the FIP cats. Normalized tissue/effusion viral loads were determined in 34 cats by a quantitative RT-PCR of nucleic acids isolated from either effusions or abdominal lymph node tissue. Twenty-one cats were PCR “serotyped” (genotyped) and had the S1/S2 region of the coronaviral spike gene amplified, cloned and sequenced from effusions or abdominal lymph node tissue. In total, 3 untreated control cats and 14 (23.3%) of the 60 antiviral-treated cats died or were euthanized during (13) or after the completion of (1) antiviral treatment. Of these 17 cats, 13 had complete necropsies performed (10 cats treated with antivirals and 3 untreated control cats). We found that anticoronaviral serologic responses were persistent and robust throughout the treatment period, primarily the IgG isotype, and focused on the viral structural Nucleocapsid and Membrane proteins. Coronavirus serologic patterns were similar for the effusions and serum/plasma of cats with FIP and in cats entering remission or that died. Viral #RNA was readily detectable in the majority of the cats in either abdominal lymph node tissue or ascites effusions, and all of the viral isolates were determined to be serotype I FIPV. Viral nucleic acids in cats treated with antiviral compounds became undetectable in ascites or abdominal lymph node tissue by 11 days post-treatment using a sensitive quantitative RT-PCR assay. The most common pathologic lesions identified in the necropsied cats were hepatitis, abdominal effusion (ascites), serositis, pancreatitis, lymphadenitis, icterus and perivasculitis. In cats treated with antiviral compounds, gross and histological lesions characteristic of FIP persisted for several weeks, while the viral antigen became progressively less detectable. https://www.mdpi.com/1999-4915/16/3/462?utm_source=dlvr.it&utm_medium=tumblr
0 notes
Text
Tonight, I participated in something so random, yet so real.
I was scrolling Reddit, get ready for bed. I did one final refresh and a post caught my attention titled “cat in crisis”.
I read the post - someone visiting my state and at a hotel trying to get a ride to a 24 hour clinic to have a cat evaluated that was screaming in pain.
I respond with an appropriate clinic.
The poster responds with how long it will take to walk.
I let him know I am willing to help. In my car and away I zoom, 20 minutes from pick up.
In the interim, he has obtained multiple towels to purrito the cat and a box for transport.
We get to where she is, she’s seriously hurt. So hurt she won’t run away, won’t even move. We manage to wrestle her, as gently as possible, from under a car, in the towels and we’re off.
Turns out he’s in town for collegiate hockey. We make small talk. He’s effusive, blown away by the help.
We get to the clinic. A wonderful doctor evaluates. Things immediately don’t look good. Her temperature is low. Her third eyelids are present, half occluding her eyes, she’s clearly having neurological issues- legs stretching and contracting. She’s crying the whole time.
And this human being I have never met before chooses to do diagnostics- FeLV/FiV first -which is negative. Then to a warmer to try and bring her temperature up while they discuss treatment. He agrees to bloodwork and Xrays.
The Xrays reveal severe abdominal obstruction. From the stomach ending on down. The vet is surprised at the amount of obstruction. There’s so much obstruction she can’t even clearly see if there’s rupture. There’s obvious distention, with bulging pockets.
He is willing to do surgery. He calls for reinforcement. Mom says no. He pleads, advising he’ll personally bring the kitten home with him. Mom disagrees. Mom asks the vet home pain the kitten is in. The vet is honest that the cat is in so much pain, the pain meds she’s been given are ineffective and she’s maxed out for her size (she’s feral and underweight). He reluctantly makes the choice to euthanize her.
Tonight, I watched the kindest, gentlest soul shell out over $1,000 to do everything possible to save this kitten and to help her pass gracefully, surrounded by love and warmth.
It was a beautiful experience in empathy and compassion. He chose to memorialize her - individual cremation and a paw print. He named her Jordan.
He cried. Sobbing cries for this wee one. He had spent hours trying to find a ride. Multiple Ubers and Lyfts cancelled because of the animal transport. In the cover of darkness, I was able to help him give this kitten a proper send off.
I wanted to bring the kitten home, but with two dogs, the kitten would not be able to safely recover from a bowel resection here. Cat rescues were all closed. No one responded to calls. She needed round the clock care for at least 24 hours just to recover from the surgery. We hadn’t even addressed if she was septic or any bloodwork yet.
She was an absolute fighter to the end though. An absolute fighter.
He and I are keeping in touch. Two strangers bonding over the strangest of circumstances.
0 notes
Text
Ascites - Symptoms, Causes, Complications, Prevention and Treatment
Ascites definition
Ascites is also defined as the fluid build-up in the space between the lining of the abdomen and abdominal organs.
Ascites is a medical condition characterized by excess abdominal fluid accumulation. This excess fluid buildup between the two layers of the peritoneum (peritoneal cavity of the abdomen) leads to abdominal swelling or distension.
Ascites is usually seen in people suffering with advanced liver disease, liver cirrhosis (permanent scarring of the liver). Transitioning from compensated to decompensated cirrhosis is indicated by the development of ascites.
Ascites is usually seen in people suffering with advanced liver disease, liver cirrhosis (permanent scarring of the liver). Transitioning from compensated to decompensated cirrhosis is indicated by the development of ascites.
Causes of Ascites
The accumulation of fluid in the abdomen, or ascites, can indicate a few underlying medical disorders, even though it can seriously impair daily life. The exact cause of ascites plays a crucial role in getting proper treatment. The key mechanisms that could cause ascites are as follows:
Increased portal pressure: Portal hypertension is the condition where the portal vein blood pressure increases. The portal vein is the vessels that carry the blood from the spleen, pancreas, and intestine to the liver. Blood flow becomes harder in the liver when it gets scarred, resulting in a back-up of blood pressure in the portal vein. Finally, this leads to increased fluid pressure in the liver and other organs of the abdomen and forces the fluid from the capillaries into the peritoneal cavity.
Sodium and water retention: Albumin is the protein that helps to manage the fluid in the bloodstream; if the liver gets damaged, it cannot produce enough albumins. Thus, it leads to low blood pressure and influences the kidneys to retain water and sodium in an attempt to compensate - these increased levels of sodium and water leak outside from the capillaries into the peritoneal cavity.
Ascites symptoms
Ascites symptoms are indications that occur in the body; they might range from mild to severe and occur suddenly or gradually. However, there are some common early stage ascites symptoms, which include:
Abdominal distension
Abdominal discomfort
Swelling in the abdomen
Feeling fullness with small amounts of food
Shortness of breath
Flank and shifting dullness on physical examination
Pleural effusion
Fatigue
Bloating
Indigestion and more
Symptoms of ascetic patients with bacterial peritonitis include:
Fever
Tenderness on the abdomen
Confusion
Symptoms of chylous ascites include:
Steatorrhea (fatty stools)
Diarrhoea (loose or watery stools)
Nausea
Oedema (swelling due to fluid accumulation)
Night sweats
Lymphadenopathy (enlargement of lymph nodes)
Early satiety (unable to take full meals due to early fullness)
Fever
Treatment of ascites depends on the underlying cause but often involves managing the contributing factors. This may include medications to reduce fluid retention, dietary changes (such as sodium restriction), and addressing the underlying medical condition. In some cases, therapeutic paracentesis (removal of fluid from the abdominal cavity) may be performed to alleviate symptoms. It's important for individuals with ascites to work closely with their doctor to determine the most appropriate course of treatment based on the underlying cause of the condition.
PACE Hospitals stands as a beacon of excellence in healthcare, committed to advancing medical science, caring for our community, and providing unparalleled patient-centered services. With a focus on compassion, innovation, and expertise, we continue to be a trusted healthcare partner for individuals seeking the highest standards of medical care.
0 notes
Text
What is tube cannulation?

Tube cannulation is a medical procedure that involves the insertion of a tube or catheter into a vessel, duct, or body cavity for a variety of therapeutic or diagnostic purposes. This procedure is commonly used in healthcare settings to provide access to specific areas of the body for the following reasons:
Medication Administration: One of the most common uses of tube cannulation is to administer medications directly into the bloodstream. For example, central venous catheters (CVCs) are often used to deliver intravenous (IV) medications, such as antibiotics, chemotherapy drugs, or nutrition solutions, directly into a large central vein.
Fluid or Blood Collection: Tubes can be used to collect samples of blood, urine, or other bodily fluids for diagnostic testing. This is commonly done through catheters or tubes that are placed in the urinary tract, blood vessels, or the gastrointestinal tract.
Nutrition and Hydration: Some patients may require tube feeding due to difficulty swallowing, gastrointestinal problems, or the need for specialized nutrition. Gastrostomy or jejunotomy tubes are examples of tubes used for this purpose.
Fluid or Gas Drainage: Certain medical conditions, such as pleural effusions or abdominal abscesses, may require the removal of excess fluid or gas. Chest tubes and abdominal drainage tubes can be inserted for this purpose.
Monitoring: Tube cannulation can be used for monitoring purposes, such as measuring central venous pressure (CVP) through a CVC or monitoring intracranial pressure (ICP) with an intraventricular catheter.
The choice of tube and its placement location depend on the patient's medical needs, the type of therapy or treatment required, and the assessment of the healthcare provider. For example:
Central Venous Catheters (CVCs) are typically inserted in large veins near the heart, often in the neck, chest, or groin.
Peripherally Inserted Central Catheters (PICCs) are usually placed in a peripheral vein, often in the arm, and threaded through to a larger vein closer to the heart.
Urinary Catheters are inserted into the bladder through the urethra or, in certain cases, directly through the abdominal wall (suprapubic catheter).
It's important to note that tube cannulation should be performed by trained healthcare professionals to ensure the safety and well-being of the patient. The procedure may require local anesthesia or sedation, and it should be carried out with aseptic techniques to minimize the risk of infection.
The duration of tube placement can vary, and tubes are typically removed when they are no longer needed, when complications arise, or as determined by the treating medical team. Proper care, monitoring, and maintenance of the tube are essential to prevent complications and ensure the best possible outcome for the patient.
Ready to prioritize your women's health? Schedule your appointment with Dr. Neha, your trusted Gynaecologist in Dubai today!"
#dr. neha lalla#gynaecologist in dubai#health & fitness#best gynecologist in thane#best indian gynaecologist in dubai
0 notes
Text
Malignant Pleural Effusion Market End-User Demand by Types, Regions, Top Players, Regional Outlook and Forecast to 2033
The global malignant pleural effusion market is expected to garner a market value of US$ 4.5 Billion in 2023 and is expected to accumulate a market value of US$ 8.06 Billion by registering a CAGR of 6% in the forecast period 2023-2033. The increasing incidence of pleural effusion disease and rising awareness of advancement in pleural effusions treatment with different types of techniques in the current market works as a driver for the market. The market for Malignant Pleural Effusion registered a CAGR of 4% in the historical period 2017-2022.
Growth of the Malignant Pleural Effusion market can be attributed to the rising burden of various diseases such as cancer and heart failure. The increasing burden of diseases in the United States is expected to create opportunities for the pleural effusions market. The data updated by the American Cancer Society’s Cancer Statistics 2022, nearly 1.9 million new cancer cases are estimated to be diagnosed in the United States in the year 2022.
Get Sample Report + Related Graphs & Charts @ https://www.futuremarketinsights.com/reports/sample/rep-gb-16230
In addition to this, the rising prevalence of pleural effusions has been contributing to the market growth. An article published by WebMD LLC in October 2021 stated that approximately 1.5 million pleural effusions are diagnosed in the United States every year and in industrialized countries, the estimated prevalence of pleural effusion is 320 cases per 100,000 people. Therefore, various factors such as awareness in wellness and health along with the research and development activities in the field like emerging novel therapeutics are increasing the efficacy of medicine as well as treatment.
Key Takeaways from the Market Study
From 2017-2022, the Malignant Pleural Effusion market grew at CAGR of 4%.
The global Malignant Pleural Effusion market is expected to grow with a 6% CAGR during 2023-2033.
As of 2033, the Malignant Pleural Effusion market is expected to reach US$ 8.06 Billion
According to the FMI analysis, hospitals account for the largest market share.
North America is expected to possess 45% market share for the Malignant Pleural Effusion market.
The Asia Pacific market is predicted to increase significantly throughout the forecast period, with a CAGR of 5% during the forecast period.
Ask Analyst for Report Customization and Explore TOC & List of Figures @ https://www.futuremarketinsights.com/ask-question/rep-gb-16230
“Various factors such as awareness in wellness and health, the diagnostics, and pathology segment are improving in the developing countries nowadays which grows the therapeutics market. The research and development activities in the field like emerging novel therapeutics, increasing the efficacy of medicine as well as treatment.” says an FMI analyst
Market Competition
Key players in the Malignant Pleural Effusion market are B. Braun SE, Becton, Dickinson and Company, Bicakcilar, Biometrix, Cook Medical, Grena, Redax, Rocket Medical, and Smith Medical.
In September 2021, BDR Pharma launched BIAPENEM to treat patients with intra-abdominal infections, lower respiratory infections, or complicated urinary tract infections. Biapenem is widely distributed and penetrates well into various tissues (e.g. lung tissue) and body fluids (e.g. sputum, pleural effusion, abdominal cavity fluid).
In April 2022, the study titled “IFN-γ Combined with T Cells in the Treatment of Refractory Malignant Pleural Effusion and Ascites” was registered in ClinicalTrials.gov for Malignant Pleural Effusion.
More Insights Available
FMI, in its new offering, presents an unbiased analysis of the global Malignant Pleural Effusion market, presenting historical analysis from 2018 to 2022 and forecast statistics for the period of 2023-2033.
The study reveals essential insights on the basis of treatment (Systemic Therapy, Therapeutic Thoracentesis, Thoracic Drainage and Pleurodesis, Indwelling Pleural Catheter), End-users (Hospitals, Ambulatory Clinics, Others), diagnosis (Imaging Tests, Pleural Thoracentesis, Pleural Fluid Cytology,Immunohistochemical Tests, Pleural Biopsy, Thoracoscopy/Pleuroscopy) & region.
Last few days to get reports at discounted prices, offer expires soon!
Request Discount@ https://www.futuremarketinsights.com/request-discount/rep-gb-16230
Key Segments Profiled in the Malignant Pleural Effusion Industry Survey
By Diagnosis:
Imaging Tests
Pleural Thoracentesis
Pleural Fluid Cytology
Immunohistochemical Tests
Pleural Biopsy
Thoracoscopy/Pleuroscopy
By End User:
Hospitals
Ambulatory Clinics
Others
By Treatment:
Systemic Therapy
Therapeutic Thoracentesis
Thoracic Drainage and Pleurodesis
Indwelling Pleural Catheter
0 notes
Text
“Taylor Roe” 33 (USA 2017)
The unidentified woman who was given the pseudonym “Taylor Roe” was 33 when she underwent a chemical abortion with vaginally administered misoprostol. She was 6 weeks pregnant.
Taylor was told that her baby was not viable, but it’s unknown what condition her child was actually diagnosed with.
After the abortion, Taylor bled heavily for four days and suffered from abdominal pain, which became worse over the course of the week. Only a few days after the abortion, she was in so much pain that she had to go to the emergency room.
Taylor was given medicine and sent home, but became even worse and developed nausea, vomiting and a fever of 101.6 F. She returned to the emergency room.
This time, ER staff noted that Taylor was now tachycardic and suffering from both leukocytosis and thrombocytosis. A CT scan detected peritoneal free fluid and multiple pleural effusions. Taylor underwent a D&C and then was admitted to the ICU in an attempt to save her life.
Despite the best efforts of the hospital, Taylor continued to decline. Plans were made for an emergency hysterectomy, but she went into cardiac arrest and died before the surgery could be carried out.
The autopsy showed the extent of the damage Taylor suffered. The results showed “a large volume of cloudy serosanguineous fluid, fibropurulent exudates, and mesenteric and pelvic lymphadenopathy, demonstrating infection and peritonitis, along with a hemorrhagic and necrotic uterus, right ovary, and right fallopian tube.” Tissue cultures were positive for clostridium sordellii. Like too many others, Taylor died of TSS (Toxic Shock Syndrome) from her legal chemical abortion. Her organs were too severely damaged for her to survive.
#pro life#tw abortion#unsafe yet legal#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion#unidentified victim#victims of roe
5 notes
·
View notes
Text
What are the symptoms that lung cancer has metastasized?
When lung cancer metastasizes, it means that cancer cells have spread from the lungs to other parts of the body. The symptoms of metastatic lung cancer can vary depending on the specific organs or tissues affected. Here are some common symptoms associated with metastasis:
1.Bone metastasis: Bone pain, fractures, and weakness.
2.Brain metastasis: Headaches, seizures, blurred vision, difficulty speaking or understanding, changes in mood or behavior, and coordination problems.
3.Liver metastasis: Jaundice (yellowing of the skin and eyes), abdominal pain or swelling, unexplained weight loss, loss of appetite, and fatigue.
4.Adrenal gland metastasis: Abdominal pain, back pain, weight loss, weakness, and changes in hormone levels.
5.Lymph node metastasis: Enlarged lymph nodes, which may be felt as lumps under the skin.
6.Skin metastasis: Skin nodules or lumps, skin ulcers, or yellowish discoloration of the skin.
7.Lung metastasis (in other lung): New or worsening cough, shortness of breath, chest pain, and recurrent lung infections.
8.Pleural metastasis (spread to the lining around the lungs): Pleural effusion (accumulation of fluid in the chest), chest pain, and shortness of breath.
It's important to note that these symptoms can also be caused by other conditions, and experiencing these symptoms does not necessarily mean that lung cancer has metastasized. If you have concerns about your health or are experiencing any unusual symptoms, it is best to consult a healthcare professional for an accurate diagnosis.
0 notes
Text
Scared of what may become
I haven't been diagnosed Anything yet but I've been feeling really horrible lately feeling like I'm gonna have a heart attack chest pains limbs being cold or numb and then I got a result back saying AV Block if anybody can help me decipher this it would be much appreciated
Davis, MD Measurements Intervals Axis Rate: 71 P: 44 PR: 246 QRS: 28 QRSD: 97 T: 39 QT: 358 QTc: 389 Interpretive Statements SINUS RHYTHM WITH FIRST DEGREE AV BLOCK No acute ST segment elevations or depressions, no STEMI. Normal axis, QTC Compared to ECG 05/12/2021 10:49:24 First degree AV block now present ST (T wave) deviation no longer present Electronically Signed On 1-23-2023 3:30:30 PST by Colin Davis, MD
Component Results
EXAM: CHEST RADIOGRAPH, 2 VIEWS, 1/23/2023 3:57 AM
HISTORY: Chest pain.
TECHNIQUE: CHEST RADIOGRAPH, 2 VIEWS.
COMPARISON: 5/12/2021.
FINDINGS: There is no focal consolidation. There is no pleural effusion. There is no pneumothorax.
The cardiac silhouette is unremarkable.
No acute bone or soft tissue abnormality is seen.
Specifically,
1 Normal thoracic aorta without dissection or aneurysm and no atherosclerotic changes. Normal heart size without pericardial effusion. 2. No pulmonary embolus. 3. No pleural effusions or pneumothorax. 4. Lungs are clear without focal consolidation pneumonia.
....... Providers: To speak with a TRA radiologist, call (253)761-4200. Patient: For further result information, please contact ordering provider.
Narrative EXAM: CT ANGIO THORACIC AORTA, DATE: 01/23/2023 at 4:18 AM
HISTORY: Acute chest pain radiating to the back
TECHNIQUE: Evaluation the chest through the renal arteries during the arterial phase of contrast enhancement. Reconstruction to include thick MIP angiographic images. Isovue-370, 1 mL
In accordance with CT policies/protocols and the ALARA principal, radiation dose reduction techniques (such as automated exposure control, adjustment of mA/kV according to patient's size and/or iterative reconstruction technique) were utilized for this examination.
COMPARISON: None
FINDINGS: The aorta from the aortic root through the upper abdominal aorta enhances normally without atherosclerotic changes, dissection, aneurysm or pseudoaneurysm. No intimal flap or intimal irregularity.
No coronary calcification.
Heart size normal. No pericardial effusion.
Central pulmonary arteries opacify normally. No pulmonary embolus.
Mediastinum and hila demonstrate no mass or adenopathy.
Lungs are clear without focal consolidation. No pulmonary edema and no suspicious nodules or masses
No pleural effusions and no pneumothorax.
Vertebral body heights well-maintained.
Upper abdomen unremarkable with normal gallbladder. No biliary duct dilatation. Visualized pancreas unremarkable and upper poles the kidneys are unremarkable
Kidneys not included
Component Results
submitted by /u/Legal-Side6464
[link] [comments]
from For issues related to heart disease, cardiac health and cholesterol control https://ift.tt/sp7tkWE
0 notes
Text
Cardiovascular diseases (CVDs): Symptoms, Risk Factors, and Types
Cardiovascular diseases refer to a group of diseases that affects your heart and blood vessels. These diseases can affect multiple parts of your heart or associated blood vessels. Not all CVD patients experience symptoms until they reach at a certain stage.
Cardiovascular diseases include various heart or blood vessel issues, such as:
Narrowing of the blood vessels in heart
Heart and blood vessel issues present since birth
Failure or improperly working heart valves
Irregular heart rhythms.
Symptoms
1. Symptoms of heart conditions
Chest pain (called as angina)
Feeling pressure, heaviness or discomfort in the chest
Shortness of breath
Fatigue
Exhaustion
Dizziness or fainting
2. Symptoms of blood vessels blockage
Pain or cramps in legs while walking
Red skin or swelling in legs
Prolonged leg sores that aren’t healing
Numbness in face or limb
Difficulty in talking, seeing or walking
These symptoms require immediate attention from a cardiovascular surgeon.
Risk factors
As per cardiovascular Surgeons, the following factors makes you more prone to develop cardiovascular disease:
High blood pressure
High cholesterol
smocking or chewing tobacco
Type 2 diabetes.
Gestational diabetes.
Less or no physical activity
Obesity.
High sodium, sugar and fat in regular diet
Alcohol consumption
Family history of heart diseases
over-the-counter medicines
Preeclampsia or toxaemia
Chronic inflammatory or autoimmune conditions.
Chronic kidney or liver disease.
Types
Aortic disease: Issues in the large blood vessel that carries blood from heart to brain and the rest of your body.
Arrhythmia: Issues in heart’s electrical conduction system which leads to abnormal heart rates.
Cerebrovascular disease: Narrowing or blockages in the blood vessels that carries blood to our brain.
Congenital heart disease: Heart and blood vessel issues present since birth, and they can also affect different parts of the heart.
Coronary artery disease: Blockage in heart’s blood vessels.
Deep vein thrombosis (DVT): Blockage in veins/vessels that carries blood back from brain/body to the heart.
Heart failure: Issues in heart pumping, leading to fluid build-up in heart and shortness of breath.
Pericardial disease: Problem with heart lining, including pericarditis and pericardial effusion.
Peripheral artery disease: Narrowing or blockages in the blood vessels of arms, legs or abdominal organs.
Valve disease: Tightening or leaking of heart valves.
Looking for best cardiovascular surgeon? Sarvodaya Hospital at Faridabad has India’s most experienced cardiovascular surgeon who will treat your CVD to ease your conditions. They are equipped with best diagnosis technology and surgical equipment’s to provide you with the best care services.
#heart failure#chronic kidney failure#liver disease#cardiovascular Surgeons#Obesity#Cardiovascular diseases
0 notes