#gastric cancer
Photo
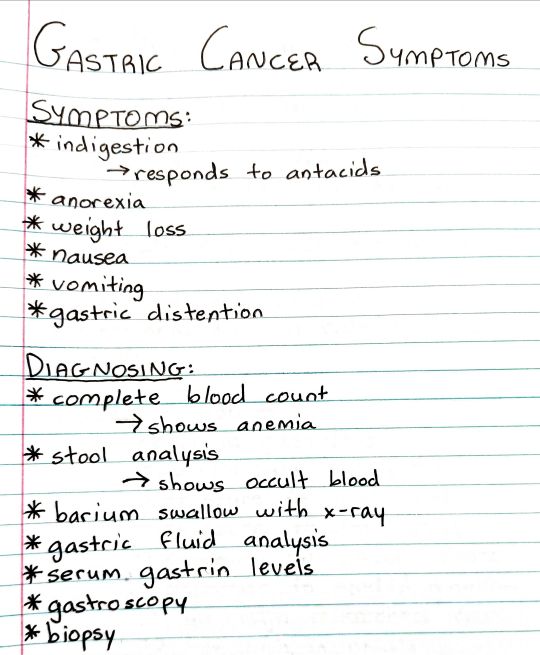
#studyblr#notes#my notes#pathology#pathophysiology#anatomy and physiology#anatomy#physiology#pathology notes#pathophysiology notes#diagnosing#symptoms#signs and symptoms#symptoms and signs#gastric cancer#cancer#oncology#oncology notes
13 notes
·
View notes
Text
Malaria presents with periodic flu-like symptoms and should be suspected in any ill patient with a history of travel from an endemic region. Diagnosis is primarily made by examining thick and thin blood smears for speciation and percent parasitemia. All malarial species produce intra-erythrocytic rings (trophozoites). Rapid antigen testing may also be available and can distinguish between P. falciparum and P. vivax. Treatment with chloroquine is standard for mild-to-moderate disease. Due to chloroquine resistance, however, artemisinin combination therapy (ACT) is commonly used. ACT options include dihydroartemisinin, artesunate, mefloquine, or artemether in combination with other antimalarials (eg, piperaquine or mefloquine).
Severe disease should be treated with intravenous artesunate. The anti-hypnozoite drug primaquine is also necessary for P. vivax and P. ovale because of their ability to cause relapse due to dormant hypnozoite forms within the liver. To prevent acute hemolysis, it is important to test for glucose-6-phosphate dehydrogenase deficiency prior to initiating primaquine. Of note, P. falciparum is known to produce fulminant disease, including hemolytic anemia, renal failure, pulmonary edema, central nervous system disease, hypoglycemia, liver failure, and lactic acidosis. Rapid treatment is therefore essential to prevent poor outcomes.
Gonorrhea is diagnosed with NAAT of a swab or culture on Thayer-Martin media. Once the samples have been obtained, the patient can be initiated on antimicrobial therapy. The standard therapy would be ceftriaxone 250 mg intramuscularly (IM) as a single dose, plus azithromycin 1 g orally (due to increasing resistance) or doxycycline 100 mg orally twice daily for 7 days.
Wilson disease results in inappropriate deposition of copper in the liver, brain, and other tissues due to impaired clearance of copper into the bile. It is an autosomal-recessive disease affecting chromosome 13. Signs and symptoms are the consequence of cirrhosis, basal ganglia deterioration, and deposition of copper in other tissues, causing hepatic failure, neurologic abnormalities, hemolytic anemia, and Kayser-Fleischer rings around the iris.
Basic labs will reveal hemolytic anemia (decreased hemoglobin and hematocrit with elevated bilirubin as well as decreased haptoglobin and increased reticulocyte count) and elevated liver enzymes due to liver inflammation and cirrhosis. Decreased ceruloplasmin (less than 20 mg/dL) and low serum copper concentration are consistent with Wilson disease and should prompt confirmatory workup, including 24-hour urine copper excretion. Low serum copper levels may seem paradoxical; however, it should be remembered that ceruloplasmin is the primary copper binding protein and is responsible for the majority of copper contained in the serum. Low ceruloplasmin results in a low total serum copper, despite the fact that total-body copper is in excess. This excess, while not measurable in the serum at a specific point in time, is measurable as increased urinary excretion over the course of the day, which is why a 24-hour urine copper is needed.
Kayser-Fleischer rings are present in 50% of patients with active liver disease but without any neurologic involvement. When neurologic symptoms present (dysarthria, dystonia, tremor, parkinsonism, choreoathetosis, ataxia, cognitive impairment), Kayser-Fleischer rings are present in 98% of patients.
Gastric cancer presents with left supraclavicular lymphadenopathy. Left supraclavicular adenopathy (known as the Virchow node) suggests an abdominal source, such as the stomach, gallbladder, or pancreas.
In any patient with an upper GI bleed, it is important to ask for recent anticoagulation use and a history of prior bleeding or endoscopy as up to 60% of recurrent GI bleeding is from the same lesion. Other important considerations in the history include: if the patient has a history of H. pylori, cirrhosis, odynophagia, or the use of antiplatelet agents.
Esophageal varices and peptic ulcers are common and easily treatable causes of bleeding in pts with cirrhosis.
Bottom Line: The most common causes of upper GI bleeding include peptic ulcer disease, severe or erosive gastritis/duodenitis/esophagitis, esophagogastric varices, portal hypertensive gastropathy, angiodysplasia, Mallory-Weiss syndrome, mass lesions (polyps/cancers).
Besides varices, other major complications of cirrhosis include ascites, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatocellular carcinoma, hepatorenal syndrome, hepatopulmonary syndrome, however, in patients with acute decompensation due to upper GI bleeding, the most urgent conditions to evaluate for include the development of hepatic encephalopathy, SBP, and hepatorenal syndrome.
Bottom Line: A patient with cirrhosis and acute upper GI bleeding should have 2 large-bore IVs or a large-bore, single-lumen central catheter placed, be resuscitated with IV fluids, transfused blood as needed, started on an IV proton pump inhibitor drip, an IV octreotide drip, and IV antibiotics for SBP prophylaxis, and will generally require ICU admission. An EGD should be performed within 24 hours of admission, but ideally as soon as possible, once the patient is hemodynamically stable.
Management of critical patients with upper GI bleeding generally follows the same trajectory. Get as much history as possible to localize risk factors for bleeding and options to inform immediate pharmacologic treatment (PPI vs octreotide vs both). Give blood and fluids. Consult gastroenterology for EGD. If the patient cannot undergo EGD or this is not available or had a recent EGD with bleeding that is not amenable to further endoscopic therapy, consult IR for embolization.
Those patients found to have SBP should receive hepatorenal syndrome prophylaxis with albumin on days 1 (1.5g/kg) and 3 (1g/kg) of admission if they meet the criteria.
Multiple trials evaluating the effectiveness of prophylactic antibiotics in cirrhotic patients hospitalized for GI bleeding suggest an overall reduction in infectious complications and possibly decreased mortality. Antibiotics may also reduce the risk of recurrent bleeding in hospitalized patients who bled from esophageal varices.
Diagnose pheochromocytoma with urine metanephrine and normetanephrine levels. The most appropriate drug therapy prior to adrenalectomy for suspected pheochromocytoma consists of phenoxybenzamine followed by the addition of propranolol (if needed for heart rate control). Preoperative treatment for surgical resection of pheochromocytoma involves alpha-receptor blockade. This can be followed by beta-receptor blockade if needed for further heart rate control, usually 2 to 3 days before surgery.
7 to 14 days of phenoxybenzamine and 2 to 3 days of propranolol prior to surgery (if needed for heart rate control), with the continuation of propranolol perioperatively. The most important aspect of treatment in patients with pheochromocytoma with respect to preoperative antihypertensive therapy is alpha-receptor blockade. Alpha-receptor blockade prevents the hypertensive effect of overstimulation by the catecholamines released from the adrenal medulla. Beta-receptor blockade should follow, which prevents rebound tachycardia (goal heart rate should be 60-80/min) in the setting of unopposed alpha blockade. The clinical guidelines from the Journal of Clinical Endocrinology and Metabolism released in 2014 currently support the use of alpha-blockers for blood pressure control prior to surgery. Beta-blockers can be added afterward if needed. Of note, selective alpha-1-receptor blockers, such as prazosin or doxazosin, may be used instead of phenoxybenzamine in certain situations, such as in patients who have significant benign prostatic hyperplasia and may already be on low doses of these medications or if the patient cannot tolerate the first-line agents listed above. Metoprolol can also be administered instead of propranolol or atenolol.
There is a rule of 10's associated with pheochromocytoma: 10% are extra-adrenal, 10% are bilateral, 10% are malignant, and 10% occur in children. Some people add that 10% will recur after excision within 10 years and 10% will be found after a significant stroke. It was previously thought that about 10% were familial; however, that number has been adjusted upward as more and more genetic and familial diseases have been linked with the development of pheochromocytoma. It is now thought that about 40% of pheochromocytomas are associated with some kind of underlying genetic predisposition. Malignant pheochromocytomas are biologically and histologically indistinguishable from benign pheochromocytomas. The only way to determine malignancy is to observe local infiltrative disease or find evidence of metastatic spread. Thus, even benign pheochromocytomas found on excision will need clinical follow-up.
Most authors advocate obtaining 24-hour fractionated urine metanephrines if the clinical suspicion is low, and serum metanephrines if the clinical suspicion is high. Serum metanephrines have a decreased specificity, and positive testing may result in unnecessary imaging and follow-up, which is why it is not recommended as the first-line test for all patients.
HAs, diaphoresis, HTN = pheo
Gastrinoma (Zollinger-Ellison) - initial test that should be ordered is a fasting serum gastrin level. If elevated, it should be followed by a secretin infusion test. Somatostatin-receptor scintigraphy is the imaging test of choice as it detects for primary or metastatic lesions. Treatment includes intravenous (IV) proton pump inhibitors and surgical resection. Zollinger-Ellison syndrome is also associated with multiple endocrine neoplasia (MEN) type 1. MEN 1 is also known as Werner's syndrome and presents with the 3 Ps: parathyroid tumors; pituitary tumors, including prolactinoma; and pancreatic endocrine tumors, including insulinomas, vipomas, glucagonomas, and Zollinger-Ellison syndrome.
The initial test of choice for Zollinger-Ellison syndrome is a fasting serum gastrin (off proton pump inhibitors). The diagnosis is confirmed with a secretin infusion test. It is associated with MEN1.
2 notes
·
View notes
Photo


You are strong! But some days we all need a little more awareness, and a few extra spoons! (in periwinkle!)
The periwinkle awareness ribbon represents those with
anorexia nervosa, anorexia, esophageal cancer, cancer, gastric cancer, irritable bowel syndrome, ibs, pulmonary hypertension, small intestine, cancer, stomach cancer, stomach
And the dark and light versions of the design are available on my Threadless store in a variety of products and background colours!
threadless dark- https://meridiandesigns.threadless.com/designs/periwinkle-awareness-pocket-dark
threadless light- https://meridiandesigns.threadless.com/designs/periwinkle-awareness-pocket-light
facebook ★ instagram ★ twitter ★ pinterest
#periwinkle#purple#blue#spoonie#chronic fatigue#invisible illness#chronic pain#chronic illness#disability#health#love#awareness#fatigue#wellness#pain#anorexia#esophageal cancer#cancer#gastric cancer#irritable bowel disease#ibs#pulmonary hypertension#small intestine cancer#stomach cancer#anorexia nervosa
1 note
·
View note
Text

LIVE: Philippine College of Physicians' PHILIPPINE DIGESTIVE HEALTH WEEK 2024 Forum
Topic: EMPOWERING FILIPINOS TO CARE FOR DIGESTIVE HEALTH
#gastroenterology #digestion #digestivesystem #gastriccancer #colorectalcancer #stomach #diarrhea #intestine #largeintestine #liver
https://www.facebook.com/share/v/5LZGgHAb2MeNdkhV/?mibextid=w8EBqM
#gastroenterology#digestivehealth#digestion#digestive system#gastric cancer#colorectal cancer#stomach#diarrhea#intestine#large intestine#liver
0 notes
Text
The gastric cancer market size was valued at $2.1 billion in 2021, and is estimated to reach $10.7 billion by 2031, growing at a CAGR of 17.9% from 2022 to 2031.
#Gastric Cancer Market#Gastric Cancer#Gastric Cancer Market Report#Gastric Cancer Market Share#Gastric Cancer Market Size#Gastric Cancer Market Forecast#Gastric Cancer Market Outlook#Gastric Cancer Market Driver#Gastric Cancer Market Trends
0 notes
Text
Recent Advances in Gastric Cancer Research
Recent Advances in Gastric Cancer: Gastric cancer is also known as stomach cancer, continues to be a significant health concern worldwide. Despite advancements in early detection and treatment, the disease often presents in advanced stages, making it challenging to manage. However, recent research has brought forth new insights and therapeutic approaches that are changing the landscape of gastric…

View On WordPress
0 notes
Text
🇬🇧 Embrace a healthier, happier life with Gastric Sleeve surgery in Istanbul! A transformative journey begins here. Contact us now! 💪
•
🇩🇪 Wählen Sie ein gesünderes, glücklicheres Leben mit einer Magenmanschette-Operation in Istanbul! Eine transformative Reise beginnt hier. Kontaktieren Sie uns jetzt! 💪
•
🇫🇷 Adoptez une vie plus saine et plus heureuse grâce à la chirurgie de la manche gastrique à Istanbul! Un voyage transformateur commence ici. Contactez-nous maintenant! 💪
•
🇮🇹 Abbraccia una vita più sana e felice con l'intervento di Sleeve gastrico a Istanbul! Un viaggio trasformativo inizia qui. Contattaci ora! 💪
•
🇪🇸 ¡Adopta una vida más saludable y feliz con la cirugía de manga gástrica en Estambul! Aquí comienza un viaje transformador. ¡Contáctanos ahora! 💪
•
🇹🇷 İstanbul'da Gastric Sleeve ameliyatı ile daha sağlıklı, daha mutlu bir hayatı kucaklayın! Dönüştürücü bir yolculuk burada başlar. Hemen bize ulaşın! 💪
•
🇷🇺 Примите более здоровую, счастливую жизнь с операцией гастробайпаса в Стамбуле! Здесь начинается трансформирующее путешествие. Свяжитесь с нами сейчас! 💪
1 note
·
View note
Text
क्या पेट का कैंसर ठीक हो सकता है?
पेट का कैंसर (Stomach cancer treatment) एक बहुत बड़ी बीमारी है लेकिन यदि आपको इसके बारे में जल्दी ही पता चल जाए तो हां पेट के कैंसर का इलाज संभव है यदि किसी को पेट का कैंसर हो जाता है तो उसके इलाज के लिए सर्जरी कीमोथेरेपी और रेडिएशन थेरेपी की जाती है।
क्या पेट का कैंसर ठीक हो सकता है | How to cure stomach cancer
पेट के कैंसर का इलाज कितना प्रभावी होगा कौन सा इलाज मरीज को दिया जाना चाहिए कितने…
View On WordPress
#cancer#cancer ka ilaj#cancer ka ilaj kaise hota hai#cancer ka ilaj kaise sambhav hai#cancer ka pata kaise lagta hai#cancer treatment#gastric cancer#How to cure stomach cancer in hindi#muh ke cancer ko kaise thik karen#pet cancer#pet cancer ka ilaaj#pet ka cancer#pet ka cancer kaise pata chalta hai#pet ka cancer kaise theek karen#pet ka cancer kaise thik hoga#Pet ka cancer ke lakshan#Pet ka cancer kyu hota#pet ka cancer kyu hota hai#pet ka cancer thik hota hai ki nahin#pet ke cancer ka gharelu upchar#pet ke cancer ka ilaaj#pet ke cancer ka ilaj#pet ke cancer ka karan#pet ke cancer ka treatment#Pet ke cancer ke karan#pet ke cancer ke lakshan#pet me cancer#Stomach cancer#Stomach cancer in hindi#stomach cancer treatment
0 notes
Text
The treatment for gastrointestinal (GI) bleeding depends on the cause, severity of bleeding, and the patient's overall health condition. Here are some common treatment approaches for GI bleeding:
Supportive care: Initially, supportive care focuses on stabilizing the patient's condition. This may include providing intravenous fluids, blood transfusions, and medications to maintain blood pressure and address symptoms of shock.
Endoscopic therapy: Endoscopy is a common procedure used to diagnose and treat GI bleeding. During an endoscopy, a flexible tube with a camera is inserted into the digestive tract to identify the bleeding source.
Endoscopic therapy can involve various interventions, such as:
Injection therapy: Injecting medications, such as epinephrine or sclerosing agents, directly into the bleeding site to promote blood vessel constriction and clot formation.
Thermal therapy: Applying heat energy (thermal coagulation) or cold therapy (cryotherapy) to the bleeding site to cauterize or freeze the bleeding vessel and stop the bleeding.
Mechanical therapy: Using clips or bands to ligate or compress the bleeding vessel, providing hemostasis.
Medications: Certain medications may be prescribed to control or reduce GI bleeding, depending on the underlying cause. For example:
Proton pump inhibitors (PPIs): These medications reduce stomach acid production and can be used to treat bleeding caused by peptic ulcers or gastroesophageal reflux disease (GERD).
H. pylori eradication therapy: If the bleeding is due to an infection with Helicobacter pylori, a combination of antibiotics and PPIs may be prescribed to eradicate the bacteria and promote ulcer healing.
Antacids and cytoprotective agents: These medications can help protect the lining of the stomach and reduce irritation in cases of gastritis or gastric ulcers.
Blood clotting medications: In some cases, medications that promote blood clotting, such as desmopressin or recombinant factor VIIa, may be used to control bleeding.
Surgery: In cases of severe or recurrent bleeding that does not respond to other treatments, surgical intervention may be necessary. Surgery may involve removing a bleeding segment of the digestive tract, repairing an ulcer or perforation, or addressing underlying conditions like gastrointestinal tumors.
Transcatheter embolization: In this procedure, a catheter is threaded through blood vessels to the site of bleeding. Embolic materials are then injected to block or reduce blood flow to the bleeding vessel, achieving hemostasis.
The choice of treatment depends on the specific circumstances, and individualized care is essential. It is crucial to consult with a healthcare professional or a gastroenterologist who can evaluate the severity of the bleeding and recommend the most appropriate treatment approach for the specific situation. There are some best specialists doctors like Dr Amit Maydeo, who is a highly efficient gastroenterologist and is associated with HN Reliance hospital in Mumbai. You may visit him to get the most accurate diagnosis and treatment plan for GI bleeding.
#health#gi bleeding#peptic ulcers#gastric cancer#stomach surgery#endoscopy#endotherapy#ulcerative colitis#crohn's disease#dr amit maydeo
0 notes
Text

Gallstones can become dangerous when they cause complications such as: Gallbladder Inflammation (Cholecystitis): Gallstones can block the cystic duct, leading to inflammation and infection of the gallbladder. This condition can cause severe abdominal pain, fever, and nausea. If left untreated, it can lead to a perforated gallbladder, abscess formation, or infection spreading to other parts of the body. Bile Duct Obstruction (Choledocholithiasis): Gallstones can travel from the gallbladder and get lodged in the bile ducts, obstructing the flow of bile. This can cause jaundice, which is characterized by yellowing of the skin and eyes, dark urine, and pale stools. Bile duct obstruction can also lead to inflammation of the bile ducts (cholangitis) or inflammation of the pancreas (pancreatitis). Infection of the Biliary System (Cholangitis): When the bile ducts are blocked by gallstones, it can lead to the buildup of bacteria and subsequent infection. Cholangitis can cause symptoms such as fever, abdominal pain, jaundice, and sepsis if left untreated.
ERCP (Endoscopic Retrograde Cholangiopancreatography) can help in saving the patient by providing both diagnostic and therapeutic interventions. There are some best doctors like Dr Amit Maydeo who perform ERCP with best efficiency. During ERCP, an endoscope is passed through the mouth, esophagus, stomach, and into the duodenum to access the opening of the bile ducts. Here's how ERCP can help: Stone Removal: ERCP allows the endoscopist to locate and remove gallstones from the bile ducts. Special instruments can be used to extract or break down the stones, relieving the blockage and restoring the flow of bile. Biliary Stenting: In cases where gallstones cannot be immediately removed, a stent can be inserted to keep the bile duct open. This helps in relieving the obstruction and allows for the passage of bile until further treatment can be performed. Sphincterotomy: In certain situations, the endoscopist may perform a sphincterotomy, which involves cutting the muscular ring (sphincter) at the opening of the bile duct. This widens the opening and facilitates the removal of gallstones. ERCP is a minimally invasive procedure that can effectively treat complications caused by gallstones in the bile ducts. By relieving the obstruction and managing associated infections, it helps in saving the patient from potentially life-threatening conditions. There are specialists like Dr Amit Maydeo who perform ERCP with great efficiency.
0 notes
Text
Which is the best cure for gastritis?
I'm not a doctor, but I can provide you some broad knowledge about gastritis treatment. The optimal gastritis treatment depends on the underlying cause and severity of the ailment. Gastritis is an inflammation of the stomach lining caused by a variety of factors including infection (e.g., Helicobacter pylori), excessive alcohol consumption, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), stress, autoimmune disorders, and other underlying health conditions.
Medications: Depending on the cause and severity of gastritis, your doctor may prescribe medications such as proton pump inhibitors (PPIs) to reduce stomach acid production, antacids to neutralize stomach acid, or antibiotics to treat an H. pylori infection.
Lifestyle modifications: Making certain changes to your lifestyle can help manage gastritis symptoms. These may include avoiding spicy and acidic foods, limiting alcohol consumption, quitting smoking, and managing stress levels.
Dietary changes: Following a gastritis-friendly diet may help alleviate symptoms. This typically involves eating smaller, more frequent meals and avoiding triggers such as spicy foods, fatty foods, caffeine, citrus fruits, and carbonated beverages. Instead, opt for a diet rich in fruits, vegetables, whole grains, lean proteins, and probiotic-rich foods.
Stress management: High levels of stress can worsen gastritis symptoms. Engaging in stress-reducing activities such as exercise, meditation, deep breathing exercises, and getting enough sleep can be beneficial.
Treating underlying conditions: If gastritis is caused by an underlying medical condition or infection, such as an H. pylori infection or an autoimmune disorder, addressing and managing that condition will be an important part of the treatment plan.
If you want to Live Healthy you should follow good health habits..
If you want to read more about this:CLICK HERE
It's crucial to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan. They will be able to evaluate your specific situation and recommend the best course of action for you

#GASTRIC#gastric sleeve#gastric bypass#gastric cancer#gastric issues#dies during gastric band surgery in turkey as heartbroken boyfriend pays tribute#health and wellness#wellness#Stress
0 notes
Text
Lupine Publishers | Pathological Aspect following Neoadjuvant Radiotherapy in Locally Advanced Rectal Cancer
Abstract
In locally advanced rectal cancer (LARC), neoadjuvant radiotherapy (RT) is usually performed. RT can avoid an aggressive operation and colostomy creation and can preserve the function of the anus. And various clinical trials for additional treatment, such as immunotherapy, which has recently attracted attention, after RT are being made. In rectal cancer, it is known that it is associated with mutational burden and MSI status rather than PD-L1 expression. Therefore, it is necessary to pay close attention to the pathological changes after RT to predict the efficacy of additional treatment after RT or to find a method for immune modulation for immunotherapy to work effectively.
Assessment of Post-Radiation Tumor Reduction and Sampling
First, the entire tumor volume is obviously reduced. Extravasated mucin, thickened and hyalinized vasculature was often observed. Compared to chemotherapy, which transforms into significant eosinophilic cytoplasm or bizarre morphology, the morphologic change of the tumor cell due to RT is slight. Because the operation is performed several weeks after RT, the tumor portion is replaced by dense fibrotic tissue and often regenerating surface epithelium rather than young fibroblasts. Because of only a tiny number of scattered tumor nests exist, it is difficult to confirm the remaining tumor tissue after RT for research grossly, even an experienced pathologist. So, it is so challenging to collect fresh tissue from an appropriate site. To proceed with research using the remaining tumor tissue after RT, it is appropriate to use formalin-fixed paraffin-embedded tissue as a laser dissection method through microscopic review. Alternatively, it is not easy to distinguish it from normal tissue, even using specific markers if fresh tissue is used. It is necessary to make a slide with the tissue on the mirror side and check whether there is a tumor or not. The evaluation of treatment responsiveness after radiotherapy is made by pathologic examination. The widely accepted tumor regression grade (TRG) is the American joint committee on cancer system, Mandard, and Dworak [1].
Tumor Budding after RT
Tumor budding is a unique tumor pattern known as one aspect of the epithelial mesenchymal transition of colorectal cancer. After RT, it is difficult to evaluate tumor budding because of the sparsely present tumor cells in a small number. However, there is a report that tumor budding of residual rectal cancer in post-RT samples is also related to prognosis such as overall survival. Loss of cohesiveness, that is, tumor budding, is related to nodal metastasis, the evaluation of tumor budding after RT was also related to disease specific recurrence in the pattern that appeared or remained after RT [2]. In the sample that received RT, it was evaluated into clusters of 4 or less tumor cells and 3-tiers - low, intermediate, and high, in the same way as the method for measuring tumor budding in general [3, 4].
Post-RT Immune Cell Infiltration and Components
Rectal cancer is a tumor with an active immune response than any other cancer. In post-RT surgical specimens, it is usually observed that immune cells are reduced, but in the early stage of RT, many inflammatory cells are thought to infiltrate as an inflammatory response. Immunoscore has also been evaluated a lot, and since TIL is known as a prognostic factor [5], it is necessary to evaluate the immune cell population after RT in the future.
Tumor Stroma in the post RT Specimen
In many studies, as an extracellular matrix, tumor stroma has been shown to affect tumor invasion and metastasis [6]. Generally, stroma-rich tumors are resistant to immunotherapy. In addition, it has been reported that stromal maturity can be used as a significant prognostic marker in a large number of cohorts in rectal cancer [7]. However, evaluation studies on the changes in stroma around the tumor after RT are not yet available.
Conclusion
Analysis of changes in the tumor surrounding microenvironment after RT will be a key to predicting the efficacy of RT and its combination therapy for chemotherapy and immunotherapy.
For more Lupine Publishers open access journals please visit our website:
https://lupinepublishers.com/index.php
For more Current Trends in Gastroenterology and Hepatology articles please click here: https://lupinepublishers.com/gastroenterology-hepatology-journal/index.php
#gastroenterotomy#hepatitis#journal#lupine publishers#open access journals#articles#gastric cancer#mini review#research#review#lupine journals#current trends in gastroenterology and hepatology
0 notes
Text
Early Sign Of Stomach Cancer
Stomach Cancer or gastric cancer develops in a person when their body’s cancer cells overpower the number of present healthy cells, which occurs in the stomach lining. While the early signs of gastric cancer can be uncertain, a few of them include indigestion, vomiting, nausea, appetite change, and heartburn.

0 notes
Text
Treatment For Gastric Cancer CancerSurgeryClinic
CancerSurgeryClinic is one of the best for cancer treatment led by Dr. Ganesh Nagarajan offers gastric cancer treatments in Mumbai and is a fairly uncommon type of cancer. The exact cause of gastric cancer is still unclear if you high smoking or salted foods and processed meat and low in vegetables are risk factors for stomach cancer. In many cases, gastric cancer can’t be completely cured, but…

View On WordPress
1 note
·
View note
Text
Best Treatment For Gastric Cancer By CancerSurgeryClinic

CancerSurgeryClinic is one of the best for cancer treatment led by Dr. Ganesh Nagarajan offers gastric cancer treatments in Mumbai and is a fairly uncommon type of cancer. The exact cause of gastric cancer is still unclear if you high smoking or salted foods and processed meat and low in vegetables are risk factors for stomach cancer. In many cases, gastric cancer can't be completely cured, but still possible to relieve symptoms and improve quality of life using chemotherapy and in some cases radiotherapy and surgery. For more details about the treatment of gastric cancer, you should visit over on the website.
0 notes
Photo

Gastric cancer is dangerous since it may not show signs and symptoms of its presence in the early stages. So, make sure to get screening done regularly.
0 notes