#gastrointestinal dysmotility
Text
Would not say that I have medical expertise in general but would say that I am pretty attuned to my own body. Correctly predicted what my doctors' differential diagnoses would be this time (adrenal issues, specifically re: cortisol; worsening GI dysmotility; potential small intestinal pseudo-obstruction)
#My small intestine is hella dilated on x-ray which bodes badly lol#I have to do 24 hour cortisol urine test for Cushing & Addison's#And we're initiating a 'more aggressive gastroparesis/dysmotility protocol'#I hope Medicaid will cover Motegrity if I do a bowel study in addition to my gastric emptying study#To show I have generalized gastrointestinal dysmotility prob secondary to dysautonomia
11 notes
·
View notes
Text
It's Gastroparesis Awareness Month
Hi! I have gastroparesis and I'm an insufferable know-it-all so let's talk about it!
Gastroparesis, or a paralyzed stomach, is a condition that causes delayed gastric emptying.
This can cause a range of symptoms and complications:
nausea
vomiting
early satiety/fullness
upper gastric pain
heartburn
malabsorption
dehydration
malnutrition
Gastroparesis can be treated by a gastroenterologist, but often needs to be managed by a motility specialist due to a lot of misconceptions about the condition. Providers, especially in the emergency department, will commonly misdiagnose gastroparesis as cannabis-hyperemesis syndome, cyclic vomiting syndrome, gastritis, food poisoning, etc.
There are several commonly known causes of gastroparesis like vagus nerve damage from diabetes, injury to the stomach, and stomach surgery like hernia repair or bariatric surgery. There are also idiopathic cases with no known cause. Other causes of gastroparesis are:
Connective tissue disorders like HSD and EDS (commonly hEDS and cEDS)
Post-viral (like COVID, viral gastritis, mononucleosis/Epstein-Barr)
Restrictive eating disorders
Autoimmune diseases like Systemic sclerosis (scleroderma), Lupus, Hashimoto's
Central nervous system disorders
Gastroparesis also has common comorbidities with conditions like:
POTS and other forms of dysautonomia (POTS, EDS, and gastroparesis are a common triad of diagnoses)
MCAS
SMAS (which can also present with similar symptoms to GP)
Intestinal dysmotility and esophageal dysmotility disorders (known as global dysmotility)
PCOS with insulin resistance
Endometriosis
SIBO/SIFO
Chronic intestinal pseudo-obstruction
Migraines
Certain medications like Ozempic and other drugs in that class act on the digestive system to delay gastric emptying, which has caused people to be diagnosed with gastroparesis. Some people report that their cases have not gone away since stopping the medication, others report feeling better after stopping. Other drugs like opiates and narcotics can cause delayed gastric and intestinal motility as well, but these are commonly known side effects of those painkiller classes.
Gastroparesis is classed based on severity and graded based on how you respond to treatment.
Severity of delay ranges from mild to very severe, and this is based on your actual stomach retention calculated at 4 hours into a gastric emptying study.
The grading scale ranges from one to three, one being mild and three being gastric failure.
There is no consistent single treatment that is proven to work for gastroparesis, and there is no cure. Treatments can consist of:
Diet changes (3 Step Gastroparesis Diet, liquid diet, oral sole source nutrition)
Prokinetic (motility stimulating) drugs
Anti-nausea medications
Proton-pump inhibitors
Gastric stimulator/gastric pacemaker
Pyloric botox and dilation
G-POEM/pyloroplasty
Post-pyloric tube feeding
Gastric venting/draining
Parenteral nutrition
IV fluids
Other surgical interventions like gastrectomy or rarely, transplant
Gastroparesis is a terrible disease and I hope that if any of these symptoms resonate with you that you can get checked out. I was misdiagnosed for a long time before getting a proper gastroparesis diagnosis, and all it took was a gastric emptying study. This is ESPECIALLY true if you're having post-COVID gastrointestinal problems that are not improving. I almost died from starvation ketoacidosis because of how serious my GP got in a short period of time post-COVID (I had GP before COVID), and now I'm tube reliant for all my nutrition and hydration.
Stay safe friends!
597 notes
·
View notes
Text
Yknow, this is likely a result of having worked too long in a Pediatric Feeding Disorders Unit, and being someone who also has both a history of extreme food selectivity (thankfully grown/ trained out of) and who struggles with dysphagia/aspiration and dysmotility (from the esophagus through the colon) but I truly think Seven of Nine would have a much more difficult time adjusting to actually eating food???
Like I worked with kids who were G-Tube and occasionally nasogastric and nasojejunal tube dependent. It isn’t easy. It’s doable, there are protocols, but ??? There’s a fair amount of discomfort involved.
Like, it takes intensive occupational therapy to develop the motor skills to chew, manipulate food within your mouth, etc…you need to ensure they can swallow safely and effectively (even if they “seem fine,” silent aspiration and fatigue can be dangerous).
Then you get into trying new foods… there’s a lot of sensory stuff!! Obviously Seven is an adult, so she likely won’t demonstrate the same overwhelming neophobia that the 2-8 year olds I worked with would have! But I imagine she would probably be picky initially (especially with Neelix’s concoctions, which most of the crew found often unpalatable due to being unusual).
And as most of us with gastrointestinal issues know, that is also no picnic (hah). She likely wouldn’t have the enzymes she once had, and I’m willing to bet her microbiome was pretty starved. Probably they have a hypo for that, but it’s still an issue…
Obvious disclaimer, it is a fairly niche thing to think about (and not pretty), this is television, entertainment, and sci-fi, so maybe they can magically make it as if she was eating her whole life…
But it’s still something that I cannot stop thinking about.
#food cw#star trek#voyager#star trek voy#voy#seven of nine#I’m so sorry guys the autism is firing on all cylinders#feeding disorders#dysphagia
300 notes
·
View notes
Text
Breakthroughs in Treatment: Gastric Motility Disorder Drug Unveiled

Gastric motility disorders can significantly impact an individual's quality of life, leading to symptoms such as bloating, nausea, and delayed gastric emptying. Fortunately, recent advancements in medical research have led to the development of promising treatments, including the introduction of novel Gastric Motility Disorder Drug therapies.
Exploring the Potential of Gastric Motility Disorder Drug:
Targeted Therapeutic Approach: Gastric Motility Disorder Drug therapies aim to address the underlying causes of gastric dysmotility, targeting specific receptors or pathways involved in gastrointestinal motility regulation. These drugs offer a more targeted and effective approach to symptom management compared to traditional treatments.
Improved Symptom Management: Clinical trials of Gastric Motility Disorder Drug therapies have shown promising results in improving symptoms associated with gastric motility disorders. From reducing bloating and abdominal discomfort to enhancing gastric emptying, these drugs offer hope for individuals struggling with gastrointestinal symptoms.
Benefits of Gastric Motility Disorder Drug Therapy:
Enhanced Treatment Efficacy: Gastric Motility Disorder Drug therapies offer enhanced treatment efficacy compared to conventional approaches. By targeting specific mechanisms involved in gastric dysmotility, these drugs can effectively alleviate symptoms and improve overall gastrointestinal function.
Increased Patient Compliance: The introduction of Gastric Motility Disorder Drug therapies may improve patient compliance with treatment regimens. With the potential for fewer side effects and improved symptom relief, patients are more likely to adhere to their prescribed medication, leading to better long-term outcomes.
Potential for Personalized Medicine: As research in Gastric Motility Disorder Drug therapies continues to advance, there is potential for personalized medicine approaches tailored to individual patient needs. By identifying specific genetic or molecular markers associated with gastric motility disorders, clinicians can prescribe targeted therapies for optimal treatment outcomes.
Get More Insights On This Topic: Gastric Motility Disorder Drug
#Gastric Motility Disorder Drug#Gastrointestinal Health#Digestive Disorders#Pharmacotherapy#Medical Innovation#Symptom Management#Healthcare Advances#Therapeutic Breakthroughs
0 notes
Text
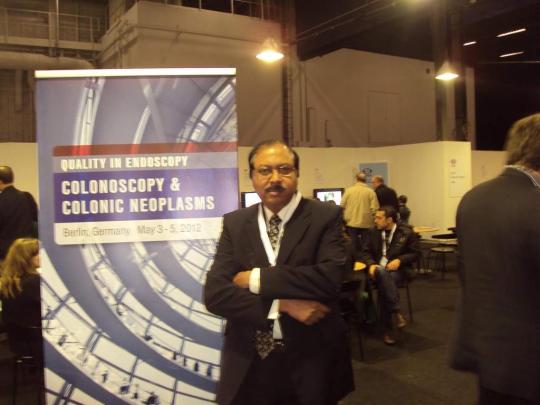
best gastroenterologist in adyar
Why would you see a gastroenterologist?
A gastroenterologist is a doctor specialized in diagnosing and treating intestinal problems. Gastroenterologists are sometimes called "GI doctors" because they specialize in conditions that affect the gastrointestinal (GI) system. Gastroenterologists comprehensively understand how the digestive system and its structures work. They primarily treat conditions that affect specific areas of the body, such as:
Stomach
Small intestine
Colon
Rectum
Esophagus
Pancreas
Gallbladder
Liver
Bile ducts
For this you need to consult best gastroenterologist in Adyar!
When to see a gastroenterologist?
Abdominal Pain or Discomfort
Chronic Digestive Issues
Changes in Bowel Habits
GI Disease Screening/Treatment
Endoscopic Procedures
Liver/Gallbladder/Pancreas Concern
Latest Technology related to Gastroenterology
Capsule endoscopy
Single balloon enteroscopy
Endoscopic ultrasound (EUS)
Endoscopic retrograde cholangiopancreatography (ERCP)
High resolution esophageal and anorectal manometry
Hydrogen breath test
What is the job of a gastroenterology specialist?
Liver disease is central focus area of a gastroenterology specialist. Huge number of patients with acute and chronic liver disease (cirrhosis) due to hepatitis B, C, A and alcohol.
The gastroenterology specialists provide advice and suggest measures to the patients with liver disease because of alcohol intake, liver viruses, etc.
Treatment for liver failure and portal hypertension
Treatment for acute &chronic pancreatitis
Treating the upper & lower gastrointestinal bleeding
Oesophageal disorders such as hiatus hernia, reflux dysmotility, etc
Gastric/duodenal disease like gastric ulcer
Intestinal and colorectal diseases like motility disorders, malabsorption, bleeding, infections, irritable bowel disease, colitis, Crohn's disease, etc.
𝐆𝐄𝐂𝐋𝐈𝐍𝐈𝐂&𝐄𝐍𝐃𝐎𝐒𝐂𝐎𝐏𝐘𝐂𝐄𝐍𝐓𝐑𝐄 – Best gastroenterologist in Adyar
This hospital was established to meet the special needs of patients with gastrointestinal diseases. It provides the latest modality of high-quality tertiary services in gastroenterology. The center has a highly qualified medical team of medical professionals led by Dr.S.Ganesh, best gastroenterology specialist in Chennai supported cutting-age equipment such as laparoscopic surgical equipment, video endoscopes, fully equipped ICUs, and highly advanced OT equipped with an image intensifier. Emergency and elective care is given for widespread liver and gastrointestinal diseases from the simplest to the most complex.
0 notes
Text
Hospital Stay and Feeding Tube Update
Well, hello there! I feel as if so much has happened over the last few months. It is kind of surreal to be on the other side of things. I am now trying my best to adjust to my new normal. I wanted to give everyone an update on all that has happened since May. This is the easiest platform to do that as I can update everyone all at once.
As many of you know, last Fall I was diagnosed with Superior Mesenteric Artery Syndrome (SMAS) and Nutcracker Syndrome (NCS). I have been struggling with severe digestive issues since I was 14, but had always managed it with medications and close monitoring. That was until I got much more ill in 2018 with worsening digestive symptoms and I was eventually diagnosed with severe irritable bowel syndrome (IBS) and an unspecified functional gastrointestinal dysmotility disorder in 2019. Then I got a combo bacterial and viral illness in the summer of 2019 and things went downhill quickly. I was diagnosed with Postural Orthostatic Tachycardia Syndrome (POTS) in early 2021 and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) in early 2022.
What happened in May? Why was I hospitalized again? Well, I was doing ok after my last hospital admission in Sept-Oct 2021. I was eating enough to maintain a little bit of weight after I successfully weaned off of TPN. So, we started to change some of my medications as they were interacting and causing some unpleasant nighttime hallucinations and cardiac issues. However, my digestive tract was not happy and I went into the worst GI flare-up I have ever had. After weaning off of some of the medications, I rapidly lost a significant amount of weight and my SMAS came back with a vengeance. This manifested as severe vomiting and horrendous pain. Now, I have dealt with vomiting for the last 5 years and I thought I was used to it. This was nothing like I had ever experienced before, so to the ER for Mae. This was after a full week of me not managing to keep any food or liquids down and none of my emergency nausea meds working.
By the time I got to the ER I was in bad shape and they admitted me immediately. However, not without a few blips. I was originally admitted to an active Covid outbreak unit, so I panicked and signed myself AMA – “Against Medical Advice”. That was honestly the scariest thing I have gone through. I returned home and proceeded to have the worst night of my life. I barely remember any of it. I remember a call with my psychologist, an ambulance ride, and arriving back in the ER. I was then sedated as the vomiting was severe and causing me to go into a panic, which would then make the vomiting worse. I was sent to a different hospital and admitted immediately again. This time on the oncology unit so as to ensure Covid safety for me as I am high risk. I am thankful for the doctors and nurses who made that hospital switch possible and took my Covid protections seriously.
Now, I am in hospital and confused as to what was to be done with me. I didn’t want to be put on TPN again as I had a horrible reaction to my PICC line and I didn’t know how they were going to treat the SMAS. I found out within the first few days that they were not going to let me leave until I had my nutrition stabilized again, which I was relieved to hear. Last time they sent me home prematurely because they didn’t have a special type of feeding tube in stock. So, I found out that during this admission they did have the feeding tube in stock and that they were finally going to trial it. Cue me waiting over a week for Interventional Radiology to find me a spot for the placement of the nasojejunal (NJ) tube.
During the first week of my hospital stay I was kept on fluids. Lactated ringers, potassium infusions, saline, and an attempt at PPN. You can imagine my veins were not very happy. I also received my first iron infusion which went swimmingly and I felt amazing. Eventually I was able to get my NJ tube placed and I tolerated it well. I thought that this is where it would end and I would be allowed to go home with my NJ tube to trial and see how I tolerated it. Instead they kept me in hospital for two more weeks to see how I tolerated it under medical supervision. Then I got the news that they would be placing a surgical tube so I would have a more permanent solution to my nutrition problems.
I was quickly booked in for surgery and I had an initial PEG tube placed. The recovery for that was brutal. I have never been in that amount of pain. I guess cutting a whole through your abdominal wall and placing a tube there isn’t what your body wants. Who would’ve thunk, lol. After a week of letting that heal, I was then taken down to have the jejunal extensions placed so I could start feeds again. Once it was all said and done, I had a beautiful PEG-J successfully placed with no major complications. It was the best outcome after so many things going wrong over the past few years. Once I was tolerating feeds again, I was allowed to go home. That ended my 5 week hospital admission.
I have now been home for over a month and the adjustment to my new life has been difficult. Due to my ME/CFS, the recovery has been extremely difficult. It sent me into a 4 week long crash and I am only just now starting to come out of the fog and return to somewhat of a baseline. I am so thankful for this tube, but the additional tasks it has added to my plate means that other things in my life have had to give. The time it takes to set up my feeds and clean my tube site is something I’m still trying to get used to. However, it has been amazing to see the colour slowly return to my face and to see some of my gastrointestinal symptoms dull a little bit. It’s amazing what stable nutrition can do.
I had a follow-up with my gastroenterologist and feeding tube nurse last week after some worsening site pain and radiating back pain. I basically couldn’t sit upright for more than a few minutes at a time for close to two weeks. They believe my GI tract is just having a bit of a temper tantrum and my abdominal muscles are still trying to regrow around the tube. So, I will be introducing some new medications over the next few weeks and if it doesn’t calm down then another scope and ultrasound are on the table. Fingers crossed my body will cooperate and I can avoid another scope. 10/10 would not recommend.
Now I am hoping that I will slowly have more energy from my feeds and will be able to start getting back to the things I love. I have to be really careful though because of all my comorbidities which make recovery much more challenging. I am just so beyond ready to be able to leave the house by myself and maybe do a couple fun things every month just to escape. You really don’t appreciate the outside world until you suddenly can’t safely access it. In combination with my feeding tube and mobility aids, I am hopeful I will be able to develop a new kind of relationship with the outside world.
I am sending so much love to people who are going through similar situations and who are trying to adapt to life 2.0. It can be really scary. I know it has been tremendously hard for me to get used to a medical device hanging out of my body. It is life giving and life sustaining, but that doesn’t mean it is easy to accept or adapt to. It is terrifying at times to know my infection risk has increased and that I have to factor in my tube to every decision that I now make. I thought for a long time that I might just be able to will my body into being able to eat and that I could avoid a permanent tube, but bodies and health don’t work that way. And now that I have made that jump I am so thankful I was brave enough to go ahead with it. I have already noticed so many positive changes in my day-to-day life.
Here’s to medical devices and modern medicine. It is astounding that we can give people a chance at life. I don’t know where I would be right now if I didn’t go through with the procedure and get this tube placed. I already appreciate it so much. I will now be properly nourished and that is worth everything. Here’s to life 2.0 and making progress! Xx
0 notes
Text
What is Irritable bowel syndrome (IBS)? Discuss Symptoms, treatment & types of it join us at the 13th World Gastroenterology, IBD & Hepatology Conference from December 15-17, 2023 in Dubai, UAE & Virtual.
IBS (Irritable Bowel Syndrome)
You may experience uncomfortable or painful abdominal symptoms if you have irritable bowel syndrome, or IBS. IBS symptoms include constipation, diarrhoea, gas, and bloating. IBS does not cause digestive problems or increase your risk of colon cancer. Symptoms are frequently manageable via dietary and lifestyle adjustments.
What precisely is irritable bowel syndrome (IBS)?
Irritable bowel syndrome, sometimes known as IBS, is a collection of symptoms that affect your digestive system. It is a common yet unpleasant gastrointestinal condition. IBS patients have excessive gas, stomach pain, and cramping.
What exactly is a functional gastrointestinal disorder?
Irritable bowel syndrome (IBS) is a form of functional gastrointestinal (GI) illness. These illnesses, often known as disorders of the gut-brain interface, are caused by issues with how your stomach and brain interact.
These issues make your digestive tract extremely sensitive. They also alter the contraction of your gut muscles. As a result, abdominal pain, diarrhoea, and constipation occur.
What are the many forms of IBS?
IBS is classified by researchers based on the type of bowel movement difficulties you encounter. The type of IBS you have can influence your treatment. Certain medications are only effective for certain forms of IBS.
People with IBS frequently have normal bowel movements on some days and abnormal ones on others. The type of IBS you have is determined by the abnormal bowel motions you have:
IBS with constipation (IBS-C): Your stool is mostly hard and lumpy.
IBS-D: The majority of your stool is loose and watery.
IBS with mixed bowel habits (IBS-M): On the same day, you experience both hard and lumpy stool movements and loose and watery movements.
What is the impact of IBS on my body?
The colon muscle contracts more in patients with IBS than in people who do not have the ailment. Cramping and pain are caused by these contractions. IBS patients also have a decreased pain tolerance. Excess bacteria in the GI tract may potentially contribute to symptoms in patients with IBS, according to research.
Who is at risk of getting IBS?
The illness most commonly affects persons in their late teens to early forties. Women are twice as likely as males to get IBS. Multiple family members may suffer from IBS.
You may be more vulnerable if you have:
IBS runs in the family.
Anxiety, tension, or emotional stress.
Intolerance to certain foods.
Physical or sexual abuse in the past.
Infection of the digestive tract.
What causes IBS?
You may have found that some things aggravate your IBS symptoms. Some meals and medications are common triggers. Emotional stress is another possible factor. Some researchers believe that IBS is the gut's reaction to pressures in life.
How widespread is IBS?
IBS affects 10% to 15% of the adult population in the United States, according to experts. However, only 5% to 7% of people are diagnosed with IBS. It is the most prevalent condition diagnosed by gastroenterologists.
What are the origins of IBS?
Researchers aren't sure what causes IBS. They believe that a combination of factors, including:
Dysmotility refers to issues with how your GI muscles contract and move food through your digestive tract.
Extra-sensitive nerves in the GI tract are known as visceral hypersensitivity.
Miscommunication between nerves in the brain and the gut is referred to as brain-gut dysfunction.
What are the symptoms of IBS?
IBS symptoms include:
Cramps or abdominal pain, commonly in the bottom portion of the abdomen.
Bloating.
Harder or softer bowel movements than normal.
Diarrhoea, constipation, or a combination of the two.
Extra petrol.
Mucus in your stool (it may appear yellowish).
Symptoms of IBS in women may worsen during their periods. These symptoms frequently reoccur, which might make you feel agitated or irritated. You'll start to feel better physically and mentally as you learn how to handle flare-ups.
What exactly is IBS treatment?
Although no single therapy is effective for everyone, most people with IBS can discover a treatment that works for them. Your IBS treatment plan will be tailored to your specific needs by your healthcare professional. Dietary and lifestyle changes are common therapy choices. A nutritionist can assist you in dev;eloping a diet that is appropriate for your lifestyle.
Connect with us: - https://gastroenterology.universeconferences.com/
Email: [email protected]
0 notes
Text
What is the Best Probiotic for IBS?
Irritable Bowel Syndrome (IBS) significantly reduces the quality of life of the people affected by the condition. Its symptoms include constant abdominal pain, diarrhea, constipation, or even a mixture of the two.
Imagine skipping school and work, getting constantly worried about dining out, and having your daily routines affected by IBS.
The main cause of irritable bowel syndrome is still unknown, but according to recent studies, having an imbalance of microorganisms living in your digestive tract may be one of the precursors of having irritable bowel syndrome for some individuals.
So, what does this information exactly mean? It means that people with IBS would benefit from restoring the good balance of bacteria inside their gut, and restoring the microbiota can significantly reduce the severity of IBS symptoms.
The easiest way to introduce beneficial bacteria into your gut microbiota is by taking probiotic supplements.
In this article, you will be guided through everything you need to know regarding probiotics, how they can help you with your IBS symptoms, and the best probiotic for IBS that you can safely take.
What are probiotics?
Probiotics are live microorganisms that are intended to have health benefits. Probiotics are found in supplements, foods, and beverages. Probiotic bacteria are essential in keeping the oral and gut microbiota.
Different probiotic strains can improve overall gut health, help your body fight autoimmune diseases, and also target other diseases.
In relation to IBS symptoms, certain probiotic strains promote an anti-inflammatory response and improve gut dysmotility, wherein the muscles of the gastrointestinal tract do not work properly which leads to issues with digestion.
A meta-analysis that consists of more than 30 studies conducted by the American College of Gastroenterology concluded that taking probiotics may significantly improve IBS symptoms.
Specifically, these symptoms include reduction of abdominal pain, bloating, and flatulence among IBS patients.
On the other hand, the meta-analysis stated that the quality of evidence found in the studies is low.
Also, particular recommendations regarding the dosage of probiotic supplements are not verified.
A clinical trial that focused on the consumption of the probiotic strain Bifidobacterium bifidum MIMBb75 reported that it can bring positive outcomes to IBS symptoms if taken once every day.
The trial also concluded that the Bifidobacterium bifidum MIMBb75 probiotic strain bonds more effectively in the intestinal cells which results in a significant increase and strengthening of the intestinal barrier.
Also, this probiotic strain enhances the overall intestinal microbiota of IBS patients.
Benefits of Probiotics
We are often asked questions regarding how exactly would a probiotic supplement help IBS patients.
Questions such as "Should I take probiotics for IBS?", "How can I benefit from taking probiotics while having IBS symptoms?", and other emerging questions about the significance of probiotics for IBS are indeed important to answer.
This section will help you learn more about the different benefits that IBS patients can get from taking probiotic-rich foods and supplements.
Fights Off Inflammation
A study revealed that using probiotics can provide significant improvement in IBS symptoms and it is mainly because of their ability to prevent and alleviate inflammation in the body.
Also, they are able to restore the natural balance of beneficial bacteria and harmful bacteria to keep the gut healthy enough to fight off inflammation.
Boosts Immune System
Probiotics can boost our immune system by helping to keep our gut healthy. A healthy gut is important for a strong immune system because it is where we produce most of our white blood cells.
Slow Down the Growth of Bad Bacteria
They can help prevent the growth of bad bacteria by competing for space and nutrients. These good bacteria adhere to the intestinal cells, thus, preventing disease-causing bacteria to grow inside the gut. Probiotics also produce antimicrobial substances and stimulate the immune system.
Prevents Excessive Gas
Probiotics can help prevent excessive gas by keeping the digestive system balanced and healthy.
When the digestive system is working properly, it is less likely to produce excess gas. Probiotics also help break down food so that the body can absorb nutrients more efficiently.
More Controlled Speed of Bowel Movements
For IBS D patients who have diarrhea as their predominant symptom, taking probiotics can help with bowel motility.
Bowel motility is referred to as the movement of food starting from the mouth and out of the body. Bowel motility is significantly reduced in terms of speed, which also reduces bowel movement.
What Are the Best Probiotics for IBS?
Now that we have learned quite a lot about probiotics and their benefits, the next step is to find the best probiotics for IBS.
It is important to choose a brand that uses Low FODMAP ingredients to ensure that no other IBS symptoms would be triggered while you consume the supplements.
Many clinical trials have revealed the best probiotics for improving the symptoms of IBS contain strains such as:
Saccharomyces boulardii
According to a study in 2012, there were several clinical trials and experiments to measure the efficiency of Saccharomyces boulardii in treating various gastrointestinal disorders and helping the gut flora return back to its normal state.
It is also mentioned that it gives a lot of beneficial effects on patients dealing with acute and chronic GI issues. This probiotic is also usually prescribed to patients with diarrheal diseases over the past 30 years.
Florastor® Daily Probiotic Supplement
The Florastor Daily Probiotic capsules are vegetarian-safe probiotic supplements that are made from yeast-based probiotics.
The main strain for this probiotic is the Saccharomyces boulardii CNCM I-745. A study regarding this supplement stated that it is effective in decreasing the frequency of diarrhea due to gastrointestinal disorders.
Patients may take the Florastor Daily Probiotic Supplement twice daily. It may also be taken in combination with your medications for IBS-related symptoms.
PROS:
Over 600 clinical studies done on the predominant ingredient
No refrigeration needed
CONS:
Expensive
Not safe for lactose intolerant patients
Provides only one strain of yeast
Lactobacillus (L.) acidophilus
Lactobacillus (L.) acidophilus is purposely trialed to test for abdominal pain and bloating due to IBS and it is currently the most prominent strain for research among the acidophilus species.
According to over 45 clinical trials, L. acidophilus is considered to be the best probiotic strain worldwide and it can definitely help improve the immune system, other gut issues, and overall health.
Casa De Sante Low FODMAP Advanced Probiotics for IBS and SIBO
This supplement is great for vegans and vegetarians. Plus, it is safe to take for patients with Small Intestinal Bacterial Overgrowth.
It is also made from all-natural ingredients containing 5.75 billion Colony Forming Units (CFU).
PROS:
Non-GMO
Vegan
Low FODMAP
Soy and Gluten-free
CONS:
Manufactured in a facility that also processes milk, egg, wheat, soy, and nuts.
Bifidobacterium bifidum MIMBb75
It was proven that taking the Bifidobacterium bifidum MIMBb75 daily can provide significant relief to all IBS symptoms.
There was more than 30% of improvement for IBS associated with abdominal pain using the Bifidobacterium bifidum MIMBb75. Other symptoms like irregular bowel movements and bloating are reduced and alleviated, thus, improving the quality of life.
Kijimea™ IBS
The globally distinctive and patent-protected bacterium strain B. bifidum MIMBb75 is present in the Kijimea™ IBS supplement. The supplement has been clinically proven to alleviate IBS symptoms like chronic abdominal pain, flatulence, bloating, diarrhea, and constipation.
The brand also claims that they manufacture these supplements without any sweeteners, preservatives, lactose, flavoring agents, and gluten. It can also be taken by people diagnosed with diabetes.
PROS:
Activated within a few seconds
Ideal for patients with diabetes
CONS:
Can cause mild gas or cramps
Probiotics and IBS-related Conditions
Probiotics and Constipation
A recent 90-day clinical trial revealed that IBS patients who have taken probiotic mixtures had favorable responses for constipation, bloating, cramping, and abdominal pain.
Among 122 IBS C patients, 66-90% reported a significant improvement for their symptoms by taking probiotics for 60 days.
Probiotics and Diarrhea
The symptoms of IBS diarrhea type (IBS D), which include loose stools, an urgent need to urinate, and abdominal pain, are likely to torment you.
There isn't a single optimal probiotic for IBS diarrhea that will completely cure the problem, but there are probiotics for IBS D that, if taken frequently, may lessen the symptoms.
The probiotic yeast Saccharomyces boulardii is one of the most promising probiotics for treating symptoms of IBS D.
According to a 2014 study, S. cerevisiae was more effective when combined with ispaghula husk, a form of dietary fiber used to treat bowel movement problems.
Boulardii had an anti-inflammatory impact that may have contributed to an improvement in symptoms overall.
Probiotics and Flatulence
The large intestine's bacteria may be to blame for excessive flatulence. Hard-to-digest dietary fibers and undigested food that enters your gut are broken down by your microbiota.
Gases may be produced as a result of this procedure, which would worsen belly pain and flatulence.
IBS sufferers may be more vulnerable to abdominal pain brought on by typical levels of gas. According to research, their gut lining is more responsive to pain signals than that of healthy individuals.
Probiotics and Bloating
Certain clinical trials using the probiotic strains Bifidobacterium infantis 35624, B. bifidum MIMBb75, and B. lactis 2‐173 010 concluded significant relief of bloating symptoms of IBS.
Probiotics and Small Intestine Bacterial Overgrowth
Patients with small intestinal bacterial overgrowth (SIBO) are not advised to take probiotics or any probiotic supplement.
The reason behind this is that taking probiotics when you have SIBO would just worsen your symptoms.
The good bacteria from the supplement would be trapped in the small intestines. The small intestines would then notice that these bacteria are not providing needed benefits to the GI tract, the small intestine will try to flush out these microbes and that's when SIBO symptoms emerge.
Are Probiotic Supplements the Best Option for Treating IBS Symptoms?
These supplements are not necessarily the best option for treating IBS symptoms. While they may help some people, there is no guarantee that they will work for everyone.
There are other options available, such as dietary changes and medications, that may be more effective for treating IBS symptoms.
Risks and Side Effects of Probiotics for IBS
There are a few risks and side effects to consider when taking probiotics for IBS. IBS patients should take note of the following risks:
Bloating, Gas, or Diarrhea
Some people may experience bloating, gas, or diarrhea. These side effects are usually mild and go away after a few days.
Small Risk of Infection
There is also a small risk of infection, especially if the probiotic is taken orally. This risk can be minimized by taking the probiotic with food or milk.
Conclusion
Probiotics are indeed helpful for individuals with gut disorders, especially IBS. However, it is always best to check with a GI expert or a Registered Dietitian before taking probiotics along with your IBS medications.
source
https://casadesante.com/blogs/digestive-wellness/best-probiotic-for-ibs
0 notes
Text
No structural abnormality in collagen or related proteins or in the genes encoding such molecules has been identified in the vast majority of patients with hEDS (hypermobile Ehlers Danlos Syndrome).
Joint hypermobility alone is very common in the general population, affecting approximately 10 to 20 percent of individuals to some degree; it may either be present in isolated joints or be more generalized throughout the body. Most people with joint hypermobility alone do not experience any problems from the condition.
The major clinical features in both HSD (Hypermobile Spectrum Disorder) and hEDS (hypermobile Ehlers Danlos Syndrome) are symptoms and findings related to the musculoskeletal system. In hEDS, there are also skin changes, including fragility of skin and supportive connective tissues, and some features common to other hereditary disorders of connective tissue (HDCT). Additionally, in both HSD and hEDS, systemic features are often present, including chronic widespread pain, fatigue, autonomic dysfunction, and gastrointestinal dysmotility.
The diagnosis of HSD and hEDS is made clinically, and that for hEDS based upon the medical history and physical examination, using the 2017 international criteria, which describe the combinations of musculoskeletal and other historical and clinical findings that may be used to make the diagnosis; there are no diagnostic laboratory tests for HSD or hEDS. A component of the criteria is ascertainment of the Beighton score for joint hypermobility, which should be evaluated in all patients suspected of having a hypermobility-related disorder. It is important to exclude other conditions with similar or overlapping features, which in some patients may require referral to a medical geneticist or other expert.
The differential diagnosis includes the conditions that have generalized joint hypermobility as a clinical feature, particularly Marfan syndrome and other types of Ehlers-Danlos syndrome (EDS).
Additional testing may be required to either help establish the diagnosis (eg, by excluding other conditions) or to further characterize symptoms or abnormal findings identified in the history and physical examination; testing depends upon the specific clinical findings and may include imaging of the peripheral joints and spine, laboratory testing to exclude other disorders, echocardiography, bone mineral density testing, evaluation for autonomic dysfunction, and other studies
1 note
·
View note
Text
Digestive System and Gastroenterology Specialist Treatment
Gastroenterology is the study of normal functioning and ailments related to the stomach, esophagus, small intestine & large intestine, pancreas, gallbladder, rectum, bile ducts, and liver. This includes the movement of substances through the stomach & intestines (motility), the digestion & absorption of nutrients in the body, removal of waste products from the system, and the functioning of the liver as a digestive organ.
What is the job of a gastroenterology specialist?
· Liver disease is central focus area of a gastroenterology specialist and there are a huge number of patients with acute and chronic liver disease (cirrhosis) due to hepatitis B, C, A and alcohol.
· The gastroenterology specialists provide advice and suggest measures to the patients with liver disease because of alcohol intake, liver viruses, etc.
· Treating liver failure and portal hypertension
· Treating acute & chronic pancreatitis
· Managing the upper & lower gastrointestinal bleeding
· Oesophageal diseases like hiatus hernia, reflux dysmotility, etc
· Gastric/duodenal disease like gastric ulcer
· Intestinal and colorectal diseases such as motility disorders, malabsorption, bleeding, infections, irritable bowel disease, colitis, Crohn's disease, etc.
Why do you choose 𝐆𝐄 𝐂𝐋𝐈𝐍𝐈𝐂 & 𝐄𝐍𝐃𝐎𝐒𝐂𝐎𝐏𝐘 𝐂𝐄𝐍𝐓𝐑𝐄?
Physicians and residents have long felt the need for quality medical care for diseases of the liver and gastrointestinal tract. GE CLINIC & ENDOSCOPY CENTRE has been established in keeping the unique needs of the patients suffering from gastrointestinal diseases in mind. It provides the latest mode of high-quality tertiary services in gastroenterology. The hospital is equipped with the best gastroenterology specialist in Velachery.
The center has a highly qualified medical team of medical professionals led by Dr. S.Ganesh, the best gastroenterology specialist in Velachery aided by cutting-age equipment such as laparoscopic surgical equipment, video endoscopes, fully equipped ICUs, and highly advanced OT equipped with an image intensifier. Emergency and elective care is given for widespread liver and gastrointestinal diseases from the simplest to the most complex.
0 notes
Text
Reading excerpts of Brzozowski's prison letters in Wiadomości and reading about his trial (trapped in the bathroom)
#The downside to Xolair working is#Temporary respite from gastrointestinal dysmotility after a long lapse#You WILL be in the bathroom
6 notes
·
View notes
Note
Theres motility specialistist?!? <- Guy who has been diagnosed with gp for 7 years. I was diagnosed at 14 and had a hard enough time finding a gastroenterologist that would see me, and then I turned 18 during COVID and I just... gave up on professional treatment for a while. To be fair I only have a mild to moderate case (I think) but damn...
Yes! They specialize in esophageal, gastric, and intestinal dysmotility! I highly encourage seeing if there are any in your area.
If you have the luxury of travel, some clinics will do one in-person appointment and then do the rest via telehealth. They can be put through out of network exceptions if you’re in the US. Mayo Clinic and Cleveland Clinic have the leading motility clinics that I’m aware of, but there are other motility specialists.
List of US Neurogastroenterologists and Motility Specialists (r/gastroparesis)
G-PACT list of US Motility Doctors
The Association of Gastrointestinal Motility Disorders also has lists of physicians, centers, dietitians, and other experts from around the world.
21 notes
·
View notes
Text
Protective Effect of Methylxanthine Fractions Separated through Bancha Herbal tea Simply leaves in opposition to Alpelisib-Induced Cardio- and Nephrotoxicities throughout Rats
5%, in which minimal Pol eta level ended up being significantly connected with large total response price (p=0.Goal), while not connected with total emergency. In addition, simply no significant link has been observed among Pol eta appearance amount together with girl or boy, get older, tobacco/alcohol record, tumor point as well as metastatic status. Conclusions: Our own data advise that Pol eta appearance may be a valuable idea sign for your performance of american platinum eagle as well as gemcitabine primarily based treatment regarding HNSCC.Launch Partly digested incontinence is really a incapacitating issue using considerable influence on standard of living. The unreal bowel sphincter can be utilized being a treatment method alternative within serious cases through which truth be told obtrusive way of treatment therapy is enough. Results Risk of infection along with hardware disappointment will be involving distinct concern within this synthetic unit. Conclusion We record an uncommon delayed side-effect: balloon dilation on account of hypertonic teeth fillings.Postoperative ileus is often a temporary digestive tract dysmotility that develops following #Link# various types of procedures and is also a standard side-effect involving stomach medical procedures. Mosapride citrate is definitely an agonist in the 5-hydroxytryptamine Several receptor and also speeds up upper stomach mobility. Simply no research features examined it's effect on #Link# digestive mobility right after surgical treatment. The aim of this research ended up being investigate whether mosapride citrate decreases the duration of postoperative ileus. Thirty individuals along with colon cancer whom experienced colectomy ended up separated into two organizations: the mosapride party and also the handle class. The mosapride group gotten mosapride 15 milligram by mouth which has a small volume of water 3 x per day, beginning upon postoperative first day. The particular control class gotten simply a small level of normal water for a passing fancy routine. People were permitted to resume mouth giving upon postoperative day time Four. Postoperative time for it to very first flatus along with defecation have been looked at, as well as the volume of food intake ended up being seen. Gastrointestinal mobility had been recorded on postoperative day time 8. The physical appearance proportion involving interdigestive moving contractions and the mobility list on the antrum and duodenum had been considerably higher inside the mosapride party in comparison to the actual management team. The time for you to very first flatus along with defecation ended up significantly quicker within the mosapride party than in the particular control group. The amount of food consumption on postoperative times Some and seven was drastically bigger inside the mosapride class compared to your management class. Mosapride citrate decreases the duration of postoperative ileus and may even improve results after stomach medical procedures.Cellular the big area involving acidity dirt throughout Asia, an effort appeared in our analysis to study the particular anti-microbial possible regarding bacterial bacteria via acidity soil associated with #Link# Mahishapat, Dhenkanal, Odisha. 4 microorganisms isolated from the garden soil sample (ph Five.
0 notes
Text
New Year's platitudes and resolutions so often emphasize health, and they leave such a sour taste in the mouths of chronically ill folks. “Healthy” just isn't an attainable goal for most of us. It is not something we can ever fully achieve through any available means - eating well, exercising more (or even at all, for some!), positive thinking, practicing yoga, drinking enough water, or doing x, y, or z - and it hurts to be constantly reminded of that with a nonstop barrage of wishes for “a healthy New Year”. Please be mindful of what you say to chronically ill/disabled folks in regards to health, at this time of year especially. <3
#chronic illness#disability#spoonie problems#spoonie life#new year's resolution#ehlers danlos syndrome#hypermobile eds#postural orthostatic tachycardia syndrome#mast cell activation syndrome#gastroparesis#gastrointestinal dysmotility#chronic migraine#etc. etc.#toxic positivity#please don't assign morality to health#people who aren't healthy are not morally inferior to healthy people OR morally culpable for their illness
232 notes
·
View notes
Text
Having a GI disorder
When all you want to do is eat yummy comforting gluten but your stomach says: I dare you to eat just one more bite of that and see what happens!

34 notes
·
View notes
Photo
#dysphagia#esophageal dysmotility#eosinophilic esophagitis#chronic illness#chronically ill#chronic illness meme#EoE#eosinophilic gastrointestinal disease#eosinophilic gastrointestinal disorders#eosinophilic disorders#eosinophilic disease#fibromyalgia#esophagus#esophageal motility disorders#My esophagus doesn't work#GERD#esophagitis#achalasia#neurological disorder
170 notes
·
View notes