#gender reassignment
Text



170 notes
·
View notes
Text
Vote for me for Rue Morgue Magazine’s Face of Horror to help me win funding for my gender reassignment surgery!!

I’m a drag performer running for the Face of Horror for Rue Morgue Magazine and there’s a $13,000 cash prize!! If y’all could vote and share this post/flyer, you would be doing me a huge favor, as i’m hoping to win the money to get surgery + a name change.
Free voting is every day via facebook, and if you’ve got a few bucks to spare, you can buy votes, and the proceeds go to the B+ Foundation to provide financial assistance to families, fund childhood cancer research, and bring awareness to the fight against childhood cancer.
VOTE HERE... IF YOU DARE!
47 notes
·
View notes
Text
“Despite a number of anatomical, hormonal, fertility, and obstetric considerations that require consideration, there is no overwhelming clinical argument against performing UTx [(uterine transplantation)] as part of GRS [(gender reassignment surgery)]. However, the increased radicality associated with the retrieval operation… potentially necessitates the use of deceased donors. Alternatively, F2M transgender men may offer an alternative donor pool should they accept the increased risk compared with standard hysterectomy.”
#trans#transgender#gender affirming healthcare#gender affirming care#trans childbirth#trans pregnancy#gender reassignment#gynecology#obstetrics#genderqueer#gender equality#science#surgery#bottom surgery#assistive reproductive technology#transhumanism
9 notes
·
View notes
Text
Go check out, follow, comment, share, whatever you wanna do to my TikTok. Explaining the reason for my first Phalloplasty repair surgery.
Appreciate it!!
#ftm#transgender#transsexual#lgbt#trans#top surgery#testosterone#phalloplasty#bottom surgery#trans man#tiktok#gender#gender marker#gender reassignment#healthcare#trans healthcare#lgbtq#advocacy#advocate
15 notes
·
View notes
Text
So are people doing gender reveals when they do their gender reassignments?
I really think y'all should....
#gender reveal#gender reassignment#gender#black tumblr#blktumblr#90s baby#blackgirlthoughts#black girl magic#quotes#self love#good vibe tribe#happiness#manifestingmindset
5 notes
·
View notes
Text
Vulvoplasty Research Notes
PLEASE NOTE THAT THE RESEARCH NOTES ARE COLLECTED FOR FUTURE OPPERATION AND UNDERSTANDING OF WHAT TO EXPECT BEFORE/DURING/AFTER VULVOPLASTY AT OHSU.
PLEASE NOTE THAT THIS INFORMATION CAN BE ANXIEY-INDUCING TO SOME.
-----------------------------------------------------------------------------------------------------------
WHAT IS VULVOPLASTY?
A vulvoplasty is a gender affirming genital reconstruction surgery that creates a neo-vulva from the existing genitalia. It fashions the external female genitalia but without a vaginal cavity. Depending on a few factors, this kind of surgery can have many different names, but in essence they are all the same:
Vulvoplasty
Vaginoplasty Without Cavity
Shallow / Minimal-Depth / Dimple / Limit-Depth Vaginoplasty
Cosmetic / Aesthetic Vaginoplasty
No-Depth / Zero Depth Vaginoplasty
Personally, I tend to call vulvoplasty - vaginoplasty, as my personal goal is to transition as much into a female without the addition of a uterus and ovaries (as the science hasn’t been developed to add these to the male body at this time). Calling it a vagina is logical in my mind as it affirms my gender as female. Also, most cis-females label their own reproductive organ as a ‘vagina’, including the clitoris and labia into the structure.
The outer characteristics of vulvoplasty are the same as those of vaginoplasty.
A clitoris and inner and outer labia are created, and the testicles and biological male sexual characteristics are removed and discarded.
The difference between a vulvoplasty and vaginoplasty is that a vulvoplasty provides a vaginal entrance that is up to 0 to 2 inches deep (depending on avaiable skin); whereas a vaginoplasty is usually 4-6 inches deep.
A benefit of vulvoplasty include:
1) Shorter Surgery Time (1.5 - 3 hours)
2) Shorter Inpatient Time (1 - 3 days)
3) Shorter Recovery Time (6-8 weeks)
4) No Need For Laser Hair Removal
5) No Dilation
6) Less Chance For Rectal Injury
Those seeking vulvoplasty should be aware that with no real depth, you will not be able to have penetrative sex.
-----------------------------------------------------------------------------------------------------------
HOW A VULVOPLASTY CREATES ‘TRUE’ FEMALE PARTS
This might be something that most people do not consider at first; but your new female parts will be actually true female parts (minus the uterus & ovaries). This is because all life on Earth in its earliest development begins as female.
This is why a vulvoplasty can be performed on a biological male; and why men have nipples on their chests and estrogen in their blood.
When a baby develops, the genitals are all the same; a urogenital slit bounded by periurethral folds and more laterally by labioscrotal swellings. It is only when the male chromosome activates, it causes the genitalia to develop differently. However, every masculine part to be traced to a feminine part. Dihydrotestosterone stimulates growth of the urogenital tubercle and induces fusion of the urethral folds and labial fold swelling during this critical period; it also induces differentiation of the prostate and inhibits growth of the vesicle vaginal septum, thereby preventing the development of the vagina
For example, the structure of the penis and clitoris are pretty much the same. It is an organ designed primarily to promote pleasure and reproduction. Both organs contain a nub or head that is packed with nerves.
The skin from the penis is used to form the area around the clitoris called the ‘hood’. Much of the shaft in a male is external, whereas a female contains the majority of her clitoris structure inside her body. Try to imagine anatomically that the inner labia are made of the penis’s ‘stretched’ skin, forming the foreskin at the end.
Scrotal skin contains a suture line down the center that once was the opening to the outer labia. The vaginal pouch is usually obliterated when the müllerian ducts are reabsorbed, although a vestigial blind vaginal pouch known as the prostatic utricle can sometimes be demonstrated. The prostate gland and the urethral glands of Cowper in the male are outgrowths of the urogenital sinus, in which male differentiation is mediated by dihydrotestosterone and requires the presence of androgen receptors
-----------------------------------------------------------------------------------------------------------
THE PREP / PRE-OP
Both vulvoplasty and vaginoplasty are major surgeries that are usually the last surgeries that MTF individuals have within 2-3 years on HRT.
Be aware of the following:
1) Persistent, well documented gender dysphoria diagnosis.
2) Capacity to make a fully informed decision and to consent for treatment.
3) 12 continuous months of hormone therapy
4) 12 continuous months of living in a gender role that is congruent with their gender identity.
5) Two letters from mental health therapist.
6) Nicotine Free for 10 weeks.
7) Documentation of recent A1C < 6.5% (diabetic patients only)
Pre-Surgery
At OHSU, it is scheduled to have a pre-surgery appointment one month before surgery. At this appointment, you will meet the Physician Assistant and be able to ask any questions before surgery.
You might be tested for nicotine and have blood work. A nicotine test will be performed on the day of surgery.
Stop taking estrogen 4 weeks before surgery. This is to reduce the risk of blood clots. Estrogen can be resumed a week after surgery.
Your surgical team might consist of the following people:
Primary Surgeon
Secondary Surgeon
A PA (physician assistant) Or RN
Medical assistants
Surgery scheduler
Resident physician’s
Physical therapists
Behavioral therapists
Social workers
Inpatient RN & CNA
-----------------------------------------------------------------------------------------------------------
SUPPLIES SUGGESTED
Roll fluff gauze: for surgical site absorption. Having 8-10 rolls be best.
Donut pillow or Hemorrihoid pillow for sitting: this will be important as it is almost a 4-hour drive. You can also use a u-shaped neck pillow or gel seat.
Maxi pads: to help with drainage. Larger is better as you don’t want it too tight.
Lots of toilet paper: You are likely to get messy.
Extra pairs of loose or mesh underwear: With dressing and maxi pads, your regular underwear may be too tight. You also may have some drainage that might ruin your underwear.
Stool softeners: Opioid pain medication and inactivity will likely cause some constipation. Miralax is recommended.
Ice pack: To reduce swelling, inflammation and pain.
Peri bottle: For the first few weeks after surgery, you should shower twice daily with gentle soap and water. Use your hand rather than a washcloth to clean the surgical site. Some patients find a peri bottle, designed for postpartem mothers, to be a gentle way to clean the area after surgery, in addition to showering twice daily.
Items to keep you entertained: computer, books, games, ect.
Snacks: to help ease emotional pain and use as a treat.
Items that make you comfortable: like a blanket, pillow, aromatherapy, eye pillow, ect.
Sore throat remedies: tea, chocolate, medicated spray. The trachea tube can leave behind irritation.
-----------------------------------------------------------------------------------------------------------
THE SURGERY
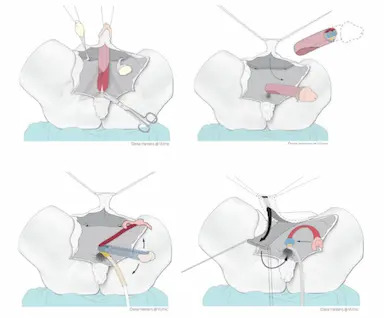
In vulvoplasty, the female genitals are created from the skin and underlying tissue of the penis. No vaginal cavity will be created. In most cases, the testicles are also removed in this operation. Be certain that you have thought about family planning before surgery.
Depending on the technique used, the operation will last anywhere from 2 to 5 hours. The operation will be performed by a plastic surgeon and/or urologist surgeon.
It starts with the insertion of a urinary catheter in the urethra.
The penile skin is removed from the shaft of the penis. The skin is shortened and sutured in order to make it look like a vagina (but without the vaginal cavity).
Then the testicles are removed, and the clitoris and inner labia are made from the glans and the foreskin. The urethra is exposed and shortened up to the new entrance.
The parts of the male genitals that will be incorporated into your new neo-vagina:
Clitoris is made out of the glans of the penis.
The outer labia are made from the scrotum.
The inner labia are made from the skin on the penis and/or urethra.
Urethra shortened and repositioned between the clitoris and vagina.
Introitus (opening of the vagina) is formed from the skin of the penis.
-----------------------------------------------------------------------------------------------------------
IMMEDIATE AFTER SURGERY & DAY 1
In accordance to OHSU Day 1 in Hospital:
After Surgery
Dr. Dy will speak with family after the surgery. Patient will be in post-anesthesia care unit for 2-3 hours for observation. It isn’t uncommon to feel nauseated (I tend to vomit after anesthesia), groggy, irritated, tearful, hungry and especially thirsty for a sore throat.
Patient will then be moved to Unit 4A (surgical unit). You will have a foley catheter in urethra, surgical packing, and drains with a collection bag. Your legs will have compression cuffs and an IV will be placed in the arm.
Medicine offered: nausea med, sore throat med, narcotic pain med, and stool softeners.
Diet: Begin with ice for sore throat. Water can be consumed in PACU. Snacks will be offered, like crackers or pudding, before the regular meal on day 2. Yogurt is advised.
Day 1
There is no strict bed rest, move as much as tolerated.
Rolling over in bed is comfortable if you do a ‘log-roll’. The bed should remain at 45 degrees or less.
Medicine Regiment: 650mg Tylenol every 6hrs. 15mg of Toradol IV every 8hrs. 5-15mg Oxycodone every 4hrs. Miralax.
No bathing, you can sponge bathe.
-----------------------------------------------------------------------------------------------------------
DAY 2
Medicine Regiment: 650mg Tylenol every 6hrs. 600mg Ibuprofen every 8hrs. 5-15mg Oxycodone every 4hrs. Miralax.
Encouraged to move around as much as possible. This will help with blood clots, maintaining your muscles, and digestion. Physical therapy suggests you do bed exercises every hour while awake.
Many patients will leave the hospital inpatient floor and go home on Day 2 with a catheter and external dressing in place. These dressings will be removed in the clinic on Day 3 or 4.
-----------------------------------------------------------------------------------------------------------
DAY 3
Medicine Regiment: 650mg Tylenol every 6hrs. 600mg Ibuprofen every 8hrs. 5-15mg Oxycodone every 4hrs. Miralax.
Today, the pressure dressing on the vulva is to be removed. Drains may be taken out today or tomorrow. Foley catheter removed. You need to try to pee without the catheter. 1-5 people find they cannot pee due to swelling, so a catheter will be placed back in. Your bladder will be scanned to see how much urine is left.
Take a shower today. User warm water, not hot! Clean ‘carefully’ all the folds and creases between your legs. Do not scrub! Do not use washcloth here!
Let the water flow over your vulva to wash away soap. Do not rub towel when drying...pat dry if possible.
Prepare for Discharge!
You and the caregivers should ask questions about anything not understood. Caregivers will pick up prescriptions before the patient leaves. Be certain to know the date of the next follow-up visit.
Transfer to the Rood Pavilion for extended stay.
-----------------------------------------------------------------------------------------------------------
RECOVERY AT ROOD
Not all hospitals offer off-campus housing, so your experience might differ. I live out of state, almost 200 miles away (4-hour commute) from OHSU; so, my care will be transferred there, giving me close access to the surgeon.
Medicine Regiment: 625mg Tylenol every 6hrs (end at first follow-up). 600mg Ibuprofen every 8hrs after taking Tylenol (end at first follow-up). 5mg Oxycodone every 6hrs PRN. 1 Lidocaine patch divided on inner tight and groin for 12hrs. Miralax. Resume your estrogen.
There is no diet restriction, however, drinking plenty of fluids is important with narcotics and flushing out the system. Miralax can be used for up to 1 month for constipation.
Try to keep your walking to 2,000 steps a day, for 4 weeks. Do not lift over 10 pounds for 4 weeks. Take stairs one at a time so you do not open sutures. Ice the mons (fatty tissue over public bone) for 20 minutes every 1-2 hours.
Be certain to rest and recover.
You will want to start using sanitary pads to collect blood from wounds.
Shower twice daily for 6 weeks after surgery. No pool or tub for 3 months! Stitches will dissolve on their own.
Appearance: Lots of swelling and bruising. To quote one trans individual, it will look gross, mutilated, or like a Frankenstein. The swelling can take many months to go down. In 6-12 months, you should start to see your vulva settling into form.
-----------------------------------------------------------------------------------------------------------
A CAREGIVER’S DUTY
A certain your caregiver knows their task and is comfortable with what is to be expected.
Surgery Day -- On site to talk to medical staff and to answer questions on the patient's behalf. Caregiver can stay in hospital in an extra bed.
Leaving Hospital -- Carry items, pick up medication, and drive.
At Home -- Help with putting you in comfortable position, give water, food, phone and supplies to patient. Observer and assist in showering and moving. This caregiver needs to be available 24 hours a day for about 14 days. This can be in person or on the phone.
The main goal is to have someone if there is an emergency, call doctors, and provide support and wound care.
Wound Care -- Help with cleaning, dressing, and observing surgical sites for 4 days.
-----------------------------------------------------------------------------------------------------------
FOLLOW-UPS
It might differ from different hospitals.
DAY 3-4 -- First Follow-Up: Remove dressing and catheter. Check surgical site and see how PT is doing with pain, urination, and BM.
4 WEEKS -- Second Follow-Up: 15-minute visit to check on health and answer questions.
3-6 MONTHS -- Third Follow-Up: 15-minute visit to check on health and answer questions. They will access the healing.
1 YEAR -- Fourth Follow-Up: 15-minute visit to check on health and answer questions. Last visit.
-----------------------------------------------------------------------------------------------------------
COMPLICATIONS DURING & AFTER SURGERY
This list is the most common complications seen in GRS patients; however, it does not mean that you will have these complications. It is just best to be aware during your recovery.
Vulvoplasty tends to have less complications as compared to vaginoplasty, but complications can happen depending on your current health.
These complications include:
Bleeding: Bleeding is to be expected after surgery. However, if it does not stop on its own in a few days, a second operation may be necessary to stem the bleeding.
Infection: Although the procedure is done in a clean and sterile way, there is always a chance of bacteria entering the wound. In the period after the operation, there is also a risk of infection. That is why it is so important to take good care of the wound at all times as infection can damage the structure.
Blood suffusion (haematoma): Some blood may accumulate in the surgical area, which may give the area a slightly blue or purple appearance, like a bruise. This will go away by itself after 2 to 4 weeks.
Fluid retention (oedema or seroma): Fluid may also accumulate in the surgical area. If this feels uncomfortable, the fluid can be removed by the physician in a follow-up.
Badly healing wound edges (wound dehiscence): After the operation, the wounds may not heal immediately, and may open up a little. Should this happen, it is recommended that you rinse the wound thoroughly with running water and, if necessary, contact your attending physician.
Hypergranulation: Hypergranulation is a very common problem. It is benign, but does involve a sizeable loss of fluids or blood. It may also have a certain odor and be painful, but it is easy to treat.
Loss of feeling/orgasm: As with any surgery, nerves may be damaged in the operation. Sometimes feeling will not be restored to what they once were. Orgasm can also change after the surgery.
Scarring: The growth in scarring tissue differs per person, skin type and surgical method. People and skin types all heal in their own way. Being overweight or a smoker means that wounds will heal less pretty than in healthy, non-smokers. Sometimes, a scar can be corrected (at least one year after the operation).
Urine spraying: One-third of people in published studies report this complication. Patients often find that it can take more than 6 months before the urine stream is more directed. If you still have bothersome urine spraying after 6 months, it can be often corrected with a second surgery.
Urinary urgency/frequency: This is a feeling of having to pee suddenly and often. This is common soon after surgery because of bladder irritation. This typically resolves on its own.
Urine leakage: This can happen without warning. This usually happens when pressure increases in the abdomen, such as with coughing, laughing or sneezing. This usually gets better on its own as you heal. Pelvic floor physical therapy can help.
-----------------------------------------------------------------------------------------------------------
END RESULTS
The final results will not be visible until after six months with the reduction of swelling. Most who have this operation tend to have an immediate negative experience after seeing their neo-vagina just after surgery.
Remember, this operation takes up to 6-12 months to complete the healing process.
The swelling and discoloration will slowly subside. The vagina will form naturally after the operation and will adapt to your body shape. For example, the color of the scrotum and the amount of fatty tissue will determine what the genitals will look like. The end result is different for everyone.
-----------------------------------------------------------------------------------------------------------
SCAR CARE
Massage is suggested to help loosen scar tissue. This can ease the discomfort and make them less visible over time. It is suggested you begin scar massage, advised by PT, 5-8 weeks after surgery. Daily exercise for 5-10 minutes.
Remember! A Massage Isn’t Meant To Hurt! Go gently to desensitized first.
-----------------------------------------------------------------------------------------------------------
CORRECTIONS
If you are not completely satisfied with the appearance or function of the genitals, you can discuss this with your plastic surgeon or urologist. They will be able to tell you whether an additional operation could lead to improvements.
Some surgeons report that nearly half of their patients will need a second surgery to fix complications or for aesthetics. Some surgeons also tell everyone that two surgeries are always necessary for a final result.
Corrections may, for example, be:
A reduction of the inner labia.
A correction of the clitoral hood.
A correction of the urethra.
In principle, corrections are not performed within 6 months of the first operation. It is advisable to wait at least one year as most issues are due to swelling.
The difficulty with cosmetic corrections is that getting them covered by insurance is difficult without a medical reason.
-----------------------------------------------------------------------------------------------------------
SEXUALITY
Your sex drive (libido) depends on the hormone testosterone. Most patients recovering from GRS report having a low sex drive for a while, as their testicles have been removed.
However, your sexual life depends not only on genital surgery, but also on many psychological and biological factors; so, do not be discouraged if you cannot reach climax at the time.
It can take upwards of 6-9 months for the nerves to heal after surgery. Nerves will not regrow for around 3-4 weeks after surgery. They will then begin to regrow at 1 millimeter a day or 1 inch a month. It seems that younger people will see the most regrowth. This packed regrowth might make sexuality more intense than before.
However, numbness is also a possibility.
It is natural to feel numb in some areas of the surgical site. With nerves regrowing, it will feel like pins and needles, tingling, and or a quick electric shock. Some find their clitoris desensitized, whereas others find it overly sensitive...it varies.
Becoming familiar with your genitals and learning to use them in a pleasurable way are significant challenges after genital surgery. It is important that you discover what gives you sexual pleasure and that you discuss this with your potential partner/partners
Some people have no desire for penetrative vaginal sex, in which case a vulvoplasty can be a good choice.
After vulvoplasty, you can still have orgasms through the stimulation of the clitoris — just like in the case of vaginoplasty. During a vulvoplasty, your surgeon will construct a clitoris from the glans and, if applicable, the foreskin of the penis.
-----------------------------------------------------------------------------------------------------------
RESUMING NORMALCY
Walking: 2000 steps (1 mile) a day for first 4 weeks | Afterwards, gradually increase. The more active you are, the more swelling there will be.
Showering: Twice daily for six weeks.
Bathing & Pools: No bathing or swimming for 3 months.
Lifting: Nothing over 10lbs for 4 weeks. | Afterwards, gradually increase.
Exertion: No workouts, running, or strenuous activities for 6 weeks. No biking for 3 months.
-----------------------------------------------------------------------------------------------------------
RESOURCES
https://genderaid.org/en/feminization/info/vulvoplasty
https://www.ncbi.nlm.nih.gov/books/NBK222286/
https://www.ohsu.edu/sites/default/files/2022-07/OHSU-vulvoplasty-booklet-2022.pdf
#gender transformation#gender#transgender#surgery#change#transformation#trans#tg#gender reassignment#gender reassignment surgery#MtF trans#male to female
17 notes
·
View notes
Text
the fact that plastic surgery has no necessity for a doctors note or therapist recommendation yet has more rates of regretting it than gender affirming care for transgender people. Crazy.
12 notes
·
View notes
Text
Not being homophobic and protecting children's well being is simply much more important than not being called transphobic or terf. Lazy attempts to insult someone won't hurt the way homophobia and children gender-reassignment treatments do.
#children's health#children's well-being#hrt#trans hrt#children hrt#gender reassignment#children#homophobia#lgb#transgender#trans#homosexuals#terf
2 notes
·
View notes
Text

Amazing red head transgender woman! She's a gift to all mankind! I love red heads!
#trans#transgender#queer#transfem#trans pride#cisgender#lgbtqia#gender reassignment#gender envy#fluid gender#genderfluid#genderqueer#genderlyblender#gender nonconforming#gender euphoria#gender stuff#neopronouns#pronouns#gender identity#genderbend#genderqueerpositivity#queer culture#lgbtlove#trans community#queer community#queer fashion#queer girl#queer nsft#beta boi#beta sissy
407 notes
·
View notes
Text
Watch "MYRA BRECKINRIDGE (1970) Theatrical Trailer - Mae West, John Huston, Raquel Welch" on YouTube
youtube
"One of the worst films ever made", which is a pity, because Gore Vidal's book was one of the best I've ever read... Ah well, rest in peace Ms. Welch.
9 notes
·
View notes
Text
you know i had to do it to 'em (chop off my tits)
#top surgery#gender reassignment#gender reassignment surgery#transsexuals#trans masc#transgender#mine
9 notes
·
View notes
Text
Russia banned gender reassignment.
I had thoughts about this, but now I don't have the rights to take at least some steps towards this.
Finita la comedia
2 notes
·
View notes
Text
anti-lgbtq+ laws in russia
recently in russia, putin has signed off on a law to basically stop the distribution of LGBTQ+ “propaganda” to “protect” children. gender reassignment has also been outlawed recently by the Russian Duma. all of this goes to show how homophobic russia is, & how theyre trying to show that only heterosexual relationships are “normal”. how sad.
#lgbtq#lgbtqplus#gender reassignment#russia#passion project#explore#discover#homosexuality#high school#history
2 notes
·
View notes
Text

I lived, bitch
2 notes
·
View notes
Text
A funny thought about the anti-abortion and anti-trans people.
Anti-trans people say that your god-given gender was the one originally assigned to you.
Anti-abortion people believe that life begins at conception.
Referring to the fact that every fetus has female parts up until 14 weeks, doesn’t that mean every biological male is actually originally female and transgender?
Maybe anti-abortion, anti-trans people should begin to refer to their fetus as a “she” until it reaches 14 weeks, and if it becomes male in the uterus, adjust its pronouns accordingly. But if anti-trans people say that doesn’t count, then they’re admitting that life doesn’t begin at conception. If they admit that it does count, then they’re agreeing with the fact that gender can scientifically change, whether in uterus, or by medical assistance.
Furthermore, let us revisit the case of intersex people. Some fetuses don’t fully transition from female to male sex by the time they are born. They can carry both biologically male and female genitals, chromosomes, and various other combined features. In many cases, people who are born intersex are forced to take on a gender they weren’t assigned at birth, and nonconsensual gender reassignment surgery and treatment is often performed on children in order to be brought to more “acceptable” characteristics for a specific sex.
A common ideology against transgender people is that someone can’t identify as something they weren’t assigned with at birth, yet the same individuals who subscribe to this ideology force intersex children into gender-reassignment surgeries, or otherwise force these children into a social gender binary that doesn’t apply to their anatomy. The idea that people who force surgeries on intersex people, yet decline gender affirming surgeries for people who want it sounds… a little contradictory, don’t you think?
Regardless, if we get caught up in the science of it all, we perpetuate the contradictory ideology that harms gender theory as a whole. Gender is a social construct. Every person is unique. Stop and think for a second before forcing your ideology onto other peoples’ identity.
I know that some people are “set in their own ways” and I understand where they’re at. I was raised to be transphobic and queerphobic. I grew up and came to my own conclusion. Saying you were raised to think a certain way is no excuse for suppressing the rights of trans and intersex people.
#transgender#trans#gender affirming#intersex#transgender science#queer science#trans people#intersex rights#trans rights#queer rights#gender reassignment#snek rambles#non-binary#agender#gender theory
4 notes
·
View notes