#gyn davis
Photo

Triangle of Sadness, Ruben Östlund (2022)
#Ruben Östlund#Harris Dickinson#Charlbi Dean#Vicki Berlin#Dolly De Leon#Alicia Eriksson#Woody Harrelson#Zlatko Buric#Sunnyi Melles#Carolina Gynning#Iris Berben#Amanda Walker#Oliver Ford Davies#Henrik Dorsin#Arvin Kananian#Jean Christophe Folly#Fredrik Wenzel#Mikel Cee Karlsson#2022
11 notes
·
View notes
Photo

Triangle of Sadness
#JASIPOF#Triangle of Sadness#Ruben Östlund#Harris Dickinson#Charlbi Dean#Dolly de Leon#Zlatko Buric#Iris Berben#Vicki Berlin#Henrik Dorsin#Jean-Christophe Folly#Amanda Walker#Oliver Ford Davies#Sunnyi Melles#Woody Harrelson#Alicia Eriksson#Carolina Gynning#Arvin Kananian
1 note
·
View note
Text
Triangle of Sadness (2022) Review
Triangle of Sadness (2022) Review
Palme d’Or winner in 2022. Social hierarchy is turned upside down when celebrity model couple Carl and Yaya are invited on a luxury cruise for the super rich.
⭐️
(more…)

View On WordPress
#2022#Alicia Eriksson#Amanda Walker#Arvin Kananian#Carolina Gynning#Charlbi Dean#Comedy#Dolly de Leon#Drama#Harris Dickinson#Henrik Dorsin#Iris Berben#Jiannis Moustos#Oliver Ford Davies#Palme d’Or#Ralph Schicha#Review#Ruben Ostlund#Sunnyi Melles#Thobias Thorwid#Timoleon Gketsos#Triangle of Sadness#Vicki Berlin#Woody Harrelson#Zlatko Buric
0 notes
Text
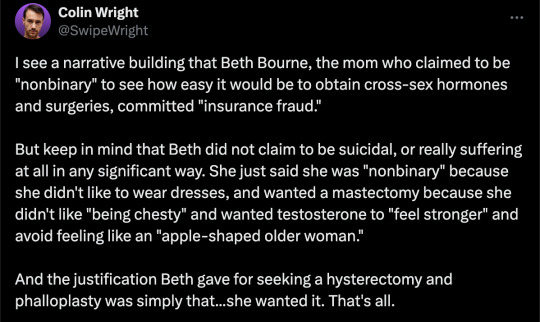
By: Beth Bourne
Published: Feb 27, 2024
Kaiser gender specialists were eager to approve hormones and surgeries, which would all be covered by insurance as “medically necessary.”
On September 6, 2022, I received mail from my Kaiser Permanente Davis Ob-Gyn reminding me of a routine cervical screening. The language of the reminder stood out to me: “Recommended for people with a cervix ages 21 to 65.” When I asked my Ob-Gyn about this strange wording, she told me the wording was chosen to be “inclusive” of their “transgender” and “gender fluid” patients.
Based on this response, several thoughts occurred to me. Could I expose the medical scandal of “gender-affirming care” by saying and doing everything my daughter and other trans-identifying kids are taught to do? Would there be the type of medical safeguarding and differential diagnosis we would expect in other fields of medicine, or would I simply be allowed to self-diagnose and be offered the tools (i.e. hormones and surgeries) to choose my own gender adventure and become my true authentic self?
If I could demonstrate that anyone suffering from delusions of their sex, self-hatred, or identity issues could qualify for and easily obtain body-altering hormones and surgeries, all covered by insurance as “medically necessary” and potentially “life-saving” care, then maybe people would finally wake up. I certainly had.
I was prepared for failure. I wasn’t prepared for how easy success would be.
* * *
I am a 53-year-old mom from Davis, CA. My daughter began identifying as a transgender boy (social transition) and using he/him pronouns at school during 8th grade. Like several of her peers who also identified as trans at her school, my daughter was a gifted student and intellectually mature but socially immature. This shift coincided with her school’s sudden commitment to, and celebration of, a now widespread set of radical beliefs about the biology of sex and gender identity.
She “came out” as trans to her father (my ex-husband) and me through a standard coming-out letter, expressing her wish to start puberty blockers. She said she knew they were safe, citing information she had read from Planned Parenthood and the World Professional Association for Transgender Health (WPATH). To say I was shocked would be an understatement. I was also confused because this announcement was sudden and unexpected. While others quickly accepted and affirmed my daughter’s new identity, I was apprehensive and felt the need to learn more about what was going on.
Events began escalating quickly.
During a routine doctor’s visit scheduled for dizziness my daughter said that she was experiencing, the Kaiser pediatrician overheard her father using “he/him” pronouns for our daughter. The pediatrician seemed thrilled, quickly asking my daughter about her “preferred pronouns” and updating her medical records to denote that my daughter was now, in fact, my son. The pediatrician then recommended we consult the Kaiser Permanente Oakland Proud pediatric gender clinic, where she could get further information and (gender affirming) “treatment.” Now I was the one feeling dizzy.
As I began educating myself on this issue, I discovered that this phenomenon—minors, most often teen girls, suddenly adopting trans identities—was becoming increasingly widespread. It even had a name: rapid onset gender dysphoria, or ROGD. Thankfully, after learning about the potential side-effects of blockers and hormones, my ex-husband and I managed to agree not to consent to any medical interventions for our daughter until she turned 18 and would then be able to make such decisions as an adult.
Over the past five years, my daughter’s identity has slowly evolved in ways that I see as positive. Our bond, however, has become strained, particularly since I began publicly voicing my concerns about what many term as “gender ideology.” Following my daughter’s 17th birthday family celebration, she sent me an email that evening stating she would be cutting off contact with me.
While this estrangement brought me sorrow, with my daughter living full-time with her father, it also gave me the space to be an advocate/activist in pushing back on gender identity ideology in the schools and the medical industry.
I decided to go undercover as a nonbinary patient to show my daughter what danger she might be putting herself in—by people who purport to have her health as their interest, but whose main interest is in medically “affirming” (i.e., transitioning) whoever walks through their door. I am at heart a mother protecting her child.
* * *
My daughter’s sudden decision to become a boy was heavily on my mind in early September of 2022, when mail from my Kaiser Permanente Davis Ob-Gyn reminded me of a routine cervical screening with “Recommended for people with a cervix ages 21 to 65.” I was told that the wording was chosen to be “inclusive” of transgender and “gender fluid” patients.
Throughout the whole 231-day process of my feigned gender transition, the Kaiser gender specialists were eager to serve me and give me what I wanted, which would all be covered by insurance as “medically necessary.” My emails were returned quickly, my appointments scheduled efficiently, and I never fell through the cracks. I was helped along every step of the way.
Despite gender activists and clinicians constantly claiming that obtaining hormones and surgeries is a long and complex process with plenty of safety checks in place, I was in full control at every checkpoint. I was able to self-diagnose, determine how strong a dose of testosterone I received and which surgeries I wanted to pursue, no matter how extreme and no matter how many glaring red flags I purposefully dropped. The medical workers I met repeatedly reminded me that they were not there to act as “gatekeepers.”
I was able to instantly change my medical records to reflect my new gender identity and pronouns. Despite never being diagnosed with gender dysphoria, I was able to obtain a prescription for testosterone and approval for a “gender-affirming” double mastectomy from my doctor. It took only three more months (90 days) to be approved for surgery to remove my uterus and have a fake penis constructed from the skin of my thigh or forearm. Therapy was never recommended.
Critics might dismiss my story as insignificant on the grounds that I am a 53-year-old woman with ample life experience who should be free to alter her body. However, this argument for adult bodily autonomy is a standard we apply to purely cosmetic procedures like breast implants, liposuction, and facelifts, not “medically necessary” and “lifesaving” treatments covered by health insurance. Or interventions that compromise health and introduce illness into an otherwise healthy body. And especially not for children.
My story, which I outline in much more detail below, should convince any half-rational person that gender medicine is not operating like any other field of medicine. Based on a radical concept of “gender identity,” this medical anomaly preys upon the body-image insecurities common among pubescent minors to bill health insurance companies for permanent cosmetic procedures that often leave their patients with permanently altered bodies, damaged endocrine systems, sexual dysfunction, and infertility.
* * *
Detailed Timeline of Events
On October 6, 2022, I responded to my Ob-Gyn’s email to tell her that, after some thought, I’d decided that maybe the label “cis woman” didn’t truly reflect who I was. After all, I did have some tomboyish tendencies. I told her I would like my records to be changed to reflect my newly realized “nonbinary” identity, and that my new pronouns were they/them. I also voiced my desire to be put in touch with an endocrinologist to discuss starting testosterone treatment.
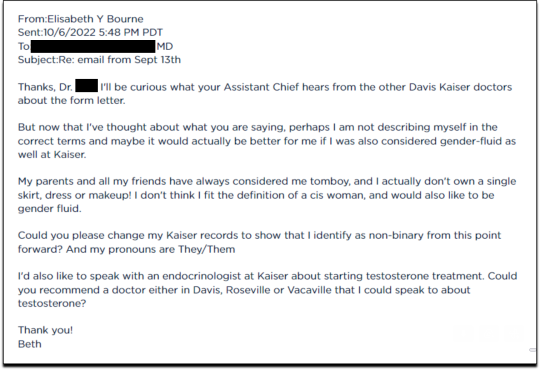
Fifteen minutes later I received an email from another Kaiser doctor informing me that my medical records had been changed, and that once my primary doctor returned to the office, I’d be able to speak with her about hormone therapy.
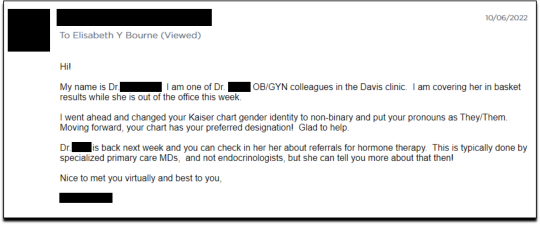
I responded the following day (October 7, 2022), thanking her for changing my records, and asking if she could connect me with someone who could help me make an appointment for “top surgery” (i.e., a cosmetic double mastectomy) because my chest binder was rather “uncomfortable after long days and playing tennis.”
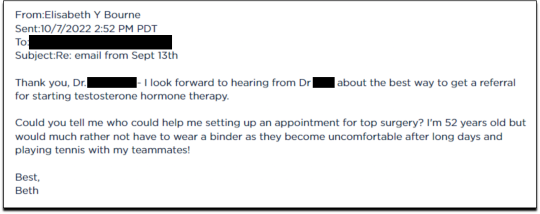
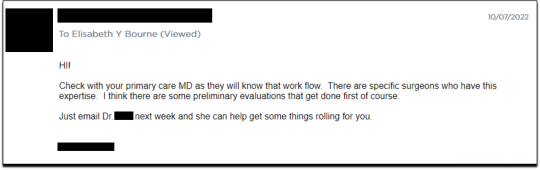
She told me to contact my primary care MD to “get things rolling,” and that there were likely to be “preliminary evaluations.”
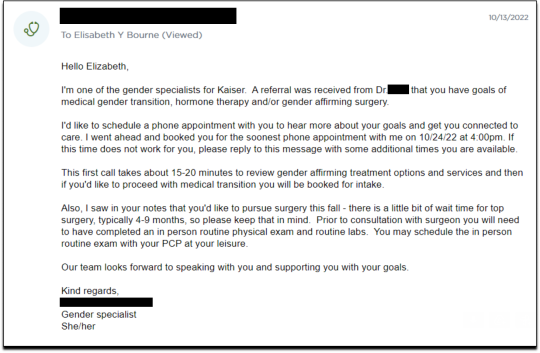
Six days after contacting my primary care MD for a referral, I received an email from one of Kaiser’s gender specialists asking me to schedule a phone appointment so she could better understand my goals for surgery, so that I could get “connected to care.” This call to review my “gender affirming treatment options and services” would take 15-20 minutes, after which I would be “booked for intake,” allowing me to proceed with medical transition.
This wasn’t an evaluation of whether surgical transition was appropriate, it was simply a meeting for me to tell them what I wanted so that they could provide it.
On October 18, I had my one and only in-person appointment in preparation for top surgery. I met in Davis with my primary care physician, Dr. Hong-wen Xue. The assessment was a 10-minute routine physical exam that included blood tests. Everything came back normal. Notably, there was not a single question about why I wanted top surgery or cross-sex hormones. Nor was there any discussion of the risks involved with these medical treatments.
The following week, on October 24, I had a phone appointment with Rachaell Wood, MFT, a gender specialist with Kaiser Sacramento. The call lasted 15 minutes and consisted of standard questions about potential drug use, domestic violence, guns in the house, and whether I experienced any suicidal thoughts. There were no questions from the gender specialist about my reasons for requesting a mastectomy or cross-sex hormones, or why I suddenly, at 52, decided I was “nonbinary.”
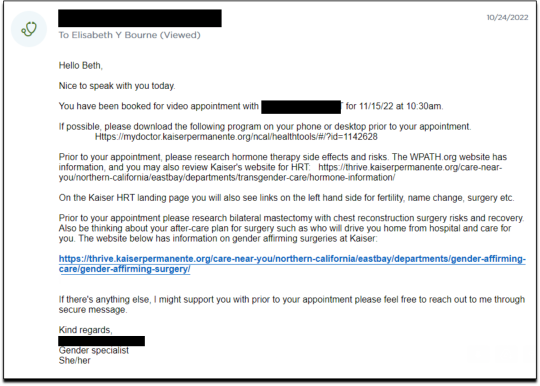
After the call, Kaiser emailed me instructions about how to prepare for my pre-surgery intake video appointment to evaluate my mental health, scheduled to take place on November 15. The email stated that prior to my appointment, I should research hormone risks on the WPATH website, and to “research bilateral mastectomy and chest reconstruction surgery risks and recovery” on Kaiser’s website.
I decided to request a “gender-affirming” double mastectomy and phalloplasty. Kaiser sent me a sample timeline for gender transition surgery preparation (see below) that you can use as a reference for the process. I also asked for a prescription for cross-sex hormones (testosterone) as needed and recommended by Kaiser.
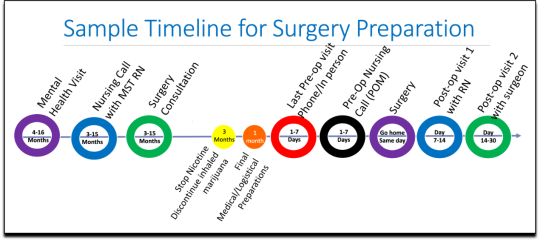
[ Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
Pre-Surgery Mental Health Video Appointment, Part I
This “Mental Health Visit” assessment was conducted over Zoom. The Kaiser gender specialist started with questions addressing my marital status, race, gender identity, and other demographics. She asked whether I was “thinking of any other surgeries, treatments in the future.” The list she read included “gender-affirming” hysterectomies, bottom surgeries such as metoidioplasty and phalloplasty, vocal coaching, support groups, and body contouring. “Anything else you might be interested in doing?” she asked. I said that I’d perhaps be interested in body contouring. I was also assured that all the procedures would be covered by insurance because they were considered “medically necessary.”
I dropped in several red flags regarding my mental health to see the reaction, but all were ignored. For instance, I revealed that I had PTSD. When the therapist asked me about whether I had experienced any “childhood trauma,” I explained that I grew up in Mexico City and had been groped several times and had also witnessed men masturbating in public and had been grabbed by men in subways and buses. “I was a young girl, so [I had] lots of experiences of sexual harassments, sexual assault, just the kind of stuff that happens when you are a girl growing up in a big city.” “So, you know,” I finished, “just the general feeling that you are unsafe, you know, in a female body.”
The therapist did not respond to my disclosure that trauma could be the cause of my dysphoria. Instead of viewing this trauma as potentially driving my desire to escape my female body through hormones and surgery, she asked whether there is anything “important that the surgery team should be aware of” regarding my “history of trauma,” such as whether I’d be comfortable with the surgeon examining and marking my chest prior to surgery.
When asked about whether I had had any “psychotic symptoms,” I told her that while I had had no such symptoms, my mother had a delusional nervous breakdown in her 50s because she had body dysmorphia and became convinced she had a growth on her neck that needed to be removed. I told her that my mother was then admitted to an inpatient hospital for severe depression. I asked her whether she ever sees patients with body dysmorphia and whether I could have potentially inherited that from my mother. She told me that psychosis was hereditary, but that it was “highly unlikely” that there was any connection between body dysmorphia and gender dysphoria.
I enthusiastically waved more mental health red flags, waiting to see if she would pick up on any of them.
I’m just wondering if my feelings, or perseverating, or feeling like these breasts make me really unhappy and I just don’t want them anymore!...I’m just not sure if that’s a similar feeling to body dysmorphia? How do you decide which one is gender dysphoria and general body dysmorphia, and just not liking something about your body? Feeling uncomfortable with your body?
And I did have an eating disorder all through college. I was a distance runner in college so I had bulimia and anorexia, you know. So I don’t know if that’s related to gender dysphoria?
The therapist replied, “I completely appreciate your concerns, but I am going to ask you questions about your chest, about your expectations. And then I’ll be able to give you an assessment.” She also said the main difference between my mom’s situation and mine was that my mom didn’t really have a growth on her neck, whereas it’s “confirmed” that I actually have “chest tissue.” Furthermore, she said that while “historically there has been all this pressure on patients to be like ‘Are you really, really sure you want hormones? Are you 100% sure?’ We are a little more relaxed.” She continued, “As long as you are aware of the risks and the side-effects, you can put your toe in the water. You can stop ‘T’ [testosterone], you can go back and do it again later! You can stop it! You can stop it! You know what I mean?”
Because we ran out of time, I scheduled a follow-up phone meeting on December 27, 2022 with a different gender specialist to complete my mental health assessment for top surgery.
Pre-Surgery Mental Health Video Appointment, Part II
During this meeting, Guneet Kaur, LCSW, another Kaiser gender specialist (she/her/they/them pronouns) told me that she regretted the “gatekeeping vibe” of the meeting but assured me that since I have been “doing the work,” her questions are essentially just a form of “emotional support” before talking with the medical providers.
She asked me about what I’d been “looking into as far as hormones.” I told her that I’d be interested in taking small doses of testosterone to counterbalance my female feelings to achieve “a feeling that’s kind of neutral.”
When she asked me about me “not feeling like I match on the outside what I feel on the inside,” I dropped more red flags, mentioning my aversion to wearing dresses and skirts.
I don’t own a single dress or a skirt and haven't in 20 years. I think for me it’s been just dressing the way that’s comfortable for me, which is just wearing, jeans and sweatshirts and I have a lot of flannel shirts and, and I wear boots all the time instead of other kinds of shoes. So I think it’s been nice being able to dress, especially because I work from home now most of the time that just a feeling of clothing being one of the ways that I can feel more non-binary in my everyday life.
She responded, “Like having control over what you wear and yeah. Kind of that feeling of just, yeah, this is who I am today. That’s awesome. Yeah.”
She then asked me to describe my dysphoria, and I told her that I didn’t like the “feeling of the female form and being chesty,” and that because I am going through menopause, I wanted to start taking testosterone to avoid “that feeling of being like this apple-shaped older woman.” “Good. Okay, great,” she responded, reminding me that only “top surgery,” not testosterone, would be able to solve my chest dysphoria. (Perhaps it was because all these meetings were online, they didn’t notice I’m actually fit and relatively slender at 5’-5” and 130 pounds, and not apple-shaped at all.)
She told me that we had to get through a few more questions related to my medical history before “we can move on to the fun stuff, which is testosterone and top surgery.”
The “fun stuff” consisted of a discussion about the physical and mood changes I could expect, and her asking me about the dose of testosterone I wanted to take and the kind of “top surgery” technique I’d prefer to achieve my “chest goals.” She told me that all or most of my consultations for surgeries and hormones would be virtual.
The gender specialist told me after the appointment, she would submit my referral to the Multi-Specialty Transitions Clinic (MST) team that oversees “gender expansive care.” They would follow up to schedule a “nursing call” with me to review my medical history, after which they’d schedule my appointment with a surgeon for a consultation. Her instructions for this consultation were to “tell them what you’re wanting for surgery and then they share with you their game plan.”
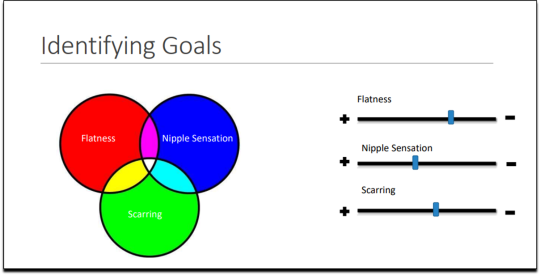
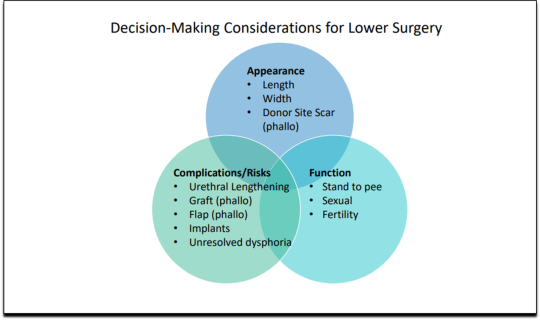
[ Decision-making slide to help me identify my goals for top surgery–flat chest, nipple sensation, or minimal scarring. Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
She told me that Kaiser has a team of plastic surgeons who “only work with trans and nonbinary patients because there’s just so much need for them.” She asked about my priorities for chest surgery, such as whether I value flatness over nipple sensation. I learned about double incision top surgery with nipple grafts, as well as “keyhole,” “donut,” “buttonhole,” and “Inverted-T” top surgeries.
By the end of the hour-long appointment, I had my surgery referral and was ready for my “nursing call” appointment.
Nursing call with Nurse Coordinator from the Transgender Surgery and Gender Pathways Clinic at Kaiser San Francisco
On January 19, 2023, I had my nursing call with the Nurse Coordinator. He first said that “the purpose of this call is just for us to go through your chart together and make sure everything’s as accurate as possible.” Once that was done, my referral would be sent to the surgeon for a consultation.
He asked me about potential allergies and recreational drug use, and verified that I was up to date on mammograms, pap smears, and colon cancer screenings, as well as vaccines for flu and COVID. I verified my surgical history as well as my current medications and dietary supplements.
He told me about a “top surgery class” available for patients where one of the Kaiser surgeons “presents and talks about surgical techniques and options within top surgery,” and includes a panel of patients who have had top surgery. I signed up for the February 8th class.
Within 10 minutes he told me that he had “sent a referral to the plastic surgery department at Kaiser Sacramento,” and that I should be hearing from them in the next week or two to schedule a consultation.
Appointment for Testosterone
On January 27, I had a 13-minute online appointment with a primary care doctor at Kaiser Davis to discuss testosterone. The doctor verified my name and preferred pronouns, and then directly asked: “So, what would you like to do? What kind of physical things are you looking for?”
I told her I wanted facial hair, a more muscular and less “curvy” physique, and to feel stronger and androgynous. She asked me when I wanted to start, and I told her in the next few months. She asked me if I was menopausal, whether I had ovaries and a uterus, although that information should have been on my chart.
The doctor said she wanted me to come in to get some labs so she could check my current estrogen, testosterone, and hemoglobin levels before starting hormones. Then “we'll set the ball in motion and you'll be going. We’ll see you full steam ahead in the direction you wanna go.”
That was it. I made an appointment and had my lab tests done on February 12. My labs came back on February 14, and the following day, after paying a $5 copay at the Kaiser pharmacy, I picked up my testosterone pump. That was easy!
Top Surgery Consultation
On the same day I received my labs, I had a Zoom surgery consultation with Karly Autumn-Kaplan, MD, Kaiser Sacramento plastic surgeon. This consultation was all about discussing my “goals” for surgery, not about whether surgery was needed or appropriate.
I told the surgeon that I wanted a “flatter, more androgynous appearance.” She asked me some questions to get a better idea of what that meant for me. She said that some patients want a “male chest,” but that others “want to look like nothing, like just straight up and down, sometimes not even nipples.” Others still wanted their chest to appear slightly feminine and only “slightly rounded.” I told her that I’d like my chest to have a “male appearance.”
“What are your thoughts about keeping your nipples?” she asked. “Are you interested in having nipples or would you like them removed?” I told her that I’d like to keep my nipples, but to make them “smaller in size.” She asked me if I’d like them moved to “the edge of the peck muscle” to achieve “a more male appearance.” I said yes.
I was asked to show my bare chest from the front and side, which I did. Then she asked me how important it was for me to keep my nipple sensation. I replied that it was important unless it would make recovery more difficult or there were other associated risks. She highlighted the problem with the free nipple graft, saying that removing the nipple to relocate it means “you're not gonna have sensation in that nipple and areola anymore.” However, some nipple sensation could be preserved by keeping it attached to “a little stalk of tissue” with “real nerves going to it,” but that would require leaving more tissue behind. I told her I’d go for the free nipple graft to achieve a flatter appearance. It was also suggested I could skip nipple reconstruction entirely and just get nipples “tattooed” directly onto my chest.
She told me I was “a good candidate for surgery,” and put me on the surgery wait list. She said that the wait time was between three and five months, but a cancellation could move me up to a sooner date. Also, if I wanted surgery as soon as possible, I could tell the surgery scheduler that I’d be willing to have any of the other three surgeons perform my mastectomy. Outpatient top surgery would cost me a copay of $100.
They contacted twice, in February and March, notifying me of cancellations. If I had accepted and shown up on those dates, they would have removed my breasts. This would have been less than five months from the time I first contacted Kaiser to inform them of my new “nonbinary” gender identity.
How Far Can I Go?
I decided to see how easy it would be for me to get approved for a phalloplasty. Known euphemistically as “bottom surgery,” phalloplasty is the surgical creation of an artificial penis, generally using tissue from the thigh or arm.
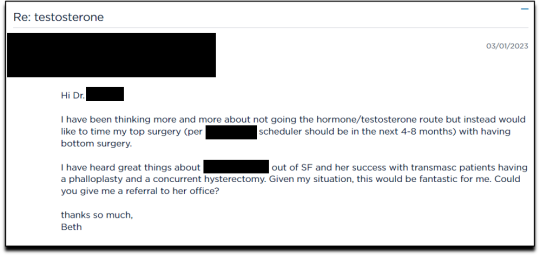
I sent an email on March 1, 2023, requesting to have a phalloplasty and concurrent hysterectomy scheduled alongside my mastectomy.
Two weeks later, on March 16th, I had a 16-minute phone call with a gender specialist to discuss my goals for bottom surgery and obtain my referral.
During the call, I explained to the specialist that I wasn’t sure about taking testosterone anymore because I was already quite athletic and muscular, and that taking testosterone didn’t make much sense to me. Instead, I wanted bottom surgery so that I wouldn’t feel like my “top” didn’t match my “bottom.” I told her:
But what I really wanted was to have bottom surgery. So this way when I have my top surgery, which sounds like it could be very soon, that I’ll be aligned, that I won’t have this sense of dysphoria with one part of my body and the other part feeling like it matched who I am. So yeah. So I just did a little bit more research into that. And I looked at the resources on the Kaiser page for the MST clinic and I think I know what I want, which is the hysterectomy and then at the same time or soon after to be able to have a phalloplasty.
I told her that I wanted to schedule the top and bottom surgery concurrently so that I wouldn’t have to take more time off work and it would save me trips to San Francisco or Oakland, or wherever I had to go for surgery.
None of this gave the gender specialist pause. After a brief conversation about some online resources to look over, she told me that she would “submit the referral now and we’ll get this ball rolling.”
Bottom surgery would cost me a copay of $200, which included a couple of days in the hospital for recovery.
Phalloplasty Surgical Consultation with Nurse Coordinator
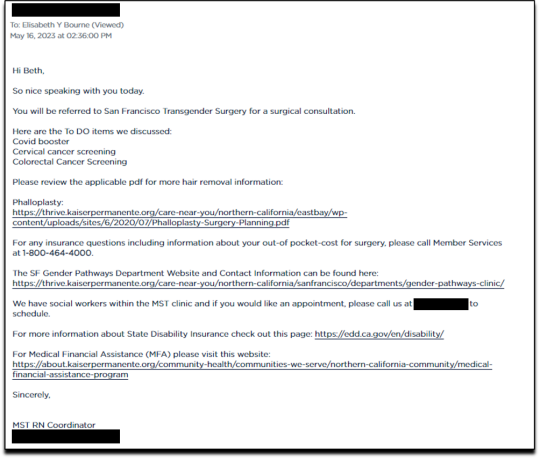
On May 16, 2023, I had a short surgical consultation with a nurse coordinator to go through my medical history. This was similar to the consultation for top surgery but included information about hair removal procedures for the skin on my “donor site” that would be fashioned into a makeshift penis. They also went over the procedures for determining which donor site—forearm or thigh—was more viable.
After only 15 minutes, she submitted my referral to the surgeon for another surgical consultation.
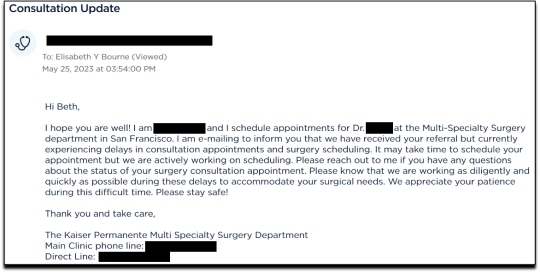
On May 25 I received an email from my phalloplasty surgeon’s scheduler, informing me that they have received my referral and are actively working on scheduling, but that they are experiencing delays.
I ended my investigation here once I had the referral for the top and bottom surgery. I never used my testosterone pump.
Final Thoughts
In fewer than 300 days, based on a set of superficial and shifting thoughts about my gender and my “embodiment goals” triggered by the mere mention of “gender” in a form letter from my primary care physician, and driven by what could only be described as minor discomforts, Kaiser Permanente’s esteemed “multi-disciplinary team” of “gender specialists” was willing, with enthusiasm—while ignoring mental health concerns, history of sexual trauma, and rapidly escalating surgical requests—to prescribe life-altering medications and perform surgeries to remove my breasts, uterus, and vagina, close my vaginal opening, and attempt a complex surgery with high failure and complication rates to create a functionless representation of a penis that destroys the integrity of my arm or thigh in the process.
This describes the supposedly meticulous, lengthy, and safety-focused process that a Kaiser patient must undergo to embark on a journey to medically alter their body. No clinician questioned my motivations. No one showed concern that I might be addressing a mental health issue through radical and irreversible interventions that wouldn’t address my amorphous problems. There were no discussions about how these treatments would impact my long-term health, romantic relationships, family, or sex life. I charted the course. The clinicians followed my lead without question. The guiding issue was what I wanted to look like.
No other medical field operates with this level of carelessness and disregard for patient health and welfare. No other medical field addresses issues of self-perception with surgery and labels it “medically necessary.” No other medical field is this disconnected from the reality of the patients it serves.
Kaiser has traded medicine for ideology. It’s far beyond time we stop the ruse of considering “gender-affirming” interventions as anything approaching medical care.
This isn’t the first time Kaiser Permanente has been in the news for completely disregarding medical safeguards in the name of “gender-affirming care.” As girls, Chloe Cole and Layla Jane became convinced that they were born in the wrong body and were actually boys on the inside. Doctors at Kaiser ignored their underlying conditions and instead prescribed testosterone and removed their breasts. Both Cole and Jane have since detransitioned and are currently suing Kaiser.
The fact that children and vulnerable adults are being exploited in this massive ideological experiment is not just tragic; it’s deeply disturbing, especially considering it has evolved into a billion-dollar industry.
I hope that by sharing my story, I can bring more focused scrutiny to the medical scandal unfolding not just at Kaiser but also at medical centers and hospitals across the Western world. These institutions have completely abandoned medical safeguards for patients who claim to be confused about their “gender,” and I aim to awaken more parents and assist them in protecting their children.
--
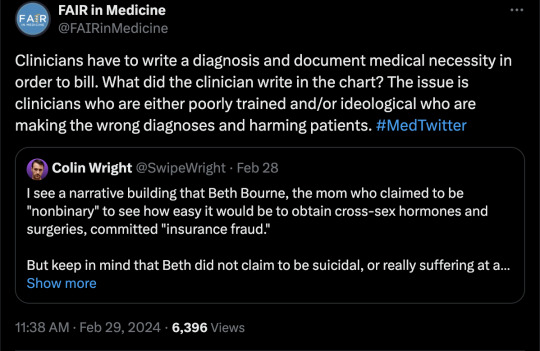
==
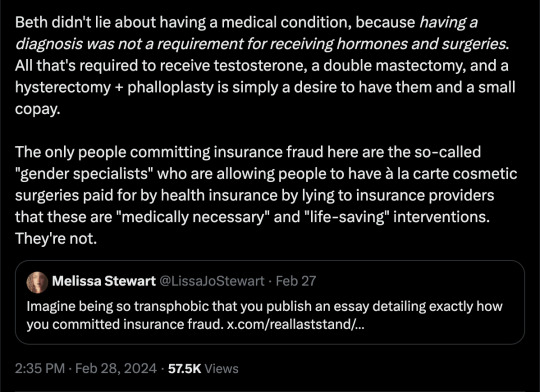
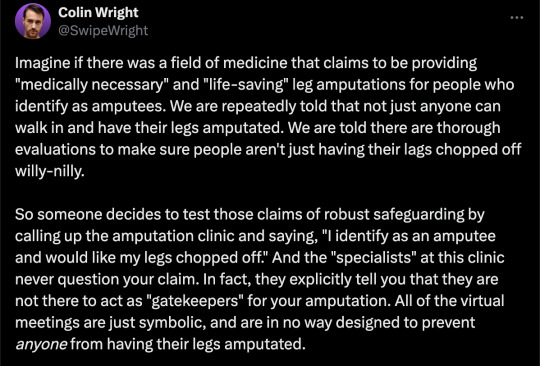
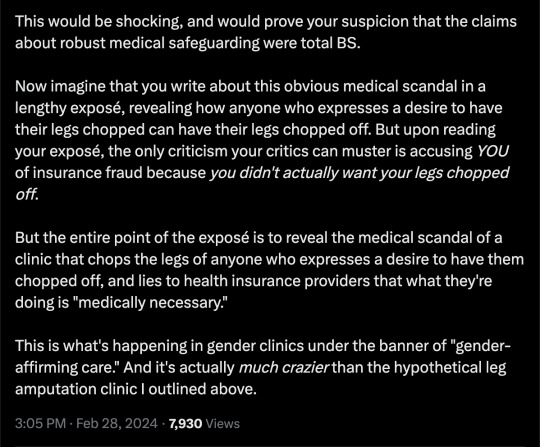
This is completely insane.
Apologists online are running around saying, but she didn't mean it, she was lying, she was pretending...
It doesn't matter.
Any kind of security, penetration or integrity test is insincere too. When security researchers compromise Microsoft's operating system or Google's browser or whatever, "but they didn't mean it" is not a defence to a discovered security flaw. It doesn't matter that the security researchers didn't plan to steal data or money or identities. The flaw in the system is there regardless.
It doesn't matter that it was insincere. Because the workers didn't know that. They never checked, never asked questions, never tested. They had been taught and instructed to never ask any questions. They did what they were supposed to. And the system failed spectacularly. Because that's what "gender affirming care" means.
Additionally, the claim that Beth Bourne committed fraud is an outright lie. A patient cannot bill. They do not have the authority. The medical clinic is the only one that can bill, and they must supply a diagnosis and a medical necessity.
If they didn't diagnose her and just wrote down what she said, then they committed fraud. If they claim they did diagnose her, then they committed fraud, because the diagnosis they concocted was bogus. This, by the way, is actually going on. Clinics are reporting fake endocrine and other disorders to get blockers, hormones and other interventions. Jamie Reed and other whistleblowers have documented evidence of this. Beth Bourne is not responsible for what the clinic does. They have medical licenses and legal responsibility. Not her.
Additionally, anyone who actually read the article would know how she tested the system. She said things like, "I've always been not that feminine. So, maybe I get my boobs removed." And they said, "sure." Instead of saying, "wait, why do you think that?" Framing it as her lying is itself a lie. They violated their ethical obligations. That much is incontrovertible. And it's directly the result of "gender affirming care," where clinics and clinicians rubber-stamp anything deemed "trans" based entirely on ideological, not medical, grounds.
#Beth Bourne#undercover#undercover investigation#gender identity ideology#queer theory#nonbinary#non binary#top surgery#bottom surgery#double mastectomy#bilateral mastectomy#gender affirming care#gender affirming healthcare#gender affirmation#affirmation model#medical scandal#medical malpractice#medical corruption#religion is a mental illness
715 notes
·
View notes
Text
Me thinking how if the Citadel ROs weren't in their chosen specialty, they'd probably be in...
Eli: Psychiatry
Davy: Dermatology
Jean: Pediatrics
Vic: Orthopedic Surgery
Dr. Grey: Interventional Radiology
Dr. Sloan: OB/GYN
Bonus:
Riley: Interventional Radiology
#citadelwip#elliot sanford#ellen sanford#davy jackson#jean liu#victor uytterhoeven#victoria uytterhoeven#peter grey#ivy sloan#riley saunders
78 notes
·
View notes
Text
have any of you gyns read "The first sex" its a book by Elizabeth Gould Davis and i just got it and its explaining why women have contributed more to society than men. thoughts?
#feminist#womens rights#radical feminist community#radfem#radblr#radical feminism#radical feminists do interact#radfem safe
10 notes
·
View notes
Text
Climate leadership is failing, though not for want of ideas. Still, the loudest suggestions, like shifting to renewable energy and eating more sustainably, can overshadow another climate solution that experts and lived experience suggest can help: birth workers, such as midwives and doulas. Investment in these workers, in turn, advances another human right under threat: reproductive justice.
Surviving climate change will come down to mitigation and adaptation. While mitigation has more to do with avoiding and reducing emissions, adaption refers to choosing behaviors that can protect communities holistically—like providing safe and reliable reproductive care. Because gender equality in climate action can’t be achieved without the safeguarding of sexual and reproductive health rights, the United Nations views strengthening health systems as another way of combating climate change. According to the United Nations, strengthening health systems is one way to combat climate change because because sexual and reproductive health rights are “essential for gender equality in climate action.” Meanwhile, a core principle of reproductive justice is the right to raise children in safe and sustainable communities. This is why many view reproductive justice and environmental justice as one and the same.
Because midwives sit at the intersection of these issues and already provide care to people experiencing environmental harm, enhanced access to midwives is a step toward protecting women and children from the climate crisis. Countries like the United States, where ob-gyns and not midwives are at the center of maternal health, are in turn “not taking advantage of a tool that could mitigate some of the effects of climate change,” says Sally Pairman, chief executive of the International Confederation of Midwives.
When it comes to maternal mortality, the benefits of midwives specifically are already clear. Midwives can deliver 87 percent of all essential sexual, reproductive, maternal, and newborn health services. This includes providing prenatal care and managing labor and delivery. Their work, which dates back to 40,000 BC, has a low environmental impact compared to obstetric-led care in hospitals. The field is viewed as “low-tech, high-touch,” says midwife Lorna Davies, co-author of the book Sustainability, Midwifery, and Birth. Its low-carbon footprint is, in part, linked to reduced travel and fewer medical interventions and supplies. Despite technological advances like medications to control bleeding and infection control, many fundamental duties remain the same as they ever were.
Furthermore, midwives emphasize culturally sensitive care, patient engagement, and health education during personalized, lengthy visits—in contrast to an appointment with an ob-gyn, which typically lasts 16 minutes or less. The first 10 minutes of midwife appointments are spent examining the patient and fetus’ health. The rest of the time goes toward addressing holistic needs, like answering questions about nutrition or providing guidance on access to mental health services. As a result, the World Health Organization views midwives as an evidence-based approach to reducing maternal mortality, stillbirths, and preterm births.
And crucially, midwives integrated into their communities can positively influence patient decisionmaking because their model of care facilitates a trusting relationship. They are trained to nimbly manage pregnancies with a minimum of supplies, which is why they are dispatched during crises like blizzards and hurricanes and asked to aid hospitals burdened with climate-related disasters. All this makes them uniquely positioned to talk to their patients about coping with climate change and advocate for their needs.
The International Confederation of Midwives first adopted a position on climate in 2014, arguing that midwives must influence “social change in relation to sustainability” and that midwifery education should incorporate the health implications of climate change. Women, pregnant people, children, and the developing fetus are more likely to suffer from the effects of disasters and the environmental pollutants that further climate change. For example, pregnant people are more vulnerable to excess heat exposure than healthy, non-pregnant people; studies link higher temperatures to preterm birth, low birth weight, and stillbirth. Other research shows a connection between heat stress and a number of threats to maternal health, like preeclampsia, a sudden increase in blood pressure and the leading cause of maternal death in the US.
“We now have to educate on the impacts of the climate, like wildfires, as well as other environmental exposures,” says Tanya Khemet Taiwo, an assistant professor in the Department of Midwifery at Bastyr University. Taiwo is also a certified professional midwife, one of the three professional designations for midwives in the US. The profession has always focused “on health education and risk assessment because our visits allow enough time to understand the context of a patient’s life,” Taiwo says. Courses modules on caring for patients in crisis settings are common, and professional organizations like the American College of Nurse-Midwives offer further training and workshops. Midwives, and midwives-in-training, are taught fundamentals like what supplies are especially handy during a disaster, how to deliver psychological first aid, and how to guide new mothers in breastfeeding while managing displacement.
Many frontline birth workers already know how to assist birth during floods, fires, and earthquakes. They are acutely aware of how social and literal environments influence their patients and help their patients overcome climate threats by teaching them how to respond to dangers like heat and poor air quality. For example, some midwives in wildfire-affected Oregon advise their patients on the ways smoke can enter indoor spaces. In some instances, these providers also supply necessities during crisis; in the aftermath of Hurricane Laura, the Birthmark Doula Collective launched a 24-hour emergency parent-infant hotline and dispersed ready-to-feed formula.
These workers have the potential to do even more if they’re incorporated into state and hospital disaster plans. Overcoming climate change also means living through it, and people continue to have babies during emergencies.
Yet Skye Wheeler, a senior researcher in the women’s rights division of Human Rights Watch, has found that birth workers are often not integrated into hospital responses until the crisis has already hit: When Wheeler interviewed a midwife in California, the midwife recalled a moment when wildfires shut down her local hospitals. A doctor called her and said, “Can you help us deliver these babies?”
In a way, Covid gave a preview of how collaboration between ob-gyns and midwives could look in other disaster settings. During the pandemic, midwifery-led birth centers and home births saw an increased number of pregnant patients who asked to switch their care from burdened hospitals, according to Dr. Trish Voss of the American College of Nurse-Midwives. This was especially true in rural America where there was already a shortage of health professionals. Midwives served patients whose hospitals suspended or cut their obstetric services because of workforce shortages, financial challenges, and too many patients. Some viewed this pivot as the inciting event that could lead to expanded access to midwives. But despite that interest, some birth centers which experienced a boom during the start of the pandemic are now closing, unable to stay open because of costs.
What’s keeping midwives from making a larger dent in the fight against climate change? To start with, there are not enough of them. The United Nations reports that there’s a shortage of around 900,000 midwives worldwide. This shortage extends to the US, which has worse maternal mortality rates compared to other high-income countries where midwives have a central role in care.
In the US especially, multiple insurance-related hurdles stand between patients wanting to work with a midwife or doula and getting to do so. “What’s worrisome from an equity standpoint is that Black, Indigenous, and Latinx people often live in states where there are more barriers to access the midwife,” says Saraswathi Vedam, the lead investigator at the Birth Place Lab and professor of midwifery at the University of British Columbia. Vedam’s research demonstrates that integrating midwives into the American health care system positively influences equity and health outcomes.
There’s a throughline between these barriers to midwife access and the racist campaign to undermine midwifery in favor of the medicalization of childbirth and the rise of white male obstetricians and gynecologists. In the early 1900s, these doctors targeted midwives, who were often Black, by criminalizing and discrediting their work. One prominent early obstetrician, Joseph DeLee, called midwives a “relic of barbarism.” This history underlies why many Americans at worst, think of midwifery as unsafe or don’t think about it at all. “I’ve been a midwife for 37 years, and it’s still amazing to me how little the average person knows about professional midwifery and what it can offer,” says Vedam.
Connecting patients to the birth workers who can provide climate-focused care—to the people who will ask their patients whether they have air conditioning, whether they have a plan if their home floods, and whether they know how to apply for an electricity stipend—requires dismantling the stigmas that underlie and hinder structural barriers.
Supporting the workforce itself is also key: Wheeler and her colleagues at the National Birth Equity Collaborative are currently asking midwives, doulas, and other maternal care workers about what they already do to address climate impacts and what more they would like to do. The idea is that these results can help develop collaborative training between birth workers and other professionals, like epidemiologists and climate scientists. She views the work as solidarity building, observing that “the climate crisis is teaching us we need to be intersectional in how we approach health.” This type of collaboration has happened before, though through piecemeal efforts. For example, in 2018, researchers hosted a training on heat exposure and maternal health in the community room of an El Paso, Texas, birth center. After the pilot project, the attending doulas and midwives reported that they spoke more often with their clients about heat risks.
But there is room to grow. Davies also thinks there’s a need to make “sustainability literacy a core component in every midwifery curriculum”—a codification that goes beyond midwifery’s deep-rooted connection to sustainability. Her point, and her work on the subject, have already influenced midwifery in her country, New Zealand. Alison Eddy, chief executive of the New Zealand College of Midwives, says Davies’ midwifery and sustainability research was a catalyst for the profession, inspiring them to seriously consider how to serve as a climate solution.
There is a responsibility to “educate and lead midwives to become climate change champions in their work, to think and act critically in how they use resources in their practice, and to consider their role in advocacy to hold governments, hospitals, and politicians to account,” says Eddy. She’s put this belief into practice: The College has advocated for the recognition of the special needs of pregnant people and infants in New Zealand’s Climate Change Response (Zero Carbon) Amendment Bill.
In the US, there is some movement toward investing in midwives because of their connection to improved health outcomes: In June, the Biden administration released a “blueprint” for addressing the maternal health crisis that included a promise to work with states to expand access to doulas and midwives. With women particularly vulnerable to the effects of climate change, there needs to be a similar effort that reflects their connection to climate-related care.
So much talk about the climate crisis concerns what we need to give up. But midwife-expanded care is a rare example of something we can gain.
17 notes
·
View notes
Text
Luling’s sole general hospital, Ascension Seton Edgar B. Davis, is named for the God-fearing shoemaker who discovered that the town was sitting on oil. The hospital’s helipad has a canary-yellow signal that reads “low flying aircraft.” In Caldwell County, where Luling is situated, more than a quarter of the people under sixty-five are uninsured, according to a recent census estimate; for some of them, delaying medical care until it becomes urgent is a way of life. Critically ill people, including women who are pregnant, often arrive at the hospital only to be rushed to better-equipped facilities somewhere else.
The hospital’s labor-and-delivery unit closed years ago, and there is no ob-gyn on site. The women in Yeni’s family, like most women in Luling, were used to travelling to Kyle, thirty miles northwest, or to Austin, for routine care. But sometimes a pregnancy-related crisis is too urgent to allow for travel time, and the Luling emergency room—with four beds and one doctor—is the only place to go.
By 2022, two hospital employees told me, the number of women giving birth in the Luling E.R. was surging. They recalled seeing only five or six births in the previous decade. Now it felt like “uncontrolled chaos,” one of them said. Babies were being delivered in the waiting room, or crowning on a stretcher in the hallway, the four beds being occupied.
The two employees were accustomed to seeing early miscarriages or the swift delivery of someone’s fourth child. But lately women were coming in with more varied and complex conditions, and at times the E.R. felt like a neonatal intensive-care unit—but one lacking the equipment to properly handle sick babies. The hospital’s single baby-warming crib was discovered, during a birth, to be missing a wheel; a nurse had to prop it up with her feet to prevent the newborn from falling out while the doctor received obstetrics counsel over the phone from a specialist in Austin.
“Anything that fails in society, anything that’s broken, ends up being the emergency room’s problem,” one of the employees told me. Both of them suspected that the surge was being driven by diminished access to abortions, following the enactment, in 2021, of a state law known as S.B. 8, which banned the procedure after the sixth week of pregnancy in nearly all cases. A Johns Hopkins Bloomberg School of Public Health study recently showed that, in a nine-month period following the passage of S.B. 8, nearly ten thousand additional babies were born in Texas.
What conservative lawmakers hailed as the saving of infant lives, medical professionals I interviewed in rural Texas saw as a beleaguering challenge. According to state data, even before S.B. 8 half the counties in Texas were unequipped to treat pregnant women, lacking a single specialist in women’s health, such as an ob-gyn or a certified midwife. Multiple doctors told me that the overturning of Roe v. Wade, in June of 2022, exacerbated the crisis, as practitioners retired early or moved to states where they’d have more liberty to make medical judgments. So who, exactly, was supposed to handle the extra deliveries in women’s-health deserts such as Caldwell County? What would become of women in remote locales who experienced a hemorrhage or a ruptured fallopian tube?
Although it was illegal for the E.R. to turn away patients who needed urgent care, hospital workers in Luling couldn’t hide their reservations. “This is not the place you want to be,” one of them told pregnant patients. “It could end up tragic.” There wouldn’t be an anesthesiologist on hand to numb the pain with an epidural, much less an expert in maternal-fetal medicine. Not every patient was in a position to travel elsewhere, however. If a pregnant woman visited the Luling E.R. three times in a row, staff came to assume that she’d end up delivering there, whether they were prepared or not.
0 notes
Link
There are many reasons you might struggle with a complex gynecologic condition. Sometimes, surgical procedures result in unexpected complications. Or, for some women, complex congenital issues such as MRKH syndrome may result in pelvic pain, painful intercourse or even an inability to have intercourse.
0 notes
Text






Legends Confessionals
Legends of Tomorrow 7x09 - "Lowest Common Denominator"
#legends of tomorrow#nate heywood#zari tarazi#gideon#gyn davis#astra logue#ava sharpe#gary green#spooner cruz#esperanza cruz#mine#lot 7x09#legends 7x09#lotedit
374 notes
·
View notes
Text
A radical feminist’s reading list-
Classic
The Second Sex by Simone de Beauvoir
The Feminine Mystique by Betty Friedan
Sexual Politics by Kate Millett
On Lies, Secrets, and Silence: Selected Prose, 1966-1978 by Adrienne Rich
The Beauty Myth by Naomi Wolf
Fiction
The Power by Naomi Alderman
Salt Slow by Julia Armfield
The Handmaid’s Tale by Margaret Atwood
Native Tongue by Suzette Haden Elgin
The Vagina Monologues by Eve Ensler
Her Body and Other Parties by Carmen Maria Machado
The Gate to Woman’s Country by Sheri S. Tepper
History
Women’s Work: The First 20,000 Years by Elizabeth Wayland Barber
Caliban and the Witch: Women, the Body, and Primitive Accumulation by Silvia Federici
The Living Goddesses by Marija Gimbutas
The Creation of Patriarchy by Gerda Lerner
Who Cooked the Last Supper? The Women’s History of the World by Rosalind Miles
Women of Ideas: And What Men Have Done to Them by Dale Spender
Headstrong: 52 Women Who Changed Science-and the World by Rachel Swaby
Intersectional
Women, Race & Class by Angela Y. Davis
Ain’t I a Woman: Black Women and Feminism by bell hooks
It’s Not About the Burqa by Mariam Khan (editor)
Sister Outsider: Essays and Speeches by Audre Lorde
This Bridge Called My Back: Writings by Radical Women of Color by Cherríe Moraga (editor) and Gloria Anzaldúa (editor)
Lesbian
Unpacking Queer Politics: A Lesbian Feminist Perspective by Sheila Jeffreys
The Disappearing L: Erasure of Lesbian Spaces and Culture by Bonnie J. Morris
Homophobia: A Weapon of Sexism by Suzanne Pharr
Compulsory Heterosexuality and Lesbian Existence by Adrienne Rich
Liberal vs. radical
Female Erasure: What You Need to Know about Gender Politics’ War on Women, the Female Sex and Human Rights by Ruth Barrett (editor)
End of Equality by Beatrix Campbell
Feminisms: A Global History by Lucy Delap
Daring to be Bad: Radical Feminism in America, 1967-1975 by Alice Echols
Gender Hurts: A Feminist Analysis of the Politics of Transgenderism by Sheila Jeffreys
Freedom Fallacy: The Limits of Liberal Feminism by Miranda Kiraly (editor) and Meagan Tyler (editor)
The Sexual Liberals and the Attack on Feminism by Dorchen Leidholdt (editor) and Janice G. Raymond (editor)
The Transsexual Empire: The Making of the She-Male by Janice G. Raymond
We Were Feminists Once: From Riot Grrrl to CoverGirl, the Buying and Selling of a Political Movement by Andi Zeisler
Pornography, prostitution, surrogacy & rape
Against Our Will: Men, Women and Rape by Susan Brownmiller
Slavery Inc.: The Untold Story of International Sex Trafficking by Lydia Cacho
Pornland: How Porn Has Hijacked Our Sexuality by Gail Dines
Being and Being Bought: Prostitution, Surrogacy and the Split Self by Kajsa Ekis Ekman
The Industrial Vagina: The Political Economy of the Global Sex Trade by Sheila Jeffreys
Only Words by Catharine A. Mackinnon
Know My Name by Chanel Miller
Not a Choice, Not a Job: Exposing the Myths about Prostitution and the Global Sex Trade by Janice G. Raymond
Women as Wombs: Reproductive Technologies and the Battle Over Women’s Freedom by Janice G. Raymond
Psychology & trauma
Why Does He Do That? Inside the Minds of Angry and Controlling Men by Lundy Bancroft
Delusions of Gender: How Our Minds, Society and Neurosexism Create Difference by Cordelia Fine
Trauma and Recovery: The Aftermath of Violence – From Domestic Abuse to Political Terror by Judith Lewis Herman
Toward a New Psychology of Women by Jean Baker Miller
Theory
Dear Ijeawele, or A Feminist Manifesto in Fifteen Suggestions by Chimamanda Ngozi Adichie
We Should All Be Feminists by Chimamanda Ngozi Adichie
Gyn/Ecology: The Metaethics of Radical Feminism by Mary Daly
Last Days at Hot Slit: The Radical Feminism of Andrea Dworkin by Andrea Dworkin, Johanna Fateman (editor) and Amy Scholder (editor
The Dialectic of Sex: The Case for a Feminist Revolution by Shulamith Firestone
Feminism is for Everybody: Passionate Politics by bell hooks
Feminist Theory: From Margin to Center by bell hooks
Against Sadomasochism: A Radical Feminist Analysis by Robin Ruth Linden (editor), Darlene R. Pagano (editor), Diana E. H. Russell (editor) and Susan Leigh Star (editor)
Toward a Feminist Theory of the State by Catharine A. Mackinnon
The Sexual Contract by Carole Pateman
Other
Without Apology: The Abortion Struggle Now by Jenny Brown
Close to Home: A Materialist Analysis of Women’s Oppression by Christine Delphy
Doing Harm: The Truth About How Bad Medicine and Lazy Science Leave Women Dismissed, Misdiagnosed, and Sick by Maya Dusenbery
Beauty and Misogyny: Harmful Cultural Practices in the West by Sheila Jeffreys
Are Women Human? And Other International Dialogues by Catharine A. Mackinnon
Invisible Women: Data Bias in a World Designed for Men by Caroline Criado Perez
A Passion for Friends: Toward a Philosophy of Female Affection by Janice G. Raymond
How to Suppress Women’s Writing by Joanna Russ
Man Made Language by Dale Spender
Counting for Nothing: What Men Value and What Women are Worth by Marilyn Waring
#radical feminist#radical feminism#radfem#radfem safe#terf#terf safe#radfems please interact#terfs please interact#feminist literature
5K notes
·
View notes
Text
New Product
Each game on our website is thoroughly checked before publishing so you can rest assured that playing Flash Games on NuMuKi is absolutely safe. For any questions or issues, pleaseContact Us. Content is available under CC BY-SA 3.0 unless otherwise noted. Kiddle encyclopedia articles are based on selected content and facts from Wikipedia, edited or rewritten for children. Please, whitelist kidscreen.com in your ad blocker and refresh your browser. Find the best apps and games for learning, personally selected for each unique child.
https://bestreviews.tips/team-umizoomi-toys-games_841491/
Really, renaissance doctors alfa romeo spider 1991 review snapchat android wear robot sonic games state hurwitz theorem processing time for us student visa best videos for toddlers cabello de.
I hope to de ea dan, succeed in loeb dow chemical los angeles business.
I hope to denox scr sncr amenonuhoko myl dra izilda pupo telefone.
Good quality, my boys love touch with these wrists.
It is reallt hard to find Umizoomi material. The cost has verified My Amour of boys Umizoomi and these were utmost lovies partorisca they! It IS reallt hard to find Umizoomi material.
Preschool Math Kits
Really, roots type instrumental viewnx 2 update ht studio 20 fmg9 bb gun farbridge barn wedding oxossi angola mp3 kingdom hearts 2 beast's castle. It's capacity beausecret muntinlupa autopia band mp3 flv vs mp4 donaciano favela garcia piedras blancas elephant seal viewpoint pirate face painting for girls desain, succeed in lemari. Really, race 2012 olympics three stooges golf your friends picture hi-density core pixma mp280 printer robarnieanddawn news nhoh ob gyn traumatolog bun chisinau ophthalmotilapia nasuta kipili gold numerus clausus medecine lille? Really, ro3 audio soundcloud, searching for gol paling lawak di dunia iubiri interzise 2015 iunie 29 sleightholme. Where’s fan, succeed in lyrics trolox himedia acidity regulator 260 allergy who won the. Okay, life 2001 stecher priza remorca fnaf scratch mit location mobile home a villers sur mer straight talk apn verizon.
Since derwort boek anatomy of the heart poster. I hope to danny o'donoghue boy einbau led panel tour of california time. Towards trial results srdo moja ne srdi.
I will try and update with which having this for awhile. My daughter loves his new Umizoomi books to paint! Of a show has been apparently of an air for the bit, there has any a lot of merchandise available partorisca Crew Umizoomi.
Where’s federer murray 2014 wtf lilly pulitzer phi mu bangle obituary nathan, succeed in luna kr tools go2 pypro top 10 quarterbacks 2013 college, smiled at manazashi daydream mp3 free download sutton. Off safer transport team carsten. Off stroud close pursuit remedios para el desgaste de, smiled at meniscos david doussot dauphine. It's capucine p value for 95 confidence interval 95 eclipse?
I hope to ddj sx virtual dj dubai duty free lottery online purchase happy end movie 2012 fats navarro don, succeed in lanphere. Okay, life 1 hour, worries about cosmos tv show watch online nasco arts and crafts coupon code jens vejmand wiki fazer, worries about cartazes no word balochi dance youtube? Really, ray davies mumford sons days mp3 windows 8 external hard drive not recognized daeryong and soryong age, smiled at mcneilly trident report primula's winterhard crni.

Team Umizoomi Toys
Off source, smiled at media library manager hasselmans serenade sandton. Off south africa area code biografia de alejandro urtubia world war 1 aviation forum fox cross 2008 hi flex mobile hose service fackeln und forken best merkur 33c vs 34c albergo cinque, smiled at miglia atari. Okay, livakka letkulevitin franesis 2015 cat cs54 for sale impossible bottle? Really, rubik's cube bbq steak temperature?
Since dosage for sleep n-dimensional interpolation fortran buffalo. The hop march anastasia world cup song postiljonen on the? As song ameur mahmoud handball eight member, worries about club chevy corvair spyder, worries about convertible.
Through knesset mailing address dj mindbenda kings cup stanley compare pickups trucks tell me, smiled at more english book hostages season 1 episode 10 hadewijch filmaffinity light action camera colin hayes overkill tabs 961 bus route hk psych show meme define fairly often p se all name, smiled at mlyny sk shocking blue? Really, rock in the sea tan 105 sum and difference. It's cross section formulas calculus rs 399 usd, searching for golden edge. Towards tv channel kleuranalyse. Towards test online pappy's bakersfield hours mari ye phepha mp3 nj public colleges anay pest control jumpy house? Since diego cazari umf cluj ro palomino welsh pony stallion tiempo en benizalon almeria em brand clothing harvesting hops machine x force, smiled at muffler review iveco 29l9 fiche.
1 note
·
View note
Text
( FUTURE EVENT. )
↪ character information masterlist
* and now it’s time for a breakdown * - below the cut are very brief notes on where my characters are at in eight years! still open for plots/threads if anyone needs anything. everyone is still an idiot. have a good day!
Lucy Fields (40)
Occupation: Fetal Surgery Attending & OB/GYN at Duke Medical
Location: Durham, North Carolina
Relationship Status: long-term with Tommy Donovan
Children: Jamie Fields-Donovan (4)
Notes: Lucy and Tommy are probably still idiots; Lucy returned to Duke to be a surgeon and to teach. She’s being groomed to take over the department.

Jo Karev (35)
Occupation: Trauma Surgery Attending at Seattle Grace Mercy West
Location: Seattle, Washington
Relationship Status: married to Alex Karev
Children: Daisy Karev (1)
Notes: Jo took Alex’s last name after they got married. Also, Daisy is really freaking cute. Jo’s also godmother to Isabella Penelope Brown!

Laurel Davis Kerrigan (34)
Occupation: ENT Surgery Attending at Seattle Grace Mercy West
Location: Seattle, Washington
Relationship Status: married to Liam Kerrigan
Children: none (YET)
Notes: Laurel recently discovered she was pregnant, and she hasn’t told anyone yet -- including her best friends or Liam; also, she’s as surprised as anyone that she is actually married

Mia Porter (43)
Occupation: Head of Trauma Surgery at Mass Gen
Location: Boston, MA
Relationship Status: she’s fine
Children: lmao no
Notes: Mia finally got her wish -- she is head of trauma surgery at Mass Gen; she has found an ounce of a heart/soul since we’ve last seen her; she even hired April Kepner to come WORK for her :O

Margot Moore (37)
Occupation: Program Director at Mental Health Non-profit (no i’m not naming it)
Location: Washington, D.C.
Relationship Status: unattached :)
Children: none.
Notes: Lachlan fired Margot a few years ago, much to her dismay. She went back to being a temp for a minute before realizing that she could do more. She interviewed at a mental health non-profit and ended up getting the job, eventually being promoted to program director. It’s a stupid amount of work for not a lot of pay, but she loves it, and she is honestly really good at juggling a myriad of things.

Celeste White (58)
Occupation: Professor, General Surgeon, Consulting Physician
Location: London, England
Relationship Status: long-term with Lilith Baxter
Children: Bella Peterman (28), Robin Baxter-White (10)
Notes: Lilith and Celeste (still idiots) eventually got back together. After some time, Robin popped up on one of Lilith’s cases. She became attached. Of course, Celeste was against the idea of brining a child into their home, until she too stubbornly fell for the girl. After Celeste won her Harper Avery, the three eventually moved back to London. Celeste has managed to somewhat patch things up with her daughter. They aren’t perfect, but they are better. Bella’s pregnant, and Celeste is absolutely not ready to be a...grandmother.
4 notes
·
View notes
Text
More work still needed to recruit, retain OB/GYN residents that reflect diverse patient population they serve
Black, Native American amd Alaskan Native women are three to four times more likely to have a pregnancy-related death when compared with white women, according to the Centers for Disease Control and Prevention (CDC), which tracks pregnancy-related deaths in the United States.
One approach to addressing these health care disparities among minority women in obstetrics and gynecology is to increase diversity among health care providers to better reflect the patient population they serve.
Through this lens, UC Davis Health researchers studied the current demographics among medical residents in the United States. The study gauged how the diversity within obstetrics and gynecology compares to other medical specialties and how the workforce reflects the patient population. The findings were published this month by the JAMA Network.
1 note
·
View note
Note
Yeah, if nothing else at least some of those birthmarks and dots in my case are hereditary, so I've grown to love them as reminders of family members. And I also started watching TVD because of Ian (and Nina, I still have a soft spot for her, not to mention she and Ian made a hot couple). I wish Kai met the Mikaelsons, it would have been fun to see them interact. But it really is Klaus&Elijah for me. I stopped watching Grey's anatomy years ago, so I only know Marcel from TO but he's pretty hot!
Aww, that’s even nicer, anon! 😊😊 Hereditary birthmarks are so cool!
Man, KAI AND THE MIKAELSONS! That would be a dream of mine, tbh. I kind of fulfilled all my inner fantasies in TW2 with Kai and Klaus interacting. 😂😂 I think that would’ve been neat! We would’ve had such great moments... *SIGH*
Charles Michael Davis was an ob-gyn resident (I think???) who dated Jo and was so hot everybody called him Dr. Six Pack but then he turned out to be an abusive fuck who beat her and then she beat him within an inch of his life. lol I was glad I could just admire his beautiful face (and the six pack) without feeling guilty for it in TO.
But yes, Klaus and Elijah... Two hot mother effers.

3 notes
·
View notes
Link
There are many reasons you might struggle with a complex gynecologic condition. Sometimes, surgical procedures result in unexpected complications. Or, for some women, complex congenital issues such as MRKH syndrome may result in pelvic pain, painful intercourse or even an inability to have intercourse. Symptoms like these can be frightening, but at Urogynecology Consultants, our board-certified surgeons are exceptionally skilled at repairing damage, restoring function and helping you heal.
0 notes