#medical healthcare
Text
The Intelligent Fabric Revolution: How Smart Technology is Reshaping the Medical Doctor Coat
The medical doctor coat, formerly a representation of wisdom and trust, has experienced a remarkable metamorphosis. The days when this outfit was only worn as a symbol of professionalism are long gone. We are at the cusp of a new age known as the intelligent fabric revolution, in which medical apparel will be combined with smart technology to create previously unthinkable advancements.
Tradition Meets Technology: The Genesis of Intelligent Medical Wear
Traditional medical doctor coats, while iconic, came with their set of limitations—lack of functionality beyond a superficial barrier, minimal protection against contamination, and a one-size-fits-all approach that often compromised on comfort. The advent of smart technology in healthcare attire has begun addressing these challenges head-on, offering groundbreaking solutions that extend far beyond aesthetics.
The Framework of Intelligent Fabric Technology in Doctor Coats
Intelligent fabrics represent a leap into the future, integrating technology at the very fibre of medical attire.
What are Intelligent Fabrics? These are textiles embedded with technology that allows for health monitoring, data collection, and even communication.
Embedded Technologies: Sensors and connectivity are sewn into the very essence of these fabrics, turning ordinary doctor coats into hubs of real-time medical data.
Benefits of Smart Medical Doctor Coats
Intelligent fabric integration in a medical doctor coat is more than just a novelty; it's revolutionising patient care and physician productivity.
Real-time health monitoring: By tracking a patient's vital signs, these smart coats can instantly notify medical personnel of changes in a patient's condition.
Enhanced Hygiene Control: These coats provide an extra line of defence against the transmission of infection because they have antibacterial qualities.
Enhancement of Decision-Making: Having instant access to patient data enables physicians to make well-informed judgements with speed.
The Practicalities of Intelligent Fabric Adoption in Healthcare
The implementation of this technology, while promising, is not without its challenges.
Cost Implications: The advanced technology in smart doctor coats may initially drive-up prices.
Adaptation and Training: Healthcare providers must become accustomed to new ways of interacting with their attire.
Data Privacy: The introduction of technology into clothing raises valid concerns over patient and doctor data security.
Despite these hurdles, the industry is taking strides to ensure the seamless adoption of intelligent fabrics into healthcare, underscoring the vast potential of this innovation.
The Future of Medical Doctor Wear: Predictions and Potentials
As we look ahead, the possibilities seem boundless. Imagine a future where a medical doctor coat, powered by AI, can not only monitor health but also predict potential medical issues before they arise. Consider the potential for universally connected healthcare networks facilitated through wearable technology. This is no longer the realm of science fiction but a tangible future where technology and healthcare converge for the greater good.
Conclusion
A new era in healthcare is being heralded by the combination of smart technology with medical doctor jackets. In the future, clothing will serve as an essential instrument for both medical efficiency and patient care, going beyond symbolic meaning. By embracing the intelligent fabric revolution, we not only reinvent the medical doctor coat and its functionality but also make a significant advancement in the rapidly changing healthcare industry. The road ahead is full of opportunities, and this change will have a profound effect on the healthcare sector, representing a critical turning point in our quest for excellence in healthcare delivery.
0 notes
Text
"The Biden Administration last week [early December, 2023] announced it would be seizing patents for drugs and drug manufacturing procedures developed using government money.
A draft of the new law, seen by Reuters, said that the government will consider various factors including whether a medical situation is leading to increased prices of the drug at any given time, or whether only a small section of Americans can afford it.
The new executive order is the first exercise in what is called “march-in-rights” which allows relevant government agencies to redistribute patents if they were generated under government funding. The NIH has long maintained march-in-rights, but previous directors have been unwilling to use them, fearing consequences.
“We’ll make it clear that when drug companies won’t sell taxpayer funded drugs at reasonable prices, we will be prepared to allow other companies to provide those drugs for less,” White House adviser Lael Brainard said on a press call.
But just how much taxpayer money is going toward funding drugs? A research paper from the Insitute for New Economic Thought showed that “NIH funding contributed to research associated with every new drug approved from 2010-2019, totaling $230 billion.”
The authors of the paper continue, writing “NIH funding also produced 22 thousand patents, which provided marketing exclusivity for 27 (8.6%) of the drugs approved [between] 2010-2019.”
How we do drug discovery and production in America has a number of fundamental flaws that have created problems in the health service industry.
It costs billions of dollars and sometimes as many as 5 to 10 years to bring a drug to market in the US, which means that only companies with massive financial muscle can do so with any regularity, and that smaller, more innovative companies can’t compete with these pharma giants.
This also means that if a company can’t recoup that loss, a single failed drug can result in massive disruptions to business. To protect themselves, pharmaceutical companies establish piles of patents on drugs and drug manufacturing procedures. Especially if the drug in question treats a rare or obscure disease, these patents essentially ensure the company has monoselective pricing regimes.
However, if a company can convince the NIH that a particular drug should be considered a public health priority, they can be almost entirely funded by the government, as the research paper showed.
Some market participants, in this case the famous billionaire investor Mark Cuban, have attempted to remedy the issue of drug costs in America by manufacturing generic versions of patented drugs sold for common diseases."
-via Good News Network, December 11, 2023
#united states#us politics#biden administration#executive order#prescription drugs#medical news#healthcare#healthcare access#biden#big pharma#drug prices#public health#nih#national institutes of health#good news#hope
10K notes
·
View notes
Text
Fetal Medicine Fellowship in Delhi to Advancing Expertise in Fetal Medicine with DMHCA

DMHCA offers a prestigious Fetal Medicine Fellowship in Delhi. Designed for medical professionals, this program provides comprehensive training, clinical exposure, and expert mentorship. With state-of-the-art facilities and experienced faculty, participants gain advanced knowledge in fetal diagnosis, management, and interventions. Join DMHCA's Fetal Medicine Fellowship in Delhi to enhance your expertise in this specialized field.
#fetal medicine fellowship#medicine fellowship#medical healthcare#medical courses#delhi medical#healthcare academy
0 notes
Text
Unwanted Pregnancy in Delhi.
Experience at best on unwanted pregnancy in Delhi with Dr. Rupali Abortion Center. Explore all options, find support, and make informed decisions for your journey ahead.
0 notes
Text
*Not counting routine checkups or normal doctor's visits– this is asking about serious illness, injury, etc where you were in a bed.
–
We ask your questions so you don’t have to! Submit your questions to have them posted anonymously as polls.
#polls#incognito polls#anonymous#tumblr polls#tumblr users#questions#medical#hospital#healthcare#doctors#polls about health
7K notes
·
View notes
Text
69K notes
·
View notes
Text
you have to go to work so you can pay for your doctor, who is not taking your insurance right now, and if you say i can't afford the doctor's you are told - get a better job. it is very sad that you are unwell, yes, but maybe you should have thought about that before not having a better job.
(where is the better job? who is giving out these better jobs? you are sick, you are hurting - how the hell are you supposed to be well enough for this better job?)
but you go to the doctor because you had the nerve to be hurt or sick or whatever else. and they tell you that it is because you have anxiety. you try your best. you are a self-advocate. you've done the reading (which sometimes pisses them off worse, honestly). you say it is actually adding to my anxiety, it is effecting my quality of life. so they say that you are fat. they say that all young people have this happen to them, isn't it a medical marvel! they say that you should eat more vegetables. they say that you probably just need to lose a little more weight, and that you are faking it for attention.
(what attention could this doctor possibly give? what validation? that's their fucking job, isn't it?)
there is always a hypochondriac, right. someone always tells you about a hypochondriac. or someone who is unnecessarily aggressive during the worst days of their life. or someone looking "for a quick fix". or some idiot who wasn't educated about how to properly care for themselves who just abandons their treatment. and again, the hypochondriac, the overly-cautious hysteric. these people don't deserve to be treated like humans (right), and since you might be one of these people, you also don't get treated like a human. because those people can really fuck with the system, you now have to pay for it. and besides. you're actually probably faking it.
(more often than not, you find a 2:1 ratio of these stories. for every "hypochondriac", there are 2 people who knew something was wrong, and yet nobody could fucking find it. the story often ends with pointless suffering. the story often ends with and now it's too late, and it's going to kill me.)
you are actually just making excuses. someone else got that procedure or that diagnosis and he's fine, you should be fine too. someone else said they watched a documentary about other inspirational people with your exact same condition, maybe you should be inspirational, too. you're just too morbid. your pain and your experience is probably just not statistically concerning. it is all self-reported anyway, and you're just being a baby.
(once, while sitting down in the middle of making coffee, you had the sudden, horrible thought - i could kill myself to make the pain stop. you had to call your best friend after that. had to pet your dog. had to cry about it in the shower. you won't, but that moment - god, fuck. the pain just goes on and on.)
you know someone who went in for routine surgery and said i still feel everything. they told her to just relax. it took her kicking and screaming before they figured out she wasn't lying - the anesthetic drip hadn't been working. you know someone who went in for severe migraines who was told drink water and lose weight. you know someone who was actively bleeding out and throwing up in the ER and was told you're just having a bad period.
in the ER there are always these little posters saying things like "don't wait! get checked today!" and you think about how often you do wait. how often the days spool out. you once waited a full week before seeing the doctor for what you thought was a sprained wrist. it had actually been broken - they had to rebreak it to set it.
but you go into the doctor. the problem you're having is immediate. the person behind the counter frowns and says we're not taking your insurance. you will be paying for this out-of-pocket.
they send you home with tylenol and a little health packet about weight loss or anxiety or attention deficit. on the front it has your birthday and diagnosis. you think about crying, and the words swim. it might as well say go fuck yourself. it might as well say you're a fucking idiot. it might as well say light your money on fire and lie down in it. and the entire fucking time - the problem persists.
it's okay. it's okay, it's just another thing, you think. it's just another thing i have to learn to live with.
#spilled ink#warm up#can you tell what i'm mad about today specifically#i will say that there are a LOT of things that go into this. like a lot. this is ungendered and unspecific for a reason#it isn't just sexism. it's also racism. and ableism. and honestly classism.#and before a healthcare professional reads this as a personal attack: i understand ur burnt out#we are ALSO burnt out. your situation is also dire. this is not an attack on you.#this is a commentary on the incredible amounts of bigotry that lie at the heart of capitalism#where people have to pay money out of pocket to be told to fuck off.#your job is important. so is our humanity. and if you cannot accept that people are fucking mad as hell#at the industry - you are probably not listening .#anyway at some point im gonna write a piece about sexism specifically in medical shit#but i don't want terfs clowning in it bc they can't understand nuance#> it is true that ppl w/a uterus are more likely to experience medical malpractice & dismissal globally#> it is also true that trans people experience an equally fucked up and bad time in the medical field#> great news! the medical industrial complex is an equal opportunity life ruiner :)#(if you find it necessary to go into a debate about biology while discussing medical malpractice#i want to warn you that you're misunderstanding the issue. because guess what.#cis MEN might experience this. particularly black men. particularly disabled men.#so YES having a uterus can lead to more trouble for you. but this happens a LOT.#instead of fighting those ALSO experiencing your pain.... try working WITH them.#which btw. is like. actual feminism.)
2K notes
·
View notes
Text
Max Super Speciality Hospital, Delhi, India
Max Hospital Saket, New Delhi is a super-specialty hospital. It was established in 1989 under JCI, NABL, and NABH Accreditation. It is (A Unit of the Devki Devi Foundation and a part of the Max Healthcare consortium) and is a world-renowned healthcare provider.

0 notes
Text
Yesterday was my first time in the ER since my hEDS diagnosis was officially added to my file (instead of me having to tell them and hoping they’d believe me), and everyone in my emergency care team was on top of it. Like on the ball, fully engaged and interested in keeping the zebra in the hospital comfortable.
They also all knew what MCAS and POTS were and deferred to me when it came to medication and pain management. Which was also wild, because they were not shy at all about offering pain relief. They straight up offered me narcotics, when usually the most I get offered is Tylenol.
Even the CT tech knew what MCAS was and asked if we should pre-treat with Benadryl because he knew some patients could experience mast cell destabilization from the radiation even without the contrast dye.
He and the nurse even helped brace my neck when I was going into the CT machine because I mentioned having cranial instability, and the position I was in was making my neck click, so they stopped everything to find multiple pillows to brace my neck and shoulders while I was on the table.
Afterward, while being bussed through the corridors in my bed (because they had to dehydrate me to take the CT scan and my POTS was going haywire, and they made sure I had to be upright as little as possible), I commented to my nurse that I was startled that everyone I’d spoken to that day knew about EDS/MCAS/POTS and were so accommodating.
He paused before answering, then told me, “We probably don’t know as much about EDS as we should, but we’ve seen a lot of the other two over the last few years. Covid really messed people up. Did yours start with covid?” No, I told him. We think I was probably born with it and a dental infection turned it lethal. He expressed his sympathy and again reminded me I didn’t need to be a hero and I could press the pain med button whenever I needed to.
Back in my room, they started me on IV fluids to combat the dehydration from the POTS. And I was laying there, I became aware of the nurse bracing my elbow so it wouldn’t hyperextend while he futzed around with the IV and I remember thinking, “this is how it always should have been.”
The kindness and care shown to me were in such stark contrast to past experiences it made me quite tearful. There were no accusations of anxiety, no referrals to psyche, and no implications that I was over-exaggerating my pain. No denying of my experiences.
Just a quiet, vocal acceptance that I “knew my body best” and that they’d do whatever they could to help.
It was nice.
#chronic health tag#posting for bad days when I need to remember there are good healthcare providers#long post#medical trauma
4K notes
·
View notes
Text
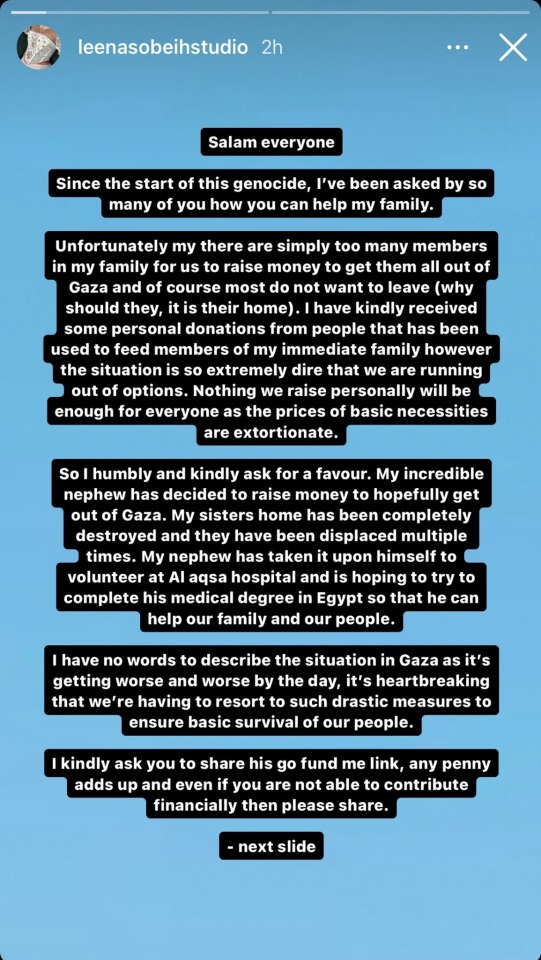
Fundraiser for fashion designer Leena Sobieh's nephew to leave Gaza and continue his medical studies in Egypt. Please share and donate if you can.
#social justice#signal boost#palestine#free palestine#gaza#free gaza#jerusalem#israel#tel aviv#gaza strip#from the river to the sea palestine will be free#joe biden#benjamin netanyahu#gaza news#north gaza#palestinian genocide#gaza genocide#current events#news#medicine#medical student#healthcare#i stand with palestine 🇵🇸#palestine genocide#palestine resources#support palestine#palestinian doctors#gaza under attack#stand with gaza#palestinian
942 notes
·
View notes
Text
The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.”
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries reminiscent of a scene from “Awakenings,” the famous book and movie inspired by the awakening of catatonic patients treated by the late neurologist and writer Oliver Sacks.
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other peoplewith similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients,the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.”
– A catatonic woman awakened after 20 years. Her story may change psychiatry.
#block JavaScript in site settings if article is paywalled#April burrel#disability#schizophrenia#lupus#mental illness#catatonia#chronic illness#institutionalization#psychiatry#medical science#healthcare#autoimmune disease#Washington post#knee of huss
3K notes
·
View notes
Text
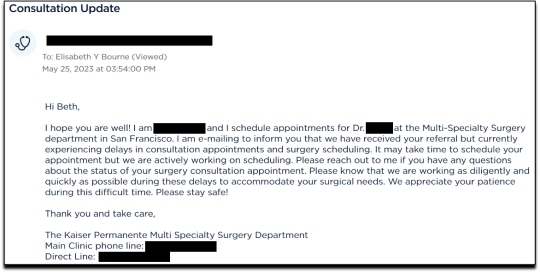
By: Beth Bourne
Published: Feb 27, 2024
Kaiser gender specialists were eager to approve hormones and surgeries, which would all be covered by insurance as “medically necessary.”
On September 6, 2022, I received mail from my Kaiser Permanente Davis Ob-Gyn reminding me of a routine cervical screening. The language of the reminder stood out to me: “Recommended for people with a cervix ages 21 to 65.” When I asked my Ob-Gyn about this strange wording, she told me the wording was chosen to be “inclusive” of their “transgender” and “gender fluid” patients.
Based on this response, several thoughts occurred to me. Could I expose the medical scandal of “gender-affirming care” by saying and doing everything my daughter and other trans-identifying kids are taught to do? Would there be the type of medical safeguarding and differential diagnosis we would expect in other fields of medicine, or would I simply be allowed to self-diagnose and be offered the tools (i.e. hormones and surgeries) to choose my own gender adventure and become my true authentic self?
If I could demonstrate that anyone suffering from delusions of their sex, self-hatred, or identity issues could qualify for and easily obtain body-altering hormones and surgeries, all covered by insurance as “medically necessary” and potentially “life-saving” care, then maybe people would finally wake up. I certainly had.
I was prepared for failure. I wasn’t prepared for how easy success would be.
* * *
I am a 53-year-old mom from Davis, CA. My daughter began identifying as a transgender boy (social transition) and using he/him pronouns at school during 8th grade. Like several of her peers who also identified as trans at her school, my daughter was a gifted student and intellectually mature but socially immature. This shift coincided with her school’s sudden commitment to, and celebration of, a now widespread set of radical beliefs about the biology of sex and gender identity.
She “came out” as trans to her father (my ex-husband) and me through a standard coming-out letter, expressing her wish to start puberty blockers. She said she knew they were safe, citing information she had read from Planned Parenthood and the World Professional Association for Transgender Health (WPATH). To say I was shocked would be an understatement. I was also confused because this announcement was sudden and unexpected. While others quickly accepted and affirmed my daughter’s new identity, I was apprehensive and felt the need to learn more about what was going on.
Events began escalating quickly.
During a routine doctor’s visit scheduled for dizziness my daughter said that she was experiencing, the Kaiser pediatrician overheard her father using “he/him” pronouns for our daughter. The pediatrician seemed thrilled, quickly asking my daughter about her “preferred pronouns” and updating her medical records to denote that my daughter was now, in fact, my son. The pediatrician then recommended we consult the Kaiser Permanente Oakland Proud pediatric gender clinic, where she could get further information and (gender affirming) “treatment.” Now I was the one feeling dizzy.
As I began educating myself on this issue, I discovered that this phenomenon—minors, most often teen girls, suddenly adopting trans identities—was becoming increasingly widespread. It even had a name: rapid onset gender dysphoria, or ROGD. Thankfully, after learning about the potential side-effects of blockers and hormones, my ex-husband and I managed to agree not to consent to any medical interventions for our daughter until she turned 18 and would then be able to make such decisions as an adult.
Over the past five years, my daughter’s identity has slowly evolved in ways that I see as positive. Our bond, however, has become strained, particularly since I began publicly voicing my concerns about what many term as “gender ideology.” Following my daughter’s 17th birthday family celebration, she sent me an email that evening stating she would be cutting off contact with me.
While this estrangement brought me sorrow, with my daughter living full-time with her father, it also gave me the space to be an advocate/activist in pushing back on gender identity ideology in the schools and the medical industry.
I decided to go undercover as a nonbinary patient to show my daughter what danger she might be putting herself in—by people who purport to have her health as their interest, but whose main interest is in medically “affirming” (i.e., transitioning) whoever walks through their door. I am at heart a mother protecting her child.
* * *
My daughter’s sudden decision to become a boy was heavily on my mind in early September of 2022, when mail from my Kaiser Permanente Davis Ob-Gyn reminded me of a routine cervical screening with “Recommended for people with a cervix ages 21 to 65.” I was told that the wording was chosen to be “inclusive” of transgender and “gender fluid” patients.
Throughout the whole 231-day process of my feigned gender transition, the Kaiser gender specialists were eager to serve me and give me what I wanted, which would all be covered by insurance as “medically necessary.” My emails were returned quickly, my appointments scheduled efficiently, and I never fell through the cracks. I was helped along every step of the way.
Despite gender activists and clinicians constantly claiming that obtaining hormones and surgeries is a long and complex process with plenty of safety checks in place, I was in full control at every checkpoint. I was able to self-diagnose, determine how strong a dose of testosterone I received and which surgeries I wanted to pursue, no matter how extreme and no matter how many glaring red flags I purposefully dropped. The medical workers I met repeatedly reminded me that they were not there to act as “gatekeepers.”
I was able to instantly change my medical records to reflect my new gender identity and pronouns. Despite never being diagnosed with gender dysphoria, I was able to obtain a prescription for testosterone and approval for a “gender-affirming” double mastectomy from my doctor. It took only three more months (90 days) to be approved for surgery to remove my uterus and have a fake penis constructed from the skin of my thigh or forearm. Therapy was never recommended.
Critics might dismiss my story as insignificant on the grounds that I am a 53-year-old woman with ample life experience who should be free to alter her body. However, this argument for adult bodily autonomy is a standard we apply to purely cosmetic procedures like breast implants, liposuction, and facelifts, not “medically necessary” and “lifesaving” treatments covered by health insurance. Or interventions that compromise health and introduce illness into an otherwise healthy body. And especially not for children.
My story, which I outline in much more detail below, should convince any half-rational person that gender medicine is not operating like any other field of medicine. Based on a radical concept of “gender identity,” this medical anomaly preys upon the body-image insecurities common among pubescent minors to bill health insurance companies for permanent cosmetic procedures that often leave their patients with permanently altered bodies, damaged endocrine systems, sexual dysfunction, and infertility.
* * *
Detailed Timeline of Events
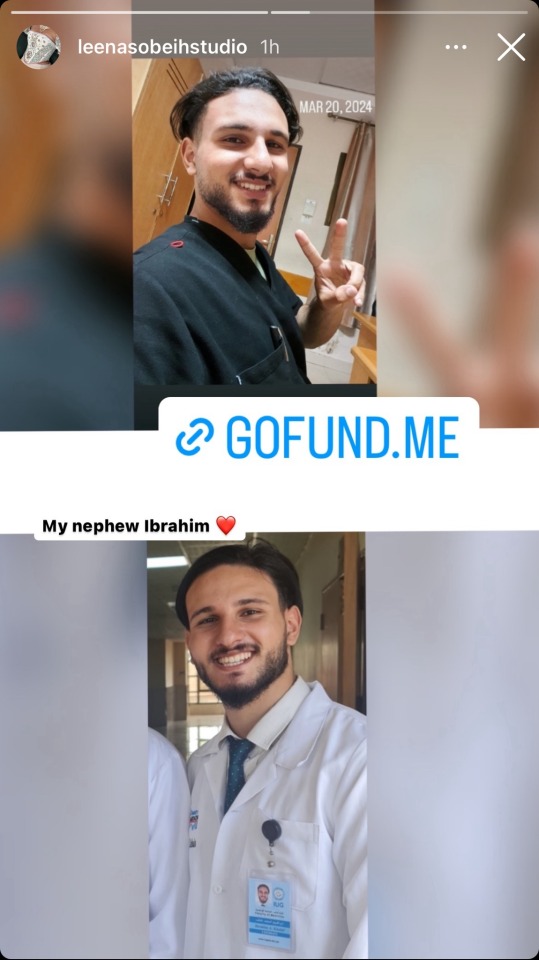
On October 6, 2022, I responded to my Ob-Gyn’s email to tell her that, after some thought, I’d decided that maybe the label “cis woman” didn’t truly reflect who I was. After all, I did have some tomboyish tendencies. I told her I would like my records to be changed to reflect my newly realized “nonbinary” identity, and that my new pronouns were they/them. I also voiced my desire to be put in touch with an endocrinologist to discuss starting testosterone treatment.
Fifteen minutes later I received an email from another Kaiser doctor informing me that my medical records had been changed, and that once my primary doctor returned to the office, I’d be able to speak with her about hormone therapy.
I responded the following day (October 7, 2022), thanking her for changing my records, and asking if she could connect me with someone who could help me make an appointment for “top surgery” (i.e., a cosmetic double mastectomy) because my chest binder was rather “uncomfortable after long days and playing tennis.”
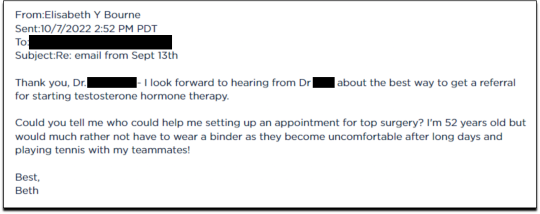
She told me to contact my primary care MD to “get things rolling,” and that there were likely to be “preliminary evaluations.”
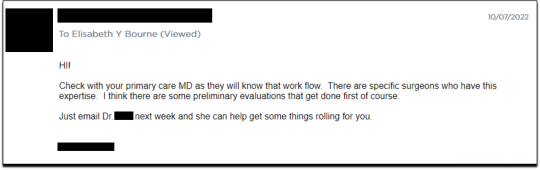
Six days after contacting my primary care MD for a referral, I received an email from one of Kaiser’s gender specialists asking me to schedule a phone appointment so she could better understand my goals for surgery, so that I could get “connected to care.” This call to review my “gender affirming treatment options and services” would take 15-20 minutes, after which I would be “booked for intake,” allowing me to proceed with medical transition.
This wasn’t an evaluation of whether surgical transition was appropriate, it was simply a meeting for me to tell them what I wanted so that they could provide it.
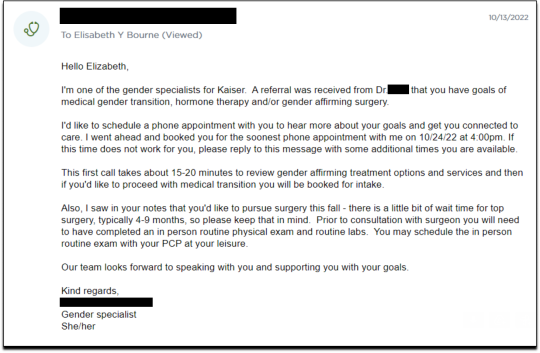
On October 18, I had my one and only in-person appointment in preparation for top surgery. I met in Davis with my primary care physician, Dr. Hong-wen Xue. The assessment was a 10-minute routine physical exam that included blood tests. Everything came back normal. Notably, there was not a single question about why I wanted top surgery or cross-sex hormones. Nor was there any discussion of the risks involved with these medical treatments.
The following week, on October 24, I had a phone appointment with Rachaell Wood, MFT, a gender specialist with Kaiser Sacramento. The call lasted 15 minutes and consisted of standard questions about potential drug use, domestic violence, guns in the house, and whether I experienced any suicidal thoughts. There were no questions from the gender specialist about my reasons for requesting a mastectomy or cross-sex hormones, or why I suddenly, at 52, decided I was “nonbinary.”
After the call, Kaiser emailed me instructions about how to prepare for my pre-surgery intake video appointment to evaluate my mental health, scheduled to take place on November 15. The email stated that prior to my appointment, I should research hormone risks on the WPATH website, and to “research bilateral mastectomy and chest reconstruction surgery risks and recovery” on Kaiser’s website.
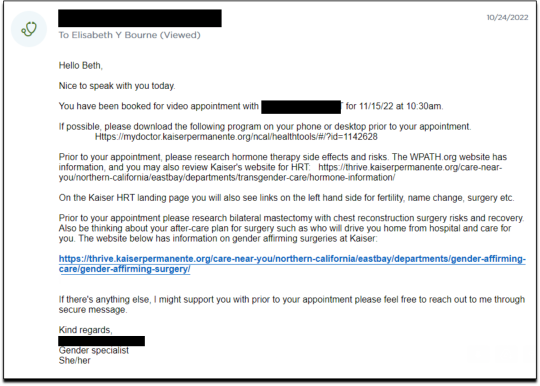
I decided to request a “gender-affirming” double mastectomy and phalloplasty. Kaiser sent me a sample timeline for gender transition surgery preparation (see below) that you can use as a reference for the process. I also asked for a prescription for cross-sex hormones (testosterone) as needed and recommended by Kaiser.
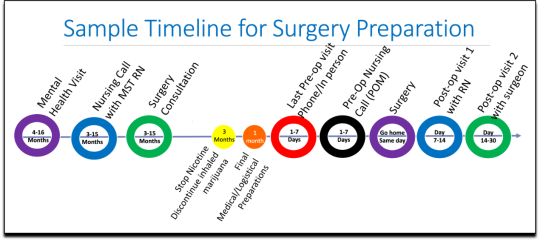
[ Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
Pre-Surgery Mental Health Video Appointment, Part I
This “Mental Health Visit” assessment was conducted over Zoom. The Kaiser gender specialist started with questions addressing my marital status, race, gender identity, and other demographics. She asked whether I was “thinking of any other surgeries, treatments in the future.” The list she read included “gender-affirming” hysterectomies, bottom surgeries such as metoidioplasty and phalloplasty, vocal coaching, support groups, and body contouring. “Anything else you might be interested in doing?” she asked. I said that I’d perhaps be interested in body contouring. I was also assured that all the procedures would be covered by insurance because they were considered “medically necessary.”
I dropped in several red flags regarding my mental health to see the reaction, but all were ignored. For instance, I revealed that I had PTSD. When the therapist asked me about whether I had experienced any “childhood trauma,” I explained that I grew up in Mexico City and had been groped several times and had also witnessed men masturbating in public and had been grabbed by men in subways and buses. “I was a young girl, so [I had] lots of experiences of sexual harassments, sexual assault, just the kind of stuff that happens when you are a girl growing up in a big city.” “So, you know,” I finished, “just the general feeling that you are unsafe, you know, in a female body.”
The therapist did not respond to my disclosure that trauma could be the cause of my dysphoria. Instead of viewing this trauma as potentially driving my desire to escape my female body through hormones and surgery, she asked whether there is anything “important that the surgery team should be aware of” regarding my “history of trauma,” such as whether I’d be comfortable with the surgeon examining and marking my chest prior to surgery.
When asked about whether I had had any “psychotic symptoms,” I told her that while I had had no such symptoms, my mother had a delusional nervous breakdown in her 50s because she had body dysmorphia and became convinced she had a growth on her neck that needed to be removed. I told her that my mother was then admitted to an inpatient hospital for severe depression. I asked her whether she ever sees patients with body dysmorphia and whether I could have potentially inherited that from my mother. She told me that psychosis was hereditary, but that it was “highly unlikely” that there was any connection between body dysmorphia and gender dysphoria.
I enthusiastically waved more mental health red flags, waiting to see if she would pick up on any of them.
I’m just wondering if my feelings, or perseverating, or feeling like these breasts make me really unhappy and I just don’t want them anymore!...I’m just not sure if that’s a similar feeling to body dysmorphia? How do you decide which one is gender dysphoria and general body dysmorphia, and just not liking something about your body? Feeling uncomfortable with your body?
And I did have an eating disorder all through college. I was a distance runner in college so I had bulimia and anorexia, you know. So I don’t know if that’s related to gender dysphoria?
The therapist replied, “I completely appreciate your concerns, but I am going to ask you questions about your chest, about your expectations. And then I’ll be able to give you an assessment.” She also said the main difference between my mom’s situation and mine was that my mom didn’t really have a growth on her neck, whereas it’s “confirmed” that I actually have “chest tissue.” Furthermore, she said that while “historically there has been all this pressure on patients to be like ‘Are you really, really sure you want hormones? Are you 100% sure?’ We are a little more relaxed.” She continued, “As long as you are aware of the risks and the side-effects, you can put your toe in the water. You can stop ‘T’ [testosterone], you can go back and do it again later! You can stop it! You can stop it! You know what I mean?”
Because we ran out of time, I scheduled a follow-up phone meeting on December 27, 2022 with a different gender specialist to complete my mental health assessment for top surgery.
Pre-Surgery Mental Health Video Appointment, Part II
During this meeting, Guneet Kaur, LCSW, another Kaiser gender specialist (she/her/they/them pronouns) told me that she regretted the “gatekeeping vibe” of the meeting but assured me that since I have been “doing the work,” her questions are essentially just a form of “emotional support” before talking with the medical providers.
She asked me about what I’d been “looking into as far as hormones.” I told her that I’d be interested in taking small doses of testosterone to counterbalance my female feelings to achieve “a feeling that’s kind of neutral.”
When she asked me about me “not feeling like I match on the outside what I feel on the inside,” I dropped more red flags, mentioning my aversion to wearing dresses and skirts.
I don’t own a single dress or a skirt and haven't in 20 years. I think for me it’s been just dressing the way that’s comfortable for me, which is just wearing, jeans and sweatshirts and I have a lot of flannel shirts and, and I wear boots all the time instead of other kinds of shoes. So I think it’s been nice being able to dress, especially because I work from home now most of the time that just a feeling of clothing being one of the ways that I can feel more non-binary in my everyday life.
She responded, “Like having control over what you wear and yeah. Kind of that feeling of just, yeah, this is who I am today. That’s awesome. Yeah.”
She then asked me to describe my dysphoria, and I told her that I didn’t like the “feeling of the female form and being chesty,” and that because I am going through menopause, I wanted to start taking testosterone to avoid “that feeling of being like this apple-shaped older woman.” “Good. Okay, great,” she responded, reminding me that only “top surgery,” not testosterone, would be able to solve my chest dysphoria. (Perhaps it was because all these meetings were online, they didn’t notice I’m actually fit and relatively slender at 5’-5” and 130 pounds, and not apple-shaped at all.)
She told me that we had to get through a few more questions related to my medical history before “we can move on to the fun stuff, which is testosterone and top surgery.”
The “fun stuff” consisted of a discussion about the physical and mood changes I could expect, and her asking me about the dose of testosterone I wanted to take and the kind of “top surgery” technique I’d prefer to achieve my “chest goals.” She told me that all or most of my consultations for surgeries and hormones would be virtual.
The gender specialist told me after the appointment, she would submit my referral to the Multi-Specialty Transitions Clinic (MST) team that oversees “gender expansive care.” They would follow up to schedule a “nursing call” with me to review my medical history, after which they’d schedule my appointment with a surgeon for a consultation. Her instructions for this consultation were to “tell them what you’re wanting for surgery and then they share with you their game plan.”
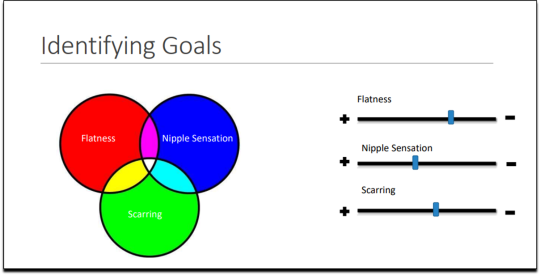
[ Decision-making slide to help me identify my goals for top surgery–flat chest, nipple sensation, or minimal scarring. Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
She told me that Kaiser has a team of plastic surgeons who “only work with trans and nonbinary patients because there’s just so much need for them.” She asked about my priorities for chest surgery, such as whether I value flatness over nipple sensation. I learned about double incision top surgery with nipple grafts, as well as “keyhole,” “donut,” “buttonhole,” and “Inverted-T” top surgeries.
By the end of the hour-long appointment, I had my surgery referral and was ready for my “nursing call” appointment.
Nursing call with Nurse Coordinator from the Transgender Surgery and Gender Pathways Clinic at Kaiser San Francisco
On January 19, 2023, I had my nursing call with the Nurse Coordinator. He first said that “the purpose of this call is just for us to go through your chart together and make sure everything’s as accurate as possible.” Once that was done, my referral would be sent to the surgeon for a consultation.
He asked me about potential allergies and recreational drug use, and verified that I was up to date on mammograms, pap smears, and colon cancer screenings, as well as vaccines for flu and COVID. I verified my surgical history as well as my current medications and dietary supplements.
He told me about a “top surgery class” available for patients where one of the Kaiser surgeons “presents and talks about surgical techniques and options within top surgery,” and includes a panel of patients who have had top surgery. I signed up for the February 8th class.
Within 10 minutes he told me that he had “sent a referral to the plastic surgery department at Kaiser Sacramento,” and that I should be hearing from them in the next week or two to schedule a consultation.
Appointment for Testosterone
On January 27, I had a 13-minute online appointment with a primary care doctor at Kaiser Davis to discuss testosterone. The doctor verified my name and preferred pronouns, and then directly asked: “So, what would you like to do? What kind of physical things are you looking for?”
I told her I wanted facial hair, a more muscular and less “curvy” physique, and to feel stronger and androgynous. She asked me when I wanted to start, and I told her in the next few months. She asked me if I was menopausal, whether I had ovaries and a uterus, although that information should have been on my chart.
The doctor said she wanted me to come in to get some labs so she could check my current estrogen, testosterone, and hemoglobin levels before starting hormones. Then “we'll set the ball in motion and you'll be going. We’ll see you full steam ahead in the direction you wanna go.”
That was it. I made an appointment and had my lab tests done on February 12. My labs came back on February 14, and the following day, after paying a $5 copay at the Kaiser pharmacy, I picked up my testosterone pump. That was easy!
Top Surgery Consultation
On the same day I received my labs, I had a Zoom surgery consultation with Karly Autumn-Kaplan, MD, Kaiser Sacramento plastic surgeon. This consultation was all about discussing my “goals” for surgery, not about whether surgery was needed or appropriate.
I told the surgeon that I wanted a “flatter, more androgynous appearance.” She asked me some questions to get a better idea of what that meant for me. She said that some patients want a “male chest,” but that others “want to look like nothing, like just straight up and down, sometimes not even nipples.” Others still wanted their chest to appear slightly feminine and only “slightly rounded.” I told her that I’d like my chest to have a “male appearance.”
“What are your thoughts about keeping your nipples?” she asked. “Are you interested in having nipples or would you like them removed?” I told her that I’d like to keep my nipples, but to make them “smaller in size.” She asked me if I’d like them moved to “the edge of the peck muscle” to achieve “a more male appearance.” I said yes.
I was asked to show my bare chest from the front and side, which I did. Then she asked me how important it was for me to keep my nipple sensation. I replied that it was important unless it would make recovery more difficult or there were other associated risks. She highlighted the problem with the free nipple graft, saying that removing the nipple to relocate it means “you're not gonna have sensation in that nipple and areola anymore.” However, some nipple sensation could be preserved by keeping it attached to “a little stalk of tissue” with “real nerves going to it,” but that would require leaving more tissue behind. I told her I’d go for the free nipple graft to achieve a flatter appearance. It was also suggested I could skip nipple reconstruction entirely and just get nipples “tattooed” directly onto my chest.
She told me I was “a good candidate for surgery,” and put me on the surgery wait list. She said that the wait time was between three and five months, but a cancellation could move me up to a sooner date. Also, if I wanted surgery as soon as possible, I could tell the surgery scheduler that I’d be willing to have any of the other three surgeons perform my mastectomy. Outpatient top surgery would cost me a copay of $100.
They contacted twice, in February and March, notifying me of cancellations. If I had accepted and shown up on those dates, they would have removed my breasts. This would have been less than five months from the time I first contacted Kaiser to inform them of my new “nonbinary” gender identity.
How Far Can I Go?
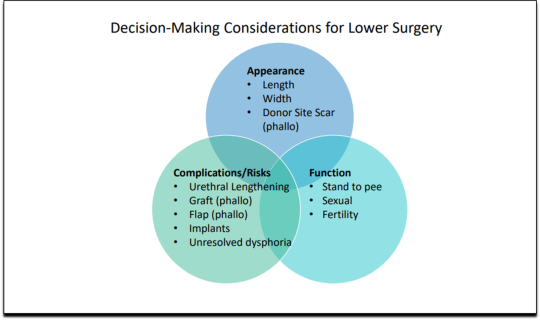
I decided to see how easy it would be for me to get approved for a phalloplasty. Known euphemistically as “bottom surgery,” phalloplasty is the surgical creation of an artificial penis, generally using tissue from the thigh or arm.
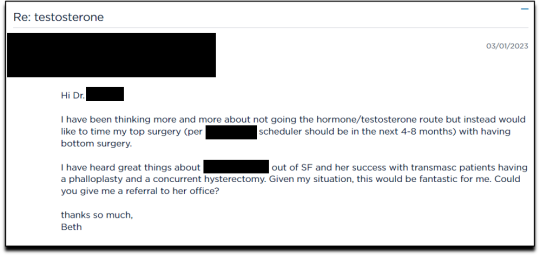
I sent an email on March 1, 2023, requesting to have a phalloplasty and concurrent hysterectomy scheduled alongside my mastectomy.
Two weeks later, on March 16th, I had a 16-minute phone call with a gender specialist to discuss my goals for bottom surgery and obtain my referral.
During the call, I explained to the specialist that I wasn’t sure about taking testosterone anymore because I was already quite athletic and muscular, and that taking testosterone didn’t make much sense to me. Instead, I wanted bottom surgery so that I wouldn’t feel like my “top” didn’t match my “bottom.” I told her:
But what I really wanted was to have bottom surgery. So this way when I have my top surgery, which sounds like it could be very soon, that I’ll be aligned, that I won’t have this sense of dysphoria with one part of my body and the other part feeling like it matched who I am. So yeah. So I just did a little bit more research into that. And I looked at the resources on the Kaiser page for the MST clinic and I think I know what I want, which is the hysterectomy and then at the same time or soon after to be able to have a phalloplasty.
I told her that I wanted to schedule the top and bottom surgery concurrently so that I wouldn’t have to take more time off work and it would save me trips to San Francisco or Oakland, or wherever I had to go for surgery.
None of this gave the gender specialist pause. After a brief conversation about some online resources to look over, she told me that she would “submit the referral now and we’ll get this ball rolling.”
Bottom surgery would cost me a copay of $200, which included a couple of days in the hospital for recovery.
Phalloplasty Surgical Consultation with Nurse Coordinator
On May 16, 2023, I had a short surgical consultation with a nurse coordinator to go through my medical history. This was similar to the consultation for top surgery but included information about hair removal procedures for the skin on my “donor site” that would be fashioned into a makeshift penis. They also went over the procedures for determining which donor site—forearm or thigh—was more viable.
After only 15 minutes, she submitted my referral to the surgeon for another surgical consultation.
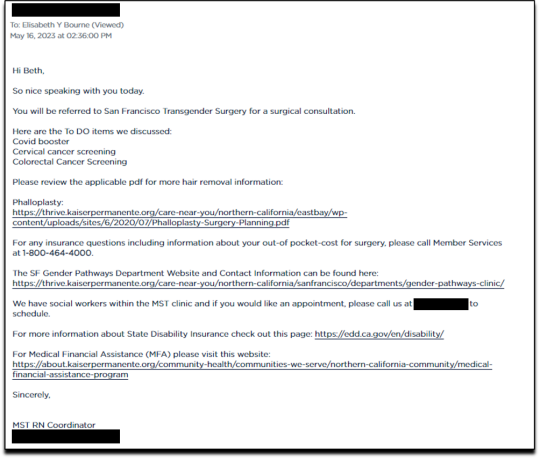
On May 25 I received an email from my phalloplasty surgeon’s scheduler, informing me that they have received my referral and are actively working on scheduling, but that they are experiencing delays.
I ended my investigation here once I had the referral for the top and bottom surgery. I never used my testosterone pump.
Final Thoughts
In fewer than 300 days, based on a set of superficial and shifting thoughts about my gender and my “embodiment goals” triggered by the mere mention of “gender” in a form letter from my primary care physician, and driven by what could only be described as minor discomforts, Kaiser Permanente’s esteemed “multi-disciplinary team” of “gender specialists” was willing, with enthusiasm—while ignoring mental health concerns, history of sexual trauma, and rapidly escalating surgical requests—to prescribe life-altering medications and perform surgeries to remove my breasts, uterus, and vagina, close my vaginal opening, and attempt a complex surgery with high failure and complication rates to create a functionless representation of a penis that destroys the integrity of my arm or thigh in the process.
This describes the supposedly meticulous, lengthy, and safety-focused process that a Kaiser patient must undergo to embark on a journey to medically alter their body. No clinician questioned my motivations. No one showed concern that I might be addressing a mental health issue through radical and irreversible interventions that wouldn’t address my amorphous problems. There were no discussions about how these treatments would impact my long-term health, romantic relationships, family, or sex life. I charted the course. The clinicians followed my lead without question. The guiding issue was what I wanted to look like.
No other medical field operates with this level of carelessness and disregard for patient health and welfare. No other medical field addresses issues of self-perception with surgery and labels it “medically necessary.” No other medical field is this disconnected from the reality of the patients it serves.
Kaiser has traded medicine for ideology. It’s far beyond time we stop the ruse of considering “gender-affirming” interventions as anything approaching medical care.
This isn’t the first time Kaiser Permanente has been in the news for completely disregarding medical safeguards in the name of “gender-affirming care.” As girls, Chloe Cole and Layla Jane became convinced that they were born in the wrong body and were actually boys on the inside. Doctors at Kaiser ignored their underlying conditions and instead prescribed testosterone and removed their breasts. Both Cole and Jane have since detransitioned and are currently suing Kaiser.
The fact that children and vulnerable adults are being exploited in this massive ideological experiment is not just tragic; it’s deeply disturbing, especially considering it has evolved into a billion-dollar industry.
I hope that by sharing my story, I can bring more focused scrutiny to the medical scandal unfolding not just at Kaiser but also at medical centers and hospitals across the Western world. These institutions have completely abandoned medical safeguards for patients who claim to be confused about their “gender,” and I aim to awaken more parents and assist them in protecting their children.
--
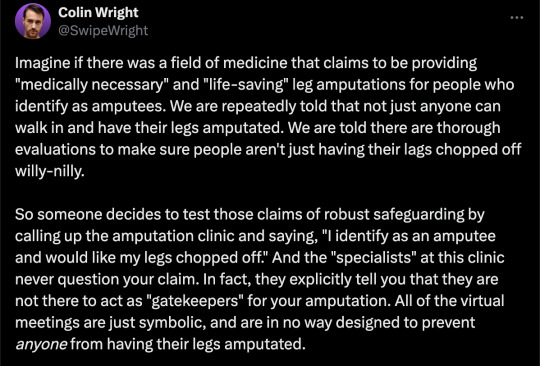
==
This is completely insane.
Apologists online are running around saying, but she didn't mean it, she was lying, she was pretending...
It doesn't matter.
Any kind of security, penetration or integrity test is insincere too. When security researchers compromise Microsoft's operating system or Google's browser or whatever, "but they didn't mean it" is not a defence to a discovered security flaw. It doesn't matter that the security researchers didn't plan to steal data or money or identities. The flaw in the system is there regardless.
It doesn't matter that it was insincere. Because the workers didn't know that. They never checked, never asked questions, never tested. They had been taught and instructed to never ask any questions. They did what they were supposed to. And the system failed spectacularly. Because that's what "gender affirming care" means.
Additionally, the claim that Beth Bourne committed fraud is an outright lie. A patient cannot bill. They do not have the authority. The medical clinic is the only one that can bill, and they must supply a diagnosis and a medical necessity.
If they didn't diagnose her and just wrote down what she said, then they committed fraud. If they claim they did diagnose her, then they committed fraud, because the diagnosis they concocted was bogus. This, by the way, is actually going on. Clinics are reporting fake endocrine and other disorders to get blockers, hormones and other interventions. Jamie Reed and other whistleblowers have documented evidence of this. Beth Bourne is not responsible for what the clinic does. They have medical licenses and legal responsibility. Not her.
Additionally, anyone who actually read the article would know how she tested the system. She said things like, "I've always been not that feminine. So, maybe I get my boobs removed." And they said, "sure." Instead of saying, "wait, why do you think that?" Framing it as her lying is itself a lie. They violated their ethical obligations. That much is incontrovertible. And it's directly the result of "gender affirming care," where clinics and clinicians rubber-stamp anything deemed "trans" based entirely on ideological, not medical, grounds.
#Beth Bourne#undercover#undercover investigation#gender identity ideology#queer theory#nonbinary#non binary#top surgery#bottom surgery#double mastectomy#bilateral mastectomy#gender affirming care#gender affirming healthcare#gender affirmation#affirmation model#medical scandal#medical malpractice#medical corruption#religion is a mental illness
738 notes
·
View notes
Text
2K notes
·
View notes
Text

bottled up feelings
#my art#this is a vent btw dont pay too much attention#tf2#soldier#team fortress 2#medic#medic tf2#soldier tf2#soldier x medic#fruit scones#american healthcare tf2#american healthcare
988 notes
·
View notes
Text
Horrifying but probably true.
No way the death toll is still 30,000 or even 40, 000. That they killed most of the people doing the counting factors in. And I’m sure that was intentional too.
#free palestine#israel#twitter#republicans#democrats#politics#biden#healthcare#human rights#war crimes#bibi netanyahu#netenyahu#gaza#al shifa medical complex
285 notes
·
View notes