#medical research
Text
"A team of researchers at Washington University in St. Louis has developed a real-time air monitor that can detect any of the SARS-CoV-2 virus variants that are present in a room in about 5 minutes.
The proof-of-concept device was created by researchers from the McKelvey School of Engineering and the School of Medicine at Washington University...
The results are contained in a July 10 publication in Nature Communications that provides details about how the technology works.
The device holds promise as a breakthrough that - when commercially available - could be used in hospitals and health care facilities, schools, congregate living quarters, and other public places to help detect not only the SARS-CoV-2 virus, but other respiratory virus aerosol such as influenza and respiratory syncytial virus (RSV) as well.
“There is nothing at the moment that tells us how safe a room is,” Cirrito said, in the university’s news release. “If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know essentially in real time, or every 5 minutes, if there is a live virus in the air.”
How It Works
The team combined expertise in biosensing with knowhow in designing instruments that measure the toxicity of air. The resulting device is an air sampler that operates based on what’s called “wet cyclone technology.” Air is sucked into the sampler at very high speeds and is then mixed centrifugally with a fluid containing a nanobody that recognizes the spike protein from the SARS-CoV-2 virus. That fluid, which lines the walls of the sampler, creates a surface vortex that traps the virus aerosols. The wet cyclone sampler has a pump that collects the fluid and sends it to the biosensor for detection of the virus using electrochemistry.
The success of the instrument is linked to the extremely high velocity it generates - the monitor has a flow rate of about 1,000 liters per minute - allowing it to sample a much larger volume of air over a 5-minute collection period than what is possible with currently available commercial samplers. It’s also compact - about one foot wide and 10 inches tall - and lights up when a virus is detected, alerting users to increase airflow or circulation in the room.
Testing the Monitor
To test the monitor, the team placed it in the apartments of two Covid-positive patients. The real-time air samples from the bedrooms were then compared with air samples collected from a virus-free control room. The device detected the RNA of the virus in the air samples from the bedrooms but did not detect any in the control air samples.
In laboratory experiments that aerosolized SARS-CoV-2 into a room-sized chamber, the wet cyclone and biosensor were able to detect varying levels of airborne virus concentrations after only a few minutes of sampling, according to the study.
“We are starting with SARS-CoV-2, but there are plans to also measure influenza, RSV, rhinovirus and other top pathogens that routinely infect people,” Cirrito said. “In a hospital setting, the monitor could be used to measure for staph or strep, which cause all kinds of complications for patients. This could really have a major impact on people’s health.”
The Washington University team is now working to commercialize the air quality monitor."
-via Forbes, July 11, 2023
-
Holy shit. I know it's still early in the technology and more testing will inevitably be needed but holy shit.
Literally, if it bears out, this could revolutionize medicine. And maybe let immunocompromised people fucking go places again
Also, for those who don't know, Nature Communications is a very prestigious scientific journal that focuses on Pretty Big Deal research. Their review process is incredibly rigorous. This is an absolutely HUGE credibility boost to this research and prototype
#covid#covid 19#pandemic#plague#rsv#influenza#the flu#science and technology#medical research#medical technology#biochemistry#immunology#good news#hope#hope posting
6K notes
·
View notes
Text
“When I share that I was pressured to abort because of Down syndrome, the standard response from the pro-choice crowd is “That is not what pro-choice means. Your choice should have been respected.” But they are missing a crucial point: the pressure from the medical community was not about me. My husband and I were pressured simply because we were an annoying obstacle between our baby and those who’d prefer him dead.”
89 notes
·
View notes
Text
For folks who *haven’t* studied property law, you may not have heard of Henrietta Lacks, a Black cancer patient whose cells were collected by doctors in 1951 and used without her consent for various research projects.
Her body, like the bodies of so many other Black women throughout history, generated massive profits in medical research, was tied to grants, and ultimately patented. Henrietta was never informed, never compensated, and her family has been fighting for decades to see ANY compensation for the lifesaving medical breakthroughs, extensive research opportunities, and obscene amounts of revenue generated by the harvesting of the cancer that would shortly thereafter claim her life.
The legal matter has only *now* been “resolved.”
128 notes
·
View notes
Text
#science#science communication#scicomm#science education#stem#science blog#biology#physics#medical science#health#medical mystery#medical research#genetics
63 notes
·
View notes
Text
28 notes
·
View notes
Text




volunteering for experiments
#ecg#male patient#medfet#electrodes#heart monitor#heart exam#breath control#apnea#medical research#medical volunteering
26 notes
·
View notes
Text

Actors role playing DID can be identified from differences in brain activation patterns, compared to people with DID - and brain activation patterns depend on whether an trauma holder alter / EP is in charge or a Apparently Normal Part / host - supporting the Theory of Structural Dissociation of the Personality (TSDP).
Multiple brain scan studies support structural dissociation, brain activation differences between alters, brain activation differences between people with DID and healthy controls or trained actors pretending to have DID.
Regions of the brain activated are those known to be associated with self-referencing and sensorimotor actions, but not the regions linked to imagination
Schlumpf YR, Reinders AATS, Nijenhuis ERS, Luechinger R, van Osch MJP, Jäncke L (2014) Dissociative Part-Dependent Resting-State Activity in Dissociative Identity Disorder: A Controlled fMRI Perfusion Study. PLoS ONE 9(6): e98795.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3791283/
#neuroscience#medical research#dissociative Identity Disorder#actually dissociative#dissociativeidentitydisorder#did research#A lot is known about DID#structural dissociation#theory of structural dissociation#theory of structural dissociation of the personality#DID evidence#Schlumpf2014#TSDP#actually traumagenic
58 notes
·
View notes
Text
Hey all, so the crowdfund is up for ReachAI. If anyone wants to go check it out it would mean a lot to me! Also you can watch the video there on IndieGOGO or here:
youtube
It should give you a bit of an idea on what ReachAI is and what the nonprofit will be doing as well as the benefits of becoming a donor (which there are even more than I talked about in the video including Webinars, 1-on-1 sessions with me, a newsletter update on research the organization is working on or right now that I am).
I am excited to be bringing ReachAI closer to launch day, I am really hoping I can raise the money to get it started! I know it could do so much good in the world :3
#programming#programmer#artificial intelligence#machine learning#technology#python programming#coding#ai#python#programmers#data science#medical research#medical technology#aicommunity#aiinnovation#Youtube
24 notes
·
View notes
Text
18 hours difference of bacteria growth
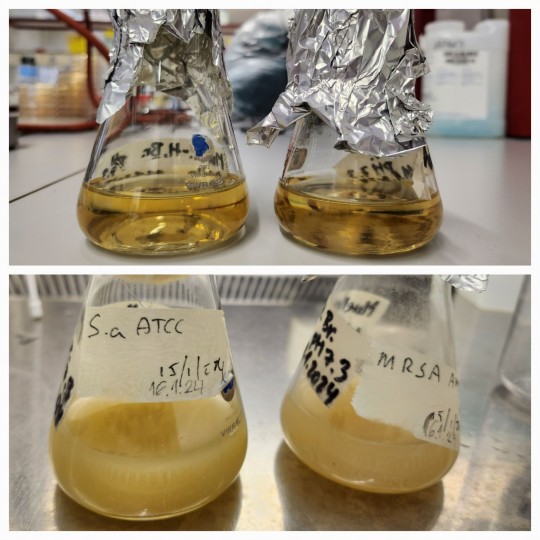
How much can Staphylococcus aureus bacteria grow in less than a day? I add a few drops of bacteria into a fresh medium (basically a meat bouillon soup) and after 18 hours I count tens of billions bacteria per milliliter.
Literally, today I had 8x10^10 bacteria/ml. They grow like crazy when given the chance.
For the next 24 hours, I let them bath in antibiotics. Hehe!
#microbiology#bacteria#MRSA#staphylococcus#antibiotic#science#research#postdoc#crazy#stem#biophysics#academia#medical research#killing time#original content
9 notes
·
View notes
Text
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
random question unrelated to the rest of my blog:
I've never had a symptomatic COVID infection. Over the entire course of the pandemic, I've had two or three mild colds and tested negative each time. I haven't been extremely cautious either, I just seem to have some resistance to the virus. (I have taken all available vaccines but haven't been masking lately, which I know is a bad idea -- I will probably start tomorrow.)
Since like 99%+ of Americans have tested positive at least once, I think that there might be something interesting going on with my physiology, and I'd love to participate in a study about it. Are there any labs trying to find COVID-free volunteers for medical research right now? I could be a control-group patient in a study about Long COVID, or it could be something more direct about immune resistance. Bonus points for research in Illinois.
9 notes
·
View notes
Text
#science#science communication#scicomm#stem#science education#science blog#biology#medical science#medical research#Medicine#biological sciences
17 notes
·
View notes
Text
#science#medicine#medical research#medical advances#pig kidney#kidney transplant#organ transplant#xenotransplantation
20 notes
·
View notes
Text
It is actually quite concerning that many youngsters consider smoking to be cool when it is so dangerous not just to your lungs but also to others. And I'm not addiction-shaming here, I just think we should discourage people from starting to smoke and offer resources to those who are already addicted.
Because new research has found that not only second-hand smoking but also third-hand smoking to have negative health consequences.
"A new study reveals that the residue of nicotine that lingers on surfaces can react with another chemical in the air to form potent carcinogens — chemicals linked to various cancers. While first-hand smoke is that inhaled directly by the smoker and second-hand is the smoke exhaled (and inhaled by others), third-hand smoke is the residue from second-hand smoke."
"The burning of tobacco releases nicotine in the form of a vapor that adsorbs strongly onto indoor surfaces, such as walls, floors, carpeting, drapes and furniture. Nicotine can persist on those materials for days, weeks and even months"
"Smoking outdoors is not much of an improvement. "Smoking outside is better than smoking indoors but nicotine residues will stick to a smoker's skin and clothing""
This even impacts newborns in the NICU!!
"Researchers interviewed parents and family members of hospitalized infants to determine household nicotine use, including conventional cigarettes, electronic cigarettes, and smokeless tobacco. They also collected samples to measure nicotine on visitor’s fingers, on NICU furniture, and in infant’s urine."
https://thirdhandsmoke.org/thirdhand-smoke-in-the-nicu-may-put-infants-at-risk/
69 notes
·
View notes
Link
Researchers from the University of Hamburg, Germany, in collaboration with researchers from Denmark, Canada, the USA, Spain, Slovakia, and Israel, have designed Drugst.One, a platform that transforms complex computational tools into user-friendly, web-based utilities for finding novel applications for existing drugs. With as little as three lines of code, Drugst.One can convert any gene or protein-based computational tool into a powerful, web-based toolkit that helps in visualizing how medicines interact with proteins and diseases, which can aid in repurposing already existing drugs. It has already been implemented with 21 different tools, including ones specializing in drug repurposing for irritable bowel disease (IBD) and investigating the smooth muscle cell (SMC) proliferation pathway.
Due to increasing medical demands, technology, over the years, has advanced and catapulted the emergence of tools that enable the identification of the genes or proteins responsible for a particular disease along with the visualization of their interactions contributing to the progression of the disease. This visualization enhances the precision of pharmaceutical treatments and minimizes side effects. It also enables drug repurposing, which eliminates the expenses required for developing new drugs.
Continue Reading
20 notes
·
View notes
Text
101 notes
·
View notes