#mental healthcare
Text
Palestinian activists in Ontario are asking you to email your reps about Bill 166. The wording of the bill is extremely vague, but it seems like the Ford government wants to open itself the possibility to meddle in mental health services provided by Universities and to change their anti-racism policies. It is very likely - with the timing - that these policy changes are going to be saught to arrest / institutionalize Palestinians for divulge during therapy, or to deny them service altogether. They want to control University campus mental healthcare, something no other province does.


@newsfromstolenland, @vague-humanoid
#cdnpoli#Ontario#post secondary education#mental healthcare#zionism#Bill 166#Doug Ford#Progressive Conservatives#Conservatives#fascism
323 notes
·
View notes
Text
The California Faculty Association is going on Strike against the California State University system!
They are fighting for:
Better pay so they can afford to live in the state they're teaching in.
More manageable workloads to allow for effective student support.
Expanded counseling services to improve students' access to mental healthcare.
All of which should be reasonable, considering:

The CSU's expendable net assets have grown from $3.3 billion in 2012, to $8.1 billion in 2022.
If CSU management funded our bargaining proposals from their annual cash surpluses, they wouldn't even have to draw from these reserves.
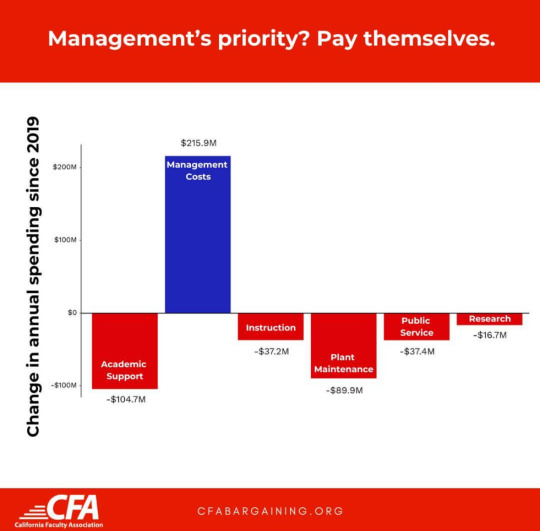
Teachers can do the math, but CSU management is hoping you can't.
#cfa strike#teachers#labor#unions#strikes#education#mental healthcare#california state university#csu#california faculty association#cfa#solidarity forever
67 notes
·
View notes
Text
PSA: Do NOT Get Your Counseling Through Thriveworks
Thriveworks is a provider of psychiatric counseling services. I’d say they’re more of a corporate chain than a clinic (they brag about having hundreds of locations after all). During my year under their “care”:
I frequently found it difficult to contact my psychiatric nurses directly when I had a concern and had to go through Thriveworks to get to them.
I was told that I could not renew my prescriptions without an appointment with my provider even though I had my appointment cancelled on me and was about to run out of antidepressants. The Thriveworks representative then apologized for the “inconvenience.”
I had to change providers three times in one year. More than once it was because my provider was leaving Thriveworks due to their own dissatisfaction with the company and its requirements of them.
Thriveworks providers do not always make it clear that they work through Thriveworks. I did not understand what Thriveworks really was until I was already tied up in the network.
Since I stopped seeing their providers they have repeatedly tried to charge me for services they are no longer rendering.
Only after the first time I complained about frivolous charges did I hear that I was considered a “subscriber” and told that they would cancel my “subscription.” A subscription model for psychiatric care is highly suspicious.
If you are seeking out a psychiatric nurse practitioner and you find out that they work through a service called Thriveworks *please* seek out an alternate care provider. Thriveworks is at best a shady and poorly run business, and at worst a scam.
Stay safe and take care of yourself!
EDIT: they sent me another charge despite telling me my account was cancelled and me not using their services since the fall! I am going to blaze this post.
266 notes
·
View notes
Text
Maybe the problem isn’t people self diagnosing! Maybe the problem is that a professional diagnosis isn’t easily accessible a lot of places! Maybe you could actually do research on how difficult it is to get a diagnosis for so many people! Maybe instead of complaining that people are self diagnosing, you could use that energy to push for better healthcare!!
#self diagnosis#pro self diagnosis#mental health#neurodivergent#mental healthcare#healthcare#neurodiversity#mental heath support#mental wellness#neurodiverse stuff#neurodiverse things#actually neurodiverse#mental heath awareness#mental illness#mental ill health#mentalheathawareness#neurodivergencies
24 notes
·
View notes
Text
Mental health diagnoses are capitalist constructs
“Mental and physical diagnoses aren’t objective facts that exist in nature, even though we usually think of them this way. While the experiences and phenomena that fall under different diagnostic categories are, of course, real, the way that we choose to categorise them is often influenced by systems of power. The difference between ‘health’ and ‘illness’, ‘order’ and ‘disorder’ is shaped by which kinds of bodies and minds are conducive to capitalism and the state. For example, the difference between ‘ordinary distress’ and ‘mental illness’ is often defined by its impact on your ability to work. The recent edition of the DSM, psychiatry’s comprehensive manual of ‘mental disorders’, mentions work almost 400 times – work is the central metric for diagnosis.
“When we look across history, it becomes even more obvious that diagnosis is tied to capitalist metrics of productivity: certain categories of illness have come in and out of existence as the conditions of production have changed. In the 19th century, the physician Samuel A. Cartwright proposed the diagnosis of ‘drapetomania’, which would describe enslaved Black people who fled from plantations. While we might think of drapetomania as a historical outlier among ‘true’ and ‘objective’ diagnoses, it is underpinned by the same logic as other diagnoses: it describes mental or physical attributes that make us less exploitable and profitable. In the 1920s, medical and psychological researchers became interested in a pathology called ‘accident-proneness’, which was applied to workers who were repeatedly injured in the brutal and dangerous factory conditions of the industrial revolution. Dyslexia, a diagnosis I have been given, also didn’t emerge until the market began to shift from manual labour towards jobs that relied on reading and writing, when all children were expected to be literate. Despite having problems with reading, I understand that in a world where reading and writing weren’t so central to our daily life, there would be no need to name my dyslexia, no need to diagnose it.
“As a system of state power, many of us rely on diagnosis to get the material things that we need to survive in the world. When illness or disability interferes with our ability to work, we often need a diagnosis to justify our lack of productivity – and for some, diagnosis is the necessary pathway to getting state benefits. If we want to get access to medication, treatment or other healing practices provided by the state, diagnosis is also the token that we need to get there. This is made all the more complicated by the fact that doctors have the power to dispense and withhold diagnoses, regardless of our personal desires. When it comes to psychiatric diagnosis, most of us know someone who has had to fight or wait for years for a diagnosis that would improve their quality of life – particularly in the realm of autism, ADHD and eating disorders. The internalised racism, sexism, classism or ableism of doctors often gets in the way of our ability to access the diagnoses that we want and need. Then there are those of us that are given diagnoses that we reject, a process that we also have no say in ...
“When we understand that psychiatric diagnoses are constructed, contested, and aren’t grounded in biological measures, the idea of ‘self-diagnosis’ starts to feel less dangerous or controversial. Self-diagnosis is grounded in the idea that, while the institution of medicine may hold useful technologies and expertise, we also hold valuable knowledge about our bodies and minds. I know many people who have found solace and respite in communities for various diagnoses, even if they don’t have an official diagnosis from a doctor. These spaces, which respect the wisdom offered by lived experience, can be valuable forums of knowledge-sharing and solidarity. Self-diagnosis also pushes against an oppressive diagnostic system that is so centred around notions of productivity.”
#anti-psychiatry#psychiatry#psychology#mental health#mental illness#mental disorders#diagnosis#mental healthcare#healthcare#neurodivergence#drapetomania#dyslexia#autism#adhd#benefits#disability#capitalism
69 notes
·
View notes
Text
If you work as a crisis mental health practitioner, and a patient presents to you in mental health crisis, and your response is "what do you want me to do about it?" and that person kills themself because you failed to meet their needs.
You've just committed manslaughter.
28 notes
·
View notes
Text
The Bipolar Brain: An Introduction
Key Terms
Bipolar: Previously called 'manic-depression' due to the nature of the mania being rooted in depression, this mood disorder is characterized by periods of mood shifts between a manic and depressed state.
Depression: A period of rest after deeply distressing events
Dopamine: A brain chemical meant to encourage pleasure, satisfaction, and motivation.
Grey matter: Also known as the cortex of the brain, this is the outer layer of the brain allows a person to have control over movement, memory, and emotions by sending signals between the different parts of the brain.
Hippocampus: The part of the brain where memories are "stored" to later be relayed to other parts of the brain, consciously or not. It is one of the deepest parts of the brain structure, making signals difficult to send or receive.
*Hypomania: A form of mania that is less severe or impactful than true mania.
Limbic system: Processes emotions and behaviors to help other parts of the brain understand survival necessities.
*Mania: A false sense of euphoria, triggered by stress
Prefrontal Cortex: The part of the brain at the front center, which controls decision making, emotional management, and impulse control.
Type 1 Bipolar: Characterized by mania that is more intense and/or frequent than depression.
Type 2 Bipolar: Characterized by depression that is more intense and/or frequent than hypomania; type 2 bipolar people do not experience "true mania".
*For the sake of this post, "mania" will refer to both hypomania and true mania. When the information only applies to true mania, it will be called "true mania".
----------
Part One: Introduction
We will be exploring the development, behavior, and remission of bipolar brains, using information learned from neuroscience, psychology, and lived experiences of bipolar people. The purpose of this is to inform those with Bipolar how to understand their own brain and take control of the disorder. This post is written by someone diagnosed with Bipolar 2, receiving treatment in the form of medication and talk therapy.
----------
Part Two: Development
This mood disorder usually develops in childhood, but can develop at any point in a person's life. It is caused by trauma, as a response to stress. Most bipolar people also have family with the disorder, implying it is genetically predisposed.
In childhood, this disorder can begin to show symptoms as early as early adolescence. Children as young as 5 have been diagnosed with early onset bipolar disorder.
After traumatic events, such as abuse, neglect, or loss, the brain is forced to find a way to cope and manage complex stress. Trauma can range from mild to severe, and still trigger the onset of bipolar disorder.
During depression, the brain "mines" for dopamine, and during mania, the brain utilizes the dopamine. Over time, without treatment, the bipolar brain will struggle to maintain an effective dopamine-mining system, and these changes will even destroy grey matter in the brain, namely in the prefrontal cortex. This change in the brain makes it more difficult for the prefrontal cortex to communicate with the limbic system, causing less control over emotions and impulses, therefore causing more reckless decisions to be made.
Due to the nature of the relationship between the prefrontal cortex and the limbic system, these two parts of the brain need strong communication. With limited grey matter, signals are weakened, or missed completely.
The hippocampus is a major part of the limbic system, and without a proper connection to send signals between the hippocampus and the prefrontal cortex, it only becomes more difficult to recall past experiences or learned skills.
The longer a bipolar person goes without treatment, the worse their stress, and the worse they respond to stress. This disorder is degenerative, and those with Type 1 Bipolar show the most loss of grey matter.
----------
Part Three: Behavior
Like a pendulum, bipolar brains swing between manic and depressive sensations and behaviors. Here are some characteristics of mood swings:
When depressed, the bipolar person attempts to "fill the void", also known as "dopamine mining". This behavior accumulates dopamine over time but does not release it. This can look like sleeping a lot, escaping into a piece of media, or fixating on an accessible hobby.
During manic swings, the bipolar person uses the dopamine accumulated during depression to compensate for the time lost and labor neglected during depression. This may look like addressing the issue directly in hyper-fixation, or avoiding the issue altogether to indulge in self-pleasure.
Episodes are different than swings. Episodes can be placed on a specific timeframe, sometimes down to the hour. Behaviors are impulsive, emotions are overwhelming, and the decisions made during episodes reflect this heavily. Below are some characteristics of a Bipolar episode, based on type of episode.
In depressive episodes, the bipolar person will display their usual depressive behaviors at a more intense, more frequent rate, and will quickly begin taking on self-destructive behaviors in an effort to punish the self for failing to meet manic expectations. Essentially, the body has gotten used to using depression to recover, and if results are not met, the body "doubles down" as a means to "force" results, in an effort to trigger mania.
Manic episodes are intense highs, often causing changes to the bipolar person's life that normally wouldn't be considered, let alone acted on. There is a false sense of euphoria that controls the impulses and emotions of the bipolar person, causing a disconnect from reality that can lead to delusions and the development of compulsive thoughts or behaviors that enable more poor stress management skills, such as overspending or reckless sexual activity.
Mixed episodes can sometimes be the introduction or ending to a manic or depressive episode, but can also happen alone. The depression attempts to self-destruct while the mania's euphoria makes those behaviors seem euphoric and desirable. These episodes are often painful and typically short-lived compared to the other two, but not necessarily so.
----------
Part Four: Remission
There is a number of ways to treat bipolar brains, though medications and talk therapy, namely CBT and DBT, are the most commonly recommended. Some bipolar brains are medication resistant, so diligent habit seeking and a strong relationship with a therapist may be the best help. Below is an incomplete list of potential treatments, and why they work.
Medication can alter the chemical changes in the brain which trigger swings and episodes. Medication will not heal the brain, it will only control it while properly using the artificial chemicals. Medication plans must be specified to the patient, so trial and error is a necessary process for disordered medicated brains.
Talk therapy flexes the grey matter, and the grey matter may even be recovered in these thought exercises and memory training sessions. These changes are more likely to have a lasting impact, so long as the new habits and beliefs remain.
Diligent habit seeking, centered around self-care and growth, will help a bipolar brain take control of how they treat their stress. While swings may be unavoidable, building a set of healthy habits can alter the way these swings are 'engaged with', meaning behaviors can change. This can be a difficult form of treatment for bipolar people, as the disorder does not consistently provide motivation for habit changes. With a healthy outlook on relapses, this issue is resolved, and habit-seeking can continue even with relapses present.
Healthy coping mechanisms to replace mania are great ways to prevent manic episodes and swings, which will in turn prevent the 'need' for a depressive swing (to recover from manic burnout). These coping mechanisms can look different for each person, but no matter what, these mechanisms must be focused on growth - not escapism, passivity, or indulgence, which are manic behaviors that have been individualized.
Remission looks different for everyone, but no matter what, bipolar is a lifelong disorder. This means that even after years of successful treatment, with no swings or episodes, this disorder is almost guaranteed to make a comeback during high stress situations like abuse or loss. Anyone who has been diagnosed with bipolar should expect to keep their coping mechanisms going for life, and adjusting the mechanisms according to the needs of the changes in their life. There are a few things remission can grant a person, such as:
The ability to work on projects and tasks irregardless of current mood
Motivation to socialize even when the body seeks isolation, making relationships stronger and more consistent
A lack of shame for the disorder or what it has put you through, making stress management less about the desired results and more about the desired process
----------
Part Five: Conclusions
There is no known cure for bipolar disorder, but those with bipolar can take control of their circumstances in small but life changing ways. The bipolar brain is simply trying to thrive even in stressful circumstances, and has only learned one biochemical pattern to do so. Treatment is all about re-training the brain's response to stress. Those who have bipolar must stop identifying with their bipolar to effectively treat it, meaning they cannot embrace their mania as 'the best version of themselves' nor the other way around with their depression. These are not personality traits, because this is not a personality disorder; these are conditions the brain is currently in.
People with bipolar disorder are not to be ashamed of themselves for what they've done to cope during depressive swings or episodes. Shame is often what maintains the cycle, as this is a major driving force of impulsive behavior. The guilt, shame, and self-loathing of a bipolar person will hold them back from developing better ways to manage stress. With an effective, individualized treatment plan, bipolar people can find themselves in remission, but should expect and accept relapse if a major stress is to occur. This is not because the treatment isn't working anymore, but because this is how the brain has developed to respond to stress, and until we find a cure, bipolar brains are to be respected as brains attempting to thrive in unforeseen circumstances - a worthy pursuit that any self-loving person would take on.
----------
Additional notes:
Comorbidity with other mental conditions can cause symptoms to be more intense or more frequent. This includes conditions like PTSD, personality disorders or autism.
Many bipolar people seem to believe that their mania "helps them" - with things like getting projects and tasks done, or socializing. This is false. Mania is what uses the energy accumulated during depression to delude the bipolar person into thinking that the only way for them to get these things done is to indulge in manic behavior. Essentially, the bipolar person is the one helping themselves get their projects and tasks done, and mania is "taking the credit".
If you have been diagnosed with bipolar disorder, you have a strong will to thrive. Trust in this, and rely on that fact to help you change your habits so that your stress management system can adjust to a more stable, secure structure.
You must read the sources for a detailed look at the different topics and ideas shared here. This post is that of my own conclusions, based off of the information in these links plus my own experiences with Bipolar Type 2. I am not a professional, and this post should not be taken as mental health advice, but rather, an exploration from an unprofessional point of view. If you need mental health advice, seek therapy or psychiatric care, and take this information to them to see how it may apply to your life.
----------
Sources:
Bipolar experiences
Dopamine & Bipolar Relationship
Grey matter information
Hippocampus information
Limbic System information
Mania & Hypomania
Mixed episodes
Prefrontal Cortex Walkthrough
#bipolar#bipolar disorder#brain health#bipolar brain#hypomania#mania#depression#manic depression#brain structure#brain development#bipolar episode#mental health#mental healthcare#psychiatry#neuropsychology#psychology#neurology#bipolar treatment#bipolar type 1#bipolar type 2#my essays#my posts
53 notes
·
View notes
Text

I know I talk a lot about issues within inpatient psychiatry and how they affect the patients (and this should frankly be the #1 priority), but I think how these issues affect the staff is important too. This paper goes into moral injury amongst psychiatric hospital staff in depth, and is the only systemic analysis I've been able to find on the topic.
Some quotes from staff members that I found particularly striking:
"The medicalisation approach of care for psychiatric patients has overlooked the principles of “care” in the context of nursing, and consequently the emphasis seems to have shifted more towards safety management. . ."
"What stops me from acting was I am part of a team . . . if I intervene in these situations I’m interfering with primary nursing, and I think I would be seen as splitting the team by taking the side of the patient."
"When I expressed my concern over what seemed like a blatant error in diagnosis, my instructor . . . who I held in really high esteem . . . just said “Docs don’t misdiagnose . . . there’s no misdiagnosing here,” and I was thinking, “Are you kidding me? Like, isn’t that against everything we’ve ever learned about critical thinking and looking at the specifics and questioning. . .?”"
"It’s not to be taken lightly when you put your hands on somebody. It’s wrong really. It’s like the opposite of therapeutic touch."
"I run to another ward when we hear the assault alarm and find a half-naked woman lying on the floor. As I understand it, the patient has “moved into top gear” and will be given an injection. . .. I’m distressed about the woman lying there half naked (why didn’t anyone think of covering her with a blanket?)"
Most of what the article discussed in the "implications for practice" section is about giving psychiatric healthcare workers more avenues to report immoral acts, along with trainings on how to deal with moral injury, but I have another takeaway. Both patients and staff are traumatized by this system. Why aren't we fundamentally changing something?
(Additionally, this system is perfect for burning out staff that have strong ethics and leaving the abusive staff to run things. So there's issues on both a systemic and individual level.)
#psychiatry#mental healthcare#inpatient psychiatry#moral injury#psychiatric abuse#abuse cw#public health#psychiatry critical#psychiatric nurse#psychiatric staff#mental health nurse#psych ward#psych hospital#tfw a cool epic paper came out JUST A FEW MONTHS AGO WOOOO#why is everyone not clambering over themselves to give this post notes. Surely there is something wrong with them and not me
12 notes
·
View notes
Text
people hear that i'm anti-psych on a lot of levels and they immediately assume that it means that i hate therapy and that i think that no one should be allowed medical treatment and blah blah blah
but that's so wrong???
firstly) i prioritize completely informed consent and autonomy. a lot of health care professionals don't, esp in mental healthcare.
secondly) i acknowledge the good that mental healthcare can do, but the system is majorly fucked and trying to find good care that is what you need is like finding a light blue needle in a stack of dark blue needles; you end up hurt a thousand times before you even get close to finding what you need, not to mention that they all look pretty similar so you could end up with a dark blue needle and get fucked up w/o realizing it
thirdly) not everyone has/needs/wants mental healthcare. which is fine, until you need/have/want mental healthcare and people stop talking to you/crap on you/etc etc bc it's so stigmatized
fourth) look all of my points boil down to completely informed consent, autonomy, and how much the system sucks.
i'm not anti-people-getting-the-care-they-need, i'm anti-the-current-psychiatric-system. cause it sucks and is inherently biased and shitty and sure it makes progress but at a snail's fuckin pace which doesn't help the people stuck in it now
#disability#mental disorders#disabled#mental disability#mental health#mental healthcare#anti-psych#anti psych#anti a lot of shit the current system sucks in a lot of ways#and just because it's somewhat better than ut used to be#doesn't mean that we should stop pushing for reform
5 notes
·
View notes
Text
Mental illness should never have to be terminal
#mental illness advocacy#mental illness representation#mental illness#mental healthcare#mental health#accessibility#mental health matters#healthcare reform#bpd#borderline stuff#borderline personality disorder#did osdd#traumagenic#trauma recovery#complex trauma#cptsd healing#audhd#adhd autistic#late diagnosed autistic#neurodiversity#cptsd recovery#depression anxiety#manic depressive#manic episode#depressive episode
5 notes
·
View notes
Text
Kathrin Mentler knows British Columbia’s mental health system inside and out.
She knows it academically because she’s studying to become a counsellor with the goal of working as a peer support worker. She also knows it personally because she’s experienced rounds of depression and anxiety throughout her life.
Mentler says she has accessed suicide prevention services dozens of times while experiencing mental health crises. She has also attempted suicide more than once and woken up in an intensive care unit, overwhelmed with gratitude for the hospital staff who kept her alive.
“I live with chronic suicidal thoughts but that doesn’t mean I never feel joy in my life,” she says.
This spring Mentler found herself in crisis and took herself to Vancouver General Hospital’s Access and Assessment Centre to get help. [...]
Continue Reading.
Tagging: @politicsofcanada
353 notes
·
View notes
Text
“A lot of what happens in psychotherapy — the most important curative factor in psychotherapy is the relationship with the client,” said Blauner, who’s been a therapist for more than 40 years.
Ending therapy is the end of an important relationship, and it’s crucial to give ample notice so that the therapist can help their patient process their feelings about the change and discuss how to move forward, Blauner said.
Any termination of care should be “planned for, discussed openly in treatment, and be an essential aspect of the treatment process that assists the client toward effective independent functioning,” wrote Jeffrey Barnett and Caroline Coffman for the Society for the Advancement of Psychotherapy.
Wow, fuck Headspace! I’m so glad I ditched that a long time ago.
If you’re in crisis, that’s ok! The 988 lifeline, Trevor Project, and Trans Lifeline are here to help.
If you’re not in crisis but still need some help, that’s ok too, look for Wysa in your mobile device’s app store.
18 notes
·
View notes
Text
I am waiting for the day someone tells me my portrayal of Treech is [_]-coded because mental health care is a nightmare and he is me. I write him as me. Maybe someone can tell me what the hell is wrong with me based on how I write him because I project onto my circus boy so hard it’s not even funny.
#that’s a lie#it’s very funny#the ballad of songbirds and snakes#tbosas#the hunger games#10th hunger games#hunger games#treech tbosas#tbosas treech#treech#treech thg#mental health#mental healthcare#sucks#fic coming about that maybe we’ll see#i’ll post the AU tho!!
6 notes
·
View notes
Text
Part of me wants to think that there's no way that Joker: Folie A Deux could possibly be worse -- meaning more triggering -- than the first one is, but then I remember that it's set in motherfucking Arkham Asylum. And as someone who has spent time in an asylum -- sorry, transitional housing program -- I can tell you that it's unfuckingpleasant. And here's a thought:
What if Todd Phillips made it a musical, so that it would be less traumatizing?
Cause that's a thing they do in psych wards -- they play music to help you cope and it works really well but SHIT. Like I kind of really want this movie to blow the whole fucking lid off of the mental healthcare industry. I want it to show how high functioning patients have their health problems downplayed and overlooked in favor of the more dramatic patients. I want it to show how you have to play along, never losing your temper and assuaging some fucking doctor's or therapist's ego so that you don't get labeled a difficult patient. Cause once you're labeled difficult you either end up discharged or strapped to a fucking gurney with a syringe in your arm.
Or how some doctor's literally use their patients as free fucking advertising for new meds.
"Oh, that antidepressant you're on hasn't been working -- well, I just got this brand new one in. No, it doesn't matter that it's only been a month. Take a sample and come back three months from now."
But also having seen the first one......JFC, I just know it's going to be absolutely nightmare inducing.
#comic books#graphic novels#dc comics#dceu#dcu#dc universe#dc movies#batman#the joker#joker folie a deux#mentally ill#mental healthcare#actually mentally ill#mental health awareness
4 notes
·
View notes
Text
Here's a hot take and a hard take for all the ipad babies on social media;
Being able to even apply for disability, snap, food stamps, or social security is in of itself white and/or mentally-abled privilege.
When you are so mentally disabled from constantly-worsening PTSD (due to poverty/trauma/abuse you cannot escape) that you break down screaming at the top of your lungs and bawling uncontrollably when put under any amount of stress or pressure or have to answer direct questions, you are literally not able to apply for benefits or help.
Full Stop, you need to wake up, grow up, and realize this reality for the neurodivergent.
Even if you are privileged enough to HAVE a caretaker or PoA, government officials and offices REFUSE to speak to anyone EXCEPT FOR YOU-- DELIBERATELY PROHIBITING mentally disabled people from being able to have assistance.
If you are incapable of self-advocating or mentally functioning enough to talk to these people who are constantly antagonizing, verbally abusing, and pushing forceful and willful and deliberate undue burden on you to make you give up, then you are put in the position I am in
You just. Fucking. Die.
Then I get little pretentious white kids who were born into money telling me that it's sooooo easy to get on disability because it was easy for THEM. Because.. they... were born into. Money.
Why do rich kids literally not get this?? Why is this such a difficult concept for you? If you were born even into middle-class wealth, you are extremely privileged. If your parents did not abuse you, you are extremely privileged.
If you are so traumatized you cannot do anything except drown in distractions or else be trapped in a screaming-crying death spiral, how exactly are you supposed to survive living in poverty in the USA? Hmmm? I am fully handicapped. I am fully disabled. Both mentally and physically. I can't sleep, I can barely eat, and I cannot talk to strangers. I can't make it a single day without at least 2-3 suicidal meltdowns.
I am already on the highest amount of psychiatric medication that I am allowed to be on for medical reasons and I am about to lose it entirely due to what was done to me costing me my healthcare. I cannot afford therapy. I cannot go to a doctor, anymore. All of that was taken away from me.
So what do you do as a severely suicidal, disabled, handicapped, mentally ill, completely non-functional trans person who has had their entire life, livelihood, livability, income, healthcare, medications, groceries, hope, dreams, plans, future, pets, house, transportation, mobility assistance devices, gender-affirming care, trans surgeries, testosterone, and entire purpose for living ripped away because of selfish, ignorant white abled people?
The government is not here to protect or save me. What has happened to me us the absolute EPITOME and PROOF that this "justice system" is deliberately and specifically engineered as a weapon of GENOCIDE for people in my categories and they hand selfish, white fascists everything they want when they are bored of people like me without a second thought.
What has happened to me is not an Accident. It was Deliberate. Purposeful.
Everything that has been done to me has been for the explicit act of getting rid of me-- permanently. Because that is what the USA cultivates, grooms, and enables. This is the prerogative of white privileged people in this country; Exterminate people like me.
How the USA and its citizens responded to Covid-19 RUINED MY ENTIRE LIFE and my entire FAMILY is just DYING. We already lost two of our housemates. Dead. FOREVER. My fucking FATHER to cancer we couldn't afford to treat and FATHER FIGURE due to my abrupt and unfair eviction. GONE.
Because of this country and what People decided to do to Me. Now the rest of us are going to die one by one.
Because of the Genocide System of America.
And you're just going to stand there and watch us starve to death or die of cancer or desperate suicide to end the suffering and torment we have been forced into.
There is NO HELP for the TRULY DISABLED.
If you are disabled and have ANY financial aid-- you're privileged as FUCK.
If people do not start Donating To My Family, we will not make it even two more months and that's GENEROUS.
If you think that "money raised" number means we are okay-- WRONG. All that money is GONE. This fundraiser has been going on for months and alot of it went to bills. We are BROKE. We have NOTHING. Wake. UP. Give us REAL HELP. We are DYING. HELLO.
#poverty#disability#financial aid#government#starving#trans#trans healthcare#disabled artist#abandoned#killed#left for dead#handicapped#neurodivergent#bpd#actually bpd#autism#ptsd#adhd#neurodivergence#mental healthcare#healthcare#trying to survive in the USA the Genocide Country#*satisfy me
13 notes
·
View notes
Note
whats up with therapists that refuse to give people a diagnosis? i dont really get the logic behind "i dont like to label my patients".
I don't get it 100% either, but I do have some guesses?
Given that many of MH professionals who refuse to diagnose say stuff like "I don't want you limiting yourself with labels!!", I think they believe that by diagnosing someone with, say, BPD, that they'll think "I have BPD and that is all I am as a person and I cannot and will never change", and that they'll then become treatment resistant and a "difficult" client. They think the solution is to never give them a diagnosis so they never have an oppertunity to use it as an "excuse", I guess. I've also heard many of them say they think it's a "self fulfilling prophecy" where the client will "Google the symptoms of the disorder and then start lying or exaggerating their symptoms to fit in with the label"...which is and awful thing to say about someone who just wants an explanation for their symptoms.
A lot of MH professionals also buy into the very ableist rhetoric of "separate the person from the illness!!! person dealing with a mental health difficulty not mentally ill person!!", and think that acknowledging that a person is mentally ill is this beyond horrible thing that makes the person less than human.
They don't have respect for their clients' rights to information about their mental health, and choose to hide the very crucial information of what the client's diagnosis is based on their own opinions of "oh but then they'll just blame everything on the diagnosis and become difficult" or "mental illness is bad so I cannot associate it with a person in any way without dehumanizing them, I cannot treat them as if they are ill, I have to treat them as if they are just sad sometimes." They don't care that knowing the name of the diagnosis provides community, better access to appropriate healthcare, an easier time advocating for yourself in treatment, self understanding and acceptance, etc.
So to sum it up, I believe it's combination of underlying saneism in MH professionals and them caring more about the possibility of their clients being "diffcult" than their clients having access to crucial and life saving info about their own health that allows them to find community and self understanding, as well as assisting their own treatment and being able to advocate form themselves with MH professionals.
Also related that I've literally only ever seen this attitude in neurotypical MH professionals, literally never in mentally ill or otherwise neurodivergent ones.
#mental illness#mental health#neurodivergent#ableism#saneism#mental healthcare#psychology#psychiatry#mentally ill#actually mentally ill
3 notes
·
View notes