#organ donation
Text
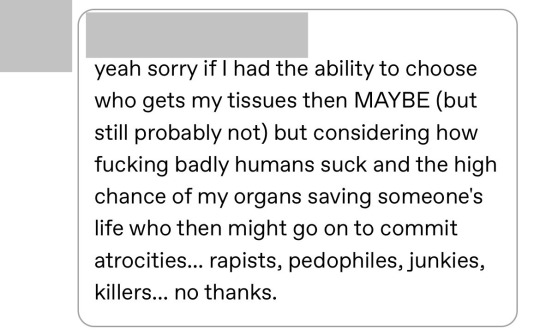
If you don’t want to donate your organs that’s your body your choice whatever I’m not gonna hassle you but this is SUCH a horrible way to view your fellow humans. If one of my kidneys saves a sick kid but the other saves a guy serving a life sentence for double homicide, I’m still taking that deal without question. Not wanting to donate because you might save the “wrong” life is wack.
408 notes
·
View notes
Text
Data spanning from 1995 to 2021 in India revealed a striking gender imbalance in organ transplants, with four men getting organ transplants for every woman. A total of 36,640 transplants took place in this period, out of which 29,000 were for men and 6,945 for women.
This substantial difference is attributed to a complex interplay of economic responsibilities, societal pressures, and deeply ingrained preferences.
Dr Anil Kumar, director of the government-run National Organ & Tissue Transplant Organisation (NOTTO) highlighted this significant aspect of the organ donation landscape.
While more men contribute as cadaver donors, a staggering 93 per cent of total organ donations in the country come from living donors, he told the Times of India newspaper.
This hints at a trend: a majority of living organ donors are women.
Socio-economic factors a driving force for women donors?
A study published in the Experimental and Clinical Transplantation Journal in 2021 delved into the intricacies of living organ transplantation in India.
The findings showed that 80 per cent of living organ donors are women, predominantly wives or mothers.
The socio-economic pressure on women to assume caregiving roles within the family emerges as a primary factor, compelling them to step forward as donors.
Men's reluctance in surgery
In many cases, men, often the primary breadwinners, hesitate to undergo surgery, contributing to the gender gap in organ recipients.
The study highlights that when the recipient is a male breadwinner, family members, especially wives or parents, feel a heightened responsibility to donate organs.
Emotional dynamics
The emotional dynamics surrounding organ donation are intricate. Women recipients, in particular, may experience guilt when their family members, especially wives or mothers, become donors.
This reluctance leads to a scenario where women recipients may find themselves on waiting lists.
Notably, Karnataka has topped the charts in organ donation in the past decade. The number of donations have risen from 102 in 2013 to 765 in the first 10 months of 2023.
A user on Ovarit added this helpful context:
"Just a little more context to this: men produce male-specific proteins (on the Y chromosome) which often get rejected by women's bodies. Since males have an X chromosome, their bodies recognize proteins from female donors. This makes it more difficult for women to receive male tissue/organs, while still being acceptable candidates for donating to men. Even still, these ratios are very disproportionate".
"As women we absolutely need to be aware of our vulnerability of being used as spare parts in a man's world. Especially when we are being socialized into believing that we need to sacrifice our bodies and lives for others- and society has developed a sense of entitlement to this sacrifice, while downplaying the suffering of women."
#organ donation#marxist feminism#India#women's rights#feminism#global feminism#intersectional feminism#women's oppression#patriarchy#sex-based oppression#gender critical#gender critical feminism#radblr
606 notes
·
View notes
Text
"For the first time, genetically modified pig kidneys provided “life-sustaining kidney function” during the course of a planned seven-day clinical study—a first step in addressing the critical crisis worldwide of kidney donor organ shortage.
The University of Alabama’s pre-clinical human study at Birmingham also advances the science and promise of xenotransplantation as a therapy to potentially cure end-stage kidney disease—just as a human-to-human transplants can.
“It has been truly extraordinary to see the first-ever preclinical demonstration that appropriately modified pig kidneys can provide normal, life-sustaining kidney function in a human safely and be achieved using a standard immunosuppression regimen,” said UAB transplant surgeon scientist Jayme Locke, M.D., director of UAB’s Comprehensive Transplant Institute and lead author of the paper...
The peer-reviewed findings published last month in JAMA Surgery describes the pioneering pre-clinical human research performed on a recipient experiencing brain death...
The pre-clinical human brain death model developed at UAB can evaluate the safety and feasibility of pig-to-human kidney xenografts, or transplants, without risk to a living human. It is named for transplant pioneer Jim Parsons, an organ donor whose family generously donated his body to advance xenotransplant kidney research, like the latest patient did.
A Critical Need
Kidney disease kills more people each year than breast or prostate cancer, while more than 90,000 people are on the transplant waiting list. More than 800,000 Americans are living with kidney failure and 240 Americans on dialysis die every day. The wait for a deceased donor kidney can be as long as five to 10 years, and almost 5,000 people per year die waiting for a kidney transplant.
Groundbreaking Study Details
The 52-year-old study subject for this research lived with hypertension and stage 2 chronic kidney disease, which affects more than one in seven U.S. adults, or an estimated 37 million Americans. As part of this study, the subject had both of his native kidneys removed and dialysis stopped, followed by a crossmatch-compatible xenotransplant with two 10 gene-edited pig kidneys, or UKidney.
The transplanted pig kidneys made urine within four minutes of re-perfusion and produced more than 37 liters of urine in the first 24 hours. The pig kidneys continued to function as they would in a living human for the entirety of the seven-day study. Also, the kidneys were still viable at the time the study was concluded.
“In the first 24 hours these kidneys made over 37 liters of urine,” said Dr. Locke. “It was really a remarkable thing to see.” ...
Gene editing in pigs to reduce immune rejection has made organ transplants from pigs to humans possible. The natural lifespan of a pig is 30 years, they are easily bred, and they have organs of similar size to humans. Genetically modified pig kidneys have been extensively tested in non-human primates, and the addition of UAB’s preclinical human research model—the Parsons Model—now provides important information about the safety and efficacy of kidneys in human transplant recipients."
-via Good News Network, September 17, 2023
#organ donation#organ donor#organ transplant#medical news#medical research#pigs#kidney transplant#kidney diseases#dialysis#good news#hope#hope posting#human biology
545 notes
·
View notes
Note
How do you think morphing technology would affect organ donations when people can morph into other people who are perfect matches of donor hosts and then have their organs removed and survive
I love this idea. It's just gross and impractical enough to feel like it fits with the realism of Animorphs, while still being the kind of thing that would be world-changing for health care. IMHO it makes more sense than the government letting everyone morph in lieu of health care — there are all kinds of security and health insurance groups that would throw up huge barriers to that idea — but it would still be huge.
Assuming there's a strict vetting process for who gets the morphing ability, you could have ~100 people who agree to acquire and morph ~100 patients a year in order to give them organs. There'd be tremendous risk involved, of course, since even a routine surgery to remove a kidney can go wrong. But you could compensate the morpher accordingly, and put limits on type of donation. (For example, I hate to say it but this wouldn't work for heart or lung transplants.)
This makes perfect sense as the kind of horrible-but-wonderful new job that would spring up in the aftermath of the Yeerk-Human War.
336 notes
·
View notes
Text
When Liam Dee began receiving hospice care shortly after starting his nursing career, he knew the rare cancer that had ravaged his body meant his organs were too damaged to donate. But the 26-year-old was grateful his tissues, including skin, corneas, tendons and bones, could still go to people who needed them.
However, his tissues were rejected when he died last November, said his mother Cindy Gates-Dee, who learned from reading her son's medical records that his "homosexual status," as noted on a screening form by a tissue specialist, meant he was declined as a high-risk donor because he'd had sex with another man in the last five years.
But neither she nor Dee's husband was asked any questions about Dee's lifestyle to determine the probability of high-risk behaviour that specialists believe lead to increased risk of HIV or hepatitis B and hepatitis C, Gates-Dee said from Aylesford, N.S.
Full article
Tagging: @politicsofcanada
#cdnpoli#canadian politics#canadian news#canada#canadian#organ donation#homophobia#medical homophobia#medical discrimination#nova scotia#death tw
285 notes
·
View notes
Text
For more than a century, scientists have tried to transplant the kidneys of animals into humans.
For more than a century, they have failed to get those organs functioning.
Now, researchers at the University of Alabama are claiming a first.
They have taken the kidneys of a genetically modified pig and successfully transplanted the organs into a brain-dead patient with the permission of his family.
Scientists have tried this before with some success, but what sets the current case study apart is that the pig kidneys quickly made urine and cleared the patient's body of creatinine.
Creatinine is a broken down part of a waste product produced mainly by our muscle cells and it can only be removed from our bodies via our kidneys through urine. So these are crucial measures of kidney function required to sustain life.
No one had succeeded in providing reliable measurements to both before.
Continue Reading.
158 notes
·
View notes
Text
I don't understand why so many people are unwilling to donate organs after death.
Donating a kidney or something while alive is quite a big step so I get why that's not as popular as it could be. But if you're dead?
Some people have religious reasons and while I still don't really agree I can understand it. But there are a lot of people (here at least) who are not religious but are still unwilling to donate organs. Why???? You don't need them if you're dead. They'll just rot or be cremated. You could save several human lives by donating them without having any reason not to.
52 notes
·
View notes
Photo

1K notes
·
View notes
Text

185 notes
·
View notes
Text

Bet this wasn't on the news.
On the left is Hagit, a religious Jew from Lod who planned to donate her kidney to her friend Yochi. On the right is Myaser, a religious Muslim from Akko who planned to donate her kidney to her husband Rifad. Both of them ended up not being a match for organ donations, but they were both matches for donating to others, and so they did.
Hagit donated her kidney to Rifad, and Myaser donated her kidney to Yochi!
Refuah Shleima to them all
54 notes
·
View notes
Text




Was really feeling myself today.
#personal#myself#me#my face#selfie#liver transplant#organ donation#organ donor#organ transplant#words#girls with red hair#girls with tattoos#sober journey#soberliving#sober#sob
24 notes
·
View notes
Text
youtube
India: 80% Organ Donors Women; 80% Organ Recipients Men | Vantage with Palki Sharma
Transcript:
Now let's talk about something that's seldom discussed: organ donation in India. One person is added to the organ donation waitlist every 10 minutes - one person every 10 minutes. It tells you how grave the situation is.
Turns out it also has a gender problem and this is according to the latest data that has come out. Four out of five organ donors in India are women. What about those who receive organs? Four out of five recipients in India are men; in other words 80% of the donors are women but 80% of the recipients are men. So why are these numbers so skewed? Our next report tells you.
Last December Indian politician Lalu Prasad Yadav underwent a kidney transplant. Sounds like a normal procedure a simple transplant surgery but it made headlines everywhere. Why? Because the donor was his daughter Rohini Achara. It was shown as a story of sacrifice; a daughter doing what she could to save her father.
The optics were great but data suggests this is the reality of India's organ donation. It's all about sacrifice and usually it's about sacrifice by women. A recent study analyzed organ donations from 1995 to 2021. 36,640 transplantations were carried out in India; 29,000 of them were for men only. 6,945 were for women. If you put those numbers into perspective basically men were 80% of the total recipients for organ donations but when it comes to donations it's a completely opposite scenario.
Women make up for 80% of the organ donors and who are these women? They are usually wives or mothers when their son or husband needs an organ they are the first to volunteer which makes them living organ donors. You see, organ donation is easier between family members this means they are genetically easier this lessens the risks of rejections but what explains this disparity?
Well the answer is socioeconomic pressure in our society. Men are seen as Breadwinners; women on the other hand are seen as caregivers. More often than not they feel pressurized to donate their organs. On the other hand men think twice in a situation like this; they hesitate to go into surgery which means most men donors in India are cadaver donors. That means they donate their organs only when they're dead.
These are stories that make for great headlines: a mother giving a kidney to her son, a wife giving her liver to her husband. They are shown as the Messiah of sacrifice and it's society that is to blame for this. Organ donation shouldn't happen under any sort of pressure it should be a choice that one should take freely.
That said the whole picture isn't too great also India's organ donation rate is quite bleak. It stands at 0.52 per million people. Every 10 minutes one person is added to the waitlist. In 2022 over 2 lakh patients needed a kidney transplant. Guess how many got it? It was only 7,500 people. That's just 3.4% so you get the gist the numbers are bad which is why more people need to step up not just women but more people should be open to donating organs. It's an act that saves lives.
#india#organ donation#sex based oppression#the way that i raged while listening to this#hearing that these women literally feel pressured to give up their ORGANS for these men#feminism#radical feminism#i hate the way that media glorifies female sacrifice as if it's this glorious thing when it really just reinforces gender inequality#notice how no one in this video is referring to uterus-havers or other genderist BS#they know exactly what women are and that this matter affects them specifically#terfsafe#terfs do interact#radblr#terfblr#TERF#Youtube
23 notes
·
View notes
Text
A surgeon who carried out the UK’s first womb transplant on a cisgender woman has said similar transplants for transgender women are probably about 10 to 20 years away.
In February, Imperial College London professor, James Smith, and his colleague, Isabel Quiroga, from the Oxford Transplant Centre, carried out the womb transplant on a married woman whose 40-year-old sister was willing to donate her own, having already given birth to two children.
The 34-year-old recipient, who lives in England and wishes not to be named, received the transplant during an operation lasting more than nine hours at the Churchill Hospital, in Oxford.
It is hoped that, in the future, womb transplants can be performed on trans women, giving them the chance to have a baby, but Smith said the reality of this is still decades away.
There is currently no “technical feasibility” to perform the operation on trans women due to a difference in the pelvic and vascular anatomy, the shape of the pelvis and issues with the microbiome – the network of micro-organisms that live in the human body, he explained...
Dr Narendra Kaushik, a surgeon in the Indian capital New Dehli, said in May 2022 that transplanting uteruses into trans women is “the future."
Uterine transplants are currently rare, costly and experimental surgeries that typically rely on donor organs. They are often done on people born without a uterus so they can become pregnant and give birth.
The first successful womb transplant took place at the University of Gothenburg in Sweden in 2014. Two years later, the operation was carried successfully once more in the US.
About 50 babies have now been born worldwide as a result of womb transplants.
Kaushik, who has 15 years of experience in gender-affirming surgeries, said: “We cannot predict exactly when this will happen but it will happen soon. We have our plans and we are very optimistic.”
-via PinkNews, August 23, 2023
#lgbtq#transgender#trans issues#trans women#trans healthcare#gender affirming care#trans rights are human rights#medical transition#organ transplant#organ donation#trans femme#united kingdom#uk#sweden#terfs are gonna have a fucking aneurysm and personally I can't wait#medical news#good news#hope
292 notes
·
View notes
Text
i just donated my kidney. it was a noble act. i saved a life. i also made some money. i sold it on the black market. i also stole it from someone else.
12 notes
·
View notes
Text
A growing number of patients who request medical assistance in dying are asking to donate their organs for transplant, says an international review that found that Canada is performing the most organ transplants from MAID patients among the four countries studied that offer this practice.
The report is the first-ever review of the growing use of this new practice around the world. The review was conducted in 2021 and the results were formally published in December 2022.
ADVERTISEMENT
“We saw everyone is working in different directions. And then we said ‘OK, well, let's start an international (discussion) of all the countries involved,’” said Dr. Johannes Mulder, a physician and MAID provider in Zwolle, Netherlands, in an interview with CTV News.
Data collected for the paper shows that in Canada, Belgium, the Netherlands and Spain, combined, 286 assisted-death recipients provide lifesaving organs for transplant to 837 patients in the years up to and including 2021.
RELATED STORIES
More than 10,000 Canadians received a medically-assisted death in 2021: report
Experts clash on whether medically assisted dying system ready for expansion by March
Veterans Affairs Canada service agent who raised medical assistance in dying 'no longer an employee'
The Death Debate: why some welcome Canada's move to assisted dying for mental illness and others fear it
Expert says government decision to delay assisted-dying expansion not necessary
Doctors in Canada, where medical assistance in dying (MAID) was decriminalized in 2016, performed almost half of the world’s organ transplants after MAID for that period (136), according to the publication.
Data from the Canadian Institute for Health Information confirms this new source of transplant organs accounted accounts for six per cent of all transplants from deceased donors in Canada in 2021. Some transplants, like those for kidneys and livers, can be done with patients who are alive.
“I was rather proud that Canada has done so well in terms of organ donation by MAID patients,” said Arthur Schafer, director of the Centre for Professional and Applied Ethics at the University of Manitoba, in an interview with CTV News.
With more than 4,000 Canadians waiting for organ transplants, some of whom are dying, he says Canada’s numbers show a strong move to turn death into a win-win.
“So I say, 'Good on us.' It’s a wonderful opportunity for someone facing death to make something significant out of the end of their life,” said Schafer.
PATIENT-DRIVEN TREND
The international review on this new practice has been overwhelmingly driven by patients who are suffering from irreversible degenerative diseases, like amyotrophic lateral sclerosis (ALS) and Parkinson’s.
“If this body has deserted me, I could do something good,” is how Mulder says patients frame their decision.
Canadian ALS patient Sharron Demchuk donated her kidneys and lungs after her medically assisted death in September of 2021. Her family says she herself pushed her doctors to consider a way she could help people after she died, becoming the first in New Brunswick to do so.
“She kept doing follow-ups, kept pushing and even though she wasn’t able to speak, she would make notes for my dad. ‘Here’s what I want you to ask them. Here’s what I want you to say,’” her daughter, Darlene Demchuk, told CTV News last year.
One of the goals of the international report, says Mulder, was to share information openly on how countries are managing this controversial and evolving new practice, including the tricky ethical and logistical issues of consent from vulnerable patients.
“What should you do, or what should what shouldn't you do? And how to keep the whole project completely voluntary,” he said of some of the concerns, noting that patients should never be pressured to choose MAID to increase the availability of donor organs.
That is a worry shared by Trudo Lemmens, a professor in health law and policy at the University of Toronto.
He points to statistics showing more than 35 per cent of Canadians who died by MAID in 2021 felt they were "a burden on family, friends or caregivers” according to a Health Canada report.
“I am concerned that people who struggle with a lack of self-esteem and self-worth may be pushed to see this as an opportunity to mean something,” said Lemmens in an email comment to CTV News.
With other countries like Australia eyeing medical assistance in dying along with organ donations, Mulder says public trust in this new medical practice must be developed and maintained.
“That’s why guidelines are necessary and should also be strict,”’ the doctor said.
184 notes
·
View notes
Link
When a donor organ becomes available to someone in need of a transplant, medical personnel need to act quickly. It only takes a few hours for expanding ice crystals to damage delicate tissue, leaving a window of less than 12 hours to assess, transport, and implant the new organ.
This not only creates a tremendous time crunch to perform a delicate procedure, but leaves many organs unviable for transplantation.
But a new breakthrough could vastly improve the landscape of liver transplantation: Scientists kept a liver preserved for three days, in non-frozen conditions, before transplanting it into a patient.
Moreover, that liver had been deemed unviable by transplant centers, since it had a tumor and came from a patient with sepsis (bacterial infection) that needed to be assessed and treated. The three-day window allowed the researchers to perform these actions, clearing the liver for transplant.
A year later, the recipient was perfectly healthy, with normal liver function and a normal quality of life. Although further investigation is necessary ahead of widespread clinical uptake, the results could mean, in the future, an increase in the number of livers deemed viable for transplantation.
Continue Reading.
763 notes
·
View notes