#psychiatric disorders
Text
Early Signs of Schizophrenia and Prevention Strategies!
Schizophrenia, a complex and often misunderstood mental disorder, affects millions of individuals worldwide. It is characterized by a range of symptoms that impact thoughts, emotions, and behavior. While the exact cause of schizophrenia remains elusive, early detection and intervention are crucial for managing the condition effectively. In this article, we delve into the early signs of…

View On WordPress
#Cognitive health#Early detection#Early intervention#Mental health awareness#Mental health education#Mental health prevention#Mental health promotion#Mental health support#Mental wellness strategies#Preventing schizophrenia#Psychiatric disorders#Psychosis signs#Schizophrenia awareness#Schizophrenia risk factors#Schizophrenia symptoms
2 notes
·
View notes
Photo
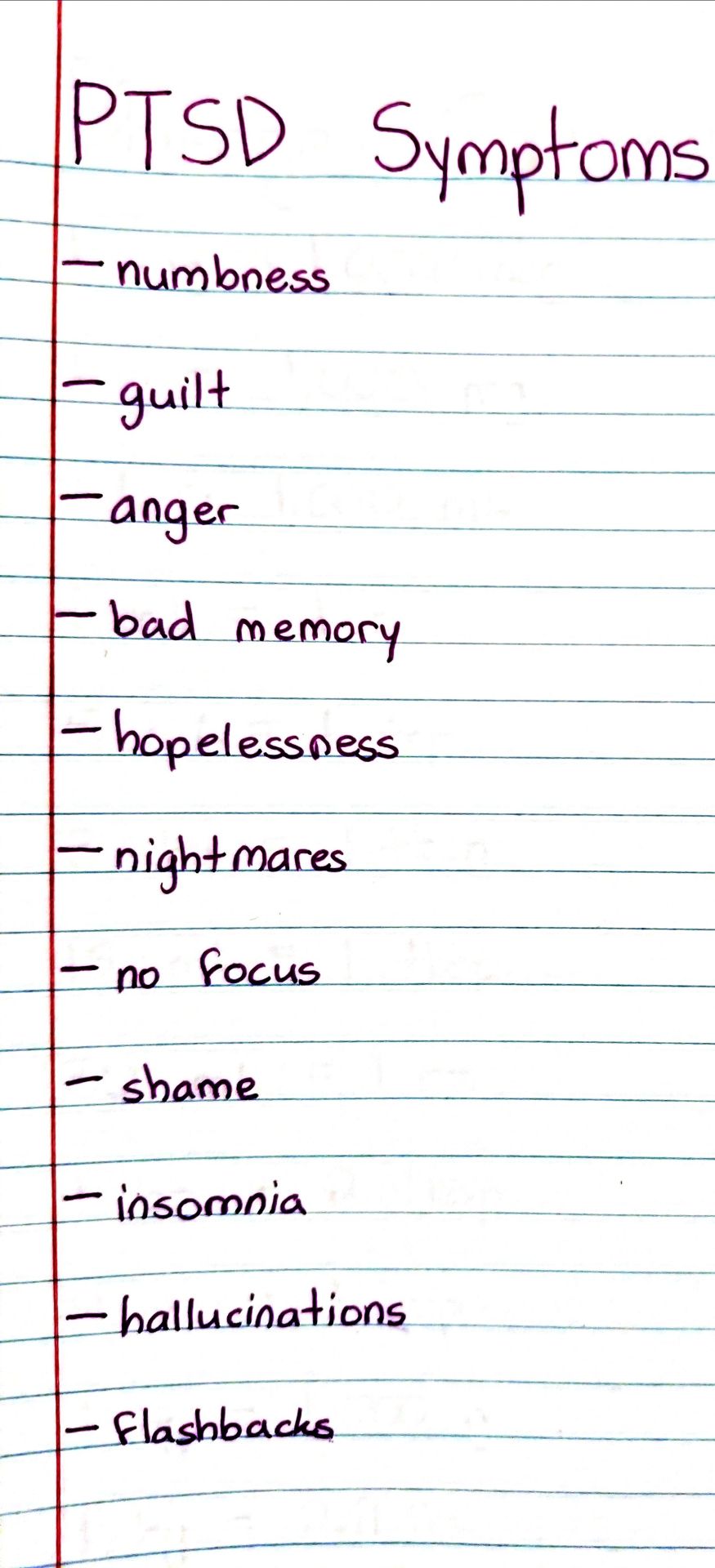
#studyblr#notes#medblr#medical notes#med notes#psychology#psychology notes#psych#psych notes#psychiatry#psychiatry notes#ptsd symptoms#ptsd#diseases and disorders#psychiatric disorders#psychiatric disorder symptoms#psychiatric symptoms#post-traumatic stress disorder#post traumatic stress disorder
5 notes
·
View notes
Text

You could say they had a fragile understanding of reality!
😄
#history#glass delusion#psychiatric disorders#king charles vi#medieval#european history#glass#fragile#shattered glass#1300s#1400s#medieval history#1500s#1600s#psychology#disorder#funny history#france#royal#medieval europe#historical figures#strange history#fragility#nickys facts
1 note
·
View note
Text
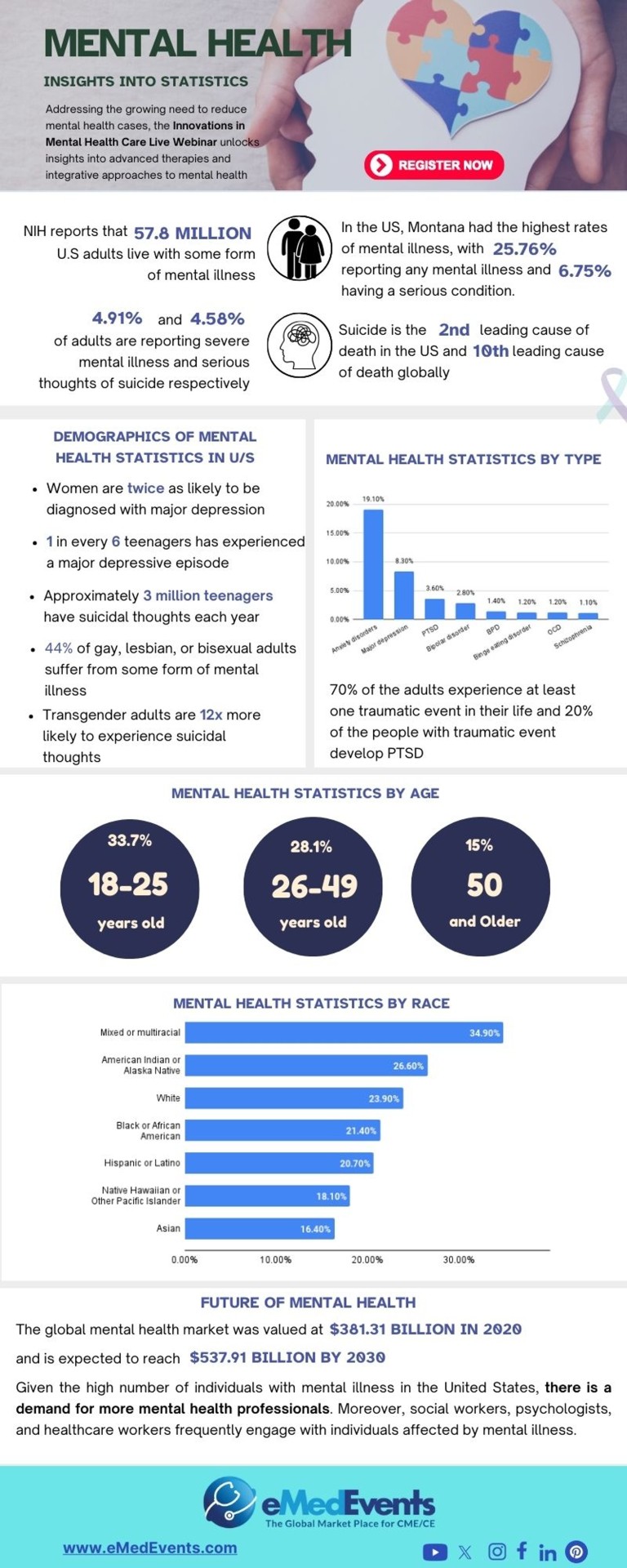
Innovations in Mental Health Webinar
Secure your spot for the upcoming mental health live webinar to uncover the advanced therapies and integrative approaches in mental health treatment
#Innovations in Mental Health Care Live#mental health professional#mental illness#psychiatry#neuroscience#Psychiatric Disorders#healthcare webinar#mental health treatment#psychology#CME Programs#CME Conferences#CME Medical courses#CME credits#doctor conferences#medical CME#Primary Care Conference#Medical CME Online#Emergency Medicine Online CME#Medical Conference Website#Physician Conferences#Medical CME Courses#Doctors CME Conferences#CME training for Physicians#Medical Event Organizer#Organizing Medical Events#Medical Conferences#Medical Speakers#Healthcare Marketplace
0 notes
Text
In a world that often prioritizes physical well-being, the significance of mental health can sometimes be overlooked. However, the reality is that mental health is an integral component of our overall well-being, influencing how we think, feel, and navigate the complexities of life.
0 notes
Text
Psychiatric loneliness.
#photography#photographer#photo#photographers on tumblr#photooftheday#photoart#psychiatry#psychiatric care#psychiatric hospital#psychiatric disorders
0 notes
Text
SOCIAL MEDIA Facebook Re: Joni • Diet and Medications / "The Pill"

link
0 notes
Photo

New Post has been published on https://www.knewtoday.net/early-signs-and-symptoms-of-psychiatric-problems-recognizing-potential-indicators/
Early Signs and Symptoms of Psychiatric Problems: Recognizing Potential Indicators

Psychiatric problems can encompass a wide range of conditions, each with its own unique set of signs and symptoms. It’s important to note that these symptoms can vary greatly depending on the specific disorder and individual factors.
Psychiatric problems, also known as mental health disorders, encompass a broad range of conditions that can significantly impact an individual’s thoughts, emotions, behaviors, and overall well-being. These conditions can affect people of all ages and backgrounds and may manifest in various ways. Recognizing the early signs and symptoms of psychiatric problems is crucial for early intervention and effective treatment.
It’s important to note that psychiatric problems are complex and multifaceted, and each disorder has its own distinct set of symptoms. Additionally, individuals may experience symptoms differently based on their unique circumstances. Nonetheless, there are some common indicators that can serve as early warning signs.
By understanding and being able to identify these early signs and symptoms, individuals, their loved ones, and healthcare professionals can intervene promptly, potentially preventing the condition from worsening or alleviating its impact on the person’s life.
In this article, we will explore some of the earliest signs and symptoms of psychiatric problems. However, it’s important to remember that self-diagnosis is not recommended, and only a qualified mental health professional can provide a definitive diagnosis. The information presented here is intended to raise awareness and promote early detection, encouraging individuals to seek appropriate professional help when needed.
Remember, mental health matters, and early recognition and intervention can make a significant difference in the lives of those affected by psychiatric problems.
Here are some common early signs and symptoms that may indicate the presence of a psychiatric problem:
Changes in mood: Persistent feelings of sadness, irritability, anger, or anxiety that seem out of proportion to the situation.
Withdrawal and social isolation: A noticeable decline in social activities, avoiding friends and family, and a preference for being alone.
Sleep disturbances: Significant changes in sleep patterns, such as insomnia or excessive sleepiness.
Changes in appetite: A noticeable decrease or increase in appetite that results in significant weight loss or gain.
Lack of concentration: Difficulty focusing, making decisions, or completing tasks that were previously manageable.
Decreased energy and motivation: Feeling consistently fatigued or lacking the drive to engage in activities once enjoyed.
Increased agitation or restlessness: Feeling constantly on edge, restless, or experiencing a sense of unease.
Unexplained physical complaints: Frequent headaches, stomachaches, or other physical symptoms without a clear medical cause.
Changes in self-care: Neglecting personal hygiene, appearance, or engaging in self-destructive behaviors.
Cognitive difficulties: Problems with memory, attention, or executive functioning (planning, organizing, problem-solving).
Changes in Mood
Changes in mood can occur for various reasons and are influenced by a combination of internal and external factors. While it’s normal to experience fluctuations in mood from time to time, persistent or extreme mood swings may indicate underlying conditions that require attention. Here are some potential causes and factors that can contribute to changes in mood:
Emotional triggers: Certain events or situations, such as receiving good news or facing a stressful event, can elicit emotional responses and cause shifts in mood.
Hormonal changes: Hormonal fluctuations, particularly in women during menstrual cycles, pregnancy, or menopause, can lead to mood swings. Hormones play a significant role in regulating mood and emotions.
Sleep disturbances: Lack of quality sleep or disruptions in sleep patterns can negatively impact mood stability. Sleep deprivation can make you more susceptible to irritability, sadness, and mood swings.
Stress and anxiety: High levels of stress and anxiety can affect mood and lead to mood swings. Coping with excessive stressors, such as work pressures or relationship difficulties, can strain emotional well-being.
Mental health conditions: Conditions like depression, bipolar disorder, and borderline personality disorder can cause significant mood swings. These conditions often require professional diagnosis and treatment.
Medications and substances: Certain medications, such as antidepressants, steroids, or hormonal treatments, may impact mood stability. Substance abuse or withdrawal can also contribute to changes in mood.
Seasonal changes: Some individuals may experience seasonal affective disorder (SAD), a type of depression that occurs during specific seasons, usually winter. Changes in light exposure and circadian rhythm disruptions can influence mood.
Lifestyle factors: Poor nutrition, lack of physical activity, and excessive alcohol or drug use can affect mood stability. Engaging in healthy habits, like regular exercise and a balanced diet, can positively impact mood.
If you’re concerned about your mood swings or notice persistent changes in your emotional well-being, it’s recommended to consult a healthcare professional or mental health provider. They can help assess your situation, provide an accurate diagnosis if necessary, and guide you toward appropriate treatment options.
Withdrawal and Social Isolation
Withdrawal and social isolation are significant aspects of mental health and can have a profound impact on an individual’s well-being. While I cannot generate images, I can provide you with information on withdrawal and social isolation.
Withdrawal refers to a behavior where individuals consciously or unconsciously distance themselves from social interactions and isolate themselves from others. It can manifest in various ways, such as avoiding social gatherings, spending excessive time alone, or withdrawing emotionally from relationships. It is often associated with mental health conditions like depression, anxiety disorders, social anxiety, and certain personality disorders.
Social isolation, on the other hand, refers to a state where individuals have limited or no social contact with others. It can result from external circumstances, such as living alone or being geographically isolated, as well as internal factors like a lack of social skills, low self-esteem, or a fear of judgment and rejection. Prolonged social isolation can significantly impact mental health and contribute to feelings of loneliness, depression, and increased vulnerability to other mental health issues.
Both withdrawal and social isolation can be early signs of underlying mental health problems. They can be influenced by a variety of factors, including personal experiences, trauma, societal pressures, and individual temperament. It is important to recognize and address these behaviors, as they can have detrimental effects on individuals’ mental, emotional, and physical well-being.
If you or someone you know is experiencing withdrawal and social isolation, it is advisable to seek professional help from a mental health provider. They can provide an accurate diagnosis, determine the underlying causes, and recommend appropriate interventions or treatments to address these issues and promote social connection and well-being.
Sleep Disturbances
Sleep disturbances are disruptions in the normal patterns of sleep, which can include difficulties falling asleep, staying asleep, or experiencing poor sleep quality. They are common symptoms associated with various psychiatric problems and can also contribute to the development or exacerbation of mental health issues. While I cannot generate images, I can provide information on sleep disturbances.
Sleep disturbances can manifest in different ways, including:
Insomnia: Difficulty falling asleep, staying asleep, or waking up too early in the morning. Insomnia can be associated with psychiatric disorders such as anxiety, depression, and post-traumatic stress disorder (PTSD).
Hypersomnia: Excessive daytime sleepiness, often leading to long or unrefreshing naps. Conditions such as major depressive disorder and certain sleep disorders, like narcolepsy, can cause hypersomnia.
Nightmares: Disturbing dreams that awaken individuals during the night, causing anxiety or fear. Nightmares can be linked to conditions like post-traumatic stress disorder (PTSD), anxiety disorders, and mood disorders.
Sleep apnea: A sleep disorder characterized by pauses in breathing or shallow breathing during sleep, leading to disrupted sleep and daytime fatigue. Sleep apnea can affect mental health by contributing to mood disorders and cognitive impairment.
Restless legs syndrome (RLS): An uncomfortable sensation in the legs, often accompanied by an irresistible urge to move them, which can disrupt sleep. RLS is associated with conditions such as depression and anxiety disorders.
Sleep disturbances and psychiatric problems often have a bidirectional relationship, meaning they can influence and exacerbate each other. Disrupted sleep can contribute to the onset or worsening of mental health conditions, and psychiatric problems can disrupt normal sleep patterns. Addressing sleep disturbances is essential for promoting overall mental well-being.
Changes in Appetite
Changes in appetite refer to significant alterations in a person’s desire to eat or the amount of food they consume. These changes can be indicators of underlying physical or mental health issues. While I cannot generate images, I can provide information on changes in appetite.
There are two primary types of appetite changes:
Increased appetite (polyphagia): This involves an abnormally heightened desire to eat and a tendency to consume larger quantities of food. It can be associated with conditions such as depression, certain types of anxiety disorders, bipolar disorder, and some medical conditions.
Decreased appetite (hypophagia or anorexia): This refers to a reduced desire to eat or a lack of interest in food. It can result in decreased food intake and weight loss. Decreased appetite can be a symptom of various mental health disorders, including major depressive disorder, generalized anxiety disorder, eating disorders (such as anorexia nervosa), and substance abuse.
Changes in appetite can significantly impact an individual’s nutritional status and overall well-being. It is important to identify the underlying cause of appetite changes and address them appropriately. A healthcare professional, such as a doctor or mental health specialist, can conduct a thorough evaluation to determine the root cause and develop a suitable treatment plan.
In some cases, changes in appetite may require a multidisciplinary approach involving mental health interventions, nutritional counseling, and medical management. Additionally, supportive measures like maintaining a balanced diet, regular exercise, and establishing healthy eating habits can also be beneficial.
Lack of Concentration
Lack of concentration, also known as difficulty focusing or sustaining attention, is a common symptom that can occur in various mental health conditions and situations. While I cannot generate images, I can provide information on the topic.
Lack of concentration refers to an inability to focus on a task or maintain attention for an extended period. It can manifest in several ways:
Distractibility: Being easily distracted by external stimuli or internal thoughts, making it challenging to stay focused on the task at hand.
Mind wandering: Frequently experiencing a wandering mind, where thoughts drift away from the present moment, causing difficulty in maintaining concentration.
Difficulty starting or completing tasks: Struggling to initiate tasks or experiencing challenges in following through and completing them due to a lack of sustained attention.
Lack of concentration can be associated with various mental health conditions, including:
Attention-deficit/hyperactivity disorder (ADHD): Individuals with ADHD often experience difficulties with concentration and attention, leading to problems in academic, work, or daily life functioning.
Anxiety disorders: Excessive worry, racing thoughts, and feelings of restlessness in anxiety disorders can impair concentration and make it challenging to focus on specific tasks.
Depression: Depressive symptoms such as fatigue, diminished motivation, and reduced cognitive functioning can lead to difficulties with concentration and attention.
Stress and overload: High levels of stress, overwhelming demands, or multitasking can impact concentration and make it harder to maintain focus.
Sleep disturbances: Lack of quality sleep or sleep disorders can significantly affect cognitive functioning, including concentration and attention.
If you or someone you know is experiencing persistent difficulty with concentration that interferes with daily functioning and quality of life, it may be helpful to seek professional evaluation. A mental health professional can conduct an assessment, identify any underlying conditions or contributing factors, and recommend appropriate interventions. Treatment options may include therapy, medication, lifestyle modifications, and developing strategies to improve focus and attention.
It’s important to address the underlying causes of lack of concentration, as improved focus and attention can enhance productivity, performance, and overall well-being.
Decreased Energy and Motivation
Decreased energy and motivation are common symptoms that can occur in various mental health conditions and situations. While I cannot generate images, I can provide information on the topic.
Decreased energy refers to a significant reduction in physical or mental vitality and can manifest as feelings of fatigue, lethargy, or a general lack of energy. Motivation refers to the drive, enthusiasm, or willingness to engage in activities or pursue goals. When energy and motivation are decreased, individuals may find it challenging to initiate tasks, experience a lack of interest or pleasure in activities, and struggle to maintain productivity.
Several mental health conditions can be associated with decreased energy and motivation, including:
Depression: Reduced energy levels and loss of interest or pleasure in previously enjoyed activities are hallmark symptoms of depression.
Anxiety disorders: Chronic worry and anxiety can be mentally and physically draining, leading to decreased energy and motivation.
Bipolar disorder: During depressive episodes of bipolar disorder, individuals may experience low energy levels and a decrease in motivation.
Chronic stress: Prolonged exposure to stress can deplete energy reserves, leading to a lack of motivation and fatigue.
Certain medical conditions and medications: Some medical conditions, such as thyroid disorders or chronic pain, can contribute to decreased energy and motivation. Additionally, certain medications may have side effects that impact energy levels.
It’s important to differentiate between a temporary decrease in energy and motivation due to situational factors (such as stress or a busy period) and persistent or significant changes that affect daily functioning and quality of life. If you or someone you know is experiencing prolonged or severe decreases in energy and motivation, it may be helpful to seek professional evaluation. A healthcare provider or mental health professional can conduct an assessment, identify underlying causes or contributing factors, and recommend appropriate interventions. Treatment options may include therapy, medication, lifestyle modifications, and developing strategies to increase energy and motivation.
Addressing decreased energy and motivation can significantly improve overall well-being and quality of life. It is important to seek support and guidance from professionals to explore the underlying causes and develop a tailored treatment plan.
Increased Agitation or Restlessness
Increased agitation or restlessness refers to a state of heightened physical or mental activity, often accompanied by a sense of inner turmoil or discomfort. While I cannot generate images, I can provide information on this topic.
Agitation and restlessness can manifest in various ways, including:
Physical restlessness: Difficulty sitting still, pacing, fidgeting, or constantly moving body parts (e.g., tapping fingers or bouncing legs).
Emotional agitation: Feeling on edge, irritable, or easily provoked. There may be a sense of inner tension or unease.
Racing thoughts: Experiencing a rapid stream of thoughts, making it challenging to focus or relax.
Impatience: Having a decreased tolerance for delays or frustrations, often resulting in heightened irritability.
Agitation and restlessness can be associated with several mental health conditions, including:
Anxiety disorders: Conditions such as generalized anxiety disorder, panic disorder, or post-traumatic stress disorder (PTSD) can lead to increased agitation and restlessness due to heightened levels of anxiety.
Bipolar disorder: During periods of mania or hypomania, individuals with bipolar disorder may experience increased energy, agitation, and restlessness.
Attention-deficit/hyperactivity disorder (ADHD): Restlessness and difficulty staying still are core symptoms of ADHD, particularly in children and adolescents.
Substance withdrawal: When an individual stops using certain substances, such as alcohol, benzodiazepines, or stimulants, they may experience agitation and restlessness as part of the withdrawal process.
It’s important to note that increased agitation and restlessness can also be influenced by situational factors such as stress, sleep deprivation, or certain medications. If you or someone you know is experiencing persistent or severe agitation or restlessness that interferes with daily functioning and well-being, it may be helpful to seek professional evaluation. A mental health professional can assess the symptoms, determine any underlying conditions or contributing factors, and recommend appropriate interventions. Treatment options may include therapy, medication, stress reduction techniques, lifestyle adjustments, and coping strategies to manage agitation and restlessness effectively.
Addressing increased agitation and restlessness is crucial for promoting overall mental well-being and reducing distress. Seeking professional help can provide guidance, support, and appropriate interventions to manage these symptoms and improve quality of life.
Unexplained Physical Complaints
Unexplained physical complaints refer to physical symptoms or sensations that cannot be adequately explained by a medical condition or a specific physical cause. These symptoms may lack a clear organic basis and may not align with the expected physiological findings. While I cannot generate images, I can provide information on this topic.
Unexplained physical complaints can manifest in various ways, including:
Chronic pain: Persistent or recurrent pain in different parts of the body, such as headaches, backaches, or joint pain, without a clear medical explanation.
Gastrointestinal issues: Frequent or chronic digestive complaints, such as abdominal pain, bloating, nausea, or changes in bowel habits, with no identifiable organic cause.
Fatigue: Persistent feelings of tiredness, low energy, or weakness that cannot be attributed to a medical condition or physical exertion.
Non-specific neurological symptoms: Experiencing unexplained sensations like tingling, numbness, dizziness, or balance problems without apparent neurological abnormalities.
Sleep disturbances: Persistent difficulties with sleep, such as insomnia or non-restorative sleep, that do not result from an identifiable sleep disorder or external factors.
These unexplained physical complaints often fall under the category of somatic symptom disorder (SSD) or related conditions. Somatic symptom disorder involves experiencing distressing physical symptoms and excessive concern or preoccupation with these symptoms, which may significantly impact daily functioning and quality of life.
It is important to approach unexplained physical complaints with a comprehensive assessment that includes both physical and psychological evaluations. Sometimes, these symptoms can be influenced by underlying mental health conditions, such as anxiety disorders, depression, or trauma-related disorders.
It’s essential to validate and address these symptoms with appropriate support and care, as understanding the mind-body connection can contribute to improved well-being and symptom management.
Changes in Self-care
Changes in self-care refer to noticeable alterations in a person’s ability or willingness to engage in activities that promote physical and emotional well-being and personal hygiene. While I cannot generate images, I can provide information on this topic.
Self-care activities encompass a wide range of behaviors, including maintaining personal hygiene, eating a balanced diet, getting regular exercise, practicing relaxation techniques, seeking social support, and attending to emotional needs. Changes in self-care can manifest in several ways:
Neglecting personal hygiene: Individuals may show a decline in grooming habits, such as not showering regularly, neglecting dental care, or wearing unwashed clothes.
Poor nutrition and appetite changes: There may be a noticeable shift in eating patterns, including reduced appetite, skipping meals, or relying on unhealthy food choices.
Lack of exercise or physical activity: A decrease in engagement in regular physical activity or a significant decline in overall mobility and energy levels.
Neglecting emotional well-being: Individuals may withdraw from activities they once enjoyed, isolate themselves socially, or disregard activities that promote emotional well-being, such as hobbies or self-reflection.
Changes in self-care can be indicative of various underlying factors, including:
Depression: Individuals experiencing depression may struggle with motivation, energy levels, and finding pleasure in self-care activities.
Anxiety disorders: Heightened anxiety can lead to difficulties in focusing on self-care, as individuals may be preoccupied with worry and physical symptoms.
Substance abuse: The misuse of substances can interfere with self-care routines and priorities, leading to neglect of personal hygiene and overall well-being.
Chronic illness or pain: Managing chronic health conditions or experiencing persistent pain can make self-care activities more challenging to accomplish.
Overwhelming stress: High levels of stress can contribute to a neglect of self-care as individuals may prioritize other responsibilities or struggle with time management.
Addressing changes in self-care is crucial for maintaining physical and emotional health. By prioritizing self-care activities, individuals can enhance their overall well-being, resilience, and quality of life.
Cognitive Difficulties
Cognitive difficulties refer to challenges or changes in various mental processes involved in thinking, understanding, remembering, and problem-solving. While I cannot generate images, I can provide information on this topic.
Cognitive difficulties can manifest in different ways, including:
Memory problems: Difficulty in remembering recent events, important information, or tasks that need to be accomplished.
Concentration and attention issues: Finding it challenging to stay focused on tasks, easily getting distracted, or experiencing a general lack of concentration.
Slowed thinking or processing speed: A noticeable delay in processing information, generating thoughts, or responding to stimuli.
Language difficulties: Struggling to find the right words, express oneself clearly, or understand written or spoken language.
Executive function deficits: Difficulties in planning, organizing, problem-solving, multitasking, or initiating and completing tasks.
Cognitive difficulties can be associated with various factors, including:
Aging: Normal age-related cognitive changes can lead to mild memory difficulties and a slight decline in cognitive functioning.
Mental health conditions: Conditions such as depression, anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), or post-traumatic stress disorder (PTSD) can impact cognitive abilities.
Neurological disorders: Conditions like Alzheimer’s disease, Parkinson’s disease, multiple sclerosis (MS), or traumatic brain injury (TBI) can cause cognitive impairments.
Medication side effects: Certain medications, particularly those affecting the central nervous system, may have cognitive side effects.
Chronic stress: Prolonged exposure to high levels of stress can impact cognitive performance, including memory and concentration.
Addressing cognitive difficulties early on is important for managing symptoms, improving cognitive functioning, and enhancing overall well-being. Professionals can provide appropriate support, guidance, and interventions to help individuals cope with and adapt to any cognitive changes they may be experiencing.
#Appetite changes#Behavioral changes#Cognitive impairment#Emotional changes#Mental health#Mental health awareness#Mood disorders#Psychiatric disorders#Self-care neglect#Sleep disturbances#Social withdrawal
0 notes
Text
i find it simultaneously funny and annoying how i take adderall to get my final projects done and i want to do everything else instead, like im motivated to do things i've been putting off for the longest but not the task i specifically took it for
#fighting the urge to create another spotify playlist#i should be writing my linguistics paper#listening to nicki minaj#adhd#psychiatric disorders#wish i wasn't neurodivergent sometimes#nicki minaj#spotify
1 note
·
View note
Text
A mysterious brain network may underlie many psychiatric disorders
Scientists have uncovered a mysterious network of brain connections that is linked to several psychiatric disorders, including schizophrenia, depression and obsessive-compulsive disorder (OCD).
This shared brain circuitry could help reveal why many patients who are diagnosed with one psychiatric illness also meet the criteria for a second.
#science#2023#psychiatric disorders#neuroscience#schizophrenia#depression#ocd#bipolar disorder#anxiety#addiction#brain#mental health
0 notes
Text
Impact of Sleep on Mental Health Key Findings!
Sleep and mental health are closely interconnected. Poor sleep can have a significant impact on psychological well-being, exacerbating existing mental health issues and potentially leading to new problems. Here are some key findings regarding the impact of sleep on mental health.
Unlocking the Secrets to Better Mental Health: Meta-analysis of Randomized Controlled Trials Reveals the Power of…

View On WordPress
#bedtime routine#CBT-I#Cognitive function#Diet#impact#key findings#Mental health#Mindfulness#mood regulation#Physical activity#professional help#Psychiatric disorders#psychological resilience#Relaxation Techniques#screen time#Sleep#Sleep deprivation#sleep environment#Sleep hygiene#sleep schedule#Stress#Stress Management
0 notes
Text
Factitious Disorder
-- a disorder where someone deceives others by appearing sick, by purposely getting sick, or by self-injury
-- can also happen when family members or caregivers falsely present others as being ill, injured, or impaired
-- symptoms can range from mild (slight exaggeration of symptoms) to severe
-- patient may make-up symptoms or tamper with medical tests
-- not the same as inventing medical problems for a practical benefit
-- challenging to identify
-- hard to treat
#studyblr#notes#medblr#medical notes#med notes#psychology#psychology notes#psych#psych notes#psychiatry#psychiatry notes#factitious disorder#tw self-injury#tw#psychological disorders#psychiatric disorders
5 notes
·
View notes
Text
When are therapists gonna understand we can be self aware? Are they really gonna die on the hill that states it’s impossible for a narcissist to know and accept what they are? I lack empathy, not basic cognitive skills. Even intellectually disabled people can know they’re intellectually disabled.
This awareness they think we’re incapable of is the type of awareness living beings have intrinsically. It’s fucking basic awareness of information and the ability to compare. This red strawberry looks just like the other red strawberry, so 4-year-old-you matches them together on your little tablet game.
Yes, I can comprehend why I would be labeled as a narcissist. I’m mentally capable of understanding how I fit the description, and I’m mentally and emotionally capable of accepting new information I learn about myself.
What I don’t understand is how the psychiatric industry can be messed up enough for a LICENSED PSYCHIATRIST to believe someone can lack an intrinsic skill that LITERALLY COMES WITH BEING CONSCIOUS like what the actual hell?!?!??!!?
#flashy ✨ vent#flashy ✨ thoughts#cluster b#actually cluster b#npd#actually npd#actually narcissistic#narcissistic personality disorder#cluster b safe#npd safe#npd stigma#self awareness#ableism#psychiatry#psychiatric ableism#tw caps
171 notes
·
View notes
Text
Our mental health clinic in Cumberland, Maryland, provides mental health services for people living with Obsessive-Compulsive Disorder (OCD). OCD is one of the illnesses that affect the quality of life. OCD is composed of thoughts (obsessions) that may induce anxiety.
0 notes
Text
Ablebodied keep saying that cripple punk is "excluding the brain" and "creating a dualism between the brain and the rest of the body" when it is not. People with a neurological disorder can call themselves cripple if they want to because neurological disorders are a physical disability.
There is no denial some physical disabilities often come with psychiatric symptoms and vise versa, but it is not the same as a mental disability or a physical disability.
Autistic people often experience motor difficulties but it is not the same as someone with mobility issues. People with multiple sclerosis often experience cognitive symptoms like executive dysfunction, but it is not the same as someone with ADHD. It's not harmful to acknowledge the differences between mental and physical disabilities.
It's possible to acknowledge interactionism without saying the two are identical and speaking over people with a physical disability.
#actually autistic#actually neurodivergent#Cpunk#cripple punk#I have a neurological disorder that is often accompanied with psychiatric symptoms but I don't go out of my way to say this is the same as-#The same as mental disability#Just to be clear neurological ≠ neurodevelopmental or mental disorder
152 notes
·
View notes
Text
Being medicated doesn't mean becoming normal.
There's this trope I've seen in media, mentally ill that take meds and suddenly become neurotypical. To me this was a harmful fantasy, thinking that medicine means cure, and a fast one.
The reality of meds is often disappointing. You still find your limitations and differences. Lots of underground symptoms and sensitivities don't ever vanish.
Being bipolar myself it often left me perplexed, the fact that I was receiving correct treatment, but still struggled. Not with acute episodes, just a baby version of previous symptoms.
I'm trying to accept bipolar as my personal disability. I figured that medicine is my support, like a cane could be for those with physical disabilities. It means I'm still not like the rest and I will always struggle, but man is it nice to have some help...
#bipolar disorder#disability#psychiatric medication#medication#actuallybipolar#actually bipolar#manic depression#actually mentally ill#manic depressive#actually manic#mania#bipolar mania#bipolar 1#bipolar 2#bipolar ii#bipolar depression#bipolar i#bipolar#lithium#lamotrigine#seroquel#zyprexa#abilify#prozac#fluoxetine#lexapro
331 notes
·
View notes