#really hoping my pulmonologist is ok
Text
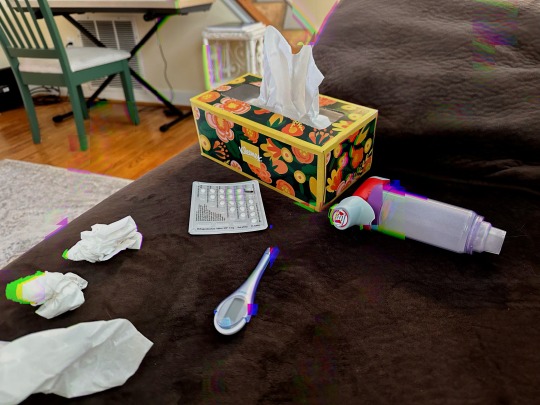
Gave myself almost-pneumonia and my couch looks like a damn stock photo.
Since the whole time I’ve been like, “Am I living one of my shitty fanfictions? Coz this sucks.” Let me tell y’all a story.
Cold weather sucks as a severe asthmatic. I moved to the South so I didn’t have to deal with the frigid winters of upstate NY. I’m basically on and off sick until Spring comes (and then there’s allergy season but I digress). I think it’s helped some, but my lungs are just fucked up ok?
Anyways I went to a concert last Saturday and it was freezing. Then I went to the zoo on Sunday with a friend and it was also cold and swarming with kids who don’t know how to cover their mouths when they cough. It was a great weekend but by Tuesday I was sick - great. I had some warning bc my friend I went to the zoo with said they got sick yesterday. But it just seemed like a minor cold and I’ve been through this a million times, I truly did not think it was gonna get too much worse. My asthma was mostly under control and I rested a lot all week.
Thursday I’m more tired, but I start nebulizer treatments and even skip ice skating class and reschedule it for Saturday bc hey, I’m responsible. But Friday I start to feel worse. Like to the point where everybody at work is like wtf go home and one of them told me she’s gonna get me holy water. But it’s okay, it’s still been SO much worse and I’m really fine.
Saturday morning I wake up and I feel like I’m cured. So I go to ice skating class. And maybe I take a little walk in the rain. Bad fuckin idea. By the end of the day I’m having full blown asthma attacks one after the other and sweating like crazy. My abdomen is aching from coughing so much that it hurts to sit up. But I really don’t want to go to the ER. Not again. So I message my pulmonologist and hope I can just say never mind I’m good now by the time he answers on Monday.
That brings us to today, Sunday. I woke up at 6am after only 4 hours of sleep because I can’t stop choking. I’m sneezing and coughing up fluorescent green stuff, my throat tastes like blood and I have a fever. I really, really didn’t want to go to the doctor but it’s time. I drag my sorry ass to urgent care where the entire hour I sit in waiting, everybody who walks by gives me a ‘goddamn’ look because I’m coughing loud enough to alert the entire damn office. I’m so embarrassed bc what if they think I’m being dramatic and wasting time - again? I awkwardly explain my situation and the doctor sends me for CXR. When it comes back he says “Well, you don’t have pneumonia yet but see alllll this stuff here? That’s inflammation. I’m gonna prescribe antibiotics and (way heavier) steroids and you might have bronchitis already but your asthma is so bad that it’s indistinguishable by now. Also with your lungs you probably won’t be able to tell you have pneumonia until it’s pretty bad.”
So anyways, that’s my week. At least I got a lot of writing done for Whumptober - didn’t have to dig very deep to find enough misery to go around to all my fav OCs lol.
#self obs#taken before I got a 10x higher dose of steroids and also antibiotics#brought to you by ~asthma~#almost pneumonia bc the doc said I probably have bronchitis but my asthma is so bad they’re indistinguishable at this point#CXR questionable#so that’s fun#anyways it’d be hot if it wasn’t me so here ya go#sicknario#snzario#snz#snzblr#snz kink#snzfucker#flu whump#illness whump#asthma#coughing
13 notes
·
View notes
Text
Health update, sort of:
I obviously failed in my goal to call new therapists by last Tuesday. I'm doing that as soon as I make this post, though.
I finally had a sleep study done. Insurance would only approve the at-home study, despite my pulmonologist saying the in-clinic studies were better and would both rule out and/or indicate much more than the at-home study. The results came back borderline for obstructive sleep apnea. An earlier post on here goes more into detail, and I'll save my thoughts on insurance directing my treatment over the judgment of doctors for another time.
Despite the nurse being wildly unhelpful about my results, I still did what she said. I had an appointment with my PCP this past Tuesday and discussed the results plus some other things with her and wanted to note some of the results here, good and bad.
First, as far as sleep, she said the at-home studies are less sensitive and empathized with me on how frustrating this can be. I appreciated that much, even if she can't do anything about it. She prescribed trazodone to help me sleep. I hope it works. She said one of the side effects is nightmares, so... we'll see.
The original reason I had the appointment was for a bloodwork follow-up. In January, I had a slightly elevated cholesterol level and an extremely low Vitamin D level (it should be 30, it was 6, like some sort of Victorian orphan). I've been on a statin drug, obviously monitoring my diet better, but apparently I was supposed to keep taking the Vitamin D supplement and not just the 12 weeks she gave me. So bloodwork was postponed until Jan. 2021.
One surprising thing: I tried to avoid taking adderall before I went because I didn't want to fuck up any results. But because I sleep like that squirrel from Ice Age, I was worried about nodding off on the two-hour drive to my doctor. So I took one to be alert. Despite that, my blood pressure was still normal/low (though higher than my usual), and my heart rate was 66. It didn't even occur to me to keep up on that metric. Last year, before I started this, I remember feeling like absolute shit just sitting on my couch and checking my heart rate. It was around 85. I checked a couple more times over the next few days and it was always about the same, between 80-85. So hearing that it was 66 was definitely surprising and felt a little like a victory I wasn't expecting.
Anyway. I will now call these other therapists and hope I make it in soon. I'm doing ok, but I want to avoid another cratering. For me, these severe depressive episodes are definitely rare now, but when they do hit, it's like being drunk. When I'm fully involved in it, it doesn't feel like it's as bad as it really is. Then, after it's worn off/gone away, you see it in hindsight and "HOLY SHIT DID I REALLY ALMOST SHAVE MY HEAD/GET THAT TATTOO?" And yes, those choices present themselves to me while I'm depressed or when I'm totally shithoused. I live a fun life.
4 notes
·
View notes
Text
In This Technology World, We Live
Top Picture Credits WebFactory Ltd/@webfactoryltd
Powered by Squarespace
In This Technology World, We Live
Technology has turned out excellent, but to sit as we all watch it grow, but leaving some of society out of this equation, is unacceptable behavior. The developers need to stop and rethink how they're developing for the communities' most astonishing invention, taking away from all our lives now but is the way we all do business, which is excellent.
So please, don't take this article out of its context.
I decided to add to some feedback I gave on Windows 10 and how my browser displays pages, and how my laptop was running, which has sparked this article.
To make things even more accessible to those who have difficulties comprehending things due to life-changing incidents beyond his/their control and that of human nature. Sometimes life-altering changes happen to one's life that turns out in debilitating un-expectancies.
For instance, "I had died over a year ago and was placed on life support for a bit. I lost 68% oxygen to the brain, leaving my body and brain getting 32%, `which the doctor's hoped would return to normal,' but instead, the way things have turned out for me today, "I have difficulties comprehending something."
All I do, is keep asking for help because I have problems understanding something, or it takes me longer to learn something, more times than not?"
I get nowhere asking, why do you think that is? Perhaps the lack of compassion or caring of someone that has a disability? Then try to sell you something to make it work for you, despicable.
Or when I go for walks to circulate blood flow, the blood clots could start forming in my arteries from peripheral artery damage. But I get winded easily, even if it's a block, but I lose oxygen and then struggle for air from another health condition. Still adding fuel to the fire, it was the loss of the oxygen in the first place, while on life support, that's caused all this.
And I have been asking the pulmonologist to be put on oxygen to get out more for blood flow.
My primary doctor saw this first hand now walking about 2000 yards and was quite concerned from the oxygen telemetry meter reading of 62% and waited about 15 minutes and retook it, reading still the same. It wasn't until 30-45 minutes later I left when my oxygen was about 82%.
The intake nurse is the one that first saw this and said, well, maybe it was the meter and went to get another one; really, she went and told the NP what was happening. All the time, I was struggling to breathe, which I knew eventually would come back up.
But, in walked my doctor or NP, that's whom I see actually, and put her hand on my shoulder, William, are you ok? Well, no, this is how I get when I walk. I have my inhalers here; I haven't smoked but two cigarettes this morning. From the walk from the main road in front of the hospital to the back here, these results.
I go through this all the time, and the pulmonary doctor knows this and still won't give me oxygen, a "broken-down society." If I die again from this, there isn't any turning back the next time and no life support next time either; I'm tired, I have a DNR in place, sad as me saying this, because of a "broken-down society."
Instead of leaving within us unresolved questions with no one having answers to them, and going within ourselves, creating even more frustrations to an individual needs? "People couldn't possibly know what that feels like and don't understand the life of another person's journey and what they face already.
Inside the individual, leaving them rendered to the feeling of the uncompassionate care they see in their eyes, and now, a new journey for them; they must walk through life this way, which is unacceptable but, undoubtedly understandable in a "broken-down society."
It's true; "I might be having these difficulties that others couldn't possibly understand." But still, one thing is for sure, "society is broken-down when other individuals boast about helping in a disability world of unexpected turnouts and leave them with an unsettledness inside because of the lack of helping."
"Before we can start to make changes in this broken-down society of uncaring people, `these changes begin within ourselves first, before they emanate outward."
"However, this is an official viewpoint that leaves me still very "Thankful," how I need to proceed with my journey through life, `which helps me become a better person today than yesterday."
I am a writer, and I too rely on this technology for writing; I like it or love it; it is part of whom I've become today. "I cannot explain how I can sit here and write something like this, but I still have a rough time understanding something now?"
Instead, we add pure cold-heartedness to the equation, sucking the lives out of them or their pockets. "What happened to the pureness of kindness?"
The lack of help when we ask for it and send you to these pages to read regardless of how "they" want to justify it; it just gets humanity and the people of it, absolutely nowhere.”
"It isn't helping anything, but adding to an unresolved solution?"
Try making something better for what an individuals' experiencing; this same incident, which I had, provoked me to write this opinion of the developing developers. Instead of focusing on "ads," please focus on the individuals' experience now?
"It will even make for a better internet experience."
I had no control over losing my life, making my comprehension this way and be this way. Things in this life happen for reasons beyond our understanding, and maybe I wrote this article as a learning tool on how much we take our lives for granted and just being human in kindness!
Written by:
William Darnell, Sr.
11/26/2020 9:33 PM
Powered by Swagger © Poetry
#technology, #comprehension, #society is broken-down,
1 note
·
View note
Note
I really hope that it was the frustration talking and u didn't actually refuse to take your meds. Like what do u want to do at this point?? Be miserable anyway on Christmas bc u got worse and also make your entire family sick with worry since u are once again neglecting your health and this can easily turn really bad?? Maybe miss your surgery bc u r too sick?? This sucks and I'm really sorry u r still dealing with it but refusing to fix it is only going to make it worse.
I started the antibiotic this morning, I just refused the prednisone. I honestly don't feel like I'm ill enough to need it. The antibiotic is intended to protect my lungs from more serious infection, so I should be covered. It's not going to cure my bronchitis -- but it'll reduce my risk of developing pneumonia. That's why I called my GP yesterday -- because I recognized that I should take something so things don't get out of control over the holidays since I've been sick for nearly 3 weeks now. I'm not totally neglectful of my health. I try sometimes. 😅💕
My peak flow is decent and I'm ok on rescue meds for now, so prednisone is gonna stay in my desk drawer. My doctor prescribed it for me because that's his job and he had to, given my symptoms. He could have prescribed it for 5 days like normal instead of trying to torture me with 10 days. 😑 He goes overboard sometimes because I'm his best friend's kid, so he'll throw meds at me whether I need them or not.
Since I've had asthma my whole life, I'll admit that I gamble with it sometimes. I don't like taking additional meds unless I'm positive they're warranted. Steroids can do more harm than good. I don't want to take them for every upper respiratory infection I have. I tend to get sick every 3-4 months so that's 3 or 4 courses of prednisone per year, which shouldn't be happening when I'm on two daily controller meds (one of which is also a steroid). So, yeah, I get frustrated. It's not healthy for me to be taking prednisone after every cold.
I'll get over this. 👍💖 Missing my surgery because I'm sick doesn't sound so bad, tbh. I'm really dreading it. 😂
I should have called my pulmonologist but I don't call him unless I'm actually dying lol.
2 notes
·
View notes
Text
Information Overload
The past 2.5 weeks have been nothing short of exhausting and an absolute rollercoaster. My Oncologist called me with the results of the PET scan however it was very vague. He said it was more extensive than just in my skin. He said maybe it was in my bones, spine, lungs, lymph nodes, neck...WHAT????? After all those negative tests somehow without any symptoms I have cancer metastasized to all these areas in a matter of 2 weeks?
We spoke about getting into see the TNBC specialist in Madison and I asked him how quicky that could happen. He said she was travelling right now and wouldn't be able to see me but that she would refer me to a colleague there who was a breast cancer specialist, although not a TNBC specialist. He mentioned it would happen in 1-2 weeks and they would call to set it up. I hung up the phone and did not feel good and I had a ton of questions.
I had looked up information on Cancer Treatment Centers of America and decided to start a conversation with them. I spent an hour and a half on the phone with them talking about getting a second opinion. I spoke with a scheduling nurse and an intake nurse that night. I spoke with a Nurse Navigator to provide a complete history and records release authorizations, and got set up for a 3 day evaluation for a second opinion.
LOTS has happened since then...
* The day after I got my PET scan results, my medical system called me, randomly, to do a survey. Of course I did it. I provided feedback about the surgeon (whom I will not see again), my oncologist, and the fact that i felt like my medical team who I had trusted for a year suddenly was jumping ship. I also mentioned that they didn't seem to know what to do, which is OK - just tell me that and tell me you're going to get me in front of the right people. I also mentioned that I was seeking a 2nd opinion from CTCA.
* The following Wednesday I went to a tailgate at a Brewers Game with my work friends. This gave me a much needed burst of strength and comfort. I did not attend the game however...because:
* The doctors at Madison called and set up appointments for me with the Oncologist and Radiation Oncologist the afternoon of the Brewers Game. I went to those and got some good information. Bottom line, I should have more genetic testing done on my tumor, including PDL-1 which hadn't been done yet. I should also have another biopsy based on the PET scan and where it was felt they would get the most concrete and usable information. I was praised by the oncologist for finding the 2 small nodes and acting on them right away (this felt really good). The Radiation Oncologist told me if it were him he'd hit it and hit it hard, being as aggressive as possible. I asked about immunotherapy and they said there were some trials that I could possibly get into. They would communicate with my oncologist, Dr. Mohammed and he would get back to me with his plan.
* Last Friday I had day 1 at CTCA. I met with my nurse navigator, my internal physician, the chaplain services, and insurance/billing services. The internal MD entered the room with all my records, printed out, highlighted, tagged, underlined, etc. He had done a lot of reading on me! He asked me more questions about the course of my treatment, etc. He was assembling my team and told me he was the team captain, he was going to get me in front of any and all who are needed for my care. I left that day with a sense of peace, and many more appointments & tests scheduled.
* Monday was day 2 at CTCA, I had a PT eval for my arms an for any swelling from losing 36 lymph nodes. They gave me more exercises but said overall there wasn't much and i should be proud of what I was doing. I also had routine labs (CBC, CMP, Iron Studies, and tumor markers) and an echocardiogram to monitor my heart for any changes from the chemo.
* Monday I also had a follow up with the Pulmonologist who did my lung biopsy and is treating for pneumonia. Based on increased coughing since tapering down to 20 mg of prednisone, we decided to go back up to 30 mg right now. He also went over the results of the PET scan and said there was an area of consolidation in my right lung that lit up that he'd like to biopsy to see what we were dealing with, cancer or infection. He mentioned that typically my type of pneumonia is treated with a taper over 6 months, but we were trying to do 6 weeks because i needed to start Xeloda. He said it would be easy to get to and he would dicuss with Dr. Mohammed.
* Monday I also received a call from Dr. Mohammed to go over my visit with Madison. Dr. Mohammed recommended getting a biopsy of my spine because he was concerned with metastasis to the bone, and also to biopsy a lymph node in my neck. I mentioned the lung biopsy recommendation from the pulmonologist and he said he would talk to him but he didn't believe it was necessary. He wanted me to first get an MRI of my spine however since the CT scan didn't show what the PET scan showed. His office would call me to set this up.
* Tuesday (yesterday) was day 3 at CTCA. I met with a Mind Body Consultant and spoke about that care with him would be integrated with my treatment to help me handle the mental aspects of going through this. I met with a nutritionist who went over my diet and labs and made recommendations on how to keep my body as strong and Immune as possible. I met with a Natropathic MD who will incorporate natural supplements while I am going thru treatment to combat side effects and strengthen my immune system. They also offer acupuncture there as an adjunct treatment. I met with my Oncologist and this was incredible. He went over my history, asked about the recommendations from Dr. Mohammed's team, and gave his recommendations. He brought in a Pulmonologist at the same time to go over my PET scan and they came up with a plan to biopsy those areas on the PET scan that measured the highest, they used objective data, not just a "concern" to make their recommendation. They talked about treatments and how I could be treated for the recurrence and pneumonia at the same time. I could be treated with a lower dose of Xeloda and possibly immunotherapy at the same time. There was immunotherapy approved earlier this year by the FDA that they would consider and if it wasn't right there were other immunotherapies available. They would get genomic testing on my tumor and biopsies and decide on what was best. So many possibilities and hope. These two physicians put my mind at rest which had been racing nonstop for weeks. They discussed was my Tumor Marker Results which were all normal except one whch was 4 points above the high range. They said we may be looking at very early and limited disease.
One thing the pulmonologist said was Organizing Pneumonia is very inflammatory and could cause my lymph nodes to swell and other things to show up positive on the PET Scan. Wouldn't that be something...if it was just in my skin and the rest was because of the pneumonia.
Today I am taking it easy. I made a decision to move forward with CTCA for now, I will have the biopsy next Tuesday. I am holding off on the MRI of my spine. I'm uncomfortable with having my spine biopsied, I don't want part of my spine removed. Especially when I have no symptoms. Objectively the doctors at CTCA said the lit up portion of the spine didn't register very high and could likely just be inflammation. They also said it would not be an easy procedure and the area that was wanted could actually be missed because it was so small. I agree, let's go after the most significant area and figure it out. When I asked if the treatment would change if I did have a biopsy of my spine, they said that it would not, it would be treated the same, as metastatic breast disease and treatment types would depend on my genomic testing on the biopsies.
My peace of mind is slowly returning. My helplessness is slowly slipping away, and my hope feels renewed. I'm going to be OK. I read something that said that there is no such thing as dying. You're either alive, or your dead, nothing else. It's true. I am alive and will be alive for a long time. My story is just going to be a bit more interesting...

9 notes
·
View notes
Video
youtube
In this video, Dr. Manteris tells you what we're all about here at Broomfield Spine + Injury, as well as how to refer your friends to our company.
Hello, my name is Nick Manteris, I’m the treating doc and owner here at Broomfield Spine + Injury. Several of my patients in the last couple of weeks had said that they want to send in some friends and family. I love that, the problem they’re saying is that there’s nothing out there that really shows anybody what we’re about here in this clinic. So this is just a short video, it’s an introduction just to tell you a little bit about who we are.
We are located in Broomfield we’re half a mile down from the Wadsworth Highway 36 interchange, 2095 West 6th Avenue. Really pretty easy to get to from anywhere in this area. It’s a small kind of family feel clinic, there’s only three of us that work here.
We specialize in back pain, neck pain, and headaches that are actually coming from the spine. One of the strongest aspects of chiropractic is chiropractors are able to really practice the way they want to. Very much how MD’s have specialties, so do chiropractors. Just the public at large doesn’t seem to know that. One of the biggest weaknesses of chiropractic is the same thing. So, if you’re in this clinic and you had great results, and you told a friend or family member to seek chiropractic care for the back pain, and they went to a different chiropractor. This is fine, but that chiropractor may not practice anything like the way we do here. The downfall of that is the family member then says, “Oh chiropractor didn’t work for me.” I think it’s really important to make a point of if you have a gallbladder attack and you went to a pulmonologist, it wouldn’t work for you either. So again what we specialize in here is this. The most common cause of chronic spine pain and chronic pain in the low back of the neck is ligament damage.
We pride ourselves in actually being to identify the location and severity of that damage, of that injury. We take a very traditional biomechanical approach to the analysis and treatment of spine pain. About 60% of headaches come from some sort of neck involvement and so, we can easily determine if that is the case and then we can go along treat it. Now if you come in or if you call and we have a chat, and it doesn’t look like that this is a good fit for you, that’s ok. We, me, lulu, we will get you the right person. Your health is everything, without health, all is lost. Anything on earth to maintain its health takes a level of care, attention, and expertise. That’s what we’re hoping to bring to our patients here. If we don’t have that expertise, we’ll find out who does. I’ve had other practitioners do that for me in the past and it was literally a lifesaver. That’s all I got, I’d love it if you would call to see if we can help you our phone number is 720-508-3982. We’re here to help and if we can we’d be happy to do it. Thanks for taking the time.
Broomfield Spine and Injury offers the best chiropractic & spinal injury treatment in Broomfield, Colorado. Dr. Nicholas Manteris is committed to providing you with the best and highest quality health care treatment for patients experiencing chronic aches and pain. This can be injuries you’ve sustained from an automobile accident, an injury from your job, or from military affairs. Broomfield spine and injury wants to help you return to your daily lives free from pain.
Contact us here at 720-508-3982 or visit our website to book an appointment with us.
#Chiropractic Broomfield#Chiropractor Broomfield#sciatica pain treatment Broomfield#chiropractic adjustment broomfield
0 notes
Text
‘Tears of joy’
With all the hurdles he had to jump—all the roadblocks he ran into along his transplant journey—no one would have blamed Holsey James if he’d just stopped fighting.
He wouldn’t have been alone in thinking he was too ill to get a pair of donor lungs.
But Holsey didn’t know how to quit.
And his doctors conspired with him, refusing to withhold hope, no matter how bleak things looked.
“I knew I wasn’t giving up. I don’t know how to give up,” said Holsey, 68, of Muskegon, Michigan.
“I would always pray, ‘Just help me get through this.’”
A second chance
With grit, resilience and quality care, Holsey battled his way back—first from prostate cancer and later from weeks on life support following a cardiac arrest—to earn a spot on the UNOS lung transplant waiting list.
That’s not to mention the ruptured intestine, internal bleeding and other issues he experienced along the way.
A turnaround like Holsey’s is stunning, according to Anupam Kumar, MD, a pulmonologist and critical care physician with the Spectrum Health Richard DeVos Heart and Lung Transplant Program.
“It’s an amazing story because, basically, he came back from death,” Dr. Kumar said.
“He came back from death to get a lung transplant to get a second chance at life. So that’s—that’s quite unheard of, to be honest.”
Holsey blames his lung disease—COPD—on years of smoking and working in metal foundries. Though he quit both more than a decade ago, the damage had been done.
For years, he hid from his family how much he struggled to breathe.
“I kind of tried to fake it,” he said. “By not telling them, I thought I was protecting them.”
By 2014 he could no longer hide his illness. When his wife, Gloria, accompanied him to the doctor one day, he left the office on oxygen.
“I was shocked,” Gloria said. “That’s how we first found out.”
Four years later, Holsey’s breathing reached a crisis point. Though he’d tried keeping up with pulmonary rehab, he could no longer drive his car, hold his grandchildren or do much of anything.
“About the last year, he just stayed in that room watching TV,” Gloria said.
In the spring of 2018 Holsey’s doctor referred him to the Spectrum Health lung transplant program.
That’s when Holsey met Dr. Kumar, who began an extensive evaluation process to assess his fitness for transplant.
“(Dr. Kumar) gave me hope every time I would go to that clinic,” Holsey said. “When I was being evaluated, he just made me feel that this was possible.”
First hurdle
Things looked promising for Holsey until he hit his first hurdle: a prostate cancer diagnosis.
That instantly disqualified him from the transplant list.
But Holsey learned that his cancer was limited and treatable. If he could beat it, the clinic might still be able to list him for transplant.
Resolving to fight, Holsey underwent radiation treatments in Muskegon—five days a week for two months.
His family gave him a lot to live for, he said, holding back tears.
“I couldn’t see leaving them alone. My wife and kids, my grandkids—I just couldn’t see leaving them alone. I was more scared about that than dying.”
Holsey emerged from his radiation treatments cancer free and ready for the transplant list.
His insurance company thought otherwise. It took advocacy from Dr. Kumar to convince his insurer to approve transplant coverage.
In November 2018, Holsey finally made it onto the list and began his wait—at home in bed, with 24/7 oxygen support.
New obstacles
In the new year, Holsey’s situation slipped from bad to worse. In late January he landed in the ICU at the Spectrum Health Fred and Lena Meijer Heart Center with respiratory failure.
Dr. Kumar stopped to see Holsey on his rounds the next day, arriving just in time to see his code blue button light up.
Holsey’s breathing and heart had stopped.
With his intimate knowledge of his patient, Dr. Kumar knew exactly how to respond.
“Immediately, as soon as he had a cardiac arrest—luckily that happened in the ICU and I was there—we involved the cardiac ICU team and put him on a machine called ECMO,” Dr. Kumar said.
The ECMO machine took over his breathing and circulatory functions, giving his body a chance to rest.
Holsey was again too ill to undergo a transplant, so the lung transplant team deactivated his status on the list.
All bets were off.
During his weeks in the ICU, Holsey faced a string of new challenges, including a ruptured intestine that required emergency ileostomy surgery.
“There was so much going on,” Gloria said. “It seemed like everything started going wrong and I was about ready to give up because I’m like, ‘God, if he’s got to keep going through this—he’s suffering too much.’”
But Holsey kept fighting and praying—“Help me get through this.”
He came off ECMO.
Then, with a trach tube and ventilator helping him breathe and a feeding tube providing nourishment, he began to recover.
So his doctors made him a pledge: If he grew strong enough, they would put him back on the transplant list.
“And I can remember thinking to myself, ‘I’ve got this much hope and I’m going to do whatever I can do.’
“I grabbed onto that rope and I held on.”
Sheer determination
By the end of February, Holsey made a huge milestone: The transplant team deemed him strong enough for reactivation on the transplant waiting list.
The team may have been as surprised as he was.
“Because he was going through so much, we never really thought he would be active on the list again,” Dr. Kumar admitted. Holsey’s sheer determination drove his rebound, the doctor said.
Holsey transferred to a local rehabilitation hospital and began physical therapy while he waited for a match. With the transplant clinic monitoring his progress and his family cheering him on, he increased his stamina.
About three weeks later, on March 22, 2019, Holsey received a phone call from his transplant coordinator, Jenee Carney.
“I’ve got good news—we got you some lungs,” he heard her say.
“It was almost surreal to me,” he said. “I didn’t think I was well enough, to be honest with you. I still felt so weak.”
Back at the Fred and Lena Meijer Heart Center, Holsey steeled himself for surgery as his surgeon, Edward Murphy, MD, awaited the final go-ahead.
“I was with Dr. Murphy outside Holsey’s room when we got the call from our team at the donor hospital telling us the lungs looked great and it was time to move him to the OR,” Carney said.
“Dr. Murphy let me tell Holsey and Gloria everything was a go,” she said. “I remember Gloria wrapping me up in a big hug and crying tears of joy.”
After all she’d seen him through, all the mental stress she bore as she walked this road beside him, Gloria finally could see the light at the end of the tunnel. She knew Holsey would be OK.
“It was just a great feeling,” she said.
Gloria can’t say enough about the support the family received the whole way through.
“I just love Dr. Kumar and Jenee. They kept us going. They didn’t give up,” she said.
“The chaplains, too—they prayed with us and visited us every day.”
New start
Despite his grit and his providers’ encouragement, Holsey, in the depths of his struggles, sometimes wondered, “Am I deserving of this?”
A year later, those doubts are gone.
Holsey has a new life and he’s not afraid to talk about it.
“I think I’ve got something to share—my experience and my strength and my hope,” he said.
Drawing on the college degree he earned at age 59—just before his COPD became debilitating—he now works part-time as a life coach for families navigating issues surrounding substance use.
“Anything that will help people,” he said.
He also hopes to advocate for organ donation, knowing the profound difference it’s made for him.
“I’m still living because somebody cared.”
‘Tears of joy’ published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
‘Tears of joy’
With all the hurdles he had to jump—all the roadblocks he ran into along his transplant journey—no one would have blamed Holsey James if he’d just stopped fighting.
He wouldn’t have been alone in thinking he was too ill to get a pair of donor lungs.
But Holsey didn’t know how to quit.
And his doctors conspired with him, refusing to withhold hope, no matter how bleak things looked.
“I knew I wasn’t giving up. I don’t know how to give up,” said Holsey, 68, of Muskegon, Michigan.
“I would always pray, ‘Just help me get through this.’”
A second chance
With grit, resilience and quality care, Holsey battled his way back—first from prostate cancer and later from weeks on life support following a cardiac arrest—to earn a spot on the UNOS lung transplant waiting list.
That’s not to mention the ruptured intestine, internal bleeding and other issues he experienced along the way.
A turnaround like Holsey’s is stunning, according to Anupam Kumar, MD, a pulmonologist and critical care physician with the Spectrum Health Richard DeVos Heart and Lung Transplant Program.
“It’s an amazing story because, basically, he came back from death,” Dr. Kumar said.
“He came back from death to get a lung transplant to get a second chance at life. So that’s—that’s quite unheard of, to be honest.”
Holsey blames his lung disease—COPD—on years of smoking and working in metal foundries. Though he quit both more than a decade ago, the damage had been done.
For years, he hid from his family how much he struggled to breathe.
“I kind of tried to fake it,” he said. “By not telling them, I thought I was protecting them.”
By 2014 he could no longer hide his illness. When his wife, Gloria, accompanied him to the doctor one day, he left the office on oxygen.
“I was shocked,” Gloria said. “That’s how we first found out.”
Four years later, Holsey’s breathing reached a crisis point. Though he’d tried keeping up with pulmonary rehab, he could no longer drive his car, hold his grandchildren or do much of anything.
“About the last year, he just stayed in that room watching TV,” Gloria said.
In the spring of 2018 Holsey’s doctor referred him to the Spectrum Health lung transplant program.
That’s when Holsey met Dr. Kumar, who began an extensive evaluation process to assess his fitness for transplant.
“(Dr. Kumar) gave me hope every time I would go to that clinic,” Holsey said. “When I was being evaluated, he just made me feel that this was possible.”
First hurdle
Things looked promising for Holsey until he hit his first hurdle: a prostate cancer diagnosis.
That instantly disqualified him from the transplant list.
But Holsey learned that his cancer was limited and treatable. If he could beat it, the clinic might still be able to list him for transplant.
Resolving to fight, Holsey underwent radiation treatments in Muskegon—five days a week for two months.
His family gave him a lot to live for, he said, holding back tears.
“I couldn’t see leaving them alone. My wife and kids, my grandkids—I just couldn’t see leaving them alone. I was more scared about that than dying.”
Holsey emerged from his radiation treatments cancer free and ready for the transplant list.
His insurance company thought otherwise. It took advocacy from Dr. Kumar to convince his insurer to approve transplant coverage.
In November 2018, Holsey finally made it onto the list and began his wait—at home in bed, with 24/7 oxygen support.
New obstacles
In the new year, Holsey’s situation slipped from bad to worse. In late January he landed in the ICU at the Spectrum Health Fred and Lena Meijer Heart Center with respiratory failure.
Dr. Kumar stopped to see Holsey on his rounds the next day, arriving just in time to see his code blue button light up.
Holsey’s breathing and heart had stopped.
With his intimate knowledge of his patient, Dr. Kumar knew exactly how to respond.
“Immediately, as soon as he had a cardiac arrest—luckily that happened in the ICU and I was there—we involved the cardiac ICU team and put him on a machine called ECMO,” Dr. Kumar said.
The ECMO machine took over his breathing and circulatory functions, giving his body a chance to rest.
Holsey was again too ill to undergo a transplant, so the lung transplant team deactivated his status on the list.
All bets were off.
During his weeks in the ICU, Holsey faced a string of new challenges, including a ruptured intestine that required emergency ileostomy surgery.
“There was so much going on,” Gloria said. “It seemed like everything started going wrong and I was about ready to give up because I’m like, ‘God, if he’s got to keep going through this—he’s suffering too much.’”
But Holsey kept fighting and praying—“Help me get through this.”
He came off ECMO.
Then, with a trach tube and ventilator helping him breathe and a feeding tube providing nourishment, he began to recover.
So his doctors made him a pledge: If he grew strong enough, they would put him back on the transplant list.
“And I can remember thinking to myself, ‘I’ve got this much hope and I’m going to do whatever I can do.’
“I grabbed onto that rope and I held on.”
Sheer determination
By the end of February, Holsey made a huge milestone: The transplant team deemed him strong enough for reactivation on the transplant waiting list.
The team may have been as surprised as he was.
“Because he was going through so much, we never really thought he would be active on the list again,” Dr. Kumar admitted. Holsey’s sheer determination drove his rebound, the doctor said.
Holsey transferred to a local rehabilitation hospital and began physical therapy while he waited for a match. With the transplant clinic monitoring his progress and his family cheering him on, he increased his stamina.
About three weeks later, on March 22, 2019, Holsey received a phone call from his transplant coordinator, Jenee Carney.
“I’ve got good news—we got you some lungs,” he heard her say.
“It was almost surreal to me,” he said. “I didn’t think I was well enough, to be honest with you. I still felt so weak.”
Back at the Fred and Lena Meijer Heart Center, Holsey steeled himself for surgery as his surgeon, Edward Murphy, MD, awaited the final go-ahead.
“I was with Dr. Murphy outside Holsey’s room when we got the call from our team at the donor hospital telling us the lungs looked great and it was time to move him to the OR,” Carney said.
“Dr. Murphy let me tell Holsey and Gloria everything was a go,” she said. “I remember Gloria wrapping me up in a big hug and crying tears of joy.”
After all she’d seen him through, all the mental stress she bore as she walked this road beside him, Gloria finally could see the light at the end of the tunnel. She knew Holsey would be OK.
“It was just a great feeling,” she said.
Gloria can’t say enough about the support the family received the whole way through.
“I just love Dr. Kumar and Jenee. They kept us going. They didn’t give up,” she said.
“The chaplains, too—they prayed with us and visited us every day.”
New start
Despite his grit and his providers’ encouragement, Holsey, in the depths of his struggles, sometimes wondered, “Am I deserving of this?”
A year later, those doubts are gone.
Holsey has a new life and he’s not afraid to talk about it.
“I think I’ve got something to share—my experience and my strength and my hope,” he said.
Drawing on the college degree he earned at age 59—just before his COPD became debilitating—he now works part-time as a life coach for families navigating issues surrounding substance use.
“Anything that will help people,” he said.
He also hopes to advocate for organ donation, knowing the profound difference it’s made for him.
“I’m still living because somebody cared.”
‘Tears of joy’ published first on https://smartdrinkingweb.tumblr.com/
0 notes
Text
Vic Tapson, MD Transcript 110
Victor F. Tapson, MD, FCCP, FRCP from Cedars-Sinai Medical Group discusses the keys to a proper CTEPH diagnosis. Dr. Tapson also talks about the importance of the CTEPH National Proceedings Conference taking place 11/9-11/10 at UCSD. www.cteph2017.com Dr. Tapson has devoted his medical career to patient care, research, and teaching in pulmonary hypertension (PH) and pulmonary embolism.
I’m Vic Tapson. I'm in Pulmonary Critical Care, and I'm at Cedars-Sinai Medical Center of Los Angeles.
Having been interested in pulmonary hypertension for many years now, and actually pulmonary embolism, this was kind of a combination of my two favorite subjects. CTEPH, or Chronic Thromboembolic Pulmonary Hypertension, is an area that's been dominated by great work that UC San Diego has done and a few other centers around the world.
So, the meeting here today is one with a lot of experts here, a lot of great lecturers. We're trying to advance this field of CTEPH, to learn how to mainly make people more aware of this disease. Not just lay people and community, but physicians. Physicians miss this diagnosis, it's hard to read on CT scan. So, you order a CT for something and people might think, "Oh, there's so scarring in the lungs" but they may not diagnose the actual clot. So, this is a significant cause of Pulmonary Hypertension, and one of the really important things about it, it's one of the few curable causes of Pulmonary Hypertension. So, awareness is a big deal. We have new drugs for this disease, which is FDA approved, for treating this disease. That drug doesn't take the place of surgery, but it's a very important drug for patients who either can't get surgery, or have surgery and still have some residual Pulmonary Hypertension.
One of the topics I was asked to talk about was something called vena cava filters, or IVC filters. These filters we put in patients that have Acute Pulmonary Embolism. Blood clots in the lungs are acute, especially if they have reasons we can't put them on a blood thinner, or they have recurrent clots in spite of being on a blood thinner. But there isn’t great data on when to use these, and in CTEPH it's been pretty much the standard of care. When someone's diagnosed with CTEPH, not only are they anticoagulated and considered for surgery, but we usually we put an IVC filter.
We had a nice debate discussing the pros and cons. We don't have a lot of data saying these filters ought to be put in, but they make us feel more comfortable. You put this filter in the vena cava, if a clot does form in a leg, you can't get to the lung. So, most of us I think are pretty comfortable that the benefit outweighs the potential risk of procedural complications, filter clotting, things like that. So, it was kind of an exciting debate, we had good discussion, and the entire meeting has been that way. It's been discussions, debates, areas where we don't have a lot of data. Discussions by experts who have been doing this for many years, that have opinions one way or the other, and we share opinions, we try to come to conclusions. One of the other great things about this meeting is, just getting ideas for future studies, future things we need to do. Whether it's finding ways to raise awareness, or whether it's designing new studies that can be done. So, it's been very exciting.
There's a lot of challenges with CTEPH, as well as with other forms of Pulmonary Hypertension. Patients often have Acute Pulmonary Embolism, they're treated with a blood thinner, they're followed for a period of time. Often the blood thinners stop, they go about their business, and then in a small percentage of cases, but a small percentage in a setting of a lot of Pulmonary Embolisms, I mean hundreds of thousands of cases of acute PE every year in the US. So that's kind of a setting, but only a small percentage get CTEPH, but because there's so many, we think it's a big number.
So how do patients get to us? They usually get more short of breath, kind of like a patient with PAH might develop shortness of breath, or more chronic shortness of breath worsening. Someone finally figures out they have PH, and then they go by our rule, we hope, and get a V/Q scan and figure out this is very likely CTEPH. So, physicians have to recognize this and that's one of the problems with it. The two key things are identify whether there's Pulmonary Hypertension or not, and identify whether it's caused by clotting. Sometimes you identify the Pulmonary Hypertension first, sometimes you identify the clot problem first. You may do a CT scan in someone short of breath, find out they have Chronic Pulmonary Embolism, and they're short of breath enough that you go ahead and get an ECHO. You find suggestions of Pulmonary Hypertension, and you get a CATH and prove it.
Or, you might find someone with PH, you've done the ECHO, you've done the CATH, you know they have PH, and then you say, "Well, could this be clots?" You do a lung scan and find out in fact that it is. So, you kind of come either way, to diagnosis but it's a tough diagnosis. I have a lot of admiration for the surgeons that do what we call PTE surgery, or sometimes called PEA, Pulmonary Endarterectomy Surgery. It's a complex operation that takes time. The key of course, identifying the right patients, making sure they are what we call operable. We believe many if most of these patients are operable.
A surgeon has to go in there, and this is a procedure done on bypass. What they're trying to do is not just get the clot out, like we might find in Acute Pulmonary Embolism, but are trying to get scar tissue out. These clots over time retract and form this fibrous scar on the vessel, so when they get in there, and they look in the vessel, they have to find a dissection plane, find it where this abnormal vessel starts, and then once they start dissecting, go down and pull this clot out. So, unlike just plucking a clot out, with Acute Pulmonary Embolism, there in there dissecting and digging, this procedure is hours and hours long. It takes a very skilled and patient surgeon.
The first thing we recommend if someone is deemed not a candidate, it's got to be that they were deemed not a candidate by an expert center. If that's what they say at UC San Diego, that's the word. If it's a big center, Duke, UC San Diego, Mass. General, one of these places. Cleveland Clinic, where they do a lot of procedures. That's going to be the final word. Maybe a smaller center, less experience, if they say this is an inoperable patient, you probably ought to get a second opinion. Talk to the guys in San Diego, or send the information out. Make sure they're not operable.
Then, if they're not operable, then we go to Medical Therapy. We've used all kinds of Medical Therapy for PH. Now we've got data and FDA approval for a drug that really works here. The reason it works is because this disease is not just clots, scars. These area is what we call smooth muscle proliferation and arterial disease independent of clots. It forms in areas of the lung as a reactive, a reaction to the clot in the lung, to low oxygen levels, etc., and you get this narrowing and constricting of these blood vessels. Frankly, it's great that even in patients who are inoperable, or who those few that have Pulmonary Hypertension left after surgery, that pressure can still come down.
It's very satisfying to see these patients come out, it's a big operation, to see them come out, recover, get out of the hospital maybe in a week or whenever they get out. They've got to be seen in the clinic fairly soon, in a couple of weeks, to make sure there's no post-operative problems, they're healing well, there's no Pericardial Effusion, no evidence of a blood clot in their leg, etc. The key is get them through the surgery. Make sure their diuresed well enough. Make sure their oxygen level's OK, make sure they're healing well, and then I'll tell you, they're on the road to recovery. It's very satisfying.
Less patients are inoperable than were 10 years ago, at a good center. We're learning more about whether we should put IVC filters in or not, we have to study these types of things. Operative techniques have improved, medications have improved, post-op care has improved and it's a team effort. It's Nursing, Pulmonologists, Cardiologists, Surgeons, Physician's Assistants, Nurse Practitioners, Anesthesiologists. It's a real team effort, it's very satisfying. These meetings are multidisciplinary meetings, so I come as a Pulmonologist and I know a lot of Pulmonary medicine, but I'm learning from Cardiologists and Surgeons and Anesthesiologists. So, I love that multidisciplinary aspect of this disease.
I'm Vic Tapson and I’m aware that I’m rare.
Learn more about pulmonary hypertension at phaware365.global. Never miss an episode with the phaware® podcast app. Follow us on facebook, twitter, instagram, youtube & linkedin @phaware #phaware #CTEPH
Listen and View more on the official phaware™ podcast site
0 notes
Text
‘Spiritual care board’ is answer to patients’ prayers
New York (CNN)Gene LoCastro was diagnosed with pulmonary fibrosis in August 2013. The painful disease causes scar tissue to grow inside the lungs, making it difficult to breathe.
"As the lung tissue thickens, your lungs can't properly move oxygen into your bloodstream," according to the National Heart, Lung and Blood Institute. "As a result, your brain and other organs don't get the oxygen they need."
Still, 48-year-old LoCastro says, he felt "more or less OK" until August of last year, at which time he was assured by his pulmonologist that his disease was progressing "normally" and there was no cause for concern.
"I was always in good shape," he said. "I always took care of myself and went to the gym ... worked out three to four days a week, haven't had a drink or drug in over nine years."
But LoCastro says he instinctively knew that something more was going on inside his body and decided to seek a second opinion. He was ultimately diagnosed with dangerous blood clots in his lungs and was admitted to NewYork-Presbyterian/Columbia University Medical Center in October.
"It was downhill from there," he said. In November, LoCastro's heart began to fail. Doctors said he needed a double lung transplant to survive.
"It was pretty nutty, the way it happened so quickly," he said. "But I also ... knew in the back of my head that I was going to be OK no matter what. I kept on saying, 'I've just got to be there for my family, be there for my daughter, my wife; stay strong.' "
A modern-day chaplain
LoCastro says his struggle to regain his strength was, on the whole, more mental than physical. "Physically, I knew I'd be able to get back at it," he said. Mentally, he tried to keep a positive attitude and did a lot of meditation to stay centered.
Shortly after arriving at NewYork-Presbyterian, LoCastro remembers, his social worker asked whether he wanted to see a priest or a chaplain. Because he considers himself more spiritual than religious, LoCastro opted for the latter and was introduced to nondenominational chaplain Joel Nightingale Berning.
"We just connected right away," LoCastro said of Berning. "We had a lot of the same interests. We just talked about life in general. Didn't have to be religion or anything else. ... Could've been baseball; could've been family."
By the time LoCastro was scheduled for a double lung transplant in December, Berning had become an invaluable member of his care team, right alongside the hospital's medical doctors and nursing staff.
"Nobody comes to the hospital wanting to be in for spiritual care -- at least not consciously," Berning said. Once they arrive, however, some patients have straightforward requests, such as physical items they need in order to pray. "The less straightforward requests are the existential questions -- emotions, feelings, spiritual pain -- that come out when people get new diagnoses or are trying to cope with some nightmare they never wanted to be in, or their batteries are low after a really long course (of treatment)," he said. "We try to be what they need us to be."
One of the challenges faced by LoCastro, and many other patients in an intensive care setting, is an inability to effectively communicate wants and needs. ICU patients are often awake and alert but intubated, meaning they have tubes down their throat and can't talk.
"My training was mostly about how to have conversations with people about their soul, whether literally or metaphorically," Berning said. "When I started out (in the ICU), I felt very useless and frustrated. I felt like I had something to offer if we could talk ... but if they don't have a physical voice, it was a real stumper."
That frustration sparked an idea that transformed LoCastro's hospital stay. Berning had long observed doctors and nurses using communication boards so patients could clearly express their physical needs. He remembers thinking: Why hasn't anyone developed a board to help patients express their spiritual desires?
Modern-day spiritual care
Berning got to work, along with his fellow chaplain, a Buddhist monk and professional artist named Seigan Ed Glassing. Together they drew up -- quite literally -- the first spiritual care board.
"Chaplains, we often talk about four basic 'flavors' of feelings: mad, sad, glad and 'afrad' -- or afraid," Berning said. "We laid it out in those columns and tried to make it very ... inclusive, colorful and easy to interact with.
"Instead of 'I'm nauseous, and I'm in pain,' it's 'I'm lonely,' 'I'm scared,' 'I'm frustrated,' 'I'm worried,' " he said. "Instead of 'turn me,' 'suction me,' 'toilet me''; it's 'hold my hand,' 'play music,' 'pray,' 'get a priest' -- stuff like that."
LoCastro began utilizing the board after his operation, when he was rendered unable to speak for weeks on end, while his body recuperated from the double lung transplant. More than using it to make requests for specific things, LoCastro sought to express how he was feeling, which didn't at all surprise Berning.
"What are (most patients) feeling and experiencing?" Berning asked rhetorically. "Most of it -- or a lot of it -- was really as you'd guess: a lot of frustration, a lot of sadness, a lot of fear. The second most commonly identified emotion was loved, which really surprised us. And I don't have an answer for exactly why that is, but it's my favorite finding, because I like to think that when people are critically ill, they do have a lot of scary, horrible, awful feelings, but we are also trying to give them as much love as possible."
Modern medical technology
"One of the biggest changes in critical care medicine over the last decade is that we try, whenever possible, not to sedate patients and not put them in medically induced comas when they're on life support -- especially (a breathing machine)," said Dr. Matthew Baldwin, a pulmonary and critical care physician at NewYork-Presbyterian who was not involved in LoCastro's care. "Studies over the past decade have shown that ... patients who receive less sedation tend to have better physical function and even better mental function."
That said, this new paradigm of care has also presented a new problem, says Baldwin. Patients are awake and alert but unable to effectively communicate.
"Oftentimes, I walk around the ICU, and I'll see a patient on a ventilator, wide awake, sitting up in bed," he said. "They'll be tapping on the side of the bed. Clearly they're anxious. You can just see it on their face."
Baldwin remembers the first time he saw Berning in the ICU, sitting at a patient's bedside, holding the spiritual care board and a dry-erase marker.
"I stood there for a moment, and I thought it was the most wonderful thing, because ... what you see is a calm patient sitting there and pointing to these things, smiling at times and nodding, despite all the numbers up on the screen, despite the mechanical ventilator at their side, giving them the breaths that they themselves alone cannot breathe. We realized immediately that this was transformative. We used to call chaplains for our consult for death, and now we call them for a consult for life."
Together, Baldwin and Berning conducted a study on how effective the board was at addressing the spiritual needs of their ICU patients. Before using the board, the 50 patients who participated rated their level of anxiety as an average of 64 on a scale of 0-100. After using the board, their average self-reported anxiety level dropped to 44, a reduction of 31%.
"It helps the patient better contextualize their illness and think about what they need to do, psychologically, to pull themselves through it and to get back on their feet," Baldwin said. "It's these coping mechanisms that we've never provided the patients before while in the ICU, is what makes this so exciting."
Like many survivors of a critical illness, LoCastro says he's battled some depression. And, Baldwin says, this is the area in which his study saw its most promising results.
"Patients said that they ... were better prepared to cope with their continued recovery after hospitalization," he said. "And they felt more at peace with who they were and what they had gone through."
See the latest news and share your comments with CNN Health on Facebook and Twitter.
For his part, LoCastro believes so highly in the power of the spiritual care he received that he regularly returns to NewYork-Presbyterian to offer words of encouragement to patients in the ICU. Like Baldwin and Berning, he hopes more hospitals across the country will integrate the spiritual care board (now licensed and sold by Vidatak) into their standard of care.
"Look, I just want to get healthy," LoCastro said. "I have two new lungs. I'm doing better than ever. I'm at 100% oxygen. I want to live a long time, and there's no reason why I can't."
More From this publisher : HERE
=>
***********************************************
Read Full Article Here: ‘Spiritual care board’ is answer to patients’ prayers
************************************
=>
‘Spiritual care board’ is answer to patients’ prayers was originally posted by A 18 MOA Top News from around
0 notes
Text
In This Technology World, We Live
Top Picture Credits Marvin Meyer/@marvelous
Powered by Unsplash
Technology has turned out excellent, but to sit as we all watch it grow, but leaving some of society out of this equation, is unacceptable behavior. The developers need to stop and rethink how they're developing for the communities' most astonishing invention, taking away from all our lives now but is the way we all do business, which is excellent.
So please, don't take this article out of its context.
I decided to add to some feedback I gave on Windows 10 and how my browser displays pages, and how my laptop was running, which has sparked this article.
To make things even more accessible to those who have difficulties comprehending things due to life-changing incidents beyond his/her control and that of human nature. Sometimes life-altering changes happen to one's life that turns out in debilitating un-expectancies.
For instance, "I had died over a year ago and was placed on life support for a bit. I lost 68% oxygen to the brain, leaving my body and brain getting 32%, `which the doctor's hoped would return to normal,' but instead, the way things have turned out for me today, "I have difficulties comprehending something."
All I do, is keep asking for help because I have problems understanding something, or it takes me longer to learn something, more times than not?"
I get nowhere asking, why do you think that is? Perhaps the lack of compassion or caring of someone that has a disability? Then try to sell you something to make it work for you, despicable.
Or when I go for walks to circulate blood flow, the blood clots could start forming in my arteries from peripheral artery damage. But I get winded easily, even if it's a block but lose oxygen and then struggle for air from another health condition. Still adding fuel to the fire, it was the loss of the oxygen in the first place, while on life support, that's caused all this.
And I have been asking the pulmonologist to be put on oxygen to get out more for blood flow.
My primary doctor saw this first hand now walking about 2000 yards and was quite concerned from the oxygen telemetry meter reading of 62% and waited about 15 minutes and retook it, reading still the same. It wasn't until 30-45 minutes later I left when my oxygen was about 82%.
The intake nurse is the one that first saw this and said, well, maybe it was the meter and went to get another one; really, she went and told the NP what was happening. All the time, I was struggling to breathe, which I knew eventually would come back up.
But, in walked my doctor or NP, that's whom I see actually, and put her hand on my shoulder, William, are you ok? Well, no, this is how I get when I walk. I have my inhalers here; I haven't smoked but two cigarettes this morning. From the walk from the main road, Creasy Lane in front of the hospital, to the back here, with these results.
I go through this all the time, and the pulmonary doctor knows this and still won't give me oxygen, a "broken-down society." If I die again from this, there isn't any turning back the next time and no life support next time either; I'm tired, I have a DNR in place, sad as me saying this, because of a "broken-down society."
Instead of leaving within us unresolved questions with no one having answers to them, and going within ourselves, creating even more frustrations to an individual needs? "People couldn't possibly know what that feels like and don't understand the life of another person's journey and what they face already unless you’ve walked in their shoes.
Inside the individual, leaving them rendered to the feeling of the uncompassionate care they see in their eyes, and now, a new journey for them; they must walk through life this way, which is unacceptable but, undoubtedly understandable in a "broken-down society."
It's true; "I might be having these difficulties that others couldn't possibly understand." But still, one thing is for sure, "society is broken-down when other individuals boast about helping in a disability world of unexpected turnouts and leave them with an unsettledness inside because of the lack of helping."
"Before we can start to make changes in this broken-down society of uncaring people, `these changes begin within ourselves first, before they emanate outward."
"However, this is an official viewpoint that leaves me still very "Thankful," how I need to proceed with my journey through life, `which helps me become a better person today than yesterday."
I am a writer, and I too rely on this technology for writing; I like it or love it; it is part of whom I've become today. "I cannot explain how I can sit here and write something like this, but I still have a rough time understanding something now?"
Instead, we add pure cold-heartedness to the equation, sucking the lives out of them or their pockets.
"What happened to the pureness of kindness?"
The lack of help when we ask for it and send you to these pages to read regardless of how "they" want to justify it; it just gets humanity and the people of it, absolutely nowhere.
"It isn't helping anything, but adding to an unresolved solution?"
Try making something better for what an individuals' experiencing; this same incident, for which had, provoked me to write this opinion of the developing developers. Instead of focusing on "ads," please focus on the individuals' experience now?
"It will even make for a better internet experience."
I had no control over losing my life, making my comprehension this way and be this way. Thing's in this life happen for reasons' beyond our understanding, just saying!
Written by:
William Darnell, Sr.
11/26/2020 9:33 PM
0 notes