#renal
Text

Save what can be saved: Day 10/48
Hey!
Histology. I've always found histology too detailed and boring, but only after my clinical rotations that I came to realize how important it is. Histology is the basis of medicine.
I didn't finish it yet but hopefully tomorrow? We will see..
#studzblr#studyblr#algeria#medicine#algerie#studying#study motivation#student#students#khabbach#48 days to save what can be saved#histologie#histology#renal#islamic studyblr#islamblr#islam
53 notes
·
View notes
Text

Kidney Correction
Cellular enzyme RAC1 underlies repair of kidney collecting ducts damaged by prolonged ureteral obstruction by controlling the rebuilding of duct cells' actin cytoskeleton which is co-ordinated with cell division
Read the published research article here
Image from work by Fabian Bock and colleagues
Division of Nephrology and Hypertension, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY-NC 4.0)
Published in Science Advances, February 2024
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#kidneyhealth#kidney#renal#cell division#cytoskeleton
9 notes
·
View notes
Text
Had a pt today who had hyperkalemia. She is a diabetic and was getting heparin for DVT prophylaxis, which can cause type 4 renal tubular acidosis. So her heparin was stopped.
Hyperkalemia that causes EKG changes should be treated with calcium gluconate (or calcium chloride), insulin, Kayexalate. Calcium chloride has more elemental calcium than calcium gluconate, so you would give less calcium chloride if you gave that instead of calcium gluconate. The dose of calcium chloride is 1 gram. The dose of calcium gluconate is 2 to 3 grams. The calcium is simply cardioprotective. Insulin just temporarily shifts potassium into the cells. Dialysis emergently removes potassium from the body. Kayexalate gets rid of potassium in the stool, but can also cause intestinal necrosis (the premixed formulation). I didn't know that! Lokelma and Patiromer (Veltassa®) can be used to get rid of potassium in the stool, and they don't cause intestinal necrosis! We don't have Lokelma or Veltassa at my hospital. Lokelma is really expensive.
You should also correct acidosis in pts who have hyperkalemia by giving them bicarbonate.
I don't remember anything about renal tubular acidosis, but risk factors for type 4 RTA: type 2 diabetes, overweight, older. It's a hyporenin, hypoaldosterone state.
10 notes
·
View notes
Text
Oedema - pitting vs non-pitting
Oedema is swelling due to excess fluids in tissues.
In pitting oedema, pressing on the affected area leaves an indentation (that persists after removing the pressure). In non-pitting oedema, the area feels firm to touch and does not form indentations.
Pitting oedema:
The excess fluid is mainly composed of water
Commonly caused by heart failure, venous insufficiency, or nephrotic syndrome
Non-pitting oedema:
The excess fluid consists of water WITH protein and salts
Usually indicates a condition of the thyroid / lymphatic system
Different types:
Lymphoedema is due to a build-up of lymphatic fluid (e.g. due to a tumour blocking lymphatic flow / after removal of lymph nodes).
Myxoedema occurs in hypothyroidism and often affected the pretibial or periorbital area.
Angioedema is localised swelling of the skin and is usually due to allergic reactions. It typically affects the face, tongue, larynx, abdomen, arms, and legs. When the larynx is affected, it may affect breathing, which is an emergency!
Lipoedema is when fat accumulates in subcutaneous tissues - it usually affects the legs/buttocks and almost exclusively occurs in postpubertal females (not the same as cellulite!)
If patients present with oedema, it's always important to test if it's pitting or non-pitting as this helps to determine the cause and correct treatment!
#med school#medical student#medicine#revision#medspo#medblr#dermatology#renal#cardiology#oedema#pitting#non-pitting#heart failure
31 notes
·
View notes
Text
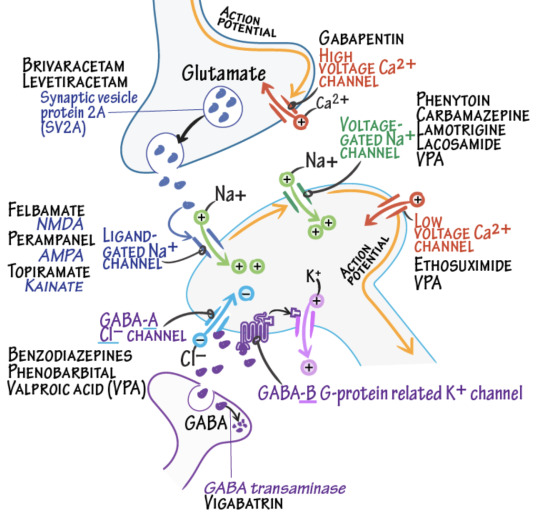
Levetiracetam (Keppra) is one of the few anti-epileptic drugs (AEDs) that is renally secreted. If a patient with seizures on Keppra has renal failure and cannot or does not want to be switched to a different AED, they can have their Keppra renally dosed (after dialysis). Keppra overdose can cause sleepiness, aggression/behavioral problems (peds>adults), hypertension (peds), vomiting.
Image: DrawItToKnowIt
10 notes
·
View notes
Text
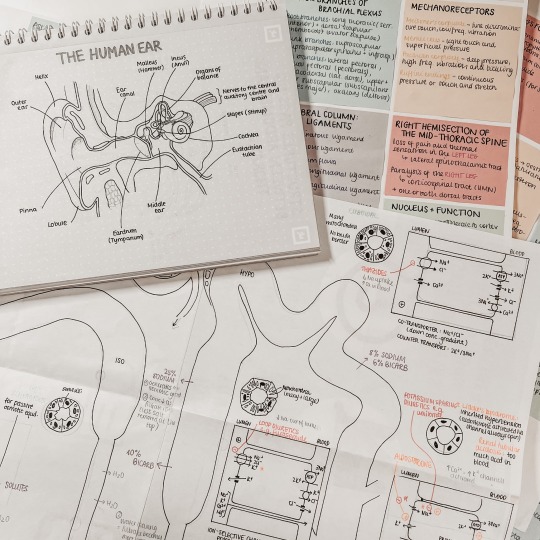
#mine#studykween#study#medicine#medical student#diagram#drawing#biology#kidney#renal#pastel#pastel aesthetic#post it notes
5 notes
·
View notes
Text
Peri-care (Perineal) and Catheter Care Female Patient
This article will review how to perform peri-care (perineal care) on a female patient with a Foley catheter.
For a complete demonstration on this nursing procedure, you can watch the video below:
Perineal and catheter care are an important part of patient care. This helps maintain the patient’s personal hygiene and decreases the risk of a catheter associated urinary tract infections…

View On WordPress
3 notes
·
View notes
Text
Day 1
#med school#get motivated#study aesthetic#dark acamedia#aestethic#studies#library#booklover#apple ipad#renal#barttersyndrome#workplace#student#medicine#harvard#usmleprep#usmle#usmlenotes#residency
4 notes
·
View notes
Text
Dehydration will Destroy your healthy life
Insufficient water in the body is known as dehydration. It has several potential causes and may pose serious health risks. Read this article for a remedy
0 notes
Text
Avanza IMSS Morelos en Programa de Trasplante Renal
🖊️#Salud | Avanza IMSS Morelos en Programa de Trasplante Renal
+INFO:

View On WordPress
0 notes
Text
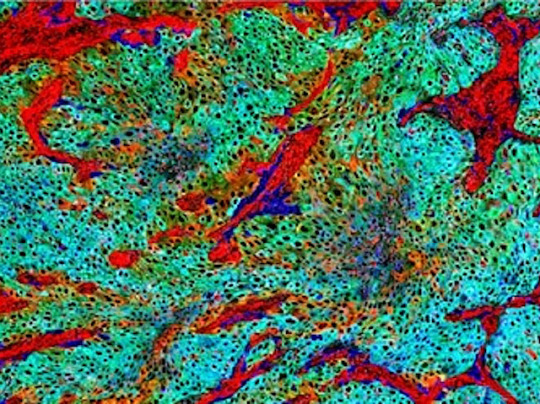
Malignant Evolution
Multi-pronged (whole-exome sequencing, RNA sequencing, and Imaging Mass Cytometry) approach characterises at the single-cell level the heterogeneity of upper tract urothelial carcinoma – cancers arising in the ureter and the kidney's 'pelvis' – from primary to metastatic
Read the published research article here
Image from work by Kentaro Ohara and colleagues
Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, New York, NY, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Nature Communications, March 2024
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#oncology#cancer#urothelial cancer#kidney#ureter#renal#metastasis
7 notes
·
View notes
Text
Vancomycin can cause ATN if the vancomycin level is supratherapeutic. After getting contrast, the Cr can continue to increase and peak 3 to 4 days after getting contrast.
Giving IV fluids and correcting acidosis prevent contrast-induced nephropathy.
Acute interstitial nephritis (AIN) will show WBC casts in the urine. The rise in the Cr level is slow in AIN.
Nephrogenic systemic fibrosis is due to the old type of gadolinium contrast used for MRI. The new gadolinium contrast has not yet been shown to cause nephrogenic systemic fibrosis. Nephrologists recommend not giving this contrast if the GFR is less than 30, but radiology guidelines still give it even if GFR is less than 30. Dialysis doesn't help with preventing the injury due to iodinated contrast.
Bicarbonate correction to greater than 22 helps prevent progression of CKD. Had a pt today who is on sodium bicarbonate to help with preventing progression of his CKD.
3 notes
·
View notes
Text
kidney A+
You need a kidney, contact me to talk
0 notes
Text

Solid renal masses detected incidentally at ultrasound or non-contrast CT are typically evaluated by multiphase CT or MRI (renal mass protocol). Cystic lesions with worrisome features (septa, nodules, significant solid component) also warrant CT or MRI.
Today's case is a 35-year-old man with a right renal mass detected at ultrasound. CT and MRI confirmed the presence of an enhancing solid renal mass. The patient underwent nephrectomy; surgical pathology revealed chromophobe renal cell carcinoma.
Case courtesy of Dalia Ibrahim, Radiopaedia.org, rID: 181044
0 notes
Text
Oliguria = output of < 500mL of urine
Creatinine clearance rate and glomerular filtration rate (both urine tests) decrease in kidney insufficiency, causing an increase in reuptake of BUN, so high serum BUN and creatinine result.
Azotemia results (high levels of nitrogen/urea in the blood)
0 notes