#tardive dystonia
Note
Hey there, do you have some cool sources on other types on involuntary movement that are not tics?
Yes, I do! Here is a list of involuntary movements, a simple description, and links to resources on them:
Akathisia -> an inability to remain still
StatPearls article
cleveland clinic article (very good)
Akinesia -> the loss of spontaneous, voluntary muscle movement
StatPearls article (free article)
healthline article
Athetosis -> slow, continuous, involuntary writhing movements commonly affecting arms and hands
healthline article
Chorea -> rapid, chaotic movements that seem to flow from one body part to another
NINDS article
StatPearls article
Dystonia -> sustained or repetitious muscular contractions; often produces abnormal posture
mayo clinic article
NINDS article
StatPearls article
Hemiballismus -> sudden, intermittent, flinging, or ballistic high amplitude movements commonly affecting proximal limb muscles
StatPearls article
Myoclonus → sudden, brief, involuntary muscle twitches
mayo clinic article
NINDS article
StatPearls article
Parkinsonism -> a clinical syndrome characterized by slowness, rigidity, tremor, and postural instability
StatPearls article
parkinson's disease vs parkinsonism
types of parkinsonism (parkinson's UK)
types of parkinsonism (parkinson's foundation)
Stereotypies -> repetitive, rhythmic movements with typical onset in early childhood
stereotypies in adults
medlink article
Tardive Dyskinesia -> uncontrollable and repetitive movements of the tongue, lips, face, trunk, and extremities
webmd article
Tics -> sudden, rapid, recurrent, and nonrhythmic movements or vocalizations
mayo clinic article on tourette syndrome
NINDS article on tourette syndrome
child mind institute article on tics and tourette
Tremor -> rhythmic back-and-forth or oscillating involuntary movements
NINDS article
classification of tremor
(at request I can find Tumblr or blog posts talking about personal experiences with some of these movements)
Basic definitions come from this article: https://www.psychiatrist.com/pcc/effects/drug-induced-abnormal-involuntary-movements-prevalence-and-treatment/
#asks answered#anon asks#involuntary movements#akathisia#akinesia#athetosis#chorea#dystonia#hemiballism#hemiballismus#myoclonus#parkinsonism#stereotypies#tardive dyskinesia#tics#tremor#links
17 notes
·
View notes
Text
15 years of disability
Here we are, on the an anniversary I never wanted, March 24, 2008.
15 years since acquiring tardive dystonia.
Let’s catch up a bit then, shall we?
First thing; still happily married to the same person, who has also became my primary caregiver.
Which leads me into, yup, I still very much have tardive dystonia and it hasn’t gotten any better. I have good days and bad days. But I’m safe and taken care of.
I also found out that I have an inoperable osteochondroma (bone growth) on my right tibia that has given me no end of acute chronic pain from apparently my early teen years onwards.
I smoke 120g of cannabis a month to manage both the tardive dystonia and acute chronic pain (and the accompanying depression, or whatever having no functional dopamine to speak of is, that goes with such things)
We currently have one cat, her name is Mystique and we’ve had her for a while now. Both Poptart and Charlie passed.
We live on the western end of downtown Calgary, in the Beltline. Great place to be.
COVID-time has compelled me to pretty much stay inside (aside from vaccinations+boosters, doctors appointments, voting and rare time of eating outside or in very well ventilated areas) and while she has to go out to work and deal household related activities, she (and we) both wear masks when we’re not in the apartment (including the hallway to the elevators). We’ve never had COVID and if we continue to be careful, then we may get through this without acquiring it. We’ve forsaken a lot in order to not get sick. We’re getting updated boosters on Sunday!
For my particular point of view, I’m back to living like I was up in Falconridge. Stuck.
We moved, in large part, to the Beltline to not be stuck. At least we’re staying safe.
And if you want to reach out and say hi again, you can ask for my email...
3 notes
·
View notes
Text
anyway um. shoutout to disabled people who move their bodies in ways that are considered "wrong" or "abnormal" regardless of the cause or how it's classified. and this isn't limited to just ambulation.
paralysis. dystonia. gait abnormalities. people with muscle weakness and/or atrophy. people with brain damage. rotational differences. clubfoot. knocked knees. other limb and bodily differences. functional deformities that affect movement. tissue contracture. muscular dystrophies. spasticity. impaired proprioception, balance, and/or coordination. chronic pain. spinal disorders. dyspraxia/DCD. apraxia. ataxia. dystaxia. tourette's syndrome and other tic disorders. conversion symptoms. tremors. neurodegenerative disease. degenerative bone diseases. joint instability. myoclonus. parkinsonism. tardive dyskenisia. various other neurological problems.
...and the list goes on.
personally i feel a bit surreal when my body not doesn't always move in the ways i want it to because that straightforward connection that's there for abled people has been disrupted in a myriad of ways. but no one is gross, ugly, or scary for being unable to move their body in ways that society considers "normal" and "healthy." no one deserves to be gawked/stared at or treated like they're subhuman because of the way their body moves.
it's okay for us to exist.
#cripple punk#cripplepunk#cpunk#neurodivergence#disabled positivity#j#idk a better term for 'functional deformity' bc afaik deformity is a term w/ negative associations#affirmations
6K notes
·
View notes
Text
“Antipsych isn’t about rejecting treatment or drugs, it’s about autonomy, it’s about power, it’s about refusing to accept as self evident a system of carceral state authoritarianism maaaaan Ⓐ”
Yea, well, that’s nice for yr private definition of antipsych. I am against treatment, when the treatment involves fucking antipsychotics
Taking antipsychotics is, under most or perhaps practically all circumstances where it happens , a terrible and shortsighted idea that you should not act on. The psychosis-alleviating primary effects fade in the long term, while debilitating side effects like tardive dyskinesia and diabetes persist, even after quitting the drug. Meaning that one’s initial experience of the drug is not an accurate guide to its overall costs and benefits. And, in the meantime, you get a high chance to experience the agonising all-consuming torture of akathisia or the stupefying self-obscuring haze of zombielike cognitive impairment, both leaving you precious little mental acuity with which to carefully weigh these pros and cons anyway. Later generations of atypical antipsychotics are an improvement in some of these respects, but these risks have not gone away and can still fuck you up for life. It’s not fucking worth it
Do shrinks and friends infringe on patients’ autonomy in forcing antipsychotics on them? Sure. But you know what else constricts the patients autonomy here? The meds themselves. If anything diminishes your bodily freedom, it’s your legs compelled to twitch by akathisia and your eyes and neck twisted up for hours by dystonia. If anything robs you of your personal agency, it’s a permanent stupefied haze incompatible with abstract thought. If someone forces you at gun point to guzzle lead paint, the problem isn’t only—the problem isn’t even mainly—that you didn’t get to choose what you did or didn’t drink: it’s that you have just ingested poison, and this is bad news
Should ppl be forcibly prevented from access to haldol if they have somehow gotten it into their heads this is their heart’s utmost desire? Uhh I mean, ig probably not. Not that this seems like a particularly pressing issue here in the real world. But if yr radical critique of psychiatry as an institution centres an abstract notion of bodily autonomy to the exclusion of the devastating nature of these particular pharmaceuticals, I am tempted to say it is less than useless
162 notes
·
View notes
Text
Which antipsychotics are considered first-generation and why are they used less often than second generation antipsychotics?
Which antipsychotics are considered first-generation and why are they used less often than second generation antipsychotics?
Which antipsychotics are considered first-generation and why are they used less often than second generation antipsychotics? Are second-generation antipsychotics more effective?
Order a plagiarism free paper now
Compare and contrast the following conditions: Tardive Dyskinesia, Acute Dystonia, Athetosis, and Tics.
View On WordPress
2 notes
·
View notes
Text
10/8/23
Fucking did not know I was supposed to be at work today! I was chilling out, enjoying my sunday morning, reading comics and whatever, and I got a call from my coworker. "You know you're supposed to be on the schedule, right?" I showed up two hours late! But my coworkers know me well enough to trust it was an honest mistake, bless them. They gave me shit about it all day.
Today's probably the first time I've ever had a patient where I've really struggled with not engaging with them too much, just because I don't want to cross the patient/nurse boundary. He's the guy from a few shifts ago who works on movies. He's my age and we love all the same stuff. I always feel horrible when my patients get the impression we don't care about them. I'm trying not to go overboard, dammit!
Anyways. One guy on my unit (subacute)'s been having some extrapyramidal symptoms. Really really intense muscular dystonia, throughout his whole body. It looks a lot like the standard kind of tardive you might see in someone's facial muscles, but its all over, and it's been getting worse all day.
See, we get lots of patients who try to fake symptoms for attention from nursing staff. We've been having it happen a lot lately, actually. Patients will show up, start to get better and then somehow mysteriously lose the ability to walk safely, and my goodness gracious they need a bunch of xrays and oh, they can't discharge now, not when they're suddenly and mysteriously ill! Yet every other symptoms the patient doesn't know or recognize or know how to fake won't be present. The patient wants the staff to give them the care and attention they crave, enough so that they'll fake being disabled to get it. It's sad.
So, I'm used to being skeptical of patients suddenly developing skeletal muscle problems while they're on my unit. This guy would say things to me like "I don't get it. I'll be resting, and I'll be fine, but as soon as I start talking to someone or trying to do something I start jerking everywhere!" Which is commonly the way patients like to fake their symptoms; only when someone's watching. But this guy... The thing is, if he was faking it, he was a great actor. He just seemed to know how to struggle with moving in a way that suggested he was not faking it, enough to make me think "yeah this might actually be real."
Staff and I were going over his meds for possible medication interactions for a while, just keeping the doctors appraised of the situation. But his symptoms got steadily worse all day, to the point where he couldn't transfer safely from his (recently acquired) wheelchair to his bed without voiding urine all over himself. Poor guy was seriously getting concerningly worse throughout the day, and that was the moment we knew "Alright, enough with the phonecalls. Doctor needs to be at the bedside."
Not too sure what happened after that. The doctor came up, did his assessment, and it was time for shift change. We gave hand off to the night nurses and now I'm home writing this. It's one of those cases I'm going to be thinking about for a few days, and following up on when I get back.
1 note
·
View note
Text
see below
Which antipsychotics are considered first-generation and why are they used less often than second generation antipsychotics? Are second-generation antipsychotics more effective?
Compare and contrast the following conditions: Tardive Dyskinesia, Acute Dystonia, Athetosis, and Tics.
View On WordPress
0 notes
Video
Actually there’s a couple spots where I could see the possible illusion I spoke about in my last post, so just a reminder that anytime in this video where it looks like I’m looking at the camera, it just means my eyes passed that direction. It’s not an indicator of what I was paying attention to.
So this happened to me during a gallery opening where some of my work was being shown. And while I was heading into extreme shutdown, and often aware less of my surroundings and more of an internal scene playing out in my head way more vividly than it should have(1), I still had the presence of mind to tape this for a minute so I could figure out what it looked like from the outside and maybe ask people questions later.
This was also five years ago or longer. Before my adrenal insufficiency or (probably-congenital) myasthenia diagnoses, but after they had begun to intertwine in extremely unpleasant ways. I now suspect high stress caused my body to enter all kinds of weird states, some of them dangerous. Later that week I took part in a stressful online interaction. It was the last straw that led to my needing to use a bipap (on settings for central apnea that also work for breathing muscle weakness) to aid my breathing muscles for most of the rest of that week.
But anyway -- the things my eyes and face were doing were very common back then when I got tired, overloaded, etc. I was sitting next to a blind woman here, and people assumed I was blind too, and began touching me to get my attention, which only made everything ten times worse. I hate being touched by drunk people and everyone was at minimum tipsy.
Anyway was wondering if anyone has experience with these kinds of eye movements that seem to be related to any of the following singly or in combination:
Autism (and/or cousins)
Catatonia-like and/or parkinson-like movement disorders (and/or cousins)
Myasthenia gravis
Congenital myasthenic syndrome
Adrenal insufficiency (not ‘adrenal fatigue’)
Any of the tardive movement disorders or things resembling them (permanent movement disorders brought on by us of neuroleptic drugs -- tardive dyskinesia, tardive dystonia, tardive akathisia, etc.)
Mayyyybe epilepsy but my seizures don’t normally look like this and I don’t think it was a seizure, just adding it for the sake of completeness
In the case of any of these, I’d be curious to know more. It’s obviously not a big deal given this was 2012, and things like this don’t happen so much anymore. But this used to be an incredibly common thing for my eyes to start doing when I got stressed, overloaded, or tired. It obviously makes m visual processing go to crap.
This nightmare was the last art opening I ever attended. Here’s a crappy photo of the painting (with a lamp and people reflected in the frame). My art never photographs well at the best of times but this one isn’t terrible considering all the reflections and the fact photographing always makes my paintings lose layers and depth:

I am glad I went-- there was a lot of great art there -- but i’d have to seriously question myself if I did it again, and take more precautions. I had been in galleries before this, but this opening was the least pleasant I’ve ever experienced just for the sheer number of drunk people. Drunk people always feel like their personal space bubble vastly overextends beyond their bodies so they’re smashing into me even when they’re not touching me, and touching me is even worse.
I felt very grateful to be included with so many good artists though, and I tried to be polite to the drunk people but I eventually lost the ability to respond at all. Hundreds of them filed by and wanted to talk or touch me or both and I couldn’t say enough to stop them, and my pre-assigned caregiver didn’t know me well enough to know I was in trouble. And you can hear the sheer number of people just on the video.
Also I felt and saw that my eyes were all over the place but I was surprised to later see in the video that other parts of my face were twitching. I didn’t feel that at all at the time.
(1) This sort of thing is highly unusual for me. It felt like I was falling endlessly down a pit and lying on the floor and getting slashed to pieces with something sharp, or something like that. At the time I interpreted it as an impending shutdown so severe that ordinary shutdown didn’t cover the experience.
#actuallyautistic#myasthenia gravis#myasthenia#adrenal insufficiency#catatonia#autistic catatonia#parkinsonism#tardive syndromes#chronic illness#movement disorders#eye movements#involuntary eye movement#involuntary movement#tardive dyskinesia#tardive dystonia#tardive akathisia#selfies#Mel#2012#epilepsy#uncontrollable eye movements#video#medical
21 notes
·
View notes
Text
Dystonia is a condition in which the patient’s muscles contract painfully and uncontrollably. It may be mild enough to not be noticed at first, but intensifies over time. Here, we offer a quick introduction to what Dystonia looks like, why it occurs, and how patients can manage it.
Understanding Dystonia
Dystonia is a movement disorder that causes muscles to contract uncontrollably. The contracture is generally painful and leads to abnormal gestures or repetitive motions. Dystonia can affect a single muscle, a muscle group, or several muscle groups all over the body. It can affect people of all ages.
Symptoms of Dystonia
The symptoms of Dystonia can vary depending on the muscles it is affecting. Common symptoms include:
Cramping in the foot or hand
Pulling in the neck
Involuntary blinking or eye movements
A ‘dragging’ sensation in the leg
Speech difficulties
Pain or exhaustion frequently follow in the aftermath of Dystonia symptoms, while fatigue may exacerbate the symptoms. Patients may also experience depression or social withdrawal because of the stress the disease causes.
Types of Dystonia
One way of classifying Dystonia is on the basis of the parts of the body it affects. Accordingly, there are five types of Dystonia:
Generalized — affecting the whole of the body or most of it
Hemidystonia — affecting the arm and leg on the same side
Segmental — affecting adjacent body parts
Focal — affecting just one body part
Multifocal — affecting more than one unrelated body part
Doctors also classify Dystonia based on its patterns. Some of them, in fact, can be regarded as syndromes in their own right. These include:
Cervical Dystonia (or torticollis) — affecting neck muscles in a manner than causes the head to be pulled backwards and forwards or twisted from side to side
Oromandibular Dystonia — affects the lip, tongue, and jaw muscles and leads to trouble speaking and swallowing
Cranial Dystonia — affects the face, head, and neck muscles and may flare up during specific tasks, such as playing a wind instrument
Blepharospasm — affects the eyes starting with uncontrolled blinking, and ultimately causes the eyes to be almost permanently closed
Paroxysmal Dystonia — affects the body only during episodes
Spasmodic Dystonia — affects the speech muscles in the throat
Torsion Dystonia — a rare disorder that affects the entire body severely
Tardive Dystonia — a treatable form of the condition that occurs because of a reaction to some drugs
Causes of Dystonia
Dystonia occurs due to a problem with the way nerve cells communicate in the basal ganglia, which is the part of the brain that initiates muscle contractions. It could be idiopathic in nature, but more often it is acquired from a stroke, a tumor, brain trauma, infection, or conditions like Multiple Sclerosis or Parkinson’s Disease. The doctor will perform a variety of tests and take a complete medical history to determine the exact root cause. Researchers continue to work on identifying genetic mutations that cause Dystonia.
Treatment for Dystonia
Depending on the severity and its underlying cause, there are several Dystonia treatment options available.
Physical Therapy, involving a combination of strength and stretching exercises to ease muscle pain and improve range of motion
Stem Cell Therapy is designed to repair the damaged cells within the body by reducing inflammation and modulating the immune system
Medicine, which is injected directly into the muscles to ease muscle contractions or taken orally to target neurotransmitters in the brain
Deep brain stimulation, which involves transmitting electrical impulses to the brain to ease the contractions
Speech Therapy, if the Dystonia is affecting the throat, lip, tongue, or jaw muscles
Occupational Therapy to help the patient perform daily tasks more effectively, often with the use of aids
Selective denervation surgery, which may be recommended to cut off the nerves involved in muscle spasms if other types of treatment haven’t been effective
Dystonia can be painful and uncomfortable to deal with, but it can be managed with appropriate treatment. It’s important to be patient with yourself and take as much time as you need to complete tasks and perform the doctor-prescribed exercises. Over time, you’ll be able to build an active, fulfilling life of your own.
5 notes
·
View notes
Text
Buspirone Hydrochloride
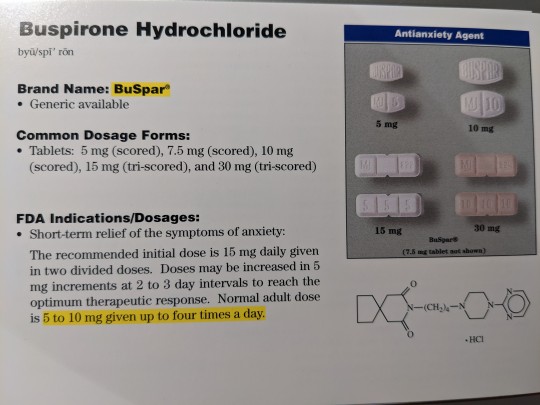

Brand Name: BuSpar
Generic Available
Common Dosage Forms:
Tablets: 5 mg (scored), 7.5 mg (scored), 10 mg (scored), 15 mg (tri-scored), 30 mg (tri-scored).
FDA Indications/Dosages:
Short-term relief of the symptoms of anxiety: The recommended initial dose is 15 mg daily given in two divided doses. Doses may be increased in 5 mg increments at 2 to 3 day intervals to reach the optimum therapeutic response. Normal adult dose is 5 to 10 mg given up to four times a day.
Pharmacology/Pharmacokinetics:
The exact mechanism of action of buspirone is vivo is not known. It may be due to a number of changes in brain chemistry including; (1) increasing the metabolism of norepinephrine in the locus coeruleus, (2) acting as a moderate presynaptic dopamine agonist, and (3) acting as a serotonin agonist. Buspirone does not significantly affect benzodiazepine or GABA receptors. Therapeutic improvement is usually seen within 7 days but may take as long as 21 days. Although indicated for short-term relief of anxiety, some patients have received up to 20 mg per day for as long as one year without altering efficiency or side effects. Discontinuation of therapy does not cause withdrawal symptoms. Peak plasma levels are reached in 1-2 hours. Elimination half-life is between 2-3 hours. Metabolism occurs in the liver and excretion primarily in the urine.
Drug Interactions:
Coadministration with MONOAMINE OXIDASE INHIBITORS may elevate blood pressure. Do not use together. Grapefruit juice may increase plasma levels and should be avoided.
Contraindications/Precautions:
Use with caution in patients with moderate to severely impaired hepatic or renal function. Because of buspirone’s ability to bind to dopamine receptors, there is a possibility of dystonia, parkinsonism, and tardive dyskinesia occurring during therapy. Use with caution during lactation. Pregnancy Category B.
Adverse Effects:
Skin rash, tachycardia, headache, fatigue, sweating, muscle pain, dream disturbances, dizziness, drowsiness, nervousness, insomnia, mood alterations, depression, dry mouth, nausea, vomiting, diarrhea or constipation, nasal congestion, blurred vision, tinnitus, and sore throat.
Patient Consultation:
May cause drowsiness or dizziness. Use caution when operating machinery or an automobile.
Report to your physician or pharmacist an abnormal involuntary movements of the tongue or facial muscles and any change in motor restlessness.
Store in a cool, dry place away from sunlight and children.
Contact a physician if the above side effects are severe or persistent.
If a dose is missed, skip it and return to normal dosing schedule.
Avoid grapefruit or grapefruit juice during therapy.
3 notes
·
View notes
Text
extra pyramidal side effects ranked:
1. tremor: I don’t mind this one and it’s actually pretty sexy of me to always be shaking all the time
2. bradykinesia: who cares
3. tardive dyskinesia: my case never got bad and my doses were decreased and my facial movements have gone away so I’m biased in saying once again it’s not that bad. lip smacking and slurping and drooling is kind of cringe though ngl
4. akathisia: restlessness to the point of pain but my episodes only lasted 30 minutes or so so I Dealt with it. still unpleasant
5. dystonia: Fresh hell on earth
5 notes
·
View notes
Text
Tumblr keep giving me ads for schizophrenia and adhd and tardive dystonia I get it you think I have menthol illness 🥴
1 note
·
View note
Photo



I fixed the spelling error and added more about how MAOIs work and their side effects.
Aside from imipramine and Doxepin, TCAs include amitriptyline, nortriptyline, and other “-triptylines.”
Bupropion (Wellbutrin) is a DA and NE reuptake inhibitor. Mirtazapine (Remeron) is an alpha 2-adrenergic receptor antagonist.
MAOIs are not used as first-line agents because of the increased safety and tolerability of newer agents, notably SSRIs/SNRIs. However, MAOIs are used for certain types of refractory depression and in refractory anxiety disorders: Phenelzine (Nardil), tranylcypromine (Parnate), isocarboxazid (Marplan).
HAM side effects (antiHistamine—sedation, weight gain; antiAdrenergic— hypotension; antiMuscarinic (anticholinergic)—dry mouth, blurred vision, urinary retention, constipation, exacerbation of neurocognitive disorders (i.e., dementias). Found in tricyclic antidepressants (TCAs) and low-potency anti - psychotics.
Serotonin syndrome: Confusion, flushing, diaphoresis, tremor, myoclonic jerks, hyperthermia, hypertonicity, rhabdomyolysis, renal failure, and death. Occurs when there is too much serotonin, classically when selective serotonin reuptake inhibitors (SSRIs) and monoamine oxidase inhibi-tors (MAOIs) are combined. As this combination is rarely seen in practice anymore, serotonin syndrome is more commonly seen when a patient is prescribed multiple medications with serotonergic activity (e.g., SSRIs/SNRIs, trazodone, Tramadol, triptans, dextromethorphan, St. John’s wort, ondansetron). Treatment: Stop medications, supportive care.
Hypertensive crisis: Caused by a buildup of stored catecholamines; triggered by the combination of MAOIs with tyramine-rich foods (e.g., red wine, cheese, chicken liver, cured meats) or with sympathomimetics.
Extrapyramidal side effects (EPS): Parkinsonism—masklike face, cog-wheel rigidity, bradykinesia, pill-rolling tremor; akathisia—restlessness, need to move, and agitation; dystonia—sustained, painful contraction of muscles of neck, tongue, eyes, diaphragm. Occur more frequently with high-potency, typical (first generation) antipsychotics, but can also be seen with atypical (second generation) antipsychotics. Reversible. Occur within hours to days of starting medications or increasing doses. In rare cases, can be life threatening (e.g., dystonia of the diaphragm causing asphyxiation).
Hyperprolactinemia: Occurs with high-potency, typical (first generation) antipsychotics and risperidone.
Tardive dyskinesia (TD): Choreoathetoid muscle movements, usually of the mouth and tongue (can affect extremities, as well). Occurs after years of antipsychotic use (more likely with high-potency, first-generation antipsychotics). Usually irreversible.
Neuroleptic malignant syndrome: Mental status changes, fever, tachycardia, hypertension, tremor, elevated creatine phosphokinase (CPK), “lead pipe” rigidity. Can be caused by any antipsychotic after a short or long time (increased with high-potency, typical antipsychotics). A medical emergency with up to a 20% mortality rate.
Drug interactions: Cytochrome P450 is a group of enzymes in the liver that metabolizes many common drugs, including psychiatric medications. Some medications induce the system, in other words the system metabolizes medications faster—drug levels decrease. Some medications inhibit the system, in other words the system metabolizes medications more slowly—drug levels increase. Common cytochrome P450 enzymes important in metabolizing psychiatric medications include CYP3A4, CYP2D6, CYP1A2, CYP2C9, CYP2C19.
Important CYP450 inducers include: Tobacco (1A2), Carbamazepine (1A2, 2C9, 3A4), Barbiturates (2C9), St. John’s wort (2C19, 3A4). Important CYP450 inhibitors include: Fluvoxamine (1A2, 2C19, 3A4), Fluoxetine (2C19, 2C9, 2D6), Paroxetine (2D6), Duloxetine (2D6), Sertraline (2D6).
New form, desvenlafaxine (Pristiq), is the active metabolite of venlafaxine; it is expensive and without known benefit over venlafaxine.
Bupropion (Wellbutrin) can decrease the seizure threshold and is contraindicated in pts with bulimia. Tricyclic antidepressants include amitriptyline, imipramine (treats enuresis), clomipramine (treats OCD), and doxepin (may be used as a sleep aid in low doses). Amitriptyline, imipramine, clompiramine, and doxepin are tertiary amines (highly anticholinergic/antihistaminergic [more sedating]/antiadrenergic [more orthostasis] with a greater lethality in overdose). Secondary amines (metabolites of tertiary amines (less anticholinergic/antihistaminic/antiadrenergic) are nortriptyline and desipramine. Tetracyclic antidepressant = amoxapine.
#antidepressants#mood stabilizers#TCAs#MAOIs#SNRI#SSRI#benzos#benzodiazepines#pharm#zoloft#tyramine#wellbutrin
6 notes
·
View notes
Photo

Friendly reminder that while it will do other things, nicotine can help with the seizures and involuntary motor control associated with Tardive Dyskinesia/dystonia, Parkinson’s, and certain other conditions. While it may have been a factor in development, its nature and relationship to the Dopamine production and reception in your brain allows the processes to cease temporarily. Not a long term fix, by any means, but if you need to get yourself through it till then, its tough to beat.
0 notes
Text
this is how i’m studying basal ganglia disorders
(hemi)ballismus (violent contralateral or bilateral thrashing)

athetosis (slow, continuous, and aimless flailing, slower than chorea)

chorea (jerky movements that appear dance-like)

dystonia (muscle contractions producing twisting and/or abnormal postural movements)

dyskinesia/tardive dyskinesia (repetitive facial movements; can result from dopamine receptor agonist use)
tremors (oscillating movement from alternating or synchronistic muscle contractions)
13 notes
·
View notes
Photo
My goal tonight is to learn about some antipsychotics so I can safely administer them during clinical tomorrow ☝🏻 Some antipsychotics, especially conventional drugs such as haloperidol (Haldol), can cause extrapyramidal side effects (EPS) such as tardive dyskinesia, acute dystonia, pseudoparkinsonism, and akathisia. These side effects can be very disruptive, so fortunately we have newer antipsychotics that have less adverse effects. Why are drugs sooo fun to learn 🤣 https://www.instagram.com/p/BsZWpCAhfnO/?utm_source=ig_tumblr_share&igshid=u9d1bd1xg0eg
4 notes
·
View notes