#the amount of editorial military looks i had to go through… pain
Text

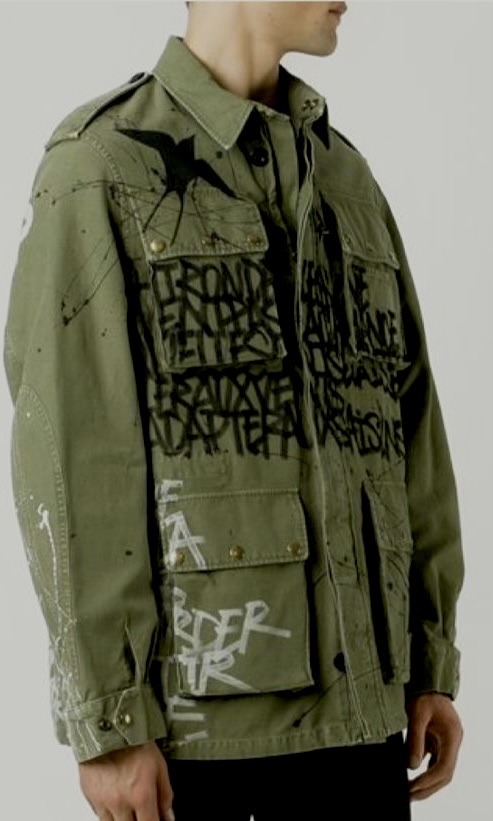




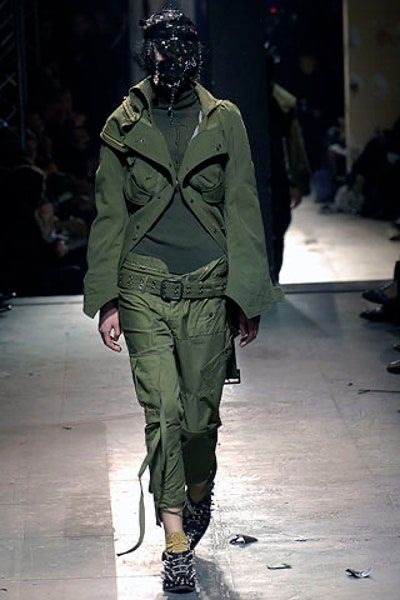
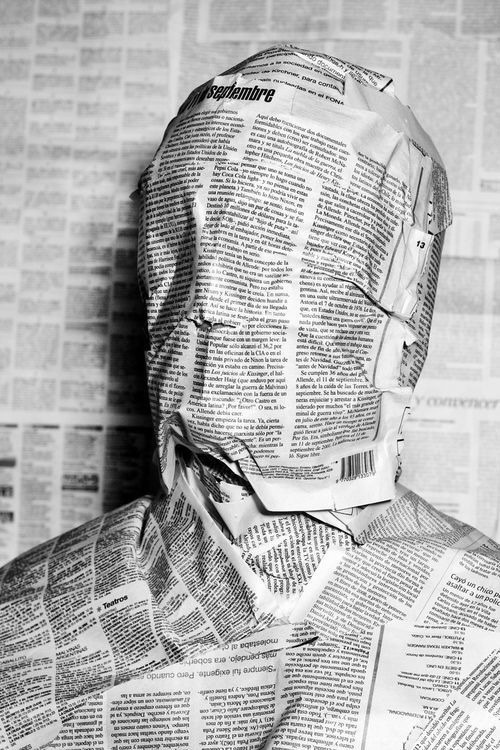

<?>The Riddler Inspired Fashion Moodboard <?>
Junya Watanabe Spring 2006 Ready-to-Wear Collection // Faith Connexion Graffiti Print Cargo Jacket // CRAIG GREEN Fall/Winter 2016 collection // R13 God Save America Coat // AW2005-2006 Raf Simons Poltergeist Parka // Reality by Sol Navedo
#THIS TOOK FOREVER YOU HAD NO IDEA#the amount of editorial military looks i had to go through… pain#anywaysss#runway fashion#fashion#junya watanabe#craig green#editorial#editorial fashion#moodboard#fashion mb#fashion moodboard#the riddler#the batman#riddler#faith connexion#raf simons#me.txt#greatest hits
725 notes
·
View notes
Link
Yves here. Reader IM Doc, an internal medicine practitioner of 30 years, trained and worked in one of the top teaching hospitals in the US for most of his career before moving to a rural hospital in an affluent pocket of Flyover. He has been giving commentary from the front lines of the pandemic. Along with current and former colleagues, he is troubled by the PR-flier-level information presented to the public about the Pfizer and Moderna vaccines, at least prior to the release of an article in the New England Journal of Medicine on the Pfizer vaccine: Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. However, he did not find the study to be reassuring. He has taken the trouble of writing up his reservations after discussing the article with his group of nine physicians that meets regularly to sanity check concerns and discuss the impact that articles will have on their practices.
By IM Doc, a internal medicine doctor working in a rural hospital in the heartlands
Right off the bat – I am as weary and concerned about this pandemic as anyone. What my little rural area has been through in the past three weeks or so has been nothing short of harrowing. This virus has the ability to render patients about as sick as I have ever seen in my life, while leaving more than half the population with minimal if any symptoms. The patients who are sick are often very sick. And instead of slow and steady improvement like we normally experience, most of these patients are assigned to a long and hard slog. Multiple complications arise. This leads to very diminished throughput in the hospital. The patients literally stack up and we have nowhere to put the new ones coming in who themselves will be there for days or weeks. On top of that are the constant donning and doffing of PPE and intense emotional experiences for the staff, who are themselves becoming patients or in this small town have grandma or Aunt Gertrude as a patient.
To put it bluntly, I want this pandemic over. And now. But I do not want an equal or even worse problem added onto the tragedy. And that is my greatest fear right now. And medical history has demonstrated conclusively over and over again: brash, poorly-thought-out, emotion-laden decisions regarding interventions in a time of crisis can exponentially increase the scale of pain and lead to even worse disasters.
I am not an anti-vaxxer. I have given tens of thousands of safe and tested vaccines over my lifetime. I am very familiar with side effects and safety problems associated with all of them. That is why I can administer them with confidence. I am also an optimist, so all of the cautions I discuss below are the result of experience and the information made public about the Pfizer vaccine, not a temperamental predisposition to see the glass as half empty.
I know this piece is long, but I wanted to completely dissect the landmark New England Journal of Medicine (from now on NEJM) publication of the first Pfizer vaccine paper. I am replicating the method of my mentor in Internal Medicine, a tall figure in 20th Century medicine. He was an internationally recognized authority and his name is on one of the foundational textbooks in his specialty. He was a master and he taught me very well, including the fundamentals of scientific inquiry and philosophy, telltale signs of sloppy or dishonest work, the order in which you should dissect someone’s work, and the statistics involved.
When I have a new medical student doing rotations with me, I give them a collection of reading. At the very top is Drug Companies & Doctors: A Story of Corruption from the New York Review of Books in 2009 by Marcia Angell, MD. She was the editor-in-chief of the NEJM, the very journal that published this Pfizer vaccine paper.
Dr. Angell’s article is the Cliffs Notes version of much longer discussions she had about corruption, corporatism, managerialism, profiteering, greed, and deception in in the medical profession. Patient care and patient concerns and indeed patient lives in her mind have been absolutely overcome by all of these other things. It is a landmark paper, and should be read by anyone who is going to interact with the medical community, because alas, this is the way it is now. I view this paper the exact same way I view Eisenhower’s speech about the military industrial complex. What she said is exactly true, and has only become orders of magnitude worse since 2009.
And now the paper.
Unfortunately, this study from Pfizer in the latest NEJM, and indeed this whole vaccine rollout, are case studies in the pathology Agnell described. There are more red flags in this paper and related events than present on any May Day in downtown Beijing. Yet all anyone hears from our media, our medical elites, and our politicians are loud hosannas and complete unquestioning acceptance of this new technique. And lately, ridicule and spite for anyone who dares to raise questions.
I have learned over thirty years as a primary care provider that Big Pharma deserves nothing from me but complete and total skepticism and the assumption that anything they put forth is pure deception until proven otherwise. Why so harsh? Well, to put it bluntly, Big Pharma has covered my psyche with 30 years of scars:
• As a very young doctor, I treated an extraordinary middle-aged woman who had contracted polio as a toddler from a poorly tested polio vaccine rolled out in an “emergency.” Tens of thousands of American kids shared her fate1
• The eight patients I took care of until they died from congestive heart failure that had been induced by a diabetes drug called Actos. The drug company knew full well heart failure was a risk during their trials. When it became obvious after the rollout, they did everything they could to obfuscate. Actos now carries a black box warning about increased risk of heart failure
• The three women who I took care of who had been made widows as their husbands died of completely unexpected heart attacks while on Vioxx. I have no proof the Vioxx did this. But when Vioxx was finally removed from the market, the mortality rate in the US fell that year by a measurable amount, inconsistent with recent trends and forecasts. Merck knew from their trials that Vioxx had a significant risk of cardiovascular events and stroke, and did absolutely nothing to relay that danger in any way. Worse, they did everything they could to muddle information and evade responsibility once the truth started to come out
• The dozens upon dozens of twenty and thirty-something patients who have been rendered emotional and spiritual zombies by the SSRIs, antipsychotics and amphetamines they have been taking since childhood. Their brain never learned what emotions were, much less how to process them and we are left with empty husks where people never developed. The SSRIs and antipsychotics were NEVER approved for anyone under 18. EVER. While there are some validated uses for stimulants in children, they are obviously overprescribed, as confirmed by long-standing media reports of their routine use as a study/performance aid. It is all about the lucre.
• The hundreds and hundreds of 40-60 year olds who have been hollowed out from the legal prescribing of opioids. All the while the docs were resisting this assault, the drug companies and the paid-off academics and medical elites were changing the rules to make physicians who did not treat any pain at all with opiates into evil Satan-worshippers. And they paid for media appearances to drive across the point: OPIATES ARE GOOD. WE HAVE MADE THEM SO YOU CANNOT GET ADDICTED. And here we are now with entire states taking more opioids than in the waning days of the Chinese Empire, and we all know how that story ended. All this misery so a family of billionaires can laugh its way to the bank.
I carry all these people and more with me daily. I would not be doing a service to their memory if I allowed myself to be duped into writing another blind prescription that was going to add yet another scar.
I will dissect the important parts of this paper exactly as my mentor described above taught me. He performed years of seminal research. He was a nationally-known expert in his field.
In medicine, especially in top-tier journals like NEJM, landmark papers are always accompanied by an editorial. These editorials are written by a national expert who almost always has “peer-reviewed” the source material as well. This is how the reader knows that an expert in the field has looked over the source material and that it supports the conclusions in the paper. My mentor did this all the time. The binders all over his office were the actual underlying data that he scrutinized to confirm the findings. There is no way on earth to print and publish the voluminous source material. Editorial review was one sure way all to assure that someone independent, with appropriate experience, confirmed the findings. This was onerous work, but he and thousands of others did it because this is the very essence of science. He was scrupulous in his editorials about findings, problems, and conclusions. It was after all his reputation as well.
My first lesson from him: READ THE EDITORIAL FIRST. It gets the problems in your head before you read the statistics and methods, etc. in the actual paper. It gives you the context of the study in history. It often includes a vigorous discussion of why the study is important.
Admittedly, over the past generation, as the corporatism and dollar-counting has taken over my profession and its ethics, this function of editorial authoring has become at times increasingly bizarre and too-obviously predisposed to conclude with glad tidings of joy, especially if pharmaceuticals are involved.
So I read the editorial first. You can find it on the NEJM webpage, in the top right corner.
And, amazingly, it is basically a recitation of the same whiz-bang Pfizer puffery that we have all been reading for the past few weeks. There really is not much new. Furthermore, it is filled with words like “triumph” and “dramatic success”. Those accolades have yet to be earned. This vaccine has not yet even been released. Surely, “triumph” is a bit premature. Those words would NEVER have been used by my mentor or similar researchers in his generation. They would have been focused on the good, the bad and the ugly. A generation ago, editorial reviewers saw their job as informing the reader and making certain the clinicians that were reading knew of any limitations or problems.
In quite frankly unprecedented fashion, two different events that were carefully reported occurred almost simultaneously with the release of both the paper and the editorial. Both of these events contradict and contravene data and conclusions reported in both the paper and the editorial and I believe they deserve immediate attention. They both belie the assertions of the editorial writers that [emphasis mine] “the (safety) pattern appears to be similar to that of other viral vaccines and does not arouse specific concern”.
First, a critical issue for any clinician is “exclusion criteria”. This refers in general to groups of subjects that were not allowed into the trial prima facie. Common examples would include over 70, patients on chemotherapy and other immunosuppressed patients, children, diabetics, etc.. This issue is important because I do not want to give my patient this vaccine (available apparently next week) to any patient that is in an excluded group. Those patients really ought to wait until more information is available – FOR THEIR OWN SAFETY. And not to mention, exclusion criteria exist because the subjects in them are usually considered more vulnerable to mayhem than average subjects. From my reading of this paper, and the accompanying editorial, one would assume there were no exclusion criteria. They certainly are never mentioned.
I reiterate, the paper is silent on this question of exclusion criteria, as is the editorial. Had my mentor seen something like “exclusion criteria” in the source material, and realized that it was not in the final paper, he would have absolutely included a notice in his editorial. This would have been after calling the principal investigator and directly questioning why there was no mention in the original paper. Patient safety should be foremost on everyone’s mind at all times in clinical research and its presentation to practitioners.
And now we know there were exclusion criteria, not because of anything Pfizer, the investigators, or the NEJM did but because of stunning news out of the UK. UPDATE: I will address this at greater length, but an alert reader did find the study protocol, which were not referenced in any way that any of the nine members in my review group could find, nor were they mentioned in the text of paper or editorial, as one would expect for a medication intended for the public at large. I apologize for the oversight, but this information was not easy to find from the article, not mentioned or linked to from the text of the article, the text of the editorial, in the “Figures/Media,” or in a supplemental document.
In the UK on day 1 of the rollout, two nurses with severe allergies experienced anaphylaxis, a life-threatening reaction to this vaccine. Only after world-wide coverage did Pfizer admit that there was an exclusion criterion for severe allergies in their study.
Ummm, Pfizer, since we are now getting ready to give this to possibly millions of people in the next few weeks – ARE THERE ANY OTHER EXCLUSION CRITERIA? Should I, as a physician, specifically not be giving this to patients with conditions that you have excluded?
Furthermore, NEJM, since you published this trial, have you bothered to at least put a correction on this trial on your website that it should NOT be given to people with severe allergies? I certainly see nothing like this.
Should someone from the NEJM or the FDA be all over Pfizer to ascertain the existence of other exclusion groups so we do not accidentally harm or kill someone over the next two weeks?
Unfortunately, Americans, you have your answer from the FDA about severe allergic reactions right from a press conference in which Dr. Peter Marks, the director of FDA’s Center for Biologics Evaluation and Research is quoted as saying:
Even people who’ve had a severe allergic reaction to food or to something in the environment in the past should be OK to get the shot….1.6% of the population has had a severe allergic reaction to a food or something in the environment. We would really not like to have that many people not be able to receive the vaccine.
Are you serious? Dr. Marks, have you ever seen an anaphylactic reaction? I live in a very rural area. Many patients live 30 minutes or more from the hospital. What if one of them had an anaphylactic reaction to this vaccine hours after administration, had no epi-pen and had to travel a half hour to get to the nearest hospital? There is a very high likelihood that a good outcome would not occur. Sometimes, as a physician, I simply cannot believe what I am hearing out of the mouths of our so-called medical leaders.
To the writers of the editorial accompanying this research:
Did you actually look at the source material? The existence of at least one exclusion criterion for severe allergic reactions had to be in there somewhere. If you did look at the source material, are there others that the physicians of America need to know about? If they were not in the source material, after the events in the UK, has anyone bothered to follow up with Pfizer about this omission?
Does anyone at NEJM or Pfizer or FDA plan to fully inform the physicians of America? Does ANYONE at NEJM or Pfizer or FDA care about patient safety?
Now for the second story that got my attention this week, an article from JAMA Internal Medicine, a subsidiary of JAMA, The Journal of the American Medical Association.
JAMA, like NEJM, is one of America’s landmark medical journals. I will assure you that JAMA is not the National Enquirer. This piece was written by a nursing researcher. It is very likely she is well-versed in all aspects of American medical research.
In her story, she details her recruitment and her experience in the Pfizer COVID trial, the same one we are dissecting here. She describes in detail her experience with the vaccine and the fact that she is concerned that many patients are likely going to feel very sick after the injection. She wrote up her own reactions, and included a very troubling one. About 15 hours after her second injection, she developed a fever of 104.9. She explained that she called her reaction to the Research Nurse promptly the next morning. The recounted the response of the Research Nurse to her information as “A lot of people have reactions after the second injection. Keep monitoring your symptoms and call us if anything changes.”
Thankfully, it appears this nurse has completely recovered. From the best I can tell, this encounter occurred in late August and early September, putting it well within the trial’s recruitment of arms as detailed in the paper.
This JAMA article impinges directly on Figure 2 on page 7 of the paper, a graphic that that lays out all the major side effects during in the trial.
It is very important to note that based on the trial’s own data, conveniently laid out on the very top of the figure in green, blue, orange and red, a temperature of 104.9F or 40.5 C is described as a Grade 4 event. The definition of a Grade 4 event is anything that is life-threatening or disabling. A fever of 104.9 can have grave consequences for any adult and is absolutely a Grade 4 event.
By law, a grade 4 event must immediately be reported to the FDA, and to the Institutional Review Board (the entity charged with overseeing the safety of the subjects) and to the original investigators. THERE IS NO EXCEPTION. One would think that would also be reported in the research paper to at least alert clinicians to be on the lookout.
I could not find any mention of this event in the text of the paper. NOT ONE. Let’s take a closer look at Figure 2 on page 7 where adverse events are reported in a table form. Please note: this is a very busy image, and in the browser version, with very low resolution graphics that are profoundly difficult to read (they are a bit clearer if you download the PDF). This is a time-tested pharmaceutical company tactic to obscure findings that they do not want you to see. My mentor warned me about ruses like these years ago, and finding one raises the possibility that deception is in play.
The area for the reporting of this Grade 4 reaction would be on the 2nd row down at the left of the set called B, titled systemic events and use of medication. The area of concern would be where the graph is marked with the number 16. Do you see a red line there? It would be at the very top. I have blown this up 4 times on my computer and see no red there. I am left to assume that this Grade 4 “Life Threatening or Disabling” event that was clearly within the time parameters of this trial was not reported in this study.
To those who say that I am making way too much out of one patient with a severe fever, let’s do a little math. There are 37,706 participants in the “Main Safety Population” (from Table 1), of which 18.860 received the vaccine.2 Let us assume that this individual was the only one that had a GRADE 4 reaction. Let us also assume that the end goal is to vaccinate every American a total of 330,000,000 people. So if we extrapolate this 1 out of 18,860 into all 330,000,000 of us, it suggest that roughly 17,500 could have this kind of fever. Now assume a 70% vaccination rate, and you get that would be approximately 12,250. I hope you now understand that in clinical medicine related to trials like this – a whole lot of nothing can turn into a whole lot of something quickly when you extrapolate to the entire targeted group. Does anyone not think that the clinicians of America should be prepared for anything like this that may be coming?
A couple more questions for NEJM and the editorial writers:
Were you ever made aware that this Grade 4 reaction occurred? Now that we have a reliable report that it occurred, has there been any attempt to investigate?
Did the Research Nurse actually report this event? If not, was she just simply not trained or was there deliberate efforts to conceal such reactions? How many more reactions were reported anywhere this trial was conducted and that did not make it to the FDA, the IRB or possibly the investigators? Is that not a cause for concern?
As if this is not enough, there is so much more wrong with this editorial. Now we are going to talk about corruption.
I want to reiterate my concern that over the past generation, as my profession has lost its way, its medical journals have turned into cheering sections for Big Pharma rather than referees and safety monitors. We all should relish the great things medical science is doing, but we should be doing EVERYTHING we can to minimize injury and death. Too often our journals have become enablers of Big Pharma deceiving our physicians and the public. Unfortunately, this paper and its editorial look troublingly like a case study of this development.
To provide context, I looked over the last month of the NEJM, the issues from November 12, 19 and 26th and December 3rd. Based on having read the NEJM over the years, I believe these four weeks are representative.
During this period, there were 15 original articles published in the fields of Oncology, General Surgery, Infectious Disease, Endocrinology, Renal, Cardiology, Pulmonary and Ear Nose & Throat. Of these 15 articles, the editors thought that eight were important enough to have an editorial from an acknowledged expert. I have read every one of these studies and the editorials as I do every week. All eight in the past month were indeed by leading experts in the field of the underlying studies. They included a COVID vaccine overview reviewed by an leading figure in vaccinology, and two COVID papers about Plaquenil and other approaches discussed by top infectious disease experts.
It was unlikely that those papers were going to get national media attention. All medical stuff.
But here we have our Pfizer vaccine paper. We have 300,000 fatalities in the USA alone and millions of cases. We have whacked our economy, we are in the depths of a national emergency. And we have a paper, the first, that may offer a glimpse of hope. Certainly this would be a landmark paper, and certainly it was treated in that manner? Right?
One would think that the doctors of America would have this study explained to them by a world-known vaccinologist? NOPE…..Maybe a virologist? NOPE….. Maybe a leading government official? Dr. Fauci? Dr. Birx? Dr. Osterholm? NOPE…..Maybe an expert in coronaviruses? NOPE…
We get the Pfizer ad glossy editorial treatment from Eric Rubin MD, the editor-in-chief of the NEJM. And Dr, Longo, an associate editor. Dr. Longo is an oncologist. Dr. Rubin is at least a recognized infectious disease doctor, but his specialty based on my Google search is mycobacterium, not virology. Again, one would normally anticipate for a paper of this importance, the editorial would be from someone with directly on point expertise.
Why would this fact been important to my mentor? (and I had the privilege of hearing him trash a paper in an open forum about a very similar issue, a paper introducing a drug to the world that later was the disaster of the decade, Vioxx) Why is this important to me and all the other physicians in my review group here in flyover country yesterday?
Because the choice of authorship of the editorial leads you to one of only several conclusions:
• Pfizer would not release the source data because of proprietary corporate concerns and no self-respecting expert would review without it
• Pfizer knew there are problems and did not want anyone with expertise to find out and publicize them
• The editors could not find a real expert willing to put their name on a discussion
• Drs. Rubin and Longo are on some kind of journey to Vanity Fair and wanted their names on an “article for the ages”
• This is a rush job, and no one had time to do anything properly, and so we just threw it all together in a flash
Readers, pick your poison. If anyone can think of a sound reason, please let me know. I am all ears.
But let’s open up the can of worms a bit more. Pfizer supports NEJM. Just a brief swipe through of recent editions yielded several Pfizer ads. A Pfizer ad appeared on my NEJM website this AM. I do not know how much they pay in advertising but appears to be quite a bit.
Americans, have we devolved so far in our grift that it is now appropriate for the EDITOR-IN-CHIEF of our landmark medical journal to be personally authoring “rah rah” editorials about a product of a client that supports his journal with ad dollars? And he has the gall to not present this conflict on his disclosure form? Really? Am I the only one worried about this type of thing?
Now we travel from the can of worms to the sewer. And this impacts every single one of us. I want you to Google the names of the people on the FDA committee that voted 17-4-1 two days ago to proceed with the Emergency Use Declaration. Go ahead – Google it. On that list, you will find the name Eric Rubin, MD. Why yes indeed, that is the very same Eric Rubin MD who wrote this editorial. Who is the Editor-in-Chief of the NEJM. A publication that certainly takes ad dollars from Pfizer. And he was one of the 17 to vote for the Pfizer product to be immediately used in an emergency fashion. Oh yes, oh yes he was.
Am I the only one who can recognize that Pfizer and other pharma companies may have some influence on Dr. Rubin thanks continued support of his employer, the NEJM? Am I the only one concerned that Dr. Rubin’s “rah rah” editorial may have been influenced by Pfizer? Is anyone else troubled that the Editor-in-Chief of the NEJM, supported by Big Pharma advertising dollars, is sitting on an FDA board to decide the fate of any pharmaceutical product? Is this not the very definition of corruption? Or at least a severe conflict of interest? I strongly suspect that a thorough evaluation of members of that committee will reveal other problems. As my grandmother always used to say, “There is never just one roach under a refrigerator.”
I looked in vain all day today for media discussions of conflicts of interest with Dr. Rubin or anyone else in a position of authority. I found nothing.
What I did find was the Boston NPR affiliate WBUR discussing Dr. Rubin’s Yes vote. You can listen yourself:
This interview left me much more concerned about Dr. Rubin’s role and what exactly he read in the raw data from Pfizer. In this interview, he admits that he as an FDA advisory member has seen no data from the Moderna trial coming up for a vote this week:
These two vaccines are fairly similar to one another, so I am hoping the data will look good, but we haven’t seen the data yet, so I reserve judgement.
Excuse me, but should not the members already have the data and be mulling over it to ask intelligent questions?
These statements left me more worried about the issues I have already brought up with the Pfizer vaccine:
We don’t know if there are particular groups that should or should not get the vaccine…We do not know what will happen to safety over the longer term.
When finally asked specifically about the UK allergic reactions and if they came up in the FDA meeting (emphasis mine):
It did come up and this was a bit of a surprise because in the trial, that trial was limited to specific kinds of participants, there were apparently no incidents like that, nevertheless this suggests it is something we are going to have to look out for.
There is absolutely not a word in the published data to suggest there was a limit to SPECIFIC PARTICIPANTS – what on earth is he talking about? Are there limited specific kinds of patients that we as physicians should be looking to vaccinate?
In a fine finish, toward the end of the interview Dr. Rubin states he is a bit relieved that low risk patients will be getting the vaccine later after we know more about the side effects with the first patients. I am really not trying to be a jerk – but are you kidding me? I thought this vaccine was a triumph with minimal side effects.
Dr. Rubin, kind sir, I really feel that you owe a clarification about your statements in the WBUR interview to the patients and caregivers of America. We are the ones with lives on the line.
First, I have the privilege of sitting on an Institutional Review Board (an independent entity that protects patient safety) and I know something about Grade 4 side effects. Just for 1 Grade 4 side effect in one subject, the accompanying documentation would often be a half a ream of paper. Because I agreed to do that job, it was my obligation to look through that documentation. That half a ream was for one side effect in one trial. Yet, you state unequivocally in this interview, that you, as a sitting member of the FDA committee that oversees the safety of the nation in this affair, have not seen any of the Moderna documentation for that upcoming meeting this week.
For readers to fully understand what I am saying, this Moderna documentation is going to be reams and reams of documents that need to be evaluated carefully to ask the right questions. And you have not yet studied this? For a meeting in just a few days? I find this deeply troubling. Your statements create the appearance the committee you are sitting on is nothing more than a rubber stamp for a decision that has already been made. This would be an absolute tragedy.
Second, Dr. Rubin, you in your position as the Editor-in-Chief of the NEJM and the editorial writer for this research, may be one of the few people on earth that have seen the original Pfizer research. Despite calling this a triumph, you state in the interview that you are relieved that younger people less likely to get the vaccine early so you will have time to wait to see if complications develop in the first patients. You have stated, despite your assertion in the editorial that the side effects were consistent with other vaccines, that “we don’t know if there are particular groups that should or should not get the vaccine”. Have you seen something in that “triumph” research that is concerning enough to you to make such statements? As a physician, I would really like a clarification on this statement, given that the shots are already rolling out today.
Now that we are past the editorial, a few words about the nuts and bolts of the paper.
I look for very specific red flags – usually making the data difficult to interpret. This study did not disappoint.
On page 5, in Table 1, the Demographic Description of the participants, go down to the AGE GROUP area. Note it is divided into only two cohorts 16-55 and >55. This is a real problem. My mentor said an honest paper should never deploy such a tactic.
You see, more than half of my patients are over 70. Why is this kind of obfuscation a real problem for my ability to trust the vaccine? Well, the intro papers to many pharmaceuticals that have gone down the drain in recent years have used this very same device. It is their way of hiding the fact that they did not put many older patients in the trial, certainly not representative of the population, and certainly not representative of who is seemingly going to get this vaccine in the first round. Do I know that 90% of the >55 group is actually between 55-58? I don’t. How hard would it be for them to do a breakdown in decades? 16-25 26-35 36-45 46-55 56-65 66-75 76-85? We have lots of computers in this country and the population breakdown is done this way on studies I read all the time. Why not do provide this information on a study that is this critically important, particularly one where elderly patients will be near the head of the line?
What are they trying to do here? Unfortunately, too often drugmakers resort to this practice to hide their failure to test their drug on the elderly to an appropriate or safe degree, knowing there would likely be lots of problems. Because of their past behavior, I ALWAYS assume this is true until proven otherwise and act accordingly with my elderly patients.
That is the world these companies have made for themselves.
Now for the tables on pages 6 and 7 about immediate side effects.
Just a brief look shows that local soreness and tenderness is very common, up to 75% with this vaccine. That is a bit high, but not that far out of range from my experience with other vaccines.
The tables on page 7 are the whoppers.
Headaches, fatigue, chills, muscle pain and joint pain appear to be very common, way more common than other vaccines I am used to, as in an order of magnitude higher. It is very clear from this table that about half the patients, especially the younger ones, are going to feel bad after this vaccine. That is extraordinary.
We are told nothing about how long these symptoms last or the amount of time at work lost. The “minimal side effects comparable with other viral vaccines” in the editorial and press releases is just not consistent at all with my experience of 30 years as a primary care physician. There was universal agreement with this assessment among my MD colleagues. They had great concern about this as a matter of fact: great concern that it will cause bad publicity and decrease administration and great concern that given this already high side effect profile, it may be much worse when it gets out to the public.
Given the fact that this virus is largely asymptomatic in more than half the people infected, what exactly are we doing here?
Furthermore, unlike other pharmaceutical papers that try to explain variances in symptoms like this, there is not a word offered about possible underlying causes of these outcomes.
The numbers of COVID cases in the placebo group vs the vaccine group have been widely publicized, from 162 cases in the placebo group down to 8 in the vaccine group, giving a relative reduction of 95%. It seemed to all of us in our review group that we do not have nearly enough patients to really make assessments. That is not a criticism. The researchers have done admirably in my opinion to get this many patients this quickly. That is still the problem: they are going to be using the first million patients or so in the general public to get a real gauge on numbers and side effects.
Another issue of grave concern to us all on Friday was the asymptomatic cases. The only subjects counted in the 162 and the 8 numbers above were patients with symptoms. Who knows how many in each cohort were asymptomatic.
This to me leads to the most important question of all, and it was again completely untouched….. How many asymptomatic patients are there? And how many who were vaccinated are still able to spread the virus? Not even an attempt to answer that question. This is critical, and is one of the ways a vaccine can backfire. If a vaccine does not provide sterilizing immunity, ie stop transmission, it is of limited use for disease control. It is great for the individual, but if they can remain without symptoms and still spread it all around it does not help from a public health standpoint.
I have described my concerns and red flags about this study. I would like to add one more thing. Pharmaceuticals that go bad rarely do so in the first few weeks or months. Rather, the adverse effects take months or years. It is a known unknown of not just vaccines but any kind of drug. Our pharma companies have become notorious for having inklings or indeed full knowledge that there is a problem early on, and saying nothing until many are maimed or killed. I will assume that this is the case in this class of drugs until proven otherwise. They are such deceivers I have no choice.
Due to sense of urgency my colleagues and Ifeel about this vaccine rollout, we had an ad hoc meeting of our Journal Club to discuss the NEJM article. Of the nine physicians at the meeting, three have already had very mild cases of COVID. Of the nine, only one is enthusiastic about these vaccines. I have a wait and see stance. I will not be taking it myself. I have too many scars, too many staring at me from the grave to take any other approach.
My patients’ feeeback on the COVID vaccine has been very different than the polls finding that 60% are ready to take it. About half my patients are in the professional/managerial classes and feature a higher level of the 0.1% than the US overall. They tend to be more blue. Most prefer to wait and thankful that health care workers were getting it first. The other half who are working class, more red, and they feel the whole thing is a hoax. They will not be getting the vaccine – likely ever.
The only enthusiasts I would call elderly Rachel Maddow fans. That really makes no sense to me at all since Operation Warp Speed was a Trump project and even Kamala Harris said she would not take a vaccine that Trump recommended.
I would say AT BEST 25% of my patients will be getting this vaccine shortly after being available. There is widespread skepticism that is not being acknowledged by our media. The pharmaceutical industry has worked tirelessly to earn every bit of that disrespect.
Please look at Dr. Angell’s seminal article from 2009. She predicted in her works, all of this and more. My profession has been captured by a cabal of corporatist MBA clones, rapacious and unethical pharmaceutical entities, and an academic elite addicted to credentialism and cronyism. They have over the years bought off and infiltrated all of our government health care regulating agencies and our public health system. And they are completely incestuous. I believe where we are now to be worse than Dr. Angell could have ever dreamed. Even more depressing, I see no way out.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
1 As a special homage to the polio patient described above, a truly exceptional woman, let me underscore that the disastrous rollout of the this polio vaccine came at a time similar to ours. Panic and malaise were in the air. The children of America and the world were being stricken with polio at an alarming rate. Dr. Alton Ochsner, a leading figure in medicine of the day, vaccinated both of his grandchildren in public in an attempt to bolster confidence in the vaccines. Within 8 days his grandson was dead of bulbar polio. All the celebrities and politicians lining up to take this vaccine on national TV should remember this tragedy. “Stupid human tricks” like this have no place in this kind of situation, and can backfire in unexpected ways. Unlike that era’s polio vaccine, there is no way on earth this vaccine can transmit COVID. However, there are those of us in the medical profession who treat the plan to make population-wide use of messenger RNA, which before these trials had been repeatedly investigated but never reached the human trial stage save in a small scale Zika vaccine study. This is no time for machismo. This is also no time for anything less than complete transparency on the part of everyone involved in the quest for safe and effective vaccines. To behave in any other way is an affront to patients like mine who have suffered and died in the past.
2 If you read the paper, you might well have wondered about that 18,860 number and even checked Table 1 to make sure it’s accurate (it is), since the third paragraph of the Abstract, under the headline “Results,” has very different figures:
A total of 43,548 participants underwent randomization, of whom 43,448 received injections: 21,720 with BNT162b2 and 21,728 with placebo.
So how did the researchers get from 21,720 injected with the vaccine to the 18,860 in the “Main Safety Population”? This sort of thing confirms the impression that this is a very incomplete or sloppy study. It is really not clear where the difference between the 37,706 and the 43,548, or for that matter, the 36,520 total subjects in the Tables 2 and 3 (Efficacy) come from. I used the 37,706 and hence the 18,860 that went with it from Table because it gave slightly smaller numbers than using the Table 2 and 3 figures, but they would be close to each other.
My concern here is the 6000ish discrepancy between the figures in the main text compared to the tables. Were they excluded? If so, why? I could not make heads or tails out of this, and accordingly kept it out of the body of this post. This kind of inconsistency really needs to be hashed out with the actual source data in hand, and should have been explained in the article, even if just in footnotes.
#covid19#covid#the rona#la rona#covid-19#covid vaccine#fuck covid#coronavirus#medecine#health#medical pharmaceuticals#pharmaceutical industry#big pharma#pfizer#vaccine rollout#operation warp speed
3 notes
·
View notes
Text
Veteran’s Appendectomy Launches Excruciating Months-Long Battle Over Bill
In late August 2019, Shannon Harness awoke to serious pain in the lower right side of his abdomen — a telltale sign of appendicitis.
He booked it to the emergency room of the only hospital in the county: Heart of the Rockies Regional Medical Center in Salida, Colorado. After a CT scan, doctors told Harness he had acute appendicitis and required immediate surgery.
A surgeon performed an appendectomy that night and released Harness the next day.
But a couple of days later, Harness felt sharp pains where his appendix had been. The pain grew until he was on the floor screaming.
“It was disturbing,” said Eliza Novick-Smith, his partner. “He has a pretty high pain tolerance,” given previous injuries from military service and mountain biking.
Harness went back to the hospital, where another CT scan revealed a blood clot the size of a brick floating in his pelvic area, a rare complication that most likely came from clipping and stapling the appendix tissue in the first surgery, said his surgeon. He would need another operation to check for the source of bleeding and to remove the clot.
After four more days in the hospital, he went home. It took him a couple of months to fully recover.
Then the bill came.
Patient: Shannon Harness, 39, an operations manager for a company that builds mountain bike trails across the country and a Marine Corps veteran. At the time of this incident, Harness had no insurance.
Total Owed: The original hospital bill was $80,232 for both surgeries — the first surgery cost $35,906 and the clot surgery cost $44,326. These amounts do not include payments to the surgeon, anesthesiologist, pathologist or radiologist.
Service Provider: Heart of the Rockies Regional Medical Center, a nonprofit critical access hospital in Colorado, where the surgeries were performed. Anesthesia, radiology and pathology were performed by other providers.
Medical Services: Laparoscopic appendectomy, followed by a second surgery a few days later, to resolve complications.
What Gives: Uninsured patients are extremely vulnerable to exorbitant hospital bills. It’s difficult to negotiate with a hospital without the leverage and bargaining power of an insurance company. Worse, uninsured patients are often billed three or four times what an insurer or government program would pay for the same service, said Anthony Wright, executive director of Health Access California, an organization advocating for affordable health care in California.
“As somebody who’s uninsured, you are getting an unnegotiated rate,” Wright said, derived from the hospital’s master price list. Insurers typically pay a rate that is a tiny fraction of that cost.
Harness was uninsured for seven years before this incident. His employer didn’t offer insurance, and the Affordable Care Act plan he qualified for cost $350 a month — an amount he didn’t have.
One option for uninsured patients is a hospital’s financial assistance program, a requirement in some states. In Colorado, every hospital is supposed to have a comprehensive charity care program for uninsured patients who earn less than 250% of the federal poverty level.
Heart of the Rockies hospital determines financial assistance on a sliding scale of family size and income. They also offer a self-pay discount of 15% to uninsured patients. Harness said the hospital’s financial services office initially told him he was ineligible for their assistance program as well as the Colorado Indigent Care Program. Harness had worked overtime the previous month and missed the qualification by around $200. The hospital would use only his past two pay stubs to verify his income, he said.
The hospital wouldn’t answer any questions about Harness’ care or bills, even though he gave it permission to do so.
Another quirk of the U.S. health care system that Harness encountered is that when surgeries don’t go as planned, and need revision with another operation, the patient (or his insurer) typically pays again. Medicare and some insurers have experimented with “bundled payments,” through which the hospital gets a set fee for the surgery and any follow-up care for 90 days thereafter.
Resolution: Harness filed a grievance with the hospital with the help of Novick-Smith, who is a lawyer, to push back on the bills for the two surgeries — $35,906 for the first and $44,326 more for the second —and express concerns with the quality of care.
Healthcare Bluebook, which estimates costs based on insurers’ claims data, says a fair price for an appendectomy in Salida is around $12,600. Dr. Gina Adrales, director of minimally invasive surgery at Johns Hopkins Medicine in Baltimore, said the complication Harness experienced is not common. The complication rate for an appendectomy is fairly low, she said.
In November, the hospital decided to give Harness a 30% discount for both surgeries, leaving him with a still hefty bill of $56,162.40.
The couple followed up repeatedly with the hospital for months, often finding representatives “hard to reach.” More than six months later, in March, the hospital told Harness he would have to pay for the second surgery because it was a risk he accepted by agreeing to the appendectomy.
Adam Fox, director of strategic engagement at Colorado Consumer Health Initiative, said it’s “especially important” to push back on bills resulting from surgical complications. “It usually indicates that something didn’t go right in the first surgery and at least that second surgery should be provided at a substantially reduced cost to the individual,” he said.
By May, the hospital gave in. Lesley Fagerberg, Heart of the Rockies’ vice president of financial services, wrote a response to Harness’ grievance, reducing the total bill by roughly the amount charged for the second surgery. But she didn’t explain how the hospital had come to that decision.
“Unfortunately, there was a complication in your appendectomy surgery,” Fagerberg wrote. “As explained in the consent to treat, a surgery/procedure has inherent risk. Your case has been reviewed and the total bill has been reduced by $31,218.60.”
Harness’ final bill from the hospital, Fagerberg wrote, stands at $22,304.17 after adjustments that included a self-pay discount.
Harness and Novick-Smith said that still seemed too high to them, and after some research, offered to pay the hospital $12,000 upfront. The hospital rejected this offer.
Now, Harness is working out a payment plan with the hospital. The hospital offers an interest-free payment plan if he can pay it off in two years, but for Harness, those monthly payments would be more than his rent.
“I would not be able to do it by myself, like, I wouldn’t have another choice other than taking out a loan,” Harness said. “Before the appendectomy, I was looking for property and homes to purchase, and that is pretty much completely off the table right now.”
Novick-Smith said she’s glad the hospital ultimately wrote off the bill for the second surgery. But she still feels angry with the hospital.
“What feels particularly hard is that the hospital markets itself in our community as this vital community resource and they provide a lot of jobs,” she said. “Their lack of transparency and lack of communication with us made this all a whole lot worse especially because there’s nowhere else to go.”
The Takeaway: The United States health care system is not forgiving to the uninsured, who, paradoxically, often face the highest bills of all patients. The benefit of having insurance is in part that your plan pays much of the bill, but also that you get the benefit of being charged the plan’s highly discounted rates. If your employer doesn’t provide health insurance, check whether you’re eligible for a public program, said Wright.
Harness now has VA Health Care. He initially avoided looking into VA Health Care because he felt “other vets needed it more.”
If you’re uninsured and stuck with a huge bill, Fox said, the first step is to ask for an itemized bill to ensure it reflects the actual service you received. The next step is to check the hospital’s charity care policy. Another resource uninsured patients can turn to are organizations like the Colorado Consumer Health Initiative.
“It’s by no means a perfect solution because there’s only so much that we can do to help consumers advocate for themselves in these cases, but we do our best,” Fox said.
If all else fails, Wright said, it’s best to put pressure on the hospital before they sell the bill to a collections agency. There’s less room for negotiation once a bill goes to collections, Wright said. And if all else really fails, you could try calling the press.
Bill of the Month is a crowdsourced investigation by KHN and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
Veteran’s Appendectomy Launches Excruciating Months-Long Battle Over Bill published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
Veteran’s Appendectomy Launches Excruciating Months-Long Battle Over Bill
In late August 2019, Shannon Harness awoke to serious pain in the lower right side of his abdomen — a telltale sign of appendicitis.
He booked it to the emergency room of the only hospital in the county: Heart of the Rockies Regional Medical Center in Salida, Colorado. After a CT scan, doctors told Harness he had acute appendicitis and required immediate surgery.
A surgeon performed an appendectomy that night and released Harness the next day.
But a couple of days later, Harness felt sharp pains where his appendix had been. The pain grew until he was on the floor screaming.
“It was disturbing,” said Eliza Novick-Smith, his partner. “He has a pretty high pain tolerance,” given previous injuries from military service and mountain biking.
Harness went back to the hospital, where another CT scan revealed a blood clot the size of a brick floating in his pelvic area, a rare complication that most likely came from clipping and stapling the appendix tissue in the first surgery, said his surgeon. He would need another operation to check for the source of bleeding and to remove the clot.
After four more days in the hospital, he went home. It took him a couple of months to fully recover.
Then the bill came.
Patient: Shannon Harness, 39, an operations manager for a company that builds mountain bike trails across the country and a Marine Corps veteran. At the time of this incident, Harness had no insurance.
Total Owed: The original hospital bill was $80,232 for both surgeries — the first surgery cost $35,906 and the clot surgery cost $44,326. These amounts do not include payments to the surgeon, anesthesiologist, pathologist or radiologist.
Service Provider: Heart of the Rockies Regional Medical Center, a nonprofit critical access hospital in Colorado, where the surgeries were performed. Anesthesia, radiology and pathology were performed by other providers.
Medical Services: Laparoscopic appendectomy, followed by a second surgery a few days later, to resolve complications.
What Gives: Uninsured patients are extremely vulnerable to exorbitant hospital bills. It’s difficult to negotiate with a hospital without the leverage and bargaining power of an insurance company. Worse, uninsured patients are often billed three or four times what an insurer or government program would pay for the same service, said Anthony Wright, executive director of Health Access California, an organization advocating for affordable health care in California.
“As somebody who’s uninsured, you are getting an unnegotiated rate,” Wright said, derived from the hospital’s master price list. Insurers typically pay a rate that is a tiny fraction of that cost.
Harness was uninsured for seven years before this incident. His employer didn’t offer insurance, and the Affordable Care Act plan he qualified for cost $350 a month — an amount he didn’t have.
One option for uninsured patients is a hospital’s financial assistance program, a requirement in some states. In Colorado, every hospital is supposed to have a comprehensive charity care program for uninsured patients who earn less than 250% of the federal poverty level.
Heart of the Rockies hospital determines financial assistance on a sliding scale of family size and income. They also offer a self-pay discount of 15% to uninsured patients. Harness said the hospital’s financial services office initially told him he was ineligible for their assistance program as well as the Colorado Indigent Care Program. Harness had worked overtime the previous month and missed the qualification by around $200. The hospital would use only his past two pay stubs to verify his income, he said.
The hospital wouldn’t answer any questions about Harness’ care or bills, even though he gave it permission to do so.
Another quirk of the U.S. health care system that Harness encountered is that when surgeries don’t go as planned, and need revision with another operation, the patient (or his insurer) typically pays again. Medicare and some insurers have experimented with “bundled payments,” through which the hospital gets a set fee for the surgery and any follow-up care for 90 days thereafter.
Resolution: Harness filed a grievance with the hospital with the help of Novick-Smith, who is a lawyer, to push back on the bills for the two surgeries — $35,906 for the first and $44,326 more for the second —and express concerns with the quality of care.
Healthcare Bluebook, which estimates costs based on insurers’ claims data, says a fair price for an appendectomy in Salida is around $12,600. Dr. Gina Adrales, director of minimally invasive surgery at Johns Hopkins Medicine in Baltimore, said the complication Harness experienced is not common. The complication rate for an appendectomy is fairly low, she said.
In November, the hospital decided to give Harness a 30% discount for both surgeries, leaving him with a still hefty bill of $56,162.40.
The couple followed up repeatedly with the hospital for months, often finding representatives “hard to reach.” More than six months later, in March, the hospital told Harness he would have to pay for the second surgery because it was a risk he accepted by agreeing to the appendectomy.
Adam Fox, director of strategic engagement at Colorado Consumer Health Initiative, said it’s “especially important” to push back on bills resulting from surgical complications. “It usually indicates that something didn’t go right in the first surgery and at least that second surgery should be provided at a substantially reduced cost to the individual,” he said.
By May, the hospital gave in. Lesley Fagerberg, Heart of the Rockies’ vice president of financial services, wrote a response to Harness’ grievance, reducing the total bill by roughly the amount charged for the second surgery. But she didn’t explain how the hospital had come to that decision.
“Unfortunately, there was a complication in your appendectomy surgery,” Fagerberg wrote. “As explained in the consent to treat, a surgery/procedure has inherent risk. Your case has been reviewed and the total bill has been reduced by $31,218.60.”
Harness’ final bill from the hospital, Fagerberg wrote, stands at $22,304.17 after adjustments that included a self-pay discount.
Harness and Novick-Smith said that still seemed too high to them, and after some research, offered to pay the hospital $12,000 upfront. The hospital rejected this offer.
Now, Harness is working out a payment plan with the hospital. The hospital offers an interest-free payment plan if he can pay it off in two years, but for Harness, those monthly payments would be more than his rent.
“I would not be able to do it by myself, like, I wouldn’t have another choice other than taking out a loan,” Harness said. “Before the appendectomy, I was looking for property and homes to purchase, and that is pretty much completely off the table right now.”
Novick-Smith said she’s glad the hospital ultimately wrote off the bill for the second surgery. But she still feels angry with the hospital.
“What feels particularly hard is that the hospital markets itself in our community as this vital community resource and they provide a lot of jobs,” she said. “Their lack of transparency and lack of communication with us made this all a whole lot worse especially because there’s nowhere else to go.”
The Takeaway: The United States health care system is not forgiving to the uninsured, who, paradoxically, often face the highest bills of all patients. The benefit of having insurance is in part that your plan pays much of the bill, but also that you get the benefit of being charged the plan’s highly discounted rates. If your employer doesn’t provide health insurance, check whether you’re eligible for a public program, said Wright.
Harness now has VA Health Care. He initially avoided looking into VA Health Care because he felt “other vets needed it more.”
If you’re uninsured and stuck with a huge bill, Fox said, the first step is to ask for an itemized bill to ensure it reflects the actual service you received. The next step is to check the hospital’s charity care policy. Another resource uninsured patients can turn to are organizations like the Colorado Consumer Health Initiative.
“It’s by no means a perfect solution because there’s only so much that we can do to help consumers advocate for themselves in these cases, but we do our best,” Fox said.
If all else fails, Wright said, it’s best to put pressure on the hospital before they sell the bill to a collections agency. There’s less room for negotiation once a bill goes to collections, Wright said. And if all else really fails, you could try calling the press.
Bill of the Month is a crowdsourced investigation by KHN and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
from Updates By Dina https://khn.org/news/bill-of-the-month-veteran-appendectomy-complication-long-battle-over-bill/
0 notes
Text
Veteran’s Appendectomy Launches Excruciating Months-Long Battle Over Bill
In late August 2019, Shannon Harness awoke to serious pain in the lower right side of his abdomen — a telltale sign of appendicitis.
He booked it to the emergency room of the only hospital in the county: Heart of the Rockies Regional Medical Center in Salida, Colorado. After a CT scan, doctors told Harness he had acute appendicitis and required immediate surgery.
A surgeon performed an appendectomy that night and released Harness the next day.
But a couple of days later, Harness felt sharp pains where his appendix had been. The pain grew until he was on the floor screaming.
“It was disturbing,” said Eliza Novick-Smith, his partner. “He has a pretty high pain tolerance,” given previous injuries from military service and mountain biking.
Harness went back to the hospital, where another CT scan revealed a blood clot the size of a brick floating in his pelvic area, a rare complication that most likely came from clipping and stapling the appendix tissue in the first surgery, said his surgeon. He would need another operation to check for the source of bleeding and to remove the clot.
After four more days in the hospital, he went home. It took him a couple of months to fully recover.
Then the bill came.
Patient: Shannon Harness, 39, an operations manager for a company that builds mountain bike trails across the country and a Marine Corps veteran. At the time of this incident, Harness had no insurance.
Total Owed: The original hospital bill was $80,232 for both surgeries — the first surgery cost $35,906 and the clot surgery cost $44,326. These amounts do not include payments to the surgeon, anesthesiologist, pathologist or radiologist.
Service Provider: Heart of the Rockies Regional Medical Center, a nonprofit critical access hospital in Colorado, where the surgeries were performed. Anesthesia, radiology and pathology were performed by other providers.
Medical Services: Laparoscopic appendectomy, followed by a second surgery a few days later, to resolve complications.
What Gives: Uninsured patients are extremely vulnerable to exorbitant hospital bills. It’s difficult to negotiate with a hospital without the leverage and bargaining power of an insurance company. Worse, uninsured patients are often billed three or four times what an insurer or government program would pay for the same service, said Anthony Wright, executive director of Health Access California, an organization advocating for affordable health care in California.
“As somebody who’s uninsured, you are getting an unnegotiated rate,” Wright said, derived from the hospital’s master price list. Insurers typically pay a rate that is a tiny fraction of that cost.
Harness was uninsured for seven years before this incident. His employer didn’t offer insurance, and the Affordable Care Act plan he qualified for cost $350 a month — an amount he didn’t have.
One option for uninsured patients is a hospital’s financial assistance program, a requirement in some states. In Colorado, every hospital is supposed to have a comprehensive charity care program for uninsured patients who earn less than 250% of the federal poverty level.
Heart of the Rockies hospital determines financial assistance on a sliding scale of family size and income. They also offer a self-pay discount of 15% to uninsured patients. Harness said the hospital’s financial services office initially told him he was ineligible for their assistance program as well as the Colorado Indigent Care Program. Harness had worked overtime the previous month and missed the qualification by around $200. The hospital would use only his past two pay stubs to verify his income, he said.
The hospital wouldn’t answer any questions about Harness’ care or bills, even though he gave it permission to do so.
Another quirk of the U.S. health care system that Harness encountered is that when surgeries don’t go as planned, and need revision with another operation, the patient (or his insurer) typically pays again. Medicare and some insurers have experimented with “bundled payments,” through which the hospital gets a set fee for the surgery and any follow-up care for 90 days thereafter.
Resolution: Harness filed a grievance with the hospital with the help of Novick-Smith, who is a lawyer, to push back on the bills for the two surgeries — $35,906 for the first and $44,326 more for the second —and express concerns with the quality of care.
Healthcare Bluebook, which estimates costs based on insurers’ claims data, says a fair price for an appendectomy in Salida is around $12,600. Dr. Gina Adrales, director of minimally invasive surgery at Johns Hopkins Medicine in Baltimore, said the complication Harness experienced is not common. The complication rate for an appendectomy is fairly low, she said.
In November, the hospital decided to give Harness a 30% discount for both surgeries, leaving him with a still hefty bill of $56,162.40.
The couple followed up repeatedly with the hospital for months, often finding representatives “hard to reach.” More than six months later, in March, the hospital told Harness he would have to pay for the second surgery because it was a risk he accepted by agreeing to the appendectomy.
Adam Fox, director of strategic engagement at Colorado Consumer Health Initiative, said it’s “especially important” to push back on bills resulting from surgical complications. “It usually indicates that something didn’t go right in the first surgery and at least that second surgery should be provided at a substantially reduced cost to the individual,” he said.
By May, the hospital gave in. Lesley Fagerberg, Heart of the Rockies’ vice president of financial services, wrote a response to Harness’ grievance, reducing the total bill by roughly the amount charged for the second surgery. But she didn’t explain how the hospital had come to that decision.
“Unfortunately, there was a complication in your appendectomy surgery,” Fagerberg wrote. “As explained in the consent to treat, a surgery/procedure has inherent risk. Your case has been reviewed and the total bill has been reduced by $31,218.60.”
Harness’ final bill from the hospital, Fagerberg wrote, stands at $22,304.17 after adjustments that included a self-pay discount.
Harness and Novick-Smith said that still seemed too high to them, and after some research, offered to pay the hospital $12,000 upfront. The hospital rejected this offer.
Now, Harness is working out a payment plan with the hospital. The hospital offers an interest-free payment plan if he can pay it off in two years, but for Harness, those monthly payments would be more than his rent.
“I would not be able to do it by myself, like, I wouldn’t have another choice other than taking out a loan,” Harness said. “Before the appendectomy, I was looking for property and homes to purchase, and that is pretty much completely off the table right now.”
Novick-Smith said she’s glad the hospital ultimately wrote off the bill for the second surgery. But she still feels angry with the hospital.
“What feels particularly hard is that the hospital markets itself in our community as this vital community resource and they provide a lot of jobs,” she said. “Their lack of transparency and lack of communication with us made this all a whole lot worse especially because there’s nowhere else to go.”
The Takeaway: The United States health care system is not forgiving to the uninsured, who, paradoxically, often face the highest bills of all patients. The benefit of having insurance is in part that your plan pays much of the bill, but also that you get the benefit of being charged the plan’s highly discounted rates. If your employer doesn’t provide health insurance, check whether you’re eligible for a public program, said Wright.
Harness now has VA Health Care. He initially avoided looking into VA Health Care because he felt “other vets needed it more.”
If you’re uninsured and stuck with a huge bill, Fox said, the first step is to ask for an itemized bill to ensure it reflects the actual service you received. The next step is to check the hospital’s charity care policy. Another resource uninsured patients can turn to are organizations like the Colorado Consumer Health Initiative.
“It’s by no means a perfect solution because there’s only so much that we can do to help consumers advocate for themselves in these cases, but we do our best,” Fox said.
If all else fails, Wright said, it’s best to put pressure on the hospital before they sell the bill to a collections agency. There’s less room for negotiation once a bill goes to collections, Wright said. And if all else really fails, you could try calling the press.
Bill of the Month is a crowdsourced investigation by KHN and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
Veteran’s Appendectomy Launches Excruciating Months-Long Battle Over Bill published first on https://smartdrinkingweb.weebly.com/
0 notes