#the rapid onset of confusion due to withdrawal
Text

i imagine the kid who made this growing up in the fringes of the okefenokee dreaming of sharing tea with the queen
#the a brief reprieve from the trauma of dislocation#traavelers#toilets#so drunk i had to grab onto the weeds to keep from falling off the edge of the world#once transplanted still sustained#the tragedy of transhuman relationships#pink blots#bathrooms#the rapture#the rapid onset of confusion due to withdrawal#i imagine the kid who made this growing up in the fringes of the okefenokee dreaming of sharing tea with the queen#pink spots#rogues#places where thieves meet#pixies#pink elephant#flying pig#dark creatures in pretty pink capes#crak#confusion#north fungi county#georgia
78 notes
·
View notes
Text
Understanding Nembutal capsules mechanism of action

Nembutal, also known as pentobarbital, is a medication primarily used for its sedative and hypnotic properties. Understanding its mechanism of action is crucial for both medical professionals and individuals seeking information about its effects and usage.
What are Nembutal Capsules?
Nembutal capsules are a pharmaceutical formulation containing pentobarbital, a barbiturate derivative. These capsules are commonly prescribed for their sedative, hypnotic, and anticonvulsant effects. They belong to the class of drugs known as central nervous system (CNS) depressants.
Mechanism of Action
Interaction with GABA Receptors
Nembutal acts primarily by enhancing the activity of gamma-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the brain. It binds to specific sites on GABA-A receptors, which are ligand-gated chloride channels. This binding results in the opening of chloride channels, leading to hyperpolarization of neuronal membranes and inhibition of neuronal excitability.
Effects on Central Nervous System
By enhancing GABAergic transmission, Nembutal produces sedative, hypnotic, and anxiolytic effects. It induces a state of calmness, relaxation, and drowsiness, making it effective for treating conditions such as insomnia, anxiety, and agitation.
Pharmacokinetics
Nembutal is well-absorbed after oral administration, with peak plasma concentrations reached within 1 to 4 hours. It is widely distributed throughout the body, including the brain, where it exerts its pharmacological effects. The drug is primarily metabolized in the liver and undergoes renal excretion.
Indications for Use
Nembutal capsules are prescribed for various medical conditions, including:
Treatment of insomnia
Management of anxiety disorders
Sedation prior to surgical procedures
Control of seizures in certain neurological conditions
Dosage and Administration
The dosage of Nembutal capsules varies depending on the indication and individual patient factors. It is typically administered orally, either as a single dose or divided into multiple doses throughout the day.
Onset and Duration of Action
The onset of action of Nembutal is rapid, with sedative effects usually observed within 30 minutes to an hour after administration. The duration of action varies but is generally 4 to 6 hours for the hypnotic effects.
Side Effects and Adverse Reactions
Common Side Effects
Common side effects of Nembutal capsules include:
Drowsiness
Dizziness
Confusion
Respiratory depression
Nausea and vomiting
Serious Adverse Reactions
Serious adverse reactions may occur with high doses or prolonged use of Nembutal, including:
Respiratory depression leading to respiratory arrest
Cardiovascular collapse
Dependence and withdrawal symptoms upon discontinuation
Contraindications
Nembutal capsules are contraindicated in individuals with:
Hypersensitivity to barbiturates
Severe respiratory insufficiency
Acute intermittent porphyria
History of substance abuse or dependence
Drug Interactions
Nembutal may interact with other medications, including:
Alcohol
Benzodiazepines
Opioids
Antidepressants
Overdose and Management
Signs of Nembutal overdose include profound central nervous system depression, respiratory depression, and cardiovascular collapse. Management of overdose involves supportive care, including airway management, respiratory support, and monitoring of vital signs.
Regulatory Status
Nembutal is a controlled substance in many countries due to its potential for abuse and dependence. It is classified as a Schedule II controlled substance in the United States under the Controlled Substances Act.
Controversies Surrounding Nembutal
Nembutal has been the subject of controversy due to its association with euthanasia and assisted suicide. Some advocacy groups and individuals argue for its availability as a means of peaceful death, while others raise ethical and legal concerns regarding its use for this purpose.
Conclusion
Nembutal capsules exert their pharmacological effects primarily by enhancing GABAergic transmission in the central nervous system. Understanding their mechanism of action, pharmacokinetics, indications for use, and potential adverse reactions is essential for safe and effective clinical practice.
Frequently Asked Questions
Is Nembutal addictive?
Nembutal has a potential for dependence and addiction, especially with prolonged use or high doses.
Can Nembutal be used for euthanasia?
While Nembutal has been used for euthanasia in some cases, its legality and ethical implications vary by jurisdiction.
What should I do if I miss a dose of Nembutal?
If you miss a dose of Nembutal, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule.
Are there any lifestyle changes I should make while taking Nembutal?
It is important to avoid alcohol and other CNS depressants while taking Nembutal, as they can increase the risk of side effects and overdose.
How should Nembutal be stored?
Nembutal capsules should be stored at room temperature away from moisture and heat. Keep them out of reach of children and pets.
0 notes
Text
“Meth Mouth”: One of the Many Reasons to Avoid Crystal Meth

“Meth mouth” is one specific effect of using the dangerous drug methamphetamine (Crystal Meth). While it may be one of the more visible outward signs of the drug, it’s not the only harmful effect of crystal meth addiction.
What is Methamphetamine?
Methamphetamine, also known as meth, is an addictive stimulant affecting the central nervous system.
Crystal methamphetamine is a version of the drug that looks like glass or rocks, and it’s got a chemical structure similar to amphetamine.
Medical professionals use Amphetamine in the treatment of attention-deficit hyperactivity disorder (ADHD).
Drug users take meth in different ways; smoked, swallowed, snorted, or injecting a dissolved version.
When someone takes methamphetamine, it increases the amount of dopamine in their brain, which causes them to feel an intense high.
Meth releases artificially high amounts of dopamine in the brain.
That then activates reward centers in the brain, making the user compulsively start taking the substance.
In the short term, meth can have side effects such as:
Increased energy and alertness
Decreased appetite
Fast breathing
Rapid heartbeat
Increased blood pressure and body temperature
Dry mouth
Violent behavior
How Long Does Meth Stay in Your System?
Users feel the effects of meth rapidly after introducing the drug into their system, especially if it’s injected or smoked. The onset speed results from the body absorbing the drug as soon as it enters the bloodstream.

The actual high of being on meth is short-lived, leading to rapid cycling where someone binges on it and uses a significant amount within a short window of time.
The half-life of meth, that’s how long it takes the body to break down the meth to one-half of the dose used, is around 12 to 34 hours.
Even though someone might not feel the euphoric high for long, they can feel the effects of the drug for up to 24 hours after the last time they used it.
If someone were to undergo a drug test, meth could show up in a blood test for up to 72 hours after use, and if you used large amounts, as long as ten days.
Detected in urine testing, meth metabolites could be detectable for three to five days after use.
Why Is Meth So Dangerous?
Meth is considered one of the most dangerous and potentially deadly illicit drugs.
Some of the reasons this is true include:
Meth is highly addictive. It’s not uncommon for people to become addicted after using it just once. It’s possibly the most addictive recreational drug available.
The intense highs of meth come with equally as intense lows. When you come down from a meth high, it can create extreme misery and depression. For instance, while high on meth you may stay awake for days, but when you crash you might end up sleeping for days.
If you inject meth, it creates a whole other set of risks in addition to the dangers of the drug itself. For example, this can put you at risk of contracting infectious diseases like hepatitis or HIV.
As a stimulant, meth raises your core body functions, including your breathing, body temperature, nausea, vomiting, diarrhea and heart rate, putting you at risk of heart attack or stroke as well as a fatal overdose.
Meth creates permanent brain damage.
While meth is one of the more dangerous and addictive drugs that exists, treatment options are available for those who are struggling, but ready to quit.
Opus Health has helped many people break the chains of this dangerous addiction.
The Long-Term Effects of Meth Abuse
There are many long-term effects of meth.
Some may be reversible with the right treatment options if you stop using the drug, while others may not be.
Long-term effects of meth use:
Weight loss
Severe dental problems
Sores from scratching
Changes in the function and structure of the brain
Memory loss
Confusion
Sleep problems
Violence
Paranoia, which is an extreme, irrational distrust of others
Hallucinations, which are images or sensory experiences that aren’t real
Bad Breath
Irregular heartbeat
Dental decay
Over time, when someone uses methamphetamine repeatedly, it causes changes in the dopamine system.
That can lead to impaired verbal learning and coordination problems.
There have been brain imaging studies of long-term meth users indicating significant changes in the areas of the brain related to memory and emotion.
One study was completed relatively recently that individuals who used meth even once were at a higher risk of developing Parkinson’s disease.
Parkinson’s affects the nerves and movement.
Addiction and dependence are also considered long-term effects of meth.
Someone dependent on meth may experience withdrawal symptoms when they stop using it.
Meth withdrawal symptoms may include severe depression, psychosis, cravings, fatigue, and anxiety.
What Is Meth Mouth?
The term meth mouth refers to dental damage and oral hygiene issues specifically related to meth addicts.
Long-term methamphetamine abuse will cause tooth decay.
This decay can be due to the effects of drugs themselves, the tendency to eat sugary foods and drink sugary beverages when on meth, and a lack of self-care.
For example, research from the American Dental Association found among meth users, 96% had cavities. In addition, 58% had tooth decay, and more than 30% had six or more missing teeth.

People who smoked meth were three times as likely to experience symptoms of meth mouth than people who used it in other ways.
Noticeable meth mouth can occur within a year of using the drug for many people.
Actual symptoms of meth mouth include dry mouth, gum disease, and tooth decay.
When someone is high on meth they might clench or grind their teeth when they are, which can also make the oral health and appearance of their mouth worse.
When you use meth, you can experience xerostomia, which is just another term for dry mouth. That then reduces your teeth’s natural protection, leading them to decay more quickly.
What is the “Faces of Meth Project”?
The appearance of meth users can be so dramatically changed by the drug that in the early 2000s, the Faces of Meth Project was born.
It’s a drug prevention initiative run by the Multnomah County Sheriff’s Office in Oregon, highlighting physical changes the drug can cause.
The project uses mug shots of repeat offenders to show the damaging effects of using meth over a period of time.
The project uses both before and after mug shots which highlight the intense deterioration caused by the drug.
Along with the effects on dental health and meth mouth, taking meth can also cause facial sores.
Often what will happen is either that someone burns themselves when they’re smoking meth, or they experience the sensation that bugs are crawling on them, causing incessant scratching, leading to bleeding and subsequent sores.
Conclusion: Seeking Treatment
If you are a methamphetamine user, or someone you know, the most important fact for you to remember is that treatment facilities like Opus Health can help.
Methamphetamine addiction is dangerous and potentially deadly, but it’s never too late to get help.
With proper treatment, it’s possible to be safe going through meth withdrawal and to enter into recovery.
Healing can occur physically, mentally, and spiritually with the right treatment.
Opus Health can help you every step of the way, from detox to aftercare.
Call us today for a free consultation with a care coordinator and take your first steps towards a new smile.
0 notes
Text
Adolescent Depression: causes, symptoms, treatment, and Parental Communication

Adolescence is a time of transition, and it is "natural" for adolescents to be moody, irritable, lonely. As a result, depression in teenagers is often misdiagnosed or merely due to normal teenage behavior.
The stresses of everyday life are also having a negative impact on our young teens. Take a look at the numbers below and be astounded.
Figures dont lie, and they are also the perfect way to highlight those details that, when introduced to the general public's attention, leave a permanent impression. It is important to capture the interest of someone who wishes to hear more about what the numbers are showing. There is no wonder that numbers are nothing more than concrete concepts with the potential to sway even the most cynical of minds, and it would even offer the young generation the real picture when it comes to teenage depression.
Twenty Percent Of Teenagers Are Sufferers
The first thing that will make you wake up and take notes of adolescent depression rates is the fact that almost one-fifth of the adolescent population of the United States has undergone a degree of psychiatric depression before reaching full adulthood.
Not just that, but ten to fifteen percent of adolescents have signs of adolescent depression, while another five percent of the adolescent population has suffered from major depression.
Second, another concerning feature of adolescent depression is the lack of social acceptance for adolescents with such an illness, and what's worst is that as many as 8% of teenagers would have witnessed the recurrence of depression at least once a year. This is concerning because depression affects just 5% of the national population.
adolescent depression usually lasts for eight months. Teenagers are now at risk of having another bout of adolescent depression within two years, with the chances of this happening ranging from twenty to forty percent, and there is also a seventy percent chance that they will have another bout of adolescent depression.
Third, a common characteristic of adolescence depression is that many teens experience seasonal depression. This form of depression is most common during the winter, but it can also be seen in areas of high altitudes. And the weather may play a role in the onset of seasonal depression, so teens must be mindful of these social influences on their mental health.
Fourth, other data on adolescent depression show that dysthymia, or a moderate type of depression that persists for a long time, affects around 2% of adolescents, and a similar number of teenagers are more likely to develop bipolar depression as they get older. Indeed, it is estimated that up to 15% of teens who have had major depression are at risk of experiencing bipolar depression later in life.
As a result, it is fair to conclude that adolescent depression can impact adolescents regardless of their socioeconomic status, economic class, ethnicity, ethnicity, or accomplishments, and that adolescent depression is a very serious mental health condition affecting teens in the United States.
There are some prominent early signs of adolescent depression. If you think your underage child is troubled, you must get treatment urgently.
Adolescent Depression Different Than Adult Depression?
Depression is a mood disease in which people feel depressed, withdrawn, lose confidence in what is going on around them, have learning difficulties, and can even commit suicide. Depressive symptoms are normal, and most people will experience them at some stage in their life even though they are not diagnosed with depression. Men have a lifetime prevalence of depression ranging from 5% to 12%, whereas women have a prevalence ranging from 10% to 25%. Severe depression ranked fourth in terms of disease dysfunction and related risk factors in 1990. Depression is expected to rate second only to heart disease as a concern by the year 2020. Depression has also been attributed to an elevated risk of cancer, respiratory failure, immune dysfunction, allergies, migraine, insomnia, infectious disease, and suicide.
The body responds similarly to depression and stress. Corticosteroids are hormones that are produced when a person is stressed or depressed. Cortisol levels in the adrenal glands rise and remain elevated during depression, affecting long-term memory. Individuals suffering from depression include increased development in the hypothalamus, pituitary gland, and adrenal glands. Long-term stress has been linked to a decline in hypothalamus volume. The hypothalamus is in charge of processing input from the autonomic nervous system and controlling feeding, sexual activity, sleep habits, impulses, and hormone secretion. People who have had repeated bouts of depression have irregular electroencephalograph sleep cycles. Enlarged ventricles and greater cerebral atrophy have been observed in depressive patients with psychotic characteristics.
Adolescent depression can show itself in a variety of ways. Adolescents and infants, according to the DSM-IV-TR, exhibit more irritability, social withdrawal, and somatic complaints. Displays of melancholy and psychomotor retardation, as seen in people with depressive disorders, are not common in teenagers. Adolescent depression, on the other hand, may be characterized by frustration, confusion, exhaustion, and lack of interest in usually pleasurable activities. Another characteristic of teen depression is that it affects both boys and girls equally.
Because of the presenting signs, adolescent depression is impossible to diagnose. Other conditions, such as Conduct Disorder, Attention-Deficit/Hyperactivity Disorder, and Anxiety, are often associated with the disorder. There are two forms of depression. Shyness, fear, worrying behavior, and avoidance are all correlated with internalizing style. Externalizing personality is linked to substance addiction and behavior disorder.
A variety of studies have associated depression and other psychosocial factors to adult pain perception. It stands to reason that depression, or symptoms of depression, will be found in teenagers who are in distress. Adolescents' sense of well-being has been attributed to low back and mid-back pain. Adolescents and children who have back pain complain that their health is bad and that they are unhappy. Physical fitness is a major indicator of depression in youth, both now and in the future. In addition, physical disorder is linked to depression.
Warning signs and symptoms Of Adolescent Depression
Poor or fluctuating grades in school, disappointment in school or at work, and a sense of inability to achieve expectations are all red flags. Withdrawal from friends, family, and hobbies is another possibility. They will become more isolated as time goes by. They can show signs of depression, hopelessness, and a lack of motivation/enthusiasm. Their self-esteem may range from poor to non-existent.
They may be unable to focus, make decisions, or miss things sometimes. Changes of sleep and appetite are possible. They can become irritable, irritated, and anxious as a result. They can become addicted to substances (self-medicate), depressed, or obsessed with death. When the adolescent exhibits some of these symptoms, continue to speak to them, even if it's just to let them know you're there for them, and get treatment right away.
There are some indicators that a person is suffering from adolescent depression. Changes in appetite, changes in sleep schedule, lack of interest in usually common sports, irritability and often irrational response to anger, and, last but not least, declarations of depression are among the signs.
Changes in appetite or eating habits are a typical and very strong indicator of teenage depression. In reality, it is one of the primary symptoms. More specifically, the signs can include eating too much, eating too little, or not eating at all for an extended period of time. These symptoms of teenage depression should not be confused with those with an eating disorder. However, these main signs may also turn into more neurotic habits, particularly as the patient begins to feel better following a diet shift.
Changes in sleep and sleep schedule, including changes of appetite or feeding pattern, are symptoms of teenage depression, but the behaviour varies from person to person. Nonetheless, a significant shift in sleep habits with no apparent cause should be regarded as a fairly solid and not-to-be-ignored warning sign.
Another well-known symptom of teenage depression is a rapid and unexplained decline in involvement in previously favored hobbies. It's not the same as when a child outgrows a passion of a certain game. If your child enjoys a sport and suddenly decides not to participate during the season, you should be concerned. It may be a symptom of teenage depression.
Another red flag, which is difficult to ignore, is when the child becomes enraged frequently or overreacts to his or her own annoyance. This may be more than just a case of more or less anticipated adolescent rebelliousness. However, distinguishing between typical juvenile misbehavior and depression-driven misbehavior requires the expertise of a trained and experienced healthcare professional.
There is no such thing as a single symptom of depression. It's still a slew of symptoms. When your child expresses despair, it may only be a terrible hair day, so if you've recently encountered any of the above symptoms of stress, it's time to take action. Call your doctor and brace yourself and your family for a bumpy trip.
Adolescent Depression - Causes and Best Treatment Options Available
Adolescent depression is a form of depression that may develop during adolescence. This form of depression is characterized by a lack of confidence, feelings of worthlessness, persistent disappointment, and discouragement, among other negative emotions. You can't tell whether an adolescent will get sad or not; often it can be predicted, but in most situations, it can be kept silent before anything happens. It is important to treat teen depression until it worsens, which could happen at any moment. You must address the issue as soon as you know you are stressed or your adolescent is depressed. It might not be an easy problem to solve, but you have to start somewhere.
Adolescent depression may be a teenager's acute reaction to such conditions or even normal stress, but it may also be a condition that they may recover from for years if they are not supported. When it comes to adolescents, depression is often caused by:
- Arguments of independence from parents
- a lack of liberty (in their minds).
- The normal maturing mechanism, as well as the tension and worry that it entails.
- Sexual hormones may play a significant role in depression.
Adolescent depression can also be a transient response to upsetting circumstances that may escalate to a lasting situation, such as:
- Failing school
- Being the victim of bullying
- Death of a relative or a close friend
- A sad breakup with a partner
Teenagers with poor self-esteem, those who are very critical of themselves, and those who believe they have little or no influence over such stressful experiences are at risk of depression. It is also well recognized that teenage girls are more likely than teenage boys to feel depression while they are going through a tough time.
Any of the risk factors are as follows:
- Unstable care giving
- Weak social skills
- Chronic illnesses
- Sexual, mental and physical child abuse
- Genetic depression - family history of the disorder
- Parental loss due to divorce or death, as well as other traumatic life activities
Any eating disorders, such as anorexia and bulimia, have been linked to adolescent depression..
Treatments
It is important to rule out any physical illnesses first, such as hypothyroidism or anemia. Depression should be considered after all physical causes have been ruled out. The below are some treatments for teenage depression:
When pursuing care for teenage depression, psychotherapy may be the first choice. Talk counseling attempts to help the troubled adolescent to improve their way of thinking. They will be taught more reasonable ways to solve their problems, as well as how to develop their interpersonal and social skills.
Medication - Antidepressants are often used for children, but with great caution. This is due to a lack of knowledge on the long-term impact of antidepressants on teenagers. Antidepressant side effects can cause children under the age of 21 to have suicidal thoughts or even attempt suicide, necessitating hospitalization.
Alternative treatments such as acupuncture, acupressure, and specifically tailored fitness plans can be beneficial to teenagers suffering from depression. Before adopting any new treatments, consult with your child's doctor.
Herbal supplements are completely safe and have far less, if any, side effects than antidepressants. Check with your child's doctor whether he or she is on any medications for any health issues. The herbs are not dangerous; however, they can diminish the potency of certain prescription drugs, putting your child at risk.
Coping With Adolescent Depression
Adolescent depression is highly common and can develop in children who will never feel it again.
Then, what happens?
It is popular for a variety of purposes. For instance, teenage hormone levels undergo drastic modifications and differences. Hormone fluctuations can disrupt a person's mental health. Technically, the condition is caused by a chemical imbalance in the brain. When chemicals or hormones get out of balance, a person becomes depressed. Adolescents are most likely to undergo the emotions when their hormones shift often..
Children are still suffering a great deal of tension. To an adult who may not have children, this will seem to be a humorous joke. They do, after all, have their whole life ahead of them. They have little commitments and are at a point in their lives where they will have a good time. Regrettably, this is not completely right. Teenagers are continually subjected to social pressure. They are pushed to be slim, to dress well, and to use drugs and alcohol. Any of these stresses, particularly drug and alcohol pressures, are difficult for a teenager to cope with. Drugs and alcohol are depressants, and if a teenager continues to use them, he or she can develop depression.
Loss is another cause. When a loved one dies, it is common for a person to feel depression. This trigger isn't just for teens.
What Should You Do?
Unfortunately, there isn't anything you can do to influence a teenager's hormones or reaction to social pressure. What you should do is speak to your kid about social pressure before they reach the age of adolescence. Describe what it is and how to deal with it. Keep a good watch on your infant as well. They may be depressed if they have severe mood swings or begin to behave abnormally. It may also be a warning if they become socially isolated and refuse to hang out with their mates. Maintain a constant line of contact with your kids. This will assist you with understanding how they are feeling.
If you or your kid suspects they are sad, take them to a mental health provider right away. You should begin by speaking with a school counselor. A school psychologist may be able to assist them in coping with their hormones and social pressure. However, if the emotions are more intense, you can see a therapist. Trained therapists are well equipped to treat teenage depression..
Adolescent Depression and Parent Communication

Photo by Ivan Samkov on Pexels.com
It is self-evident that puberty is a time of accelerated growth. The child's social responsibility extends into the home, and peer relationships tend to take precedence. Simultaneously, molecular changes are taking place, resulting in bursts of physical and academic development. It's no surprise that so many teenagers report feeling anxious and pressured.
Despite the above causes, most teenagers adapt to maturity without incident and grow up to be well-adjusted adults. In particular, study over the last ten years suggests that roughly 80% of all teenagers achieve maturity without major difficulties. Many of the remaining 20% face transition challenges as a result of a variety of reasons such as family conflicts, peer interactions, and educational pressures. For others, the end result is sadness, and normal development is halted.
Depression in puberty resembles adult depression. The adolescent is filled with depression, hopelessness, and a lack of interest in a brighter future. Eating and sleeping habits may change; friendships and family relationships may suffer; and school grades may begin to fall. In certain circumstances, the stress subsides and life resumes normalcy. However, if depression persists, the adolescent's life trajectory will be permanently changed, leading to school failure, drug misuse, and an unstable adult lifestyle.
Fortunately, parents may take a variety of measures to assist their teen in overcoming stress and returning to normal functioning.
To begin, it is critical to understand the improvements in the teen's biochemistry predispose them to emotional control issues. As a result, juvenile populations experience emotional extremes more often than infant or adult populations. Some days can feel like a roller coaster of emotional highs and lows. As a result, adults can become irritated and impatient when a teenager expresses his or her feelings.
Second, it is critical to recognize that these emotional responses are very genuine, and that often just listening can be extremely beneficial to the teen. For example, when teenagers are so dependent on their peers, the absence of a best friend or first girlfriend is always viewed as tragic. And parents who are sympathetic to their teen's sadness may grow impatient as the teen's storms of crying, sleepless nights, and sullen demeanor disrupt the family environment. However, if parents are not present, teens can find another person to speak to. Someone else is usually another teenager who lacks the loyalty, empathy, and intelligence needed to be genuinely helpful. Furthermore, as hidden confidantes become Facebook comments, trust problems often emerge.
Parents wield considerable strength.
Read the full article
0 notes
Text
Phenobarbital
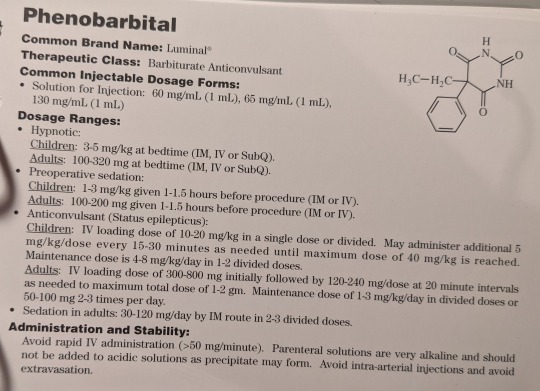

This medication is a Schedule IV drug.
Common Brand Names: Luminal
Therapeutic Class: Barbiturate anticonvulsant
Common Injectable Dosage Forms:
Solution for Injection: 60 mg/mL (1 mL), 65 mg/mL (1 mL), 130 mg/mL (1 mL)
Dosage Ranges:
Hypnotic:
Children: 3-5 mg/kg at bedtime (IM, IV, or SQ)
Adults: 100-320 mg at bedtime (IM, IV, or SQ)
Preoperative Sedation:
Children: 1-3 mg/kg given 1-1.5 hours before procedure (IM or IV)
Adults: 100-200 mg given 1-1.5 hours before procedure (IM or IV)
Anticonvulsant (Status Epilepticus):
Children: IV loading dose of 10-20 mg/kg in a single dose or divided. May administer additional 5 mg/kg/dose every 15-30 minutes as needed until maximum dose of 40 mg/kg is reached. Maintenance dose is 4-8 mg/kg/day in 1-2 divided doses.
Adults: IV loading dose of 300-800 mg initially followed by 120-240 mg/dose at 20-minute intervals as needed to maximum total dose of 1-2 g. Maintenance dose of 1-3 mg/kg/day in divided doses or 50-100 mg 2-3 times per day.
Sedation in adults: 30-120 mg/day by IM route in 2-3 divided doses.
Administration and Stability:
Avoid rapid IV administration (>50 mg/minute). Parenteral solutions are very alkaline and should not be added to acidic solutions as precipitate may form. Avoid intra-arterial injections and avoid extravasation.
Pharmacology/Pharmacokinetics:
Phenobarbital is a short-acting barbiturate with sedative, hypnotic, and anticonvulsant activity. Barbiturates depress the sensory cortex, decrease motor activity, alter cerebellar function, and produce drowsiness, sedation, and hypnosis. In high doses, barbiturates exhibit anticonvulsant activity and they produce dose-dependent respiratory depression. Onset of action is within 5 minutes when given IV with a peak effect in about 30 minutes. Duration of effect is about 4-10 hours and half-life is about 53-140 hours in adults and up to 500 hours in neonates.
Drug and Lab Interactions:
Phenobarbital is a strong inducer of CYP3A4 and CYP2A6 enzymes. When combined with other CNS depressants, ethanol, opioid analgesics, antidepressants, or benzodiazepines, additive respiratory and CNS depression may occur. Phenobarbital may decrease the effects of oral contraceptives, benzodiazepines, calcium channel blockers, rifampin, and venlafaxine. Barbiturates may also enhance the metabolism of methadone, resulting in methadone withdrawal symptoms.
Contraindications/Precautions:
Use with caution in severe hepatic impairment, dyspnea, porphyria, and pregnancy. Also use with caution in patients with hypovolemic shock, CHF, previous addictions to sedatives/hypnotics, and renal dysfunction. Phenobarbital is not recommended for use in the elderly due to its long half-life. Abrupt withdrawal of phenobarbital in patients with epilepsy may result in status epilepticus. Pregnancy Category D.
Monitoring Parameters:
Phenobarbital serum concentration, mental status, CBS, LFTs, and seizure activity.
Adverse Effects:
Possible side effects include bradycardia, hypotension, syncope, drowsiness, CNS excitation or depression, confusion, agitation, dizziness, hallucinations, Stevens-Johnson syndrome, nausea/vomiting, as well as hematologic changes.
Common Clinical Applications:
Used in the management of generalized tonic-clonic and partial seizures. Phenobarbital is also used as a sedative.
#sigler injectable drug cards#7th edition#phenobarbital#luminal#barbiturate#anticonvulsant#drug facts
1 note
·
View note
Text
How Long Does Hydrocodone Stay in Your System, Urine, Blood, Hair, Saliva, Drug Test
What is Hydrocodone? What is used for?
Hydrocodone is a generic name for an opioid analgesic drug. Chemically hydrocodone is also known as dihydrocodeinone . It is a semi-synthetic opioid medicine that is synthesized from codeine. Hysingla ER and Zohydro ER are long-acting forms of hydrocodone that are used for permanent treatment for the treatment of moderate to severe pain. The prolonged release form of hydrocodone is not to be used as needed for pain. Hydrocodone is also commonly used in liquid form as an antitussive / antitussive.
Click here for more detail How Long Does Hydrocodone Stay in Your System,
How does Hydrocodone work?
Hydrocodone works as an opioid agonist for opioid receptors in the brain. This medication blocks the perception of pain in the cerebral cortex of the brain. Hydrocodone reduces synaptic chemical transmission in the brain, which then inhibits the sensation of pain in the higher centers of the brain.
The agonist actions in the μ and k receptors cause analgesia, decrease in body temperature and miosis. The agonist activity in the μ receptor may also cause the suppression of opioid withdrawal, while the antagonist activity may result in the precipitation of abstinence. Hydrocodone acts in several areas within the brain by involving several neurotransmitter systems to relieve pain, but the precise mechanism has not yet been fully understood.
Side effects of Hydrocodone
Common side effects of hydrocodone that usually do not require medical attention include:
dizziness
drowsiness
Itch
nausea
vomiting
Side effects that patients should report to their doctor or health professional as soon as possible, since they can be very serious include:
shortness of breath, wheezing
allergic reactions such as rash, itching or hives, swelling of the face, lips or tongue
Confusion
light dizziness or fainting
How long does hydrocodone last in your system?
Studies have shown that the half-life of elimination of hydrocodone is an average of 3.8 hours. This means that your body will take less than 4 hours to excrete 50% of the dose of hydrocodone administered. This means that the body will excrete hydrocodone from its system for 20.9 hours.
However, other findings suggest that there could be a greater difference in the half-life of drugs, which ranges from 3.3 hours to 4.1 hours. This indicates that some patients can eliminate the drug much faster during 18.15 hours, while others may have a prolonged systemic time of elimination with 22.55 hours. In most patients, hydrocodone must be eliminated from the body in 1 day, however, it may not eliminate the active metabolite of hydrocodone, called norhydrocodone, for up to 2 days.
There are many factors that can influence the time that hydrocodone and its active metabolites will remain in your system. These factors can be internal or individual, such as: age, genetics, body mass, liver and kidney function, etc. External factors such as the frequency of hydrocodone use and other medications taken at the same time may also have an influence.
How long does hydrocodone last in your Urine
It depends on the test used. A urine test with 3 drugs usually just checks the presence of marijuana, cocaine and meth. If they check the hydrocodone, it usually leaves your system after 3 days, if you do not take them every day, then they stay for about 2 weeks. The best thing you can do if you are worried about failure is to go to the emergency room and tell them that you have hurt your back and they will either give you a hydrocodone or a slice with enough to last a couple of days, after which you it will be good. Because they are prescribed to you.
How long does hydrocodone last in your blood?
In normal situations, hydrocodone should be detectable in the blood for one day after the last dose is administered.
How long does hydrocodone last in your hair?
Hydrocodone can be detected in hair up to 90 days.
How long does hydrocodone last in your saliva?
In saliva, hydrocodone can be detected up to 1 day after administration, while norhydrocodone can remain detectable for up to 2 days.
How long will Hydrocodone last in your system if you inhale it?
If hydrocodone is inhaled, it will pass into your system more quickly than after ingestion. There is no time to waste in the absorption of the drug. The effects are almost immediate. Depending on the amount of hydrocodone taken, it will remain approximately in the body for 12-24 hours after administration.
How does age affect the elimination of hydrocodone?
The elderly (over 65) compared to younger individuals often metabolize and eliminate medications at much slower rates. Your organs such as the liver or kidneys may have a lower function and / or your internal blood flow is reduced to the liver. In addition, the elderly often take many other medications and some of them may delay the metabolism or excretion of hydrocodone.
How height / weight / body fat affects the elimination of hydrocodone?
The patient’s height, weight, and amount of fat can influence how quickly the body removes the medication from the system. In theory, the taller and heavier patients should eliminate 5 mg of hydrocodone faster compared to the shorter and lighter individuals. This is due to the fact that the lower the dose of the drug given to its height / weight, the faster the elimination, vice versa also applies.
How genetics affects the elimination of hydrocodone?
It is known that different genes influence the metabolism of drugs, including hydrocodone. Genes that regulate hepatic CYP450 enzymes such as CYP2D6 can be very influential if a patient metabolizes hydrocodone at a faster or slower rate than the average. Based on genetics, certain patients are classified as “fast metabolizers”, while others are “slow metabolizers”. This can result in different effects of medications, but also variability in elimination rates.
How does the elimination of hydrocodone affect food?
Foods such as carbohydrates can slow down the absorption of hydrocodone if taken together. However, taking hydrocodone on an empty stomach may increase the absorption of this medication. The differences in absorption time could influence the speed of elimination of the drug from the body. Those who ingest a high-carbohydrate meal along with hydrocodone, the elimination may be delayed.
How does liver or kidney function affect the elimination of hydrocodone?
Since hydrocodone is metabolized in the liver, liver problems and impaired hepatic function can prolong the half-life and prolong the elimination of hydrocodone. For example, someone with cirrhosis or hepatitis may take hours more to metabolize and eliminate hydrocodone from their system compared to healthy people. In addition, kidney failure can also delay the elimination of the medication.
How does urinary pH affect the elimination of hydrocodone?
Patients with more acid urine can eliminate hydrocodone and metabolize it more effectively than those with highly alkaline urine. It is known that the alkalinity of the urine promotes the re-absorption of the drug before its elimination and, therefore, slows down the clearance.
Is hydrocodone water soluble or fat soluble?
ater. Opiates are very soluble in water if they are not in their free form, but hydrocodone is not in its free form, so it is water-soluble.
Acetaminophen (Tylenol), ibuprofen, aspirin are only very slightly soluble in water and are practically insoluble at low temperatures.
Which color of hydrocodone syrup is the strongest?
Yellow (tussionex 10 mg hydrocodone) * Strongest
Red (Hydromet 5 mg hydrocodone)
-Here is the catch, yellow has 10 mg of hydrocodone, but for a long time, so it is released slowly, and it did not hit you quickly.
Red has only 5 mg of hydrocodone, but is instantaneously released, so it has a rapid onset. Although less powerful
Combination of these facts Yellow and red are approximately equal in their effects, and each of them is strong in its own way. So, you get one of these colors that you have, what you do. I tried both and I would go with the yellow one.
– knowing that the yellow color is weaker and the red color is higher due to the unperforated ingredients that the two syrups differ from each other
How does the frequency of Hydrocodone use affect its elimination?
Users of a single dose (patients who use hydrocodone only once) are more likely to eliminate the drug faster from the body than those who use it regularly for a prolonged period. This is likely to be caused by the fact that when hydrocodone is used frequently for several days, hydrocodone and its metabolites will accumulate in the body until the “peak” is reached. Once the “peak” is reached, the cleaning time will be extended.
Single and infrequent users will probably accumulate hydrocodone compared to frequent users. Such patients should be able to excrete the drug efficiently from the body in less than 2 days. However, long-term users who are being treated with chronic hydrocodone may take more than 2 days to completely eliminate hydrocodone.
How other medications affect the elimination of hydrocodone?
Because hydrocodone is metabolized by the cytochrome 450 CYP2D6 isoenzyme, all drugs that affect CYP2D6 can reduce or prolong the half-life of hydrocodone. It is known that drugs classified as CYP2D6 inhibitors affect the body’s ability to eliminate hydrocodone from the body.
The CYP2D6 inhibitors are: SSRI medications (such as paroxetine, citalopram, fluoxetine, etc.), codeine, methadone, amiodarone, serindole, yohimbine, and more. Certain inhibitors of CYP2D6 can slow down metabolism to a greater degree than others and dosing often plays a role. There are also drugs known as “inducers” of CYP2D6, such as dexamethasone and rifampin, which can improve the metabolism of hydrocodone. These medications improve the metabolism of hydrocodone,
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on NewsRecording.
from WordPress https://ift.tt/30aAsVZ
via News Recording
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on NewsPerception.
from WordPress https://ift.tt/2Z4L3CM
via News Perception
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on Midwest.
from WordPress https://ift.tt/2AhIdk9
via Midwest Register
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on News TV Station.
from WordPress https://ift.tt/3hTbR07
via News TV Station
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on LakeviewGazette.
from WordPress https://ift.tt/2ztDnzL
via Lakeview Gazette
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on Mountain Post.
from WordPress https://ift.tt/37BKVxf
via Mountain Post Gazette
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on Daily Post Tribune.
from WordPress https://ift.tt/3047ZCY
via Daily Post Tribune
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on Business Tribune.
from WordPress https://ift.tt/2THfBHi
via Business Tribune
0 notes
Text
How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak
Originally posted on Eleanor Health
As the COVID-19 outbreak continues to put a strain on the nation’s healthcare system at-large, it also puts people with addiction at a greater risk for serious health problems, including withdrawal from alcohol, opioids and other drugs. In light of stay-at-home orders and the need to practice social distancing, some people with addiction may be unable to access substances. Others may think this is a good time to “go cold turkey” and quit their substance use.
In reality, suddenly stopping substance use, either involuntarily or voluntarily, can lead to withdrawal. Depending on the substance and severity of the addiction, withdrawal symptoms can be mild, moderate, severe, or potentially fatal. Withdrawal is especially high-risk for people with pre-existing medical conditions and pregnant women.
With many hospitals’ resources already exhausted, it may be difficult to seek timely medical help for withdrawal, especially if people are hesitant to leave their homes at this time. Here is what you need to know about withdrawal, some ways to manage withdrawal symptoms at-home and when to seek medical help.
Alcohol Withdrawal
In an effort to stop the spread of the novel coronavirus, most states have classified restaurants and bars as non-essential businesses, requiring them to shut their doors to patrons for the foreseeable future. Certain states have even required liquor stores to close. For people with an addiction to alcohol, these circumstances can pose a serious risk and increase their likelihood of withdrawal symptoms occurring.
For people who drink excessively, over time, the brain becomes used to the high level of alcohol being consumed. When the body’s level of alcohol suddenly drops, the brain becomes overstimulated, which causes uncomfortable physical and mental effects of withdrawal. Symptoms can begin within a few hours of a person’s last drink and peak usually peak around 72 hours after the last drink. The symptoms can include:
Trembling (body shakes, often most noticeably in the hands)
Headache
Nausea
Vomiting
Loss of appetite
Chest pain
Fever
Sweating (most noticeably from the palms or face)
Insomnia
Anxiety
The most severe syndrome of alcohol withdrawal is delirium tremens, which develops due to sudden and severe changes in the central nervous system. Often referred to as the DTs, the symptoms usually begin within 48 to 96 hours after the last drink but in some cases, may occur 7 to 10 days following the last time alcohol was consumed. After the initial onset, symptoms may worsen very quickly and can include:
Seizures
Confusion
Vivid hallucinations (seeing, feeling, or hearing things that aren’t there like bugs crawling on the skin)
Rapid mood changes and sudden bursts of energy
Fatigue and sleepiness
Tremors
Delirium tremens is the most severe withdrawal syndrome and could result in serious health problems or death if untreated. If a person develops any symptoms of delirium tremens, they should seek medical attention right away. During this time of the COVID-19 outbreak when it may be difficult to leave the house or see a medical professional in-person, telehealth can be an appropriate way to seek help. Due to the virus outbreak, many telehealth services are waiving co-pays at this time.
Benzodiazepines Withdrawal
Benzodiazepines are a group of medications, which like alcohol, are central nervous system depressants. They are used to treat anxiety, panic disorders, insomnia, and seizures. Often referred to as benzos, some of the most familiar brand names include Valium, Xanax, Ativan, and Klonopin.
This class of medication can be habit-forming, even when prescribed at therapeutic doses. The body can become physically dependent on the medication, in as little as 30 days of use, which is why it is generally only prescribed for short-term use. As soon as physical dependency sets in, withdrawal can occur whenever a person reduces their dose or abruptly stops taking it altogether.
Depending on the specific benzodiazepine, the timeframe for experiencing withdrawal symptoms can begin in as little as 8 hours or as long as a week. With shorter-acting drugs like Xanax and Ativan, symptoms typically begin with 24 hours and peak after 72 hours. For longer-acting drugs like Klonopin and Valium, withdrawal usually begins within 48 hours to one week after the last dose. Because benzodiazepines work in the same part of the brain as alcohol, symptoms of benzo withdrawal are the same as alcohol withdrawal and can include:
Seizures
Muscle spasms and tremors
Dizziness and lightheadedness
Ringing in the ears, blurred vision, and sensitivity to light
Anxiety, panic attacks, and depression
Insomnia
Headache
Like alcohol withdrawal, the most severe form of benzo withdrawal is delirium tremens (see earlier in this article). The dTs are more likely to develop in individuals who have become dependent on shorter-acting benzodiazepines like Xanax and Ativan, but can also develop in those using longer-acting benzos. If a person develops any symptoms of delirium tremens as a result of benzodiazepine withdrawal, they should seek medical attention right away.
Opioid Withdrawal
Opioids are a class of drugs used to treat pain, which can be divided into two categories: opiates and synthetic opioids. Opiates are drugs that originated from the opium poppy plant and include morphine, codeine, heroin, and opium. Synthetic opioids are prescription drugs manufactured in laboratories, like Oxycontin, Vicodin, and Dilaudid, but have similar effects to the drugs naturally derived from opium poppies.
Both categories of opioids can cause physical dependence and addiction. The longer a person takes opioids, the more their body needs to feel the same effects. If opioid usage is stopped suddenly, a person could begin to feel withdrawal symptoms within 24 hours of their last use, including:
Muscle aches
Restlessness
Anxiety, irritability, or agitation
Watery eyes and runny nose
Sweating
Insomnia
As time progresses, symptoms may change and become more intense-feeling after the first day. They include:
Diarrhea and stomach cramping
Nausea and vomiting
Rapid heartbeat and high blood pressure
Blurry vision
Goosebumps on the skin
At-Home Treatment for Withdrawal
To avoid developing severe symptoms of withdrawal, an individual should gradually reduce the amount of the substance used whether that is alcohol, benzodiazepines or opioids. For example, if you typically drink a bottle of vodka daily, rather than stopping cold turkey, you would slowly reduce your drinking over several days — drinking ¾ of a bottle on day 1, half a bottle the second day and ¼ of the bottle on the third day.
While serious withdrawal symptoms require immediate medical attention, many of the milder symptoms can be treated at home with over-the-counter medicines or home remedies.
For nausea and vomiting: antacids (TUMS, Milk of Magnesia, Alka-Seltzer) and bismuth subsalicylate (Pepto-Bismol, Kaopectate)
For diarrhea: bismuth subsalicylate (Pepto-Bismol, Kaopectate) and loperamide (Imodium)
For muscle aches: ibuprofen (Advil) or acetaminophen (Tylenol)
For dehydration: water or Pedialyte/Hydralyte
For high blood pressure and checking vital signs: a blood pressure cuff (can be purchased from a drugstore or online retailer)
Withdrawal can be a stressful situation, made even more overwhelming by the virus outbreak. This may cause certain people to experience significant emotional changes as they go through the withdrawal process, including intense feelings of helplessness and suicidal thoughts.
Receiving emotional support and reassurance during withdrawal can make a world of difference in a person’s outlook. To access help while practicing social-distancing, there are a variety of hotlines and online resources that can help make withdrawal feel less overwhelming, including:
We the Village
Suicide Prevention Lifeline: 1-800-273-8255
Crisis Text Line: 741741
Even with the unusual circumstances caused by the COVID-19 outbreak, it is still possible to seek treatment for addiction. If you or someone you love is going through withdrawal, we’re here to help.
Contact us today to set up a virtual intake and start your #RecoveryForLife.
About Eleanor Health – Durham
Our mission at Eleanor Health is to help people struggling with addiction live amazing lives. As an integrated, multidisciplinary team, we’re focused on delivering whole-person, comprehensive care. We are passionate about transforming the quality, delivery, and accessibility of addiction treatment. Every member of our team works together integrating care and coordinating services to improve our members’ quality of life.
Contact Eleanor Health – Durham
3711 University Drive
Durham
NC 27707
United States
919-752-4028
Website: https://www.eleanorhealth.com/locations/north-carolina/durham
The post How To Help Someone Through Drug or Alcohol Withdrawal During the COVID-19 Outbreak appeared first on AllTheTimeNews.
from WordPress https://ift.tt/2TmdZTa
via All The Time News
0 notes