#zikey
Text

'Just a passing visit. I was in the neighborhood, y'know... I mean, specifically your neighborhood... to see you...'
'So, not really a passing visit? A very specific visit.'
'...yeah'.
~~~
Mikey is a terrible liar.
Just admit you wanted to see her~
I'm trying to write a short story to go with this that'll I'll upload to ao3 to go with this, but it's proving slow going...
#drawings#ocs#tmnt 2016#teenage mutant ninja turtles#oc x canon#michelangelo#zandii#zikey#tmnt 2014#tmnt bayverse#tmnt mikey
286 notes
·
View notes
Text

Parezco una ex novia del Richard Zikey🤨
0 notes
Link
New content! CHAPTER THREE HAS BEEN POSTED!

Chapters: 3/?
Fandom: TMNT - Fandom, Teenage Mutant Ninja Turtles - All Media Types, Teenage Mutant Ninja Turtles (Bay Movies)
Rating: Teen And Up Audiences
Warnings: Graphic Depictions Of Violence
Relationships: Michelangelo (TMNT)/Original Character(s), Michelangelo (TMNT)/Original Female Character(s), michelangelo (tmnt)/zandii, mikey/zandii, zikey
Characters: Michelangelo (TMNT), Zandii - Character
Additional Tags: Human Turtles (TMNT), Human/Turtle Relationships (TMNT), Alternate Universe - Human, Human Michelangelo (TMNT), Human Leonardo (TMNT), Human Raphael, Human Donatello (TMNT), Human Splinter, Good Parent Splinter (TMNT), hamato yoshi - splinter, tagged, wumpusandzandii
5 notes
·
View notes
Text
Nothing makes me happier than Mikey. Everything can be collapsing around me and he’ll still make me feel happy and safe and loved. Nothing has made me feel happier than thinking of him. He’s my sunshine on a rainy day. I love him so much. Asghk
9 notes
·
View notes
Text


i made some smol reesh!!!
5 notes
·
View notes
Text
me crowe and jeffs gc is called ZACOBELL now and guess who has that url saved? me
#im considering password protecting it and using it to post highlights from the char#*chat#before it was called zikey vs zax with paddle and peach emojis
4 notes
·
View notes
Video
Pada dasarnya yang special gak pernah nyakitin itu Martabak Mmmh.....Bener gak ya 🤪🤪🤪 ??? Search aja "Zikei's" di gofood Dan grabfood supaya spesial buat kalian...... #cisauktangerang #cisauk #cisaukiswonderland #cisaukpointapartment #dirumahaja #corona #saiji #pasarmodernintermodabsd #workfromhome https://www.instagram.com/p/B99QjU9JeGA/?igshid=yj14gwmhmy7b
#cisauktangerang#cisauk#cisaukiswonderland#cisaukpointapartment#dirumahaja#corona#saiji#pasarmodernintermodabsd#workfromhome
1 note
·
View note
Text

You, you love it how I move you
You love it how I touch you
My one, when all is said and done
You'll believe God is a woman
Their favourite past time is dancing together and slowly spinning in a world of their own~ ♡
#drawings#tmnt 2016#tmnt#oc x canon#zandii#michelangelo#zikey#teenage mutant ninja turtles#tmnt bayverse#tmnt 2014#tmnt mikey
209 notes
·
View notes
Photo
Pra quem fez na quarta só 3pts, nada mal terminar com 40... Que Zika essas duas últimas rodadas hein! 😤😢 Agradecemos ao André, Jucilei e Diego pela força aqui no meu Esquema! 👏😆
0 notes
Link
Chapters: 2/?
Fandom: TMNT - Fandom, Teenage Mutant Ninja Turtles - All Media Types, Teenage Mutant Ninja Turtles (Bay Movies)
Rating: Teen And Up Audiences
Warnings: Graphic Depictions Of Violence
Relationships: Michelangelo (TMNT)/Original Character(s), Michelangelo (TMNT)/Original Female Character(s), michelangelo (tmnt)/zandii, mikey/zandii, zikey
Characters: Michelangelo (TMNT), Zandii - Character
Additional Tags: Human Turtles (TMNT), Human/Turtle Relationships (TMNT), Alternate Universe - Human, Human Michelangelo (TMNT), Human Leonardo (TMNT), Human Raphael, Human Donatello (TMNT), Human Splinter, Good Parent Splinter (TMNT), hamato yoshi - splinter, tagged, wumpusandzandii
Series: Part 1 of Tagged
Summary:
Graffiti artist and professional dancer Zandii tries to show her appreciation for NY's vigilantes by spreading their family tag, when she can escape her terrible job, that is. Michelangelo happens upon her work in progress, and quickly runs into more trouble than he could imagine.
2 notes
·
View notes
Photo

A wonderful commission I got done by @jessk-art and omg I can’t stop looking at it still <3 <3
Go follow her and commission her, she’s the best! asdfghjkl
#not my art#art for me#commission#zikey#tmnt#tmnt 2016#human!michelangelo#zandii#human!tmnt#jessk-art
60 notes
·
View notes
Video
Zikey Starenhowser https://www.instagram.com/p/B8zSD1jpTrL/?igshid=lwxafwcq34v3
0 notes
Text
Takahiro A. Kato et al., Does the ‘hikikomori’ syndrome of social withdrawal exist outside Japan?: A preliminary international investigation, 47 Soc Psychiatry Psychatr Epidemiol 47 (2012)
Abstract
Purpose
To explore whether the ‘hikikomori’ syndrome (social withdrawal) described in Japan exists in other countries, and if so, how patients with the syndrome are diagnosed and treated.
Methods
Two hikikomori case vignettes were sent to psychiatrists in Australia, Bangladesh, India, Iran, Japan, Korea, Taiwan, Thailand and the USA. Participants rated the syndrome's prevalence in their country, etiology, diagnosis, suicide risk, and treatment.
Results
Out of 247 responses to the questionnaire (123 from Japan and 124 from other countries), 239 were enrolled in the analysis. Respondents’ felt the hikikomori syndrome is seen in all countries examined and especially in urban areas. Biopsychosocial, cultural, and environmental factors were all listed as probable causes of hikikomori, and differences among countries were not significant. Japanese psychiatrists suggested treatment in outpatient wards and some did not think that psychiatric treatment is necessary. Psychiatrists in other countries opted for more active treatment such as hospitalization.
Conclusions
Patients with the hikikomori syndrome are perceived as occurring across a variety of cultures by psychiatrists in multiple countries. Our results provide a rational basis for study of the existence and epidemiology of hikikomori in clinical or community populations in international settings.
Introduction
Culture, society and history strongly influence the form of psychiatric diseases [1-3]. Japan has been experiencing very rapid socioeconomic and cultural changes, impacting the lifestyle, behavior and mentality of all Japanese [4]. It has been suggested that the unique cultural background and recent sociocultural changes in Japan have conspired to create a new syndrome of social withdrawal [5] called ‘hikikomori’’. The hikikomori syndrome has been defined as complete withdrawal from society for 6 months or longer [6,7,5]. In the latest version (October 2010) of the Oxford dictionary an entry on hikikomori has been included: “(in Japan) the abnormal avoidance of social contact, typically by adolescent males/a person who avoids social contact [Origins] Japanese, literally ‘staying indoors, (social) withdrawal’.”
Though hikikomori was first described in Japan, it is unclear whether the phenomenon may exist elsewhere. Experts have debated as to whether hikikomori is a culture-bound syndrome specific to Japan or a syndrome that can be classified using the criteria of the ICD-10 or DSM-IV [8-10]. Furthermore, some have reported hikikomori-like phenomena in countries such as Oman, Spain and Korea [11-13]. However, the only rigorous epidemiological study of hikikomori is from Japan, and it indicated a lifetime prevalence of over 1% among young adults in Japan [14].
Thus, the main purpose of this study was to conduct a preliminary investigation of whether patients with typical hikikomori syndrome as perceived as occurring in Japan and other countries by psychiatrists, and if so how cases are evaluated and treated.
Methods
Participants
The participants of the study were psychiatric residents (trainees) and psychiatrists of varying ages in nine countries. They were asked to consider the two case vignettes and fill in an anonymous questionnaire dealing with the cases, diagnosis and other issues related to their understanding of the syndrome. The survey was conducted in two waves. In the first (May – July 2010), the survey in Japan was conducted by local coordinators who belong to two psychiatric hospitals (Hizen Psychiatric Center in Saga and Zikei Hospital in Okayama) and six university hospitals and their affiliated hospitals throughout Japan (Kyushu University in Fukuoka, University of Occupational and Environmental Health in Kitakyushu, Kyoto prefecture University in Kyoto, Keio University in Tokyo, Teikyo University in Tokyo, and Sapporo Medical University in Sapporo). Each local coordinator was instructed to distribute the survey to a convenience sample of psychiatrists, though we specifically requested recruitment of psychiatrists of differing ages and years of experience. The questionnaire was distributed in-person or via mail.
In the second wave, the survey was translated between Japanese and English using backtranslation. We identified – with the help of the international section of the Japanese Society of Psychiatry and Neurology (JSPN) and the network of Young Psychiatrists Organization in each country – local coordinators in each country who were given instructions identical to those in Japan. Surveys were collected (especially in their own local community), and returned to the principal investigator (T.A.K.) by August 2010.
The questionnaire
We developed two case vignettes of hikikomori in Japan based on a review of the literature and experts’ comments [5,8,9]. Hikikomori experts in Japan suggest a focus on prolonged cases with problematic behaviors [15-17], which we incorporated into the case vignettes. Also, researchers and clinicians have described a number of clinical and historical correlations with hikikomori (e.g., being bullied in school, poor academic performance, and intermittent violent outbursts) that we included [15-17]. A complete mental status examination and follow-up data were not described for cases in order to stimulate the imagination of participants. The second case vignette was adapted from one previously published [8]. The questionnaire was self-administered and participants evaluated the following on a 5-point Likert scales after reading each case vignette: Frequency of the case in one's country, cause, diagnosis, suicide risk assessment, and treatment plan. Demographic information about the participants including their experience and length of training in psychiatry were also noted.
The case vignettes were described as follows:
<Clinical case A>
Case: Mr. A, a 15-year-old junior high school student. (His parents say) He obstinately refuses to see us and never comes out of his own room.
Social history: He is the first son, with a younger brother. He is brought up by his father who is a company employee and his mother who works part-time. His father, a salesman, has been transferred every 2-3 years and moved with his whole family, but when he entered junior high school, his father moved by himself, so he now lives with his mother and a brother 3 years his junior. There was nothing particularly problematic during his development and his school grades were medium, but not bad. He naturally found it hard to make friends and he would prefer reading books rather than sports. Half a year after entering junior high school, he suddenly stopped going to school. At home, he is absorbed in PC games and Internet, he hardly ever leaves his room, and his day and night are reversed.
Past psychiatric history: None
Family history: None
History of Present Illness: After 2 years of his school absenteeism, when his entrance exams for senior high school were near at hand, his father returned home and warned him: “Why don't you go to school once in a while? Can't you be serious about your future?”, to which he yelled: “I don't need you tell me that!” and he suddenly used violence on his father. While his father was dumbfounded, he headed back to his room. A few days later, his parents made up their mind to force him to come with them to the nearby psychiatric faculty where he is examined by you.
Drug history: None
Mental Status Exam on First Interview:
Mr. A, just standing between his parents kept silent, with his head hung down. His parents bowed and described his life history and problematic situations. From beginning to end, he just kept looking downwards. His attitude does not imply any psychotic experience, such as delusion/hallucination. He just seems to be withdrawn into his own shell. Even when you addressed him: “Mr. A”, he did not reply at all.
<Clinical case B>
Case: Mr. B, a 24-year-old male living with his parents. (His parents say) He never comes out of his own room. (Mr. B) just keeps saying “I don't know”.
Social history: He is an only child. He is brought up by his parents in a two-bedroom urban apartment. There was nothing particularly problematic during his development until elementary school. In junior high school, he often skipped school and avoided mingling with peers, which he linked to experiences such as being bullied by classmates in elementary school. His academic performance was historically good, and he directly entered a middle-class university of engineering faculty, but three years ago (third grade, 21 years old) Mr. B dropped out of university for lack of motivation.
Family history: None
History of Present Illness: For the last three years he has hardly ever left his room, spending 23 hours a day behind its closed door. He eats food prepared by his mother who leaves trays outside his bedroom. He sleeps all day, then awakes in the evening to spend his time surfing the Internet, chatting on online bulletin boards, reading manga (comic books), and playing video games. Despite parental encouragement, he has repeatedly resisted going to vocational school or taking a job.
Psychiatric history: Since last year, his parents have taken him to several local hospitals where he was variously diagnosed with ‘depression’ and 'latent schizophrenia’. On mental status exam, he had a flat affect, denied depressed mood or anxiety, and answered most questions by saying ‘I don't know’. Neuro-psychological testing revealed no cognitive abnormalities. Brain imaging and standard screening laboratory studies for altered mental status were unremarkable. He failed trials of psychotropic medications including antidepressants and antipsychotics.
Mental Status Exam on First Interview:
Expecting a possible solution of his social withdrawal, his parents brought him to the psychiatric faculty where he is examined by you. Mr. B, just standing between his parents kept silent politely. His attitude does not imply any psychotic experience, such as delusion/hallucination. He just seems to be a quiet person. Even when you addressed him, he just replied “I don't know”.
Statistical Analysis
Statistical analysis was performed using SPSS 16.0J (SPSS Japan Inc., Tokyo, Japan). Data were expressed with mean and standard deviation (SD). Data from Japan and all other countries were split into two groups and compared by unpaired t-test. In addition, data from Japan, Korea, Australia and Taiwan each met the criteria of n > 18, and thus were analyzed by a one-way analysis of variance (ANOVA) followed by Tukey honestly significant difference (HSD) post hoc test. Significance was set at a level of p < 0.05.
Results
Participants
The Japanese questionnaire was distributed to 165 psychiatrists in Japan and 123 responded (response rate: 74.5%). The English translated questionnaire was distributed to 144 psychiatrists in other countries and 124 responded: 34 from Korea, 22 from Australia, 19 from Taiwan, 10 from each of Bangladesh, Iran, India, and the USA, and 9 from Thailand (response rate: 86.1%). Eight subjects were excluded because of incomplete data, for a final n of 239 participants (male/female/sex-unknown=145/91/3) enrolled in analysis. Details of participants are shown in Table 1.
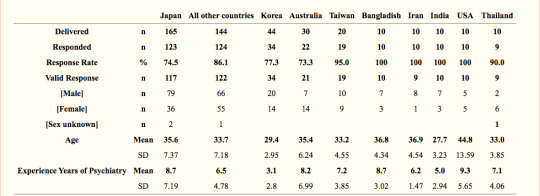
Table 1. Demographics of participants.
Frequency
The participants felt that people with hikikomori syndrome were seen in all countries and that they are more frequently seen in urban areas, especially in Taiwan (Table 2). In the majority of countries, adults with hikikomori syndrome (case B) were less frequently seen than teenagers with the hikikomori syndrome (case A).
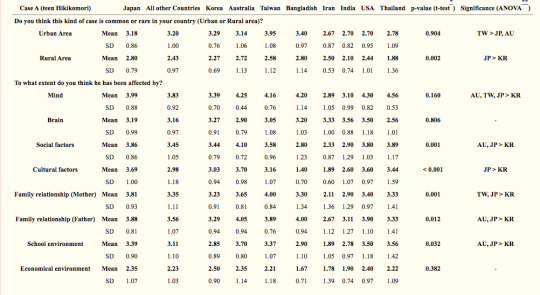


Table 2. Participants’ opinions regarding the prevalence and causes of the hikikomori vignette cases.
Causes
Psychological factors were reported to be extremely common causes of hikikomori in many countries including Japan, especially for teen hikikomori (Table 2). Social and cultural factors were also often noted, except in Bangladesh and Iran. Others pointed to parental influences, especially in relation to teen hikikomori. However, for adult hikikomori, brain (biological) factors were highlighted. Japanese psychiatrists regarded factors of psychosis, mood and personality equally as causes, while other countries’ psychiatrists valued factors of mood and personality to be more significant, especially regarding teen hikikomori. Factors of psychosis were raised in particular for teen hikikomori by psychiatrists in India, Iran, Korea, the USA, and Japan.
Diagnosis
Just 30 % of Japanese psychiatrists reported that both hikikomori cases could be diagnosed using ICD-10/DSV-IV criteria, whereas about 50 % of them did not consider ICD-10/DSV-IV criteria to apply to these cases. On the other hand, psychiatrists in other countries have differing opinions regarding the application of the ICD-10/DSV-IV criteria (Table 3). When participants were asked details for their diagnosis, they offered a variety of diagnoses such as adjustment disorder, anxiety disorder, autism spectrum disorders, conduct disorder, dysthymia, impulse control disorder, prodromal schizophrenia, schizoid personality disorder, simple schizophrenia, and social phobia. Some participants from Japan, Korea, Taiwan, Thailand and the USA diagnosed the cases as hikikomori. In addition, some Korean psychiatrists diagnosed the patients described in the vignettes as having Internet Addiction.
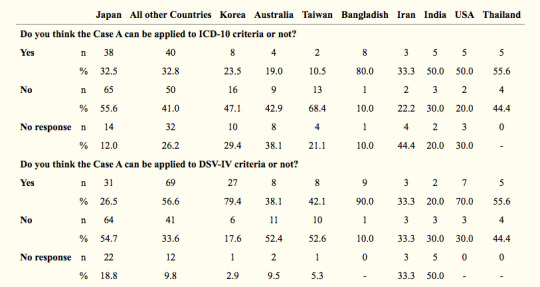
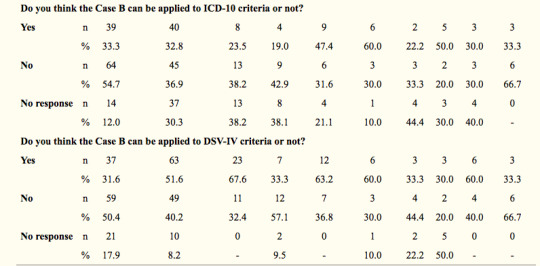
Table 3. Participants’ opinions regarding the diagnosis of the hikikomori vignette cases
Suicide Risk
Korean psychiatrists estimated suicide risk for the both cases to be significantly higher than all other countries (Table 4).
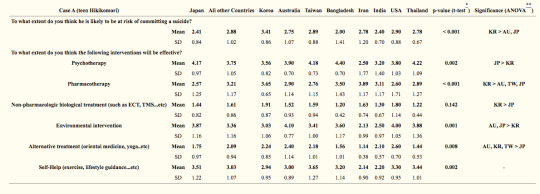
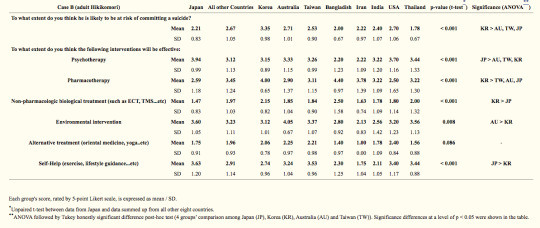
Table 4. Participants’ opinions regarding the suicide risk of the hikikomori vignette cases and the preferable interventions.
Treatment Setting
A large difference in selection of treatment method was found between psychiatrists in Japan and other countries (Figure 1). Japanese psychiatrists suggested treatment in outpatient wards and some even said no psychiatric treatment was necessary. Participants in other countries opted for more active treatments, and some Korean psychiatrists felt that the treatment of choice would be locked ward hospitalization.
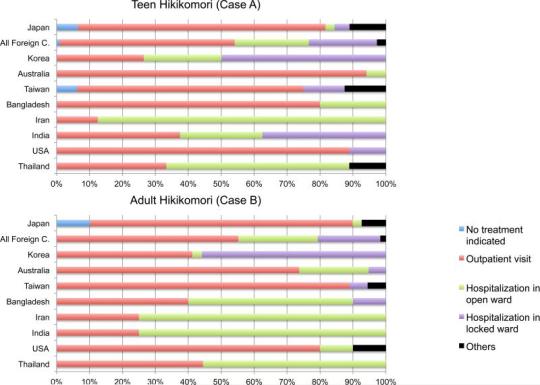
Figure 1. Where should the hikikomori cases be treated?
Participants were asked the following question [Where should the case A/B be treated at this point?]. Their choices were expressed as percentage in each country.
Interventions
Therapeutic interventions that were recommended are shown in Table 4. Overall, there were no significant differences found between treatment recommendations made by Japanese psychiatrists and those from other countries. There were a number of significant differences between specific countries, however. Japanese psychiatrists tended to choose psychotherapy as the most favored approach for the cases, especially for teen hikikomori. Pharmacotherapy was preferred by Bangladeshi, Iranian and Korean psychiatrists. Psychiatrists from all countries, especially Australia and Japan, recommended environmental interventions. Taiwanese psychiatrists choose self-help as the most preferable intervention for adult hikikomori. Alternative treatments such as traditional Chinese medicine and yoga for the teen hikikomori were recommended in many countries except Japan.
Discussion
To our knowledge, this is the first international study to explore the opinions of clinicians about the hikikomori syndrome in Japan and other countries. It revealed that typical hikikomori cases seem to exist not only in Japan but also in other parts of Asia, Australia and the USA.
There was no consensus among the psychiatrists about the causes of the syndrome. Biopsychosocial, cultural, and environmental factors including parental and school factors were all regarded as probable causes of hikikomori. These factors have significant influence on various psychiatric diseases and problematic behaviors such as juvenile delinquency and bullying [18-23]. Since these problematic behaviors found in modern society are also seen as related to hikikomori [15-17], we may have found results suggesting higher prevalence in urban areas.
Surprisingly, some psychiatrists in Japan felt people with the hikikomori syndrome do not need psychiatric treatment. Most psychiatrists from other countries suggested that hospitalization is the preferred treatment. This difference might be related to the fact that hikikomori-like phenomena have been seen in Japan for a long time and have become somewhat acceptable behavior within Japanese society [24,8]. Japanese cultural acceptance of hikikomori may be considered within the concept of ‘amae’ [25]. Takeo Doi, a psychiatrist and psychoanalyst, described Japanese dependent behaviors with the word amae. The person who is acting amae may beg or plead, or alternatively act selfishly and indulgently, while secure in the knowledge that the caregiver will forgive this. The behavior of children towards their parents is the most typical example of amae. Doi argued that child-rearing practices in the Western society seek to stop this kind of dependence in children, whereas in Japan it persists into adulthood in all kinds of social relationships [25]. Even now, compared to Western societies, in Asian societies including Korea, Japan and Taiwan, young people tend to be more economically dependent on their parents, and this phenomenon seems to be one of the expressed form of amae [26]. Hikikomori may be indirectly promoted by amae which makes parents accept their child staying at home. Even though the concept of amae was originally considered to be uniquely Japanese, contemporary opinions suggest that amae is actually more universal in nature [27]. Thus, there is an interesting parallel to hikikomori that has been thought of as unique to Japan but, as our preliminary results show, is perceived by psychiatrists as occurring in a variety of other countries.
Our results extend rather than clarify the debate over diagnosis of hikikomori. In our survey, a variety of diagnoses, such as psychosis, depression anxiety and personality disorders, were proffered. Opinions as to whether hikikomori cases can be diagnosed using ICD-10/DSV-IV criteria differed depending on the participants’ countries and the cases’ age of onset. Similarly, Kondo and his colleagues recently reported that among 29 hikikomori cases who visited one prefectural mental health welfare center in Japan, 24 cases could be diagnosed using the DSM-IV criteria such as schizophrenia (3 cases), Asperger's syndrome (6), personality disorders (4), social phobia (4), and adjustment disorders (2). Based on this survey, Kondo et al. suggested that most hikikomori cases could be diagnosed with the present diagnostic criteria [16]. However, a recent epidemiological survey in Japan reported approximately a fifty-fifty split between hikikomori who had experienced a psychiatric disorder and had not [14]. These data and other studies that have not been able to diagnose all cases of hikikomori may suggest the existence of ‘primary hikikomori’ that is not an expression of any other psychiatric disorder [28,8,9,5,29]. In order to clarify differences between ‘primary hikikomori’ (social withdrawal not associated with any underlying psychiatric disorder) and ‘secondary hikikomori’ (social withdrawal caused by an established psychiatric disorder), further epidemiological and psychopathological studies are needed. Structured diagnostic interviews such as the SCID (Structured Clinical Interview for DSM-IV) should be applied. If some hikikomori cases prove to be not associated with any conventional psychiatric diagnoses, hikikomori should be added to the DSM-5 or the ICD-11. Even if all hikikomori cases prove to be within some kind of psychiatric disorders, it is valuable to continue to focus on the hikikomori phenomenon because of its associated morbidity, similar to how suicidality is examined in various fields of psychiatry [30]. Reducing the burden of hikikomori symptoms, regardless of what psychiatric disorders patients may have, may provide a worthwhile improvement in their quality of life, and this suggests another direction of future hikikomori research.
There are historical examples that may have lessons for the hikikomori debate. First, eating disorders emerged during an era of rapid sociocultural changes in the 1950-1970s [31-33]. Thus, it might be that the hikikomori phenomenon is a particular contemporary expression of psychopathology too.
Second, taijin kyofusho, a Japanese cultural variant of social phobia included in the DSM-IV TR appendix of culture-bound syndromes, is relevant to the hikikomori discussion [34]. Teo and Gaw compared the psychiatric literature's discussion of taijin kyofusho and hikikomori, proposing hikikomori as another type of culture-bound syndrome [8,9] as follows; The two conditions share similar epidemiological factors. Taijin kyofusho is known to be common among the same youthful age group and have the same bias toward males [35]. Nakamura and Shioji reported a case series study of 24 consecutive taijin kyofusho treated on an inpatient unit, and they revealed that 7 (29%) of the patients fit what they regarded to be a “hikikomori subtype” [36]. Taijin kyofusho's core feature is fear of offence or hurting others through awkward social interaction or because of perceived physical defect such as body odor, blushing, and eye-to-eye contact [37], while such features are not obviously expressed by typical cases of hikikomori including our vignette cases. To clarify the similarity and difference between the two conditions, further epidemiological, psychopathological and cultural studies are warranted. Previous study of DSM diagnosis of taijin kyofusho by American mental health practitioners revealed a tendency similar to psychiatrists in our study to apply a range of personality, anxiety, and psychotic diagnostic labels (Tanaka-Matsumi, 1979). Given this diagnostic heterogeneity based on ICD and DSM criteria, there may be utility in creating and using specific diagnostic criteria for the hikikomori syndrome [28,8,9].
Third, there were great debates on Latah paradox in the early 1980's between psychiatrists and medical anthropologists [38,39]. They argued whether Latah is a locally specific phenomenon (a culture-bound syndrome) or a common syndrome that can be classified in a taxonomy. The modern discussion as to whether hikikomori is a culture-bound syndrome or not bears similarity to the argument of the Latah paradox. Further appropriate studies are needed to clarify this issue.
Interestingly, some Korean psychiatrists diagnosed the vignette cases as Internet addiction. Korea is one of the first countries to describe Internet addiction among the young [40-42]. In Korea, Internet addiction is often actively treated [43]. In addition, risk of suicide among younger generations is high in Korea [44]. Limited evidence has supported a connection between Internet usage and suicide [45], and this might have influenced the preference of Korean psychiatrists for very active therapeutic strategies, such as the hospitalization of patients with the hikikomori syndrome in locked wards. On the other hand, Japanese psychiatrists tend to regard the risk of suicide to be low and choose relatively passive interventions for the hikikomori. This is in contrast to the recently reported Internet-related suicide pacts in Japan [45-47]. Ozawa-de Silva pointed out a clear resemblance between hikikomori and Internet suicide pacts as their main communication tool is the Internet, and these individuals have reduced social interaction and social support. Perhaps then Japanese psychiatrists should pay much more attention to hikikomori and associated Internet addiction and suicide.
Our result from Japanese psychiatrists revealed that psychotherapy is regarded to be the most favored approach for the cases especially for teen hikikomori. Various psychotherapeutic approaches such as psychodynamic psychotherapy, group therapy and family therapy have been conducted and reported to be effective by Japanese psychiatrists [15-17]. Also, home visits were reported to be effective intervention for hikikomori cases, especially to reduce violent behaviors [48]. Therapeutic strategies based on Japanese psychiatrists’ experience with hikikomori may be useful to psychiatrists and mental health professionals in other countries.
Limitations
The first limitation of this study is that data are a convenience sample from limited areas in the countries concerned, and therefore may not reflect the opinion of all psychiatrists in these countries. In addition, the different length of psychiatric training in each country and predominance of young psychiatrists may have influenced our results. Our recent international survey focusing on impacts of biopsychosocial factors on psychiatric training revealed that psychiatric diagnosis and treatment strategy is significantly influenced by psychiatric education in each country [49], and this may have also influenced diagnostic and therapeutic decisions in each country. The sample in this study may not be representative of the wide spectrum of psychiatrists’ experience and theoretical orientations since detailed characteristics of the participants were not obtained. Our results should not be interpreted as offering actual epidemiological data on frequency and etiology of hikikomori across cultures. Second, the questionnaire was developed for this study, and its psychometric characteristics have not been established. Third, vignettes inherently offer a limited clinical picture and might not reflect what would happen in real clinical settings. Nonetheless, the utility of clinical vignette surveys in comparing perceptions of diagnoses by clinicians in different countries has been established [50].
Conclusion
Our case vignette survey indicates that the hikikomori syndrome, previously thought to exist only in Japan, is perceived by psychiatrists to exist in many other countries. It is particularly perceived as occurring in urban areas and might be associated with rapid global sociocultural changes. There is no consensus among psychiatrists within or across countries about the causes, diagnosis and therapeutic interventions for hikikomori yet. International collaboration should help to clarify the nature of the syndrome and produce guidelines regarding the diagnosis and treatment of the syndrome. Further epidemiological and psychopathological studies using structured diagnostic interviews and validated psychometric instruments would also be needed to confirm our findings, and to produce information about the public health importance of the hikikomori syndrome.
References
Tseng WS. Handbook of Cultural Psychiatry. Academic Press; San Diego, CA.: 2001.
Wasan AD, Neufeld K, Jayaram G. Practice patterns and treatment choices among psychiatrists in New Delhi, India: a qualitative and quantitative study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(2):109–119.
Alarcon RD. Culture, cultural factors and psychiatric diagnosis: review and projections. World Psychiatry. 2009;8(3):131–139.
Ogata Y, Izumi Y, Kitaike T. Mobile-phone e-mail use, social networks, and loneliness among Japanese high school students (in Japanese). Nippon Koshu Eisei Zasshi. 2006;53(7):480–492.
Saito T. Social Withdrawal (Shakaiteki Hikikomori). PHP Shinsho (in Japanese), Tokyo. 1998
Kaneko S. Japan's 'socially withdrawn youths' and time constraints in Japanese society: Management and conceptualization of time in a support group for 'hikikomori. Time and Society. 2006;15(2-3):233–249.
Watts J. Public health experts concerned about “hikikomori”. Lancet. 2002;359(9312):1131.
Teo AR. A new form of social withdrawal in Japan: a review of hikikomori. Int J Soc Psychiatry. 2010;56(2):178–185.
Teo AR, Gaw AC. Hikikomori, a Japanese culture-bound syndrome of social withdrawal?: A proposal for DSM-5. J Nerv Ment Dis. 2010;198(6):444–449.
Borovoy A. Japan's hidden youths: mainstreaming the emotionally distressed in Japan. Cult Med Psychiatry. 2008;32(4):552–576.Garcia-Campayo J, Alda M, Sobradiel N, Sanz Abos B. [A case report of hikikomori in Spain]. Med Clin (Barc) 2007;129(8):318–319.
Sakamoto N, Martin RG, Kumano H, Kuboki T, Al-Adawi S. Hikikomori, is it a culture-reactive or culture-bound syndrome? Nidotherapy and a clinical vignette from Oman. Int J Psychiatry Med. 2005;35(2):191–198.
Lee KM, Koo JG, Kim EJ, Lee SH. The Psychosocial Characteristics of Oiettolie Adolescents (in Korean). The Korean Journal of Counseling and Psychotherapy. 2001;13(1):147–162.
Koyama A, Miyake Y, Kawakami N, Tsuchiya M, Tachimori H, Takeshima T. Lifetime prevalence, psychiatric comorbidity and demographic correlates of “hikikomori” in a community population in Japan. Psychiatry Res. 2010;176(1):69–74.
Kano R, Kondo N. Seinen no Hikikomori (Adolescent Social Withdrawal)(in Japanese). Iwasaki gakuzyutsu shuppansha, Tokyo. 2000
Kondo N, Iwazaki H, Kobayashi M, Miyazawa H. Psychiatric background of social withdrawal in adolescence (in Japanese). Seishin Shinkeigaku Zasshi. 2007;109(9):834–843
Saito K. Hikikomori No Hyouka-Shien Ni Kansuru Gaido-Rain [Guideline of Hikikomori for their evaluations and supports] Ministry of Health, Labour and Welfare; Tokyo: 2010. (http://www.ncgmkohnodai.go.jp/pdf/jidouseishin/22ncgm_hikikomori.pdf)
Trumpf J, Margraf J, Vriends N, Meyer AH, Becker ES. Specific phobia predicts psychopathology in young women. Soc Psychiatry Psychiatr Epidemiol. 2010;45(12):1161–1166.
Nolfe G, Petrella C, Zontini G, Uttieri S. Association between bullying at work and mental disorders: gender differences in the Italian people. Soc Psychiatry Psychiatr Epidemiol. 2010;45(11):1037–1041.
Canino G, Polanczyk G, Bauermeister JJ, Rohde LA, Frick PJ. Does the prevalence of CD and ODD vary across cultures? Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):695–704.
Eichelsheim VI, Buist KL, Dekovic M, Wissink IB, Frijns T, van Lier PA, Koot HM, Meeus WH. Associations among the parent-adolescent relationship, aggression and delinquency in different ethnic groups: a replication across two Dutch samples. Soc Psychiatry Psychiatr Epidemiol. 2010;45(3):293–300.
Coid J, Yang M. Violence and delayed social independence among young adult British men. Soc Psychiatry Psychiatr Epidemiol. 2010;45(3):301–308.
Rydell AM. Family factors and children's disruptive behaviour: an investigation of links between demographic characteristics, negative life events and symptoms of ODD and ADHD. Soc Psychiatry Psychiatr Epidemiol. 2010;45(2):233–244.
Kitayama O, Saito T, Watanabe T, Muto S. Zadankan Hikikomori Ni Tsuite (Forum Hikikomori)(in Japanese). In: Watanabe T, Muto S, editors. Gendai No Esprit 403-Hikikomori- Shibundo, Tokyo: 2001. pp. 5–34.
Doi T. The Anatomy of Dependence. Kodensha International; Tokyo: 1973.
Kato T. The Significance of Communicating with Neighbors for Young Psychiatrists. World Cultural Psychiatry Research Review. 2008;3(4):219–225. (http://www.wcprr.org/pdf/203-204/2008.2004.219225.pdf)
Niiya Y, Ellsworth PC, Yamaguchi S. Amae in Japan and the United States: an exploration of a “culturally unique” emotion. Emotion. 2006;6(2):279–295.
Malagon A, Alvaro P, Corcoles D, Martin-Lopez LM, Bulbena A. ' hikikomori': a new diagnosis or a syndrome associated with a psychiatric diagnosis? Int J Soc Psychiatry. 2010;56(5):558–559.
Kinugasa T. Young Adults and withdrawal (Yangu Adaruto No Hikikomori) (in Japanese). Rinsho Shinkeigaku. 1998;27:147–152.
Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074.
Hsu LK, Lee S. Is weight phobia always necessary for a diagnosis of anorexia nervosa? Am J Psychiatry. 1993;150(10):1466–1471.
Pavlova B, Uher R, Dragomirecka E, Papezova H. Trends in hospital admissions for eating disorders in a country undergoing a socio-cultural transition, the Czech Republic 1981-2005. Soc Psychiatry Psychiatr Epidemiol. 2010;45(5):541–550.
Miller MN, Pumariega AJ. Culture and eating disorders: a historical and cross-cultural review. Psychiatry. 2001;64(2):93–110.
American-Psychiatric-Association . Diagnostic and Statistical Manual of Mental Disorders (4th ed) American Psychiatric Association; Washington (DC): 2000.
Russell JG. Anxiety disorders in Japan: a review of the Japanese literature on shinkeishitsu and taijinkyofusho. Culture, medicine and psychiatry. 1989;13(4):391–403.
Nakamura K, Shioji R. Taijin kyoufushou to hikikomori (in Japanese). Rinshou Seishin Igaku (Clin Psychiatry) 1997;26:1169–1176.
Kirmayer LJ. The place of culture in psychiatric nosology: Taijin kyofusho and DSM-III-R. The Journal of nervous and mental disease. 1991;179(1):19–28.
Simons RC. The resolution of the Latah paradox. The Journal of nervous and mental disease. 1980;168(4):195–206.
Kenny MG. Paradox lost. The latah problem revisited. The Journal of nervous and mental disease. 1983;171(3):159–167.
Aboujaoude E. Problematic Internet use: an overview. World Psychiatry. 2010;9(2):85–90.
Young K. Internet addiction over the decade: a personal look back. World Psychiatry. 2010;9(2):91.
Ha JH, Yoo HJ, Cho IH, Chin B, Shin D, Kim JH. Psychiatric comorbidity assessed in Korean children and adolescents who screen positive for Internet addiction. J Clin Psychiatry. 2006;67(5):821–826.
Yen CF, Yen JY, Ko CH. Internet addiction: ongoing research in Asia. World Psychiatry. 2010;9(2):97.
Jeon HJ, Lee JY, Lee YM, Hong JP, Won SH, Cho SJ, Kim JY, Chang SM, Lee D, Lee HW, Cho MJ. Lifetime prevalence and correlates of suicidal ideation, plan, and single and multiple attempts in a Korean nationwide study. J Nerv Ment Dis. 2010;198(9):643–646.
Hagihara A, Miyazaki S, Tarumi K. Internet use and suicide among younger age groups between 1989 and 2008 in Japan. Acta Psychiatr Scand. 2010;121(6):485. author reply 485-486.
Naito A. Internet suicide in Japan: implications for child and adolescent mental health. Clin Child Psychol Psychiatry. 2007;12(4):583–597.
Ozawa-de Silva C. Too lonely to die alone: internet suicide pacts and existential suffering in Japan. Cult Med Psychiatry. 2008;32(4):516–551.
Kondo N, Sakai M, Ishikawa S, Niimuras J, Tanoue M. Home visits for social withdrawal cases in community mental health and child welfare services (in Japanese). Seishin Shinkeigaku Zasshi. 2008;110(7):536–545.
Kato TA, Tateno M, Umene-Nakano W, Balhara YP, Teo AR, Fujisawa D, Sasaki R, Ishida T, Kanba S. Impact of biopsychosocial factors on psychiatric training in Japan and overseas: are psychiatrists oriented to mind, brain, or sociocultural issues? Psychiatry Clin Neurosci. 2010;64(5):520–530.
Tanaka-Matsumi J. Taijin Kyofusho: diagnostic and cultural issues in Japanese psychiatry. Cult Med Psychiatry. 1979;3(3):231–245.
0 notes