Text
Understanding Bow Legs and Knock Knees: Causes, Symptoms, and Treatment

Bow legs and knock knees are two common orthopedic conditions that affect the alignment of the legs, often leading to concerns about appearance and potential health issues. While both conditions involve deviations from the normal alignment of the legs, they differ in their presentation and underlying causes. In this article, we'll delve into what bow legs and knock knees are, their causes, symptoms, and available treatments.
What are Bow Legs and Knock Knees?
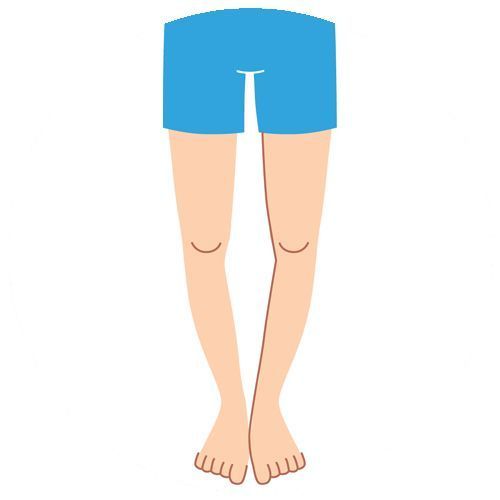
Bow Legs (Genu Varum): Bow legs refer to a condition where the legs curve outward at the knees while the ankles remain together when a person stands with their feet together. This creates a distinct gap between the knees even when the ankles touch.
Knock Knees (Genu Valgum): Knock knees, on the other hand, involve a condition where the knees angle inward and touch each other when a person stands with their feet together. This results in a wider-than-normal gap between the ankles.
Causes of Bow Legs and Knock Knees:
1. Developmental Factors: Both bow legs and knock knees can develop during childhood as part of a normal growth process. In infants, bow legs are often a natural result of being cramped in the womb, and they typically straighten out as the child begins to walk. Similarly, knock knees are common during the toddler years as children develop their walking skills, with the condition usually resolving by around age seven.
2. Rickets: Rickets is a condition caused by a deficiency in vitamin D, calcium, or phosphate, which can lead to soft and weak bones. In severe cases, rickets can cause bow legs as the weakened bones are unable to support the weight of the body properly.
3. Blount's Disease: Blount's disease is a growth disorder that affects the tibia, the larger of the two bones in the lower leg. It can cause the inner part of the tibia to stop growing, leading to bow legs, especially if left untreated.
4. Osteomalacia: Similar to rickets, osteomalacia is a condition characterized by softening of the bones, usually due to a deficiency in vitamin D. Bow legs can develop as a result of the weakened bones.
5. Genetic Factors: In some cases, bow legs and knock knees may be inherited, with certain genetic factors predisposing individuals to these conditions.
Symptoms of Bow Legs and Knock Knees:
1. Visible Leg Deformity: The most obvious symptom of bow legs and knock knees is the visible deviation from the normal alignment of the legs when standing.
2. Knee Pain: In some cases, individuals with bow legs or knock knees may experience pain around the knees, particularly during physical activities or prolonged standing.
3. Difficulty Walking: Severe cases of bow legs or knock knees can interfere with normal walking patterns, leading to difficulties in mobility.
4. Joint Stiffness: Bow legs and knock knees can sometimes be accompanied by joint stiffness, making it uncomfortable to move the legs freely.
Treatment Options for Bow Legs and Knock Knees:
1. Observation: In many cases, especially in young children, bow legs and knock knees may resolve on their own as the child grows and develops. Observation by a healthcare professional is often recommended to monitor the condition's progress.
2. Orthotic Devices: For individuals with mild to moderate bow legs or knock knees, orthotic devices such as shoe inserts or braces may help improve alignment and alleviate symptoms.
3. Physical Therapy: Physical therapy exercises focused on strengthening the muscles around the knees and improving overall leg alignment can be beneficial for individuals with bow legs or knock knees.
4. Surgery: In severe cases or when other treatment options have been ineffective, surgery may be recommended to correct the alignment of the legs. Surgical procedures for bow legs and knock knees typically involve adjusting the positioning of the bones to achieve a more normal alignment.
5. Management of Underlying Conditions: If bow legs or knock knees are caused by underlying conditions such as rickets or osteomalacia, treatment of the underlying condition is essential for addressing the leg deformity.
Conclusion:
Bow legs and knock knees are common orthopedic conditions that can affect individuals of all ages, from infants to adults. While they may be a natural part of growth and development in some cases, they can also be caused by underlying medical conditions or genetic factors. Early diagnosis and appropriate treatment are important for managing these conditions and preventing potential complications. By understanding the causes, symptoms, and treatment options for bow legs and knock knees, individuals can take proactive steps to address these issues and maintain optimal leg health. If you or someone you know is concerned about bow legs or knock knees, consulting with a healthcare professional is the first step toward finding the most suitable treatment approach.
0 notes
Text
Understanding Slipped Capital Femoral Epiphysis (SCFE): Causes, Symptoms, and Treatment

Introduction:
Slipped Capital Femoral Epiphysis (SCFE) is a relatively rare but potentially serious hip disorder that mainly affects adolescents during their growth spurts. This condition occurs when the ball at the top of the thigh bone (femur) slips off the neck of the bone at the hip joint. Understanding SCFE is crucial for early detection and treatment to prevent long-term complications. In this article, we delve into the causes, symptoms, diagnosis, and treatment options for SCFE.
What Causes SCFE?
The exact cause of SCFE is not fully understood, but it is believed to be related to a combination of factors, including:
Growth spurts: SCFE often occurs during periods of rapid growth, typically in pre-adolescents and adolescents. The growth plate at the top of the femur is weaker during these growth spurts, making it more susceptible to slipping.
Obesity: Excess weight puts added pressure on the growth plate, increasing the risk of it slipping. Obese children are more likely to develop SCFE compared to those of normal weight.
Hormonal changes: Hormonal changes during puberty may also contribute to the weakening of the growth plate, making it more prone to slipping.
Genetics: There may be a genetic predisposition to SCFE, as it tends to run in families.
Symptoms of SCFE:
SCFE can present with various symptoms, which may include:
Hip or knee pain: Persistent pain in the hip, groin, thigh, or knee, particularly during physical activity, is a common symptom of SCFE.
Limping: A noticeable limp or inability to bear weight on the affected leg may occur due to pain and instability in the hip joint.
Limited range of motion: Reduced flexibility and range of motion in the hip joint may be observed, making it difficult to perform certain movements.
Outward rotation of the leg: The affected leg may appear to turn outward due to the displacement of the femoral head.
Diagnosis of SCFE:
Diagnosing SCFE typically involves a combination of medical history review, physical examination, and imaging tests. The healthcare provider will inquire about the child's symptoms and perform a physical examination to assess the range of motion and stability of the hip joint.
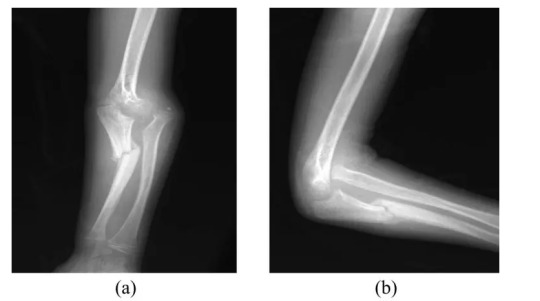
Imaging tests are essential for confirming the diagnosis and determining the severity of the condition. X-rays are commonly used to visualize the position of the femoral head relative to the femoral neck. In SCFE, characteristic findings on x-rays include a slippage of the femoral head in relation to the neck, often described as a "ice cream slipping off a cone" appearance.
In some cases, additional imaging studies such as MRI or CT scans may be ordered to obtain more detailed images of the hip joint and surrounding structures.
Treatment Options for SCFE:
The primary goals of treatment for SCFE are to stabilize the hip joint, relieve symptoms, and prevent further slippage. The treatment approach may vary depending on the severity of the condition and the child's age and overall health. Common treatment options include:
Surgical intervention: In most cases of SCFE, surgery is necessary to stabilize the hip joint and prevent further slippage. The two main surgical procedures used to treat SCFE are:
a. In Situ Fixation: This involves inserting screws or pins into the femoral head and neck to hold them in place and prevent further slippage.
b. Realignment Osteotomy: In severe cases or when the slip is chronic, a realignment osteotomy may be performed to reposition the femoral head and neck into the correct alignment.
Non-surgical management: In some mild cases of SCFE, non-surgical measures such as rest, activity modification, and physical therapy may be recommended to alleviate symptoms and prevent worsening of the condition. However, close monitoring is essential to detect any progression of the slip.
Post-operative Care and Rehabilitation:
Following surgery, a period of immobilization and restricted weight-bearing may be necessary to allow the hip joint to heal properly. Physical therapy is an integral part of rehabilitation to improve strength, flexibility, and mobility of the hip joint. The rehabilitation process is tailored to each individual's needs and may continue for several months to achieve optimal recovery.
Long-term Outlook:
With prompt diagnosis and appropriate treatment, most children with SCFE can expect favorable outcomes and return to normal activities. However, untreated or poorly managed SCFE can lead to serious complications such as hip joint deformity, osteoarthritis, and chronic pain later in life. Regular follow-up appointments and monitoring are essential to detect any signs of recurrence or complications early on.
Conclusion:
Slipped Capital Femoral Epiphysis (SCFE) is a potentially debilitating hip disorder that primarily affects adolescents during their growth spurts. Early recognition of symptoms and timely intervention are crucial for preventing long-term complications and ensuring optimal outcomes. By understanding the causes, symptoms, and treatment options for SCFE, healthcare providers, parents, and caregivers can work together to provide the best possible care for children affected by this condition.
0 notes
Text
Orthopedic Screening of Newborns: Early Detection for Lifelong Health

Orthopedic screening of newborns plays a crucial role in identifying congenital musculoskeletal abnormalities early on, allowing for timely intervention and treatment. These screenings are vital for ensuring the proper development and function of a child's bones, muscles, and joints throughout their life.
During the initial examination shortly after birth, healthcare providers conduct a thorough assessment of the newborn's musculoskeletal system. This assessment includes a visual inspection and palpation of the baby's limbs, spine, and joints to detect any abnormalities or asymmetries. Additionally, specific orthopedic maneuvers may be performed to assess for conditions such as hip dysplasia or clubfoot.
One of the most common conditions screened for in newborns is developmental dysplasia of the hip (DDH). DDH occurs when the hip joint fails to develop properly, potentially leading to long-term issues with mobility and function if left untreated. Early detection through orthopedic screening allows for non-invasive interventions such as harnesses or braces to properly align the hip joint and promote normal development.
Another condition that may be identified during newborn orthopedic screening is clubfoot, a congenital deformity characterized by inwardly twisted or rotated feet. Prompt intervention with techniques such as the Ponseti method, involving gentle manipulation and casting of the foot, can effectively correct clubfoot and prevent future complications.
In addition to these specific conditions, orthopedic screening also helps identify general musculoskeletal abnormalities such as limb length discrepancies, joint contractures, or spinal deformities. Early detection of these issues allows for appropriate referrals to pediatric orthopedic specialists for further evaluation and management.
The benefits of orthopedic screening extend beyond infancy, as timely intervention can prevent long-term disability and improve overall quality of life for affected children. By addressing musculoskeletal abnormalities early on, healthcare providers can minimize the need for extensive treatments or surgeries later in life.
Furthermore, orthopedic screening serves as an essential component of comprehensive newborn care, ensuring that all aspects of a child's health are thoroughly evaluated from the very beginning. Early identification of musculoskeletal issues enables healthcare providers to collaborate with families to develop personalized treatment plans and provide ongoing support throughout the child's development.
It's important to note that while orthopedic screening is a routine part of newborn care in many healthcare settings, not all infants will require intervention. However, for those who do, early detection and appropriate management can make a significant difference in their long-term outcomes.
In conclusion, orthopedic screening of newborns plays a critical role in identifying and addressing musculoskeletal abnormalities early in life. By detecting conditions such as DDH, clubfoot, and spinal deformities at birth, healthcare providers can initiate timely interventions that promote optimal development and function. Through comprehensive newborn care that includes orthopedic screening, we can ensure the lifelong health and well-being of every child.
0 notes
Text
Understanding Various Aspects of Bow Legs Treatment
Each infant is born bowlegged as he remained in mother’s womb in a folded position. Hence, bow legs are considered normal in children whose age is less than 18 months. As the child starts walking, his legs get straightened gradually. But bow legs are considered as a physical deformity if it is present when the child is about 3 years old. As a form of physical deformity, bow legs or genu varum is marked by bowing of the child’s lower leg in relation to his thigh.
Bow legs may be caused due to a variety of illnesses. Normally, the physical deformity is caused due to abnormal development of bones or fractures that have not healed properly. However, bow legs are also caused due to Blount’s disease, or lead or fluoride poisoning. Sometimes the physical deformity is caused due to rickets, an illness caused due to lack of Vitamin D.
The parents can identify the physical deformity based on a number of symptoms. They can know if the child is bowlegged when his knees to not touch while standing with both feet together. Also, a bowlegged child can bow his symmetrically on both sides of his body. The parents must avail the assistance of a seasoned orthopaedic immediately if bow legs continue in a child whose age is more than 3 years.
A seasoned child orthopaedic can diagnose bow legs simply by observing the child’s knees. Some healthcare providers even diagnose bow legs by measuring the distance between two knees of the child when he lies on the back. However, the orthopaedic also perform blood test to check if the deformity is caused due to rickets. They even recommend x-rays when the bowing is extreme or based on the test results. But x-ray is recommended only if the child is older than 3 years.
The seasoned orthopaedics monitors the growth of the bow legged child constantly, and observe his knees once in 6 months. Also, they recommend treatment for bowleg only when the child’s condition is extreme. Many orthopaedics treat bow legs through special braces, casts, or shoes. The skilled orthopaedics also corrects the deformity in an adolescent child by performing bow legs surgery. However, the bow legs treatment varies based on the specific condition of each child.
The parents do not have any option to prevent bow legs. Hence, they must avail the assistance of a skilled orthopaedic to monitor the child’s condition and prevent his condition from becoming extreme. The orthopaedic will further recommend the best way to treat bow legs on time and avoid chances of developing arthritis in the knees or hips. Also, the parents must choose a skilled and experienced orthopedic to avail modern treatment, and correct the physical deformity with minimal scar and morbidity.
0 notes
Text
What is the most common surgery for an orthopedic surgeon?
Pediatric orthopedics is a specialized branch of orthopedic medicine that focuses on the diagnosis and treatment of musculoskeletal conditions in children, from infancy through adolescence. Pediatric orthopedic surgeons are medical doctors who have completed additional training in orthopedic surgery with a specific focus on children.
Children’s bones, muscles, and joints are still growing and developing, which can lead to unique orthopedic conditions and challenges. Pediatric orthopedic surgeons are experts in managing these conditions and providing appropriate treatment options for children.

Some common conditions that pediatric orthopedic surgeons treat include:
Congenital anomalies: These are conditions that children are born with, such as clubfoot, hip dysplasia, limb length discrepancies, and scoliosis.
Fractures and trauma: Children are prone to fractures due to their active lifestyles. Pediatric orthopedic surgeons are skilled in treating fractures and ensuring proper healing.
Sports injuries: Children and adolescents who participate in sports are susceptible to sports-related injuries, including sprains, strains, fractures, and ligament tears. Pediatric orthopedic surgeons can diagnose and treat these injuries, often with a focus on preserving future joint function.
Musculoskeletal infections: Children may develop infections in their bones or joints, such as osteomyelitis or septic arthritis. Pediatric orthopedic surgeons work closely with infectious disease specialists to provide appropriate treatment.
Neuromuscular conditions: Certain neurological conditions, such as cerebral palsy or spina bifida, can affect a child’s musculoskeletal system. Pediatric orthopedic surgeons collaborate with other specialists to develop comprehensive treatment plans for these patients.
Growth-related conditions: Children may experience conditions related to abnormal growth, such as limb length discrepancies or angular deformities. Pediatric orthopedic surgeons can assess and manage these conditions through various treatment options, including surgery, bracing, or physical therapy.

Pediatric orthopedic surgeons often work in collaboration with other healthcare professionals, including pediatricians, physical therapists, occupational therapists, and rehabilitation specialists, to provide comprehensive care for children with orthopedic conditions.
0 notes
Text
What are overuse injuries in the pediatric population?
Overuse injuries in pediatrics refer to a category of injuries that occur when a child or adolescent repeatedly engages in a specific physical activity or sport, placing excessive stress on a particular part of their body. These injuries are common among young athletes who train intensively or participate in a single sport year-round. Overuse injuries can lead to pain, impaired performance, and potentially long-term musculoskeletal issues. Here are some key points to understand about overuse injuries in pediatrics:

Types of Overuse Injuries:Overuse injuries can affect various parts of the body, including:
Growth Plate Injuries: The growth plates, areas of developing tissue near the ends of bones, are vulnerable to overuse injuries.
Stress Fractures: These are small cracks or fractures in bones due to repetitive impact.
Tendonitis: Inflammation of tendons caused by repetitive movements.
Muscle Strains: Overuse can lead to strains or tears in muscles.
Apophysitis: Inflammation of the bony attachment points of muscles, commonly seen in areas like the heel (Sever’s disease) or knee (Osgood-Schlatter disease).
Risk Factors:Several factors increase the risk of overuse injuries in pediatric athletes, including:
Specialization: Young athletes who specialize in a single sport and train intensively year-round are more susceptible to overuse injuries.
Growth and Development: Rapid growth during puberty can change the biomechanics of a child’s body, making them more prone to injury.
Inadequate Rest: Lack of adequate rest and recovery between activities or seasons can contribute to overuse injuries.
Symptoms:The symptoms of overuse injuries may include pain, swelling, tenderness, reduced range of motion, and a decline in athletic performance. Children may also experience pain that worsens with activity and improves with rest.
Prevention and Management:Preventing overuse injuries in pediatrics involves a combination of strategies:
Monitoring Load: Coaches, parents, and athletes should be vigilant about monitoring training loads to ensure they are appropriate for the child’s age and development.
Periodization: Training should incorporate periods of rest, cross-training, and reduced intensity to allow the body to recover.
Proper Technique: Teaching young athletes correct techniques and movement patterns can help reduce the risk of overuse injuries.
Adequate Rest: Children should have scheduled rest days and avoid year-round intensive training in a single sport.
Early Intervention: If an overuse injury occurs, early intervention, including rest, physical therapy, and sometimes bracing, is essential to prevent long-term consequences.
Importance of Multisport Participation:Encouraging children to participate in multiple sports or activities can reduce the risk of overuse injuries by promoting a more balanced use of their bodies and reducing the strain on specific muscle groups and joints.
In conclusion, overuse injuries in pediatrics are a significant concern, especially among young athletes. Preventing these injuries involves a combination of strategies, with a focus on proper training, rest, and early intervention to protect the growing bodies of children and adolescents.
#paediatric orthopaedics kolkata#paediatric orthopaedics india#flat feet correction#diagnose cerebral palsy#club foot treatment
0 notes
Text
Identifying and Treating Neglected Fracture in Kids
According to the Canadian Paediatric Society, “Fractures are common injuries in childhood. While most fractures are caused by accidental trauma, inflicted trauma (maltreatment) is a serious and potentially unrecognized cause of fractures, particularly in infants and young children.”
Fractures in children occur when excessive force is applied to the bone. As the bone cannot absorb excessive force, broken bones or fractures occur. Excessive force can cause multiple fractures or specific fractures like wrist fracture, elbow fracture, or femur fracture.
Also, fractures in kids occur due to a variety of reasons – trauma, falls, direct hit, injuries, and lack of calcium. You cannot control or change the causes and number of fractures in your child. But you must treat the neglected factors early and properly to keep your child fit by eliminating the chances of functional disability and permanent deformity.
What Should You Know to Treat a Neglected Fracture in Your Child Successfully?
Symptoms
A neglected fracture might occur in your child due to a variety of reasons. Also, the symptoms of neglected broken bones vary from one child to another. You can identify neglected fractures based on common systems like pain, swelling, bruising, redness, and warmth. Also, the affected area sometimes appears deformed due to the broken bone. It is always important to consult a pediatric orthopedic surgeon once your child finds it difficult to use or move the injured bone normally and naturally.
Diagnosis
Experienced pediatric orthopedic surgeons diagnose neglected fractures in a variety of ways. They always start diagnosing by inspecting the affected area closely and physically. The physical inspection, along with the child’s medical history, helps experienced orthopedic surgeons to identify the condition and causes of the fracture. However, it is also common for orthopedic surgeons to identify the cause of broken bones by recommending X-rays, CT scans, MRI scans, and similar imaging examinations.
Treatment Options
The orthopedic surgeons diagnose neglected fractures in a variety of ways according to the severity and symptoms of the broken bone. Also, they prepare a personalized treatment plan for the neglected fracture based on your child’s age, medical history, and severity of the fracture. Also, they keep in mind your child’s capacity to tolerate specific medication or treatment options.

Experienced pediatric orthopedic surgeons always start treating neglected fractures through non-surgical procedures like medication, cast/splint, and traction. But they treat neglected fractures surgically when the non-medical procedures do not work. They perform surgeries to reposition the broken bones or implant fixation devices.
Recovery
The non-medical procedures treat neglected fractures gradually over a period of time. Your child will become fit and active after taking medication or wearing the cast/splint regularly for a specific duration. However, you must get the affected area inspected by the orthopedic surgeon regularly according to the treatment plan. On the other hand, your child needs to rest the affected bone completely and follow operation-care recommended by the surgeon when the neglected fracture is treated surgically.
You can easily get a neglected fracture in your child diagnosed accurately and treated effectively by consulting an experienced pediatric orthopedic surgeon. The orthopedic surgeons will help you to eliminate the risk of functional disability and permanent deformity by treating neglected fractures accurately and successfully.
#paediatric orthopaedics kolkata#cerebral palsy#paediatric orthopaedics india#diagnose cerebral palsy#flat feet correction
0 notes
Text
Recognizing Signs of Cerebral Palsy in a Child
As a permanent and complex disorder, cerebral palsy is caused due to damage caused to the brain of a child. The brain damage can occur due to a number of reasons. Also, the damage may be caused to the child’s brain before, during or after his birth. At present, there is no permanent cure for cerebral palsy. The seasoned orthopedics tries to reduce the symptoms and effects of the permanent disorder through medication, orthotic devices, speech therapy, physical therapy or occupational therapy.

Simple Ways to Care for a Child with Cerebral Palsy
It is always important for parents to get their kids diagnosed and treated for cerebral palsy immediately. Also, they must understand various aspects of cerebral palsy management to make the child feel comfortable. But cerebral palsy is often diagnosed only after 18 months of the child’s birth. There are many instances when parents failed to diagnose symptoms of mild cerebral palsy when the kid is 3 to 5 years old. That is why; it become essential for parents to know how to recognize the signs of cerebral palsy in a kid.
To identify the developmental disabilities, the parent must understand know four distinct categories of developmental progress of a child. Broadly, the developmental progress of a child of a child can be divided into four categories – physical, social, cognitive and emotional. Also, the parent must know the normal stages of development to identify the developmental issues immediately. However, the parents must get the child diagnosed for cerebral palsy when they notice lack of physical development.
The parents must get the child diagnosed for cerebral palsy when the child does not meet common developmental milestones like crawling, sitting, walking, rolling over, visual alertness, and picking of small objects. The orthopedic will observe the development of the child over a specific period of time and screen the child regularly to identify improvement disabilities. He will further observe and assess the development of the child based on his posture, muscle tones and reflexes. However, the severity and symptoms of cerebral palsy differ from one child to another.
The child with cerebral palsy further experiences symptoms of the disorder according to the location of movement problems. The symptoms further get aggravated if the child is not provided with adequate care and effective treatment on time. Hence, it is important for parents to get the child diagnosed for cerebral palsy immediately and promptly. At the same time, they also need to ensure that the child is diagnosed and treated by a skilled and experienced orthopedic to manage and reduce symptoms of the complex disorder over a longer period of time.
Know more about stay social with us on: Facebook .
0 notes
Text
What causes joint infection in newborn?
Infections in newborn babies are a serious concern and can potentially affect any part of the body, including joints. Joint infections in newborns are generally referred to as septic arthritis or infectious arthritis. This condition occurs when bacteria or other infectious agents enter a joint and cause inflammation.

Common causes of joint infections in newborns include bacteria such as Staphylococcus and Streptococcus. These infections can occur due to various reasons:
Bacterial Spread: Bacteria can enter the baby’s body through various routes, such as during delivery if the mother has a bacterial infection, or through the baby’s skin if hygiene isn’t maintained.
Hospital Environments: Newborns in hospitals are particularly vulnerable to infections due to their weak immune systems and exposure to various potential sources of infection.
Compromised Immune System: Premature babies or babies with other medical conditions that weaken their immune systems are at a higher risk.
Invasive Procedures: Invasive procedures or interventions, such as the insertion of catheters or IV lines, can introduce bacteria into the baby’s body.
The signs and symptoms of joint infections in newborns can include:
Swelling and Redness: The infected joint may appear swollen, red, and warm to the touch.
Pain and Discomfort: The baby might show signs of discomfort, irritability, and difficulty moving the affected limb.
Fever: A fever is a common sign of infection in babies. It might be accompanied by other signs of illness.
Limited Movement: The baby might avoid moving the affected joint due to pain.
Lethargy: The baby may be unusually tired or inactive.
If you suspect that a newborn might have a joint infection, it’s crucial to seek immediate medical attention. A healthcare provider will likely perform various tests, such as blood tests and imaging (like ultrasound or MRI), to confirm the diagnosis and determine the appropriate treatment. Treatment usually involves antibiotics to target the specific bacteria causing the infection. In severe cases, drainage of the infected joint might be necessary.
Prevention is essential to avoid such infections. Maintaining proper hygiene during childbirth, regular handwashing before handling the baby, and following hospital protocols for infection control can help minimize the risk of infections in newborns.
Keep in mind that medical practices and recommendations may have evolved since my last update in September 2021. Always consult a qualified healthcare professional or pediatrician for the most current and accurate information regarding newborn health and infections.
See More Visit at: https://www.kidsorthopedic.com/contact/
Know more about our affordable and quality products stay social with us on: Facebook .
0 notes
Text
Orthopedic Screening of New Born by Dr Soumya Paik
Orthopedic screening of a newborn baby is an essential part of the overall neonatal assessment to ensure proper musculoskeletal development and detect any congenital or developmental abnormalities early on. Here are some key aspects to consider during orthopedic screening:

Physical Examination: A thorough physical examination of the baby’s musculoskeletal system is conducted by a healthcare provider. This examination typically involves observing the baby’s posture, movement, and overall alignment of limbs and joints.
Hip Dysplasia: Hip dysplasia is a common condition where the hip joint doesn’t develop properly. The Ortolani and Barlow tests are commonly used to screen for hip dysplasia. These tests involve gentle manipulation of the hips to check for stability and proper hip joint formation.
Clubfoot: Clubfoot is a congenital condition where the foot is twisted out of its normal position. The healthcare provider will examine the baby’s feet to check for any abnormal positioning or rigidity.
Spinal Alignment: The baby’s spine is examined to ensure proper alignment. Any signs of spinal curvature or abnormalities should be noted.
Limbs and Joints: The healthcare provider will check the baby’s limbs and joints for any signs of deformities, contractures, or limited range of motion. Conditions like congenital limb anomalies or joint contractures may be identified during this examination.
Polydactyly and Syndactyly: These conditions involve extra fingers (polydactyly) or fused fingers (syndactyly). The baby’s hands and fingers are carefully examined for any such abnormalities.
Neuromuscular Function: The healthcare provider may assess the baby’s neuromuscular function by observing their muscle tone, reflexes, and responsiveness to stimuli.
Referral for Further Evaluation: If any abnormalities are suspected or identified during the screening, the baby may be referred to a pediatric orthopedic specialist for further evaluation and management.
It’s important to note that orthopedic screening of a newborn is usually performed by trained healthcare professionals, such as pediatricians or neonatologists. Regular follow-up appointments and assessments may be recommended to monitor the baby’s musculoskeletal development as they grow.
Remember that every baby is unique, and minor variations in musculoskeletal development can be normal. However, early detection and intervention for any significant abnormalities can help ensure the best possible outcomes for the baby’s long-term musculoskeletal health.
0 notes
Text
What are the safety measures to prevent sports injuries for your kids?
When it comes to preventing sports injuries in children, several safety measures can be implemented. Here are some key recommendations:

Proper warm-up and stretching: Encourage your kids to warm up their bodies before any physical activity. This can include light aerobic exercises and dynamic stretches to increase blood flow and flexibility, reducing the risk of muscle strains or sprains.
Use appropriate equipment: Ensure that your children are equipped with the proper gear for their chosen sport. This may include helmets, mouthguards, shin guards, padding, and supportive footwear. Make sure the equipment fits properly and is in good condition.
Supervision and coaching: Ensure that your children participate in sports under the supervision of trained coaches or instructors who prioritize safety. Qualified coaches can teach proper techniques, enforce rules, and provide guidance on injury prevention.
Conditioning and fitness: Encourage your children to maintain overall fitness and conditioning levels appropriate for their sport. Regular exercise and conditioning activities can help improve strength, flexibility, and coordination, reducing the risk of injuries.
Age-appropriate activities: Ensure that the sports and activities your children engage in are appropriate for their age and skill level. Pushing children to participate in activities beyond their capabilities can increase the risk of injuries.
Rest and recovery: Encourage your children to take regular breaks during practice sessions and games. Rest and recovery are crucial to prevent overuse injuries. It’s important to balance physical activity with proper rest periods.
Hydration and nutrition: Teach your children the importance of staying hydrated before, during, and after physical activity. Provide them with healthy snacks and meals to fuel their bodies and aid in muscle recovery.
Encourage open communication: Teach your children to communicate openly with coaches and teammates about any pain, discomfort, or concerns they may have. It’s crucial to address potential issues early on to prevent further injuries.
Avoid specialization and overtraining: Encourage your children to participate in a variety of sports and activities rather than specializing in one sport too early. Overtraining and repetitive movements can increase the risk of overuse injuries and burnout.
Educate about safety guidelines: Teach your children the importance of following the rules and safety guidelines of their chosen sport. Emphasize good sportsmanship, fair play, and respect for teammates and opponents.
Remember, while these safety measures can help reduce the risk of injuries, accidents can still occur. If your child sustains an injury, seek appropriate Paediatric Orthopaedic Doctor attention and follow the recommended treatment and rehabilitation process.
0 notes
Text
Identifying and Treating Pediatric Trigger Thumb Accurately
A trigger finger is one of the painful health conditions that make your child’s thumb locked in a bent or flexed position. The child cannot pull the bent thumb straight without using her other hand. Often children experience trigger fingers or trigger thumb between the ages of 1 year to three years. A child can experience trigger thumb despite having no medical problem or sustaining any injury.
According to Children’s National, “Trigger thumb is caused by a mismatch between the size of the flexor tendon to the thumb and the tendon sheath (the fibrous band over the tendon) causing difficulties with the gliding motion of the thumb. When the sheath is too tight, the enlarged tendon can lock in one position. This can cause clicking, popping with motion, or a fixed flexed position of the thumb.”
Often adults experience trigger fingers due to injury, trauma, or overuse. But children do not experience this health problem due to any of these reasons. Often orthopedic surgeons find it challenging to identify the causes of pediatric trigger thumb accurately. But they diagnose and treat this health condition in a variety of ways. That is why; you must understand important aspects of pediatric trigger thumb before visiting an experienced orthopedic surgeon.
What Should You Know to Treat Pediatric Trigger Thumb Successfully? Common Symptoms/Signs
When a trigger thumb occurs, your child cannot straighten a finger stuck in a bent position without using his other hand. But you must remember the common signs or symptoms of pediatric trigger thumb are clicking, catching, and popping sensations the child experienced when he moves the affected thumb. Also, you can identify this health condition by looking for the presence of a bump or nodule at the base of the affected thumb.
Diagnosis
The orthopedic surgeons diagnose pediatric trigger thumb by conducting a physical examination and assessing your child’s medical history. While diagnosing this health condition, experienced orthopedic surgeons always look for dislocated joints or fractured bones. Likewise, they recommend imaging tests to ensure that the functionality of the finger is not being affected by any other health problems.
Treatment Options
Experienced pediatric orthopedics always start treating trigger thumbs through non-surgical procedures. They advise parents to normalize the affected thumb by combining stretching, splinting, and massaging. You need to learn these techniques from the orthopedic surgeon and perform these non-surgical procedures regularly at home. The non-surgical procedure treats trigger thumbs in most cases over a few months.
However, the orthopedic surgeon will treat trigger thumb surgically only when the non-surgical techniques do not work. He will perform a surgical procedure called trigger thumb release to remove additional pressure from the tendon by removing the A1 pulley. The trigger thumb will remain bandaged for several weeks after the surgery. Your child will start using the thumb naturally and normally after two to three weeks after the trigger thumb release surgery.
The symptoms and causes of pediatric trigger thumb vary from one child to another. But you must consult an experienced orthopedic surgeon without any delay to get the health condition diagnosed accurately and treat the health condition successfully.
0 notes
Text
What is a differential diagnosis of trigger finger?
Trigger thumb, also known as stenosing tenosynovitis, is a condition that affects the tendons in the thumb. It is characterized by the thumb getting stuck in a bent position and then suddenly popping or snapping straight. The name “trigger thumb” comes from the way the thumb moves, similar to pulling the trigger of a gun.
The primary cause of trigger thumb is the thickening or inflammation of the tendon sheath, which is the protective covering of the tendon. This thickening narrows the space through which the tendon moves, making it difficult for the thumb to straighten. The exact cause of trigger thumb is often unknown, but it can be associated with repetitive hand movements, gripping activities, or certain medical conditions like rheumatoid arthritis.

Symptoms of trigger thumb typically include:
The thumb becoming locked in a bent position.
A popping or snapping sensation when the thumb is straightened.
Pain or discomfort at the base of the thumb.
Tenderness or a lump at the base of the thumb.
Treatment options for trigger thumb may vary depending on the severity of the condition. Initially, conservative treatments are usually recommended, which may include:
Resting the thumb and avoiding activities that worsen the symptoms.
Applying ice to the affected area to reduce inflammation.
Taking over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and inflammation.
Wearing a splint or brace to immobilize the thumb and allow it to rest.
Doing stretching and strengthening exercises under the guidance of a healthcare professional.
If conservative treatments do not provide relief, medical interventions may be considered. These can include:
Corticosteroid injections: Injecting a corticosteroid medication into the tendon sheath can help reduce inflammation and relieve symptoms.
Percutaneous release: A minimally invasive procedure where a needle is used to cut the thickened tendon sheath, allowing the tendon to move more freely.
Open surgery: In severe cases or when other treatments fail, a surgeon may perform a surgical procedure to release the tendon sheath and provide long-term relief.

It is important to consult with a healthcare professional, such as a doctor or an orthopedic specialist, for an accurate diagnosis and appropriate treatment options for trigger thumb. They can evaluate your specific condition and provide personalized recommendations.
0 notes
Text
Physical Therapies for Cerebral Palsy Treatment
Cerebral Palsy (CP) is a neurological disorder that affects movement, coordination, and muscle tone. It is caused by damage to the brain before, during, or after birth. Physical therapy is an essential part of the treatment for CP, and it can help improve mobility, balance, and strength. In this article, we will discuss the different physical therapies for cerebral palsy.
Passive Range of Motion (PROM) Exercises: Passive Range of Motion exercises are designed to improve joint mobility and flexibility. These exercises are performed with the help of a physical therapist or caregiver, who moves the patient’s limbs through a range of motion. PROM exercises are often used in the early stages of CP, when the patient has limited mobility and muscle tone. These exercises help prevent muscle contractures, which are a common complication of CP.
Active Range of Motion (AROM) Exercises: Active Range of Motion exercises are designed to improve muscle strength and coordination. These exercises are performed by the patient, who moves their limbs through a range of motion. AROM exercises can help improve muscle tone and prevent muscle weakness. These exercises are often used in the later stages of CP, when the patient has improved mobility and muscle tone.
Strengthening Exercises: Strengthening exercises are designed to improve muscle strength and endurance. These exercises involve resistance training, using weights or resistance bands. Strengthening exercises can help improve posture, balance, and coordination. They can also prevent muscle weakness and atrophy.
Stretching Exercises: Stretching exercises are designed to improve flexibility and range of motion. These exercises involve holding a stretch for a set period, typically 30 seconds. Stretching exercises can help prevent muscle contractures and improve posture. They can also improve joint mobility and reduce the risk of joint pain.
Aquatic Therapy: Aquatic therapy is a form of physical therapy that is performed in water. This therapy is designed to reduce the impact of gravity on the body, which can help improve mobility and reduce muscle spasms. Aquatic therapy can help improve muscle strength and endurance, as well as reduce pain and inflammation.
Constraint-Induced Movement Therapy (CIMT): Constraint-Induced Movement Therapy is a type of physical therapy that is designed to improve mobility and function in the affected limbs. This therapy involves restraining the unaffected limb, forcing the patient to use the affected limb. CIMT can help improve motor control and coordination, as well as reduce muscle spasms.
Neurodevelopmental Therapy (NDT): Neurodevelopmental Therapy is a type of physical therapy that is designed to improve motor function and coordination. NDT focuses on improving movement patterns and postures, as well as promoting muscle control and coordination. NDT can help improve overall mobility and function, as well as reduce muscle spasticity.
Functional Electrical Stimulation (FES):Functional Electrical Stimulation is a type of physical therapy that uses electrical stimulation to stimulate muscles and nerves. FES can help improve muscle strength and coordination, as well as reduce muscle spasms. FES can also help improve functional abilities, such as walking and standing.
Orthotics: Orthotics are devices that are designed to improve posture and reduce muscle spasms. Orthotics can include braces, splints, and casts. Orthotics can help improve mobility and function, as well as reduce the risk of contractures and deformities.
Botox Injections: Botox injections are a type of medical treatment that can help reduce muscle spasms and stiffness. Botox injections work by blocking the neurotransmitters that signal the muscles to contract. Botox injections can help improve overall mobility and function, as well as reduce the risk of contractures and deformities.
0 notes
Text
Speech Therapy for Cerebral Palsy Treatment in Kids
Cerebral palsy is a neurological disorder that can affect various aspects of a child’s development, including speech and language skills. Children with cerebral palsy may have difficulty with communication due to challenges with muscle control, coordination, and oral motor function. This can make it challenging for them to express themselves effectively, understand others, and participate in social interactions.
Speech therapy is an essential intervention for children with cerebral palsy who experience communication difficulties. Speech therapists work with children and their families to assess their speech and language skills, identify specific challenges, and develop personalized treatment plans to improve their communication abilities.
The goal of speech therapy for cerebral palsy is to improve the child’s overall ability to communicate and participate in daily activities. This may involve a range of interventions and techniques, including:
Oral motor exercises: Children with cerebral palsy may have difficulty with oral motor function, which can impact their ability to speak clearly. Speech therapists may use exercises to strengthen the muscles in the mouth, lips, and tongue, which can help improve speech clarity.
Augmentative and alternative communication (AAC): For children who struggle with speech or are nonverbal, speech therapists may introduce AAC devices or systems to support communication. These devices can range from low-tech tools like picture boards to high-tech devices like speech-generating tablets.
Language development: Speech therapists may work with children to improve their understanding and use of language. This can include activities to develop vocabulary, sentence structure, and conversational skills.
Articulation therapy: Children with cerebral palsy may have difficulty with articulation, making it hard for them to form words and sounds correctly. Speech therapists may use articulation therapy to help children improve their ability to produce sounds and speak more clearly.
Social communication skills: Children with cerebral palsy may struggle with social interactions due to difficulties with communication. Speech therapists may work with them to improve their ability to understand and respond appropriately to social cues, engage in conversation, and make friends.
Speech therapy for cerebral palsy is typically conducted in individual or small group sessions, and progress is closely monitored to ensure that the child is making meaningful gains in their communication skills. It is also essential for parents and caregivers to be involved in the therapy process, as they can provide valuable support and reinforcement of the techniques and strategies used in therapy.
Overall, speech therapy is a critical component of the care plan for children with cerebral palsy who experience communication challenges. By working with a skilled speech therapist, children with cerebral palsy can improve their ability to communicate effectively, express themselves, and engage in social interactions, enhancing their overall quality of life.
1 note
·
View note
Text
Occupational Therapies for Cerebral Palsy Treatment in Kids
Planning a corporate event or holiday party anywhere in White Plains or Westchester, NY can be challenging. You need to consider certain factors like the guest list, catering, and entertainment. However, one of the most significant aspects of planning any event is choosing the right venue. Whether you are looking for an event space for corporate events in White Plains or holiday parties in Westchester NY, continue reading a few tips to find the right venue.

Consider the location.
When it comes to planning an event, location is a key factor. You have to consider the convenience of the venue for your guests. If you are inviting most guests from out of town, you have to look for a venue that is accessible to hotels or public transportation. If you're planning a holiday party or a corporate event, the venue must be easy to access and have ample parking.
Focus on the capacity and layout.
The venue's capacity and layout play a significant role in choosing an event space. You have to make sure that the venue accommodates your guests comfortably. After all, you don't want your guests to feel cramped or overcrowded in the event space.
Besides, you should consider the layout of the venue. Please check whether it has ample space that you can use for different purposes, such as a cocktail hour or a dance floor.
Check out the amenities and services.
After that, you will need to check the amenities and services provided by the event space. You have to know whether they have in-house catering, audio-visual equipment, or decoration. Discuss with them whether they will provide staff for the event like the servers or a coordinator. Feel free to ask about any extra costs for these services.
Consider the venue's atmosphere and style.
You should consider the atmosphere and style of the event venue. You should know whether the venue matches the theme of your event. If you're planning a corporate event, you can choose a professional and sophisticated venue. If you're planning a holiday party, you should look for an event venue that looks festive and fun.
Final Consideration -
Finding the right event space for corporate events in White Plains and holiday parties in Westchester NY can be challenging. You will need to consider the location, capacity and layout, amenities and services, atmosphere and style and narrow down your options and find the right selection for your event. With a little research and planning, your event is sure to be a success.
So, you should consider booking Coliseum for planning corporate events in White Plains or holiday parties in Westchester NY. Let us make your event successful and engaging.
0 notes
Text
Cerebral Palsy in Kids, Treatment & Care Options in India
Cerebral palsy is a group of neurological disorders that affect movement and posture. It is the most common motor disability in childhood and affects about 3 in every 1,000 children in India. While there is no cure for cerebral palsy, there are treatments and care options available that can help manage symptoms and improve quality of life. In this article, we will discuss pediatric cerebral palsy treatment and care.

Diagnosis and Early Intervention:
Early diagnosis and intervention are critical in managing cerebral palsy. If you suspect that your child may have cerebral palsy, it is important to speak with a healthcare professional as soon as possible. A pediatrician, neurologist, or developmental pediatrician can perform a physical examination and order tests such as magnetic resonance imaging (MRI) or a computed tomography (CT) scan to diagnose cerebral palsy.
Once a diagnosis is made, early intervention services can be provided. These may include physical therapy, occupational therapy, speech therapy, and assistive technology services. These services can help children with cerebral palsy develop new skills, improve muscle strength and mobility, and manage symptoms.
Medications:
In some cases, medications may be prescribed to help manage symptoms of cerebral palsy. For example, muscle relaxants can help reduce muscle spasms and improve range of motion. Anticonvulsant medications may be prescribed to control seizures, which can sometimes occur in children with cerebral palsy. Botulinum toxin injections may also be used to reduce muscle stiffness and spasticity.
Surgery:
In some cases, surgery may be recommended to improve mobility and reduce pain in children with cerebral palsy. Surgery may be used to lengthen or shorten muscles, improve joint alignment, or correct scoliosis. It is important to discuss the potential risks and benefits of surgery with a healthcare professional and to carefully consider all options before making a decision.
Care and Support:
In addition to medical treatments, care and support are important for children with cerebral palsy. This may include physical therapy, occupational therapy, and speech therapy, as well as psychological support and counseling for both the child and their family. Assistive devices such as wheelchairs, braces, and communication devices can also help improve quality of life.
It is important for families to work closely with healthcare professionals to develop a care plan that meets the individual needs of the child with cerebral palsy. This may involve coordinating care between multiple specialists, such as neurologists, physical therapists, and orthopedic surgeons.
Conclusion:
Pediatric cerebral palsy treatment and care require a multidisciplinary approach that involves a range of healthcare professionals and support services. While there is no cure for cerebral palsy, early diagnosis and intervention, medications, surgery, and care and support can help manage symptoms and improve quality of life. It is important for families to work closely with healthcare professionals and to be aware of all available options in order to provide the best possible care for their child with cerebral palsy.
0 notes