Text
Causes of lower back pain?

Many people continue to suffer from low back pain. If not you, then several people you know—neighbours, coworkers, friends, and relatives, to name a few. That is what the statistics show. Because it is so common worldwide, millions of people want to know "what causes low back pain." Is this normal and expected as we get older? Is it inherited? Will you have to have surgery? You might expect the answer depending on who you ask.
To begin with, no two people feel the same amount of pain. Some people experience low back pain on the right side, while others experience it on the left. Some people experience low back pain that extends into the hip.
Low Back Pain Causes
Most low back pain instances are mechanical in origin, meaning they are caused by a physical component of the lumbar spine failing. Muscles, fascia (muscle sheath), ligaments, tendons, vertebrae, vertebral joints, and discs. When nerve roots become compressed due to dysfunction, it causes nerve discomfort, which commonly manifests as shooting / radiating pain and numbness down the buttock to the lower extremity; sometimes as far as the sole.
The following are the main types of mechanical low back pain:
Congenital Deformities
Anomalies in the spinal column development can sometimes obstruct adequate movement and balance, putting undue stress on soft tissues and nerves, causing discomfort, stiffness, pains, and a loss of range of motion and flexibility. Examples include fused vertebrae, scoliosis, spina bifida, pars defect, hyperkyphosis, and hyperlordosis.
Injuries
Acute tissue damage triggers the inflammatory response responsible for pain creation. Ligament sprains cause low back discomfort, ruptured intervertebral discs from a herniated or prolapsed nucleus pulposus, muscle and tendon strains, muscular spasms, and fractures. These can be traumatic from a single incidence, such as a sports injury, or cumulative over time, typically years, resulting from repeating a specific action or sitting/slouching, leading to degenerative disc degeneration.
Changes in Degeneration
In all cases, the vertebral joint surfaces lose their smooth borders and form jagged bone spurs known as osteophytes. You can have many osteophytes in your spine and not feel any pain. Over the age of 40, you most likely have them. However, problems arise when the osteophytes grow large enough to narrow the openings where nerves pass through, known as the foramen. This narrowing of the foramen is known as spinal stenosis, and it can occur in the intervertebral foramen (IFVs), which are small holes formed by adjacent vertebrae through which nerve roots pass, as well as the central canal, which houses the spinal cord and cauda equina.
It can cause shooting pain down one or both legs, numbness, tingling, leg muscle weakness, atrophy, and loss of sensation. Because osteophytes do not resorb and only grow in size over time, the only option is spinal decompression surgery, which involves shaving the osteophytes away to make more room for the nerves.
Joints deteriorate over time. Most doctors will tell patients that their condition is due to "normal" wear and tear. Among the factors that contribute to lumbar spine degeneration are:
overweightness.
Predisposition due to genetics.
Sedentary behaviour/lack of physical activity.
A lot of sitting (airline pilot, police officer, truckers, data entry).
Arduous labour.
Football, especially, is a contact sport.
Occupation or pastime involving hard landings (basketball, gymnastics, parachuting, etc.)
Previous injuries/accidents, such as slips and falls and car accidents.
Dietary deficiencies (your body needs proper nutrients to heal tissues).
Tobacco use (smoking reduces oxygen to cells and may trigger inflammation).
Spinal degeneration is described by doctors using three terms:
When referring to the vertebrae as a whole, the term spondylosis is used.
Degenerative joint disease, also known as DJD, is a condition that affects the vertebral joints.
Degenerative disc disease, also known as DDD, is a condition that affects the intervertebral discs.
0 notes
Text
Pain and Injury Doctor

PainandInjuryDoctor provides an alternative method of pain management. The foundation of all self-treatment strategies taught on this site is optimising the body's healing potential. It includes eating a nutritious diet, detoxifying the significant organs, reducing stress, and exercising. Then, self-care procedures promote healing and restore strength, flexibility, and coordination. It is accomplished by applying a combination of joint and soft tissue mobilisation, exercise rehabilitation, and specialised therapeutic equipment.
0 notes
Text
Pain and Injury Doctor

PainandInjuryDoctor provides an alternative method of pain management. The foundation of all self-treatment strategies taught on this site is optimising the body's healing potential. It includes eating a nutritious diet, detoxifying the significant organs, reducing stress, and exercising. Then, self-care procedures promote healing and restore strength, flexibility, and coordination. It is accomplished by applying a combination of joint and soft tissue mobilisation, exercise rehabilitation, and specialised therapeutic equipment.
0 notes
Text
What exactly is red light therapy?

Red light therapy is a skin-improvement treatment that employs red light to reduce tiny wrinkles, scars, redness, and acne. It's also used in medicine to treat tendinitis, sprains/strains, and arthritis by reducing discomfort and speeding up the healing process in the joints. It is used in clinical and cosmetic settings.
0 notes
Text
What Is the use of Red Light Therapy?

Increase the speed of wound healing.
It should alleviate joint pain.
It should minimize stretch marks.
Wrinkles, fine lines, and age spots are reduced in appearance.
Psoriasis, rosacea, and eczema can all be improved.
Enhance the look of new scars.
People's hair growth will improve.
Acne relief.
How Does Red Light Therapy Work?
It is well known that light can cause biological changes in living organisms. Photosynthesis, the series of biochemical reactions in which sunlight energy catalyzes the formation of sugar in plants, is perhaps the most well-known. Chloroplasts absorb light photons, tiny structures in plants that provide the biological machinery to synthesize glucose from inorganic carbon dioxide and water.
The pathway is most likely similar to red light. Many studies have been conducted over the years to determine the mechanism of red light photobiomodulation, i.e. the nature of its therapeutic effects. What is certain is that red light is absorbed in the nucleus and mitochondria of cells in locations known as chromophores. Mitochondria (image below) are structures that produce energy for the cell, similar to the previously mentioned chloroplasts in plant cells. The nucleus houses DNA, which serves as a template for protein synthesis.
In short, red light stimulation raises the energy state of electrons in diseased tissues, allowing for faster/enhanced reactions between adjacent molecules, as electron interactions between atoms are the foundation of all biochemical reactions. This might cause the cell's functions, including respiration (creating ATP from glucose via the Krebs cycle, i.e. energy production), waste removal, and gas exchange, to "speed up." This activity is referred to as redox signalling, and it is the leading hypothesis for the mechanism of red light photobiomodulation.
Increased cellular signalling results in:
If the cell is a fibroblast, it may result in faster wound healing because fibroblasts migrate to the injured or damaged site to synthesize and lay down collagen fibres.
If the cell is a stem cell, it may promote stem cell differentiation into fibroblasts or chondrocytes, which produce collagen and cartilage, respectively.
If the cell is an epidermal cell, it could mean faster cell turnover in skin conditions like eczema and psoriasis to clear out abnormal cells.
Cells are programmed to respond to specific extracellular signal molecules for development, tissue repair, immunity, and homeostasis. Errors in signalling interactions can result in diseases like cancer, autoimmunity (like rheumatoid arthritis), and diabetes. Given this, it is reasonable to believe that if red light therapy can improve cell signalling, it can benefit these cellular functions and aid in tissue healing and pain relief.
Red Light Therapy reduces inflammation.
Inflammation is the body's reaction to an injury or irritant, characterised by redness, swelling, and pain. Multiple protein clotting factors in the blood and tissues are involved in a complex series of actions. It also comprises cytokines, chemical signalling molecules used by cells to communicate and coordinate activities inside and between them. Inflammation also involves macrophages, basophils (a kind of white blood cell that secretes histamine and heparin to make blood vessels permeable and manage to clot), and fibroblasts, all engaged in the healing process. Red light has been shown in several studies to lessen tissue inflammation.
Chronic inflammation is involved in arthritis, irritable bowel syndrome, vascular disease, diabetes, and even Alzheimer's disease. Inflammation frequently becomes out of control at the injury/damaged tissue site and contributes to the problem by increasing pain and delaying healing. This is the rationale behind using anti-inflammatory medications such as steroids and non-steroidal anti-inflammatory drugs such as Tylenol and Ibuprofen to treat inflammation.
According to one study, one of the most reproducible effects of photobiomodulation [from red light] is reducing overall inflammation. Red light therapy's ability to reduce inflammation is most likely to improve cell signalling and molecular flow. This is especially important for inflammatory diseases of the joints and acute trauma, lung disorders, and brain injuries that result in inflammation.
0 notes
Text
Low Back Pain

Make Lower Back Pain Free Living your New Year’s Resolution in 2022! Discover Pulsed EMF and Red Light, the best home therapy routine your money can buy. Pulsed EMF.com. Researched-backed, safe and affordable.
0 notes
Text
Two Modalities to Heal Low Back Pain in Half the Time
Hey, I know there are millions of pages on the internet on how to fix low back pain. It can be a dizzying experience searching through them. If you are prone to getting lower back pain or have chronic pain issues, Pulsed EMF and Red Light Therapy are two, powerful and safe modalities that can be used at home for self-treatment and are easy to operate. Best of all, they have a long history of medical research to support their use in treating pain and healing injury. It does require a modest investment, but what is more important to your health and well-being? Without this, nothing else matters. For more information visit: https://bit.ly/3qLSQUe

0 notes
Text
A Look into George Floyd’s Cause of Death, From an Anatomical Perspective
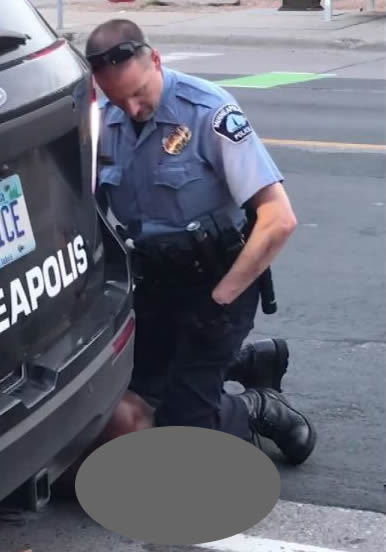
On May 25, 2020 an African-American man named George Floyd was apprehended by four police officers in Minneapolis, Minnesota. During the apprehension, a police officer named Derek Chauvin placed the handcuffed Floyd prone on the street, then knelt over him, placing his left knee on top of Mr. Floyd’s neck. From the image circulated in the media, it appears that Chauvin exerted his full weight over his bent knee. He kept his knee in position for 8 minutes and 46 seconds despite please from Floyd that he could not breathe. Tragically, Mr. Floyd died at the scene. Two autopsies on Mr. Floyd ruled the death a homicide. The county version “revealed no physical findings that support a diagnosis of traumatic asphyxia or strangulation” while a private autopsy ruled he died of “asphyxiation due to neck and back compression.” Asphyxiation is the deprivation of oxgyen to the body, resulting in death. Chauvin was fired and arrested shortly after the incident, and charged with 3rd degree murder and second degree manslaughter.
This tragic and awful case spurred protests and civil disobedience throughout major cities in the U.S., against systemic police brutality and racism towards African-American men, which continues as I write this. It is also a case that has drawn interest in the medical and forensics community, as to how exactly George Floyd died. This is important to investigate, as it has consequences for the trial and also provides information to police forces to help them determine which types of restraints should and should not be used.
Before discussing the medical aspects of Mr. Floyd’s death, I want to emphasize that the most important thing about this incident is that a man unnecessarily lost his life to a trusted law enforcement officer, in a most inhumane way. It is especially bad because of the systemic racism element to it, and the fact that Chauvin had several opportunities to get off of him in time after being warned by another officer at the scene and multiple witnesses, but failed to do so. This was a textbook lesson on how not to subdue a person, and the price of this lesson is going to play out for weeks to months and will be costly to society in more ways than one.
That being said, I will discuss the anatomical and physiological factors involved in Mr. Floyd’s death. There is some controversy over how he died, which will determine what sentence, if any, Derek Chauvin will receive.
As you will see, the neck contains several structures directly tied to sustaining life, which is why the neck is a logical target when it comes to martial arts/ self-defense, and yes, murder.
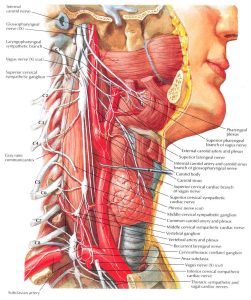
Mr. Floyd was lying prone (stomach down) with his hands handcuffed behind his back and neck turned to his right. So when Chauvin placed his knee over his neck it contacted the lateral (side) aspect of his neck and some of the anterior portion. The critical structures found at the side of the neck include the vertebral arteries, cervical nerve roots, carotid arteries, jugular veins and lymphatic vessels. Attached to the carotid artery is the carotid body, a cluster of special cells that detect oxygen saturation levels in the blood leaving the heart, and passes the information to the brain, which the brain uses to regulate heart and breathing rates accordingly.
Inside the cervical spine (the neck bones) there is the spinal cord which is comprised of the neuron axon bundles that control body movement and sensation; and lying just outside and against the cervical spine is the sympathetic chain ganglia, which play a role in innervating the heart, lungs, adrenal glands (adrenaline secretion) and other organs during “fight or flight” moments of stress.
The critical structures found in the anterior neck are the esophagus, trachea (wind pipe), larynx and thyroid gland. Also present but not critical to life are the vocal cords.
The contact area on Mr, Floyd’s neck, based on the typical size of a bent knee, was about 4 square inches. Chauvin weighs about 170 pounds, so I estimate that the force placed on Mr. Floyd’s lateral-anterior neck was (.9)(170 lbs)/4 in sq. =153 lbs/ 4 in sq. = 38.25 lbs./in sq. So imagine four, 40 pound dumbells stacked and resting on the side of your neck for nearly 9 minutes.
What I believed happened is blood flow to the brain was cut off, making Mr. Floyd unconscious after a few minutes, as would happen in a martial arts choke hold. We can assume the loss of consciousness due to restricted blood flow to the brain occured the moment he stopped talking. Chauvin kept his knee in place for nearly 3 minutes after Floyd stopped moving. If there was any chance of resuscitation, that chance ended with this additional time of compression.
The pressure also activated Mr. Floyd’s sympathetic chain ganglion, which caused a surge of adrenalin– a neurotransmitter secreted by the adrenal glands of the kidneys that prepares the body’s response to stress. This increased his heart rate, increased blood pressure by vasoconstricting his arteries; dilated his pupils, and attempted to increase breathing rate. However, with Chauvin’s knee on Floyd’s neck, the increased respiratory rate did not result in more oxygen getting to the body and the diaphragm, the sheet of muscle that pulls down and expands the lungs for breathing may have spasmed as it fought against the air blockage.
Most of Chauvin’s knee was over the side of the neck, but the front (anterior) was subject to some compression. This likely partially collapsed the trachea, restricting air flow. Mr. Floyd was initially able to express his inabilty to breathe, suggesting that his trachea was still patent, but his words became less and less as the seconds ticked. Perhaps Chauvin’s knee shifted forward with his weight, slowly closing off the trachea. This makes sense, as the neck has a curved contour which would promote such slipping.
As the knee hold persisted cutting blood flow to his brain, Mr. Floyd’s blood rapidly turned acidic as all oxygen was used up (the brain has a high metabolic rate and therefore a high rate of oxygen consumption) and CO2 levels were rapidly rising (CO2 is a byproduct of cell respiration). This may have affected his speech center, which is supported by the fact he stopped talking a few minutes after the knee hold. The apneustic (breathing) center in his brainstem was starting to break down as well from the hypoxia (insufficient oxygen), hampering his breathing further.
It’s not clear at what point Mr. Floyd expired. Coroners define time of death at the point when brain activity ceases. But the nature of Mr. Floyd’s death was so prolonged, it is likely he experienced irreversible brain damage and would have been in a vegetative state even if Chauvin had gotten off of him a little earlier and Mr. Floyd was given immediate medical attention.
One of the tell-tale signs of asphyxia by strangulation is ruptured blood vessels in the conjunctiva (whites of eyes) and face, called petechial hemmorhaging. This information, as far as I know, is not available to the public. If there was no evidence of this, I can see why the county autopsy reached the conclusion that he did not die of asphyxia. In this case, it would suggest that Mr. Floyd’s primary cause of death was something else; perhaps sudden stoppage of the heart due to a breakdown in the cardioregulatory system. But, it is not clear if you can die from asphyxia from “gradual” strangulation and not have petechial hemmorhaging. It could also be that death was from a combination of both asphyxia and heart stoppage.
The autopsy did not mention fractured cervical vertebrae, which I could see happening if it were a smaller-framed person. The force Chauvin exerted on the neck appears enough to break one or several neck bones, especially if the person had osteopenia (bone thinning). Fractured neck vertebrae often result in spinal cord damage and paralysis.
Conclusion
George Floyd’s tragic death is a wake-up call for police forces across the country. Knees to the neck to restrain someone must be prohibited. There are too many ways for this to go wrong, given the high concentration of structures critical to maintaining life that reside in the neck. I understand that safety to police officers is important and fully support it, but it must not be accomplished by jeopardizing the safety of the person being restrained.
0 notes
Link
TREAT YOUR BODY WELL WITH PULSED ELECTROMAGNETIC FIELD THERAPY

A wonderful collection of chemical products, tiny organelles such as mitochondria and genetic code in the lipid membrane is the primary unit of our bodies. This lipid membrane made of cholesterol is a double layer that isolates the cell contents from the outside. There is a negative charge on the inside side of the membrane, whereas the outside layer is positive. This is not a closed system cell membrane. It has "gates" that can transport ions as needed in, and out the cell, such as potassium, sodium and calcium. But the work of these gates needs electrical currents or pulses – visit here PainandInjuryDoctor.com for PEMF treatment.
0 notes
Text
How Pulsed Electromagnetic Field Therapy (PEMF) Can Improve Your Health

Pulsed electromagnetic field therapy, or PEMF is a safe, effective treatment for many types of health conditions. Some people use it for arthritic pain, while others use it for fibromyalgia, insomnia, and even chronic lung and cardiovascular illnesses. Unlike medicine and surgery, PEMF therapy doesn’t have dangerous or serious side effects.
There are many types of PEMF machines on the market, direct to consumer so it doesn’t require multiple trips to the doctor for treatment. The beauty of this is that PEMF can be used on-demand: whenever you have an acute flare-up or especially bad day; or, for daily maintenance of health.
And, since it is safe and doesn’t involve drugs, PEMF therapy can be used with other interventions that you may be currently using to reduce pain and inflammation, which leads to faster healing and recovery.
You may be wondering at this point, “how does Pulsed EMF work?”
PEMF – The Basics
As the name implies, PEMF therapy uses magnetic pulses that it sends into the body to speed up healing of weak cells, and therefore recovery. The human body emanates electric charges (think brain and nerve impulses and charged molecules and ions like Ca+, Mg+, H+ and OH-) and just like inanimate things that require electricity or batteries to keep them going, your body needs “recharging” once in a while. Several trillions of cells comprise your body, depending on how big you are, so it’s not surprising that many of them can break down at any time.
Healthy, normally-functioning cells have a balance between positive and negative charges (see image below). As these charges flow inside and between adjacent cells, electrical currents are produced. This electrical flow is the means by which nutrients and waste products enter and exit through cells, via special structures called ion channels. For example, when nerves are stimulated, they “depolarize,” where the negative and positive charges rapidly exchange position (inside vs. outside the membrane) and move down the nerve. This is called an “action potential” and is the actual means by which our nerves are able to contract our muscles, control our organs and send sensory signals to our brain.

When this critical flow of electrical currents through cells is disrupted, cells don’t carry out their functions as well as they need to. This leads to illness and symptoms. Things like trauma, disease processes, and exposure to toxins can alter these electrical signals. Pulsed electromagnetic therapy uses the same, natural frequencies produced in the body to give these cells a boost in energy. This restores the positive and negative charges in the weakened cells to their ideal state so they can once again function normally.
You may have heard of the dangers of electromagnetic fields (EMF) or electromagnetic radiation, especially if you follow alternative health websites. The frequencies used for PEMF therapy is nowhere near that of harmful EMF such as X-rays, gamma rays and microwaves. PEMF generates non-ionizing radiation, identical in frequencies already emitted by your body and therefore generally accepted as harmless to humans.
Health Benefits of PEMF therapy
There are many research studies that support the use of PEMF therapy for a wide range of disorders, from acute (recent; active) injury or health problems to chronic pain.
According to studies, PEMFs are useful in treating post-surgical pain; pain related to diabetic neuropathy, joint pain from osteoarthritis, and chronic lower back pain. PEMF therapy has also been shown to increase the healing rate of nonunion fractures, and even increase bone density in those who have osteoporosis. PEMFs ability to increase microcirculation to tissues is likely a factor.
Perhaps most impressively, PEMFs can help your body decrease inflammation, which is present in many chronic conditions including fibromyalgia, inflammatory arthritis, chronic fatigue syndrome, and autoimmune disorders such as Chron’s disease.
There are even studies that found PEMF therapy to have measureable, positive effects on those battling depression and anxiety, with long-term, daily treatment.
Conclusion: Pulsed EMF is a safe alternative for healing
If you are battling disease and/or pain, consider trying Pulsed EMF. It has scientific research going back over 40 years that support its many health benefits, and it is comparatively safe/ low risk to most individuals (those with heart conditions and implants should check with their doctor first). PEMF machines produce electromagnetic fields at the same frequency as the human body’s, so cells respond to them in a positive way.
PEMF machines available for home use are low intensity, so there is no danger of excessive exposure that could lead to significant adverse side effects. Treatment time can vary from just a few minutes to continuous, overnight use, depending on the problem being treated. The machines offered on our site are established leaders in PEMF technology, from the Russian-manufactured Almagia line to the HTC products—FlexPulse, BioBalance and TeslaFit lines.
There are some higher intensity machines (TeslaFit) meant for use in clinics that are more effective for long-standing, chronic conditions rooted deep inside the body; but most conditions can benefit from the lower intensity units.
The FlexPulse is a low intensity, portable PEMF unit available direct to consumer. It was developed based on NASA stem cell research done over 15 years ago, and decades of research on brain entrainment (synchronizing biological frequencies) and neurofeedback. By increasing stem cell (cells that can turn into any type of cell) production, the FlexPulse promotes safe, natural regeneration with no side effects. Specific, pre-programmed frequencies mimic brain patterns to promote relaxation or alertness, enhance sleep, and relieve pain depending on your treatment goals.
The FlexPulse is a compact, wearable system that comes with two small pad applicators making it easy to use anytime, anywhere. The system comes with a 30 -day satisfaction guarantee and a 2-year International warranty, making it a no-risk healing alternative.
Check out our full line of Pulsed EMF machines here.
Watch the video below where I explain how Pulsed EMF can re-energize weak cells and help restore health.
0 notes
Link
Understanding Wrist and Hand Pain

Many elements – the first of all is asymmetrical muscle activation – depend on the correct operation of hand and wrist joints. The muscles that aid stability in movement and rest surround every joint in the body. Read More: https://painandinjurydoctor.com/
0 notes
Text
How I Got Trigger Finger and What I Did to Treat It
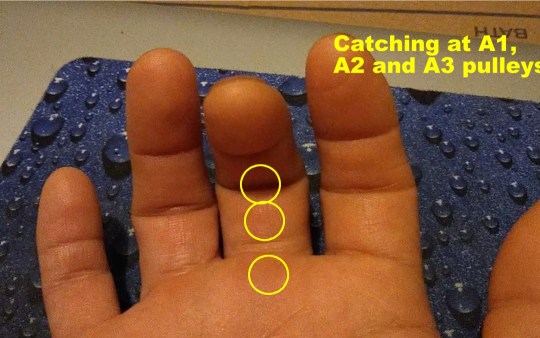
In my case, I have trigger finger in the middle and ring fingers of my right hand, mostly in the A1 and A2 pulley, and less in the A3, with the middle finger being more problematic. Pain is most pronounced in the middle of the night and upon waking, then gets better rather quickly in my case, in the first waking hour of the day. This is because as you sleep, there is less movement of the joints and less synovium produced, causing them to be stiffer.
I have the classic symptom where there is locking of those fingers when I move them from the natural, half-open relaxed hand to fully extending the fingers. As I force them past the locked angle, they snap at the A1 and A2 pulleys, then straighten out. It’s momentarily painful, but tolerable. But for some people, it’s a lot worse. All those weeks of sustained power gripping and twisting caused the flexor tendons and synovium to rub excessively against the ligaments holding them in place, causing microtears and initiating the inflammatory response.
TREATMENT FOR TRIGGER FINGER
The medical standard of care for trigger finger is corticosteroid injection below the affected ligament. This quickly knocks down the inflammation, and in some cases, symptomatic improvement happens within seconds. However, some patients report pain following the injection, and slower or no results.
Splinting is sometimes attempted. The idea is that if you immobilize the tendon, inflammation will stop and the tendon will shrink and heal, bringing things back to normal. However, this is not always the case. Sometimes inflammation takes a life of its own, and prolongs long after the injurious event ceases.
If neither corticosteroid injection nor finger splinting fail to correct the problem, surgery is an option. Direct, open surgery and percutaneous (minimal incision, special surgical tools) surgery are the two options, with direct surgery usually having better results. This is where the ligament is cut to provide more room for the tendon to move. This is possible because the adjacent ligament serves as a backup; for example, the A2 can back up A1 if A1 needs to be cut/ split apart. However, as you can imagine such destruction of a functional component means some strength and stability are sacrificed. I’m sure those having this kind of surgery lose some power in their grip.
MY TREATMENT STRATEGY
As I write this article, my trigger fingers have improved about 75%, from their worst presentation. It could be that my connective tissues are in pretty good shape; my healing capacity is strong; my injury was not very severe; or my treatment regimen is helping accelerate healing. Some sufferers don’t see such a quick pace of resolution.
Here is what I’m doing: as I mentioned, the symptoms are most pronounced in the middle of the night (when I get up to use the bathroom) and upon waking. In the middle of the night, I simply don’t move my fingers, and go back to sleep.
In the morning, I run cold water over my hand for 2 minutes, and gently move my fingers. I get the snapping, but it dissipates shortly after. I still feel some stiffness and soreness in my knuckles throughout the day, but no snapping.
I get localized cryotherapy done on my fingers. Cryotherapy is extremely cold air, as in sub-zero, for 3 minutes. The cold not only slows inflammation, it is said to cause a shock to the sensory nerves, which causes the central nervous system to respond by increasing blood flow, fibroblast activity, and nutrients to the area.
Note: the image above is a localized cryotherapy session on my hand, for a previous complaint. The red dot is not red light therapy; it is a laser thermometer the technician uses to measure my skin temperature so that it doesn’t too low (his hand is visible in the picture). Localized cryotherapy can reach temperatures of -30 degrees F.
Lastly, I apply red light therapy. I’m an advocate of this therapeutic technology and have written articles about it. Red light therapy is actually an electromagnetic waveform (600-880 nanometer wavelengths) that appears red to the human eye. It’s not the red you get from shining a light through a red lens; it’s a specific waveform in the electromagnetic spectrum generated from an LED (light-emitting diode). The device I use uses three LEDs, one of which emits a waveform closer to infrared and therefore does not appear to be red as it is invisible. The electromagnetic energy is at a frequency that gets absorbed by cell mitochondria and other structures, which can result in changed oxidative states that lead to cell signaling that initiates reparative processes, such as increased ATP production and increased membrane permeability. This lessens inflammation and stimulates healing.
I anticipate my trigger fingers to fully recover, to pre-injury status. I will continue to do these therapies, as I feel they are partly responsible for my good results.
BOTTOM LINE
Prevention is the best cure: if you know you are going to be using your hands a lot, such as starting on a do-it-yourself project involving power tools and hard gripping, know that this can cause trigger finger. Do what you can to minimize the stress to your hands—take frequent breaks; don’t overdo it/ don’t hold a power grip for more than a few seconds; and rest and stretch your hands often. Don’t rush it. Trigger finger creeps up on you, and by the time you notice it, it is too late. The presentations are different from person to person, depending on age, health, fitness and so on. I am lucky as my condition is resolving; others are not so lucky and wind up getting surgery and permanent percent loss of hand function. So make sure you keep prevention in mind. If you do get it, try the treatment methods for trigger finger described here that have worked for me.
It’s been a while since my last article. Between the weekly-changing COVID restrictions in my area and major house renovations, I have been delinquent with my life mission of helping others manage and heal their pain and injuries, on their own. But today, I’m back on track. Today, I’ll talk about a peculiar condition known as Trigger Finger.
But first, a little background:
For those who ever engaged in do-it-yourself home renovations such as landscaping, fence building, paver-laying and bathroom and kitchen remodeling you know how much stress it can put on your body. This is my story of how I developed trigger finger for the first time in my life, and serves as a “lessons learned” opportunity for others so that they can be spared the inconveniences of this condition..
For the last 10 years, I would categorize my daily physical activity as “moderate.” I would go the gym and lift free weights (reps over max); do various cardio fitness classes such as the Les Mills classes and Bootcamp; and run 3 miles about 3x/week. My average time in the gym I would say was 60-90 minutes, with about half of that actual exercising. At home, I would be working on my website and producing videos. This did require prolonged sitting, but I would get up every 30 minutes or so to walk around to relieve pressure to my lumbar spine.
Starting the second week of this past July, I started the aforementioned home renovation projects. I basically went straight from moderate activity to short bursts of sustained intense activity, daily for over four weeks. Since I didn’t have any major musculoskeletal impediments other than a chronic right AC (acromioclavicular) joint sprain, I moved freely as though I was in my 20s, which wasn’t such a good idea. The combination of the intense movement patterns my body wasn’t used to, plus my age, took a significant toll after four weeks.
Here are some of the heavy labor activities that I engaged in:
Carrying heavy lumber from Home Depot and loading into a pickup truck, about 10 trips
Carrying 50 and 80 pound bags of concrete mix and sand, for my paver project, about 5 trips.
Used a 2-person auger (about 120 pounds; gasoline powered) to drill several 3’ deep post holes
Shoveled piles and piles of dirt (pickup truck loads—about 10x)
Hauled away bulk trash to the dumpster
Carried 100 clay 12”x12” paver squares (bricks) from a truck to my yard and positioned them carefully
Used hand tools that required hard gripping and/or twisting including various types of saws, wrenches and screwdrivers
Used vibrational tools including a miter saw, reciprocating saw, drill, and nail gun
By the third week, I was starting to feel pain at my right AC joint, my left wrist, and both hands especially my right, dominant hand. Thankfully, despite frequent bending at the waist my lower back wasn’t affected. I attributed the AC join pain to aggravation of the old strain (I rate it a Grade 2 or 3 sprain – partial tearing, but intact). What happened is the heavy lifting placed a repetitious load on that unstable joint, causing the acromion and distal clavicle to aggravate surrounding soft tissues, particularly the supraspinatous tendon, and the insertion points of the ligament. My doctor suggested my pain was impingement syndrome—compression of the supraspinatous tendon where it passes below the acromion– which could be occurring, but I’m certain most of the pain is emanating from the joint itself because I can reproduce the pain simply by pressing it with my fingertip. I’ll tell you how I’m treating this in the next article.
I believe my left wrist pain is a Grade 2 strain of the flexor ulnaris tendon where it inserts into the distal ulnar’s styloid process; caused when I lost control of the auger. The auger is a very powerful machine that requires two people to operate (see picture above). Not being familiar with using one, I wasn’t prepared for the powerful torque it generated, and lost control of it, hurting my wrist.
The third problem that I’m dealing with is trigger finger. This is the first time I’ve had it and let me tell you, it’s not very pleasant.
Trigger finger is so named because as you attempt to straighten out your finger after closing your hand, the finger “catches” mid-way, and pain is felt in one or several joint capsules usually on the palmar side. Then, as you power through the restriction the pain increases and a popping/snapping sensation occurs right before it straightens out, just like how a gun trigger offers gradual resistance then suddenly releases at a point. See the short video below of my actual trigger finger taken this morning that explains this.
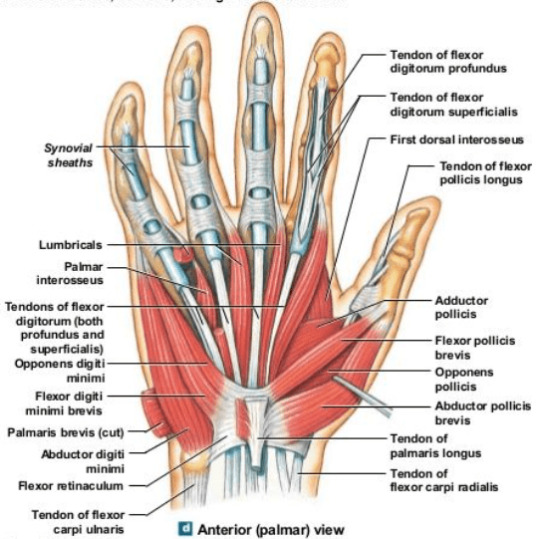
Trigger finger is a stenosing tenosynovitis disorder. Stenosing means narrowing of a passageway in the body; tenosynovitis refers to inflammation of the tendon and synovium. The synovium is a specialized layer of tissue surrounding the tendon in areas where it rubs against other structures in the body. Synovium secretes synovial fluid, a biological lubricant that helps reduce friction where the tendon moves. Synovium also lines the synovial joints of the body which include the hips, knees, shoulders, elbows, spine and joints of the hands and feet.
There are three, main populations of trigger finger sufferers: young children (up to 8 years old); trigger finger as a comorbidity to a primary disease; and adults experiencing trauma/ stress to the hands, typically in the 40s-50s. It tends to affect women more, and the most common finger is the thumb although it can occur in any finger, and in multiple fingers at the same time.
In children, trigger finger is believed to be due to uneven growth rates of the hand flexor tendons and the ligaments, where the tendon growth outpaces the growth of the ligaments that hold them against the finger bones.
Trigger finger is observed to often occur alongside certain other diseases such as carpal tunnel syndrome, diabetes, hypothyroidism, gout, rheumatoid arthritis, and amyloidosis; each probably having different etiologies involving the dysfunction causing the primary disease. Diabetics seem to be affected by trigger finger at a higher rate than the regular population, and it is uncertain why. With diabetes mellitus, there are high levels of glucose in the blood, and usually high insulin levels. Insulin is considered an anabolic hormone associated with tissue growth, so this may be a possible explanation for the increased incidence of trigger finger in diabetics, if the growth leads to tendon hypertrophy (enlargement).
For the third group, which the rest of this article will address, trigger finger is caused by hypertrophy and inflammation of the finger flexor tendons at the synovial sheath, typically from repetitious hand movements, especially those involving power gripping and vibration, making them chafe against the ligaments that hold them down to the finger bones (phalanges). (Remember, ligaments connect two bones, while tendons connect a muscle to a bone; both are components of all moveable joints). Imagine these ligaments as slips of Scotch tape forming a tunnel over the bone. As the hypertrophied (enlarged) section of the tendon enters the narrow tunnel during extension (straightening out of the finger), it gets stuck in that tunnel momentarily; much like how a big person trying to climb out of a small bathroom window can get stuck before being able to make it through. Then, as the tendon makes it past that entrance, it causes the popping sensation.
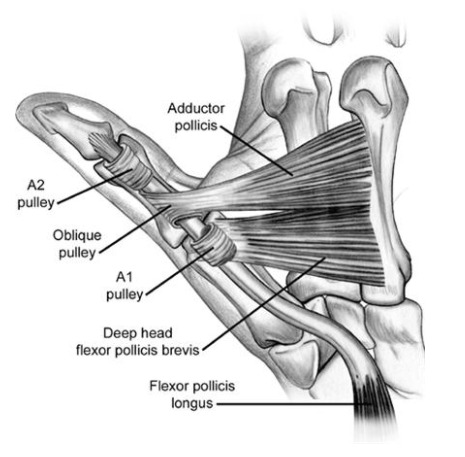
Orthopedic specialists identify the tendon-ligament structures involved in hand movement as pulleys. Remember from basic physics, a pulley is one of the simple machines (the others being a lever, plane and gear). This is an appropriate name because the tendons and ligaments accomplish work just like the cables and pulleys used in cranes.
Image courtesy of OrthoBullets.com
The A1 pulley is at the metacarpo-phalangeal joint, commonly called the knuckles. It’s where the proximal phalanx connects to the respective metacarpal bone. This is where trigger finger usually occurs. Those who have it here feel the pain and popping/snapping on the palmar side of the knuckle.
The A2 pulley encircles the proximal phalanx, or first finger bone, from the knuckle.
The A3 pulley is at the PIP, or proximal interphalangeal joint—the first joint from the knuckle connecting the proximal and intermediate phalanges (first and second bones of the finger). This is also a common area of trigger finger.
The A4 pulley encircles the intermediate phalanx (second bone of the finger from the knuckle).
The A5 pulley is at the DIP, or distal interphalangeal joint, the furthest joint of the finger connecting the intermediate and distal phalanges (second and third bones of the finger, from the knuckle). Although triggering can happen here, it is less common.
Since the thumb is comprised of only two phalanges, it has an A1 and A2 pulley only. Trigger finger affecting the thumb almost always occurs at the A1 pulley. Unlike the other fingers, your thumb can move in multiple planes, much like the shoulder joint. It has a unique pulley called the oblique pulley that allows it to touch the pinky, a movement called thumb opposition.
In my case, I have trigger finger in the middle and ring fingers of my right hand, mostly in the A1 and A2 pulley, and less in the A3, with the middle finger being more problematic. Pain is most pronounced in the middle of the night and upon waking, then gets better rather quickly in my case, in the first waking hour of the day. This is because as you sleep, there is less movement of the joints and less synovium produced, causing them to be stiffer.
I have the classic symptom where there is locking of those fingers when I move them from the natural, half-open relaxed hand to fully extending the fingers. As I force them past the locked angle, they snap at the A1 and A2 pulleys, then straighten out. It’s momentarily painful, but tolerable. But for some people, it’s a lot worse. All those weeks of sustained power gripping and twisting caused the flexor tendons and synovium to rub excessively against the ligaments holding them in place, causing microtears and initiating the inflammatory response.
TREATMENT FOR TRIGGER FINGER
The medical standard of care for trigger finger is corticosteroid injection below the affected ligament. This quickly knocks down the inflammation, and in some cases, symptomatic improvement happens within seconds. However, some patients report pain following the injection, and slower or no results.
Splinting is sometimes attempted. The idea is that if you immobilize the tendon, inflammation will stop and the tendon will shrink and heal, bringing things back to normal. However, this is not always the case. Sometimes inflammation takes a life of its own, and prolongs long after the injurious event ceases.
If neither corticosteroid injection nor finger splinting fail to correct the problem, surgery is an option. Direct, open surgery and percutaneous (minimal incision, special surgical tools) surgery are the two options, with direct surgery usually having better results. This is where the ligament is cut to provide more room for the tendon to move. This is possible because the adjacent ligament serves as a backup; for example, the A2 can back up A1 if A1 needs to be cut/ split apart. However, as you can imagine such destruction of a functional component means some strength and stability are sacrificed. I’m sure those having this kind of surgery lose some power in their grip.
MY TREATMENT STRATEGY
As I write this article, my trigger fingers have improved about 75%, from their worst presentation. It could be that my connective tissues are in pretty good shape; my healing capacity is strong; my injury was not very severe; or my treatment regimen is helping accelerate healing. Some sufferers don’t see such a quick pace of resolution.
Here is what I’m doing: as I mentioned, the symptoms are most pronounced in the middle of the night (when I get up to use the bathroom) and upon waking. In the middle of the night, I simply don’t move my fingers, and go back to sleep.
In the morning, I run cold water over my hand for 2 minutes, and gently move my fingers. I get the snapping, but it dissipates shortly after. I still feel some stiffness and soreness in my knuckles throughout the day, but no snapping.
I get localized cryotherapy done on my fingers. Cryotherapy is extremely cold air, as in sub-zero, for 3 minutes. The cold not only slows inflammation, it is said to cause a shock to the sensory nerves, which causes the central nervous system to respond by increasing blood flow, fibroblast activity, and nutrients to the area.
Note: the image above is a localized cryotherapy session on my hand, for a previous complaint. The red dot is not red light therapy; it is a laser thermometer the technician uses to measure my skin temperature so that it doesn’t too low (his hand is visible in the picture). Localized cryotherapy can reach temperatures of -30 degrees F.
Lastly, I apply red light therapy. I’m an advocate of this therapeutic technology and have written articles about it. Red light therapy is actually an electromagnetic waveform (600-880 nanometer wavelengths) that appears red to the human eye. It’s not the red you get from shining a light through a red lens; it’s a specific waveform in the electromagnetic spectrum generated from an LED (light-emitting diode). The device I use uses three LEDs, one of which emits a waveform closer to infrared and therefore does not appear to be red as it is invisible. The electromagnetic energy is at a frequency that gets absorbed by cell mitochondria and other structures, which can result in changed oxidative states that lead to cell signaling that initiates reparative processes, such as increased ATP production and increased membrane permeability. This lessens inflammation and stimulates healing.
I anticipate my trigger fingers to fully recover, to pre-injury status. I will continue to do these therapies, as I feel they are partly responsible for my good results.
BOTTOM LINE
Prevention is the best cure: if you know you are going to be using your hands a lot, such as starting on a do-it-yourself project involving power tools and hard gripping, know that this can cause trigger finger. Do what you can to minimize the stress to your hands—take frequent breaks; don’t overdo it/ don’t hold a power grip for more than a few seconds; and rest and stretch your hands often. Don’t rush it. Trigger finger creeps up on you, and by the time you notice it, it is too late. The presentations are different from person to person, depending on age, health, fitness and so on. I am lucky as my condition is resolving; others are not so lucky and wind up getting surgery and permanent percent loss of hand function. So make sure you keep prevention in mind. If you do get it, try the treatment methods for trigger finger described here that have worked for me.
1 note
·
View note
Link
Understand the reason for Knee Pain sooner rather than later

The knee joint lies between the thigh and the leg and works synchronously with the hip and the ankle joints to provide smooth body spread. The main components of the knee joint are The Synovial Fluid (the lubricant between the two joints), Menisci (a coil is acting like the Shock Absorber), Four large ligaments (strong ligaments preventing bones from moving or dislocating in the wrong direction), A surface of the muscle which offers additional joint stability.
0 notes
Text
The Good Thing That Came Out of the COVID-19 Pandemic

Dear Readers,
As you know, it has been a really tough 2020 so far, worldwide.
Here in the U.S. we’re still battling COVID-19; dealing with hurricanes, social unrest from racial conflict; a very divisive political situation, and here in California where I live, forest fires (about 400 burning at the same time at one point) enough to cause air quality warnings far away from the fires.
I know some of you are in Europe, Asia, Australia and the Middle East. I hope things aren’t so bad over there.
But enough of that. We must focus on living and make necessary adjustments to carry on with our lives.
There is an old Chinese saying that goes something like this: From crisis, there is opportunity (forgive me if I butchered it; no insult intended).
For the COVID pandemic, this turned out to be true: millions, if not billions of people all over the world learned that they could do a lot of things that they normally did in person, online. And for those who already did this well before COVID, they learned how to do it even better.
Shopping, buying groceries and sundries, attending school, working, holding meetings, attending church services, getting music lessons, and socializing are just some of the activities people learned how to effectively do online, thanks to being quarantined.
And, in my opinion, the most significant thing people are doing more of online, thanks to COVID: healthcare. Telemedicine, also called telehealth involves using a telephone and/or webcam to communicate with a health professional instead of in person, face-to-face for the purpose of improving one’s health. It also encompasses “consuming” health care content in digital format via the internet such as pre-recorded videos, slides, images, flow charts, white papers, and audio files and podcasts. I wrote about this over five years ago when I decided to transition my practice to a telehealth model.
Telehealth was just starting to gain traction right before COVID, but the pandemic accelerated its acceptance. The need to quarantine and social distance forced doctors and their patients to interact online, and things will never be the same (in a good way). We were hesitating at the edge of the swimming pool and COVID pushed us into that cold water, figuratively speaking.
Webcams, Internet, Wireless Connectivity and Mobile Devices Finally Transform Healthcare
The “planets aligned” for telemedicine, and very soon it’s going to be as common as buying groceries. To me, it’s overdue. I hope that telehealth not only enables healthcare for millions more lives on the planet, it will drive healthcare costs down. The cost savings to hospitals are obvious; and those savings should be passed on to the insured and paying patients. We’ll see if that happens. While I know people are used to tradition, starting from the days of the old country doctor with good bedside manners I think in 2020 and beyond, people are going to be just fine seeing their doctor online for simple and routine visits.
And the implications go beyond the actual care: telemedicine will save time and money on a macroeconomic scale, and will be actually good for the environment in more ways than one: less cars on the road (no need to drive to see your doctor); less electricity and other overhead expenses needed to keep a large building operable, less printed paper, etc.
Telehealth Is Ideal for your Average Doctor Visit
The vast majority of things that cause people to seek a doctor are non-emergency, and lifestyle related. Non-emergency means not life-threatening, or risk of serious injury. Lifestyle related means conditions that are largely borne out of lifestyle choices—high-calorie/ junk food diets; alcohol use, smoking, inadequate exercise, occupational/work-related, etc. and are usually chronic; i.e. having a long history–diabetes, high blood pressure, indigestion, arthritis, joint pain, etc. These conditions can be self-managed with proper medical guidance provided remotely via webcam. I believe that if lifestyle choices can cause illness, different lifestyle choices can reverse or minimize those same illnesses, which can be taught via telehealth.
Then there are the cases that are non-emergency, single incident: fevers, rashes, stomach aches, allergies, minor cuts and scrapes, and things of that nature. Sure, some cases of stomach aches and headaches can actually be something dire like cancer. But doctors know that such “red flag” scenarios are comparatively rare, as in less than one percent of all cases; therefore, the vast majority of them can be handled via telehealth. Besides, the doctor can decide at the initial telehealth session if the patient should come in the office, if he/she suspects a red flag.
A Typical In-Office Doctor Visit
Typically when you go to a doctor/ primary care physician, you are given a list of disorders and told to check off any that apply to you recently—stomach pain, headaches, vomiting, fever, etc.
Then, you are asked a bunch of questions related to your complaint. This is called taking your history (of your condition). The nurse practitioner or doctor may do this.
The doctor may or may not examine you, such as checking your eyes, ears, nose, and mouth; temperature, blood pressure, heart rate, lungs and so on depending on your history and complaint.
The doctor then takes this information and comes up with a diagnosis or two. You may be referred for diagnostic testing, again depending on what you came in for, such as an X-ray, MRI, ultrasound or blood test.
You may get a prescription for medications or medical device, and a printout of home care instructions, and then you’re done with your office visit.
With the exception of a physical examination involving touching and diagnostic tests, everything I just explained can be done via a telehealth visit on your computer. But as technology advances, more and more medical procedures will be performed remotely via a secure internet connection.
I believe that in the very near future, there will be apps and computer peripherals capable of doing diagnostic tests which will allow your doctor to get real-time diagnostic data during your telehealth visit. It’s already possible for blood sugar, body temperature, heart and lung auscultation and blood pressure.
Imagine wearing gloves with special, embedded sensors in the fingertips that transfer sensory information via the internet to “receiver” gloves that your doctor wears, 20 miles away. During a telehealth visit, you can palpate (feel) your glands, abdomen, lymph nodes, etc. and this sensory information is immediately felt by your doctor, as though he was right there palpating and examining you.
Or, imagine an ultrasound device that plugs into your HD port that transfers images of your thyroid to your doctor via the internet.
The possibilities are endless, and it bodes well for global health. Imagine all the people who can be helped, all over the world, via telehealth. It’s truly an exciting time in healthcare.
Telemedicine for Muscle and Joint Pain and Injuries
Every day, millions of people worldwide sustain or develop some sort of musculoskeletal (affecting muscles, joints, tendons, ligaments, bone) pain, whether it’s their low back, neck, shoulder, hip, knee, hand or other body part. If not treated right, it can become permanent or chronic.
Chronic pain, and even acute (recent onset) musculoskeletal pain can effectively be addressed via telehealth (this is the domain of my platform, Pain and Injury Doctor, and it’s my goal to help a million people worldwide eliminate their pain).
Available medical procedures for musculoskeletal conditions requiring an in-office visit such as surgery and cortisone injection are usually not the first intervention choice for such pain. Conservative care is the standard of care for the vast majority of non-emergency musculoskeletal pain and injury–an ideal application for telehealth.
For example, if you were to go to your doctor for sudden onset low back pain, you would most likely be given a prescription for anti-inflammatory medications, if not advised to just take over-the-counter NSAIDs such as Motrin, and rest. You would also be given a printout of home care instructions, such as applying ice every two hours; avoiding heavy lifting and certain body positions; and doing certain stretches and exercises. As you can imagine, such an office visit could easily be accomplished via a telehealth session. No need to drive yourself to the doctor’s office for this.
But what about chiropractic or physical therapy? You can’t get these physical treatments through your webcam. Yes, chiropractic has been shown to be effective for acute and chronic low back pain, but available studies typically don’t conclude that chiropractic for low back pain is superior or more economical than exercise instruction or traditional medical care. Same with physical therapy. However, as a “biased” chiropractor myself, I believe the benefit of spinal adjustments is not just pain relief, but improved soft tissue healing and structural alignment; two things that I believe can help reduce the chance of flare ups/ chronicity.
So get a couple of chiropractic adjustments if you can, but know that you can overcome typical back pain through self-rehabilitation as well (see my video on how to treat low back pain).

Many Types of Pain Can Be Self-Cured
Take a second to look at my logo. It looks like a red cross, but it’s actually four converging red arrows that form a figure of a person showing vitality, with arms and legs apart. The four arrows represent four pillars of self-care that my platform, The Pain and Injury Doctor, centers on:
Lifestyle modification (nutrition, mindset, healthy habits)
Using select home therapy equipment
Rehabilitative exercises
Manual therapy
These are four things that people suffering from pain are capable of doing by themselves, and sometimes with the help of a partner (manual therapy). All of the Self Treatment Videos on Pain and Injury Doctor incorporate these four elements of self-care (some are still being produced as of this writing). Isn’t this more interesting than a bottle of Motrin?
Conclusion
I will close with this: research shows that when patients are actively engaged in their healthcare, they tend to experience better health outcomes and it’s not hard to figure out why. By participating in your own health, you have “skin in the game;” i.e. you are invested in your health rather than being passive and wanting health to be “given” to you by a doctor through medicine or treatments. Mindset is what drives behavior, and those who are passive about their health are the ones who pay no attention until it’s too late—they don’t eat healthy; they don’t exercise enough; they voluntarily ingest toxins (junk food, alcohol, and smoking) and engage in health-risky behaviors. For many health conditions, by the time the primary symptom is noticeable, the disease has already set in; for example, onset of bone pain from metastasized cancer; or the first sign of pain and stiffness from knee osteoarthritis.
Being actively engaged and invested in one’s health will pay huge dividends in one’s quality of life, and longevity. So, in order for telemedicine/ telehealth to work for you, you need to have this mindset. You have to “do the work.” I can show you clinically proven self-treatment techniques to treat common neck pain, but they obviously won’t work if you don’t do them, and do them diligently.
Self-care for managing musculoskeletal pain is a natural fit for the telemedicine model of health care, which made its world debut this year. I’m excited to produce content that can help you defeat pain, without visiting a doctor’s office. I’m especially excited if your are one of the millions of people who don’t have health insurance or access to a health professional, and I am able to help improve your quality of life by showing you how to self-manage your pain.
If there is anyone you know who can benefit from this site, please share. Take care.
Dr. P
0 notes
Link
Suffering from Neck Pain?

Treatment for cervical spondylitis: Cervical discomfort is sometimes called pain in the neck. Nerves, bones, joints and muscles linked network in the cervical or cervical spine. It performs the vital role of supporting and moving the head but can occasionally be uncomfortable. visit us for more: https://painandinjurydoctor.com/
0 notes
Text
The 30 Day Pain Relief Challenge Kick Off

It’s 2021 and time to kick off the 30 Day Pain Relief Challenge!
But first I want to acknowledge what’s on everyone’s mind.
2020 began with an unexpected crisis, the COVID-19 pandemic. A new corona virus strain emerged; highly contagious and deadly for certain individuals, and for which there was no vaccine. As of this writing, over 85 million people worldwide have contracted the virus, with 1.85 million dying from it. The United States is being hit the hardest, with 20.8 million cases and 352,000 dead. The numbers are expected to spike following the holiday season, thanks to many people choosing to get together in large groups and ignoring the risk. So please, remain extra vigilant the next two weeks because chances are, there are more viruses around you than there were a month ago, ready to find a new host.
As we navigate through COVID-19 in 2021, life must still go on. I know many have been hurt economically, and their number-one priority is to find a way to get back on their feet. It is not an easy thing to do, especially if you lost your job and the life skills you possess are in an industry that has been permanently impacted by the pandemic. If this describes your situation, I sincerely hope you find a way to re-position or re-invent yourself, to get back to earning a living.
While COVID-19 dominates the news and peoples’ attention, we must not lose focus on the many other challenges life presents that also need our attention. How would you rate your health at the start of the new year? How about your energy levels and endurance?
Quarantining and social distancing have a way of discouraging exercising and promoting over-eating, a terrible combination to health. When one is restricted from going outside and going to a gym (although a gym is not necessary for staying fit, but I digress…) and constantly bombarded by news of doom and gloom, the tendency is to stay home, surf the web, and eat, more than you typically do (what else is there to do in such a scenario?). And for many, the choice is high-calorie comfort food. This can lead to unwanted weight gain, muscle atrophy, joint pain, and so on.
If you are not feeling 100%, then I encourage you to open all the emails I’ll be sending over the next 30 days—the 30 Day Pain Relief Challenge is about to kick off, and email is how it will be executed.
And what exactly is the challenge? It’s about challenging yourself to get out of your comfort zone and do all the things I will suggest in the coming days so that you can get out of pain, or significantly knock it down to levels you haven’t experienced in a long time.
The other reward may be that you will lose 10 pounds or more; will have more energy, and will notice that your mind/ thinking is clearer. This is because the methods I’ll go over target your body and all its systems; not just the area of pain. It is wholistic.
But first let me explain how you will be measuring your results. After all, pain is subjective. You need some kind of tool to quantify your improvement, so read on.
Pain, aches, discomfort or whatever you want to call it affects your health. There is mental health and physical health; both important to happiness in different ways. Your physical and mental health are impacted, even just a little and perhaps unnoticeable to you, if you have chronic pain/aches/discomfort. Less-than-optimal physical and mental health impacts quality of life. Quality of life in this sense refers to your ability to physically do what you need or want to do; whether it be your job; recreational activity such as playing golf or swimming; or activities of daily living; i.e. taking care of yourself and your personal needs.
Why You Might Have a Disability if You Have Pain
If you live with chronic pain, you likely have some degree of disability.
“Me disabled?” you might be thinking. “No way!”
The word “disability” is often misconstrued. Disability doesn’t necessarily mean “disabled” and in a wheel chair. It simply means not being able to perform a certain task without some degree of difficulty or impediment; or not being able to do it at all.
Doctors (medical examiners) who issue disability certificates or write medical-legal reports are tasked to determine the degree to which someone is disabled. Their findings determine the patient’s disability compensation from the insurance company or government agency. They use observation, physical exam procedures, diagnostic tests like X-rays and nerve conduction; and instruments to measure strength, pain perception, reflexes, coordination, and range of motion. Any deficiency is expressed as a percent disabled, and there are laws that define levels of disability.
For example, in the insurance industry, the loss of both eyes, or the loss of two limbs equates to “100% disability.” Not being able to maintain a tight grip could be rated as 20% disability if the person’s occupation requires power gripping machinery.
Disability can also be subjectively quantified using Disability questionnaires where the patient rates his/ her ability to perform certain tasks on a scale of zero to some number; and the level of pain. In some questionnaires, the zero rating means you have zero difficulty doing the task (best score), while in others the zero rating means you cannot do the task at all (worst score).
For example, the following is one section of the Oswestry Low Back Pain Disability Questionnaire. Imagine having low back pain and rating yourself (0 to 5) on your ability to lift things:
LIFTING:
0 – I can lift heavy weights without extra pain
1 – I can lift heavy weights but it gives extra pain
2 – Pain prevents me from lifting heavy weights off the floor, but I can manage if they are conveniently positioned, i.e. on a table
3 – Pain prevents me from lifting heavy weights, but I can manage light to medium weights if they are conveniently positioned
4 – I can lift very light weights
5 – I cannot lift or carry anything at all
When rating yourself, you must try to be as objective as possible—don’t over rate your ability; nor under rate it. Give each question some thought.
Then, you add up the numbers, divide it by the total number of points and multiply by 100 to get a percentage score.
If the zero rating is assigned to “full ability to do the task” (like the Oswestry above), then the score is interpreted as “percent disabled.” So, an individual with no low back disability whatsoever will score zero out of 50 and his rating will therefore be zero percent disabled; i.e. 100% functional. If his score is 30, then 30/50 x (100) = 60% disabled.
Below is an example of an Oswestry Low Back Pain Disability Questionnaire completely filled out:

In the above example, the total points out of all ten questions is 19, which is considered a Moderate disability, out of No, Mild, Moderate, Severe and Total Disability. In this case, 19/50 x 100 = 38% disabled due to low back pain. Now this person has a baseline for his condition, and can set goals to lower it each time; perhaps to 20% after a month, then 10% after three months of therapy.
If the zero rating is instead assigned to “no ability to do the task,” the score is interpreted as “percent functional.” This is how the Upper and Lower Extremity Disability questionnaires are designed. So a score of zero in this case means zero percent functional (totally disabled), and 30% means you are 30% functional (you lost 70% function in that limb).
Please note that Disability questionnaires are used as tools to quantify and set baselines for pain and functional capacity; your scores do not officially establish any disability you may have, they simply provide a more tangible interpretation of pain.
Quantifying pain/disability, even if subjective, gives you a sense of how significant it is; i.e. how much it affects your life. Secondly, it can be used as a tool to measure your improvement over time, after doing some therapy and/or rehabilitation (strength and coordination exercises). This lets you know if what you did works for your condition, and therefore, whether to continue or discontinue it.
For example, if your baseline Oswestry score was 60%, and you were prescribed some McKenzie exercises for one week and a follow- up score was 40%, it suggests that those exercises improved your condition and you should continue or progress to the next level. If it was 60% or higher, you should discontinue the exercises and try another approach.
You don’t have to see a doctor to use Disability questionnaires to subjectively assess your disability. They are fairly straightforward to use and you can download the forms from the internet (see below; I’ve done it for you).
Determine Your Pain/Disability Baseline
If you have low back pain, neck pain, shoulder pain, or lower or upper limb pain then I suggest monitoring your condition using the appropriate disability questionnaire. If you are getting therapy, your doctor should be having you fill these forms (or something similar) out each visit and going over the results with you. It’s substandard care if you don’t know if the therapy you are getting or exercises you are doing is helping; these questionnaires will prompt you to think about the change or lack of change in your functional capacity, and will help you assess your care so that you can take appropriate action.
Below you will find forms to assess any musculoskeletal pain you are having. If you wish to participate in the 30 Day Pain Relief Challenge, print out the appropriate disability questionnaire; rate your abilities as objectively as you can and calculate your score; set it aside, and be ready to fill out a new questionnaire after 30 days of diligently doing the things I will cover over the next 30 days.
My goal is for participants to experience at least a 50% improvement in their pain/ disability scores. If you have any friends who might be interested in participating, please refer them to my site, https://PainandInjuryDoctor.com and have them enter their email in the opt in form.
0 notes
Link
How many of us suffer from chronic pain, and what are the consequences?

Yes, "pain sucks!" says one who has lived with chronic pain for a long time." Suppose we don't work together as researchers, clinicians, and politicians to understand chronic pain as more than a biological nociceptive experience. In that case, we'll keep things the way they are: strained clinical relationships and a lack of efficacy in treating chronic pain. Visit https://painandinjurydoctor.com/ to learn more about chronic pain.
0 notes