Text
CREATING CITIES FOR ALL
An age friendly city
The number of older persons in the world over the age of 60 is expected to double from the current 600 million to 1.2 billion by 2025 and the vast majority of live in their homes and communities, but in areas that have not been designed with their needs and capacities in mind (World Health Organization, n.d.).

Image from National Seniors Strategy
The City of Hamilton: Becoming Age Friendly
youtube
2014: Hamilton City Council endorses Hamilton’s Age Friendly Plan
2015: The World Health Organization’s Network of Age Friendly Cities and Communities certifies Hamilton as a member of the network
In a collaborative partnership, the city of Hamilton, Ontario worked with the Hamilton Council on Aging and the Hamilton Seniors Advisory Committee to develop a plan for an age friendly city. In developing its plan, over 700 older adults and community stakeholders from various sectors were engage in and contributed to the development of the plan
Examples of initiatives towards an Age friendly city in Hamilton
· Has increased their fleet of vehicles and transitioned from buses to accessible and non-accessible vans to improve customer service.
· Installation of new pedestrian crossovers and traffic signal have Pedestrian Count Down timers.
· New and enhanced opportunities for older adults to learn how to use new information technology devices.
· Diversity training on an annual basis for 30 professionals working with older adults.
· Community paramedicine program to support older adults with chronic health conditions to remain in their own homes.
· Recreation centers offering low cost fitness and social programs for older adults.
Age friendly communities are supported by the activity theory which assumes that people age successfully if they maintain social interactions and are socially active (social and fitness programs) and the continuity theory which assumes that older individuals continue to contribute to society that same as before (volunteering, employment) (Horgan, n.d.).
References
City of Hamilton & Hamilton Council on Aging. (2019). 2014-2019 Age friendly Hamilton community progress report. Retrieved from: https://www.hamilton.ca/sites/default/files/media/browser/2019-04-05/age-friendly-2014to2019-community-progress-report.pdf
City of Hamilton. (2016). Hamilton is an age-friendly city! [Video File]. Retrieved from: https://www.youtube.com/watch?v=wLE7Y5x9r2g&feature=emb_title
City of Hamilton. (2014). Hamilton’s Plan for an Age-Friendly City. Retrieved from https://www.hamilton.ca/sites/default/files/media/browser/2016-01-20/hamilton-plan-age-friendly-strategy.pdf
Horgan, S (n.d.). Social Theories of Aging. [Power point presentation]. Retrieved from Queens University website: https://onq.queensu.ca/d2l/le/content/321165/viewContent/1868375/View
World Health Organization, (n.d.). Global Age-Friendly Cities Project Retrieved from: https://www.who.int/ageing/projects/age-friendly_cities.pdf?ua=1
Accessible design vs Universal design: What is the difference?

Image from Universal design: Center for excellence in universal design
Accessible design
Describes a site, building, facility, or portion thereof that complies with the minimum accessibility standards.
Its purpose if to meet the environmental and communication needs of the functional limitations of people with disabilities.
Accessible design aims at minimum requirements to achieve usability.
Focused on the needs of people with disabilities.
Universal design
Design of products and environments to be usable by all people, to the greatest extent possible, without the need for adaptation or specialized design.
Considers the wide spectrum of human abilities.

Image from ECS Accessibility team
Older adult who are living with mental health difficulties have what could be termed as “invisible disabilities”, it is therefore important that in the context of universal designs that we create environments that are inclusive to all. Urban planners, and different funding organizations should collaborate with health care providers such as occupational therapists in creating an environment that is usable for all.
National Center on Health, Physical Activity and Disability (n.d.). Accessible Design vs. Universal Design. Retrieved from: https://www.nchpad.org/529/2457/Designing~for~Inclusive~Play~~~Applying~the~Principles~of~Universal~Design~to~the~Playground
Bringing generations together
Older people who are most familiar to children are their grandparents particularly maternal grandmothers (Thompson & Weaver, 2016). Children are not exempt from championing ageist attitudes given that age-based prejudices permeate our cultural expectations of older adults (ibid) There is evidence to suggest that when younger people interact with older adults, they are less likely to maintain ageist stereotypes (ibid). Many communities are creating intergenerational programs to bring together children, young adults and older adults.
Intergenerational projects have considerable benefits that include:
• strengthening communities to become more age-friendly by breaking down barriers between ages and stereotypes by one age group toward another.
• teaching the young about aging while teaching the aged about youth.
• establishing relationships that help diminish the impact of declining physical and mental health on older people.
• nurturing careers in health care and a lifelong commitment to volunteerism among youth
• improving health outcomes and quality-of-life for the elderly
• building self-esteem and satisfaction for both age groups through the learning of new skills
(B.C. Care Providers Association, 2009)
Bridges Together: Everyone Benefits from Intergenerational Connections

Image from Changing aging
An example of an Intergenerational program:
In 2017, the McMaser University launched their co-generational housing program with the goal of connecting graduate student with older adults in the McMaster community for a mutually beneficial housing relationship (City of Hamilton & Hamilton Council on Aging. (2019). This is in keeping with the social exchange theory which assumes successful aging as having resources that are of value to exchange (Horgan, n.d) in this case, the older adult may benefit from companionship and assistance with chores around the house while the student gets a place to stay.
References
BC Care Providers Association. (2009). Creating caring communities: A guide to establishing intergenerational programs for schools, care facilities andcommunity groups.
City of Hamilton & Hamilton Council on Aging. (2019). 2014-2019 Age friendly Hamilton community progress report. Retrieved from: https://www.hamilton.ca/sites/default/files/media/browser/2019-04-05/age-friendly-2014to2019-community-progress-report.pdf
Horgan, S (n.d.). Social Theories of Aging. [Power point presentation]. Retrieved from Queens University website: https://onq.queensu.ca/d2l/le/content/321165/viewContent/1868375/View
Thompson, E. H., & Weaver, A. J. (2016). Making Connections: The Legacy of an Intergenerational Program. Gerontologist. https://doi.org/10.1093/geront/gnv064
0 notes
Text
CARING FOR OLDER ADULTS: WHAT SHOULD YOU KNOW?
Access to care
The fastest growing age group in Ontario are seniors who are 65 years and older and it is projected that by the year 2041, 25% of Ontario’s population will be over the age of 65 (Government of Ontario, 2017) The provincial government launched a plan recognizing the need to enhance the lives of Ontario seniors so that they can remain independent, healthy and socially connected at all stages of their lives (ibid). This in keeping with the activity theory, which posits that the way to age optimally is to remain as active as possible in three areas: physical, mental and social (Palmore, 2017). Even though this plan was launched under the previous provincial government, the current government also seems to have a focus on improving and supporting the lives of older adults as outlined below..
A plan from the current Ontario provincial government

https://budget.ontario.ca/2018/chapter-1.html
One issue that was not addressed in Ontario’s action plan for seniors was improving timely access to psychiatric care. For seniors who are living with mental illness, it is important that they have timely access to care as poor outcomes have been linked to delayed treatment (Loebach & Ayoubzadeh, 2017). The government of Ontario has been successful in implementing mandatory reporting wait times for many surgical and medical services which has led to great improvements in wait times for cataract surgery (61% reduction), hip replacements (53% reduction), coronary angiography (51% reduction) and cancer surgery (22% reduction) (ibid). Psychiatry services for mental health care in Ontario have lengthy wait times and there are no mandatory reporting wait times for these services (Loebach & Ayoubzadeh, 2017). This will be an important issue that the government will have to address as our population continues to age and as they move to integrating the healthcare system.
(Loebach & Ayoubzadeh, 2017).
28 days – Wait-time averages for various psychiatric services suggested by Canadian Psychiatric Association
45 days – Average wait for adult mental health counselling and treatment
57 days – Average wait for outpatient services for mood disorders
47 days – Average wait for inpatient services for mood disorders
References
Government of Ontario. (2017). Aging with Confidence: Ontario’s Action Plan for Seniors. Government of Ontario. Retrieved from https://files.ontario.ca/ontarios_seniors_strategy_2017.pdf
Loebach, R., & Ayoubzadeh, S. (2017). Wait times for psychiatric care in Ontario. University of Western Ontario Medical Journal.https://doi.org/10.5206/uwomj.v86i2.2027
Palmore, E. B. (2017). Auto-Gerontology: A Personal Odyssey. Journal of Applied Gerontology, 36(11), 1295–1305. https://doi.org/10.1177/0733464816648140
Robinson, K. M. (2010). Policy Issues in Mental Health Among the Elderly. Nursing Clinics of North America. https://doi.org/10.1016/j.cnur.2010.06.005
Polypharmacy and medication safety
youtube
Polypharmacy in an aging population
Polypharmacy is classified as the use of five or more prescription medications and is common among seniors and can lead to decreased compliance with medication routines and problems with drug interactions (Reason, Terner, Moses McKeag, Tipper, & Webster, 2012). The use of prescription medication increases with age partly due to multiple illnesses in older adults and it is therefore crucial that doctors effectively manage prescription medication (Reason et al., 2012). Due to physiological changes that occur as we age that change the way the body responds to and processes medication, older adults are at increased risk of adverse drug reactions (ADR) such as unsteadiness, confusion, delirium, depression and dependence (Bernier, 2017). It is essential to complete medication reviews and have discussions about side effects with older adults and because of the physiological changes associated with aging, there may be a need to change medication dosages and routines to decrease the risk of ADRs (Reason et al., 2012).
Here are some startling numbers on medication use in older adults
66.1% of seniors took 5 or more drugs; 28.0% took 10 or more drugs; and 9.3% took 15 or more drugs (2014).
39% of Canadians in long-term-care received at least one antipsychotic (2014).
Only 4% of seniors in British Columbia in residential care have a diagnosis of a psychiatric disorder, BUT 34% are on antipsychotic medications (2015).
Over 27,000 Canadian seniors had an adverse drug related reaction leading to hospitalization (2011).

The biomedical model presumes that mental illnesses like schizophrenia, major depressive disorder, attention deficit/hyperactivity disorder (ADHD), and substance use disorders are biologically based brain disorders (Deacon, 2013). Treatment mainly involves prescribing psychotropic drugs to modify/improve bio-chemical imbalances (Horgan, n.d., Module 4). When medication is prescribed to at risk populations, supervising them can be very complicated and physicians may need access to electronic medical records and to consult with a clinical pharmacist who can play an important role of completing medication reviews and educating patients and other team members about safer medication usage (Bernier, 2017). Having team members working as part of an interdisciplinary team can improve the management of patient medication. Having a trusting multidisciplinary team relationship is important for effective collaboration, communication and knowledge sharing (Kirst et al., 2017). It is also important that when individuals visit different care providers that there is a coordination of information regarding drug prescriptions otherwise there is a risk of over prescribing. An integrated care system would minimize this risk an decrease the risk of ADR for older adults with normal and abnormal mental health issues.
References
Bernier, N. F. (2017). Improving Prescription Drug Safety for Canadian Seniors. Ideas Analysis Debate Since.
Deacon, B. J. (2013). The biomedical model of mental disorder: A critical analysis of its validity, utility, and effects on psychotherapy research. Clinical Psychology Review. https://doi.org/10.1016/j.cpr.2012.09.007
Horgan, 2 (n.d.) Module 4: Models of mental health care.[Power point presentation]. Retrieved from Queen’s university website
Kirst, M., Im, J., Burns, T., Baker, G. R., Goldhar, J., O’Campo, P., … Wodchis, W. P. (2017). What works in implementation of integrated care programs for older adults with complex needs? A realist review. International Journal for Quality in Health Care. https://doi.org/10.1093/intqhc/mzx095
Reason, B., Terner, M., Moses McKeag, A., Tipper, B., & Webster, G. (2012). The impact of polypharmacy on the health of Canadian seniors. Family Practice.https://doi.org/10.1093/fampra/cmr124
SLUCare Physician Group (2016). Polypharmacy in an aging population. [Video File]. Retrieved from: https://www.youtube.com/watch?v=f0DaJhQDQ_Y
Falls
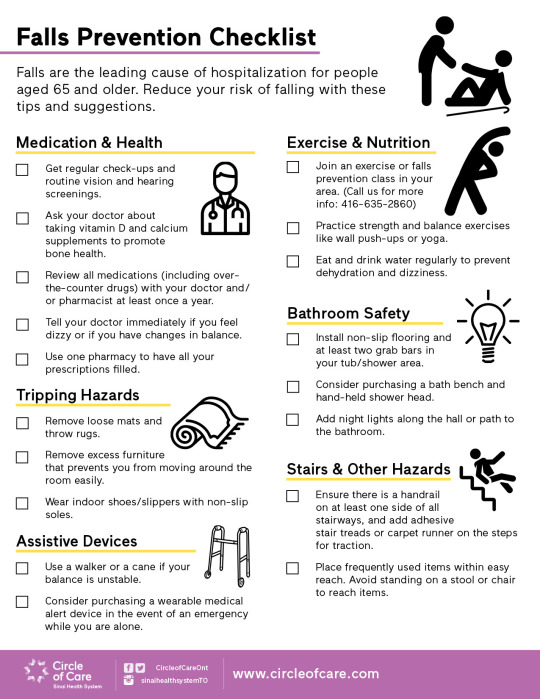
The leading cause of injury and death among older adults and a significant public health issue is falls which affect one in three adults over the age of 65 every year and 50% percent of adults over the age of 80 (Ambrose, Paul, & Hausdorff, 2013). Experiencing a fall can be devastating both physical and psychologically and could result in disability, chronic pain, loss of independence, reduced quality of life, and even death (Public Health Agency of Canada, 2014).


Images from OccupationalTherapy.com
In 2018, the province of Ontario introduced the falls prevention equipment funding policy with the purpose of providing additional funding to Long-Term Care (LTC) homes to acquire equipment including devices and assistive aids that will help prevent residents from falling or suffering injuries from falls (Ministry of health and long-term care, 2018) .With this funding comes the expectations that LTC home will maintain or improve their performance measures on residents who are falling or being transferred to the hospital for fall related incidents (ibid). With the prevalence of falls among seniors, the focus of health care providers should also be in assessing for falls risk factors and address modifiable factors. Implementing a checklist such as one below as part of a healthcare providers assessment could be a first step in decreasing the risk of falls in older adults with normal or abnormal mental health issues.
References
Ambrose, A. F., Paul, G., & Hausdorff, J. M. (2013). Risk factors for falls among older adults: A review of the literature. Maturitas.https://doi.org/10.1016/j.maturitas.2013.02.009
Ministry of Health and Long-Term Care. (2018). Falls prevention equipment funding policy . Retrieved from: http://www.health.gov.on.ca/en/public/programs/ltc/docs/Falls_Prevention_Funding_Policy.pdf
Public Health Agency of Canada. (2014). Seniors’ falls in Canada: second report. Ottawa, ON: Her Majesty the Queen in Right of Canada, as represented by the Minister of Health. Retrieved from http://www.phac-aspc.gc.ca/seniors-aines/publications/public/injury-blessure/seniors_fallschutes_aines/assets/pdf/seniors_falls-chutes_aines-eng.pdf.
0 notes
Text
“ I WANT TO STAY HOME”
Aging at home
One of the goals in the province of Ontario’s action plan was to help seniors be healthier and stay at home longer, to promote senior friendly communities that enhance well-being and participation, and to help seniors live safely, independently, and with dignity (Government of Ontario). There are more than 419,000 Canadians over the age of 65 who are living with diagnosed dementia (Public Health Agency of Canada, 2019) which is a progressive illness characterized by cognitive and functional decline making people increasingly dependent on support and susceptible to nursing home placement (Thoma-Lürken, Bleijlevens, Lexis, de Witte, & Hamers, 2018). The majority of people living with dementia want to live at home for as long as possible which is also the aim of many policies in Western Countries (ibid). The province of Ontario introduced the aging at home strategy which provides a variety of community-based services for seniors and their caregivers to allow them to stay healthy and live independently and with dignity in their home (Chazen & Jensen, 2010). Strategies like these help healthcare providers to support patients’ return home if feasible by accessing available community funded supports.

youtube
NIH Senior Health: Adult Day Care
Adult day programs are one way to support individuals living with dementia continue to live at home. Adult day programs (ADP) offer full or partial day programs for older adults living in the community including those with Alzheimer’s disease and dementia. Adult day programs that include respite for caregivers, continuous attendance, and interventions increase the well-being of both the caregivers and the participants with regard to feelings of isolation, guilt, and worry (Thompson & Fletcher, 2019) .

References
Chazen, H. & Jensen, D. (2010). Ontario News: Aging at home strategy. Retrieved from: https://news.ontario.ca/mohltc/en/2010/8/aging-at-home-strategy.html
Government of Ontario. (2017). Aging with Confidence: Ontario’s Action Plan for Seniors. Government of Ontario. Retrieved from https://files.ontario.ca/ontarios_seniors_strategy_2017.pdf
NIH Senior Health (2015). Adult Day Care. [Video File]. Retrieved from:https://www.youtube.com/watch?time_continue=4&v=ceE69chsbRE&feature=emb_logo
Public Health Agency of Canada (2019). A Dementia Strategy for Canada: Together We Aspire. Retrieved from https://www.canada.ca/content/dam/phac-aspc/images/services/publications/diseases-conditions/dementia-strategy/National%20Dementia%20Strategy_ENG.pdf
Thoma-Lürken, T., Bleijlevens, M. H. C., Lexis, M. A. S., de Witte, L. P., & Hamers, J. P. H. (2018). Facilitating aging in place: A qualitative study of practical problems preventing people with dementia from living at home. Geriatric Nursing. https://doi.org/10.1016/j.gerinurse.2017.05.003
Caring in dementia
youtube
Robert Levenson speaking about caregiving
The number of people in the world reported to be suffering from dementia is high at a reported 47.5 million people with the number expected to go up to 75.6 million by the year 2030 (Liu et al., 2017). This is very concerning considering that these individuals will need care as the disease progresses. Family caregivers who provide care for individuals with dementia experience extreme strain and increased stress because of the progression of the individual’s behavioral challenges and neuropsychiatric conditions (ibid). Care-giving for an individual with dementia has been linked to a range of adverse mental health consequences such as depression and anxiety and increased rates of mood disorders with about a third of caregivers meeting diagnostic criteria for depression (Tremont, 2011). Caregivers experiencing negative consequences from caring for persons with dementia is critical as it could determine whether an individual with dementia would have to be admitted to long-term care (Liu et al., 2017) in order to preserve the health of the caregiver. If an individual living with dementia has to move to a long-term care home, the caregiver may experience feelings of guilt (Public Health Agency of Canada, 2019).

Image from Comfort life
If the caregiver is taking care of the individual with dementia, then who is taking care of the caregiver? As part of the dementia strategy, the government is focused on improving support for family/friend caregivers through access to resources and supports. Some caregivers may not even be aware of when they need extra support or how to use or access resources that are available such as adult day programs, respite programs and education programs. Respite care provides caregivers with mental and physical relief and allows them time on their own for self-care (Public Health Agency of Canada, 2019). Some examples of caregiver support that should continue to be supported as the province moves towards integrating our healthcare system:
· In-home support by trained individuals who will come and provide companionship and assistance with activities of daily living.
· Long-term care homes can provide respite by allowing for short stays for people living with dementia.
· Adult day programs where a person living with dementia can attend and participate in activities and socialize with others and does not require for the primary caregiver to be present.
It is important to be aware of the potential for caregiver burden in caring for individuals caring for dementia. It is imperative that as providers we address not only the needs of the patient, but also the caregivers. In an integrated system providers can share resources such as First Link through the Alzheimer’s society which is focused on supporting both the person with dementia and their caregivers and have also simplified the referral process by allowing for direct referrals.
References:
Levenson, R. (2008) Caregiving. [Video File]. Retrieved from:https://www.youtube.com/watch?time_continue=2&v=KP4u3gHVz2g&feature=emb_logo
Liu, H. Y., Yang, C. T., Wang, Y. N., Hsu, W. C., Huang, T. H., Lin, Y. E., … Shyu, Y. I. L. (2017). Balancing competing needs mediates the association of caregiving demand with caregiver role strain and depressive symptoms of dementia caregivers: A cross-sectional study. Journal of Advanced Nursing. https://doi.org/10.1111/jan.13379
Public Health Agency of Canada (2019). A Dementia Strategy for Canada: Together We Aspire. Retrieved from Government of Canada website: https://www.canada.ca/content/dam/phac-aspc/images/services/publications/diseases-conditions/dementia-strategy/National%20Dementia%20Strategy_ENG.pdf
Tremont, G. (2011). Family caregiving in dementia. Medicine and Health, Rhode Island.
Having a case manager
In Ontario, various organizations use a case management approach. For example, the Home and Community Care through the Local Health Integration Care responsible for coordinating home care services in the province have case managers who disburse care of different health care providers to clients based on their needs (Government of Ontario, 2014). First Link is also another program established by the Alzheimer Society with the aim of linking individuals with dementia with available supports as early as possible in the disease process (McAiney, Hillier, Stolee, Harvey, & Michael, 2012). In a bid to streamline their referral process and to decrease the need for patients to repeat their story to different service providers, the regional geriatric program (RPG) central has a central referral process for community based Specialized Geriatric Services (Geriatric Medicine and Geriatric Psychiatry) and Behavioural Supports Ontario (Regional Geriatric Program Central (2015).

The goal of these programs is to make navigation easier for the older adults and their caregivers. Even so, there continues to be fragmentation as the coordination of services is at an organizational level or is disease or services specific. What if I am an older adult who has services through all the above programs, are my providers working together? With the introduction of Bill 74, The People’s Health Care Act, the government of Ontario’s goal is to establish a new model of integrated public health care delivery where providers are expected to work directly with one another to offer the highest quality, coordinated care, protecting patients from disruptive transitions through the system (The People’s Health Care Act, 2019). This is a change that is unlikely to take a short time to achieve, as it requires change on so many levels. Will the creation of Ontario Health Teams be the answer to easier access to health and social services and make it easier to navigate the system? This we will have to wait and see as the transformation of the Ontario health system takes place. Until then, individuals will have to continue depending on case managers that are within our current system to help them navigate the healthcare system and facilitating their desire to live at home or as long as possible..
References
Bill 74, The People’s Health Care Act. (2019). 42nd Legislature, 1st session. Retrieved from Legislative Assembly of Ontario website:https://www.ola.org/sites/default/files/node-files/bill/document/pdf/2019/2019-04/b074ra_e.pdf
Government of Ontario. (2014). Home and Community Care: How to get help for patients and seniors who need support living at home. Retrieved from:https://www.ontario.ca/page/homecare-seniors
McAiney, C. A., Hillier, L. M., Stolee, P., Harvey, D., & Michael, J. (2012). ‘Throwing a lifeline’: the role of First LinkTM in enhancing support for individuals with dementia and their caregivers. Neurodegenerative Disease Management.https://doi.org/10.2217/nmt.12.66
0 notes
Text
IS THIS NORMAL? DEPRESSION, ANXIETY AND DEMENTIA
Changes in memory

Image from Memory and Aging Center, New Jersey
Older adults are stereotyped as people for whom memory is on the decline and therefore when they forget it is not taken lightly (Cavanaugh & Blanchard-Fields, 2015). For example, if I forget an appointment or forget to take my prescribed medication, there would less likely to be concern about my cognition, but if my mother did the same, there would be questions as to whether she was experiencing cognitive changes or had cognitive impairment. This is an issue of ageism. Changes in memory are a normal part of the aging process and there are subtle effects of mild memory changes on complex activities of daily living such as managing money, transportation or medications (Parikh, Troyer, Maione, & Murphy, 2016). On the other hand, damage to the brain resulting from physical or mental health disorders can result in profound decrements in different types of memory which then makes it difficult for people to learn and remember new facts and events resulting in serious disruption of everyday life (Cavanaugh & Blanchard-Fields, 2015). The continuity theory assumes that when older adults adapt to changes related to the process of normal aging, their past life forms a foundation or any decisions they make and it is normal to retain the structure of thought, activities and habits (Naderyan et al, 2019). Many older adults simply find ways to compensate for their memory changes by increasing their use of memory strategies and aids (Parikh et al., 2016), but in many instances, older adults are stigmatized by seen as less capable and competent when they are unable to perform tasks and make use of resources in the ways they once did (Horgan, 2019).

Our society is centered largely around the needs and the values of younger people (Horgan, 2019) which can also be reflected in how our healthcare system is set-up. Our healthcare system can be sometimes difficult to navigate not only for older adults experiencing normal aging memory changes but especially for those with cognitive deficits. The system is set-up in silos and there is little to no integration particularly between the health and social service sectors because for so long they have been considered separate addressing separate issues. When integrating systems, it is important to consider the cognitive changes that are likely to affect older adults and what that means. For example, when referring a patient to another service and expecting that an older adult with cognitive impairment to remember to pick up and phone and make that call or to know where to go for their appointment. How do we create a system where it is easier for patients with normal or abnormal mental health issues to navigate? Is a system where patients have a case manager or care coordinator the answer? A system where a patient can reach out to care provider who can help them navigate the system, but with an increasingly aging population, is this sustainable in the long run?
References
Cavanaugh, J.C., & Blanchard-Fields, F. (2015). Adult development and aging, 7th ed. Adult Development and Aging, 7th Ed.
Parikh, P. K., Troyer, A. K., Maione, A. M., & Murphy, K. J. (2016). The Impact of Memory Change on Daily Life in Normal Aging and Mild Cognitive Impairment. Gerontologist. https://doi.org/10.1093/geront/gnv030
Horgan, S. (2019). AGHE 821: Special topic: Stigma. Module 2 [Course Presentation]. Retrieved from: https://onq.queensu.ca/d2l/le/content/321165/viewContent/1868385/View
Naderyan, S., Sahaf, R., Ali Akbari Kamrani, A., Abolfathi Momtaz, Y., & Ghasemzadeh, H. (2019). Papi Sh. Physical Activity Among Iranian Former Sportsmen and Athletes as Possible Evidence for Continuity Theory of Aging. Iranian Rehabilitation Journal, 17(2), 141-148.
Dementia

Image from Centre for Addictions and Mental Health
In 2015–16, just over 400,000 Canadians over the age of 65 years were reported to be living with diagnosed dementia and since this number did not include anyone under the age of 65, the number may be even higher (Public Health Agency of Canada, 2019). These numbers are expected to get worse as the number of older people increases. The World Health Organization (WHO) has identified dementia as a public priority and therefore suggested that a wider public health approach is required to improve the care and well-being of those living with dementia and their caregivers (WHO, 2012). In addition, WHO recommended that the goals of the approach should either be stated in an independent policy or guidelines or be integrated into current health, mental health or polices and guidelines for older people. They also advice that integrated and coordinated health and social care and services will be required to meet the needs of people who are diagnosed with dementia and their caregivers (WHO, 2012).

Image from Kindly care
In response, Canada’s first national strategy on dementia was presented this year with some key goals such as improving the welfare of those living with dementia and their caregivers making sure that they feel valued and supported, working together with key partners on dementia, including with people living with dementia, caregivers, and communities and developing integrated, person-centered quality care based on evidence-informed best practices across all settings. The strategy identifies three national objectives: prevent dementia, advance therapies and find a cure, improve the quality of life for people living with dementia and their caregivers (Public Health Agency of Canada, 2019). As we go into future with the expectation that there will be an even larger number of people with dementia, we hope that the plans that are outlined in the strategy will have been implemented by then.
Normal age related cognition Vs. Mild cognitive impairment Vs. Dementia

Image from www.my-dementia.com
References
Public Health Agency of Canada (2019). A Dementia Strategy for Canada: Together We Aspire. Retrieved from https://www.canada.ca/content/dam/phac-aspc/images/services/publications/diseases-conditions/dementia-strategy/National%20Dementia%20Strategy_ENG.pdf
WHO (World Health Organization). (2012). Dementia: a public health priority
Depression and anxiety
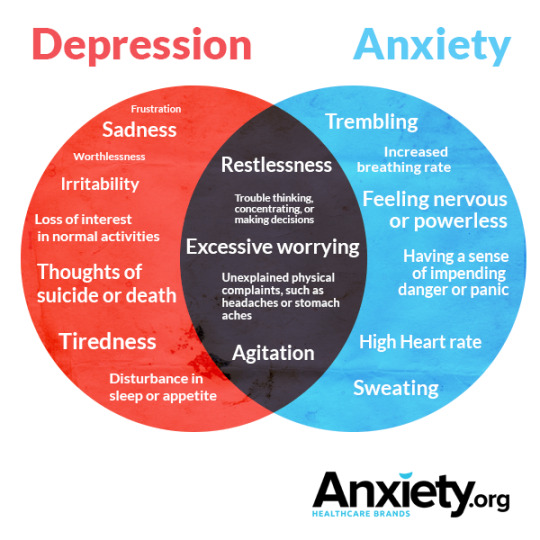
Distinguishing Depression From Anxiety In Older Adults
Even though older adults are more susceptible to experiencing depression and anxiety, there illnesses are not considered a normal part of aging and many older adults experience these issues due to having difficulties coping with physical, mental and social changes that are linked to aging. If left untreated, these issues can become more serious chronic health conditions (Horgan, n.d.).
Anxiety disorders have been found to be more common than depression and yet there is more literature on depression and a much less developed knowledge base on anxiety (Segal, Qualls, & Smyer, 2018). In 2012, a Cochrane review of collaborative care for depression and anxiety found 74 trials were focused on depression and only 5 were focused on anxiety and related disorders (Kroenke & Unutzer, 2017). Having comorbid medical disorders that produce symptoms that are the same as anxiety disorders makes it difficult for many health providers to diagnose. (Segal et al., 2018). Depression on the other hand, presents with the same symptoms in older and younger patients and when seen by their family doctor, patients will complain about symptoms such as being tired, losing weight, many unexplained health syndromes, difficulties with memory, decreased appetite, decreased social interest, decreased self-care, need to use alcohol or tranquilizers rather than identify as being depressed (Kok & Reynolds, 2017). The collaboration and integration of primary care and Mental health and addictions providers is considered as a way of improving care access for patients with mental health disorders.
youtube
Mental health matters: Depression and anxiety in older adults
Beyond the formal psycho-geriatric, acute and long-term care systems many community health services do not service adults over the age of 65 (Canadian Mental Health Association, 2009) There seems to be a separation in the treatment of neurocognitive disorders such as Alzheimer’s and dementia and other psychiatric disorders such as anxiety, depression, schizophrenia and others. Our healthcare system also seems to be set-up in segregation, and this can certainly make it difficult for older persons to navigate to try and determine where they can receive services. While working on improving the care provided to people with mental health and addictions (MH&A), primary care and mental health providers recognized the importance of collaborating given that primary care is the first and for some Canadians the only point of contact in our MH&A system (Kates et. Al, 2011). While addressing issues related to mental health, it is important to acknowledge that there are two specific groups that emerge, those who are aging and already have a mental illness and those who have mental disorders diagnosed in older age most frequently depression and anxiety disorder that are as a result of comorbidities with chronic illnesses, many losses and medication interaction (Canadian Mental Health Association, 2009).
References
Canadian Mental Health Association (2009). Focus on Seniors: Response to Every Door is the Right Door: Towards a 10-Year Mental Health and Addictions Strategy. Retrieved from https://ontario.cmha.ca/documents/focus-on-seniors-response-to-every-door-is-the-right-door-towards-a-10-year-mental-health-and-addictions-strategy/
Horgan, S. (n.d.). Normal Vs. Abnormal Health in Older Adults. [PowerPoint presentation] Retrieved from Queen’s University website: https://onq.queensu.ca/d2l/le/content/321165/viewContent/1868376/View
Kates, N., Mazowita, G., Lemire, F., Jayabarathan, A., Bland, R., Selby, P., … & Audet, D. (2011). The evolution of collaborative mental health care in Canada: A shared vision for the future. Canadian Journal of Psychiatry, 56(5), I1.
Kok, R. M., & Reynolds, C. F. (2017). Management of depression in older adults: A review. JAMA - Journal of the American Medical Association.https://doi.org/10.1001/jama.2017.5706
Kroenke, K., & Unutzer, J. (2017). Closing the False Divide: Sustainable Approaches to Integrating Mental Health Services into Primary Care. Journal of General Internal Medicine. https://doi.org/10.1007/s11606-016-3967-9
Landsberg, M., & Oliver, D. (2016). Mental Health Matters: Depression and anxiety in older adults. [Video File]. Retrieved from: https://www.youtube.com/watch?v=6oc7jf98ATg
0 notes
Text
THE 3 S: SOCIAL DETERMINANTS, STIGMA AND SOCIAL ISOLATION
Social determinants of health
There are many factors that have influence on an individual’s health and even though there maybe a general pattern of mental health and mental disorders among older adults, there may be individual difference (Segal, Qualls, & Smyer, 2018) and these have to be taken into account when working older adults with normal and abnormal mental health. Determinants of health are the wide range of personal, social, economic and environmental elements that determine individual and population health (Word Health Organization, n.d.). Factors that could impact an individual’s health include genetics, income and education level, where a person lives, the condition of their environment and the relationship they have with family and friends (ibid). Social determinants of health can also have an impact on a person’s health, and this includes income, transportation, being a new immigrant, food security, access to affordable housing and caregiver burden (Segal, Qualls, & Smyer, 2018).The biophysical model of mental disorders assumes that the origin of many of the mental illnesses are because of a combination of biological (ex. genetics, medical disorders), psychological (ex. Personality traits, coping strategies) and social factors (ex, socioeconomic status, race, culture (Segal et al., 2018). The factors in the biophysical model of mental health disorders are similar to the determinants of health which may impact older adults with normal and abnormal mental health. Even though many physicians may acknowledge that social determinants impact the health of their patients, many are uncertain of how they can intercede (Andermann, 2016). Tackling the issue of social determinants of health involves the collaboration of many sectors and various levels of government (ibid). It is critical for providers to be aware of how social determinants may impact the health of their patients. For example, if my patient does not have transportation it is unlikely they will be able to go to their appointments or go out and buy food, if they are lacking food, their health will be impacted, if they do not have secure housing, this is likely to impact their health negatively. We cannot separate social determinants and health issues, they go hand in hand and it is probable that if we address the social determinants impacting older adults, then it is likely that they will have improved health outcomes.
WHAT CAUSES HEALTH INEQUALITIES?

Image from Access Alliance
Determinants of health can have a negative impact on an individual’s ability to participate in physical or social activities. The activity theory asserts that for one to age optimally, they have to keep as active as possible in three areas: physical, mental and social (Palmore, 2017). The theory has been criticized for not recognizing the fact that society and the environment may limit the amount of activity an older person is able to maintain (ibid). Social participation and physical activity among older people is greater in industrial countries compared to developing countries thus the activity theory of aging is likely to be championed in areas where economic and social conditions enable social participation of older people (Asiamah, 2017).
youtube
The statistics in the video are based on the state of Colorado, but the fundamentals are universal and can apply to any other city, province or even country.
References
Andermann, A. (2016). Taking action on the social determinants of health in clinical practice: A framework for health professionals. CMAJ. https://doi.org/10.1503/cmaj.160177
Asiamah, N. (2017). Social engagement and physical activity: Commentary on why the activity and disengagement theories of ageing may both be valid. Cogent Medicine, 4(1), 2016–2018. https://doi.org/10.1080/2331205x.2017.1289664
Center for health progress (2013). Social determinants of health [Video File]. Retrieved from: https://www.youtube.com/watch?v=I7iSYi3ziTI
Palmore, E. B. (2017). Auto-Gerontology: A Personal Odyssey. Journal of Applied Gerontology, 36(11), 1295–1305. https://doi.org/10.1177/0733464816648140
Stigma

Image from Mental Health Commission of Canada
Successful aging has been defined as having no physical disability, subjective health and psychological well-being, social functioning and having no cognitive impairment (Bryant et al., 2012). With these reported criteria of aging, one could see how the stigma of aging is exacerbated for those who do not full-fill these expectations, especially for those who have mental illness. Many older adults are unwilling to seek mental health treatment, which may be linked to high levels of perceived public stigma toward mental illness and negative attitudes toward mental health treatment (Benjenk, Buchongo, Amaize, Martinez, & Chen, 2019). Older adults who are of racial and ethnic minority background have reported experiencing what would be considered to be triple stigma, which consists of being old, mentally ill and from being ethnic minority (Jimenez, Bartels, Cardenas, & Alegría, 2013). Many older adults have reported concerns about public stigma (Sirey, Franklin, McKenzie, Ghosh, & Raue, 2014). Some of the barriers experienced by older adults include:
· Personal and public stigma being a major barrier to seeking mental health treatment(Sirey et al., 2014).
· Physicians and providers in non-mental health settings indicate that stigma is a barrier to successful mental health referrals (Sirey et al., 2014).
· Having undiagnosed or underdiagnosed mental health conditions with primary care providers being less likely to refer older adults to mental health treatment (Benjenk et al., 2019).
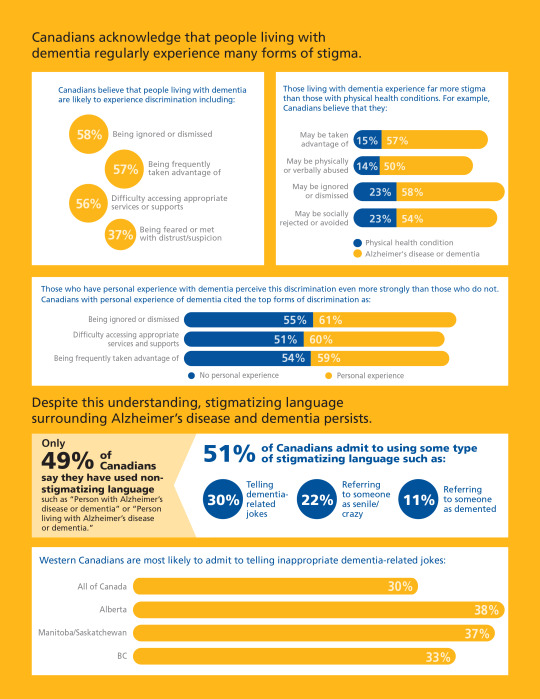
Image from Alzheimer’s Society of Canada
Given that there have long been silos throughout healthcare between psychiatry and mental health and physical health, there is clear need to integrate behavioral and mental health in health service delivery (Benjenk et al., 2019). An example of how this can be achieved include having a collaborative care model where nurses working in hospitals and primary care can screen older patients for mental health issues, recommend treatment and collaborative with psychiatrists on challenging cases (ibid). Collaborative models such as the one between the McMaster Health Team and the family physicians in Hamilton can help improve access for individuals who are afraid of being stigmatized but may already have an established relationship with their primary care provider.
References
Benjenk, I., Buchongo, P., Amaize, A., Martinez, G. S., & Chen, J. (2019). Overcoming the Dual Stigma of Mental Illness and Aging: Preparing New Nurses to Care for the Mental Health Needs of Older Adults. American Journal of Geriatric Psychiatry. https://doi.org/10.1016/j.jagp.2018.12.028
Bryant, C., Bei, B., Gilson, K., Komiti, A., Jackson, H., & Judd, F. (2012). The relationship between attitudes to aging and physical and mental health in older adults. International Psychogeriatrics / IPA. https://doi.org/10.1017/S1041610212000774
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest, Supplement. https://doi.org/10.1177/1529100614531398
Jimenez, D. E., Bartels, S. J., Cardenas, V., & Alegría, M. (2013). Stigmatizing attitudes toward mental illness among racial/ethnic older adults in primary care. International Journal of Geriatric Psychiatry. https://doi.org/10.1002/gps.3928
Sirey, J. A., Franklin, A. J., McKenzie, S. E., Ghosh, S., & Raue, P. J. (2014). Race, stigma, and mental health referrals among clients of aging services who screened positive for depression. Psychiatric Services. https://doi.org/10.1176/appi.ps.201200530
Social isolation

Image from Welbi
Older adults are at increased risk of experiencing social isolation as they are likely to report decreased contact due to a diminished personal role in the society, loss in social network ties, barriers to access due to mobility problems, a decreased ability to engage in equal social relationships due to increased frailty and loneliness (Cho et al., 2019). Adults who are socially isolated at risk for having a number of health risks, including increased blood pressure , decreased cognitive function, depression and mortality (Coyle & Dugan, 2012). In support of the activity theory of aging, it has been long been recognized that if we participate in activities such as volunteer work, hobbies, visiting friends and exercise we will experience both positive physical and mental health outcomes, reducing the risk of ill health and be protected against decline in cognition and depressive symptoms (Fox, Morrow-Howell, Herbers, Battista, & Baum, 2017) Battista, & Baum, 2017). In contrast the disengagement theory which assumes that older adults no longer have the stamina or desire to remain involved socially and that they can no longer contribute to society in a meaningful way (Horgan, 2019) could possibly perpetuate social isolation. And when older adults are isolated, they are less likely to access the healthcare system when they need it, and just like social determinants and stigma, these issues should not be ignored or thought of as a normal part of aging, because they are not!
Social isolation is considered to be modifiable factor there is definitely an opportunity to create programs that encourage social connections for older adults such as (Coyle & Dugan, 2012):
· Volunteer visiting programs
· Psychosocial group rehabilitation
· Use of technology for social networking
· Senior recreation programs
References
Cho, J. H. J., Olmstead, R., Choi, H., Carrillo, C., Seeman, T. E., & Irwin, M. R. (2019). Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging and Mental Health. https://doi.org/10.1080/13607863.2018.1481928
Coyle, C. E., & Dugan, E. (2012). Social isolation, loneliness and health among older adults. Journal of Aging and Health. https://doi.org/10.1177/0898264312460275
Fox, K., Morrow-Howell, N., Herbers, S., Battista, P., & Baum, C. M. (2017). Activity disengagement: Understanding challenges and opportunities for reengagement. Occupational Therapy International. https://doi.org/10.1155/2017/1983414
0 notes
Text
INTEGRATING CARE
Introduction

Image from SouthEast LHIN
I chose this blog topic because it closely aligns with my current work on the Health Links model of care project. The Health Links model of care is a key commitment of the Ministry of Health and Long-Term Care in integrating care for patients with complex health conditions such as those living with mental health and/or addictions and people who are frail (Ministry of Health and Long-Term Care Ontario, 2015). Health Links is also the foundation of the People’s Health Care Act; Bill 74 passed earlier this year. The purpose of this legislation is to guide the creation of Ontario Health Teams with the mandate of delivering integrated and coordinated services across health and social service sectors (The People’s Health Care Act, 2019). In delivering Health Links model of care, social and health service providers are required to use a Coordinated Care Plan (CCP) (Click on link to see the CCP). The CCP is a communication tool for patients, their families/caregivers, and providers with the focus on what is most important to the client/patient. The information obtained to complete the CCP is inclusive of physical health, mental health and addictions, assessing physical, psychological, social and spiritual supports (“Coordinated Care Plan User Guide Version 2.1,” 2018)
Bill 74, The People's Health Care Act, 2019
https://www.ola.org/en/legislative-business/bills/parliament-42/session-1/bill-74
As an occupational therapist working in Ontario, I am very interested in seeing what changes will take place in our healthcare system and how this will impact service delivery particularly for seniors with normal and abnormal mental health. Here is hoping that the new changes to the healthcare system will address some of the barriers experienced by seniors with mental health issues such as difficulty finding appropriate mental health providers, long wait lists, difficulty with transportation and mental health stigma (Segal et al., 2018).
In this blog I will be exploring various issues that impact adults with normal and abnormal mental health as they navigate the health care system.
References
Bill 74, The People’s Health Care Act. (2019). 42nd Legislature, 1st session. Retrieved from Legislative Assembly of Ontario website: https://www.ola.org/sites/default/files/node-files/bill/document/pdf/2019/2019-04/b074ra_e.pdf
Cordinated Care Plan User Guide Version 2.1. (2018). Retrieved from Health Quatlity Ontario website: https://www.hqontario.ca/Portals/0/documents/qi/health-links/ccm-coordinated-care-plan-user-guide-v2.1-en.pdf
Segal, D. L., Qualls, S. H., & Smyer, M. A. (2018). Aging and Mental Health (3rd ed.).
What is integrated care?

Image from Better Health Together. Western Sydney Integrated Care Program
Integrated care refers to bringing together inputs, delivery, management and organization of services as a way to improve access and quality of services, improve efficiency and patient satisfaction. (Plochg, Ilinca, & Noordegraaf, 2017). When looking at our current health system, health issues are being managed in a disconnected and fragmented way where there is no coordination of services across providers, settings or in the timing of the care that is provided (de Carvalho et al., 2017). This makes it difficult for patients who want to access services to know where to go and if they are accessing different services many times they have to repeat their health history due to a disjointed system. The Ontario provincial government has been exploring ways to improve health care in the province and one of the ways they have been looking to do that is through the integration of the healthcare system. The goal of integrated healthcare models is to connect health and social systems to improve the coordination of services across the different sectors and enhance patient and caregiver experience (Kirst et al., 2017).

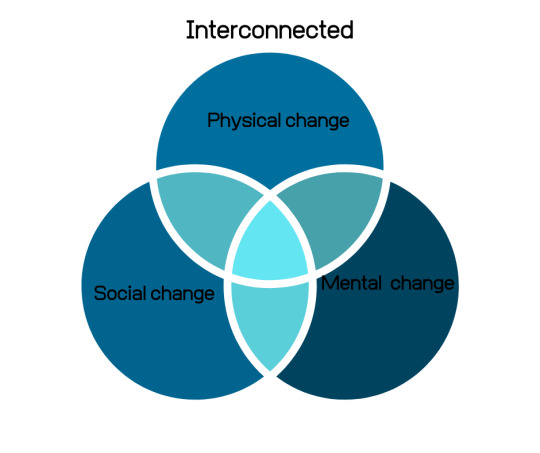
The population in Canada is increasingly aging and the care needs of aging adults will increase exponentially. As people age and experience normal mental health decline, they become more vulnerable for getting more serious mental health illnesses and living with more complex and interrelated mental, physical and social health issues (Salinda, n.d.). The complicated interactions of physical and mental health for older adults which need close supervision of a patient’s physical well-being require collaboration among providers. (Segal, Qualls, & Smyer, 2018). There is a need to have a healthcare system that is responsive to these needs and not treat them separately. In an integrated system an individual experiencing physical, mental and social change would have their services coordinated and connected across sectors. Evidence suggest that for patients with chronic and combined physical and mental health conditions, care that is integrated leads to better results and is more cost efficient (Oldham, 2013).
References
de Carvalho, I. A., Epping-Jordan, J. A., Pot, A. M., Kelley, E., Toro, N., Thiyagarajan, J. A., & Beard, J. R. (2017). Organizing integrated health-care services to meet older people’s needs. Bulletin of the World Health Organization. https://doi.org/10.2471/BLT.16.187617
Kirst, M., Im, J., Burns, T., Baker, G. R., Goldhar, J., O’Campo, P., … Wodchis, W. P. (2017). What works in implementation of integrated care programs for older adults with complex needs? A realist review. International Journal for Quality in Health Care. https://doi.org/10.1093/intqhc/mzx095
Oldham, J. (2013). Integrated care. Journal of Psychiatric Practice. https://doi.org/10.1177/146245679900300305
Plochg, T., Ilinca, S., & Noordegraaf, M. (2017). Beyond integrated care. Journal of Health Services Research and Policy. https://doi.org/10.1177/1355819617697998
Salinda, H (n.d.). AGHE 821. Module 1: Mental Health & Aging: Aging well [PowerPoint presentation] Retrieved from Queen’s University website: https://onq.queensu.ca/d2l/le/content/321165/viewContent/1968574/View
Segal, D. L., Qualls, S. H., & Smyer, M. A. (2018). Aging and Mental Health (3rd ed.).
Bringing health and social services together
Medical and mental health and addiction systems exist in separate silos, making it difficult for patients to navigate (Sebastian, 2017). As previously mentioned, our current health system is mostly fragmented; with patients having to visit different providers related to either their mental health, social or medical needs. There is always an attempt to address all these three areas of need separately but we have to recognize that unless one’s basic needs are met, good overall health is hard to achieve (Sebastian, 2017). The lack of co-ordination and the lack of a holistic approach within health and social care for older persons result in unsatisfactory care (Gustafsson, Kristensson, Holst, Willman, & Bohman, 2013). These patients often struggle with knowing whom to call when they need non-emergent help and any information provided to them could be overwhelming.
youtube
Tom Sebastian talking about Integrated care: connecting medical and behavioral care
Is a case management model the answer? A case management model is a way of intervening in a fragmented health system with the aim of improving the coordination of different services, such as health and social care (Gustafsson et al., 2013). It has been suggested that medical and behavioral health care providers should work closely with social service providers to develop comprehensive care plans (Sebastian, 2017) and to improve continuity of care (Gustafsson et al., 2013). A case management system could work especially well for those patients who are having difficulty with their memories, by having one-point person to help them navigate the health and social systems.
References
Gustafsson, M., Kristensson, J., Holst, G., Willman, A., & Bohman, D. (2013). Case managers for older persons with multi-morbidity and their everyday work - A focused ethnography. BMC Health Services Research.https://doi.org/10.1186/1472-6963-13-496
Sebastian, T. (2017, December). Integrated care: Connecting medical and behavioral care [Video file]. Retrieved from: https://www.youtube.com/watch?v=0lzmaBpBEag&t=19s
An Integrated care model: Mental health and primary care

Mental health disorders account for about a quarter of all health related disabilities in the world and more patients get treatment for mental illness in primary care than in a mental health specially setting (Kroenke & Unutzer, 2017). In Ontario in order to access psychiatry services, you have to be admitted in an inpatient setting or get a referral from your primary care physician to a psychiatrist and wait times can be long for what are considered non-urgent cases. Primary care providers and mental health and addictions (MH&A) providers have been taking steps to collaborate and integrate care either within a single service or within a team where they share care planning and decision making, have a common medical record (Kates et al., 2011). Collaborative care models involve mental MH&A providers working with primary care while an integrated care model involves MH&A workers working within and as part of primary care and patients perceive it as a routine part of their health (Kroenke & Unutzer, 2017).
An example of this type of integrated care model has been established by the Hamilton Family Health Team Mental Health Program (HFHT-MHP) where mental health providers have been integrated into over 81 offices of 150 family physicians where the focus is on providing ready access mental health care in a place that is convenient and easy to access for patients with mental health issues (Kates, McPherson-Doe, & George, 2011). Some of the benefits of the program have been, reduced wait times for first assessment, access to MH&A for adults over age of 65 who would otherwise experience lengthy wait times, early detection and treatment of MH&A problems, communication and coordination of care among providers (ibid). Integrated and collaborative models of care have the potential of improving access to care and enhancing the experience of older adults, which is one of the goals of The People’s HealthCare Act, 2019. This type of model has the opportunity of engaging models of mental health care that are not just bio-medical and focused on medication for intervention, but also psychodynamic, cognitive-behavioral, stress and coping and family systems models by including other health professionals such as psychotherapists, social workers and psychologists.
References
Kates, N., Mazowita, G., Lemire, F., Jayabarathan, A., Bland, R., Selby, P., ... & Audet, D. (2011). The evolution of collaborative mental health care in Canada: A shared vision for the future. Canadian Journal of Psychiatry, 56(5), I1.
Kates, N., McPherson-Doe, C., & George, L. (2011). Integrating mental health services within primary care settings: The hamilton family health team. Journal of Ambulatory Care Management. https://doi.org/10.1097/JAC.0b013e31820f6435
Kroenke, K., & Unutzer, J. (2017). Closing the False Divide: Sustainable Approaches to Integrating Mental Health Services into Primary Care. Journal of General Internal Medicine. https://doi.org/10.1007/s11606-016-3967-9
1 note
·
View note