Text
Depression and Anxiety Frequency in Patients Hospitalized on the Guadalajara Regional Military Hospital in the Month of April 2019
Abstract
Observe and Identify patients that presented depression and anxiety using the Hospital Anxiety Diagnosis Scale (HADS), Zung & Conde scale and ASQ 15 scale on Guadalajara Regional Military Hospital during the month of April 01st to April 30th, 2019. Methods: This is a cohort, nonexperimental, observational, prospective and longitudinal study with PubMed and NCBI articles as variables. Findings: Most patients presented anxiety, most patients had a chronic illness, depression was seen mostly in patients older than 50 years old, there was inadequate diet, lack of sleep, and low distress level.
Introduction
Depression and anxiety affect most people around the world, it is characterized by a presence of fear, loss of interest, feelings of guilt or self-esteem that are more commonly associated with sleep disorders, lack of appetite, lack of energy or difficulty concentrating. Depression can become chronic or recurrent and difficult the overall performance on a daily basis, or capacity to live day by day, in its most dangerous form it can lead often to suicide and its lowest form it can be treated with medication and professional psychotherapy [1]. Anxiety is one of the major disorders and its characterized by persistent concern during any activity or routine it is difficult to treat, and it can affect the way a person feels physically [2]. During this investigation we will observe a sample that was taken on the Guadalajara Regional Military Hospital during the month of April a sample of 56 patients presented anxiety and depression according to three scales that were applied.
HADS (hospital anxiety diagnosis scale)
The Hospital Anxiety Diagnosis Scale is an auto applicable questionnaire integrated by 14 items with subscales of seven items one for impared questions and one with pair questions for depression, the authors for this scale are Zigmund and Snaith who proposed this in 1983 and defined the concepts of anxiety and depression the objective of this scale is to identify if the patient has being tensed, concerned or frightened in any way, the 8 items that form the depression subscale are centered around anhedonia with a maximum score that binds from 0 to a 39 score, in which 0-9 score means lack of stress, 10-19 means low stress, 19 to 29 means mild stress and 30 to 39 means anxiety and severe depression.
Zung & conde scale: Its and auto applicable scale consisting of 20 phrases related to depression formed by 10 negative phrases and 10 positive phrases which relate to strong somatic symptoms and 8 cognitive items for each group contemplating the scale with two items referee to mood and other psychotic symptoms [3].
Depression and anxiety: Severe Depression: Its characterized by a combination of symptoms that interfere with capacity to work, sleep, study, eat and enjoy daily basis activities.
Dysthymic disorder: Its characterized by symptoms that is somewhat between 2 years and beyond but less severe, it incapacitates the patient and it prevents him from having a normal life accompanied by a severe depression episode during life [4-6].
Psychotic depression: Occurs during severe depression and its accompanied by some form of psychosis accompanied by delirium and hallucinations.
Seasonal Depression: Its characterized by depression that appears during Winter or times of decreased sunlight.
Bipolar Disorder: Its characterized by maniac depression disorder that its accompanied by cyclic mood swings and depression state, its often seen in patients with cancer, HIV/Aids and Parkinson.
Symptoms
Emotional
Are accompanied by guilt ideas, a severe disease, ideas of sadness never going to heal, loneliness, lack of concentration because patient will eventually die.
Physical
Difficulty eating, or basic needs, weight loss, mood swings.
Negative thoughts
This is mostly seen in older patients, self-stem problems, most cases are seen in patients over 60 years old, or below 45 years old.
Methods
This is a cohort, non-experimental, observational, prospective and longitudinal study in which scholarity was evaluated, cause of hospitalization, age, previous diseases, job and the days patient had been hospitalized.
56 patients both men and women older tan 18 years old were evaluated during this study, a random sample was taken in which every patient has the same possibility of presenting depression or anxiety [6-8]. Patients hospitalized in the women’s hospital room, the men’s hospital room, and the room that consisted of patients that had the rank of major in the Mexican armed forces or above excluding patients that belonged to Intensive care unit, using the Hospital Anxiety Diagnosis Scale, Zung & Conde Scale and ASQ-15 Scale were used during this study (Figure 1-3) [9,10].
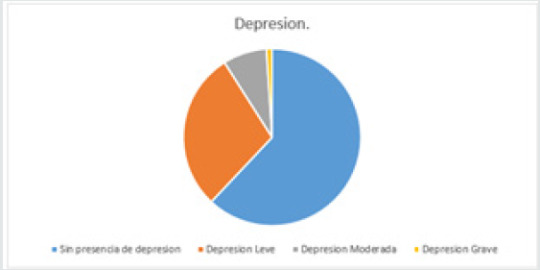
Figure 1: Patients with depression. Fuente. Zung & Conde Depression Scale. 62% of the patients did not present depression 34 patients, 16 patients had low depression 29%, also 8% of the patients had moderate depression which represented 4 patients also 2 of the patients representing 1% presented what could be considered as severe depression.
Figure 2: Most common ages seen during study. 42% of the patients presented depression were over 50 years old. 35% of the patients presented depression between 40-50 years of age. 17% of the patients that presented depression had between 30-40 years of age. 6% of the patients had between the ages of 20 to 30 years of age.
Figure 3: Patients that had some sort of stress evaluated by HADS scale.
a) 43% of the patients had lack of stress.
b) 46% of the patients had low level stress.
c) 11% of the patients had moderate stress.
d) 0% of the patients had severe stress
Justification
This study was conducted to observe what was the impact of being hospitalized and the relation it had with depression and anxiety in patient, we pretended to find viable date that allowed us to expose the hospital environment and the presence of disease, anxiety and depression (Figure 4) [11,12].
Figure 4: Most common diseases (12 patients didn’t have an illness):
a) Hypertension: 16
b) Diabetes Mellitus:12
c) Renal Insufficiency: 4
d) Ulcerative Colitis:1
e) Hepatic Cirrosis: 3
f) Lung Cancer: 3
g) Cervical Cancer:1
h) Fractures: 4
Results
Figure 1 Patients with depression. Fuente. Zung & Conde Depression Scale. 62% of the patients did not present depression 34 patients, 16 patients had low depression 29%, also 8% of the patients had moderate depression which represented 4 patients also 2 of the patients representing 1% presented what could be considered as severe depression (Figure 5,6).
Figure 5: Civil Status:
a) Married: 54%
b) Separated: 35%
c) Single: 11%
Figure 6: Patients that presented anxiety
a) 64% presented anxiety 35 patients
b) 36% did not present anxiety 21 patients
c) 86% No
d) 14% Yes
Conclusion
Referred to this subject we understand this two disorders are preventable and the patient if its treated and seeks help with time he can change his daily habits, our suggestions are that a stable lifestyle with a well-balanced diet consisting of fruit, vegetables, meat, daily exercise, stable relationships with family and friends, alongside no work stress, in addition to a good mental stability can lead to a good life and to prevent this type of disorders also to prevent chronic illness which were seen during this study on most patients that indicated feeling anxious or depressed, if they are in this state also to take medication on time and with the help of family members and friend.
a) We observe most patients presented a low depression level
b) Most patients presented anxiety
c) Most patients had a chronic illness
d) Patients over 50 years old presented higher depression levels
e) Most patients were married
Most patients had low level stress level.
Read More About This Article Click on Below Link:
https://lupinepublishers.com/neurology-brain-disorders-journal/fulltext/depression-and-anxiety-frequency-in-patients-hospitalized-on-the-guadalajara-regional-military-hospital-in-the-month-of-april-2019.ID.000171.php
Read more Lupine Publishers Google Scholar Articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=X9lN_1AAAAAJ&citation_for_view=X9lN_1AAAAAJ:PcT55Ow6fAIC
#Lupine Publishers#Lupine Publishers Group#Online Journal of Diabetes and Obesity#Journal of Neurology and Brain Disorders#Journal of Neurology
0 notes
Text
Blissful Thanksgiving!!!

Greetings from OJNBD!!
Wishing you a harvest of blessings, good health and good times. Happy Thanksgiving day!
#Lupine Publishers#Lupine Publishers Group#OJNBD#online journal of neurology and brain disorders#Journal of Neurology#Journal of Neurosurgery#Journal of Neurology and Brain Disorders
0 notes
Text
Lupine Publishers| Swiss Cheese Pattern a Harbinger of Dementia or an Incidental Finding in an Unusual Case?
upine Publishers| Journal of Neurology and Brain Disorders

Abstract
Go to
Dilated Virchow Robin (VR) spaces are pial- line fluid filled structures which surround the walls of small penetrating vessels. In a severe form they develop a swiss cheese pattern or a cribriform pattern in straitum which may predispose to cognitive impairment. We report a patient with change in personality associated with diffuse atrophy, hypometabolism, microbleeds and swiss cheese striatum which is rare.
Keywords: Swiss cheese pattern; Dementia; Virchow robin space
Abbreviations: VR: Virchow Robin; MRI: Magnetic Resonance Imaging; FLAIR: Fluid Attenuated Inversion Recovery; CSF: Cerebrospinal Fluid
Introduction
Go to
Virchow Robin (VR) spaces are pial-lined, fluid filled, structures which surround the walls of small penetrating arterioles and venules as they course from subarachnoid space to brain parenchyma. These often appear in basal ganglia and centrum semi vale and are reflected in Magnetic Resonance Imaging(MRI) brain as hypointense in T1-weighted images, hyperintense on T2-weighted and hypointense on Fluid Attenuated Inversion Recovery(FLAIR) images, thus distinguished from pathological white matter lesions by persistent is intensity to Cerebrospinal Fluid(CSF) on all sequences, lack of enhancement and sharply defined margins. Dilated VR spaces can appear on neuroimaging as single enlarged cavity(up to 2cm in diameter) or may appear as hundreds of bilateral 1-2 mm foci in the basal ganglia, subcortical white matter and sub insular area lateral to lentiform nucleus, a pattern sometimes referred to as etat crible or cribriform or Swiss cheese striatum.
Though a common finding in elderly population, studies have shown that enlarged VR spaces are a marker of small vessel disease and associated with incident dementia and depression. Multiple mechanisms for giant VR spaces have been described which include mechanical trauma due to CSF pulsation, fluid exudation due to abnormalities of the vessel wall abnormality and ischemic injury to perivascular tissue causing ex vacuo effect. The precise function of VR spaces is not completely understood. They are believed to serve as a lymphatic of brain also known as the glymphatic system whereby CSF exchanges with the interstitial fluid within the brain parenchyma, including clearing the interstitial solutes such as betaamyloid.
Epidemiology
Dilated Virchow robin spaces were described Durant-Fardel in 1843. In a study of healthy participants using high resolution images prevalence was 1.6%. In radiological studies involving patients VR spaces were found in 3% patients under 20 years of age. In addition, studies have shown higher rate of cognitive decline with dilated VR spaces, which is intriguing, and its elucidation may improve the complex understanding of role of vascular alterations and higher risk of cognitive decline [1]. Furthermore, dilated VR spaces have different topographically patterns in microangiopathies like cerebral amyloid angiopathy where they are mostly seen in centrum semiovale and hypertensive angiopathy where they are predominantly seen in basal ganglia [2]. To date, longitudinal data with regard to significance of dilated VR spaces in healthy older adults is scarce. However small number of studies have shown association with development of new onset dementia. Prevalence is more in vascular dementia compared to Alzheimer’s dementia and healthy controls.
Clinical presentation
Increased basal ganglia or centrum semiovale perivascular spaces have been associated with worse nonverbal reasoning and visuospatial cognitive abilities. Various clinical presentations have been reported which include parkinsonism, hemisensory symptoms and in addition depending on the size of the VR space causing mass effect. Dilated VR spaces have been associated with vascular dementia and also have been correlated with reduced cognitive function [3]. Thus for a clinician differential diagnosis of dilated spaces should always be considered in view of multiple mimics like multiple lacunar infarctions, cryptococcosis, multiple sclerosis, mucopolysaccharidosis, cystic neoplasms and arachnoid cysts. Knowledge of their signal changes in neuroimaging may help in differentiating these lesions from dilated VR spaces.
Clinical case
Figure 1: (A) T1-weighted MRI showed bilateral frontal and anterior temporal lobe atrophy; (B, C) T2/FLAIR hyperintensities showing confluent foci in the bilateral deep and periventricular white matter, and prominent perivascular spaces in bilateral basal ganglia suggestive of a swiss cheese pattern.
Figure 2: (A) SWI sequence showing multiple foci of blooming in bilateral basal ganglia, thalami, cerebral hemispheres, brainstem and left cerebellar hemisphere. (B) Positron emission tomography (PET) MRI brain showing hypometabolism in bilateral parietal lobes, medial and anterior temporal lobes and orbitofrontal cortex. (C) PET MRI brain showing hypometabolism in dilated VR spaces in the striatum.
60 year old female, presented with the 5 years history of change in personality associated with behavioural disturbances in the form of getting angry for trivial issues and screaming at family members, trying to pick things in front of her, telling that insects are crawling on her clothes. Since last 2 years caregivers report history of fluctuating restlessness, wandering aimlessly, muttering to self, disinhibited behaviour and apathy. Since last 6 months she had lost concern for family members, started becoming slow in her activities especially walking and became completely dependent for her daily activities of living. There was also history of incontinence without any concern. There was no history of food faddism, utilization behaviour, myoclonic jerks, seizure, recurrent falls, bulbar symptoms, weight loss, change in bowel habits. Patient was diagnosed case of hypertension since 5 years and was on medications. She was not cooperative for mental status examination. Her physical examination revealed mild bradykinesia, brisk reflexes, mildly wide based gait with reduced clearance and primitive reflexes were present. Blood investigation were all normal. MRI brain T1-weighted image (Figure 1A) showed bilateral frontal and anterior temporal lobe atrophy, confluent foci of T2/FLAIR hyperintensities (Figure1B and C) in the bilateral deep and periventricular white matter and T2 weighted image showed prominent perivascular spaces in bilateral basal ganglia suggestive of a swiss cheese pattern. In addition, there were multiple foci of blooming on Susceptible Weighted Images (SWI) (Figure 2A) are seen in the bilateral basal ganglia, thalami, cerebral hemispheres, brainstem and left cerebellar hemisphere. Positron Emission Tomography (PET) MRI brain (Figure 2B) showed hypometabolism in bilateral parietal lobes, medial and anterior temporal lobes and orbitofrontal cortex. PET MRI brain (Figure 2C) showed hypometabolism in dilated VR spaces in the striatum. Final diagnosis of mixed dementia associated with swiss cheese brain syndrome was considered and patient was managed as per standard guidelines for dementia. In addition to Vascular dementia, more commonly mixed dementia includes Alzheimer’s dementia, however patient had predominant features suggestive of Frontotemporal dementia which less commonly associated with microbleeds and dilated VR spaces as seen in this patient. Whether it is a combination of multiple dementias contributed by enlarged VR spaces will remain unanswered.
Conclusion
Go to
Dilated VR spaces may be an either an incidental finding on MRI without any pertinent manifestations. However, evidence suggests that these may be predisposing risk factor for cognitive impairment. Whether estimating the burden of perivascular spaces may help in predicting development of cognitive impairment and type of dementia, remains undetermined and may require further research.
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publishers Group#OJNBD Journal#Online Journal of Neurology and Brain Disorders#Journal of Neurology#Journal of Neurosurgery
0 notes
Text
Lupine Publishers| Antiaging, Cognition and Anti-Inflammatory Potential of the Biofield Energy Treatment in Vitamin D3 Deficiency Diet (VDD) Induced Sprague Dawley Rats
Lupine Publishers| Journal of Neurology and Brain Disorders

Abstract
A proprietary formulation was designed that consist of minerals (zinc, magnesium, iron, calcium, selenium, and copper), vitamins (pyridoxine HCl, cyanocobalamin, ascorbic acid, alpha tocopherol, and cholecalciferol), Panax ginsengextract, β-carotene, and cannabidiol isolate. The present study was aimed to evaluate the impact of Consciousness Energy Healing Treatment (the Trivedi Effect®) on a novel test formulation in male Sprague Dawley (SD) rats, fed with vitamin D3 deficiency diet (VDD) for antiaging/cognitive and anti-inflammatory activities. The test formulation was divided into two parts. One part was denoted as the untreated test formulation without any Biofield Energy Treatment, while the other part was defined as the Biofield Energy Treated sample, which received the Biofield Energy Healing Treatment by renowned Biofield Energy Healer, Mr. Mahendra Kumar Trivedi. The level of Klotho protein (anti-aging biomarker) in cerebro-spinal fluids (CSF) was significantly increased by 44.2%, 92.0%, 44.2%, and 43.1% in the Biofield Energy Treatment per se to animals from day -15 (G6), Biofield Energy Treated test formulation from day -15 (G7), Biofield Energy Treatment per seplus Biofield Energy Treated test formulation from day -15 (G8), and Biofield Energy Treatment per seanimals plus untreated test formulation (G9) groups, respectively as compared to the disease control group (G2). The level of β-endorphin in CSF (cognition, pain and inflammation biomarker) was significantly increased by 418.4%, 1155.7% (p≤0.01), 890.4% (p≤0.01), 351%, and 566.7% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the G4. Moreover, serotonin level in CSF was increased by 94.8%, and 63.4% in the G6 and G9 groups, respectively as compared to the G4. The level of 1, 25 (OH)2D3 in CSF was significantly increased by 61.8%, 33.4%, 61.5%, 64.5%, and 30.6% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the VDD induced group (G2). Further, the level of c-reactive protein (CRP, inflammation biomarker) in serum was reduced by 21.2%, 23.1%, 19.8%, 22.4%, and 23.1% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the G2 group. Altogether, results suggested that the Biofield Treated test formulation and Biofield Energy Treatment per se significantly increased antiaging, cognitive, and anti-inflammatory biomarkers that could be helpful in various aging/psychiatric or inflammatory disorders. Thus, the results showed a significant slowdown of disease progression and all other disease-related complications/symptoms in the preventive Biofield Energy Treatment group per seand the Biofield Energy Treated Test formulation groups (viz. G6, G7, G8, and G9) as compared to the disease control group.
Keywords: Biofield Treatment;antiaging; The Trivedi Effect®;klotho;β-endorphin;serotonin; Vitamin D3 deficiency diet;calcitriol
Introduction
Deficiency of vitamin D3 is directly linked to various health problems like osteoporosis, cognitive decline, cardiovascular disease, depression, diabetes, hypertension, and cancer [1,2]. Vitamin D is very essential for bone health in adults and children. Its sufficient concentration prevents osteomalacia, muscle weakness, and protect fractures. The processes by which intake of vitamin D3 like synthesis through skin via UV-rays and absorption from foods become less efficient with age [3]. Hence, hypovitaminosis of vitamin D3 is more prevalence worldwide [4]. Based on this situation authors constructed the current research work to evaluate the impact of Consciousness Energy Healing Treatment on aging after induction of Vitamin D3Deficiency Diet (VDD) in Sprague Dawley rats. The newly formulated test formulation, which is a combination of multiple minerals (iron, copper, zinc, magnesium, calcium, and selenium), vitamins (ascorbic acid, cholecalciferol, pyridoxine HCl, alpha tocopherol, and cyanocobalamin), panax ginseng extract, and cannabidiol isolate. Each component of this test formulation commonly used as nutraceutical supplement [5-8]. Biofield Therapy (or Healing Modalities) is one of the approach of Complementary and Alternative Medicine (CAM) therapies now considering as the first-line model of treatment against several disorders. Based on the obtained data from National Health Interview Survey (NHIS) 2012, reported that most of the Americans used the dietary supplement as complementary health approaches than conventional medicine therapy. Besides, The National Center of Complementary and Integrative Health (NCCIH) has recognized and accepted Biofield Energy Healing as a CAM health care approach in addition to other therapies, medicines and practices such as Tai Chi, Qi Gong, Ayurvedic medicine, Rolfing structural integration, deep breathing, yoga, natural products, chiropractic/osteopathic manipulation, massage, meditation, relaxation techniques, aromatherapy, acupuncture, progressive relaxation, hypnotherapy, healing touch, mindfulness, special diets, naturopathy, homeopathy, guided imagery, acupressure, traditional Chinese herbs and medicines, pilates, movement therapy, Reiki, essential oils, cranial sacral therapy and applied prayer.
Human Biofield Energy has subtle energy that can work effectively [9]. CAM therapies have been practiced worldwide with reported clinical benefits in different health disease profiles [10]. This energy can be harnessed and transmitted by individuals into living and non-living things via the process of Biofield Energy Healing. Biofield Energy Treatment (the Trivedi Effect®) has been published in numerous peer-reviewed science journals with significant outcomes in many scientific fields such as cancer research [11, 12], microbiology and biotechnology [13-15], pharmaceutical science [16-19], agricultural science [20-22], materials science [23-25], dietary supplement [26,27], skin health [28,29], human health and wellness. The planned to evaluate the impact of the Biofield Energy Healing Treatment (the Trivedi Effect®) on the test formulation for antioxidant action concerning lipid peroxidation, antioxidant activity using standard assays.
Materials and Methods
Chemicals and reagents
Calcitriol, pyridoxine hydrochloride (vitamin B6), beta carotene (retinol, Provit A), zinc chloride, and magnesium (II) gluconate were purchased from TCI, Japan. Copper chloride, calcium chloride, cyanocobalamin (vitamin B12), cholecalciferol (vitamin D3), sodium carboxymethyl cellulose (Na-CMC), vitamin E (Alpha-Tocopherol), and iron (II) sulfate were procured from Sigma-Aldrich, USA. Sodium selenate and ascorbic acid were obtained from Alfa Aesar, India. Panax ginsengextract and cannabidiol isolate were obtained from Panacea Phytoextracts, India and Standard Hemp Company, USA, respectively. Other chemicals used in this experiment were analytical grade procured from India.
Experimental animals
Randomly breed male Sprague Dawley (SD) rats with body weight ranges from 200 to 300 gm were used in this study. The animals were purchased from M/s. Vivo Bio Tech, Hyderabad, India. Animals were randomly divided into nine groups based on their body weights consist of 6 animals of each group. They were kept individually in sterilized polypropylene cages with stainless steel top grill having provision for holding pellet feed and drinking water bottle fitted with stainless steel sipper tube. The animals were maintained as per standard protocol throughout the experiment.
Consciousness energy healing strategies
The test formulation was divided into two parts. One part of each ingredient was considered as the untreated test formulation, where no Biofield Energy Treatment was provided. Another part of each ingredient was received Biofield Energy Treatment by Mr. Mahendra Kumar Trivedi (the Trivedi Effect®) under laboratory conditions for ~3 minutes in the research laboratory, Dabur Research Foundation, New Delhi, India. Besides, three group of animals were also received Biofield Energy Treatment under laboratory conditions for ~3 minutes. The energy transmission was done without touching the samples or animals. Similarly, the control samples were subjected to “sham” healer under the same laboratory conditions for ~3 minutes for comparison purposes. The “sham” healer did not have any knowledge about the Biofield Energy Treatment. After that, the Biofield Energy Treated and untreated test formulations were kept in the similar sealed condition and used as per the study plan. The Biofield Energy Treated animals were also be taken back to experimental room for further proceedings.
Experimental procedure
Seven days after acclimatization, animals were randomized and grouped based on body weight. All the animals except G1 were fed with Vitamin D3 deficient diet (VDD) from day -12 to till the end of the experiment. To induce CYP24A1 expression, to accelerate the catabolism of endogenous vitamin D3, the rats (Group G2 to G6) were receive intraperitoneal injections of 40 ng of 19-nor-1,25- dihydroxyvitamin D2 (Paricalcitol) on days -12, -10, -8, -6, -4, -2, day 1, 3 and 5. Group G1 to G5 animals were dosed with respective formulations from Day 1 to till the end of the experiment. However, Group G6 were not be dosed. Animals (50% of the animals from each group) were kept for overnight fasting on Day 56 (Tentative). However, remaining 50% animals were dosed with respective formulations and were kept for fasting on Day 57 (Tentative) next day animals were bled and serum was separated for the estimation of C-reactive protein (CRP). After bleeding, cerebrospinal fluid (CSF) were collected by standard in-house method using stereotaxic instrument for the estimation of KLOTHO, Beta-Endorphin, Serotonin, and 1, 25 (OH)2 D3 by ELISA method.
Estimation of klotho protein, beta-Endorphin, serotonin and 1, 25 (Oh)2 D3 In cerebrospinal fluids (CSF)
The Klotho protein expression was determined using Rat Klotho ELISA Kit in rat’s CSF in according to the manufacturer’s instructions [30].
Assessment of Serum C-reactive protein (CRP)
Serum C-reactive protein were estimated using standard ELISA assay followed by manufacturer instructions. Serum was collected from all the animals after completion of the experiment was examined for level of CRP. The detailed test procedure of the identification of serum C-reactive protein were performed using manufactured instructions as per individual ELISA kit. The CRP level was tested using CUSABIO, ELISA Assay Kit as per manufacturer instructions.
Statistical analysis
The data were expressed as mean ± Standard Error of Mean (SEM) and subjected to statistical analysis using Sigma Plot (Version 11.0). For multiple comparison One-way analysis of variance (ANOVA) followed by post-hoc analysis by Dunnett’s test and for between two groups comparison Student’s t-test was performed. The p≤0.05 was considered as statistically significant.
Results and Discussion
Estimation of klotho protein in Cerebrospinal fluids (CSF)
Figure 1: The effect of the test formulation on the level of Klotho protein in cerebrospinal fluids (CSF) in male Sprague Dawley rats. G: Group; G1: Normal control (0.5% CMC); G2: Disease control (VDD: Vitamin D3 deficient diet + 0.5% CMC); G3: Reference item (VDD + Calcitriol); G4: (VDD + untreated test formulation); G5: (VDD + Biofield Energy Treated test formulation); G6: (VDD + Biofield Energy Treatment per se to animals from day -15; G7: (VDD + Biofield Energy Treated test formulation from day -15); G8: (VDD + Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15), and G9: (VDD + Biofield Energy Treatment per se animals plus untreated test formulation). Values are expressed as mean ± SEM, n=6 in each group.
The impact of the test formulation on the expression of Klotho protein in Cerebrospinal Fluids (CSF) is shown in Figure 1. The level of Klotho protein in the normal control (G1) group was 419.71 ± 75.81 pg/mL and it was decreased by 41.52% in the disease control (G2) group (245.43 ± 69.12 pg/mL) induced by vitamin D3 Deficiency Diet (VDD). The positive control (calcitriol) showed 95.46% increase the level of Klotho protein expression as compared to the G2 group. Further, expression of Klotho protein was significantly increased by 9.31%, 44.24%, 91.97%, 44.24%, and 43.07% in the untreated test formulation (G4), Biofield Energy Treatment per se to animals from day -15 (G6), Biofield Energy Treated test formulation from day -15 (G7), Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15 (G8), and Biofield Energy Treatment per se animals plus untreated test formulation (G9) groups, respectively as compared to the G2 group. Further, the level of Klotho protein was significantly increased by 31.95%, 75.61%, 31.95%, and 30.88% in the G6, G7, G8, and G9 groups, respectively as compared to the untreated test formulation group (G4). Klotho protein acts as an anti-aging biomarker. Klotho gene is recognized as a putative aging-suppressor gene, has a great interest and provides more useful information of the aging process. Data obtained from one experiment in mice reported that the overexpression of the Klotho gene extends the lifespan, and mutations to the klotho gene which shorten the lifespan [31,32].
Assessment of CSF biomarker - β-endorphin
The level of β-endorphin in the normal control group (G1) was 44.48 ± 7.87 pg/mL and it was significantly (p≤0.01) decreased by 69.51% in the disease control (G2) group (13.56 ± 4.36 pg/mL) induced by vitamin D3 Deficiency Diet (VDD). Besides, secretion of β-endorphin was significantly increased by 75.59%, 325.37% (p≤0.001), 235.47% (p≤0.001), 52.80%, and 125.88% in the Biofield Energy Treated test formulation (G4), Biofield Energy Treatment per se to animals from day -15 (G6), Biofield Energy Treated test formulation from day -15 (G7), Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15 (G8), and Biofield Energy Treatment per se animals plus untreated test formulation (G9) groups, respectively as compared to the G2 group. Further, the level of β-endorphin was significantly increased by 418.74%, 1156.64% (p≤0.01), 891.07% (p≤0.01), 351.42%, and 567.32% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the untreated test formulation group (G4). β-endorphin is an endogenous opioid neuropeptide and peptide hormone, considered as cognition, pain and inflammatory biomarker Figure 2. It is produced in certain neurons within the central nervous system and peripheral nervous system to relieve pain when bound to their mu-opioid receptors [33].
Figure 2: The effect of the test formulation on the level of β-endorphin in cerebrospinal fluids (CSF) in male Sprague Dawley rats. G: Group; G1: Normal control (0.5% CMC); G2: Disease control (VDD: Vitamin D3 deficient diet + 0.5% CMC); G3: Reference item (VDD + Calcitriol); G4: (VDD + untreated test formulation); G5: (VDD + Biofield Energy Treated test formulation); G6: (VDD + Biofield Energy Treatment per se to animals from day -15; G7: (VDD + Biofield Energy Treated test formulation from day -15); G8: (VDD + Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15), and G9: (VDD + Biofield Energy Treatment per se animals plus untreated test formulation). Values are expressed as mean ± SEM, n=6 in each group. ***p≤0.001 vs. G2, ##p≤0.01 vs. G4, and **p≤0.01 vs. G1.
Estimation of 5-hydroxy tryptamine (Serotonin) in CSF
The level of serotonin or 5-hydroxy tryptamine (5-HT) in the normal control group (G1) was 7.29 ± 1.03 ng/mL and it was significantly (p≤0.05) decreased by 58.02% in the disease control (G2) group (3.06 ± 0.93 ng/mL) induced by vitamin D3 Deficiency Diet (VDD). Besides, secretion was increased by 29.41% and 17.32% in the positive control (G3) and Biofield Energy Treatment per se to animals from day -15 (G6) groups, respectively as compared to the G2 group. Further, the level of serotonin was increased by 16.30%, 95.11% and 63.59% in the G5, G6, and G9 groups, respectively as compared to the untreated test formulation group (G4). Serotonin (5-HT) in neuron and neurotransmitter loss leads to aging. The incomplete neurodegenerative processes and serotonergic neurotransmission also leads to aging process [34]. In this experiment, the Biofield Energy Treated test formulation had significantly improve the level of serotonin, which might reduce aging process Figure 3.
Figure 3: Effect of the test formulation on the level of serotonin in cerebrospinal fluids (CSF) in male Sprague Dawley rats. G: Group; G1: Normal control (0.5% CMC); G2: Disease control (VDD: Vitamin D3 deficient diet + 0.5% CMC); G3: Reference item (VDD + Calcitriol); G4: (VDD + untreated test formulation); G5: (VDD + Biofield Energy Treated test formulation); G6: (VDD + Biofield Energy Treatment per se to animals from day -15; G7: (VDD + Biofield Energy Treated test formulation from day -15); G8: (VDD + Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15), and G9: (VDD + Biofield Energy Treatment per se animals plus untreated test formulation). Values are expressed as mean ± SEM, n=6 in each group. *p≤0.05 vs. G1.
Evaluation of 1, 25 (OH)2 D3 in CSF
The level of 1, 25 (OH)2 D3 in the normal control group (G1) was 1.67 ± 0.78 ng/mL and it was significantly decreased by 53.89% in the disease control (G2) group (0.77 ± 0.07 ng/mL) induced by vitamin D3 Deficiency Diet (VDD) is shown in Figure 4. The positive control group (G3) had significantly increased the level of 1, 25 (OH)2 D3 by 105.19% compared to the G2 group. Besides, the level of 1, 25 (OH)2 D3 was significantly increased by 31.17%, 62.34%, 33.77%, 62.34%, 64.94%, and 31.17% in the Biofield Energy Treated test formulation (G4), Biofield Energy Treated test formulation (G5), Biofield Energy Treatment per se to animals from day -15 (G6), Biofield Energy Treated test formulation from day -15 (G7), Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15 (G8), and Biofield Energy Treatment per se animals plus untreated test formulation (G9) groups, respectively compared to the G2 group. Further, the level of 1, 25 (OH)2 D3was also significantly increased by 23.76%, 23.76%, and 25.74% in the G5, G7, and G8 groups, respectively.
Figure 4: The effect of the test formulation on the level of 1, 25 (OH)2 D3 in cerebrospinal fluids (CSF) in male Sprague Dawley rats. G: Group; G1: Normal control (0.5% CMC); G2: Disease control (VDD: Vitamin D3 deficient diet + 0.5% CMC); G3: Reference item (VDD + Calcitriol); G4: (VDD + untreated test formulation); G5: (VDD + Biofield Energy Treated test formulation); G6: (VDD + Biofield Energy Treatment per se to animals from day -15; G7: (VDD + Biofield Energy Treated test formulation from day -15); G8: (VDD + Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15), and G9: (VDD + Biofield Energy Treatment per se animals plus untreated test formulation). Values are expressed as mean ± SEM, n=6 in each group.
Effect of the test formulation on serum CRP level
Figure 5: The effect of the Test formulation on change in serum CRP level in vitamin D3 deficiency diet-induced Sprague Dawley rats. G: Group; G1: Normal control (0.5% CMC); G2: Disease control (VDD: Vitamin D3 deficient diet + 0.5% CMC); G3: Reference item (VDD + Calcitriol); G4: (VDD + untreated test formulation); G5: (VDD + Biofield Energy Treated test formulation); G6: (VDD + Biofield Energy Treatment per se to animals from day -15; G7: (VDD + Biofield Energy Treated test formulation from day -15); G8: (VDD + Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15), and G9: (VDD + Biofield Energy Treatment per se animals plus untreated test formulation). Values are expressed as mean ± SEM, n=6 in each group. ***p≤0.001 vs. G1 and G2.
The effect of the novel test formulation on the level of serum c-reactive protein (CRP) is presented in Figure 1. The serum CRP level in the disease control (vitamin D3 deficiency) group was 895.29 ± 6.02 ng/mL, which was found to be 98.06% higher than that of the normal control (G1) group 452.04 ± 3.80 ng/mL. However, calcitriol group (G3) showed reduced serum CRP level (704.59 ± 6.81 ng/ mL) by 21.30% as compared with the G2 group. The experimental groups such as untreated test formulation to the untreated animals (G4) showed reduced CRP level (708.06 ± 6.37 ng/mL) by 20.91% as compared with the G2 group. Similarly, Biofield Energy Treated test formulation to the untreated animals (G5) reduced the serum CRP level (705.79 ± 4.38 ng/mL) by 21.17% as compared to the G2 group. Biofield Energy Treatment per se to the animals (G6) reduced the CRP level (688.59 ± 6.46 ng/mL) by 23.09% lower as compared to the G2 group. In addition, 15 days pre-treatment of Biofield Energy Treated test formulation (G7) reduced the CRP level (718.14 ± 2.95 ng/mL) by 19.79% as compared to the G2. Another group, 15 days pre-treatment of Biofield Energy Treated test formulation to the Biofield Energy Treated animals (G8) reduced the CRP level (694.41 ± 5.89 ng/mL) by 22.44% as compared to the G2. Similarly, the untreated test formulation to the Biofield Energy Treated animals (G9) reduced the CRP level (688.61 ± 13.29 ng/ mL) by 23.09% as compared to the G2 group. CRP is one of the major inflammatory biomarkers (highly sensitive protein) for inflammatory disorders [35,36]. Thus, Biofield Energy Treatment per se and the test formulation significantly reduced the serum CRP, which significantly improve the inflammatory conditions Figure 5.
In this research plan, four groups were considered as preventive maintenance groups. These groups were G6 (Biofield Energy Treatment per se to animals at -15 days), G7 (Biofield Energy Treated test formulation from day -15), G8 (Biofield Energy Treatment per se to animals along with Biofield Treated test formulation from day -15), and G9 (Biofield treatment per se at -15 days to animals with untreated test formulation). The results showed a significant slowdown of disease progression and all other disease-related symptoms/complications and also reduced the chances of disease susceptibility in these groups. Specifically, group G6 (preventive Biofield Energy Treatment group per se at -15 days) showed the best results as a preventive treatment group compared to the other groups. Based on the overall data, it suggests that the Biofield Energy Healing Therapy was found to be most effective and beneficial to prevent and protect from the occurrence of any type of disease in the rat model. The data indicated that this therapy could act as a preventive maintenance therapy to prevent the occurrence of disease, slow down the disease progression when disease-related complications are present which will ultimately improve the overall health and quality of life.
Conclusion
Results of the study revealed that the level of Klotho protein (anti-aging biomarker) in cerebro-spinal fluids were significantly increased by 44.2%, 92.0%, 44.2%, and 43.1% in the Biofield Energy Treatment per se to animals from day -15 (G6), Biofield Energy Treated test formulation from day -15 (G7), Biofield Energy Treatment per se plus Biofield Energy Treated test formulation from day -15 (G8), and Biofield Energy Treatment per se animals plus untreated test formulation (G9) groups, respectively as compared to the disease control group (G2). Moreover, the level of β-endorphin (cognition, pain and inflammation biomarker) was significantly increased by 418.4%, 1155.7% (p≤0.01), 890.4% (p≤0.01), 351%, and 566.7% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the G4 group. Moreover, serotonin level was increased by 94.8%, and 63.4% in the G6 and G9 groups, respectively as compared to the G4. Further, 1, 25 (OH)2 D3 was significantly increased by 61.8%, 33.4%, 61.5%, 64.5%, and 30.6% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the VDD induced group (G2). The level of c-reactive protein (CRP, inflammation biomarker) was reduced by 21.2%, 23.1%, 19.8%, 22.4%, and 23.1% in the G5, G6, G7, G8, and G9 groups, respectively as compared to the G2 group. The current findings conclude that the Trivedi Effect®-Biofield Energy Healing Treatment has significantly enhanced the antiaging, cognitive, and anti-inflammatory biomarkers level that could be helpful in various aging/psychiatric or inflammatory disorders. which can also be used to improve the overall health. Biofield Energy Healing Treatment (The Trivedi Effect®) per se showed the best results with respect to different beneficial efficacy and biomarker parameters in the preventive maintenance group, G6, as compared to the other preventive maintenance groups (G7, G8, and G9) in the rat model study.
The Biofield Energy Healing Treatment also helped to slow down the disease progression and disease-related complications impacting the overall animals’ health. These data suggested that Biofield Energy Treatment per se and Biofield Energy Treated Test formulation in combination would be the best treatment strategy to prevent and protect from the occurrence of any type of disease. Therefore, the Biofield Energy Healing Treatment (the Trivedi Effect®) per se might be effective in healthy humans when used as a preventive maintenance therapy to sustain good health, to boost overall health, promote healthy aging and increase quality of life. In the presence of disease, the Biofield Energy therapy might reduce the severity of any acute/chronic disease (such as auto-immune related and inflammatory disorders) and / or slow the disease progression. Thus, the Biofield Energy Treated test formulation may act as an effective anti-inflammatory and immunomodulatory product for various autoimmune disorders such as Addison Disease, Systemic Fibromyalgia, Lupus Erythematosus, Hashimoto Thyroiditis, Celiac Disease (gluten-sensitive enteropathy), Multiple Sclerosis, Dermatomyositis, Graves’ Disease, Pernicious Anemia, Aplastic Anemia, Type 1 Diabetes, Myasthenia Gravis, Crohn’s Disease, Vasculitis, Scleroderma, Rheumatoid Arthritis, Psoriasis, Reactive Arthritis, Sjogren Syndrome, Chronic Fatigue Syndrome, Vitiligo, and Alopecia Areata, as well as inflammatory disorders such as Irritable Bowel Syndrome (IBS), Asthma, Ulcerative Colitis, Parkinson’s Disease, Alzheimer’s Disease, Dermatitis, Atherosclerosis, Hepatitis, and Diverticulitis. Further, the Biofield Energy Healing Treated test formulation can also be used in the prevention of immune-mediated tissue damage in cases of organ transplants like kidney transplants, heart transplants, and liver transplants, and in the improvement of overall health and quality of life.
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publishers Group#OJNBD Journal#Online Journal of Neurology and Brain Disorders#Journal of Neurology#Journal of Brain Disorders#Journal of Neurosurgery
0 notes
Text
Lupine Publishers| Schizophrenia, Carbonyl Stress and Carnosine
Lupine Publishers| Journal of Neurology and Brain Disorders

Abstract
Go to
Recent research suggests that schizophrenia is associated with the development of an advanced aging phenotype (carbonyl stress) and erythrocytes from schizophrenics also exhibit symptoms of cellular aging (increased levels of glycated proteins and ubiquitinated proteins), possibly due to excessive glycolysis-induced methylglyoxal (MG) generation. The endogenous dipeptide carnosine (beta-alanyl-L-histidine), which can delay cellular aging, suppress glycolysis and inhibit MG-induced protein glycation, also exerts some beneficial effects towards schizophrenia. Carnosine is present in human erythrocytes and the olfactory bulb (olfactory dysfunction is associated with schizophrenia). It is suggested that enhanced erythrocyte and olfactory carnosine levels may be more therapeutic towards schizophrenia, if carnosine was also administered intra-nasally to avoid serum carnosinase activity.
Keywords:Carnosine; glycation; methylglyoxal; erythrocyte; aging; nasal administration
Introduction
Go to
Schizophrenia and carbonyl stress
Many studies have indicated a relationship between schizophrenia and dysfunctional energy metabolism [1-3] whilst others indicate that carbonyl stress and generation of advanced glycation end-products (AGEs) accompany schizophrenia [4,5]. Furthermore, a recent study suggests that changes in glycolysis and accelerated cellular aging in glial cells contribute to the condition [6]. The glycolytic intermediates glyceraldehyde-3-phosphate and dihydroxyacetone-phosphate are the most likely sources of AGE formation due to their ability to spontaneously decompose into methylglyoxal (MG). MG is well recognized as a major glycating agent and is thought to be responsible for much macromolecular modifications associated with type-2 diabetes and age-related neurodegenerative conditions [7,8]. However, there is no clear evidence whether suppression of MG generation, via decreased glycolytic activity, has any effect on schizophrenia. The suggestion that schizophrenia seems to be associated with accelerated cellular aging [6] is supported by another recent observation reporting that erythrocytes obtained from schizophrenics contain elevated mounts of ubiquitinated proteins [9]. This might arise from either increased generation of targets for ubiquitination (e.g. aberrant polypeptides or denatured misfolded proteins), or decreased de-ubiquitinating activity, or decreased proteasomal proteolytic activity which would normally complete polypeptide destruction. Interestingly, MG and other agents responsible for carbonyl stress, also induce protein cross-linking which not only renders the target protein less susceptible to proteolytic attack but can also result in inhibition of proteasome activity generally [10]. Thus, it is conceivable that excessive glycolysis can provoke an aging phenotype (AGE accumulation and proteostatic dysfunction) via increased MG generation; such a relationship has been demonstrated in mice fed a high glycemic- index diet [11]. Never-the-less it is necessary to show whether glycation compromises proteostatic in erythrocytes from schizophrenics.
Erythrocytes and schizophrenia
A number of recent papers have revealed that erythrocytes obtained from patients with neurological problems, such as Alzheimer’s Disease (AD) and Parkinson’s Disease (PD), exhibit symptoms typical of aging cells in general. For example, compromised proteolytic activity and MG detoxification were detected in AD erythrocytes [12] and accumulation of aggregated protein occurs in red cells from PD patients [13]. Furthermore, dysfunctional energy metabolism, especially in relation to glycolysis culminating in carbonyl stress, are now regarded as characteristics of both AD and PD [14,15]. Therefore, it is not surprising that evidence of carbonyl stress is also accompanied by enhanced protein glycation [16] and accumulation of ubiquitinated proteins [9] in erythrocytes (and possibly other cells) obtained from schizophrenic individuals [17]. Moreover, one of the glycated proteins from “schizophrenic” red cells has been identified as a selenium-binding protein (SBP1) [18]; dysfunctional selenium metabolism has long been regarded as an important contributor to schizophrenia [19,20]. Selenium plays an important role in Sulphur metabolism required for synthesis of antioxidant enzymes such as glutathione peroxidase [21]. Thus, one is beginning to understand the relationship between AGE generation, carbonyl and oxidative stress and the apparently disparate biochemical attributes to schizophrenia.
Carnosine, carbonyl stress and schizophrenia
That erythrocytes can contain elevated amounts of MG and glycated proteins suggests the possibility that such red cells could become systemic sources of MG and AGEs to the brain and other tissues, following MG-induced eryptosis [22]. Consequently, it is important to consider whether suppression of carbonyl stress, not only in erythrocytes but in astrocytes and glia, could possibly be a therapeutic strategy. The naturally occurring dipeptide carnosine (beta-alanyl-L-histidine) has been shown to suppress glycolysis in cultured cells [23,24], delay replicative senescence [25], stimulate proteolysis of long-lived proteins in late passage cells [26] and inhibit AGE formation [27]. Furthermore, there is one study showing that schizophrenics subjected to dietary supplementation with carnosine exhibited some beneficial effects [28], possibly due to the dipeptide’s pluripotent properties [29]. It is also interesting to note that
a) Olfactory dysfunction is also associated with schizophrenia [30,31] and
b) Carnosine is enriched in the olfactory bulb [32].
Thus, one has to consider whether raising olfactory carnosine levels could also be useful. However, all studies employing dietary carnosine supplementation are subject to the problem of the presence of serum carnosinase activity which would destroy the dipeptide [33]. There is an alternative route however, which is to use an intra-nasal approach. This could involve a nasal spray of a carnosine solution; another approach could involve use of carnosine powder. Indeed “snorting” carnosine could be far more useful than most white powders some people use, be it illegal drugs or “medicinal snuff “of old. In fact, intra-nasal delivery of potential therapeutic agents is currently being explored [34] with respect to neurodegenerative conditions, as proposed many years ago [35].
Carnosine has been detected in human erythrocytes [36] but in lower amounts when obtained from elderly individuals [36]. It is presumed that red cell carnosine is synthesized (from betaalanine and histidine) during erythropoiesis. Consequently, it would be useful to determine whether dietary supplementation with carnosine or beta-alanine raises erythrocyte carnosine levels and whether there are any beneficial effects with respect to the recognized changes in “schizophrenic” erythrocytes. Additionally, it is suggested that any carnosine (dietary or nasally administered) supplementation period should last for at least 120 days to ensure maximal numbers of carnosine-enriched erythrocytes. It has been proposed that excessive and continuous glycolysis in erythrocytes enhances red cell MG levels, and thus also facilitate delivery of erythrocyte MG to the tissues including the brain [22]. Consequently, it will be also important to determine whether such supplementation protocols decrease carbonyl stress and MG levels not only in red cells but the tissues generally including glia [6]
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publishers Group#OJNBD#Online Journal of Neurology and Brain Disorders#Journal of Neurology
0 notes
Text
Lupine Publishers| Primary Lateral Sclerosis, Report of a Case and Bibliography Revision
Lupine Publishers| Journal of Neurology and Brain Disorders
Abstract
Introduction: Primary lateral sclerosis is a rare disease involving the upper motor neuron, producing a bulbospinal spasticity. The course of the disease is insidious and progressive, usually starting with the lower extremities, and later becoming a tetrapyremidal syndrome. As a rare disease, diagnosis in most cases is exclusionary, and the patient should be studied extensively, clinically, including a thorough medical history, laboratorial and with the relevant cabinet studies.
Classic Case: It is male patient who starts his clinical picture about a year ago with weakness in left pelvic limb, subsequently accompanied by pain and paresthesias, manifesting the same symptomatology later in the contralateral leg and upper left limb. Currently is added index and middle toe hypoesthesia, moderate tremor in left arm, with the contrast of the middle toe over the ring of said hand. It has an inability to lift light objects for short periods of time, as well as fatigue in short periods of time when performing daily activities, which greatly limits their daily life.
Conclusion: Motor neurone diseases are divided into two groups, and in the case studied, the upper motor neuron is exclusively affected. As it is a rare disease, with a low incidence, multiple differential diagnoses will be considered before concluding in it, considering it a diagnosis of exclusion. The natural history of the disease will always have a grim outcome, with poor prognosis for life and function, despite the measures taken to change the course of the disease.
Keywords:Motoneuron; upper; spastic; resonance
Introduction
Primary lateral sclerosis is a rare disease involving the upper motoneuron, which is characterized by a progressive bulbospinal spasticity, with selective degeneration of pyramidal neurons located in the precentral convolution [1]. Primary lateral sclerosis makes up approximately 1% to 4% of all patients with motor neuron diseases [2]. The onset of the disease is insidious, with a slow and progressive spastic paralysis, usually starting at the lower extremities, and then becoming a tetrapyremidal syndrome. On average, patients are estimated to have a life prognosis greater than 10 years from the onset of symptoms. Hyperreflexia, moderate weakness, dizziness, lack of coordination may also occur within the clinical picture. In the physical examination you can find spasticity, increased osteotendinous reflexes, and as a predominant sign, stiffness [2,3]. Diagnosis is usually performed clinically, relying on MAGNETIC resonance imaging, among other studies, to rule out other pathological entities, showing in this study a marked atrophy in the primary motor cortex [3]. In some studies, diffusion magnetic resonance imaging has been used, showing a functional increase in cerebral axonal activity, especially the brain-cerebellar, which could explain an adaptive process through functional neuroplasticity, however, the prognosis of the disease remains unfavorable and irreversible despite these changes [4]. Although there are some diagnostic criteria for the disease, as it is a rare entity, not all inclusions for it are always met, so it is usually a diagnosis of exclusion [5,6] (Figure 1).
Figure 1: Diagnostic criteria proposed by Pringle and Cols.
Clinical Case
They are a 42-year-old male patient, who started his clinical picture about a year ago, when when he is parading, I notice some weakness in left pelvic limb, progressing over the course of the days to diffuse pain and local paresthesias, and subsequently having the same problem in the contralateral leg and then to upper left limb throughout, progressively to date. Currently, adding to the above, it has hypoesthesia of index and middle toe, stiffness in all the arcs of the movement of the affected limbs, moderate tremor in the left arm, with the oversetting of the middle toe over the ring of said hand. Symptomatology is exacerbated in the mornings. It has an inability to lift light objects for short periods of time, as well as fatigue in short periods of time when performing daily activities, which greatly limits their daily life. It denies important here family backgrounds, as well as surgeries, drug addictions, or known diseases (Figure 2).
Figure 2: Cervical spinal MRI where you see a normal morphology without compromise spinal cord.
Discussion
Primary lateral sclerosis is a rare disease affecting the upper motor motoneuron of the primary motor area (pre-central circumvolution),characterized by having an insidious onset in people with no known risk factors, with a clinical picture in which a spastic paresis of lower limbs of onset predominates that can be generalized until tetra pares progressively increasing over the years and which is usually a long-evolving disease. Diseases of the motor neuron are divided into those that affect the upper and lower, in this case we focus on the first case, which are located inside the cerebral cortex and send axons that form the pyramidal pathway, to later defuse and finally connect to the spinal cord. The manifestations secondary to the lesion of the upper motoneuron are as follows: spastic paralysis, amyotrophy (by disuse), absence of tracing, exalted myotatic reflexes and extensive plantar response.
As it is a disease with a low incidence and few reported cases, it should never be considered as a diagnosis of first instance, having to rule out other differential diagnoses, so over time various diagnostic criteria have been defined to realize the disease, however, as well mentioned, it is a rare disease, so no definitive consensus has been created for the diagnosis and scrutiny of the disease, however, we can lead our diagnostic approach means of any of these, such as the criteria of pringle and cabbage, through a well-established clinic, conducting a thorough clinical history, laboratory studies, ranging from general analyses such as hematic biometry, blood chemistry, functional tests, to cytological examinations of cerebrospinal fluid, quantification of vitamin B12 in serum, trepamic tests, as well as cabinet studies such as electromyography and MRI, where the absence of other pathological entities is verified and in the latter study a marked cortical atrophy of the pre-central turn. Despite the above, it should be noted that the disease may not follow a specific pattern within its natural history, so it may vary the presentation and sequence of them.
Conclusion
Motor neuron diseases are divided into two groups, and in the case studied, the upper motoneuron is exclusively affected, differing from each other by the form of presentation and clinical manifestations. As it is a rare disease, with a low incidence, multiple differential diagnoses will be considered before concluding in it, considering a diagnosis of exclusion, and thus, a thorough medical history should be made with a proper examination conducting laboratory and cabinet studies relevant to this situation. Although it is a long-term disease with a longer life expectancy than amyotrophic lateral sclerosis, the natural history of the disease will always have a grim outcome, with poor prognosis for life and function, taking into account there is no cure for the disease other than supportive treatment.
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publishers Group#OJNBD#Journal of Neurology and Brain Disorders#Online Journal of Neurology and Brain Disorders#Neurology
1 note
·
View note
Text
Lupine Publishers| Objective Structured Examinations as Supplemental Equipment for Amending Emotional Intelligence: A Pilot Survey

Lupine Publishers| Journal of Neurology and Brain Disorders
Abstract
Background: The scientific study of emotional intelligence (EI) in organizations has gained considerable research activity over recent years because it is being concerned with awareness and management of one’s own feelings and emotions in daily living activities. The objective of the present study was to investigate the relationship between EI of a group of psychiatric residents and their academic achievement to see that whether proper training and evaluation by new educative instruments can recompense any degree of shortage in EI.
Methods: Consistent with a cross-sectional survey design, 31 psychiatric residents had been requested to answer to The Schutte Self Report Emotional Intelligence Test (SSEIT), in June 2014, for examining the situation with respect to objective structured examinations, like mini-Clinical Examination Exercise (mini-CEX), Objective Structured Clinical Examination (OSCE), and chartstimulated recall (CSR) scores, which had been taken in the earlier 6 months. SSEIT score of 90 had been taken as demarcating point for dividing the sample population into two parallel groups, including the first group with SSEIT score lower than 90 and second group with SSEIT score equal to or more than 90.
Results: The response rate was 93.54%. In line with the results, there was no meaningful relationship between the aforesaid first group and second group as regards the relationship between SSEIT’s score and the mean total score of Mini-CEX, OSCE, and CSR, which had been examined in the preceding 6 months.
Conclusion: The current study demonstrates that EI does not seem to be a fixed problem in psychiatric residents, and enough exercise along with improvement of necessary interrogating or clinical skills may improve or compensate for unsatisfactory EI.
Keywords:Emotional Intelligence; Objectives Structural Examinations; Psychiatric Residents
Introduction
The scientific study of Emotional Intelligence (EI) in organizations has gained considerable research activity over recent years [1]. Simultaneously researchers have investigated and raised concerns about the appropriate way to measure EI in various studies [2]. Although EI has been the subject of much attention at both popular and academic level, only now are answers provided to some of the fundamental questions posed about the construct [3]. Dulewicz, Higgs and Slaski confirm that in literature there appears to be some debate about what constitutes the domain of EI, about terminology used to describe the construct and about methods used to measure it [4]. One method that has been used widely in research to measure EI is the Schutte Emotional Intelligence Scale (SEIS) [5]. Dulewicz et al. state that EI is not a new concept [4]. Mayer, Salovey and Caruso [6] define the concept of EI as the capacity to reason about emotions, and of emotions to enhance thinking. EI includes the abilities to accurately perceive emotions, to access and generate emotions in order to assist thoughts, to understand emotions and emotional knowledge, and to reflectively regulate emotions in order to promote emotional and intellectual growth [6]. Dulewicz and Higgs [4] define EI as being concerned with being aware of and managing one’s own feelings and emotions; being sensitive to and influencing others; sustaining one’s motivation; and balancing one’s motivation and drive with intuitive, conscientious and ethical behavior. It is apparent that from this theoretical perspective EI refers specifically to the co-operative combination of intelligence and emotion [7]. EI emphasizes the importance of self-awareness and understanding, redressing a perceived imbalance between intellect and emotion in the life of the collective Western mind [7]. Zeidner et al. further state that EI also connects with several cutting-edge areas of psychological science, including the neuroscience of emotion, self-regulation theory, studies of meta-cognition, and the search for human cognitive abilities beyond ‘traditional’ academic intelligence. Given the core proposition that it is a combination of IQ and EI that determines life success, a question arises as to whether or not it is feasible to measure EI [4]. On the other hand, an Objective Structured Clinical Examination (OSCE) is a modern type of examination often used in health sciences (e.g. Midwifery, orthoptics, optometry, medicine, naturopathic medicine, physician assistants/associates, physical therapy, radiography, nursing, pharmacy, dentistry, chiropractic medicine, paramedicine, podiatry, veterinary medicine). It is designed to test clinical skill performance and competence in skills such as communication, clinical examination, medical procedures / prescription, exercise prescription, joint mobilization / manipulation techniques, radiographic positioning, radiographic image evaluation and interpretation of results [8]. Simulation is a new exciting technology incorporated in undergraduate medical curriculum. It is well accepted by educators across the world to improve experiential learning by enhancing the performance of medical professionals [9]. Simulation is defined as imitation of the “real world” setting to model the environment, resources needed, and the people involved [10]. Educators have encountered educational challenges by reforming the curriculum, developing problem-based learning, and promoting research as well as independent learning. Nevertheless, disparity still persists between the preclinical and clinical environment. Preclinical medical students have minimal contact with clinical cases and are apprehensive when they commence their clinical years and internship. Many students feel that they are inefficient in history taking, physical examination, diagnosis, and management. Medical simulation has been adopted to bridge this educational gap and provide an opportunity to learn from errors [11]. The objective of the present study is to investigate the relationship between EI of a group of psychiatric residents and their academic achievement to see that whether proper training and evaluation by new educative instruments can recompense any degree of shortage in EI.
Methods
A cross-sectional appraisal scheme was used in the present assessment. Psychiatric residents were informed about the objective and method of the study, voluntary format of contribution, anonymity and privacy of information. The study was accomplished during June 2014. Total existing population of psychiatric residents was selected as the sample for this study (n=31). Among the total 31 psychiatric residents, 29 participants (93.54%) responded to the evaluation. While one of the participants was reluctant to participate in the assessment, another one was absent during the assessment. Two different types of tools were used in the current estimation. The first one was a demographic inquiry form that involved four queries of sex, age, year of training and educational outcomes regarding their objective structured examinations, including Mini-Clinical Examination Exercise (Mini- CEX), Objective Structured Clinical Examination (OSCE), and Chart-Stimulated Recall (CSR) scores. It deserves to be mentioned that Mini-CEX is a method of appraisal that can be used to evaluate the clinical skill of residents and can enhance student learning and develop student professionalism in serving patients [12]. CSR, as well, has been utilized by active specialists in medicine as a reliable and valid instrument to find strengths and weaknesses in medical practice [13]. OSCE, too, is a modern form of scrutiny that is planned to test clinical skills such as clinical examination, communication, medical procedures / prescription, etc. [14]. The second instrument involved the Schutte Self Report Emotional Intelligence Test (SSEIT), which was developed by Schutte et al. [5]. This tool measures trait EI by means of 33 self-referencing items that evaluate EI level of the person. Individuals score the level they agree or disagree with every single announcement on a 5-point measure oscillating between 1 (strongly disagree) and 5 (strongly agree). Three items among the thirty-three ones [15], are inversely scored. According to Schutte et al., while the two-week test-retest reliability co-efficient of SSEIT is around 0.78, the scale has high internal consistency with Cronbach’s alpha (α) ranging from 0.87 to 0.90 (31). SSEIT scale has been used in different studies with a range of samples including adolescents, adults, and secondary school apprentices, and it is easy to apprehend and score [5]. SSEIT score of 90 is usually taken as a cut-off point. While SSEIT score of 90 or higher includes: low average (90-99), high average (100-109), competent (110-119), strength (120-129) and significant strength (130+), SSEIT score of 89 and lower consists of: consider improvement (70-89) and consider development (69 or less), based on Mayer’s guidelines [15].
Statistical Analysis
Demographic characteristics were analyzed by comparison of proportions regarding gender and year of study and comparison of means (t-test) regarding age, scholastic evaluative scores and EI. Data analysis was conducted using MedCalc Statistical Software version 15.2. Statistical significance was determined as a P≤0.05.
Results
The demographic characteristics of the study participants are described below in Table 1, and there was no significant baseline demographic difference between male and female participants regarding ethnicity, quantity, age and SSEIT score (Table 1). Among 31 psychiatric residents of the University of Social Welfare and Rehabilitation Sciences, 29 participants (93.54%) answered back to the survey and replied to the Schutte Self Report Emotional Intelligence Test in June 2014.One of the residents was reluctant to participate and another one was on leave during the assessment. 17.24% (n=5), 27.58% (n=8), 24.13% (n=7) and 31.03% (n=9) of the participants were 1st year, 2nd year, 3rd year and finally 4th year post graduate trainee, respectively (Table 2). According to the findings and based on ANOVA, there was no significant difference among four groups of participants with respect to the SSEIT scores (Table 3). In the current evaluation, SSEIT score of 90 was taken as a demarcating point. As a result, while SSEIT score of 90 or higher could include: Low average (90-99), High average (100- 109) , Competent (110-119), Strength (120-129) and Significant Strength(130+), SSEIT score of 89 and lower as well could consist Consider Improvement (70-89) and Consider Development (69 or less), based on Mayer’s guidelines (Mayer, et al., 2002, p. 18). On the whole, in the present sample population, 34.48% (n=11) of the participants had SSEIT score of 89 or lesser (first target group, with a SSEIT score of 83.45+/-3.98), and 79.31% (n=18) of the contributors had SSEIT score of 90 or higher (second target group, with a SSEIT score of 101.5+/-9.03) (Table 4). While quantitatively and base on ‘Comparison of Proportions’ there was no significant difference among those two target groups (z = -1.8383, p<0.06, C I 95% = -0.49, 0.01), comparison of means showed a significant difference, with respect to SSEIT score, among them (p<0.000) (Table 4). But as the main objective of the present assessment and based on between-group analysis and comparison of means, while the mean total scores of the 2nd Group ( with SSEIT score = or >90 ) was commonly higher than the first group (with SSEIT score <90 ) in objective structured examinations, including Mini-CEX, OSCE and CSR , no significant difference was evident among those two target groups regarding their performance in those objective educational tools for assessment of trainee’s skills(p<0.10, p<0.09 , p<0.16, respectively) (Table 5). Post-hoc power analysis showed a power equal to 0.36 on behalf of this trial, which turned to power=0.74 in compromised power analysis.
Discussion
Simulation based education is a promising discipline that provides secure and effectual learning platform for students. The clinical sessions can be planned, observed and repeated to facilitate learning [16]. Exposure to simulation for medical students is a valuable tool to enhance knowledge and student self-confidence at a key transition period prior to beginning of internship [16]. Students report difficulty in applying theoretical knowledge and perceive shortcomings in integrating basic science knowledge with clinical practice [17]. Imparting medical knowledge and skills without placing a patient at an increased risk of complications can be attained through simulation sessions for undergraduate medical students who do not have complete autonomy in diagnosis and management of clinical cases [18]. One of the most challenging aspects of teaching residents is identifying tools for assessment for learning. Assessment for learning allows teachers to see where their residents are doing well and where they need further instruction; as well, it allows teachers to target instruction during the assessment to further residents’ understanding [19]. An OSCE, as the prototype of such kind of innovative evaluations, usually comprises a circuit of short (the usual is 5–10 minutes although some use up to 15 minute) stations, in which each candidate is examined on a one-to-one basis with one or two impartial examiner(s) and either real or simulated patients (actors or electronic patient simulators). Each station has a different examiner, as opposed to the traditional method of clinical examinations where a candidate would be assigned to an examiner for the entire examination. Candidates rotate through the stations, completing all the stations on their circuit. In this way, all candidates take the same stations. It is considered to be an improvement over traditional examination methods because the stations can be standardized enabling fairer peer comparison and complex procedures can be assessed without endangering patient’s health. As the name suggests, an OSCE is designed to be objective (all candidates are assessed using exactly the same stations (although if real patients are used, their signs may vary slightly) with the same marking scheme, structured (stations in OSCEs have a very specific task. Where simulated patients are used, detailed scripts are provided to ensure that the information that they give is the same to all candidates, including the emotions that the patient should use during the consultation.
Instructions are carefully written to ensure that the candidate is given a very specific task to complete, and, finally, clinicaloriented (the OSCE is designed to apply clinical and theoretical knowledge. Where theoretical knowledge is required, for example, answering questions from the examiner at the end of the station, then the questions are standardized and the candidate is only asked questions that are on the mark sheet and if the candidate is asked any others then there will be no marks for them) [20,21]. So, competent performance requires not only requisite knowledge and skills but also beliefs of personal efficacy to use both effectively. Anyhow, the relationship between clinical experience and student performance is complex. Well-organized and strategic learning styles appear to influence the benefits of increased clinical exposure. Direct observation of clinical skills is a critical first step in helping trainees to improve their clinical skills [22]. Back to our discussion and according to the findings of the present assessment, while significant difference was palpable between two groups of psychiatric residents regarding emotional intelligence, based on SSEIT score, no significant correlation was evident between that factor and academic performance of participants. Such a result may not be in harmony with the suggestion of Carrothers et al. [23] who had suggested using EI as part of the selection process for medical students and Stratton et al. [24], who stated that Individuals with low levels of EI may lack the ability to relate empathetically with patients as they are unable to recognize feelings, distress, and mood , or belief of McQueen [25] who said that low levels of EI leads to a negative impact on the doctor–patient relationship . In contrast, our finding was more in agreement with Stratton et al. [24] who found only a modest correlation between EI, and students’ clinical skills assessed by standardized patients in an Objective Structured Clinical Examination (OSCE). On the other hand it could not deny the view of Arora et al. [26] who noted that higher EI may play a role in maintaining good physician–patient relationships, improved teamwork and communication skills, better stress management, and superior commitment and leadership, since generally higher scores in the aforesaid objective assessments were observable, as well, in the present assessment and in the group with higher SSEIT score, though non-significantly. On the other hand, non-significant difference between two groups regarding objective assessment tools could be attributed to the preparation of psychiatric residents, from the start, respecting basic principles and techniques of interview, in general, and sympathy, rapport, verbal and non-verbal communication, specially.
Such an inference is in harmony with the standpoint of Stoller et al. [27] who had recommended that a spiral curriculum should be used to develop EI skills of physicians. Also, while Austin et al. [28] found a gender-based difference and significantly higher overall EI and empathy in female medical students, as like as Carrothers et al. [23], in the present assessment as well higher SSEIT score was evident in female residents, but it was not a significant variance. Such discrepancies may necessitate taking into consideration other interconnected factors that may easily be ignored during scientific assessments, as like as culture, which has been declared by Cherniss and Goleman [29] as a factor that can influence both an individual’s response to an event and the subsequent response selection. In this regard, anthropologists also suggest that cultures have conventions and norms that influence the management of emotions in individuals [30]. These cultural values create commonality and predictability among individuals in their interpretation and response to emotional stimuli. Past research has shown that Whites score lower on EI tests than Hispanics and Blacks [30], a finding that is not in congruence with the later educational and social achievements. Therefore, it is important to study EI in different cultures and ethnic populations to gain insights into their emotional processes. One conclusion from this assessment could include that, while enhancement of rapport, sympathy and emotional intelligence skills, according to Stoller et al. [27], can be an auspicious enlightening approach, selection of medical students based on EI is a discriminating dogma. Also, too much stress on significance of EI by medical mentors is not reasonable, since still a notable unpredictability exists regarding the subject. Evidence based medicine cannot be established on uncertain grounds. If psychiatric training can make low EI a trifling phenomenon, so it can happen in other areas of clinical practice as well. Anyhow , while small sample size, constrained number of objective assessment tools, restriction of study to merely psychiatric residents, limitation of study to a short period of assessment, lack of control or comparison group were among the weaknesses of this study, which limit the generalization of its results, it was simply a pilot exploration. Additional investigations in future with larger sample populations and more systematized approach will certainly help to explore in this regard more meticulously.
Conclusion
The current study demonstrates that EI does not seem to be a fixed problem in psychiatric residents, and enough exercise along with improvement of necessary interrogating or clinical skills may improve or compensate for unsatisfactory EI.
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publishers Group#OJNBD#Online Journal of Neurology and Brain Disorders#Neurology#Neurosurgery
0 notes
Text
Lupine Publishers| The Arapetic of the use of the Gum of Mascar in your Different Presentations to Minimize the Dream Inerance and Deprivation

Lupine Publishers| Journal of Neurology and Brain Disorders
Abstract
Introduction: Sleep is defined as the natural, periodic and reversible decrease in perception of the external environment, with the preservation of a certain degree of reactivity to the environment and autonomous functions. Sleep consists of 2 phases, REM phase and NREM phase, these phases alternate at night in the form of five to six cycles; of which the NREM phase is 75% presented and the REM by 25%.
Thertita mark: Caffeine is a readily available short-acting stimulant that has been shown to reduce some of the deficits associated with sleep loss. With the rubber mark the absorption is carried out on the oral mucosa, which generates a greater bioavailability of the active substance and an immediate mechanism of action. The effective response dose can range from 100 mg to 200 mg and the effect arises from 6 min of administered the active substance. It is important to note that the dose of caffeine in chewing gum is directly proportional to the effects on sleep inertia, as well as the duration and maintenance of them.
Discussion: Being able to analyze the mechanisms of action of caffeine on sleep inertia, helps us to make a comparison of chewing gum with caffeine vs placebo (simple gum). Chewing generates for a short period of time the maintenance of performance on simple and complex tasks and improves alertness, with caffeine these same effects look prolonged for longer.
Conclusion: Caffeinated gum is an effective therapeutic presentation on sleep inertia. The dosage for a positive response ranges from 75 to 200 mg depending on the circumstances of sleep restriction. That is, thanks to the effects generated by chewing on the state of alertness and cognition and the potentialization and duration of them by caffeine.
Introduction
Sleep disorders cause alterations in the quality of life of each and every patient. At least two-thirds of those with chronic degenerative diseases are affected by sleep disorders, the most common being the female sex.
Many individuals are subjected to night jobs where a constant state of alertness is required and scientifically proven how this affects the quality of life of each of the employees; for sleep is one of the most indispensable pillars of daily life, as it maintains critical aspects of cognition for optimal mental performance, as well as in mood, alertness and performance during working days and activities of the and everyday life. Awakening abruptly involves something known as “sleep inertia,” which is characterized by impaired performance and subjective lack of alertness for a transitional period, which hardly progresses to a good cognition. It is well known that chewing facilitates concentration, maintains alertness and improves performance in cognitive tasks, but the question is how effective is by itself the effect of chewing a simple chewing gum vs to one that contains Caffeine? Therefore, one of the objectives of this research work, is to analyze the effects of chewing from a simple chewing gum to one that contains caffeine, verify the effectiveness by reversing the sleep inertia of each of them and know the mechanism of action , the pharmacokinetics, bioavailability and absorption of a caffeinated gum during sleep deprivation.
Theoretical mark
Normal sleep progresses in various stages: NREM (nonrapid eye movement) phase and REM (rapid eye movement) phase. These cycles alternate at night in the form of 5 to 6 cycles. In 75% of normal nighttime sleep is NREM and 25% REM.
Phase brake
It happens every 90 minutes or so. It is characterized by zero muscle tone, presence of active sleep, as the electrical activity of the brain is maximum while the body is at full rest, rapid eye movements, heart rate as well as respiratory evidence of increased basal metabolism and the amount of gastric juice.
Step nrem
Also known as “deep sleep,” it facilitates body rest and consists of 3 phases.
a) Phase N1 (Surface Sleep): very light sleep stage, lasting several minutes. It is characterized by a slight decrease in heart rate, breathing, muscle tone, general state of deep rest, relaxed and drowsy, maintaining active the ability to perceive external stimuli.
b) Phase N2 (Surface Sleep): characterized in EEG by sleep spindles and k complexes. Its duration is 10 to 15 minutes. At this stage the muscle tone relaxes further, slightly decreases body temperature and respiratory and cardiac rate, disappearing eye movements.
c) Phase N3 (Deep Sleep): Characterized by a global slowdown of the electrical path and the appearance of slow waves and high voltage (deltas) whose total duration must be greater than 20% and less than 50% of the plot. Sensory perception decreases markedly, as does heart and respiratory rates. Relaxation of the muscles is intensified. It is more difficult to wake up the subject, and if he does, he finds himself disoriented and confused. It is the fundamental stage for the subject to rest subjectively and objectively.
This research work was done based on various medical studies, where it is addressed from the rate of absorption, the bioavailability, the pharmacokinetics of caffeine in chewing gum, the effects of chewing, how is caffeine it reverses sleep inertia, assessing cognitive performance, mood and alertness after caffeinated gum is administered to the composition, formulation and design of said chewing gum. It will also include in a systematized way each and every one of the articles selected to carry out a bibliographic review and thus carry out a complete study of the effects and effectiveness of chewing gum with caffeine to minimize the inertia of sleep , based on scientific evidence from some experimental studies in which there is certainty of efficacy of it, since caffeine is involved in the autonomic nervous system and exerts its effects by acting as an adenosine receptor antagonist. The approach is an essential part of the daily life of the human being, since it is the pillar to be able to perform any cognitive activity, maintain an effective and consistent performance in order to successfully complete actions of daily life and working days. Fatigue can cause various complications and over time can affect the health of the individual, as well as leading to a reduction in efficiency during the day and the increase in the incidence of any type of accidents [1,2]. Caffeine is a white odorless powder that can have different molecular presentations, can range from an anhydride substance to contain a water molecule. Caffeine is a methylxanthine that inhibits the enzyme phosphodiesterase, generating an antagonistic effect on the central receptors of adenosine, this adenosine occurs during daily activities and binds to its receptors, generating a feeling of fatigue and consequently an induction into sleep. Due to the similarity of adenosine to caffeine, the latter takes place in adenosine receptors and thereby prevents the transmission of the fatigue signal generating that the person can continue performing his daily and work activities for a longer period, since contrary to the feeling of insomnia. Caffeine is a Central Nervous System (CNS) stimulant that can promote wakefulness and increase mental activity. In addition, it can stimulate the respiratory center, increase the frequency and depth of breathing and increase total muscle work. Caffeine is usually consumed and/or commonly administered in the form of a liquid substance, although there are other types of presentations such as tablets or capsules. A new way to consume caffeine is through chewing gum which in turn can provide additional advantages, some of them are:
a) Absorption is done through the oral mucosa, resulting in a greater bioavailability of the active substance at the systemic level.
b) Effective and immediate mechanism of action (oral mucosa).
c) It is easy to use and is suitable even for pediatric patients or patients with difficulty swallowing tablets or tablets.
d) It generates fewer side effects as the active substance is released in proportion to chewing.
e) The primary liver metabolism of the active substance is avoided, as they are absorbed directly by the oral mucosa.
f) Lower risk of overdose by chewing effect.
Chewing is a physiological motor activity involving many neural pathways, this action is associated with increased blood flow at the cerebral and orofacial level which in turn implies effectiveness in increasing alertness, physical well-being and improving memory performance. The active substance (caffeine) of chewing gum is released in proportion to chewing, this in turn is absorbed through the oral mucosa and another percentage of it is swallowed as a bolus with saliva, reaches the gastrointestinal tract and thanks to the caffeine is s the absorption rate is faster compared to that of the tablet. In addition, it is important to mention that the control of the release of caffeine in chewing gum is for a long time and improves the variability of the release and retention times of the drug, being these other advantages of this new form administration of the Caffeine.
It is important to note that the effectiveness of this chewing gum with the active substance which is caffeine, has to be argued based on studies that corroborate that effectiveness, such is the case of the P300 signal that is obtained thanks to an electroencephalogram, this signal is a neural record that is projected as a positive deflection and in turn measures the potential of the presence, magnitude, topography and duration of signaling of cognitive function. The signal is acquired more strongly around the parietal electrodes, although it has been suggested that there are also interactions between the frontal and temporal regions. Recent studies say that this P300 wave is composed of 2 secondary waves known as “P3A and P3B signals”, these components respond individually to different stimuli and it has been suggested that the P3A wave originates in the frontal care mechanisms driven by stimuli during task processing, while P3B originates from parieto-temporal activity associated with attention and memory processing.
The potential related to the P300 signal had shortened latency after chewing gum, and the frontal and temporal beta power was increased by chewing the gum after performing a sustained attention task. The quantitative effects on the EEG of chewing gum without cognitive performance seem to be moderated by the taste, suggesting that chewing gum may alter alertness in the absence of cognitive performance. Working under pressure, i.e. in a setback, was associated with increased activity in the anterior cingulate cortex and left frontal convolution, where the motor neural regions of alertness and executive tasks are located [3]. This same effect was found when chewing gum without taste or smell, suggesting that the motor activity of chewing may be a key factor in explaining these results, however it is unclear whether a higher level of motor activity in chewing will increase associated effects, as there is evidence that a more vigorous chewing or a greater resistance to chewing does not moderate the effects on memory, the fact that chewing gum can increase arousal, it therefore reaches a peak and descends and it’s while decreasing cognitive function in performing tasks that require attention (increasing heart rate and beta power during surveillance), this suggests that it is more plausible that more vigorous chewing can have a greater effect on attention to a short-term that in memory.
That is, chewing alone generates a potentization of the performance of a simple task as a result of a reflective motor activity that is generated in the body in the face of sleep deprivation, but this does not mean that this performance is maintained. One study shows that administering only 200 mg of caffeine in conjunction with chewing gum, improves nothing more the performance of simple and complex activities and/or tasks, but also improves alertness compared to chewing without the active substance. In turn the period of pre-eyetion and cardiac autonomous activity remain unchanged during chewing with or without caffeine, generating a response reflected in the increase of parasympathetic activity with changes in rr intervals in the EEG, the latter mentioned above are predictors of the speed and accuracy in the most complex cognitive tasks during sleep deprivation, alertness and performance maintenance during the realization of them.
Some other studies show evidence that the use of caffeine in chewing gum is also equally effective in dispensing sleep in the face of a post siesta; in a double-blind study with 15 adults as participants they were given this chewing gum containing 100 mg of caffeine at the hour and 6 hours after waking up vs. placebo, they were subsequently assigned psychomotor tasks before a watch dog at 0 , 6, 12 and 18 minutes. The rating of the tests was carried out based on the response rate and the number of hits during the tests. Among the results it was observed that 100 mg of caffeine did not fully restore performance, but showed an improvement in response rate by 85% compared to placebo 73%; since the effect of caffeine was evident at 6 min after waking up, which continued to improve performance until 18 minutes, i.e. the results indicate that 100 mg of caffeine substantially attenuates sleep inertia in the face of a sudden awakening by a time-values period, but higher doses (200 mg) are expected to more easily antagonize sleep inertia as a whole for a longer prolonging period.
Discussion
The purpose of this article is to evaluate based on a collection of articles the efficacy of caffeine as an active substance in a new therapeutic presentation vs placebo, studying the pharmacokinetics, bioavailability and half-life of caffeine. Among the bibliographic reviews that were addressed for the realization of this article, it is evidence that caffeine in chewing gum is a novel and new presentation that is effective in counteracting sleep inertia, improving alertness, cognition and maintaining performance during the simple and complex activities of daily life. It is important to note that the effects of caffeine are directly proportional to the dose administered in patients as well as on the route of administration. Chewing a gum without the active substance (placebo) generates a later maintenance of performance as well as alertness with the difference that these effects occur over a very short period of time.
Conclusion
Caffeine is an odorless powder that inhibits the enzyme phosphodiesterase, which generates an antagonistic effect on the central receptors of adenosine resulting in antagonism of the transmission of the fatigue signal, promoting wakefulness and increasing mental activity. The effect of chewing is associated with increased orofacial blood flow that increases alertness, physical well-being and memory performance. A combination of chewing gum with caffeine enhances and synergizes the effects that chewing alone generates, resulting in a new, novel and effective therapeutic presentation on sleep inertia, since it is easy to use and its absorption is done through the oral mucosa, which generates a greater bioavailability of the active substance and an immediate mechanism of action, in turn those effects are present for a prolonged period since the caffeine inside the gum is released in a way proportional to chewing. Caffeine can provide better alertness and performance at doses of 75 to 150 mg after acute sleep restriction and at doses of 200 to 600 mg after one night or more sleep loss. Caffeine is unlikely to have negative effects on sleep that follows 8 hours or more after administration. However, frequent use of caffeine can lead toilet and withdrawal syndrome.
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publisher group#OJNBD#Neurology and Brain Sciences#Journal of Neurology and Brain Disorders#Online Journal of Neurology and Brain Disorders
0 notes
Text
Happy Thanksgiving!

Today is the time to be thankful, remember good times, and embrace those who enrich our lives. I’m thankful for a lot of things. Happy Thanksgiving to all! from our Online Journal of Neurology and Brain Disorders (OJNBD)
1 note
·
View note
Text
Lupine Publishers | Continuous or Intermittent? Which Regimen of Enteral Nutrition is Better for Acute Stroke Patients? a Systematic Review and Meta-Analysis

Lupine Publishers | Journal of Neurology and Brain Disorders
Abstract
Background and purpose: Enteral nutrition via nasogastric tube in acute stroke patients with dysphagia is an important determinant of patient outcomes. It is unclear whether intermittent or continuous feeding is more efficacious. The aim of this review is to examine the current evidence comparing the effectiveness of intermittent versus continuous feeding in stroke patients in terms of nutritional status, gastrointestinal intolerance and other complications.
Methods: A systematic review of randomized controlled studies comparing intermittent with continuous nasogastric feeding in acute stroke patients was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Metaanalyses) guidance using predefined search terms. The search was conducted in MEDLINE and EMBASE up to 1st March 2019. Two independent reviewers assessed study quality using the Joanna Briggs Institute Critical Appraisal Tool. Meta-analyses were conducted, where appropriate, using a random-effects model to pool risk ratio with corresponding 95% CI.
Results: Three studies including a total of 184 patients were identified. All three were medium to low quality. The definition of intermittent enteral nutrition within each study varied considerably in terms of volume, rate and mode of delivery. Achievement of nutritional targets was the same for both feeding patterns in the one study it was reported. Only aspiration pneumonia and diarrhea were measured by all three studies. There was no significant difference in the incidence of aspiration pneumonia (RR 0.91, 95% CI 0.53-1.57, p=0.74, I2=50%) and diarrhea (RR 1.74, 95% CI 0.70-4.30, p=0.23, I2=42%) between the two patterns of feeding. Other outcomes including, vomiting, gastric retention, mortality, pre-albumin and nasogastric tube complications showed no significant differences.
Conclusion: There is very little and low-quality evidence to inform patterns of enteral feeding after stroke. The available evidence shows no significant difference in nutritional achievement and complications between intermittent and continuous nasogastric tube feeding in acute stroke patients.
Keywords: Stroke; Enteral; Nutrition; Nasogastric; Dysphagia
Background
Dysphagia occurs in up to 50% of patients following a stroke [1- 4] and increases the risk of pneumonia almost ten-fold [5]. Strokerelated pneumonia is associated with longer length of hospital stay, worse levels of disability and increased mortality [6-9]. In most dysphagic patients, adaptation of the consistency of diet and fluids is sufficient to ensure that the swallow is safe. However, in a small proportion insertion of a Nasogastric Tube (NGT) is required to ensure safe and adequate nutrition. Despite this, more than twothirds of NGT-fed stroke patients still develop pneumonia [10] Gastric dysmotility is a well-documented phenomenon that occurs in critically ill patients, including acute stroke patients, whereby incomplete gastric emptying results in stasis, heightening the risk of reflux and aspiration of gastric contents [10-13]. NGT bolus feeding was first described by Morrison et al. [14] in 1895 for children with Diphtheria, who received 6-ounce bolus feeds 3 times a day via NGT. However, it wasn’t until 1910s when Morgan et al. [15] and Jones et al. [16] began administering their enteral feeds “drop by drop” rather than as a bolus. Contemporaneously, the regimen most frequently used in most patients requiring enteral feeding is continuous (i.e. low volume pumped feed lasting 16-24 hours without interruption). However, recent attention has been afforded to examining whether a discontinuous feeding strategy - often described as either intermittent or bolus (i.e. high volume of feed administered over a short period multiple times a day) - could reduce patients’ risk of pneumonia and achieve better nutrition and digestive tolerance.
Intermittent feeding reflects normal human feeding patterns more closely than continuous feeding. A period of fasting interrupted by the ingestion of a discrete meal causes gastric distension and subsequent stimulation of gut motility, secretion of digestive enzymes and metabolic responses to nutrient loading [17- 18]. This physiological gastrointestinal response to intermittent feeding has been demonstrated in healthy adults, neonates and intensive care populations [17-20]. While there are good theoretical reasons to assume that intermittent feeding is more physiological, most stroke patients in the UK receive nasogastric feeding continuously, as there are concerns that intermittent feeding may be less well tolerated. Guidance and practice relating to enteral feeding after stroke differs between countries; with the American Heart Association [21] and the Royal College of Physicians [22] not addressing the issue, Australian Guidelines allowing for both options [23] and intermittent feeding described as “traditional” in China [24]. The aim of this systematic review is to determine whether there are differences in the achievement of adequate nutrition, gastrointestinal tolerance, and metabolic stability between intermittent and continuous nasogastric feeding.
Methods
This systematic review and meta-analysis were prepared according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [25].
Criteria for Considering Studies for this Review
The inclusion criteria for this review were:
a. Population: Acute stroke patients aged 18 or more with a nasogastric tube receiving enteral nutrition
b. Intervention: Intermittent enteral nutrition: by bolus, gravity systems or infusion pump several times a day with a rest between feeds
c. Control: Continuous enteral nutrition: with gravity systems or infusion pumps, without interruption for a minimum period of 12 hours/day
d. Outcomes: Nutritional status, aspiration pneumonia, diarrhea, vomiting, gastric distension, gastric retention, hyperglycemia, pre-albumin, mortality, length of stay, and NGT complications
e. Study Design: Randomized controlled trials or pseudo-randomised controlled trials (a study without true randomisation) that compared continuous and intermittent enteral feeding methods.
Search Strategy
A literature search was performed using MEDLINE (1966 – 1st March 2019) and EMBASE (1974– 1st March 2019). Studies were searched for using the terms enteral, nutrition, nasogastric, gastrointestinal, feeding as Medical Subject Heading (MeSH) and free text terms. These were combined with the set operator “AND” with following terms: intermittent, continuous as both MeSH and free text terms. Publications were restricted to those studying adult populations, defined as greater than 18 years old, with a documented diagnosis of stroke according to accepted international criteria [26]. This search strategy is described in Appendix 1. The reference lists of all eligible studies that were identified were also comprehensively searched for studies not identified using the initial search strategy. This search was performed independently by two reviewers.
Selection of studies
Two reviewers (GDP and ET) assessed the studies independently for inclusion using the title and abstract. In cases where relevance could not be determined solely from the abstract, the full text was consulted. Any disagreements were resolved by consensus with a third reviewer (CR).
Data extraction and management
Data extraction was done manually by two reviewers (GDP and ET). Differences were discussed and adjudicated in faceto- face meetings. Foreign language papers were translated, and descriptions of each study were derived. This included authors, year of publication, type of participant, location, study design, sample size, age and gender of participants, exclusion criteria, when feeding was started, monitoring period, nasogastric tube size, type of feed and definitions of each intervention. In addition, data was extracted for definition and results of each outcome from all studies.
Assessment of risk of bias in included studies
Methodological quality of the studies was assessed using the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (MAStARI) Critical Appraisal tool for experimental studies [27].
Data synthesis
The studies presented in this review all fitted the conceptual definitions of intermittent and continuous enteral nutrition, as outlined in the inclusion criteria. However, there were differences in the volume, rate and temperature of nutrient delivered. In addition, two of the studies did not use true randomisation. Taking into consideration these limitations, a meta-analysis has been carried out with the outcome’s diarrhea and aspiration pneumonia, as these were the outcomes assessed by all studies. Narrative synthesis was used where outcomes did not allow meta-analysis. The meta-analysis was performed using Review Manager (RevMan) Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. Data was extracted from all three studies for the outcome’s diarrhea and aspiration pneumonia. We calculated risk ratios (RR) and 95% CIs using the Mantel–Haenszel model. Statistical heterogeneity among trials was assessed by the I2 test, with I2 >50 representing possible substantial heterogeneity. The meta-analysis was performed with a random‐effects model irrespective of the level of heterogeneity as the included trials varied considerably in a number of methodological features.
For more Neurology and Brain Disorders Journals please click on below link: https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link: https://lupinepublishers.com/
#Lupine Publishers#Lupine Publishers Group#OJNBD#Neurology Journal#Online Journal of Neurology and Brain Disorders
0 notes
Text
Lupine Publishers| Concomitant Cervical Spine Infection with Mycobacterium Tuberculosis and Pyogenic Bacteria Causing Spinal Cord Compression

Lupine Publishers| Journal of Neurology and Brain Disorders
Case Report
A 57-year-old man presented to the emergency room with neck back pain for about 2 months, unresponsive to nonsteroidal antiinflammatory drugs and progressive course of upper and lower extremity weakness with no sphincter dysfunction. The patient had no predisposing risk factors such as recent spinal surgery, trauma, instrumentation, distal site of infection, immunosuppression, diabetes. He was apyrexial. Physical examination showed marked mid neck tenderness, no palpable masses were felt, no lymph nodes were felt. Neurological examination of his extremities, spasticity was positive, and power was decreased 3/5 in both lower extremities, 2/5 in both upper extremities. Bilateral Babinski signs were present and deep tendon reflexes were increased.
Full blood count and biochemistry showed white blood cell count (WBC) 10,269/L (neutrophils 71.3%; lymphocytes 21.8%; monocytes 2.2%; WBC 4.4 to 11.3/L); C-reactive protein 13.86 mg/dL (0.1 to 6 mg/dL). Magnetic Resonance imaging of the cervical spine showed the collapsed body of C4 with epidural abscess formation, complicating with spinal cord compression. He underwent urgent anterior cervical decompression and evacuation of anterior epidural abscess with fusion. The material underwent histologic examination and aerobic, anaerobic, fungal, mycobacterial cultures. A tuberculous granuloma was detected on histology. Ziehl-Neelsen stain confirmed the diagnosis. Cultures also detected Staphylococcus aureus. Treatment was started with rifampin (600 mg), Isoniazid (300 mg), ethambutol (25 mg/kg), pyrazinamide (25 mg/kg), and levofloxacin 750 mg for two months. This was followed by seven months of isoniazid and rifampin. The patient was referred to rehabilitation. One year later, the patient is able to walk independently, and the back pain is gone.
Spondylodiscitis can be etiologically classified as pyogenic, granulomatous (tuberculosis, brucellosis, or fungal infection), or parasitic. Pyogenic spondylodiscitis commonly affects the lumbar column and more rarely affects the thoracic and the cervical column [1,2] (Figure 1). S. aureus is the predominant pathogen in pyogenic spondylodiscitis, followed in older people by enterobacteria, mainly Escherichia coli, Proteus, Klebsiella, and Enterobacter [2-4]. Mycobacterium tuberculosis is the most common cause of spondylodiscitis worldwide. Tuberculosis affects mostly the thoracic spine and involves two or more vertebral segments. The main contamination routes are hematogenous spread, external inoculation, or involvement from adjacent tissue [5]. Isolation of pyogenic bacteria from an abscess may guide the clinician to disregard the possibility of spine tuberculosis. It is recommended, therefore, to made mycobacterial culture and histopathological examination for all suspicious cases even when there is positive culture of pyogenic bacteria.
For More Neurology and Brain Disorders Journals Please click on below link
https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link https://lupinepublishers.com/
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
#Lupine Publishers#Lupine Publishers Group#Online Journal of Neurology and Brain Disorders#OJNBD#Neurologyjournal
0 notes
Text
Lupine Publishers| Neurological, Neuropsychiatric and Psychiatric Symptoms During COVID- 19 Infection and After Recovery: A Systematic Review of Observational Studies

Lupine Publishers| Journal of Neurology and Brain Disorders
Abstract
Background: The SARS-CoV-2 virus causes a wide spectrum of disease severity. Initial manifestations include fever, dry cough, and constitutional symptoms, which may progress to respiratory disease. There may also be neurological and psychiatric manifestations, involving both the central and peripheral nervous system.
Methods: We performed a literature search of the databases PubMed, EMBASE, The Cochrane Library and Web of Science for observational studies reporting neurological, psychiatric, and neuropsychiatric effects of COVID-19. This was followed by a narrative synthesis to summarise the data and discuss neuropsychiatric associations, symptom severity, management, and recovery.
Findings: The most frequently reported neurological symptoms were ageusia, hyposmia/anosmia, dizziness, headache, and loss of consciousness. Statistically significant relationships were noted between Asian ethnicity and peripheral neuropathy (p=0·0001) and neuro-syndromic symptoms (p=0·001). ITU admission was found to have a statistically significant relationship with male sex (p=0·024). Depression and anxiety were also identified both during and after infection. The most frequent treatments used were intravenous immunoglobulins, followed by antibiotics, antivirals, and hydroxychloroquine; with mean treatment duration of 6 days.
Interpretation: Various neuropsychiatric symptoms have been associated with COVID-19 infection. More studies are required to further our knowledge in the management of neurological and psychiatric symptoms during and after COVID-19 infection
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARSCoV- 2) is a novel virus, initially discovered in the city of Wuhan, China [1]. SARS-CoV-2 causes coronavirus disease (COVID-19), which has led to an ongoing global pandemic. Despite belonging to the coronavirus family, which usually cause self- limiting upper respiratory tract infections, SARS-CoV-2 is often more virulent than most coronaviruses and may lead to severe respiratory disease [2].
The mechanism of action for SARS-CoV-2 may relate to a specific tropism for respiratory tract mucosal cells through the attachment of viral surface proteins to angiotensin-converting enzyme (ACE) 2 receptors [3]. After infection, the virus causes a wide spectrum of disease severity, with most patients suffering a mild self-limiting disease. Initial manifestations include fever, dry cough and constitutional symptoms (headache, fatigue, myalgia, arthralgia), progressing to respiratory disease of mild to moderate severity [2,4]. Other disease manifestations include gastrointestinal symptoms (nausea, vomiting, diarrhoea), sore throat, skin rashes, anosmia, ageusia, and chest pain [5]. In patients with underlying comorbidities or advanced age, the infection may be complicated with acute respiratory distress syndrome (ARDS), acute renal failure, sepsis, multi-organ failure and death [6,7]. As the pandemic of COVID-19 persists, the knowledge of the clinical disease spectrum is still unfolding. Medical literature of COVID-19 infected patients reveals a variety of extra-pulmonary organ involvement [8]. Among these, COVID-19 has been associated with several neurological and psychiatric effects, involving both the central and peripheral nervous system [9].
Methods
This systematic review follows the Preferred Reporting Items for Systematic reviews and MetaAnalyses (PRISMA) statement [10] and was registered in the PROSPERO International Prospective Register of Systematic Reviews (number CRD42020203770 at www.crd.york.ac.uk/PROSPERO).
Search Strategy
The literature search was performed in August 2020 using the databases PubMed, EMBASE, The Cochrane Library and Web of Science, from their respective inception dates. The following search terms were used:
(Neuro* OR Nervous OR Psychiatry* OR Mental) AND (COVID OR Corona*)
The search strategies incorporated both medical subject headings (MeSH) and free-text terms, which were adapted according to the database searched. Grey literature was also searched. Reference lists of the identified papers and reviews were hand-searched. Publication languages included English and Greek. There were no publication period restrictions.
Inclusion and Exclusion Criteria
Included studies were observational studies reporting neurological, psychiatric, and neuropsychiatric effects of COVID-19. The included participants were COVID-19 patients of any ethnic origin, sex/gender, age, country, and were either actively infected from COVID-19 at the time of the study or had recovered. We did not include studies examining psychiatric effects on the general population as an indirect result of the pandemic.
Main Outcomes
The main outcomes included neurological, psychiatric, and neuropsychiatric effects of COVID-19, either based on clinical diagnosis or relevant diagnostic questionnaires. Information about recovery and treatment was reported when available.
Screening
Titles were screened for inclusion, followed by screening of abstracts, and then content. One author (SS) screened the papers, and any disagreements were resolved by discussion with the review’s primary author (MS) and the other authors.
Data Extraction
The Cochrane good practice data extraction form was used for data extraction. Data extraction from reviews involved the NICE extraction form, and the data were extracted in an electronic format.
Risk of Bias/Quality Assessment
The quality and risk of bias were assessed by the Mixed Methods tool for Appraisal (MMAT). The guidance from the Centre for Reviews and Dissemination was used for the appraisal of review papers. Discrepancies were resolved by discussion within the authors’ team.
Strategy for Data Synthesis
We performed a narrative synthesis review of original studies and reviews reporting neurological, psychiatric, and neuropsychiatric effects in COVID-19 patients.
We summarised the data and discussed:
a) Neuropsychiatric associations
b) Symptom severity
c) Management and
d) Recovery
Information from the various identified studies was analysed, summarised, and compared.
Results
Following our literature search, we identified a total of 7,460 papers. After removing the duplicated and irrelevant papers, 328 full text articles remained to be assessed for eligibility using the inclusion and exclusion criteria. Of these, 313 studies were included in the final narrative synthesis: specifically, 307 studies for neurological symptoms and 7 studies for psychiatric symptoms, as shown in Figure 1. A total of 15 full text papers were excluded as they were either not relevant (n=4) or unrelated to COVID-19 infection (n=11).
Figure 1: PRISMA flowchart of selected studies.
Neurological Symptoms
A total of 307 studies for neurological symptoms were included in the narrative synthesis, as mentioned above, of which 202 were case reports, 53 case series, 2 retrospective studies, 21 cohort studies, 15 systematic reviews, 8 cross-sectional studies, 3 casecontrol studies, and 3 retrospective case series. A summary of the studies included in the systematic review is shown in Table 1, and a complete list of the studies is provided in Supplementary Material 1. The mean age of the patients included was 55·11 (±17.91) years. Most of the patients in our cohort were males (61%) and the majority of the participants were Asians (57%).
Table 1: Summary of studies included in the systematic review for neurological symptoms.
Clinical Presentation
A total of 107 studies (42·7%), involving 26,758 patients, included a full account of neurological symptoms experienced by the participants following COVID-19 infection. Table 2 presents the frequency of symptoms and their resolution. The most reported symptoms were ageusia (n=390), hyposmia/anosmia (n=480), dizziness (n=230), headache (n=860), and loss of consciousness (n=310).
Table 2: Frequency and recovery rates of different COVID-19 neurological presentations.
Moreover, a significant number of patients experienced severe neurological manifestations, such as seizures (n=260), acute cerebrovascular events (n=500), cerebellar syndromes (n=70), peripheral neuropathies (n=90), meningitis/encephalitis (n=380), encephalopathies (n=380), neurological syndromes such as Guillain-Barre syndrome (n=320), and spinal cord syndromes (n=30).
A statistically significant relationship was noted between ethnicity and peripheral neuropathy (p=0·0001) as well as between ethnicity and neuro-syndromic symptoms (p=0·001), with Asian patients being more likely to experience these symptoms. Both sexes were statistically as likely to present with symptoms of ageusia (p=0·0001), dizziness (p=0·033), gastrointestinal symptoms (p=0·0001), and anorexia (p=0·0001). However, flu-like symptoms were statistically more prevalent in females (p=0·008), whereas hyposmia (p=0·037) and haemoptysis (p=0·0001) was more frequent in males.
Following recovery from COVID-19 infection, a large proportion of patients demonstrated a complete resolution of their symptoms. Specifically, patients presenting with loss of consciousness and ageusia reported the highest resolution rates (93% and 92% respectively), while the patients that experienced spinal cord syndromes had the lowest resolution rates of their symptoms (33%).
Treatments
The most frequent treatments used in the studies analysed were intravenous immunoglobulins (IVIG) (20·17%), followed by antibiotics such as azithromycin (19·29%), antivirals (14·91%), and hydroxychloroquine (10·52%). However, a combination of therapies was required for treatment in some patients. Figure 2 illustrates the different types of drugs that the COVID-19 patients received during their admission and how the drug therapy is markedly heterogeneous among this group of patients.
Figure 2: Drug type administered to COVID-19 patients.
The most common route of drug administration was intravenous (65%), although oral drug administration and intramuscular injections were also utilised. Patients received treatment for a mean duration of 6 (±4) days.
Prognosis
Patients admitted to an Intensive Therapy Unit (ITU) were reported in 126 studies. Figure 3 shows the different types of management that patients received when admitted to ITU and illustrates that the most common cause of ITU admission was the need for respiratory support with intubation and mechanical ventilation (84% of the cases).
Figure 3: Types of ITU management received by patients.
ITU admission was found to have a statistically significant relationship with males (p=0·024), but not age. Interestingly, there was a statistically significant relationship with ITU admission and symptoms of hyposmia/anosmia (p=0·0001), headache (p=0·035), acute CVA (p=0·0001), seizure (p=0·001), meningitis (p=0·034), and encephalopathies (p=0·0001).
Psychiatric Symptoms
We identified seven studies reporting psychiatric effects, of which five were cross-sectional studies, one was a retrospective cohort study, and one was a case report. Details of the six studies are reported in Table 3. The studies involved 299,000 patients in total, of which 44% were male and 56% were female. Half of the studies were reported in China. Three studies involved 171 patients in hospital settings while having active COVID-19 infection, three studies involved 498 patients at home after recovery, and one study involved 62,354 patients covering both inpatients during infection and those at home after recovery. All studies identified depression and anxiety as being relevant to COVID-19 infection, both during and after infection. Additionally, one study reported suicidality during infection, two studies reported post-traumatic stress disorder after infection, one study suggested obsessivecompulsive disorder after infection, one study suggested insomnia after infection, one study suggested a higher incidence of psychosis, and two studies suggested a higher incidence of dementia diagnosis as being relevant to having been diagnosed with COVID-19.
Table 3: Studies reporting psychiatric effects related to COVID-19 infection.
Discussion
The literature published on the neurological symptoms observed in patients with COVID-19 is vast. Through our review, we aimed to summarise all available literature, as well as include more recent studies that older reviews may not have included. Our review specifically served to identify and examine the frequency and severity of these symptoms through combining this existing literature. In total, 307 neurological studies covering 60,097 patients, were included in this systematic review, which has shown that COVID-19 is associated with a large variety of neurological symptoms. The most frequently reported symptoms included ageusia, hyposmia/anosmia, dizziness, headache, and loss of consciousness. These symptoms are not specific to SARSCoV- 2 infection and are of low severity, however they may suggest neurotropism. They also associate with high resolution rates (all >80%). The most common severe neurological complication of COVID-19 was acute cerebrovascular events. This result is in keeping with other systematic reviews [18,19].
Direct neurological damage including ischemic strokes, meningitis/encephalitis, or Guillain-Barre syndrome are relatively common extra-pulmonary neurological presentations according to our review. These results should be the springboard for further research efforts aiming to distinguish whether these neurological entities are a consequence of direct brain injury/infection or an interaction with other vascular comorbidities of patients suffering severe/critical COVID-19 disease.
A significant proportion of COVID-19 patients were asymptomatic due to the course of SARS-CoV-2 infection. In addition, patients may not present with respiratory symptoms or fever but still have initial neurological manifestations. Thus, when patients present with neurological symptoms, despite the absence of respiratory symptoms, clinicians should maintain a high level of clinical suspicion for the possibility of underlying COVID-19 asymptomatic infection.
The resolution rates of neurological symptoms also varied. Patients presenting with loss of consciousness and ageusia reported the highest resolution rates (93% and 92% respectively), with ageusia resolution rates being 100% in one study [20]. On the other hand, patients who experienced spinal cord syndromes, such as acute myelitis, had the lowest resolution rates of their symptoms (33%). This finding is supported by the established poor overall outcomes associated with acute myelitis, with only approximately one-third of patients experiencing a favourable outcome [21].
A statistically significant relationship was noted between Asian ethnicity and peripheral neuropathy. The relationship between ethnicity and peripheral neuropathy in the context of COVID-19 has yet to be explored. However, peripheral neuropathy as a complication of diabetes has been found to be more prevalent among Caucasian patients [22] and less common in those with Indo- Asian and African- Caribbean origins [23]. Moreover, a statistically significant relationship was noted between Asian ethnicity and neuro-syndromic symptoms. Nonetheless, it is important to note that both of these relationships may have been influenced by the fact that the majority of the participants in the studies included were Asian and that a number of papers did not disclose the ethnicity of their participants.
Additionally, flu-like symptoms were statistically more prevalent in females, possibly because males have been found to have a higher risk of severe illness with COVID-19 [24]. Hyposmia and haemoptysis were statistically more prevalent in males. This is in contrast to several previous studies that found hyposmia to be more common in females with COVID-19 infection [25-28]. However, our patient cohort was predominantly male (62%), which may have contributed to the differing results. Regarding haemoptysis, it is a very uncommon presentation that was only present in 10 patients.
ITU admission was found to have a statistically significant relationship with male sex, but not with age. A meta-analysis of patients with COVID-19 also demonstrated a relationship between sex and ITU admission, with male patients having almost three times the probability of requiring ITU admission compared to females [29]. Surprisingly, our study did not determine any relationship between age and ITU admission. In contrast, another meta-analysis found that patients greater than 70 years old have a higher risk of needing intensive care [30]. Furthermore, there was a statistically significant relationship between ITU admission and the symptoms of hyposmia/anosmia, headache, acute CVA, seizure, meningitis, and encephalopathies.
Treatment varied, with several different therapies and drug routes being used depending on the neurological manifestation and severity of the presentation. The most frequent treatments used were intravenous immunoglobulins (IVIG), followed by antibiotics such as azithromycin, antivirals, and hydroxychloroquine, with patients receiving treatment for a mean duration of 6 days. A systematic review assessing treatment strategies for COVID-19 similarly found antivirals, antimalarials, and antibiotics to be the mainstay of treatment [31]. The frequency of IVIG can be attributed to its use in treating many different neurological conditions, most notably Guillain-Barre Syndrome, which was the fourth most common neurological complication reported in this review. Finally, it is important to consider that the COVID-19 pandemic is rapidly evolving and that treatment options are continually being trialled and developed.
Even though we established an abundance of studies for neurological symptoms, there appears to be a lack of studies regarding the psychiatric effects during and after COVID-19 infection. Nonetheless, all the studies we were able to identify reporting psychiatric effects have found depression and anxiety to be relevant, both during and after infection with COVID-19. In severe cases, there may even be a risk of patients attempting suicide. Compared to people who had flu or other respiratory tract infections, COVID-19 survivors were more likely to receive a diagnosis of anxiety of depression over the same period [17]. It was found that involving psychiatric care for these patients was effective in reducing their symptoms of anxiety and depression. Without proper psychiatric intervention, there is a risk that these psychiatric symptoms could increase the risk of suicidal ideation. Overall, it is recommended that psychiatric and/or psychological support should be available in hospitals to patients admitted to medical wards due to COVID-19, as well as in the community following recovery. This process may involve both the use of pharmacological and/or psychological interventions. Given the fact that COVID-19 survivors were at higher risk of receiving a diagnosis of dementia at 6-months follow-up, access to memory clinics should also be available to this group of patients. More studies examining the short-term and long-term psychiatric effects during and after COVID-19 infection are required in the future to obtain a better understanding of the symptoms, as well as to develop effective management strategies.
For more Neurology and Brain Disorders Journals click on below link
https://lupinepublishers.com/neurology-brain-disorders-journal/
For more Lupine Publishers Please click on below link https://lupinepublishers.com/
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
#Lupinepublishers#LupinePublisherGroup#Journal of Neurology#Journal of Neurology and Brain Disorders#OJNBD
0 notes
Text
Lupine Publishers| Cervical Tarlov Cyst Mimicking Spinal Hydatid Disease: Case Report

Abstract
Go to
Background: Perineurial (Tarlov) cysts are usually incidental findings during magnetic resonance imaging of the lumbosacral spine. The Cervical localization have been reported to be a rare occurrence. We report such a case where a high cervical perineural cyst was masquerading as a spinal hydatid disease.
Case Presentation: We report a case of symptomatic cervical Tarlov cyst in a 9 years old girl operated on twice for pulmonary and hepatic hydatid cyst. Spinal magnetic resonance imaging (MRI) showed an extradural intraspinal lesion with fluid-equivalent signal extending from C5 to T2. Based on the history, the diagnosis of spinal hydatid disease was suggested. Surgical excision of the cyst resulted in significant improvement in patient symptoms, and histological examination revealed the diagnosis of a Tarlov cyst.
Conclusion: Cervical perineural (Tarlov) cyst can be symptomatic by causing nerve root compression and can be mistaken as a spinal hydatid disease on imaging. Surgical treatment can be curative.
Keywords: Tarlov Cyst; Hydatid Cyst; Diagnosis; Management MRI; Cervical Spine
Abbreviations: TC: Tarlov Cyst; CSF: Cerebrospinal Fluid; MRI: Magnetic Resonance Imaging
Introduction
Go to
Tarlov Cyst (TC) is defined as a cystic dilatation between the perineurium and endoneurium of spinal nerve roots, located at level of the spinal ganglion and filled with Cerebrospinal Fluid (CSF) but without communication with the perineurial subarachnoid space [1]. It is most often found in the sacral spine with a prevalence of 4.6% in the general population with about 13% of those being symptomatic [1,2]. The Cervical localization have been reported to be a rare occurrence [3], to our knowledge there are only five published cases of symptomatic cervical Tarlov cyst [4]. MRI of the spine is the gold standard imaging modality for the diagnostics. This is a case report of a symptomatic cervical TC that was masquerading as a spinal hydatid disease. To our knowledge, only five other cases of symptomatic cervical TC have been published [3,4].
Case Presentation
Go to
A 9-year-old girl, with medical history of surgery for pulmonary and hepatic hydatid cysts at age of 8, treated with anthelmintic with good outcome. As far as her past medical history is concerned, there were a history of cervical plexus trauma at the age of 6 with monoparesis sequelae of the left arm. She presented with a 4-week history of gradually developing left hemiparesis. On clinical exam, all deep tendon reflexes were normal. Proximal muscle strength of the left leg and the ipsilateral upper extremity was 3/5. Electromyography (EMG) showed abolition of motor and sensory responses of nerves SPE and SPI on the left upper limb. MRI of the cervical spine showed intraspinal cystic lesion of extra-Dural location lateralized to the left, extending from C5 to T2 causing a stenosis of the adjacent foramina, without contrast enhancement of the cyst wall (Figure 1). Based on the imaging and the history of patient, the diagnosis of a spinal hydatid disease was suspected. Neurosurgical indication was agreed, and the patient underwent a C4-T2 laminotomy (Figure 2), intraoperatively, cystic lesions strongly adhered to the dural mater with an appearance that was evoking congenital cysts. At this point, we opened the capsule and a clear CSF-like liquid came out from the cyst, we conducted a careful excision with Dural plasty. The histological examination showed fibrous tissue and the presence of neural elements, which is typical for perineural cysts. Postoperatively, the patient experienced significant improvement in her symptoms, represented by improved left lower-limb strength. A postoperative MRI of the cervical spine was performed after 6 months showed no recurrence of the cyst (Figure 3).
For more information about Online Journal of Neurology and Brain Disorders archive page click on below link
https://lupinepublishers.com/neurology-brain-disorders-journal/archive.php
For more information about lupine publishers click on below link
https://lupinepublishers.com/index.php
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
0 notes
Text
Lupine Publishers| New Year Wishes
Lupine Publishers| Journal of Neurology

Wave goodbye to the old and embrace the new with hope, dreams, and ambition. Wishing you a Happy New Year full of happiness!
#Neuroscience#Neurology and Brain Disorders#neurology#brain development#brain disorders#brain#Lupinepublishers#Lupine publishers#Lupine Publishers Group
0 notes
Text
Lupine Publishers| The Extra Dural Hematoma Complicating a Decompressive Craniectomy about One Case
Lupine Publishers| Journal of Neurology

Abstract
Go to
The extra-dural hematoma or epidural hematoma is a collection of blood formed between the dura mater and the internal table of the skull bone. The origin is traumatic most often causing an arterial lesion more particularly of the meningeal artery; this explains the topographical predilection of extra dural hematoma for the temporal zone with 50% of cases according to (BRICOLO 1984); rarely the cause may be a post-traumatic lesion of a venous sinus or a bone bleed at the level of the fracture site. In this respect, 5 to 10% of forms without fracture exist (BRICOLO 1984). Classic in traumatology and more readily the young subject 60% between 10 and 40 years. Beyond 60 years the dura matter adheres to the internal table of the bone and gives it a less releasable character in the area of Gérard Marchand which explains the rarity of this lesion after 65 years.
Case Report
Go to
Mr A. M, 21 years old, with no notable antecedents, smoking and alcoholism known as a motorcycle accident victim overturned by a car with a cranial impact point followed by immediate loss of consciousness, picked up by firefighters and sent to the emergency room; at admission the clinical examination found that the patient is unconscious, he smelled alcohol with a Glasgow score estimated at 7/15, hemodynamically stable and blood pressure 120/60mmhg. Neurologic examination found a left anisocoria bilateral palpebral contusions with stigmata of otorrhagia in tthe left auditory canal, the rest of the clinical examination was normal. The body scan demonstrated foci of left and right parietal basal temporal hemorrhagic contusions were observed, diffuse cerebral edema with mass effect on the left ventricle and two non-displaced fracture lines of the right parietal bone. On the cervical and abdominal there was nothing to signal. The patient was intubated, sedated and ventilated and then sent to the operating room for a left fronto-temporoparietal decompression with a sub temporal craniectomy (Figure 1). The Intervention happened without incident, the patient remained intubated, sedated and ventilated. On day 1, a cerebral CT scan is performed and shows a voluminous contralateral frontal-temporal-parietal extra-dural hematoma with deviation of the median line and herniation of the brain through the craniectomy and a quasi-right hemisphere ischemia. The time to return to the operating room to evacuate the hematoma it makes the soul.
Discussion
Go to
Serious head injuries (GCS ≤ 8 [1]) remain a serious public health problem in developed countries because of the major sequelae they cause to a young and active population: approximately 43% of trauma patients cranial need a third person in everyday life [2]. The cranial box is an inextensible container, in which a physiological Intracranial Pressure (ICP) prevails, normally: 5 to 15 mmgh. PIC increases with slanting position, jugular vein compression, nociceptive stimuli, agitation, respirator mismatch, endothoracic pressure, hypercapnia, hypoxia, epileptic seizures, temperature, hyponatremia (Na <120mmol/ l) and Hypertension. The content of the skull can be divided into three parts: the brain parenchyma which accounts for 90% of the contents (including intra and extracellular fluids and the cell membrane), arterial and venous blood volume, and Cerebrospinal Fluid (CSF) which count for the remaining 10%.
As a result, an intracranial Hypertension that is a conflict between the container and the content can develop when it changes in volume of one of these three elements of the content:
a) Due to a process occupying space (hydrocephalus, hematoma, tumor).
b) Because of a cerebral edema reaction to a pathological process (head trauma, cerebral ischemia).
Only the volumes of CSF and blood (in its extra sinus venous portion) can be reduced to give space to the neo-volume, these are the only compensating elements. Once these compensatory mechanisms are exhausted, a small increase in volume leads to a significant increase in the ICP. Many pathological conditions are likely to lead to HTIC, of which cerebral edema seems to be the most common cause. The main risk of head trauma is the occurrence of HTIC incompatible with a sufficient Cerebral Perfusion Pressure (CPP) [3], and responsible for the mortality found in 50% of traumatized cranial [4], as shown by the curve pressure-volume of Langfitt. The decompressive craniectomy, by the removal of a large bone component associated with a sub temporal craniectomy and a plasty of enlargement of the dura mater, is proposed in certain refractory HTIC situations in a context of progressive secondary lesions. His indications are difficult to ask. Its use seems to be associated with an improvement of the vital prognosis but remains controversial with regard to the functional prognosis of the survivors [5].
Figure 1: Day zero Cerebral CT scan shows on the parenchymal window patches (B, C, D) of left temporo-parietal hemorrhagic contusion foci, diffuse edema with erasing of the basal cisterns and mass effect on the medial line and lateral ventricle. The bony window (A) shows a two contralateral non-displaced fracture line opposite some contusion focus.
This surgical technique was proposed in the early twentieth century to try to improve the prognosis of tumor resection surgery. Its effect is correlated with size of a craniectomy [6], observed at a scan by emergence of cisterns of a base and reduction of deviation of a median line. For twenty years, this technique has been used to treat refractory HTICs for any other treatment, especially after failure of barbiturate coma and hypocapnia. The study by Yoo et al, proves the effectiveness of this technique on the reduction of intracranial pressure. This work shows the rapid decrease in intraventricular pressure immediately after bone decompression (decrease of 50±16.6% of the initial value), the opening of the dura allowing a decrease in intracranial pressure of approximately 34.5% [7]. Historically, decompressive craniectomy has been used to treat intracranial hypertension secondary to Reye’s syndrome in children [1,8]. Stefini et al. [9] have reported good results after craniectomy for the treatment of hemorrhagic infarction secondary to venous sinus thrombosis. In the surgical treatment of spontaneous hematomas, Dierssen et al. [10] found a significant improvement in the mortality rate in treated patients by evacuation of the hematoma with craniectomy compared to a series treated only by evacuation of the hematoma. Complications of the Decompressive Component [11,12].
Complications of Craniectomy can be Divided into: a) Early complications dominated by hematomas.
b) Secondary complications, mainly: Hydrome and infections
. a) Early Complications: [13] Precociously, hemorrhagic complications and hematomas are the main complications. Decompression and decline of ICP are likely to promote the development of contralateral acute or extradural subdural hematoma. The increase in haemorrhagic lesions with craniectomy has been described as being favored by small flaps that promote the formation of localized cerebral hernias. These complications and the continuation of intensive care surveillance justify the establishment or maintenance of postoperative monitoring of ICP.
b) Secondary Complications: After decompressive surgery, the brain undergoes several changes regarding: hemodynamics with venous drainage, cerebrospinal fluid movement, and general metabolism. This is more clinically evident in patients who experience improvement and subsequent deterioration of neurological status within a few weeks to months after decompressive craniectomy with concave depression above the flap site. This phenomenon has been described as the scalp flap syndrome. The neurological signs may be limited to fatiguability, discomfort, depression, intolerance to vibration, headaches, more rarely sensory and / or motor deficits that may appear.
In 1977, Yamaura et al. [14] published a study of 33 patients with the scalp flap syndrome after craniectomy, and reported neurological improvement after bone segment reimplantation in 88% of patients with mild symptomatology published a study of 5 cases with neurological deterioration after craniectomy, which was improved by cranioplasty [15]. Some authors have explained the physiopathology of this phenomenon by the transmission of atmospheric pressure to the cranial cavity. The treatment of this syndrome consists in reconstituting the skull by a cranioplasty. Fodstad et al. [16] Studied cerebrospinal fluid dynamics before and after cranioplasty, and found an increase in cerebrospinal fluid pressure after cranioplasty in patients with this syndrome. Winkler et al., Studied the effect of cranioplasty on hemodynamics and cerebral metabolism, found improvement in blood flow and increased regional and general brain metabolism after cranioplasty. They also found that the increase in glucose metabolism after cranioplasty is a sign of good prognosis for patients operated on by decompressive craniectomy [17]. In one study, out of 23 patients with early cranioplasty, 8 weeks after the craniectomy, Liang et al, reported recovery of neurological signs in the majority of patients after early cranioplasty [18]. Other complications are not negligible, Yoo et al. [19]. reported an incidence of 13% d subdural hygroma and a 13% incidence of cranioplasty infection. To analyze infectious complications after craniectomy, a Moroccan study of a series of 170 patients operated by craniectomy, found infectious complications in 30 patients (17.60%) including 9 patients: scalp infection, 13 meningitis, 3 empyema, 3 abscesses and 2 osteitis. The risk factors identified were the urgency of the surgery, the duration of the surgery ≥ 200 minutes and the length of stay in the intensive care unit ≥72 hours [20-30]. Guerra et al, found infectious complications in 2% of the patients. patients included in this study, sub-dural hygroma in 26% and hydrocephalus in 14% [21, 31-45].
In a recent study by Rodrigo et al, among 89 patients treated with decompressive craniectomy for severe head trauma, the authors found 34.8% of patients who developed complications, with hydrocephalus in 7 patients (7.9%), subdural hydrome in 10 patients (11.3%) and infectious complications in 14 patients (15.9%). Aarabi et al, found in a series of 50 patients treated with decompressive craniectomy, hydrocephalus in 5 patients, hemorrhagic complications in 8 patients and subdural hydrome in 25 patients [9]. Polin et al, reported 28, 5% hydrocephalus after craniectomy [22,46-55]. Su, Ho and Wangont reported a case of subdural hydrome after decompressive craniectomy in a 63-yearold man who suffered a serious head injury resulting in a fronto subdural hematoma. -temporo-parietal with a mass effect. The condition of the patient improved after drainage of the hydromel [23, 56-59]. Kombogiorgas et al, made a retrospective study of 107 children treated with supra-tentorial decompressive craniectomy for several diagnoses, children who were presented with epilepsy are excluded, and the prophylactic anticonvulsant was given to 52% of children. 12% (13 children) developed epilepsy (predominantly female), 1.8% (2 patients) developed postoperative infection.
Conclusion
Go to
Figure 2: The CT scan done on J1 postoperative(E,F,G,H) shows a herniation of the cerebral parenchyma in a narrower opening of craniectomy with aggravation of foci of hemorrhagic contusion and diffuse edema erasing the cisterns of the base, an extra dural hematoma fronto-temporo-parietal right with quasi-hemispheric ischemia leading to a deviation of the median line and meningeal hemorrhage.
In relation to the literature, there are more cases of sub-dural hygroma, infection, post-craniectomy epilepsy and extradural hematoma [29]. This leads us to conclude that the controlateral extra-dural hematoma complicating the decompressive component is a real but rare entity whose pathophysiology can be explained by the existence of a post-traumatic contralateral bone lesion clogged by the hard-faced mother. reinforced by the cerebral parenchyma before the craniectomy, the existence of a small vascular lesion in this case the average meningeal artery or one of its branches compressed and pressed against the internal table of the bone by the cerebral parenchyma oedematous via the hard mother before the decompressive craniectomy. In this case the extra dural hematoma is developed after the lifting of the compression via the decompressive craniectomy with herniation of the cerebral parenchyma (Figure 2).
For more Lupine Publishers Open Access Journals Please visit our website:
https://lupinepublishers.us/
For more Open Access Journal of Neurology & Neurosurgery articles Please Click Here:
https://lupinepublishers.com/neurology-brain-disorders-journal/
#Neurology and Brain Disorders#Neuroscience#neurology#neuro#neuroscientist#brain development#brain#brain disorders#Lupinepublishers#Lupine publishers#Lupine Publishers Group
0 notes
Text
Lupine Publishers| Christmas wishes
Lupine Publishers| Journal of Neurology

May this festive season sparkle and shine, may all of your wishes and dreams come true, and may you feel this happiness all year round. Merry Christmas!
#Lupinepublishers#Lupine publishers#Lupine Publishers Group#Neuroscience#Neurology and Brain Disorders#neurology#neuro#brain#brain disorders
0 notes
Text
Lupine Publishers | The Terrible Triad Miracle
The terrible triad injury of the elbow is a fracture-dislocation injury consisting of a radial head fracture, coronoid fracture and dislocation of the elbow [1-5]. It was first described by Hotchkiss in 1996 and named so due to the poor outcomes experienced by these patients [1]. Despite surgical management these injuries often go on to develop various complications: recurrent instability, stiffness, posttraumatic arthritis, heterotopic ossification and fixation failure. This injury is relatively uncommon and studies attempting to analyze outcomes often have a low number of subjects [1]. We present a case of a terrible triad injury with exceptional range of motion outcomes within a short time frame (Figure 1 and 2).

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Introduction: The terrible triad injury of the elbow is a fracture-dislocation injury consisting of a radial head fracture, coronoid fracture and dislocation of the elbow. This injury is relatively uncommon and despite surgical management these injuries often go on to develop various complications.
Case Presentation: Presented is a terrible triad elbow injury of the left elbow in an 18-year-old male. The patient underwent open reduction internal fixation of the elbow and achieved exceptional outcomes. The joint was adequately stabilized through addressing the coronoid fracture and highly comminuted radial head. He was subsequently followed in clinic and placed on a conservative rehab approach.
Conclusion: Despite recent trends, the joint was aggressively stabilized, and the patient was placed through conservative rehab. In this case, the patient was able to achieve satisfactory outcomes in a short period of time.
Keywords: Elbow; Fracture Dislocation; Terrible Triad Injury
Introduction
The terrible triad injury of the elbow is a fracture-dislocation injury consisting of a radial head fracture, coronoid fracture and dislocation of the elbow [1-5]. It was first described by Hotchkiss in 1996 and named so due to the poor outcomes experienced by these patients [1]. Despite surgical management these injuries often go on to develop various complications: recurrent instability, stiffness, posttraumatic arthritis, heterotopic ossification and fixation failure. This injury is relatively uncommon and studies attempting to analyze outcomes often have a low number of subjects [1]. We present a case of a terrible triad injury with exceptional range of motion outcomes within a short time frame (Figure 1 and 2).
Case Presentation
A healthy 18-year-old male presented to West Houston Orthopedics for evaluation of left elbow pain. He fell two days ago while skateboarding and was evaluated at an outside emergency department. He was diagnosed with a left elbow fracturedislocation treated at the time with reduction and splinting. At his initial orthopedic clinic visit, evaluation of radiographs revealed a reduced left elbow fracture-dislocation with a displaced, comminuted fracture of the coronoid and associated displaced, comminuted fracture of the radial head. CT scan of the elbow revealed displaced and extensively comminuted intra-articular fracture of the radial head involving at least 40-50% of the articular surface. The coronoid process was extensively comminuted with sublime tubercle involvement and likely the distal insertion of the ulnar collateral ligament (Figure 3). Mildly displaced fractures along the posterior capitellum were also identified. The patient was treated with open reduction internal fixation (ORIF) left radial head, ORIF coronoid process and lateral collateral ligament reconstruction 5 days after presentation to clinic. A single extensor digitorum communis splitting approach was used to gain access to the joint. The exposed radial head was in one large piece and several smaller pieces which included 3 pieces amenable to fixation. The anterior capsule incision was then extended to access the coronoid fracture. Fragmented cartilage pieces from the ulnohumeral and radiocapitellar joint were removed from the joint. An attempt to fixate a larger coronoid fragment was made; however, the piece further fragmented, and fixation was no longer possible. A 1.8 mm suture anchor was then placed for suture fixation of the anterior capsule following radial head fixation. The larger radial head fragments were reduced and fixated using two mini headless screws placed with compression.
The remaining coronoid fragments were removed from the joint and the Fiber Wire was used to fixate the anterior capsule to the remaining coronoid. Fluoroscopy confirmed reduction of the fracture with concentric joint reduction with the elbow flexed and supinated. The LCL was repaired using 0 Vicryl. The annular ligament was similarly repaired along the radial head and neck. Hard copy radiographs were obtained after closure and confirmed reduction of the fracture with concentric elbow joint reduction and placement of hardware. Table 1 highlights the post-operative management of this patient along with his active range of motion at each visit.
Discussion
The approach to surgical management of terrible triad injuries is still highly variable and outcomes are not well established. Giannicola et al. studied 78 elbows with complex elbow instability and found flexion, extension, pronation and supination at 3 months to be 131°, 18°, 76° and 72° respectively [2]. In a review done by Rodriguez-Martin et al. analyzing 137 elbow triad injuries from 5 studies following a protocol of fixation or replacement of radial head, fixation of coronoid fracture and repair of LCL complex, the weighted average flexion was 131.98°, extension was -16.19°, forearm pronation was 76.35° and forearm supination was 62.45° [3]. In this case, the patient was able to achieve full range of motion of his elbow at just 3 months post-op without pain or signs of heterotopic ossification. Several factors may explain the favorable outcomes: the patient was young and healthy, the anterior capsule was stabilized to the coronoid, the radial head was fixed rather than replaced and the patient was progressed cautiously with close monitoring in a hinged elbow brace. The patient was also kept in a static splint for the first month of treatment without motion or PT.
There is increasing support for active elbow motion days after surgery in order to recruit the dynamic stabilizers of the elbow [3]. The idea that the elbow should never be immobilized is often viewed as dogma [4]. In the case of this patient, a more conservative rehab approach was utilized secondary to concern that formal physical therapy might stress the fixation too soon. The patient remained immobilized until 4 weeks post-operatively, at which point a hinged elbow brace prescription was given. The hinged brace was not fully unlocked until 8 weeks post-op. Additionally, formal physical therapy was delayed because of confidence that this patient would be compliant with home exercises. Given patient compliance and close monitoring, he was given a home exercise program six weeks post-operatively and a formal physical therapy referral at eight weeks post-operatively. While there is growing consensus that the coronoid fracture should be addressed due to its role in humeroulnar sagittal stability [1-5]; Chemama et al. recommend that type 1 coronoid fractures may be neglected. In this case we opted to reinsert the capsule via anchors for improved humeroulnar joint stability [5]. In addition to coronoid stabilization, we fixated the native radial head despite it being in greater than 3 pieces. An argument can be made that fixation of the radial head should be attempted prior to replacement. Watters et al found that arthroplasty had similar results to fixation; however, they further concluded that long-term studies need to be performed to identify the impact of late complications of arthroplasty such as loosening. In a young patient, the risk of arthroplasty revision in the long run may outweigh the risks carried by fixation [6] (Figure 4).
Conclusion
We report a case of a terrible triad injury in a young male who achieved an exceptional outcome despite early and extended immobilization of the joint. Despite recent trends to mobilize the joint early, the patient was able to achieve satisfactory outcomes in a short period of time. Furthermore, the joint was adequately stabilized through addressing the coronoid fracture and fixating a highly comminuted radial head.
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
4 notes
·
View notes