#neurologynursing
Text
Patients who lie about their care
We’ve all seen that meme of the angry old lady with the words commenting on how she tells her family she hasn’t been bathed in days, even though she really just keeps refusing to be cleaned up. I’m sure many people have seen that meme as well as real life scenario in the hospital or even nursing home.
For the past year I’ve experienced some instances of this occurring where patients lie to family, other staff etc and throw the nursing staff under the bus.
First was a patient let’s called “Mr K”. He had a surgery that was painful, he had a low pain tolerance. Not only did he ask for pain medications (usually narcotics) but he demanded and raised his voice each time as well. When the nursing staff would explain the consequences of having too much, he would only raise his voice even more and have an angrier face on. When he became unresponsive, the staff tried every trick in the book they learn. He did no flinch even slightly at the most painful ways to arouse a patient awake. The doctors in the room had asked what he was given, the list was relayed by the patient’s nurse. The shock on the face of the doctors is something that cannot be explained with words or imitations. The patient was in the bed, eyes closed, barely breathing and the staff was scrounging to assess and get the supplies needed. In this case, NARCAN. The miracle drug being used on the streets more often than before. Easier to come by than insulin and Epipens. Narcan was given to this patient, a couple times, he finally woke up. Looking like he just woke up from a horrible drunk passed out evening of fun and puking. When he finally woke up enough to put the blame on somebody, he chose the nursing staff, of course. “Mr. K, we had to narcan you, you had taken too many pain medications too close together”. Mr K then followed up with this statement “I told the nurses not to give me anymore, but they kept pushing the pain meds on me, the nurses need to be more careful next time”. Moments like this will happen whether you want them to or not.
Most recently I had a patient who decided she enjoyed making me miserable. Let’s call her Mrs. P. She is a common frequent flier, always coming into the hospital for chronic issues and never seems to leave early enough. One of her fun activities, fun for her, is making the staff miserable and keeping us from our patients, even emergencies. The other day I was getting ready to give her medications. Then Mrs. P decided she would not take her meds until her bed was exactly how she wanted it. This comes after spending an hour in her room fixing her bed. After she refused her meds, i had to go help a patient out where time was of the essence. After I returned to see if Mrs. P would take her medications I got a call from my PCT that Mrs. P had told my boss that I wouldn’t give her her medications. I then had to go in the room with the patient, yes it was awkward, and tell my boss that the patient was not telling her the truth.
#neurologynurse#patientstories#benicetoyournurse#neuronurse#neurologynursing#learnfromexperience#jewishnurse#strokenursing#nurse#nurselife#registered nurse#storytime#medicalstories#medicalstorytime
2 notes
·
View notes
Video
Nurse life #Nurse #NurseLife #NurseAnesthetist #NursePractitioner #RegisteredNurse #LicensePracticalNurse #LicenseVocationalNurse #CardiologyNurse #PediatricNurse #ICUNurse #StepDowners #OncologyNurse #PulmonologyNurse #PodiatryNurse #DiabetesEducatorNurse #CRNA #HomeCareNurse #MessSearchNurse #PacuNurse #ScrubNurse #CriticalCareNurse #neurologynurse #NursingStudent #iwanttobeanurse #nursingrock #bnr https://www.instagram.com/p/B_dDnXbH7CO/?igshid=1cvii0rfdg8vq
#nurse#nurselife#nurseanesthetist#nursepractitioner#registerednurse#licensepracticalnurse#licensevocationalnurse#cardiologynurse#pediatricnurse#icunurse#stepdowners#oncologynurse#pulmonologynurse#podiatrynurse#diabeteseducatornurse#crna#homecarenurse#messsearchnurse#pacunurse#scrubnurse#criticalcarenurse#neurologynurse#nursingstudent#iwanttobeanurse#nursingrock#bnr
0 notes
Text
The strong and scary patients
Most of the people you come across as patients in the hospital won’t try to hurt you. Of the ones who do, some do it on purpose or on accident because of their medical condition. Both are no fun to deal with, the first one pisses me off more.
Awhile ago I had a patient, lets call him Mr. O. He was old, weak in his legs and got confused at night, sundowning as they call it. This occurred pretty quickly. The orientation questions we ask patients: Do you know where you are? What year is it? Is it daytime or nighttime? Who is the president? What is your name? Etc. The answers to these questions can change rapidly and quite drastically. The answers can go from semi normal to out of this world, literally. That’s a story for another time.
So this man, Mr. O, he was a very nice man normally, loved to chat and always kept himself busy with crosswords or coloring for fun. He also enjoyed a good documentary during the daytime when things got slow for his care. This sundowning that he did occurred without much warning, although I knew it would, just not when, it would happen. He first seemed to forget it was sleeping time. He began to think we were in his home. Then he thought it was a prison, which is a common confusion among patients who sundown. When someone looks frail and old, don’t underestimate their abilities to take you down during this confused state. The man didn’t feel pain from his massive surgery, didn’t even flinch when he tried to escape from the unit, eloping we call it.
He stayed in the hallway and wouldn’t leave. Screaming and disrupting our other confused patients, we tried to de-escalate the situation. The way that sounds makes it seem we chat and calm him and get things back to normal. If only this were true. He began to try to hit us, kick us and he even put a curse on us. Spitting usually comes with the territory. The easiest part of this, he had no drains attached or anything that would cause bleeding or limbs to fall off or break.
We had to call something that is basically a code for when a patient becomes uncontrollable in a situation where more people are needed and more specialists are needed, like psychology, to assess the situation. After we called this code, you could hear it overhead in the hospital speaker system. While other units probably could see a young person causing a disruption or a middle aged person becoming upset at their care, this was a very old person, who at first sight looked like he could fall with a simple push of your pinky. Let that be a lesson, don’t underestimate the strength in someone who doesn’t understand even the slightest bit of reality.
Multiple hospital officers came, along with the psych department, the patients surgical team as well as some people from the unit and head of nursing for the hospital staff. He began to try to throw punches that barely made the officers flinch, although I could see the surprise in their face when this happened. The staff that responded were calm, not shouting, nothing in their hands and kept their faces in a neutral look. Eventually the officers took a “walk” with the patient which led back to his room. Some medications, restraints and call to the family awhile later, solved the current problem at hand. However this was one night. For the rest of the stay, the patient had moments like this. Scary for the family, staff and patient as well.
During the following day, the patient was told why he had restraints on, he didn’t believe his ears. He had this sad face on, concerned about us and wanted to make sure nobody was hurt in this incident. It truly is sad when our minds are no longer under our control.
The next patient that I had with the same code announced was Mrs. Y. She wasn’t old, wasn’t young either, but strong in her arms and legs, not something you want in a confused patient. Her diagnosis wasn’t tricky or rare, seemed like a simple case of medications, physical therapy and rest. Despite the simple sounding diagnosis and treatment, it was far from it. She would become upset at the simplest little change in light or darkness in the room, staff members in the room and even when a medication was mentioned. The unpredictability became her biggest trigger. Ironically that part became predictable.
One day I was going to give her a medication, nothing extreme, it was one pill, not large and something she had taken before. I didn’t see it as something huge for her, but was cautioned just the same. As I walked in the room she became almost manic. She was rambling on about nothing, upset at my lack of response or understanding and seemed to be fed off of the simple reactions I had, even the non verbal ones. She had this look in her face, something I had seen in patients who attack their nurses or want to. I stayed by the door for a quick escape just in case. I left the room shortly thereafter and the room stayed calm for a bit. While cleaning up an incontinent patient I got a call. My gloves covered in poop, wipes all over the bed and not even close to finishing up with the patient. My PCT then got the phone from my pocket and I could hear a loud noise and words like “bed”, “sheets”, “tearing”, “belligerent”. None of the words sounded to get better as I listened to the conversation. I didn’t have to hear more to know what I was getting myself into, going back into that room.
I walked back to the room and found Mrs. Y on the top of the bed, sitting like a monkey with her knees to her chest, arms around her legs and food stuffed all around her. She had crumbs everywhere, medical supplies on the floor and this pacing look on her face. Pacing, closed fist and not talking are big non verbal cues of anger and a possible outburst. She showed all of the signs. She was in the perfect spot to fall, hit her head, end up with a TBI or worse, death. All nurses fear the day their patient falls and it’s not a simple day of paperwork or further education with the patient and their family members.
This patient, Mrs. Y, started to try to move from the bed, to the chair, to the doorway. She was becoming more manic by the second. I called in another nurse for backup and more manpower if needed. I then made the call I didn’t want to make. This usually opens a can of worms for some, however, she was well-known in the officer community at this hospital. Lots of these code strongs had been called for her. It normally required some medication, IM or IV depending on the incident in front of us, a psych consult and a report about what led you to call the code strong.
You would think a sedating medication would help with this, but no, it didn’t not. If anything it calmed the manic behavior, but continued her appetite for no sleep and more talking. Mrs. Y is a classic example of this code strong we call in hospitals. Luckily nobody was hurt and the patient was safe without any incident.
Saving the best one for last, of course.
Where would we be without the challenge that tests our abilities with language, bodily fluids and insults.
I had a shift once where I was talking with a patient about general medical concerns, nothing drastic. I could hear a loud noise, someone’s voice, but nothing specific. I opened the patient’s door and heard a language I couldn’t speak and loads of English where words like “calm down”, “don’t hit”, “my arm!” And more were said. I could tell the situation wasn’t getting any calmer so I decided to go assist the nurse with this patient. My language abilities aren’t vast and the ones I do know, besides English, I can survive shopping, asking about how people are and going to the bathroom. Nothing exciting or helpful in this setting.
I walk into the room and see an older lady, let’s call her Mrs. S, screaming at staff, trying to hit people, calling the nurses whores in her language and more that I am glad I didn’t understand. She didn’t have her dentures in, but despite this fact, she still attempted to bite the staff preventing her from falling off of the bed. Even with all of the effort put into this incident, we still had to make the call for a code strong. Officers came, psych came etc. It was a fiasco in two languages. It was as chaotic as it sounds, probably more. She continued to curse us, try to bite us, scratch us and more. It was more amusing than scary luckily.
It seems insensitive to call it amusing, however in the nursing world, if you can’t laugh at what stresses you out, you will go mad.
Code strongs are sometimes, but not always predictable. When they happen you need a good team of nurses, security, psychologists and more to assist with the patient and what is causing them to get aggressive or just in general, act out of character.
#neurologynursing#neuronurse#neurologynurse#codestrong#challenges#patientstorytime#patientstories#medicalstorytime#medicalstories#medical
0 notes
Text
Naked people
I got report from the night shift nurse, back when I did day shift, and had no idea what I was getting into. As usual the report was relatively normal for a neurology patient. They weren’t fully oriented and sometimes impulsive as well. As soon as I walked into the room, the patient was completely naked and confused as hell. They looked at me like I was an alien, possibly because I had clothes on.
Later on in the day the patient took their gown off again. After asking them nicely to let me put a new one back on them, first thing they said was “NO! MAKE ME!”
I’ve had older male patients refuse to wear their gowns, telemetry leads, socks, SCD pumps etc. They lay there on a bed, door open, sometimes screaming. When this happens I try to keep their family members less embarrassed by this. If your mom or dad was completely naked in front of you and hospital staff, how would you react? Probably not positively, maybe even a nervous laugh?
#neurologynurse#neuronursing#neuro#neurologynursing#learn from experience#patientstories#medicalstorytime#medicalstories#patientstorytime
0 notes
Text
Difficult patients and their family
While working with my patient one night I knew before I walked into the room that it would trust my abilities to be patient (something I am not known for) and ignore insults. Before I walked into the room I could hear muffling crying sounds and “kvetching” as us Jews call it. I opened their door, let’s call this pt Mrs. B., and found her shaking while holding the hospital phone, a distinct odor (most likely passing gas from having surgery), and her with this look on her face. Her face was scrunched in disgust, wet cheeks from crying and her hands trembling from stressing herself out. I introduced myself, with a smile on my face, asked her what I could do for her. First response I get out of my patient, whom I have never met before, was “Who the fuck are you? Can’t you see what’s wrong? This place is so full of confused people who don’t know anything.”
As someone who has been cursed out for no reason, by my patients, this wasn’t a big deal and didn’t get to me. During this time I had 3 other patients who were needing much more attention at this time. Spending more time a healthy patients room tends to happen more than we wish. Usually these patients take our attention because of the fact that they can speak, walk and complain. I had 3 others who either couldn’t communicate, needed total care assistance and giving their medications can take a long time.
This wonderful lady Mrs. B had me in there while she vented about many things. As she listed these issues I thought a few things in my head. 1) Why is she blaming me for something I wouldn’t know since I just met this woman. 2) None of this information is true, 3) Let me explain the correct information so the family doesn’t get conflicting information.
I attempted to calm her down however at certain times, there is nothing you can do. She wouldn’t get off of the phone and I wanted to prevent a conversation on both sides of her head. As someone who is already overwhelmed, I didn’t want to add to this distress. The moment she hit the red “hang up” button on the hospital phone she turned to me. Before I could even consider saying something she yelled at me again. I calmly spoke to her and offered my knowledge and resources to the doctor’s notes in the computer. She agreed, to my surprise.
I then read her the notes explaining why to her questions: Why this medicine? Why am I on contact precautions? Why am I quarantined? Why do I need these blood tests? Why do you need to test my urine? Why am I still here? Etc.
These questions I could answer with ease, as all answers are in the chart. After each answer I gave, I was met with more resistance from the patient. It seemed as though anything I could say, wouldn’t get what she wanted; something magical to get her pain free and less frustrated with the past experience in her current hospital stay. It had been a good amount of time after I left. After wearing the contact gown and gloves my body was sweaty, my hair stuck to my skin and I had my other patients to see, nurses needing a witness for insulin, nerve blocks and more that required my full attention.
As my hands were being dried with paper towels my hospital phone range with an outside number. As I threw the paper towel in the trash I knew what was coming. I was right, the patient’s family was calling to chew someone out and I was the person to chew out. It didn’t matter that I had only spoken to the patient once so far and that I didn’t give her the information that had upset her.
First words I hear on the phone “Hi, this is Mrs. B’s sister, is this her nurse for the night”? I immediately wanted to say no, but instead I said “Yes, my name is ********, what can I do for you?” they immediately went to their strong voices and accusations and confusion about the conversation. I then calmly had told them that this information was simply just a misunderstanding without setting blame on anybody. I decided education is the best way to prevent further issues. By the end of the conversation the family members on the phone were relaxed, relieved and no longer shouting. They thanked me for spending time with me on the phone and I said I was happy to clear up any confusion and fears they had.
When I went back to the door of the patient’ room I could hear her crying and calling her family once again. The same information she relayed the first time. Education is important for patients in the hospital, but you cannot control how much they absorb and understand, or want to understand.
Fast forward to the early morning hours of my shift and then comes the can of worms. I don’t mean a can that can be held in one hand, it’s more like a tub or massive tank of worms.
Sitting outside of the room charting away I could hear coughing and something that sounded like crying. She hit the call bell and my PCT when to go check on her. I can hear louder coughing, crying, whimpering and the words “trouble breathing”. These words mean a lot to a nurse, doctor etc. I jumped up from my chair, put my gown on and then went into the room.
I ask her to hear it in her own words. As she is coughing I hear “I can’t stop coughing and am having trouble breathing”. I grab the pulse ox near our vitals machine and turn towards Mrs. B. Immediately she gives me a look of hate and confusion, did not know anybody could feel both things at the same time or even show it on their face. She turns her head towards me a bit more and says “what the fuck do you think you’re doing with that?”. I try to explain to her that this will help us to see the oxygen in her blood, to make sure she’s getting enough air. I then tell her it will help us to know if she needs oxygen during this breathing trouble and coughing issue. Before I can even bring my hand closer to her finger she yells at me “This hospital doesn’t know what they are doing. I tell you I’m having trouble breathing and you don’t know what to do. I’m in pain and you do nothing!”. It doesn’t matter what I say or do, but her mind is made up. She will no longer listen to my advice or explanations. As a nurse I can tell when my words will reach a patient or not.
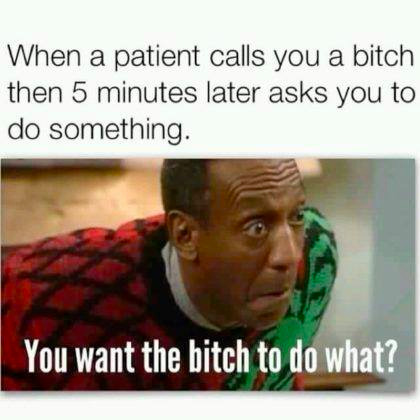
She then continued on swearing, shouting and insulting me, the hospital, doctors etc. Within minutes she called again with her call bell and started asking for pain medications.
#neuronursing#neurologynurse#strokenursing#strokenurse#meanpatients#patientstories#medicalstorytime#medicalstories#patientstorytime#whyme
1 note
·
View note
Text
Doubting yourself as a nurse
When taking care of a patient recently, I was precepting some students. This student had gone over medications before walking into the room, checked all information and confirmed her knowledge.
She walked into the room, a patient and their spouse were in there. The pt asked what meds were to be given at this time. The student responded with the correct medications and what she had looked up before walking into the room. That’s when the spouse starting shouting at the student. The spouse had told this student that they were wrong, didn’t know what they were talking about or doing. Then this person said that next time the student should know what they are doing before they walk into the room and shouldn’t be doing such things if they don’t know.
The student left the room a bit dazed and confused at what had just happened. After all, she had looked up the information from a reliable source, confirmed it with a practicing RN and learned about it in her pharmacology course in school. She didn’t understand how she could be wrong with such basic pharmacological information.
I then told this student, “DONT EVER LET A PT OR THEIR FAMILY MAKE YOU DOUBT YOURSELF”. As nurses we tend to question what we know since our brains have had to absorb quite a lot in a short period of time and absorb even more in our workplace even quicker than we did in school. This was a great lesson for the student and experienced RN. We tend to question ourselves, whether or not someone else does it for us. But the lesson the students took from this was that, when in doubt, look it up, ask another RN and remind yourself you know more than you think.
#neuronursing#neurologynurse#jewishnurse#preceptingfuturerns#strokenursing#confidentnurse#newnurse#lessonsinnursing
0 notes