#nurseantics
Text
Work has just been a lot to handle lately. I admit I have a very fragile resolve. Blow after blow of near misses, miscommunication, and disappointments are giving me feelings of incompetence and not feeling good enough for my job. My morale is low, my energy to keep going is utterly drained, and my anxiety an all time high. I need a pause. I need a recharge. I need a great cup of coffee.
#nurse#nursing#nurseantics#nurselife#rn#nurse antics#nurse life#healthcare#white cap#nurblr#nurse story#whitecap#nursing problems#nurse stories#nurse problems
10 notes
·
View notes
Text
Today was just a shitty day that started horrid and never let up. Coming back to my unit after transferring a patient to another ward, I was just plain exhausted. My shoulders drooping and my face defeated, I saw my patient’s relative walk towards me with a smile. She said, “let me give you a hug”, and I just let her and hugged her back. I needed it today.
#nurse#nursing#nurseantics#nurselife#rn#nurse antics#nurse life#healthcare#white cap#nurblr#nurse story#nurse humor#whitecap#nursing problems#nurse stories#nurse problems
5 notes
·
View notes
Text
When you work in a clinic and you can’t go home on time because your diabetic patient thought he’d skip his 34units of humulin M3 in the morning because “we’re gonna give it to him in the clinic anyway” and now his blood sugar is unreadable!
#nursing#nurse#nurseantics#nurse antics#nurselife#nurse life#white cap#rn#nurblr#healthcare#nurse humor#nurse story#nursing problems#whitecap#nurse stories#nurse problems
5 notes
·
View notes
Text
Context: I work in an elderly assessment unit where most of my patients are above 65 years old and have dementia. I needed to transfer my patient to another bed-space and to be more efficient, I transfer them with their beds.
Me: Hi patient, the other room is ready for you now. Would you like to lie down and I’ll give you a ride?
Patient: gasps*. At my age!?
11 notes
·
View notes
Text

Can you guess who’s NOT the nurse in this flat? 🤣
#nurse#nursing#nurseantics#nurselife#rn#nursestory#songs#whitecap#white cap#nursing problems#nurse humor#nurse antics#work from home
6 notes
·
View notes
Text
Patient: It was nice meeting you. You are always smiling and laughing.
Me: Thank you. That was my coping mechanism. 😂
16 notes
·
View notes
Text

You know you had a busy day when you come home with faded tattoos on your arms. 🤣
3 notes
·
View notes
Text
Employers nowadays are more concerned of diversity over competency. Don’t get me wrong. Diversity provides equal opportunities to minority groups (BAME which I am part of). But if competency no longer holds value because diversity takes precedence, institutions start to fail.
1 note
·
View note
Text
Asking a student nurse how she is doing on a busy day when really, I am asking myself how I am doing coz it’s f***ing chaos out there.
10 notes
·
View notes
Text
Converations with family be like...
Mom: Can you check on your grandma? She said she’s not feeling too good.
Me: (After checking on her) Let’s bring her for a check up. She might need some medications.
Mom: I have some herbal medication that a friend gave me. I think that will help.
6 notes
·
View notes
Text
To The Nurses Who Forgot:
We are a noble profession.
We take pride in our degree, because it represents the hardships we surpassed to attain the title we have now. We wear our uniforms with confidence, parading down the corridors, knowing that every exhausting shift is a reflection of our calling.
We have the ability to act independently. We were taught to assess thoroughly, think in anticipation, and to respond accordingly.
We are to be part of a team. We have sworn servitude to the people in need, not to other professionals we work with.
Most importantly, we have the capacity to do good; to bring comfort not only to those afflicted, but also to those affected. Kind words and genuine concern, subtle they may seem, aids healing.
We are not without mistake. No one is. But we continue to strive for excellence in our field, to consistently achieve quality of care. We uphold a standard of professionalism, and still maintain our sense of humanity. That is what keeps us true. That is what keeps us noble.
With nothing but love and respect for our humble profession; sincerely,
My father’s daughter.

#nurse#nursing#nurseantics#nurselife#rn#nurse antics#nurse life#healthcare#nurblr#white cap#nurse story
70 notes
·
View notes
Text
Worst Fears
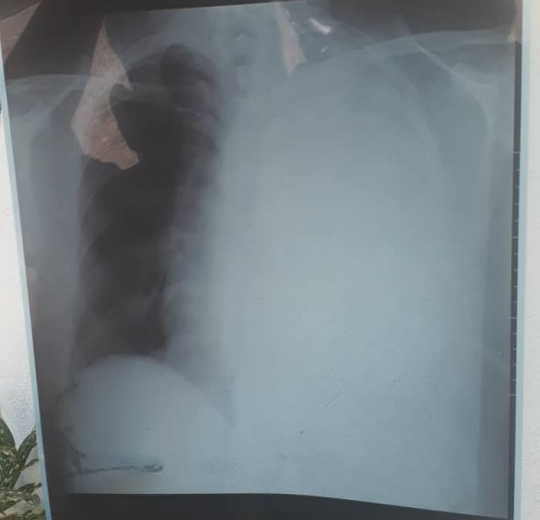
This is my dad’s chest x-ray. My heart sank when I saw it. It’s been sinking every day since then.
I have never seen my father in a position of vulnerability. He is always that figure of intellect and stubbornness, unwilling to be defeated. But hearing him ask the doctor how much time he has left to live, with his voice cracking and his eyes close to tears, it broke me completely. I struggle to keep my eyes dry writing this.
PLEOMORPHIC SARCOMA. Whatever the fuck that is. Apparently it is an aggressive type of cancer and my dad only has 18 months to 3 years to live. 18 months to 3 fucking years. And the clock ticks everyday.
I became a nurse with the vision of serving my family when they need me. Now I am living my worst fear - unable to take care of my own family, my dad who needs me, because I work so far away from home. I could have organized his appointments and his medications. I could have flushed his chest tube to make sure it doesn’t get blocked. I could have changed his chest tube dressings properly. I could have made sure he eats well and takes his supplements so he doesn’t lose any more weight. I could have checked on his vitals regularly. I could have done measures to help him breathe better. I could have given his wife, my mother, the emotional support she needs. I could have been with his children, my siblings, through what is going on and help them understand the situation. But I’m not home, and all these things I am doing for strangers.
It angers me knowing that there are people out there who do not appreciate how lucky they are to have free healthcare. Coming from a third world country where, a lot of times, life and death is determined by how much you can pay, I feel stuck not knowing what to do. I want to go home to take care of my father, but that would mean spending money that I could otherwise send home to help with medical bills. Coz maybe, that money can pay the chemo that buys him more time to live. Maybe, it would save his life. I am terrified of the thought that I will not be able to afford to keep my father alive. And nothing breaks me more than that.
Maybe I don’t want to go home because I am afraid. Work keeps me busy. Being far away is my escape. Going home means seeing my father in his current state, and facing the reality of our lives everyday. Because maybe I am still in denial, hoping that tomorrow I will wake up realizing that all of this is a dream.
11 notes
·
View notes
Quote
Sometimes I wonder whether my confused patient is having hallucinations or paranormal activities in the middle of the night
Post Nightshift Delirium
35 notes
·
View notes
Text
Nurse-Patient Interaction #2, Stand Your Ground
Haven’t been posting in a while. So here’s a conversation with my confused, falls-risk patient who keeps getting out of bed in the wee hours of the morning.
Patient: *Gets out of bed, dazed and irritable.
Me: Patient, get back to bed!
P: Shut up!
M: Get back to bed!
P: Oh, shut up!
M: Go to sleep!
P: Shut up!
M: Get back to bed!
P: *curses*. Shut up!
M: Go to sleep!
P: *Climbs back to bed and goes to sleep.
😂 oh the Joys of Nursing!
Happy holidays everyone!
7 notes
·
View notes
Text
Accidentally telling the Doctor to “Get Out” instead of “Go ahead” while I was holding the door for him.
Post nightshift delirium
23 notes
·
View notes
Text
Hear ye, Hear ye, Medics!
On a day shift, a patient came in for debridement of an injured left toe. She also had been having nausea and vomiting, which is being managed with PRN antisickness. The day went by, I left at the end of my day shift, had a day off, and came back the next day shift. This is the patient’s 3rd day in the hospital. She was still feeling nauseated, and barely keeps in anything she eats despite trying. I talked to her about how she was feeling. I found out that through the whole 3 days, her food intake was equivalent to just one sandwich. She has a stomachache and has been burping a lot. I went through her medications and noticed she hasn’t had anything for stomach acid control. So I went to the doctor and discussed the patient’s situation. I suggested that the patient might benefit from having omeprazole and similar medications prescribed for the above reasons. The doctor told me she will add more antisickness meds but she will read through the notes and see if she will prescribe omeprazole. She never did. The next day, the consultant came to review the patient. After having seen the patient, he ordered for PPI’s to be given IV.
On a night shift, I called the night doctor for my 82y.o. Female, who came in with an unwitnessed fall, cause unknown. I told the doctor I was concerned that I had not seen my patient eat/drink anything, and that I am not sure if she had anything in the day as she came to the ward at 7pm. She only takes in sips of the water we offer her. BP is 99/45, peeing good amounts, but even so, I felt she would benefit from having fluids overnight. The doctor’s response? “Patients sleep at night. They don’t drink”. She will not prescribe fluids because the patient doesn’t need it as she is not hypotensive. I called the doctor again 2 hours after. Same patient, different concern. However, I reminded her of the fluids. Clearly sounding pissed, doctor insisted that the patient doesn’t need it, the blood pressure is fine. Doctor came at 7am in the morning to review the patient for a different concern. She prescribed fluids coz the patient’s tongue and body seemed dry.
Called the same doctor on a night shift for a patient who is non diabetic, but has had episodes of her blood sugar dropping the previous day, cause unknown. Patient came in with nausea and vomiting, hasn’t had much to eat/drink coz she couldn’t keep it down. The long day doctor had seen the patient before his shift finished and had intended to prescribe a bag of glucose for her to run overnight, however, may have forgotten to do so before he left. Since the blood sugar was initially fine at 8pm. I opted to monitor it whilst I was made aware that the Night doctor was attending a cardiac arrest. Blood sugar that night was 8.2mmols, 7.7mmols, and 5.2mmols at 8pm, 10pm, and 12mn respectively; clearly down-trending. So I decided to call the night doctor and told her all about it. Her response, “she doesn’t need it. She is not having hypoglycemia”. I told her that the patient had an episode of hypoglycemia with a sudden drop of BM 3.3 the night before. She still insisted that the patient didn’t need it. An hour later, she prescribed gucose. BM was 4.1.
Doctors, hear us out. Yes, you know more than we do. That is a given. It doesn’t mean we don’t know how to analyse a situation and anticipate outcomes. We are here not to bother you, rather, we are here to advocate for our patient’s well being. They are our priority, first and foremost. So please, listen up.
83 notes
·
View notes