Text
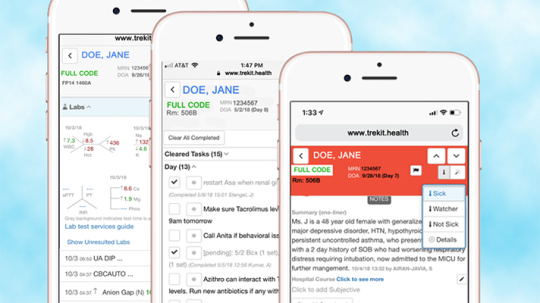
Care coordination tech reduces readmissions, length of stay at Penn Medicine
One of the main issues faced by Penn Medicine and the inpatient consult service at the Perelman School of Medicine at the University of Pennsylvania is accurate, rapid, reliable transfers of information between teams.
THE PROBLEM
Whether sharing information between a team of primary care doctors during the handoff process, communicating with consulting specialties or gathering information across multiple hospitalizations of the same patient, seamless and consistent data sharing is paramount for providing the highest level of care.
While electronic health records have their place in the IT ecosystem, they lack the usability necessary to meet clinicians' needs in these areas, said Dr. Misha Rosenbach, director of the inpatient consult service at the Perelman School of Medicine at the University of Pennsylvania and associate program director of the dermatology residency.
The interface requires multiple steps to understand a cohesive patient history with lengthy, often difficult-to-read progress notes that do not really fit into the clinical workflow, often adding to duplicative administrative work and taking clinicians away from patient care, he said.
PROPOSAL
Penn Medicine decided to partner with care coordination technology vendor TrekIT Health, which was initially developed in 2016 at Penn as a product called Carelign to reduce clinicians' reliance on paper in clinical workflows and communication.
It has been successfully adopted by almost all inpatient services at Penn Medicine's four urban hospitals. This year, the clinical lead for the project has since co-founded TrekIT Health to commercialize the product as TrekIT.
TrekIT helps in each of the aforementioned settings – knowing where patients are in the hospital, who is seeing them, what the clinicians are thinking, and then communicating all of that information safely, securely and simply among and between various healthcare teams, Rosenbach explained.
It does so in a way that's easy to read, review and visualize, even while walking around doing rounds in the hospital, or when called to see an acute patient, because you can readily see the important data you need, and read about the active issues on your phone while you are walking to the patient's room, he added.
TrekIT gives providers a collaborative space to put their thoughts together and intuitively pairs them with the chart so they can see the doctor's notes without a lot of fluff, use copy/paste, use repetitive text, and handle billing/medical-legal documentation, said Rosenbach.
You get the core information, paired with the most updated labs, paired with the patient location, and you get it in real time, in a way that you can easily digest it and find what you are looking for on a mobile device, he said.
MARKETPLACE
There are a variety of care coordination technologies on the health IT marketplace. Vendors include Cipherhealth, eQHealth, GSI Health, Imprivata, Microsoft, Optum and pMD.
MEETING THE CHALLENGE
TrekIT's platform is integrated into Penn Medicine's Epic system, but it is also available in a browser from any desktop or, more important, from any mobile device. The tool brings real-time vitals, labs and medications, critical elements clinicians need to see.
Because of the technology, physicians now are able to coordinate and collaborate between all members of the clinical team, from doctors to nurses, therapists and others.
Groups using the technology during clinical rounds access real-time data about their patients 50 percent more often than teams that don't, but spend 25 percent less time logging into their devices.
Dr. Misha Rosenbach, Perelman School of Medicine, University of Pennsylvania
Our group is a primary consulting service, so our role is to see hospitalized patients and add our thoughts on our organ-system and how it impacts their hospitalization, Rosenbach explained.
We are moving toward using TrekIT as our main handoff tool, for example, during service changes, to use this as a way to conveniently convey our team's thoughts and active treatment plan/issue management on our consult service from one team to another, he added.
Click on page 2 below to read how Penn Medicine reduced readmissions and risk-adjusted length of stay, and more.
0 notes
Text
Post-acute facility trims length of stay by 3-5 days with alerts tech

Cedar View Rehabilitation and Healthcare Center, a skilled nursing facility in Methuen, Massachusetts, operated by Marquis Health Services, was reviewing hospital discharge summaries and relied on a patient’s or family’s memories to piece together a patient’s encounter history.
THE PROBLEM
Sometimes the provider organization also received input from a hospital’s external case manager, but consistently obtaining accurate information proved challenging. After it discharged a patient, it had no way to track their subsequent encounters with the health system.
PROPOSAL
Cedar View turned to vendor PatientPing, which provides real-time alerts from hospitals, emergency departments and post-acute care providers every time a patient goes through a transition of care. The vendor also supplies key clinical data that is valuable for placing a patient’s situation in context, as well as contact information for their healthcare providers.
MARKETPLACE
Vendors of healthcare alerts technology include ECRI Institute, Healthix and Spok. Some health information exchanges also offer forms of clinical event notifications.
MEETING THE CHALLENGE
The members of the Cedar View care team who have PatientPing alerts sent to their desktops or texted to their phones include the admissions coordinator, the external clinical screener, the facility care manager, the social worker, the administrator and the director of nursing.
The care team monitors the alerts all day and has found them very useful for tracking patients, making bed offers and collaborating with other providers, said Andrea Gele, vice president of case management and reimbursement at Cedar View Rehabilitation and Healthcare Center.
“When Cedar View admits a patient, the staff uses PatientPing to validate the number of the patient’s remaining Medicare-covered days by looking at how long they were in the hospital,” she explained. “Information from PatientPing also allows team members to reach out to facilities or home care agencies from which the patient previously received care.”
In one example, an elderly, at-risk patient had a history of frequent hospitalizations and had recently been discharged from Cedar View. Following another hospitalization, the patient refused to let a home care nurse enter her home, and the home health agency reported this to Cedar View.
PatientPing notifications enabled the Cedar View care team to see that the patient presented to the emergency department following a fall that left her with multiple fractures. Cedar View then intervened and the patient returned to the Cedar View facility with a strong discharge plan. This direct transfer from the emergency department averted an unnecessary readmission to the hospital.
Click on page 2 below to learn how Cedar View reduced length of stay and readmissions.
0 notes
Text
Amazons new machine learning offerings promise wide range of healthcare applications

Amazon has released new machine learning tools with a wide range of applications for the healthcare space.
The new Amazon Elastic Inference service harnesses a scalable GPU model, enabling customers to choose the amount of computing power they need with the option to scale up or down as demands dictate.
GPUs provide a tremendous surge in machine learning power for massive datasets such medical imaging. This system provides cost-effective computing power to serve predictions to medical researchers at a scalable level.
Meanwhile, new additions to Amazon Sagemaker, a machine learning framework hosted on AWS, have healthcare applications as well.
SageMaker Ground Truth uses active learning and can be trained in real time to perform data labelling and processing, such image and text classification, or object detection. Labelling a dataset of millions of documents is a resource intensive task that often stands in the way of allowing machine learning to serve predictions.
SageMaker Neo optimizes machine learning instances during the training phase, allowing health organizations to wring maximum efficiency out of whatever hardware architecture they might be using for their prediction environment.
And SageMaker RL is a reinforced learning program which can be used where building a prior dataset would either be infeasible or prohibitively expensive, according to Amazon’s blog post. Reinforced Learning uses continuous feedback to constantly improve problem solving and make increasingly relevant actions, officials said.
WHY IT MATTERS
As data proliferates in healthcare organizations, the need to quickly and efficiently process it is vital both to improving patient outcomes as well as developing revenue streams from the information captured. Advances in computing technology, especially GPUs, have allowed machine learning to grow by leaps and bounds.
However, the physical architecture that enables these services can be prohibitively expensive for a healthcare system. Amazon’s cloud-based offerings enable data workers to harness the power of the advanced AI in a scalable and cost-effective environment.
With petabytes of unstructured data being generated in hospital systems every day, our goal is to take this information and convert it into useful insights that can be efficiently accessed and understood, Anish Kejariwal, director of software engineering for Roche Diagnostics Information Solutions, said in an Amazon blog post.
THE LARGER TREND
Amazon’s cloud computing and machine learning offerings have been making increased inroads into the healthcare space. It has developed healthcare-specific tools to analyze patient records and a more and more of its portfolio is HIPAA-eligible as it continues to home in on healthcare. Machine learning is being deployed throughout the industry and in some cases is dramatically reducing the amount of time spent by clinicians.
Earlier this week, AWS also unveiled Amazon Comprehend Medical, new HIPAA-eligible machine learning tool, enabling developers to process unstructured medical text and spot specific data such as diagnosis, treatments, dosages, symptoms and more.
So much of today's healthcare data is unstructured medical text – written notes and audio transcripts, prescriptions, pathology and radiology reports – exists as hard-to-mine unstructured data. With the new Comprehend Medical tool, developers only need to provide unstructured medical text, said Amazon in a blog post. The service will 'read' the text and then identify and return the medical information contained within it.
Moreover, the technology will also highlight protected health information, officials said, and no data processed by the service is stored. (Comprehend Medical is covered under AWS' business associate agreement.)
With no machine learning experience required – there are no models to train – and the ability to be integrated with existing services via API, the tool could be a valuable resource for clinical decision support, revenue cycle management, pop health, clinical trials and more, Amazon said.
ON THE RECORD
The process of developing clinical trials and connecting them with the right patients requires research teams to sift through and label mountains of unstructured medical record data, Matthew Trunnell, CIO at Fred Hutchinson Cancer Research Center, said in the blog post.
Amazon Comprehend Medical will reduce this time burden from hours per record to seconds, he said. This is a vital step toward getting researchers rapid access to the information they need when they need it so they can find actionable insights to advance lifesaving therapies for patients.
Benjamin Harris is a Maine-based freelance writer and and former new media producer for HIMSS Media.
Twitter: @BenzoHarris.
<![CDATA[/* ><!]]>*/
0 notes
Text
AI, working with standard CT scans, could help predict under-diagnosed conditions
Israeli healthcare system Calit Health System teamed with analytics company Zebra Medical Vision to develop ways artificial intelligence could be leveraged to help predict two major under-diagnosed medical conditions: osteoporotic fractures and coronary vascular events. Using CT scan data, the AI tools showed improvements in predicting instances of both.
WHY IT MATTERS
In each case, when AI was paired with existing predictive and diagnostic measures it was able to improve both the "sensitivity and specificity" of the clinical predictions, leading to much better predictions of future health events, said Calit Health and Zebra Medical officials.
In the instance of cardiovascular CT scan data the companies reported a "net 4.5 percent categorical risk-reclassification improvement." With osteoporotic fractures, the use of an AI-derived risk score led to better results than those of existing predictive measures, they said.
CT scan data is already captured but has not always been put to use in predicting other medical events, researchers point out.
This study found that only 20 percent of those at risk for osteoporotic fractures undergo any screening, but that 66 percent undergo CT scans for other reasons. The cardiovascular AI "pertains to all studies which are performed on a routine basis involving the chest CT," the study notes, meaning that there is a wide range of data ripe for predictive analytics.
THE LARGER TREND
Osteoporotic fractures and cardiovascular health are some of the costliest areas of American healthcare. The price tag of fractures comes to $18 billion per year, and heart health costs the nation a half billion a year currently and is expected to double in the next 20 years.
More generally, AI technology is increasingly being developed as a "second set of eyes" in screening for and predicting ailments. The tools are also serving to augment non-specialist medical practitioners, who may be eventually able to administer some specialized tests in a primary care setting instead of a more invasive exam.
Overall, AI is helping researchers pinpoint and understand small changes that even a trained eye can occasionally miss. As a wide range of medical images are paired with predictive analytics, the hope is that more easily preventable medical conditions can be averted entirely, or at least before they become serious and costly.
ON THE RECORD
"We are pleased with the results of these two groundbreaking research projects and are looking forward to getting them into practice," said Ran Balicer, head of Clalit's Research Institute. "While there is an increasing number of AI applications in imaging, aiming to mimic and automate human radiologist' reading, there is larger untapped potential in these imaging studies – one can use AI to extract predictive insights unavailable to date, that support high-impact population health interventions to tackle chronic diseases."
0 notes
Text
What This Mom Learned About Food Culture in America After Her Baby Stopped Eating

You’ll want to have tissues handy when you dive into The Eating Instinct: Food Culture, Body Image, and Guilt in America. Though the new book from Virginia Sole-Smith might sound at first blush like a feminist or body-positivity book—both of which it is—it’s also a deeply personal, heart-wrenching story.
Sole-Smith’s elder daughter, Violet, stopped eating by mouth at nine weeks old, and didn’t start again until she was about 16 months old. Rare congenital heart defects landed Violet in the hospital four weeks into her tiny life, and she emerged with what’s known medically as an oral aversion or infantile anorexia. It’s “when a child refuses to eat as a way of protecting herself from perceived trauma,” writes Sole-Smith. Violet was restricted to feeding tubes for much of her infancy, leaving her mother stricken, frightened, and wondering, “What does it mean to learn to eat, in a world that’s telling us not to eat?”
A journalist who covers health, parenting, lifestyle, and culture, Sole-Smith dove into the topic with a reporter’s zeal for talking to experts. She interviewed dieticians (including some with their own eating disorders), poverty-stricken moms recovering from cocaine addictions, “health at every size” activists, anti-fat doctors, and plenty of researchers. The result is a data-packed book with the epic tale of little Violet re-learning to eat threaded throughout.
Here, Sole-Smith delves deeper into a few of the topics she covered in her book.
Your book ends with your desire to feed your younger daughter by mouth. Did that work?
Beatrix is 10 months old and a very typical eater; she took swimmingly to breastfeeding and bottle-feeding. I really went into baby number two thinking my number one goal is a baby who eats by mouth. I am not picky. I also knew after the devastating experience with Violet and breastfeeding [that] I didn’t want all that pressure on my shoulders.
We did combination feeding [a mix of breast milk and formula] from the beginning. She had a little formula her first night [to] help take the pressure off. My milk took a couple days to come in. … Then we did what worked. I was like, “I’m not listening to anyone this time. Tell everyone to shut up. I’m going to feed the baby the way that makes sense.”
The “breast is best” breast-feeding pressure thing that moms hear; is it hammered a lot?
A few years ago when I had Violet it really felt like I had to breast-feed this baby or I had failed as a mother. I don’t think that’s quite there anymore. What I’m still seeing is now a set of “allowed” circumstances in which you can [choose not to] breast-feed but you have to have failed at it. … “It’s OK to be using formula if you had a traumatic birth. If there are reasons … because XYZ happened.”
We’re not yet to a place where people can generally do what I did [with Beatrix], which is, “I’m going to do what works and not feel bad about it. I’m gonna stop breast-feeding when it stops being fun.”
Isn’t breast-feeding also a big time commitment for women?
It’s a huge time commitment. Anyone who says, ‘Oh, breast-feeding is free,’ doesn’t think a woman’s time is worth anything. My billable hours are [worth] a lot more than a can of formula. It’s another way that our culture is saying, “We control women’s bodies; we control women and food.” That’s what I’m arguing against in the book. There’s a lot of overlap between diet culture messages and exclusive breastfeeding messages. I think the two have gotten pretty murky. The literature is not cut-and-dry on what the healthiest choice is. There are many circumstances where formula is the healthiest choice for the baby. We don’t celebrate that. We just say, “Women need to turn their bodies over to the babies,” just like we say the rest of the time, “Women have to be as thin as possible.” It’s all of a piece, in my mind.
Trying to get Violet to eat by mouth, you used the “division of responsibility” theory. Can you explain it?
It’s a theory developed by Ellyn Satter, a family therapist and nutritionist, back in the 80s. She’s written several books about it, but I’m seeing it more and more in the mainstream conversations around kids, which is really exciting. The premise of it is that children are autonomous beings who should have agency over their bodies and what goes into their bodies. Rather than parents being in charge of every bite of food and meticulously counting out portions and all that, it says, “Nope, parents and children are in a feeding relationship, and they each have certain roles.”
Parents are in charge of what food is offered, where it’s offered (preferably at a table, not in front of the TV or mindlessly grazing around the house), and when it’s offered. They try to keep kids on a schedule so that kids have time to get hungry and come to the table hungry. After that—after they’ve said, “OK, we’re eating dinner at this time, and this place, and here’s what your choices are,” the parents’ job is done.
Kids are in charge of how much they eat, which of the foods they eat of what you offer, and even whether they eat at that meal. They’re in charge of listening to their bodies, in terms of hunger and fullness, and in terms of, “Of the foods you’re offering me, what do I really need right now? Maybe I don’t really need a piece of chicken at this meal; maybe I’m really hungry just for the pasta.” That’s fine. We kind of trust kids to listen to their bodies and know what they’re really hungry for.
Having seen parent friends negotiate “one more piece of chicken before you’re done,” I feel like this must be controversial. Is it?
We had to do division of responsibility; we were in an extreme situation. What I see with parents who are feeding kids in more typical situations, is when they’re not practicing division of responsibility, it’s probably fine for a while, depending on the temperament of your kid. A lot of kids are like, “Yeah, I’ll have another bite of broccoli, whatever. My mom really cares that I finish all these blueberries, so I’ll just do it.” … That’s fine. Not every family will find that strategy problematic, at least in the short term.
But what will happen over time is that child is being given the message that many of us received as kids of, “I don’t know what’s best for my body. I don’t know what I’m hungry and full for. When I do feel full, maybe I can’t trust that, because somebody else—this adult that I love and I trust—is saying, ‘No, no, no. I know what your body needs. It doesn’t need a cookie. You shouldn’t want a cookie. You should want broccoli.’” That doesn’t line up with the kid’s [experience]. It’s a really confusing message to send to kids.
My concern is that over time, with typical eaters, that leads to undercutting their sense of trust in their own bodies, and that makes them much more vulnerable to the messages of diet culture. Because now they’ve sort of grown up thinking, “I don’t know what’s best for me with food.” So of course when they’re struggling with weight, or feeling unhappy with their body for whatever reason, they think, “I must need a diet or this external rules to tell me what to do because I’ve never known. No one’s ever said, ‘[You] know what’s best for your body.’”
I want to be clear: It’s not about shaming parents who do that. It’s just about thinking long-term. We’re thinking short term, “I gotta get this kid through eating without a meltdown.” I have all the empathy in the world for that. Those short-term decisions are hard to pull off. … What you want long-term isn’t always what you want short-term.
Some would say, “Kids are wrong that they need cookies. I know more than they do.”
What I would say is, I don’t think any of us know as much as we think we know about nutrition. The nutrition advice is always changing. When I was a kid in the ‘80s, it was all about fat, and low-fat and fat free, and now we’re all, “More with the avocados and coconut oil!” The science on this is not settled in any way.
To say I’m gonna follow nutrition instead of letting my kids listen to their own bodies, you’re not taking the more cut-and-dry fact-based approach by any means. There is good data supporting division of responsibility. It’s not as robust as I’d like, but we are starting to see more data supporting that teaching kids to honor hunger and fullness is a way to put them towards a healthier relationship with food. The parent is still in charge of choosing the what. You are still choosing the nutrition. But we’re not dictators. We’re more benign leaders.
We always have a banana on the dinner table; it’s one of my daughter’s safe foods. If she’s not going to eat the rest of the meal, I know she’ll eat the banana, and I’ve accommodated her that way.
In your book’s conclusion, you dream of a world of judgment-free, guilt-free eating. Are you an intuitive eating proponent?
Yeah. I’m in no way an expert on it. I’m not a dietician or someone who can offer the specifics of how you learn that. It’s something that I aspire to and practice myself, I try to encourage it with my kids, and as with all things, I’m always overly hesitant to use the label, because there are lots of diet plans marketed around intuitive eating that are really not. Caveat that I’m for trueintuitive eating, not intuitive eating with a goal of weight loss. It’s the only way I’ve found that makes sense.
1 note
·
View note