Text
Private Health Insurance Market Fluctuations
Health Insurance is one of the most accessible types of insurance. Employees have the advantage of being provided for by their employees with the choice of taking dependents under them. Although there is a provision of health care insurance for most middle class workers and individuals and their families, the rate of insured in health plans are at an uncertain level.
For private and personal insurance providers around the globe, it is not a normal market share. Westhill Insurance Consulting, one of the internet’s oldest insurance information sites, compared health care insurance ratio in certain companies in different parts of the globe. Bermuda, one of the world’s top ranking countries to provide quality insurance faired better than the status of insured in Westhill’s main branch in Massachusetts. In Asia, Singapore is at its highest peak compared to insurance of other providers in developing cities like Hong Kong, Kuala Lumpur, Malaysia and Jakarta, Indonesia.
According to reviews, the United States is lagging behind. If this continues, developing countries depending on the innovations and adaptation from the West can be put into jeopardy. The worldwide issue which causes market fluctuations among private health insurance providers is the rate of medical errors. These errors may have been prevented if legitimate and specialized physicians are being provided for. Instead, most doctors listed under insurance are those consisting general medical practice. For better quality physician and equipment used, an individual has to avail a more expensive premium.
The rising cost of insurance is putting trauma to clients. In response, they take services from fraudulent insurance providers who offers cheaper premium only to discover later that they get scammed.
Such problems require better innovations and technological advancement, a reform on the system or at least, a consideration for the choice of specialist. Innovative solutions involves every aspect of health care—its delivery to consumers, its technology, and its business models. Indeed, a great deal of money has been spent on the search for solutions, a few has been addressed.
The fluctuation in the market poses superior threat to many insurance companies. Many analysts are convinced that the change in the process and the overall method is the solution for the fluctuation. A revamp of the system to integrate technology, new equipment and more qualified physicians can help stabilize the increase of insured clients in private health providers. Unless this problem be controlled and put attention to, fluctuation will continue to dominate the market.
#Private Health Insurance Market Fluctuations#westhill healthcare consulting jakarta usa united kingdom
0 notes
Text
Health Insurance for Young Adults
As we grow older, our responsibilities add up. Having a health insurance should be one of the priorities that we should think of. By the time you are old enough to fend for yourself, you are then required to get an insurance. However, many young adults are still confused on its importance.
1. It may be Illegal
When you are living in the United States, Affordable Care Act (ACA) compels you to purchase insurance. Going without insurance for three months would force you to pay a penalty of $325 or 2% of your monthly income, whichever is higher. In developing countries, uninsured individuals have the option to purchase from private companies but laws are already drafted for completion. In cities like Jakarta, Indonesia and Bangkok, Thailand, more than half of their unemployed population goes uninsured.
2. If you are a full-time employee, your employer should provide you with insurance
Most companies require employees work for set period before benefits can be provided. It usually takes 3-6 months in a probationary period before regularization, by which insurance is given. It is in any law in any states and government to mandate to every employer to provide employee benefits.
3. Your parents may still be able to cover you
Individuals under the age of 26 can still be listed under their parents’ coverage. They can still cover even a modest premium cost.
4. You can do it alone
If you are not insured under your parents’ plan or purchasing insurance under your employer is not an option, you have the choice to purchase your own insurance from trusted private companies. If you are buying online, just make sure you are dealing with a legitimate company as there are a lot of scammers operating in the net. If you are looking for a sound advice, you can ask from consulting companies. Westhill Insurance Consulting is one of the longest running catalysts in insurance consulting and the staff can definitely guide you in buying from the best.
5. Know the Difference between HMO and PPO
Health Maintenance Organizations (HMO) and Preferred Provider Organization (PPO) are two different typed of health insurance. HMOs have lower premiums than PPO as its coverage is more limited. Doctors in HMO have to be in-network while in PPO, in-networks are more flexible and you have the option to see doctors outside of your coverage with extra coverage. Review the type you are insured into and make sure you know your coverage.
0 notes
Text
Medical Insurance for Expatriates
Expatriates may find it hard to avail of health insurance when they are in a foreign place. The system varies from that of your own nation and customs of availing is a far cry especially in developing nations.
Luckily, developing countries like Indonesia and Thailand are starting to expand its insurance’s scope to a more international level, catering to both local and foreign individuals.
Companies operating in Jakarta, Indonesia, for instance, realize the importance of a comprehensive medical plan to cover sickness and accidents that happen to the staff that they hire.
Westhill Insurance Consulting is also aware of the struggles faced by expatriates when it comes to getting insurance. What preparations do you do then?
1. Find out before you come
The company who hired you and the person you are working for should provide medical insurance for you and your family members just as they do with local folks. Ask for details from your employer to ensure that your policy will adequate cover your family members for sickness, accidents or emergencies, on home leave and when you are visiting other countries for work-related purposes.
If you are joining a new company, remember that they may never love you more than when you first join. Do not rely on promises that medical insurance coverage will be sorted out when you arrive. It could be the case that what the company considers ideal coverage may not meet your expectations. Be sure before you arrive that you understand what medical coverage your company provides for regular medical concerns, major medical situations such as surgery or deliveries, and medical evacuation both inter- and internationally.
A little warning, if you are in a country like Indonesia, for instance, being a foreigner is more likely to be scammed than locals since your lack of knowledge of the customs would be obvious. Make sure you don’t fall into fraudulent acts.
2. Know if there are Medical Evacuations
Medical evacuations are a big factor in medical coverage, as the quality of medical service available in outlying areas in Indonesia will be quite poor. In such areas, emergency medical evacuation (medevac) to a large city or a neighboring country is considered essential.
3. Options in medical insurance coverage
As an example, international medical insurance plans from the U.K. include emergency medical evacuation with the possible addition of major outpatient services to cover everything but minor outpatient claims, which are often excluded to keep costs down. Therefore, outpatient claims are typically subject to a deductible related to the illness.
A patient may have several doctor and specialist visits plus prescribed medicine for one particular bout of sickness and still be subject to only one deductible amount. A point worth noting is that a person could be undergoing outpatient treatment related to a very serious illness, which would not be covered under a local clinic scheme.
0 notes
Text
Expansion of Health Insurance to Developing Nations
With the challenge of today’s generation, health risk is greatly increasing. Today’s citizens have greatly recognized the danger of going out every day. Health insurance is also in demand in the market and is considered as one of the most necessary insurance to have.
Developing nations are already increasing its insurance economy and even building its own campaign towards the totality of health insurance patrons.
According to a report released by Westhill Insurance Consulting, health insurance has already been accepted as a necessary part of each household.
Indonesia is one of developing nations who has proven too slowly adapt health insurance in its system. With over 200 million citizens flocking on the national health insurance registration in Jakarta, Bali, Sumatra and major places in the country, the government has been proud to predict that it may be possible to see all of the archipelago’s population already avail of health insurance.
To cater to rural areas of developing nations on the other hand, reliable, always‐on broadband wireless connectivity makes a new health care model possible: instead of asking the patient to go to the nearest clinic or hospital, the mobile health care worker reaches out to the patients where they live and when they need care, bringing access to a broad set of medical resources through voice, data, and video applications.
The only challenge in pursuing health care insurance in developing nations is the fraudulent deeds happening among their people because of the lack of security and loose protection from the authorities.
To prevent these scams from happening and keeping more victims from losing their hard-earned money for a non-existent medical assistance, many companies and non-profit organizations are continuously seeking reforms. Universal Health Coverage (UHC) initiatives have sought to create awareness in and provide guidance to countries on how to improve the design and functioning of their health systems based on evidence of what works for achieving the goal of universal coverage. Meeting this goal is, however, challenging, because the available evidence rarely explores the causal link between the design features of these UHC schemes and the outcomes observed, and substantial heterogeneity exists regarding the robustness of the available evidence.
UHC reviews and indicates possible intervention to both low and middle-income countries for improvement. Affordability is currently the main concern for the organization to both solve the problem of the small number of health care insurance holders and keep scams from happening.
Hopefully, more solution can be presented as we look forward for a healthier life in the near future.
0 notes
Video
youtube
Clinical Trials Supported by Insurance
Trials involving human patients are crucial to the advancement of clinical science. But they’re not without risk. Fortunately, insurers are willing to cover them.
Westhill Insurance Consulting, one of the most trusted on-line insurance consultant that offer consumer information on reasonably priced health and medical coverage has these following things to review if you are planning to take part in a clinical test.
Here are the conditions the federal law requires for a health insurance to cover:
You must be eligible for the trial
The trial must be an approved clinical trial
The trial does not involve out-of-network doctors or hospitals, if out-of-network care is not part of your plan
Also, if you do join an approved clinical trial, most health plans cannot refuse to let you take part or limit your benefits.
Approved clinical trials are research studies that:
Test ways to prevent, detect, or treat cancer or other life-threatening diseases.
Are funded or approved by the federal government, have submitted an IND application to the FDA , or are exempt from the IND requirements. IND stands for Investigational New Drug. In most cases, a new drug must have an IND application submitted to the FDA in order to be given to people in a clinical trial.
Health plans are not required to cover the research costs of a clinical trial. Examples of these costs include extra blood tests or scans that are done purely for the sake of the clinical trial. Often, the research sponsor will cover such costs. Warnings must be posted days before the outcome to prevent further complaints from both the sponsor and the insurance company.
Plans are also not required to cover the costs of out-of-network doctors or hospitals, if the plan does not usually do so. But if your plan does cover out-of-network doctors or hospitals, they are required to cover these costs if you take part in a clinical trial.
Clinical tests which are made in a different city such as those in Tokyo, Japan, Jakarta, Indonesia and Kuala Lumpur, Malaysia may not be included in the coverage as well.
Challenging trials
One challenge for underwriters is the relatively small premium base measured against a trend for higher [insured] limits to be requested.
Clinical trials policies normally have “claims made” wordings which means that insurance coverage does not automatically extend beyond the trial dates. The potential gap is where you arrange insurance, let the policy end and have no insurance for an event which may occur sometime in the future that can be attached to the clinical trial.
Serious problems in clinical trials are rare, as Rossano points out. “But what I would say is that clinical trials are not without risk. The risk of a clinical trial is that the human body is very complex and in rare cases there can be unforeseen outcomes, as happened in cases like TeGenaro.”
0 notes
Text
The Role of Health Insurance to Family Planning
World Health Organization (WHO) has stated that universal health coverage – ensuring that all people obtain health services they need without suffering financial hardships when paying for them – is a global priority for this year. They also declared that universal health coverage as “the single most powerful concept that public health has to offer”.
Several developing countries such as Indonesia, the Philippines, Rwanda, Vietnam, Kenya and Nigeria among others have demonstrated a strong commitment to universal health coverage, with many others slated to follow suit. Jakarta, the capital of Indonesia is already paving its way to offering a more extensive health insurance coverage that can cater different places in the inter-island archipelago.
Westhill Insurance Consulting Company, your guide to health insurance concerns located in Australia has been in partnership with varied insurance companies which has the goal of expanding the reach of health insurance.
Given this momentum, it is time to think critically about how the goals of universal health coverage can be advanced through health insurance to ensure that women worldwide are empowered to choose the size, timing, and spacing of their families.
Health insurance pays for all or part of medical or surgical expenses for the insured, mitigating out- of-pocket payments as a barrier to health care and providing financial risk protection against catastrophic health expenditures. Different types of insurance models have varying funding sources and provider payment. Many countries have some form of insurance program in place and coverage has increased considerably.
Many reviews say that it would be better for insurance companies to include family planning in their policies and terms especially in over-populated countries like Indonesia which remains the 4th most populous in the world and China which tops the chart. It is well established that family planning results in benefits beyond reducing unmet need and lowering fertility—benefits such as fewer maternal and child deaths and complications from abortions; and improved nutrition outcomes among women, infants, and children. Given the high cost of addressing maternal and child health, these benefits can lead to considerable savings for health systems and insurance providers. Critics have complaints though that if this be passed, couples can make this reason for pre-marital sex which continues to be a moral issue in countries centered by this insurance idea.
When developing insurance programs, governments and health insurance providers must carefully decide on a benefits package that clearly describes the types of services covered, along with levels of coverage and any applicable exclusions and/or limits on services. Since lack of access and inability to pay are important reasons women do not use family planning, inclusion of family planning services in health insurance programs could increase uptake. The Commission on Macroeconomics and Health has suggested criteria for choosing essential health interventions. Family planning is a strong match to the key criteria because it is a technically effective intervention, can be delivered successfully, addresses health issues that impose a heavy burden on society, and has benefits beyond the intervention itself.
#westhill consulting health Insurance USA#Jakarta#UK the role of health insurance to family planning
0 notes
Text
HMO vs PPO
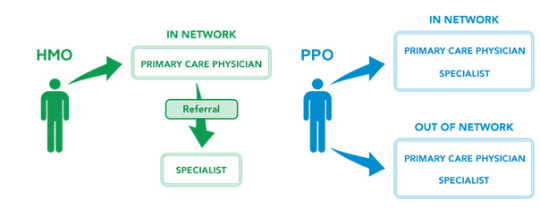
Most of us who are employed know that we have corresponding health insurance. For others who choose their own insurance, agents might have explained what should be provided and covered for our policies. One of the things that we should be aware of is the type of a managed care plan we need: either an HMO or PPO to avoid complaints, frustrations and disappointments added to our consultation to the doctor. If this is the first time you are hearing this, then, you are not alone. Some insurance are already fixed that agents do not care to mention it anymore.
Westhill Insurance Consulting took the liberty to differentiate each one from the other.
HMO actually stands for Health Maintenance Organization while PPO is an abbreviation of Preferred Provider Organization. Less common are point-of-service (POS) plans that combine the features of an HMO and a PPO. In developing cities like Singapore, Kuala Lumpur, Malaysia, Jakarta, Indonesia and Beijing China, HMO is mostly used by employers for their health care insurance.
To put into an outline, here are the facts that are needed to be reviewed and considered between the two:
Do I need to choose doctors, hospitals and other providers?
• HMO: you must choose doctors, hospitals and other providers
• PPO: you can choose doctors, hospitals and other providers.
Do I need to have a Primary Care Physician (PCP)?
• HMO: Yes, your HMO will not provide coverage if you do not have a PCP.
• PPO: No, you can receive care from any doctor you choose. But remember, you will pay more if the doctors you choose are not "preferred" providers.
How do I see a specialist?
• HMO: Referral is needed from your PCP to see a specialist or if you have to undergo other special test exams such as x-rays, except in emergency situations. Your PCP also must refer you to a specialist who is in the HMO network.
• PPO: You do not need a referral to see a specialist. However, some specialists will only see patients who are referred to them by a primary care doctor. And, some PPOs require that you get a prior approval for certain expensive services, such as MRIs.
Do I have to file any insurance claims?
• HMO: All of the providers in the HMO network are required to file a claim to get paid. You do not have to file a claim, and your provider may not charge you directly or send you a bill.
• PPO: If you get your healthcare from a network provider you usually do not need to file a claim. However, if you go out of network for services you may have to pay the provider in full and then file a claim with the PPO to get reimbursed. The money you receive from the PPO will most likely be only part of the bill. You are responsible for any part of the doctor's fee that the PPO does not pay.
0 notes
Text
Critical Health Insurance Plans for Critical Health Ailments
There are a lot of health care insurance nowadays with thousands of healthcare insurance companies scattered around the world. Individuals and organizations are slowly starting to appreciate their importance in today’s practical yet expensive lifestyle and health demands. If you are a person living with cancer or a survivor or with any other critical ailment, it is important to make sure that the health insurance plan you choose covers the prescription drugs you mostly need.
Westhill Insurance Consulting gives out warnings on the spread of fraudulent insurance that are emerging targeting the need of cancer patients for insurance. Reports have already been shown in the developing city of Jakarta, Indonesia and Mumbai, India. Here are the tips that we must remember when we avail of critical health insurance for critical health ailment:
All new health insurance plans must provide a benefit package that includes prescription drugs, but the actual drugs that are covered will vary by plan. As you think about the kind of health insurance coverage you or a family member needs, look carefully at the kind of prescription drug coverage the plan offers to make sure the drugs you take will be covered. Because many cancer drugs can be extremely expensive, so making sure that your plan covers the specific drugs you take may save money.
Things You Need to Consider
o Medications You Take: The first step is to make a list of all of the prescription medications you currently are taking, including pain medication and anti-nausea drugs. You will need this information to be able to compare the coverage offered by different insurance plans.
o Drug Formularies: Most insurance plans have a formulary – a list of the drugs the plan covers. Check the formulary of each insurance plan you are considering to make sure that it includes the medications you are taking. You can find out your plan’s formulary by checking their web site or calling the plan directly. Agents can also help you determine which health plan to choose.
o Cost Sharing: You will want to carefully compare the cost sharing different plans charge you when you fill a prescription drug. Some plans charge co-pay, which is a flat rate the patient pays per prescription. Other plans charge a coinsurance, a percent of the total cost of the drug owed by the patient. For cancer drugs, coinsurance will almost always be more expensive than co-pay.
0 notes
Text
Finding Private Health Insurance
Many of us have to rely on the company’s health care insurance provider. Lucky for those people who can stay in one job for years. How about those people who jumps from one venture to the other? Westhill Insurance Consulting has faced queries on the best alternative whenever unemployment comes near. Private health insurance is the main source of health coverage for the majority of people in the United States alone. For elderly citizens and eligible children and families from low-income households, public programs are the primary source of health cover.
If you are not covered by a publicly funded program, or if your coverage is only partial, you will need to have some kind of private health insurance. In developing cities like Tokyo, Japan, Seoul, South Korea, Jakarta, Indonesia and Singapore, millions of people have found themselves with no health cover at all. Reviews show that uninsured people reaches up to 46 million. Tens of millions more have inadequate insurance.
Best ways to find the best suitable private insurance for you are:
• One plan or separate plans - adding a spouse or offspring to a plan may be ideal, but not always so. In some cases, shoppers may find better deals by checking what is around first. It is important to balance to benefits offered against the amount that has to be paid out in premiums, in every case.
• Is your doctor included? - if you are considering an interesting plan, make sure your doctor or clinic is listed in their network of healthcare professionals. Otherwise, you may either have to change doctors, or pay out-of-pocket for the one you prefer.
• Only choose relevant options - do not choose a plan with options you do not need, in order to keep your premium costs to a minimum. If the purchaser or spouse is a female over 45, it is unlikely maternity coverage is a top priority. Even prescription plan coverage most likely will not cover all drugs, especially the newer, more expensive ones.
• Big premiums today, or in the future? - if you have little disposable income and enjoy good health, you might find it more convenient to opt for a high-deductible plan to start with, that has progressively lower monthly premiums with the passing of time. If your health care requirements are high now, a low-deductible plan to start with may be a better choice.
0 notes
Video
youtube
The Best Fit in Healthcare Insurance
With the widespread of insurance nowadays, people are confused which one is legit and which one is a fraud; which can offer better and which one cost less. Choosing the right health coverage has never been easy, and the health reform law has made things more complicated. Besides sorting through differences in premiums, deductibles, and copayments, you need to consider new provisions in the law that have recently kicked in and could impact your coverage for the coming year. Westhill Insurance Consulting can help you clear away any confusion, doubts and complaints.
Health insurance should cover any medical need you may have, now or in the future.
Buying insurance on your own used to be riskier because many plans didn’t cover important things such as prescription drugs or mental health care. Every kind of health insurance must now cover preventive care, with no deductibles, co-pays, or other types of out-of-pocket expenses. That includes Pap and cholesterol tests, mammograms, immunizations, and colonoscopies when age- and condition-appropriate.
But even though you no longer have to worry about your basic health care needs being covered, you’ll still have to navigate lots of other confusing choices. That’s true even if you get coverage through a job, because more than half of workers have a choice of two or more types of health plans.
1. Do you want to pay for care now or later?
All health plans have to come up with enough money to pay for the medical expenses of their members.
You can choose to collect most of the money up front in the form of premiums. If you have a high premium, you’ll pay a smaller share out of your own pocket, in the form of deductibles, co-insurance, and co-pays. Or plans can go the other way, charging smaller premiums but asking you to pay a bigger share on your own.
2. Are you OK with a small network of docs?
Doctors and hospitals accept lower fees from insurers if they know they’ll be part of a small, or “narrow,” network, because that guarantees them a bigger share of the plan’s business. There’s no evidence that you’ll get worse care in narrow networks. And they can save you about 20 percent over larger networks. But make sure that the plan has enough choice of doctors and hospitals in your area—a particular consideration if you live in a rural area. In Singapore and Jakarta, Indonesia and other developing nation, seldom can you choose this kind of benefit. You might as well review and check with your insurance provider for assurance.
0 notes
Text
Lapses in Insurance Coverage
Insurance has been around since people have realized it should be. Yet sometimes, we cannot avoid not paying for our premiums especially when we encounter financial instability. These are called lapses. Westhill Insurance Consulting gives you the outlines of what you should review once you missed paying your premiums.
Grace Period Must Happen Before Lapse
To prevent a life insurance policy from lapsing each and every time a premium payment is slightly late, every state in the country requires that a life insurance policy first go through what is known as a grace period after a payment is missed. This is a period of time (usually 30 days) where despite the missed payment; the insurance policy will still provide coverage and make a full payout if the insured dies.
Only after the grace period has passed without receiving the due premiums can the life insurance company consider the policy to be lapsed. Once a life insurance policy lapses the life insurance company is not under any legal obligation to pay the beneficiaries if an insured person passes away.
Most Policies Can Be Reinstated After Lapsing
After a policy first lapses, the owner may have the option to reinstate the policy. You want to make sure that you reinstate your policy as quickly as possible after a lapse. Different companies have different rules for reinstatement so you shouldn’t file a complaint or burst into frustrations when your insurance company refuses to reinstate your policy as it should already be stated when you were reading the terms before you signed for the coverage.
Importance of Reinstatement Period Lapse
The reinstatement period is very important to policy owners and insured persons for a couple of reasons. The first reason is as discussed, the insured person may not need to go through the underwriting process. If a person has had a major health change, he/she may not necessarily be aware of the change. The underwriting process may uncover more about a person’s health than they ever knew, for better and worse. Avoiding underwriting when possible almost always leads to lower insurance premiums.
The second reason the reinstatement period is very important is that even with the same health rating, a new life insurance policy will always be more expensive than an old policy, because the insured person has aged. The older the insured person, the higher the rates will be, all else being equal. The bottom line is: Reinstating a life insurance policy rather than taking out a new policy will save money.
Reinstatement Will Cost More than One Month Premium
After a policy has lapsed, a larger payment must be made to reinstate the policy. It is in the best interest of a policy holder never to let a policy lapse. Developing cities like Bangkok, Thailand, Jakarta, Indonesia and Kuala Lumpur, Malaysia are strict in reinstatement and its cost as personal insurance are rare.
References:
https://groups.diigo.com/group/westhill-healthcare-consulting
https://www.linkedin.com/groups/Westhill-Consulting-Insurance-5110019
0 notes
Text
Insurance in a Divorce
Divorce is one of the most devastating events in one couple’s life.
While most divorcing couples focus on the delicate and often difficult issues of child custody and dividing assets, breaking up can be hard to do in terms of your insurance policies, too. Whether the policies are in place for protection or as an investment, divorcing spouses need to review them in the context of their new financial circumstances. Westhill Insurance Consulting has listed some matters to be prioritized during this delicate time.
1. Life insurance
Your first step should be to check the beneficiaries on your life insurance, whether you have term or permanent policies. People sometimes forget the existence of their life insurance policies, yet often the amount of money involved is higher than their other assets. If you forget to change the beneficiary of your policy and you pass away, your ex-spouse could get the money instead of your new spouse."
Melody Juge, managing director of Life Income Management in Flat Rock, N.C., says splitting spouses should negotiate ownership of life insurance policies as part of the divorce settlement.
"If your spouse has an insurance policy that you're depending on to take care of you and your kids if he dies, you should have (the) ownership changed to yourself instead of your spouse," says Juge. "If not, your spouse could change the beneficiary or simply stop paying the premiums."
2. Health insurance
Many couples share health insurance under one spouse's employee benefits package; a divorce will require a policy change.
When you work and have previously been covered by your spouse's company, you can generally obtain health insurance through your own employer after a divorce.
Also, the federal law known as the Consolidated Omnibus Budget Reconciliation Act, or COBRA, allows a person going through a divorce to stay on a spouse's group policy for a limited time. But you'd have to pay the full premium yourself. Developing cities like Kuala Lumpur, Malaysia, Singapore and Jakarta, Indonesia are now creating an act similar to COBRA for divorce protection.
3. Home and car insurance
Liability insurance policies for your home and car are particularly important to maintain during and after a divorce.
Divorcing spouses should immediately notify their insurance companies if an asset such as a car or home changes ownership to avoid filing more complaints and causing more crease.
4. Long-term care insurance
Hook says long-term care insurance policies are individual insurance policies, so there would not be much impact from a divorce. But some insurance companies offer a discount for covering a married couple, and that would be eliminated after a split.
Premiums for long-term care insurance should be estimated as part of your expenses during the divorce settlement. Hook suggests that divorcing spouses in their 50s who don't have long-term care coverage should be sure to purchase some.
0 notes
Text
Tips for handling early-year medical expenses

The clock on insurance deductibles reset on Jan. 1, and that means big medical bills are in store for some. Patients may be required to pay thousands of dollars before their health care coverage kicks in.
Insurers typically begin or renew policies in January, and that means customers could face some daunting cost-sharing requirements in the first few months of the year. That’s especially true if they need surgery or have a particularly expensive prescription.
Deductibles topping $3,000 are common among plans sold on the health care overhaul’s public insurance exchanges, which provide coverage for millions. Companies also have been raising deductibles for years on employer-sponsored health plans, the most common form of coverage in the United States. Plus cost-sharing requirements for Medicare prescription drug coverage renew every year.
All this adds up to a business boon for organizations like the Patient Access Network Foundation, which offers grants to help cover prescription costs for dozens of life-threatening, chronic or rare diseases. The nonprofit had to hire about 80 temporary employees to help handle the heavy workload it receives at the start of the year. It fielded 4,000 calls a day last month, double its normal total.
“Everybody who works doing what we do has the same challenge,” CEO Daniel Klein said.
Klein’s foundation is one option patients can turn to if too many expenses hit at the start of the year. Here are some other tips.
Understand your coverage: You can’t prepare for medical expenses until you know how big the bills might be. Your insurance should come with a plan summary that lays out important numbers.
Start by understanding your plan’s deductibles, which can differ significantly depending on whether care is received inside or outside the insurer’s network of providers.
If you take prescriptions, double check how much they will cost. Drug coverage is commonly divided into tiers based on price, and costs can change from year to year.
Most coverage offers some protection by capping the amount you are required to pay each year. But these caps might still expose patients to sizeable bills because they can climb higher than $6,000 for an individual and $13,000 for a family.
Talk to your doctor: Physicians may be able to offer less-expensive treatment alternatives, but be clear on whether these choices are equally effective. If you’re planning a surgery, ask whether it can be delayed, perhaps after you may have satisfied your deductible.
Avoid skipping care entirely. That may make your condition worse, and the unpaid deductible you’re trying to avoid might still need to be satisfied.
Seek help: Big medical expenses at the start of the year can be shocking, especially for patients who are already dealing with leftover holiday bills or other financial headaches. There are a number of agencies that have years of experience helping patients deal with this.
The Patient Access Network Foundation can offer grants of more than $10,000 in some cases to help with expenses. It also provides a list of additional organizations that can assist.
Drug makers frequently help cover out-of-pocket expenses for some of their priciest products. Contact the company that makes your medication or check out the Partnership for Prescription Assistance.
That site, which is supported by drug makers, acts as a clearinghouse to help link patients to hundreds of assistance programs.
Shop around: Many insurers now offer smartphone apps or other services that help patients compare prices for care based on their coverage. It pays to shop around for non-urgent care because costs can vary quite a bit.
For instance, the cost of a primary care doctor visit can range from $117 to $461 inside an insurer’s coverage network in San Francisco, according to Cast light Health Inc., which has designed a technology platform to help employers manage costs and employees shop for care.
Plan ahead: Many employer-sponsored high-deductible plans come with health savings accounts that can ease the sting from early-year medical expenses. These accounts can let families set aside as much as $6,650 before taxes for medical expenses, and employers often contribute to them. But that safeguard requires some foresight. You generally have to sign up for it before your coverage begins.
If you can’t start a health savings account, you can set aside some money from each paycheck in a savings account. If that expense never hits, keep the money parked. You may need it next year, when your coverage renews your deductible resets once again.
1 note
·
View note
Text
Insure your Business in the Clouds

In the turn of the most technologically advanced era yet come more and more advanced fraudulent acts as well. The genius invention of cyber insurance have helped small, medium and large scale businesses in securing their data, shared information and hacked systems. These cyber insurance have already reached not only the leading nations in the world but developing cities and countries as well such as Singapore, Jakarta, Indonesia, Kuala Lumpur, Malaysia, Beijing, China, Tokyo, Japan and many more. If you are one of those who have individual experience with spam, scams, hacks and other illegal computer malpractice, then we at Westhill Insurance Consulting would want to enumerate top ten reasons why cyber insurance is important:
1. Data is one of the most important assets yet it is not covered by standard insurance policies. It is many times worth as the physical product or service that a company is offering. Yet, most business owners do not realize the worth of these data and do not have a standard policy when the files are corrupted, damaged or destroyed. A cyber policy can provide comprehensive cover for data restoration and rectification of a loss no matter how it was caused and up to the full policy limits.
2. Systems are critical to operating your day to day business but their downtime is not covered by the standard business operations interruption insurance. All businesses rely to available systems to operate and organize their business. In the event of a hack attack, scam or computer virus a traditional business interruption policy would not respond. Cyber insurance can cover for the loss of profits associated with a system outrage that is caused by a non-physical peril like a computer virus or service attack.
3. Cyber crime is the fastest growing crime in the world but most attacks are not covered by the standard property and crime insurance. New crimes and complaints are emerging every day. With the use of the internet means that they are exposed to the world’s criminals and is vulnerable to attack any time of the day and night. Cyber insurance can provide comprehensive crime cover for a wide range of electronic perils that are increasingly threatening the financial resources of today’s businesses.
4. Your reputation is your number one asset and it is a must that you are to insure it. Any business is built on its reputation. Although there are indeed some reputational risks that cannot be insured, you can insure your reputation in the event of a security breach. When your systems, files and data have been compromised, you run a very big risk of losing the trust of your most loyal clients which can harm not only your business but your whole life as well. Cyber insurance can not only help pay for the costs of engaging a PR firm to help restore this, but also for the loss of future sales that arise as a direct result of customers switching to your competitors.
More insurance consultations can be found at http://www.westhillinsuranceconsulting.com/blog/. Learn more about insurance for your family and your own welfare.
0 notes
Text
The 5 Best Money Lessons We Learned Last Year

1. It’s Smart to Prepare for a Breach
How many data breaches from 2014 can you name? The freshest one in your mind is probably the Sony hack, but there were also attacks on Home Depot, Staples, Dairy Queen, P.F. Chang’s the list goes on. Credit.com Co-Founder and Chairman Adam Levin recently wrote about the most important lessons you can learn from the Sony hack, encouraging consumers and companies to prioritize data security and behave with the knowledge that your personal information and correspondence could be exposed at any time.
Prepare for the possibility of fraud by monitoring your credit, regularly reviewing account activity and knowing what to do if your personal information has been stolen. Do what you can to strengthen your data security, but know that so much of it is beyond your control, so the best thing you can do is know how to react to a breach.
2. Communication Is Crucial to Getting Debt-Free as a Couple
We published several success stories about getting out of debt, but some of the most memorable involved couples working together to conquer their finances. The stories had similar themes: Ellie Kay married her husband without knowing about his $40,000 of consumer debt, and Ja’Net Adams was unaware her husband took out student loans to pay for college. Both families eventually hit breaking points where they realized debt was holding them back, and they needed to make drastic changes to get rid of it.
Getting out of debt is never easy, and the more people who are involved, the more complicated it can be. At the same time, having someone to work through the challenges with you can be extremely helpful. Adams’ and Kay’s stories highlight two crucial elements of getting debt free: staying committed to a plan and remaining open and honest about the process’ progress and challenges. Those lessons apply to any personal finance goal, whether you’re planning with a family or on your own.
3. Staying Up to Date on Your Credit Is Easier Than Ever
There’s really no excuse these days for not knowing what’s going on with your credit. You can get two of your credit scores for free every 30 days on Credit.com, and you probably have access to other free credit score tools, too. FICO rolled out a program called FICO Open Access, which allows consumers with certain financial products (including Discover credit cards and some Sallie Mae student loans) to review their FICO scores for free. In the past year, many more of these programs have become available to consumers, free of charge, because there’s a strong belief that an informed consumer makes better financial decisions.
Looking at the same credit score periodically helps you understand how your behavior, like credit card use and loan repayment, affects your credit. It can also help you spot and stop fraud and identity theft.
4. Paying for Health Services Is Harder Than It Should Be
In September, Credit.com Director of Consumer Education Gerri Detweiler broke her hand, resulting in a trip to the ER and a messy experience with medical bills.
“Our medical billing system is far too complicated and convoluted,” Detweiler wrote in a December post for Credit.com. “For all the talk of putting patients more in charge of their care, there is little opportunity to make informed decisions. One of the main things that irked me was my complete inability to confirm whether I received the services my insurance company and I paid for.”
This is coming from a woman whose first question upon arriving at the emergency room was whether the provider was in her insurance network. Detweiler’s experience shows you have to be exceptionally persistent in gathering information about your medical bills, otherwise you’ll easily lose track of something and possibly receive a collection notice about it. Even with her diligent record-keeping and frequent efforts to communicate with billing departments, Detweiler still doesn’t have all the answers she wants about her brief emergency room visit.
5. More Education on Student Loan Debt Is Needed
In December, the Brookings Institution released a report saying about half of students polled in a nationally representative survey didn’t know how much they borrowed for their education. That’s absurd. How can people prepare to repay debt if they have no idea how much of it they have?
Add this to the general consensus that borrowers aren’t well enough aware of their student loan repayment options, and the high default rate among student loan borrowers makes a lot of sense. Granted, the share of borrowers who defaulted within three years of entering repayment declined this year, from 14.7% to 13.7%, but that’s still a huge default rate. Considering it takes months of missed payments to default in the first place, there are millions of borrowers who are having serious trouble repaying their education debt who haven’t yet hit the dreaded point of default.
Not only do students need to have a better idea of what they’re getting themselves into when they take out student loans, they need to be well versed in their repayment options, should they find themselves unable to make the payments.
A lot happened in the personal finance world in 2014, and 2015 is sure to be similarly eventful. If these stories are any indication, the best thing you can do to ensure a productive financial year is to make sure you’re informed about your financial situation, credit standing and options for getting out or staying out of debt.
0 notes
Text
Data breach trends for 2015: Credit cards, healthcare records will be vulnerable
The data breaches of 2014 have yet to fade into memory, and we already have 2015 looming. Experian's 2015 Data Breach Industry Forecast gives us much to anticipate, and I've asked security experts to weigh in with their thoughts for the coming year as well.
Experian highlights a number of key factors that will drive or contribute to data breaches in 2015. A few of them aren't surprising: Organizations are focusing too much on external attacks when insiders are a significantly bigger threat, and attackers are likely to go after cloud-based services and data. A few new factors, however, merit your attention.
First, there is a looming deadline of October, 2015 for retailers to upgrade to point-of-sale systems capable of processing chip-and-PIN credit cards. As banks and credit card issuers adopt more secure chip-and-PIN cards, and more consumers have them in hand, it will be significantly more difficult to clone cards or perpetrate credit card fraud. That’s why Experian expects cybercriminals to increase the volume of attacks early in 2015, to compromise as much as possible while they still can.
The third thing that stands out in the Experian report is an increased focus on healthcare breaches. Electronic medical records and the explosion of health or fitness-related wearable devices make sensitive personal health information more vulnerable than ever to being compromised or exposed.
The risk of health related data being breached is also a concern voiced by Ken Westin, security analyst with Tripwire. He pointed out that part of the reason that retail breaches have escalated is because cybercriminals have developed the technologies and market for monetizing that data. “The bad news is that other industries can easily become targets once a market develops for the type of data they have. I am particularly concerned about health insurance fraud—its driving increasing demand for health care records and most healthcare organizations are not prepared for the level of sophistication and persistence we have seen from attackers in the retail segment.”
“There will absolutely be more breaches in 2015—possibly even more than we saw in 2014 due to the booming underground market for hackers and cybercriminals around both credit card data and identity theft,” warned Kevin Routhier, founder and CEO of Core Telligent. “This growing market, coupled with readily available and productized rootkits, malware and other tools will continue to drive more data breaches in the coming years as this is a lucrative practice for enterprising criminals.”
The rise in data breach headlines, however, may not necessarily suggest an increase in actual data breaches. It’s possible that organizations are just getting better at discovering that they’ve been breached, so it gets more attention than it would have in previous years.
Tim Erlin, director of IT risk and security strategy for Tripwire, echoed that sentiment. “The plethora of announced breaches in the news this year is, by definition, a trailing indicator of actual breach activity. You can only discover breaches that have happened, and there’s no indication that we’re at the end of the road with existing breach activity. Because we expect organizations to improve their ability to detect the breaches, we’ll see the pattern of announcements continue through 2015.”
The combination of a rise in actual data breach attacks and an increase in the ability to discover them will make 2015 a busy year for data breaches. Whether we’re defending against new attacks, or just detecting existing breaches that have already compromised organizations, there will be no shortage of data breach headlines in 2015.
For more info: Westhill Insurance Consulting Data breach trends for 2015: Credit cards, healthcare records will be vulnerable.
0 notes
Text
Medicare Overbilling Probes Run Into Political Pressure
When investigators suspected that Houston’s Riverside General Hospital had filed Medicare claims for patients who weren’t treated, they moved to block all payments to the facility. Then politics intervened.
Rep. Sheila Jackson Lee, a Texas Democrat, contacted the federal official who oversees Medicare, Marilyn Tavenner, asking her to back down, according to documents reviewed by The Wall Street Journal. In a June 2012 letter to Ms. Tavenner, Rep. Jackson Lee said blocking payments had put the hospital at financial risk and “jeopardized” patients needing Medicare.
Weeks later, Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services, instructed deputies to restore most payments to the hospital even as the agency was cooperating in a criminal investigation of the facility, according to former investigators and documents. “These changes are at the direction of the Administrator and have the highest priority,” a Medicare official wrote to investigators.
About two months after that order, Riverside’s top executive was indicted in a $158 million fraud scheme. The hospital was barred from Medicare this May, and the CEO was convicted in October.
What happened at Riverside General Hospital shows how political pressure from medical providers and elected officials can collide with efforts to rein in waste and abuse in the nearly $600 billion, taxpayer-funded Medicare system. More than a dozen former investigators and CMS officials said in interviews that they faced questions from members of Congress about policy changes or punitive action affecting providers or individual doctors.
Ricky Sluder, a former senior investigator for a Medicare contractor who oversaw part of the Riverside investigation, said “it was extremely frustrating to stall an investigation to give some explanation to a lawmaker. It’s providers’ way of using political power.”
In an emailed statement, Medicare administrator Ms. Tavenner said the Riverside episode “reflected the tension between fraud prevention and access to care.” She said she wasn’t aware of the pending indictments and that her job required her to “balance two important policy goals” — saving taxpayer money and protecting Medicare’s beneficiaries.
A spokesman for Rep. Jackson Lee declined to comment.
Medicare has reported that during the 2013 fiscal year, waste, fraud and abuse accounted for an estimated $34.6 billion in improper payments to medical providers. CMS says it clawed back about $9 billion that year through audits and investigations.
Medicare hires contractors to enforce antifraud rules and fight improper billing. The contractors can suspend payments to doctors and hospitals and revoke billing privileges. They also can block some payments to review claims — called “prepayment review.”
Such actions can squeeze medical providers and even threaten to put them out of business. Medical providers sometimes seek help from elected officials. Politicians have a stake in such disputes: Health providers often provide jobs and valued services in their districts, and can be campaign contributors.
Houston’s Riverside hospital, for example, had treated patients in that district for nearly 100 years and employed about 200 in 2011.
Ted Doolittle, a former deputy director of the Center for Program Integrity, CMS’s antifraud unit, said most legislators support Medicare’s efforts to fight fraud. But “the member who just lost 150 jobs in her district at the hands of faceless Washington bureaucrats, she is flipping livid,” he said.
Mr. Doolittle, who left the agency in May and joined law firm LeClairRyan, said the antifraud office should be sheltered from political pressure, which he said can interfere with investigations. CMS’s top fraud investigator reports to Ms. Tavenner, who was appointed by President Barack Obama in 2011 and whose agency is overseen by Congress.
In her statement, Ms. Tavenner said: “I must be available and responsive to each of the constituencies that CMS serves, including our beneficiaries, professional associations and elected officials.”
Over the past five full years, medical providers and health-care interests spent $2.5 billion lobbying federal officials and lawmakers, according to the Center for Responsive Politics, fueled in part by a surge before passage of the 2010 health law. That constitutes 15% of all federal lobbying over that period.
The health-care industry long has contributed to lawmakers who oversee government health spending. In the current election cycle, for example, hospitals and nursing homes gave $218,800 to Rep. Kevin Brady, the Texas Republican who became chairman of the House Ways and Means health subcommittee last year, through his personal campaign fund and two political-action committees, according the Center for Responsive Politics. Those contributors gave $39,500 to him in 2012 when he didn’t hold the key position, and when his overall contributions also were less. Prior chairmen of health committees also saw jumps in such donations.
The Ways and Means Committee crafted a March bill that barred Medicare recovery auditors from scrutinizing short hospital stays — historically, an area of concern for incorrect payments — until April 2015. Last month, Rep. Brady put forward a discussion draft for a bill to overhaul audits of those short stays and provide a “comprehensive solution” to hospital payments for those visits, according to a statement from his office.
Hospital lobbyists credited the Ways and Means Committee and Rep. Brady for helping on the audit issue.
A spokeswoman for Rep. Brady said he supports the Medicare audit program “and wants to ensure it is accomplishing its mission — deterring fraud, waste and abuse.” But the current rules for short hospital stays, she said, are “arbitrary” and lack “clinical basis.” She said the March decision was made by Republican leaders in the House.
Medicare providers under investigation sometimes contact lobbying organizations for help.
Medicare investigators began looking into Florida skilled-nursing facilities in 2011 and found what they considered suspicious billing patterns at 33 homes. CMS contractor SafeGuard Services LLC was concerned about how often Florida nursing facilities were charging for the costliest physical and occupational-therapy services, according to documents. About a quarter of the 33 facilities were paid at least 20% more a day than their local rivals, a Journal analysis of Medicare data found.
Three of the 33 are owned by Plaza Health Network. Plaza Chief Executive William Zubkoff previously ran a hospital that was barred in 2006 from billing Medicare and other federal health-care programs following fraud allegations. The U.S. attorney’s office for the Southern District of Florida also is investigating whistleblower allegations that Plaza paid kickbacks for patient referrals between 2008 and 2011.
Lawyers for Plaza and Dr. Zubkoff said neither has done anything wrong and both are cooperating with the investigation. They said Dr. Zubkoff wasn’t personally accused of wrongdoing in the 2006 matter.
By 2012, the Medicare investigators had partially blocked payments to the 33 nursing homes.
Some of the nursing homes contacted the Florida Health Care Association, a trade group. It asked lawmakers and Florida Governor Rick Scott, a Republican, for assistance, according to the group’s director and emails.
Gov. Scott contacted Ms. Tavenner, according to a person familiar with the investigation. The two had once worked together at hospital operator HCA Holdings Inc., where both had been executives. The governor’s office connected CMS to the Florida Health Care Association. The trade group put an owner of two of the nursing homes, William Kelsey, on the phone with Ms. Tavenner.
Mr. Kelsey told her the prepayment reviews were “creating a real hardship on the business, staff and residents,” he recalled recently.
On Aug. 22, 2012, Ms. Tavenner ordered the agency’s antifraud officials to release payments for the 33 homes, including the two operated by Mr. Kelsey, according to emails.
A CMS spokesman said Ms. Tavenner got involved to ensure the agency was “preserving access and quality of care.” The spokesman said Ms. Tavenner “often discusses issues and concerns with elected officials . . . including Gov. Scott.”
In an email ordering SafeGuard to restore payments, John Spiegel, a Medicare antifraud official, said one reason for the action was that the nursing homes were “established providers with long-standing history.”
“Thanks to you and Governor Scott, some sanity has prevailed,” Florida Health Care Association Executive Director J. Emmett Reed wrote to a Scott staffer that Aug. 22.
The spokesman for Gov. Scott said he couldn’t confirm or deny that the governor called Ms. Tavenner about the nursing homes.
Medicare later told its antifraud contractors to avoid using “prepayment review” on skilled-nursing facilities without first receiving approval from CMS, according to documents. The CMS spokesman said the agency instructed contractors to use other approaches to recoup money before resorting to prepayment review.
Former investigators for SafeGuard, a unit of Hewlett-Packard Co., said that decision stripped them of an important tool for fighting fraud and chilled their nursing-home probe. SafeGuard referred questions to CMS.
The CMS spokesman said there is “no single viewpoint” about the value of various antifraud tools, and the agency must also consider patients’ access to care.
As of January 2014, none of the Florida nursing homes caught in SafeGuard’s probe faced any new prepayment action, a former investigator said.
The CMS spokesman said the agency advised law enforcement of its concerns about seven of the nursing homes and that its antifraud investigators referred 30 of them to another contractor to attempt to recoup excess payments.
Houston’s Riverside General Hospital already had been tangling with law enforcement before Rep. Jackson Lee contacted CMS.
In February 2012, in a separate case, the hospital’s assistant administrator, Mohammad Khan, pleaded guilty to defrauding Medicare, admitting that many services weren’t medically necessary and in some cases never provided.
By that time, Medicare antifraud contractor Health Integrity LLC had concluded that 88% of a sampling of Riverside’s partial-hospitalization claims — Medicare’s term for certain outpatient mental-health services — were incorrect, according to government records.
That June 8, Medicare suspended all payments to the facility and put its claims on prepayment review.
Then Rep. Jackson Lee jumped in. In a June 18 letter to Ms. Tavenner, she said the action could harm the “most vulnerable patients.”
Mr. Doolittle, a senior Medicare antifraud official at the time, responded in writing that “the balance favors protecting [Medicare] and the taxpayers,” and the agency would continue to block funds.
At a follow-up meeting that July with Medicare antifraud officials, Rep. Jackson Lee argued that Riverside was the area’s only provider of certain mental-health services, according to CMS investigation records.
Medicare antifraud officials determined that six other providers within 10 miles of Riverside offered the same services, records show, and they again declined to restore payments.
Rep. Jackson Lee spoke with Ms. Tavenner, according to people familiar with the investigation. Ms. Tavenner “listened to her concerns” about how the payment suspension could limit patients’ access to care, the Medicare spokesman said.
Afterward, Ms. Tavenner instructed her antifraud team to restore 70% of Medicare payments to Riverside, effective immediately, according to an email to contractors from a Medicare antifraud official.
At that time, a criminal investigation into Riverside executives, including CEO Earnest Gibson III, was already under way. Ms. Tavenner’s spokesman told the Journal she was unaware of details of the criminal investigation when she ordered the resumption of payments. However, Ms. Tavenner and senior Medicare officials had discussed the possibility of pending law-enforcement action in a conference call earlier the same day, according to one person who was on the call.
Two months after Ms. Tavenner ordered the payment release, federal agents arrested Mr. Gibson at the hospital and charged him with crimes related to health-care fraud.
Medicare officials resumed blocking payments to Riverside, according to investigation records. This May, Riverside’s Medicare billing privileges were revoked for two years, Medicare emails show. A lawyer for the hospital, Clement Aldridge Jr., said the facility now is “on its last breath,” with most of it closed.
Garnet Coleman, the state representative for Riverside’s district, said that after the payments stopped, “there were no patients, so there was no money.” He said low-income people now have fewer choices for psychiatric care.
“We need that kind of care in the community,” he said. But in the end, he said, it became clear to him that the person handling the disputed program “broke the rules.”
Mr. Gibson, the CEO, was convicted in October. His lawyer, Dick DeGuerin, said his client is innocent and is seeking a new trial.
In a recent interview, Mr. Gibson said he was unaware of fraudulent billing at the time, and that he later learned that an employee and some contractors submitted fraudulent bills for their own gain. He said executives sought to retract incorrect bills.
Mr. Gibson said he sought help from Rep. Jackson Lee to “make sure we got a fair shot.”
This June 12, Rep. Jackson Lee requested a phone meeting with Ms. Tavenner to discuss Riverside, an email shows.
CMS employees prepared talking points for Ms. Tavenner, advising her to inform the congresswoman that a revocation of hospital billing privileges is “appealable,” an email shows.
Asked about the June meeting, the Medicare spokesman said Ms. Tavenner “tries to listen to as many of the concerns that are raised as possible and ask many questions of our CMS staff to make sure we are preserving access and quality of care while aggressively preventing and punishing fraud.”
#Medicare Overbilling Probes Run Into Political Pressure#Westhill Consulting Healthcare and Insurance
0 notes