Text
6 months into being a doc
I completely forgot about this little Tumblr blog but here I am 6 months down the line.
Enjoying the job, falling in love with medicine and actually finding it so much more interesting now that I'm working... I love all my seniors and colleagues and have been taken care of so well. I'm learning so much all the time, and I do love it.
The hours can be tough, but I'm grateful all the same. Proud of how far I've come and wish I hadn't been so petrified of becoming a doctor... it really isn't as scary as I thought it would be.
2 notes
·
View notes
Text
doing my first set of nights as a doctor
1 note
·
View note
Text
i saw a quote that said “i feel like i’m constantly worrying about the next part of my life without realizing that i’m right in the middle of what i used to look forward to.” and i felt that.
18K notes
·
View notes
Note
Hey! Hope you're well. I was wondering what sorts of tasks you had to do as an F1 or F2 on nights on call. And when would you involve someone more senior?
Hello! It depends on what kind of Hospital At Night protocol your hospital has. But broadly speaking, it’ll be things like:
re-siting cannulas, if your nurses can’t do it. Because those IV antibiotics can’t give themselves.
Prescribing paracetamol for people who are in pain/ have a headache/have a temperature of 37.5. Do this, but it will never be your first priority.
Someone will want tablets to sleep. Have a high threshold for starting these.
“This patient hasn’t opened their bowels for 10 days”…. and people decide to tell you at 5am.
This chart needs rewriting. Yes, really. You will curse the day team for not doing their job, but eventually you’ll probably go and do this anyway.
This patient needs to go home but the TTO isn’t done. Nobody cares about the fact that you don’t know the patient or anything about their 6 month stay. You might get time to do this eventually, but clinical needs will have to come first. This will not be a popular decision.
Someone wants opioid pain relief. Unless it is an urgent acute medical emergency in which opioids are indicated as part of best practice (like sickle cell crises, burns, MIs,) use your WHO pain ladder. Be VERY wary.
“Doctor, this patient is agitated, can’t you give them something to calm them down”. Remember that a good calming chat has much fewer side effects. Tell them to call security, and encourage adequate nursing staffing/requests for extra staffing if patients need 1 on 1 care. If you must use pharmacological means, for their best interests, check your hospital’s sedation protocol before you give anything.
You do not have to prescribe anything you do not feel safe prescribing. It is your name on the prescription. Your GMC number.
Do not take patients’ or relatives’ words on dosages; if you don’t have a report from the GP, or a box with a label on it, be careful. People often think they remember their dosages, and some do, but many are… somewhat confused about what they take.
“Doctor, the fluids ran out for Bed 7 on ward 8, would you like some more fluids written up?”. Don’t prescribe any fluids without a look at someone’s U&Es and their fluid status/ a listen to their lungs. Iatrogenic fluid overload and hypokalaemia/hypernatremia are a real thing.
“The bloods just came back from the lab, and the creatinine is 400/ potassium is 8 / D dimer is 5078 / Troponin is 497″. The day team should have handed over the case and why they did these tests, but now you’ve got another thing to sort out.
Early on in your shift there might be at least one set of patient relatives who don’t know that the patient’s actual medical team have gone home, don’t listen to what the nurses tell them, and ask for ‘the doctor’ to come and tell them the same thing. You might have time to speak to them (doubtful); I usually warn the nurse to tell them that I will be around if and when I can, but they may not still be there, because I’m dealing with sick patients. And that the best thing to do would be for them to call the ward the next day to book a meeting with the regular doctors.
Never say ‘no’ to a nurse’s request for you to come do something. Be polite when they bleep you, let them know you will come as soon as you can. If it’s low on your list, warn them you may be some time.
prescribing the warfarin that people forgot to write up duting the day. What’s the INR? Who knows? Protip: be careful about changing people’s dosages in the middle of the night if you don’t know the entire history.
dealing with hypoglycaemic patients; hours of coaxing patients to eat some toast already.
dealing with hyperglycaemic patients; is it DKA or not?
Everyone is Falling Down, falling down, falling down. Falls reviews will be your least favourite job, because they could have been avoided.
Someone has melaena! Or haematemesis, or both. Oh no. Upper GI bleeds will buy patients an OGD in the morning and possibly a blood transfusion overnight.
Oh, the haematuria! Is it because they use their catheter as a stress toy, or is there something sinister?
“Doctor, we can’t catheterise this patient because of something to do with their prostate, so please come and do it.”
This patient has been coughing for 3 days, and you’ll never guess what their saturations are doing now! (spoiler alert: they have HAP)
Someone is having chest pain and their ECG is kinda funny; the only time you will see a STEMI outside of the cath lab is on the ward. This is what calling your reg is for; you can give the initial treatment but they will need to get them a ticket to the cath lab stat.
This patient is having SOB and everyone thinks it’s pneumonia, but the surgeons gave them 8L of fluid today; Flash Flooding of the Lungs.
Sepsis! At the disco. Sepsis! on the ward. Sepsis! is basically hiding everywhere. Have a low threshold for diagnosing sepsis.
“Doctor, something just doesn’t look right about this patient.” Have a very low threshold for calling for help on this one. Nurses know.
Somebody had a seizure, and by the time you get there, they no longer have a seizure. If they are still having a seizure, put out a crash call for status epilepticus.
This patient is DNACPR and for ward based care, so they are almost at he limit of what we can do, but now they look peaky and their blood pressure is dropping, can you please do something? You will, but they will probably die anyway. Do not be afraid to ask for senior help, even if they tell you “you’re doing all we can do”. It always feels hard when you reach the limit of what you can do.
Somebody died, but it’s OK, because they were expected to die. You just need to certify them at some point. Worry about your living patients first.
CRRAAAASH CAAAALL! ALL HANDS ON DECK! Everyone will show up to this one.
Those are the kinds of things you might see on nights, but by no means an exhaustive list. Your bleep will keep on ringing. Make sure to take time to eat and pee at some point. Prioritise things in order of clinical urgency. The key is that you get as much detail as possible on the phone from the nurses. The patient’s name, hospital number, DOB, ward number and bed number. Then their observations and situation. When you go there, assess them through an ABCDE framework. If they are stable, examine them then look through their notes. This is the time when you make a judgement of how ill they are. If they are stable enough that you don’t feel they are about to die on you, then you can start treatment or investigation then discuss with a senior. But if they are really unstable, there is nothing wrong with calling the SpR even then, or putting out a peri-arrest call. If you need to initiate a treatment, then you start it. If you need investigations, then you take and send them. Most of the time, this will be enough.If they are unstable, you need to ensure that they are improving before you move on. If your initial treatments don’t stabilise the patient, then you should reassess them and call for senior help. If you are facing several very-sick sounding patients, then call your other colleagues; the SHOs on call, the reg. Don’t be afraid to let your seniors know that you have 3 sick patients to attend and can’t attend all of them at once. Your reg on call is ultimately your team leader on the ground, and they won’t know what’s going on with you unless you tell them.If you need help, you can always ask for advice.
Your hospitla intranet will have lots of useful protocols on it. I kept the most common ones I needed printed out in my clipboard. A handbook of medicine (or acute medicine) in your bag/pocket can be really useful. I go into more detail in my posts about surviving nights and tips for new docs (can be found on my #tips for new docs hashtag). Hope this helps!
72 notes
·
View notes
Text
Junior doctors in England to strike for four days in April
20 notes
·
View notes
Text
sitting the prescribing exam today and then after that... I’m done!
0 notes
Link
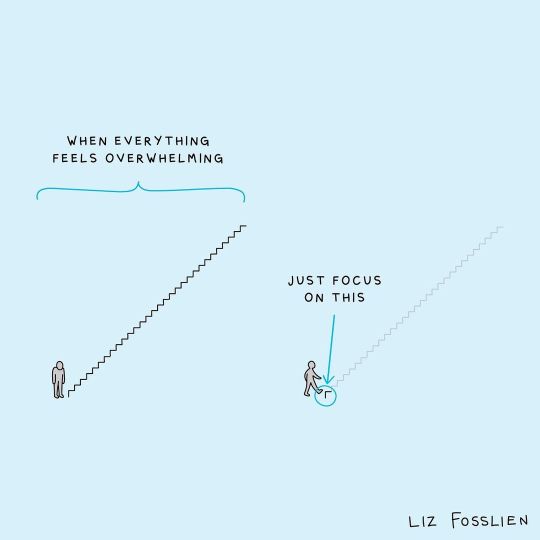
“I believe this message, more than almost any other, can benefit medical students. He says this: “We start here, and we go there. But it’s not that simple, is it? Our paths may be circuitous or direct. We may gaze excitedly ahead, or cast our eyes regretfully behind. Until we reach our destination it exists only in our minds. It is what we have imagined it to be. And yet we tend to neglect the journey, which is real, in favor of the destination, which is not. For too long I neglected this journey. It was an obstacle to be overcome, an ordeal to be endured; for I had never chosen the journey, I had chosen the destination. But now that the journey has ended, I have discovered that here isn’t so important after all. I find myself looking back with particular fondness for how I got here.”
Brent Schnipke at Boonshoft School of Medicine at Wright State University reviews the book Hot Lights, Cold Steel, which explains that we should appreciate the journey through medicine more than the destination we are trying to reach.
64 notes
·
View notes
Quote
Study, as this is the only thing you can do as a student, for now. Study, while you are still given the opportunity, as not everyone is given the chance to be educated. Study, so you would know how to make a difference, not just for yourself, but for the whole world.
Me (intellectual zombie)
537 notes
·
View notes
Text

It is time to take the books and start studying, you will achieve your goals📚🎓✨
5K notes
·
View notes
Photo



Cleaned my desk and took some more photos of the mountains you guys seemed to like! This time they looked pink.
2K notes
·
View notes
Text
One OSCE down, one OSCE to go. I cannot believe in 12 hours I will have completed all my medical exams at Medical school...
Final ever medical school finals done!
#inshallah anyway#also PSA doesn't count#although I'm sure my tone will change in a few months lol#it's crazy#I feel so weirdly sentimental about it all
2 notes
·
View notes
Text
Onto the OSCE in a week eurgh 🧟
Final ever medical school finals done!
2 notes
·
View notes
Text
Final ever medical school finals done!
2 notes
·
View notes