#pre-exposure prophylaxis (PrEP)
Text
Embracing Hope and Unity: A Reflection on World AIDS Day
As we come together on December 1st to observe World AIDS Day, it’s not just a day on the calendar; it’s a powerful reminder of solidarity, compassion, and the ongoing fight against HIV/AIDS. In this blog post, we’ll delve into the significance of World AIDS Day, the progress made, and the importance of continuing our collective efforts.
International Men’s Day: A Tribute to Men’s…

View On WordPress
#Acquired Immunodeficiency Syndrome#antiretroviral drugs#CD4 cells (T cells)#community engagement#compassion#December 1st#End inequalities. End AIDS. End pandemics#Ending the HIV/AIDS epidemic#fight against HIV/AIDS#HIV prevention#HIV treatment#pre-exposure prophylaxis (PrEP)#Putting communities at the center#significance of World AIDS Day#solidarity#Stigma and discrimination#WHO#World AIDS Day
0 notes
Text
My dear lgbt+ kids,
Let's talk about PrEP and PEP.
PrEP is short for pre-exposure prophylaxis. It's a safe* and highly effective medicine (pills or shots) you can take to reduce your chances of getting HIV. When taken as prescribed, it reduces the risk of getting HIV from sex by about 99% and the risk of getting it from drug injection by at least 74% (Source)
PrEP may be the right choice for you if you have an ongoing risk of HIV exposure. For example, if you:
have frequently changing sexual partners, or
are a sex worker, or
do not consistently use condoms, or
have an HIV-positive partner, or
have been diagnosed with another sexually transmitted disease, or
have used multiple courses of PEP (see below), or
inject drugs and share needles, syringes, or other drug injection equipment (for example, cookers).
Even if none of these apply to you, PrEP could still be helpful for you - talk to a healthcare professional about your individual situation.
Some more important info:
Teenagers can take PrEP if they are at risk!
Before beginning PrEP, you must take a test to make sure you are currently HIV-negative.
PrEP takes some time to work (about 7 days for anal sex, about 21 days for vaginal sex or drug use).
It's not the right choice if you think you may already have been exposed to HIV - if you think you have been exposed within the last 72 hours, ask for PEP right away.
PrEP is much less effective when not taken as prescribed.
PEP is short for post-exposure prophylaxis. It's medicine for emergency situations. You can take it after possible exposure to HIV (e.g if a condom broke or after sexual assault). It's safe* and highly effective but only if taken within 72 hours of exposure - when it comes to PEP, every hour counts! Don't wait, talk right away to a health care provider, an emergency room doctor, or an urgent care provider.
PEP is not a substitute for condoms and doesn't provide ongoing protection.
*While they are safe, PrEP and PEP can have side effects (such as nausea). In almost all cases, these side effects aren’t life-threatening. They usually go away on their own or can be easily treated. Talk to a healthcare professional if you are concerned about side effects.
With all my love,
Your Tumblr Dad
924 notes
·
View notes
Text
"Five people have gone into remission thanks to advancements in medicine — and a sixth patient may also now be free of HIV.
One of the biggest breakthroughs in HIV/AIDS prevention in recent years is the widespread use of PrEP (pre-exposure prophylaxis).
This drug therapy, approved by the Federal Drug Administration in 2012, has been a key player in preventing HIV transmission through sex or injection drug use. Antiretroviral drugs, such as PrEP, also slow the replication of the virus and prevent it from progressing to AIDS.
Although PrEP has become a more accessible treatment for the virus, scientists have been hurriedly working towards cures for HIV for decades — and we’re finally seeing some results.
In February of this year, scientists in Germany confirmed a fifth-ever patient had been cured of HIV after receiving stem cell transplants that include genetic mutations that carry a resistance to HIV.
But it looks like a sixth patient may soon be able to join this very exclusive club.
The man, referred to as the “Geneva patient,” underwent a stem cell transplant after cancer treatment, though these cells did not include the HIV-resistant genetic mutation.
Still, he went off antiretroviral therapy for HIV in November 2021, and his viral load remains undetectable.
Instead, doctors are researching whether a drug called ruxolitinib may be partially responsible for his recovery.
Ruxolitinib decreases inflammation associated with HIV by blocking two proteins, JAK1 and JAK2. This helps kill off “reservoir cells” that lay dormant in the body and have a potential to cause rebounds in patients with HIV.
Experts say the AIDS crisis can end by 2030 across the globe — as long as leaders prioritize this goal.
A new report from UNAIDS shows a clear, optimistic path to ending the AIDS crisis. (This looks like a 90% reduction in cases by 2030.)
The organization’s report includes data and case studies that show that ending AIDS is a political and financial choice — and that governments that have prioritized a path towards progress are seeing extraordinary results.
By following the data, science, and evidence; tackling inequality; and ensuring sufficient and sustainable funding across communities, the global community could wipe out the AIDS pandemic by the end of the decade.
The report demonstrates that progress has been strongest in the countries and regions that have the most financial investments, like eastern and southern Africa, where new HIV infections have been reduced by 57% since 2010.
Investments in treatments, education, and access to care have also led to a 58% reduction in new HIV infections among children from 2010 to 2022 — the lowest number since the 1980’s.
Plus, the number of people on antiretroviral treatment around the globe has risen from 7.7 million in 2010 to 29.8 million in 2022.
The moral of the story? This goal can be achieved, if world leaders put their minds — and wallets — to it.
A region in Australia might be the first place in the world to reach the United Nations targets for ending HIV transmission.
Researchers believe that the central district of Sydney, Australia is close to becoming the first locality in the world to reach the UN’s target for ending transmission of HIV.
Specifically, new infections among gay men have fallen by 88% between 2010 and 2022. In fact, there were only 11 new HIV cases recorded in central Sydney last year, and almost all HIV-positive Australians are on antiretroviral drugs.
... "These numbers show us that virtual elimination of HIV transmissions is possible. Now, we need to look closely at what has worked in Sydney, and adapt it for other cities and regions across Australia.”
Namibia is ahead of schedule in UN targets to end HIV/AIDS.
Although the virus is still the leading cause of death in Namibia, the country is well on track to hit 95-95-95 UNAIDS targets before its 2030 deadline.
In Namibia, 92% of people know their HIV status, 99% of people living with HIV are on treatment, and 94% of people living with HIV who are on treatment are virally suppressed.
In addition to these exciting statistics, new infections have plummeted. The estimated rate of new HIV infections in Namibia is five times lower than it was in 2002, according to the Centers for Disease Control & Prevention.
These encouraging numbers are thanks to the investment and strategic response of PEPFAR, but also to the willingness of local governmental agencies and organizations to adhere to the UN’s Fast-Track approach.
Breakthroughs are being made in HIV vaccine therapies.
Long before we were all asking each other “Pfizer or Moderna?” about our COVID-19 vaccines, scientists have been researching the potential of mRNA vaccines in treating some of the world’s deadliest diseases — like HIV.
And with the success of our mainstream mRNA vaccines, an HIV inoculation remains a goal for researchers across the globe.
Last year, the National Institutes of Health launched a clinical trial of three mRNA vaccines for HIV, and similar studies are being conducted in Rwanda and South Africa, as well.
CAR T-cell clinical trials are underway to potentially cure HIV.
This spring, UC Davis Health researchers have dosed the second participant in their clinical trial, which poses the use of CAR T-cell therapy as a potential cure for HIV.
The study involves taking a participant’s own white blood cells (called T-cells), and modifying them so they can identify and target HIV cells, ultimately controlling the virus without medication.
The first participant in the study was dosed with anti-HIV T-cells last August, and the trial is the first of its kind to utilize this technology to potentially treat HIV.
Of course, the trials have a long way to go, and the lab is still preparing to dose a third participant for the study, but CAR T-cell treatments have been successful for lupus and forms of cancer in the past...
“So far, there have been no adverse events observed that were related to the treatment, and the two participants are doing fine.”
Guidance on how to reduce stigma and discrimination due to HIV/AIDS is reaching people around the globe.
While the stigma surrounding HIV and AIDS has significantly decreased — especially towards the LGBTQ+ community — with advancements in treatment and prevention, discrimination is certainly not gone.
While most people now understand HIV/AIDS better than they did decades ago, those most impacted by the virus (like gay men and low-income women and children) still face ongoing barriers to care and economic security.
It is vital to maintain awareness and education interventions.
After all, experts suggest that eliminating discrimination and stigma are key factors in reducing disease. And not eliminating stigma impedes HIV services, argues UNAIDS, “limiting access to and acceptance of prevention services, engagement in care, and adherence to antiretroviral therapy.”
Luckily, UNAIDS provides guidance on how to reduce stigma and discrimination in the community, workplace, education, health care, justice, and emergency settings.
The goal is to, of course, decrease stigma in order to decrease disease, but also to provide folks with the culturally significant support they need to live safe, integrated lives — with or without disease.
For instance, a 2022 study conducted in Northern Uganda showed that local cultural knowledge passed through Elders was a successful intervention in reducing HIV-related stigma among young people.
“Research in school settings has shown that the use of local cultural stories, songs, myths, riddles, and proverbs increases resilient coping responses among students and strengthens positive and socially accepted morals and values,” the study’s discussion reads.
So, while an uptick in acceptance gives us hope, it also gives us a directive: Keep telling the accurate, full, and human stories behind HIV/AIDS, and we’ll all be better for it. "
-via GoodGoodGood, August 3, 2023
#hiv#hiv/aids#aids crisis#public health#medical research#vaccines#australia#namibia#united nations#queer issues#trans issues#lgbtq issues#lgbtq community#infection prevention#good news#hope
268 notes
·
View notes
Text
Love in the Big City: Part Four- Regret, Rain, Love, and Loss
Well, it’s official. Love in the Big City, Part Four may have been short but it cemented itself as my favorite portion of the book. I asked @antonhur when he was so graciously answering questions what his favorite scene in the book was, and I can see why he said when they were lying in the rain in Bangkok; Late Rainy Season Vacation indeed. When I first started this book, I was talking with a few mutuals like @bengiyo and @lurkingshan wondering how I would feel about Young by the end of this book, because I was not a huge fan of his character in Part One. But I have very much enjoyed seeing his progress across these parts. I said already in my post about Part One that my biggest struggle with Young and the thing I think primarily contributes to the change in his friendship with Jaehee is that he cannot be serious, he cannot, does not allow himself to feel. And in Part Four, he’s finally admitting to it.
“I was too late to put things back the way they’d been”
“That is how my memories of him are preserved under glass, safe and pristine, forever apart from me”
“I’ve no choice but to stand at arm’s length”
Part Four is my favorite part of this novel because Part Four is full of ghosts. Not only the ghost of Gyu-ho, but the ghost of all that came before. The rooftop party with Gyu-ho where he got plastered on whatever alcohol he could, where now he sits and drinks champagne, a ghost of both his relationship and the way he spent his college years. Going through Habibi’s wallet, a ghost of when he snuck a look at Hyung’s secrets all those years before. The text messages Young saw on Habibi’s phone about a family member with cancer, a ghost of his mother’s own diagnosis. Habibi himself, getting unexpectedly deep for only a moment before forcing the conversation away from anything real, a ghost of Young himself, and all the times he just could not bring himself to be open and honest with the people around him.
Just like learning about the HIV diagnosis recontextualizes everything that came before it (see a wonderful essay about that by @twig-tea here) ending this book with the admission that his only wish a year ago was for Gyu-ho recontextualizes my understanding of how aware Young was about his own modus operandi. I operated under a much different assumption that Young didn’t know what he had until it was gone, that Young was not aware of how far his fears ran, of how distant he had made himself. I assumed Part Four was where Young starts to realize himself the way he’d behaved in the past and how that contributed to the downfall of his relationship to Gyu-ho. But now I think he knew it all along and he just didn’t trust us enough to say it until the end. Because I’m not quite sure even by the end of this book Young trusts us enough to be completely honest.
I talked in my post for Part Three about HIV treatments and prevention methods, and mentioned Truvada, (generic name: emtricitabine-tenofovir) which is a pre-exposure prophylaxis medication that can be taken to prevent someone without HIV from getting HIV should they have an exposure. I mentioned there that at the time of Young’s relationship with Gyu-ho, Truvada was not available on the market in South Korea. But as it turns out, Teno-Em (tenofovir-emtricitibine), a generic PrEP medication, was available in Bangkok by 2015. In Part Four, Young describes going to a pharmacy and getting a generic medication, and he writes the errand in such a way as to make the whole thing seem shady. And maybe it was. But maybe he was just afraid, and that fear colored his own perceptions of what was going down:
My expectation had been that the place would be hidden away in some seedy alley, but it was right there on the main street. The interior was almost the same as any other pharmacy. I showed the pharmacist a picture of the generic version of what I needed. The pharmacist, if he really was a pharmacist, took out a bottle of pills and explained to us, in English, how they worked. He said that taking just one a day at a set time was enough to perfectly prevent the disease. He really said the word “perfectly.” How could he be so confident? He added that taking two of the pills before risky intercourse and then a pill every twenty-four hours for two more doses was enough to prevent transmission.
The facts are these: the pharmacy was on a main street, the pharmacy looked like a pharmacy, the pharmacist was able to explain how the medication worked, and the pill regimen for prevention was accurate to the pill regimen for PrEP.
Could they have still been shady? Sure. But I think it is far more likely that Young and his historically terrible experiences with medicine have colored his perception of healthcare and placed doubt in his head over the legitimacy of this medication. Which, learning that Young and Gyu-ho have unprotected sex in Bangkok, makes me wonder if Young’s doubts about the pharmacy added another reason for him to let Gyu-ho go to Shanghai alone, if the meds they got in Bangkok weren’t real, if they didn’t work, then he likely gave Gyu-ho HV.
Young talked about stains in this part, about permanency- the soy sauce on the mattress, the crack in the toilet and he talked about fleeting things- immediately losing the shape of Habibi’s face when he stepped outside the door, the lantern burning up and turning to ash with all the dreams, all the wishes Young had, or just the one. Regret seems to hold a permanent place in Young’s spirit, as does loss. Love is something I think he thought did not exist, or if it did then it was fleeting. He loved Jaehee and lost her, his first boyfriend died, the obsession he had over Hyung could only be described as dickmatized. But when he gave away Gyu-ho’s love, when he let Gyu-ho go to Shanghai alone, it was one of the few times in the entire novel we saw Young grieve. He fully collapsed under the weight of it all, barely leaving bed, not having the energy to maintain his typical routines, trying to root out the memories of Gyu-ho in his head by writing him out, and killing him over and over and over again.
I find myself stuck, thinking about what is perhaps my favorite line in the book:
“Sometimes his very existence to me is the existence of love itself”
Gyu-ho’s existence is Young’s idea of love; to kill Gyu-ho, to remove him from existence is to kill Young’s idea of love. “The made-up Gyu-ho in my writing got hurt or died many times, and is always resurrected, as if love saves his life- whereas the real Gyu-ho lives and breathes and keeps moving on.” Young’s regret is a permanency in his life, just as his love for Gyu-ho is a permanency. All he wished for was Gyu-ho, but Young’s inability to be honest, deeply, emotionally honest, all the fear, all the emptiness, all the pain got in the way. I am not a person who minds a melancholy end, regret, remorse, grief, love. These are all a part of life. The only thing I hope is that one day Young can lay down in the pouring rain and feel peace the way Gyu-ho did that day in Bangkok.
#litbc#litbc book club#love in the big city#love in the big city book club#very much looking forward to seeing these television adaptations#thank you to shan and ben for the brilliant idea to have a book club#it has been so much fun participating in this event!
20 notes
·
View notes
Text
It is spelt AIDS, which can be stylised to Aids - it is not a plural, it stands for Acquired Immune Deficciency Syndrome. HIV stands for Human Immunodeficiency Virus.
You cannot transmit AIDS to somebody else. HIV is the one which is transmitted; AIDS comes as a result of untreated HIV. We have no cure for HIV, but we do have treatments.
It is very rare for somebody to become diagnosed with AIDS in today's modern world, as HIV treatment has gotten incredibly effective.
PEP (Post-Exposure Prophylaxis) is taken within three days of exposure to the virus, and is an emergency measure which can stop the virus from taking hold. PEP is taken AFTER exposure.
PrEP (Pre-Exposure Prophylaxis) reduces the chance of getting HIV by stopping the virus from replicating before it can take hold; you take it before risk of exposure. PrEP is taken BEFORE exposure.
ART (Antiretroviral therapy) is taken by people living with HIV; it surpresses the virus, which stop the virus from replicating. This is taken every day, to try to make the Viral Load as low as possible - that is to have a low amount of HIV virus in your body. The end goal is for tests to come back negative - Undetectable equals Untransmittable (U=U) - if it cannot be detected by tests, it cannot me transmitted.
Go forth, spell it correctly. And donate to THT, whilst you're at it - THT is a wonderful organisation which offers HIV testing, post-HIV living advice, and does other important work for our wonderful community, such as their incredible non-judgemental chemsex support group.
6 notes
·
View notes
Text
A federal judge in Texas on Thursday blocked Obamacare's mandate that health insurance plans cover preventive care, including screenings for certain cancers and pre-exposure prophylaxis against HIV (PrEP), at no cost to patients.
U.S. District Judge Reed O'Connor in Fort Worth, Texas, previously found that the PrEP mandate violated a federal religious freedom law and that other no-cost preventive care mandates were based on recommendations by an illegally appointed task force.
Mr Biden what you must do is ignore this ruling, state unequivocally that this ruling is invalid because the flag in the courtroom has a fringe on it.
20 notes
·
View notes
Text
On the eve of Valentine’s Day, Martin* received a piece of particularly bad news from a friend: "I've just been tested, and you're the only person I have had unprotected sex with. Voilà, I have syphilis now."
Martin rushed off to get tested: He tested positive. Once he had gotten over the shock, he quickly went through his list of sexual partners and remembered a recent encounter with a woman with whom he had not used protection. After a brief exchange, she confirmed she had syphilis and had been a carrier for some time. But just like Martin, she had preferred taking the risk rather than having protected sex.
Martin’s case is not unique. According to a report issued by the French health authority Santé Publique in December, sexually transmitted bacterial infections (namely, chlamydia, gonorrhoea and syphilis, as opposed to HIV, which is a virus) rose sharply in mainland France between 2020 and 2022.
Although chlamydia remains the most recurring sexually transmitted infection (STI) in absolute terms, up 16 percent from 2020 with 102 cases per 100,000 inhabitants, experts are alarmed by the sharp rise in gonococcal infections, and especially the huge increase in syphilis. The number of gonococcal infections jumped by 91 percent (44 cases per 100,000 inhabitants) in the two-year period while syphilis soared 110 percent, to 21 cases per 100,000 inhabitants.
Syphilis first appeared in the Middle Ages and was nearly eliminated in the second half of the 20th century, but in recent years it has resurfaced in most Western countries, particularly in the United States. According to the US Centers for Disease Control and Prevention, syphilis has now reached its highest infection rate since the 1950s, the New York Times reported in a January article.
With more than 207,000 cases diagnosed in 2022, the last year for which data is available, the US now has an infection rate of 17 cases per 100,000 inhabitants – an increase of 80 percent since 2018.
PrEP, a false sense of safety?
So why is this happening? Doctors say scientific advances, especially in the fight against HIV, are partly to blame. "People are protecting themselves less and less, in part because they’re no longer afraid of AIDS, since the scientific advances mean that it is now possible to lead an uncomplicated life even you have HIV," Pierre Tattevin, the head of the infectious diseases department at Rennes University Hospital, explained.
According to most doctors, people “relax” when they don’t have to fear HIV anymore. “That's the negative effect of using PrEP,” said Jean-Paul Stahl, infectiologist and emeritus professor of infectious diseases at Grenoble University.
PrEP, a pre-exposure prophylaxis, is a retroviral drug that is taken before any potential exposure to the HIV virus in order to help prevent contamination. It has become extremely popular in the past few years, especially among gay and bisexual men who are single. The pill is routinely offered in public hospitals to anyone reporting to have had sex with more than 10 different partners in the past 12 months, regardless of whether they have had protected sex or not.
“PrEP gives users the impression that they are protected from everything, and they think they can have all kinds of risky sexual relations, but it only protects them against HIV,” Stahl warned.
The danger of dating apps
But according to Pierre Tattevin, there is also another reason for the steep rise in STIs. “It’s become extremely easy to find sexual partners via dating apps. You multiply partners without knowing who they are, what their habits are, or what their [sexual] history is,” Stahl, who also presides the French Infectious Diseases Society (SPILF), said.
According to the December report by Santé Publique, the men most at risk of contracting gonorrhoea or syphilis, representing nearly 80% of cases, have multiple partners and a history of STIs.
More generally, it is men who are most affected: they account for 77 percent of gonococcal cases and more than 90 percent of syphilis cases. For the majority of syphilis cases, men aged 50 and over are most affected.
Chlamydia, on the other hand, affects women more, especially young women aged between 15 and 25.
Great risk to pregnant women
The public fear of syphilis has diminished in the past half century or so thanks to a safe and very effective treatment for it: antibiotics. "It's a cure, of course, and once it's cured, there are no further effects or complications if the infection is detected quickly," Stahl said.
Except that, if left untreated, syphilis is a very serious disease. It can damage the heart, brain and eyesight, and could go as far as to cause deafness and paralysis. An infection during pregnancy can lead to miscarriage or stillbirth. Children who survive through birth may also suffer vision or hearing problems, and developmental delays.
While the number of syphilis cases only increased slightly among heterosexual women in 2021 and 2022, "around three quarters of syphilis cases involved MSM [men who have sex with men], regardless of the year surveyed”, the study said.
The researchers further warned that "STIs represent a major public health problem because of their transmissibility (to partners and mother and foetus), their frequency, the long-term complications they cause (chronic pelvic pain, upper genital infections, infertility, cancer, etc.) and their role in HIV transmissions".
‘Can’t hand out condoms to everyone’
Doctors say that although the number of registered STI cases is on the rise in France, it is also a testament to the fact that the country has a well-functioning testing system, which is essential to stopping an epidemic.
“When you miss one case, you then end up with two more cases, and if you miss two cases, you then end up with four,” Dr Jay Varma, chief medical officer at Siga Technologies and a former deputy commissioner of health for New York City, said in an interview with the New York Times. “That’s how epidemics grow.”
Tattevin agreed. "Our different governments have pursued good policies in recent years, with free testing centres. We need to test even more, especially patients at risk,” he said.
In addition to information campaigns, Stahl insisted on personal responsibility. “Those who use PrEP need to know what they're risking. Because some know about the risks involved but decide to take them anyway," he said. “Scientific information is always beneficial, but at the end of the day, the decision comes down to each and every individual.”
"The government can't hand out condoms to everyone," he said.
Martin, meanwhile, continues his conquests: sometimes protected, sometimes not, but for now, at least he is cured.
*The first name has been changed at the request of the person.
4 notes
·
View notes
Text
Brazilian regulators greenlight HIV prevention drug

Brazil’s federal health regulator Anvisa has approved injectable cabotegravir, a pre-exposure prophylaxis (PrEP) medication for HIV. The registration was published in the official gazette on June 5.
Injectable cabotegravir has been recommended as a preventative treatment for HIV by the European Medicines Agency (EMA) since October 2020. The U.S. Food and Drug Administration (FDA) approved it in late 2021 for use in at-risk adults and adolescents over at least 35 kilograms for pre-exposure prophylaxis to reduce the risk of sexually acquired HIV.
In 2022, the World Health Organization also recommended that member countries approve injectable cabotegravir as PrEP for HIV.
Continue reading.
#brazil#politics#healthcare#hiv aids#brazilian politics#anvisa#mod nise da silveira#image description in alt
16 notes
·
View notes
Text
The Weather
A study in Clinical Infectious Diseases reported “that the risk of developing symptomatic illness within 14 days was 5 times greater when contacts were exposed to an asymptomatic [COVID]-positive child in their household.” Nearly 11% of household contacts developed symptoms within 14 days of exposure. The study also found, during a 3-month follow-up, that 6 out of 77 asymptomatic children developed Long COVID. The likelihood of developing symptoms from asymptomatic exposure is higher than we might expect. Continue to spread awareness of asymptomatic spread and advocate for increased infection control measures at your local schools.
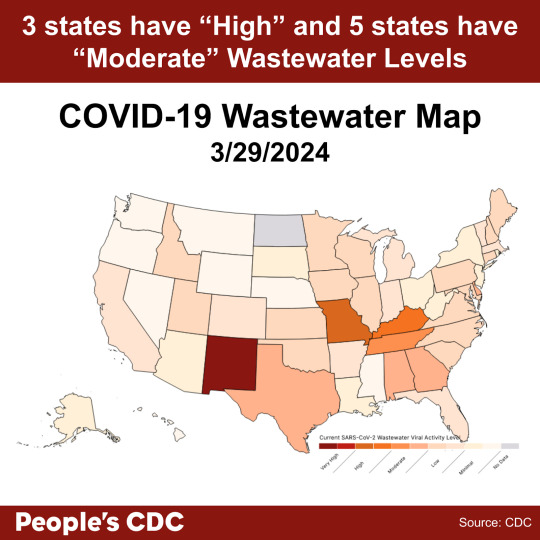
COVID wastewater levels are decreasing. As of 3/29/24, New Mexico is “Very High,” Arkansas and Kentucky are “High,” and the rest of the states are “Moderate” to “Low” levels of SARS-CoV-2 detected in wastewater.
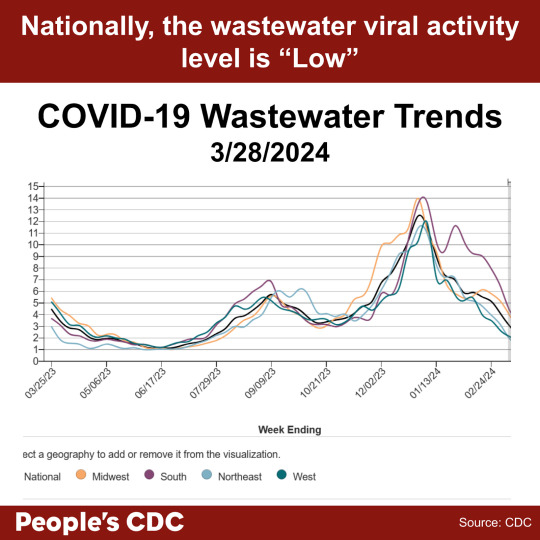
Wastewater levels continue to show a downward trend in the provisional data (gray shaded area) in all regions. The national wastewater levels are overall indicated as “Low.” While lower wastewater levels indicate decreased spread, it is important to continue to take precautions against infection. Holidays and spring breaks may bring people in closer proximity, so be sure to wear a mask to protect yourself and your community.
Wins
As we work to take more actions against the removal of vital public health measures, we remind you that you can still watch the recording of the People’s CDC press conference from March 13 and read the press release here. We would also like to remind you of the pre-proof of the People’s CDC External Review in the American Journal of Preventive Medicine Focus. The publication highlights the shortcomings of the CDC’s approach to public health and recommends a more equitable pandemic response.
News sources have published articles about the frustrations of people who continue to take COVID precautions. Time Magazine published an article presenting “both sides,” highlighting protest from people working with the CDC and concern from citizens and experts alike. While we are glad to see our voices be published in popular media, we are also saddened that “returning to normal” under economic and political pressure is so valued.
Treatments
Invyvid has received an FDA emergency use authorization for Pemgarda, a pre-exposure prophylaxis (PrEP) for people with immunocompromising conditions. Pemgarda is approved for people 12 and older with moderate to severe immunocompromise who are less likely to produce an adequate immune response to COVID vaccination alone. According to a press release from Invyvid, Pemgarda will release to market “imminently.”
Pre-exposure prophylaxis is commonly used for folks at high risk for exposure to HIV. As access to PrEP for HIV has been instrumental in keeping people safe, we hope that PrEP for COVID will be a useful tool for our community members with immune compromise. We also urge you to continue to wear high-quality masks and take other precautions to protect those most vulnerable.
Long COVID
People Magazine recently published an article highlighting an essay by Ziyad Al-Aly, physician and clinical epidemiologist, that pools data from several studies showing that COVID infection has lasting impacts on brain health. The review points out several impacts to cognitive functioning, including memory loss, spatial reasoning, and planning. Additionally, imaging studies have shown significant impact to brain tissue from inflammation, among other processes. The publication may be validating to those who experience lower cognitive function following COVID infection, including brain fog and memory dysfunction.
Take Action
We know that taking precautions–including masking, testing, and improving air quality–helps prevent the spread of airborne viral infection. Introducing more stringent precautions slowed outbreaks in the hematology ward of a hospital. The CDC recently released tips to improve ventilation. Help us urge the CDC to take other measures, including reinstating isolation periods.
Additionally, the home Test to Treat program is ending in April 2024. The program provides un-or-underinsured adults with free COVID and flu tests. If a participant in the program tests positive, they can also receive free healthcare via telehealth services. Join us to help save the program that helps so many at-risk people!
#op#covid#covid19#covid-19#covid 19#pcdc#people's cdc#long covid#covid pandemic#covid news#covid conscious#covid isn't over#pandemic#sars cov 2#coronavirus pandemic#coronavirus#sars-cov-2#cdc#prep#hiv#covid treatment#prep for covid#prep for covid-19#immunocompromised#disability#medical#uspol#img#links#described in alt text
2 notes
·
View notes
Text
It's World AIDS Day so I wanted to run through a couple quick points
HIV is treatable! There's been incredible advancements in the treatment of HIV in the last few decades. Life expectancy for those living with HIV is the same as someone without the virus if they are on treatment.
U=U: If you're on treatment and your viral load is undetectable, you cannot transmit HIV to your partners.
PrEP is widely available. If you belong to a group that has an increased incidence of HIV transmission, you should be able to access Pre-Exposure Prophylaxis. Essentially this is a combination of two medications that is highly effective at preventing transmission of HIV. In some countries (such as the UK), you can access PrEP for free, however you can also source PrEP online in over 100 countries.
Knowledge is power. Knowing your status helps ensure you can access treatment early and prevent transmission to others. And remember, anyone who is sexually active can get HIV. Get tested regularly if you can
Anyways lets continue to destigmatise HIV, reduce transmission, and get everyone who needs it on treatment
#world aids day#hiv#anyways just spent an afternoon giving out prep#and it's genuinely one of the most satisfying things to do#like a tablet you can take once a day and it gives you up to 99% protection against HIV?#thats an amazing advancement
23 notes
·
View notes
Text
A federal appeals court panel appeared skeptical on Tuesday of calls to impose a nationwide freeze on Obamacare’s rules for no-cost coverage of preventive care while litigation continues — a move the Biden administration warned would threaten access to a range of services for millions of people on employer-sponsored insurance and Obamacare’s individual market.
Both sides in the case agreed that the individual Texas businesses that sued over the mandate should be shielded from it while the case makes its way through the courts. But they split on whether more harm would be caused by keeping the current coverage rules intact for everyone else in the country or by suspending them nationwide.
Attorneys representing the Texas employers and individual workers challenging the policy argued that because
the United States Preventive Services Task Force is made up of outside experts who are not Senate-confirmed or overseen by Senate-confirmed government employees, their recommendations of what preventive services should be covered by insurance — from syphilis tests to depression screenings — must be “set aside” and can’t be enforced.
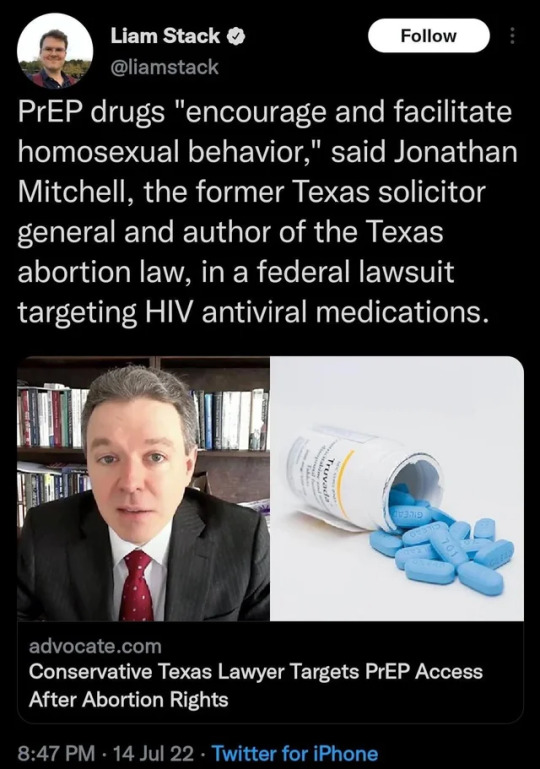
Their suit also claims the Obamacare requirement for insurance to cover the pre-exposure prophylaxis pill used to prevent transmission of HIV — known as PrEP — violates the religious rights of the challengers. In their legal briefs, they equated covering the highly effective medication with encouraging homosexuality and promiscuity.
The merits of those legal arguments didn’t come up in Tuesday’s hearing before the 5th U.S. Circuit Court of Appeals in New Orleans, which focused squarely on whether the nationwide freeze of the Obamacare mandate a lower court ordered in March went too far.
That ruling, Justice Department attorney Alisa Klein told the court, was a “legal error” that “extinguished the rights of about 150 million people who are not parties to the case.”
Klein urged the appeals court judges to consider the “balance of equities,” arguing that there would be no harm done to the already-protected plaintiffs by putting the nationwide injunction on hold, but great harm done to everyone else if they failed to do so.
“It can’t be overstated how important the guarantee of cost-free access is when patients go to get their mammograms and colonoscopies,” she said. “We’re talking about 50 different types of care.”
The attorney for the conservative challengers, Jonathan Mitchell, responded that the nationwide ruling was appropriate because “agency actions must be set aside if they are unlawful.”
Mitchell — the architect of the six-week abortion ban Texas imposed before Roe was overturned — attempted to reassure the judges that imposing a nationwide injunction wouldn’t cause harm because insurers are unlikely to drop coverage of preventive care services while the case is still in process.
The judges on the appeals court panel seemed unconvinced.
Leslie Southwick — an appointee of former President George W. Bush — called that assertion “speculative” and said it was “very unusual” to be asked to rule on “our sense of how insurance companies would react.”
“I’m not sure what we have to go on,” he said.
The judges also grilled Mitchell on whether a win for his side would solve his clients’ problem — a legal threshold known as “redressability.” When Mitchell argued that individual workers he represents who are refusing to buy insurance because of the PrEP coverage requirement would be able to get covered if the mandate were lifted, Judge Stephen Higginson noted that the workers’ own affidavits “don’t say that.”
Higginson — an appointee of former President Barack Obama — pointed out that only one of the four workers came anywhere close to making that claim, and that he expressed “a desire to buy insurance, not a specific intent.”
Mitchell acknowledged that there’s no “iron-clad guarantee” his clients would buy health insurance if courts blocked the Obamacare mandate.
In closing, the judges urged both him and the DOJ to try to broker a compromise that would more narrowly tailor the nationwide ruling without infringing on the rights of the plaintiffs.
Tuesday’s hearing was the latest in a months-long saga over the preventive care mandate that’s been in place for more than a decade.
Texas District Court Judge Reed O’Connor — the author of several rulings against pieces of Obamacare — issued a nationwide ruling in March for the challengers, striking down all of the decisions made by the United States Preventive Services Task Force since 2010 about what insurers must cover without cost sharing.
In May, the 5th Circuit Court issued an administrative stay of that lower court ruling — keeping the current coverage rules in place while the case proceeds.
Public health groups warn of serious consequences if O’Connor’s ruling is upheld — citing research showing that even small out-of-pocket costs deter many people from seeking preventive care, leading to sicker patients and more costly treatments. Medical experts are particularly worried that coverage rollbacks would exacerbate already record rates of sexually transmitted diseases by making testing and treatment services unaffordable for vulnerable populations.
Many major insurers have pledged to maintain preventive care at no cost to patients for the time being no matter what courts decide, but experts fear that patients could eventually be hit with out-of-pocket charges should the 5th Circuit and Supreme Court side with the challengers.
The case also throws more than two-dozen new recommendations the federal task force is currently weighing in jeopardy, rules that could expand coverage of everything from prenatal care to speech therapy to osteoporosis.
3 notes
·
View notes
Text
The ruling from U.S. District Judge Reed O'Connor focuses on claims from Braidwood Management, a Christian for-profit corporation owned by Steven Hotze, that its rights were violated by the mandate under the Religious Freedom Restoration Act.
At the center of the decision are pre-exposure prophylaxis drugs, or PrEP drugs, which research has showed these reduce the risk of contracting HIV from sex by about 99%. But Hotze, whose company provides health insurance to about 70 employees, argued that offering coverage for PrEP drugs encouraged "homosexual behavior" and violated "his religious beliefs by making him complicit in encouraging those behaviors."
The pro life party, everybody!
13 notes
·
View notes
Text
ICAP in Tajikistan Helps Catalyze Early Initiation of Lifesaving HIV Treatment for All

For people living with HIV, the chances of developing AIDS or another serious illness is considerably lower the sooner one begins antiretroviral treatment (ART). Additionally, a suppressed viral load helps prevent perinatal transmission of HIV and leads to less likelihood of HIV transmission to sexual partners.
With funding from the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC), ICAP in Tajikistan collaborated with the Republican AIDS Center and local partners to execute revisions to national guidelines outlining that people living with HIV should be initiated on ART within seven days of diagnosis.
Previously, national guidelines stated that ART prescription for an individual diagnosed with HIV could be anywhere from two to eight weeks. Several obstacles, including stigmatization of an HIV diagnosis and HIV-related health appointments, lack of diagnosis acceptance, and limited guidance for health care professionals prescribing ART, also impeded the process of getting people living with HIV the treatment they needed, and fast. In 2020, there were 9,500 people living with HIV in Tajikistan who knew their status and only 8,000 on ART.
“This new guideline will make a major difference in the health of people living with HIV and those at risk of acquiring the virus,” said Zumrad Maxumova, MD, PhD, ICAP national coordinator in Tajikistan. “Timely initiation of ART is critical to achieving viral suppression and is one of the main factors in ending the HIV epidemic globally.”
Updating national HIV guidelines can mean a small change with a major impact. Institutional and government support behind new HIV health facility procedures not only helps health care providers prioritize how to best address an individual’s health needs but signifies the value of addressing such areas as the HIV epidemic, which globally continues to bear stigmatization.
To ensure streamlined implementation of the new guidelines, every two weeks ICAP and health facility staff used patient data to evaluate the number of days between HIV diagnosis and ART initiation. Cases of delayed ART initiation were analyzed and discussed with facility staff to develop a performance improvement plan. To further motivate prompt initiation on ART for people living with HIV, ICAP in Tajikistan also introduced quarterly performance-based incentives to members of site-level clinical teams, including physicians, nurses, and peer consultants.
“ICAP also proposed to ensure introduction of lifelong ART for everyone, regardless of the number of CD4 [a measure of the strength of your immune system] cells, including children, adults, and pregnant and lactating women living with HIV,” added Maxumova.

From January to May 2022, a total of 296 new cases of HIV infection were detected at 45 PEPFAR-supported sites. Of these, 278 people living with HIV started ART within the newly recommended seven-day period.
As a result of ICAP’s support to help end the HIV epidemic in Tajikistan – including such efforts as development of national guidelines, site-level mentoring of providers to improve HIV testing and treatment, roll-out of pre-exposure prophylaxis (PrEP), and development of a confidential electronic HIV case management system – ICAP in Tajikistan was recently awarded a Certificate of Appreciation by the Ministry of Health at the country’s National HIV Forum. Nearly 100 people participated in the forum, including representatives of government agencies of Tajikistan, non-governmental organizations, grantors, and international partners such as the United Nations Development Programme (UNDP), UNAIDS, and CDC.
“ICAP and its partners have made a great deal of progress in addressing HIV in Tajikistan, but there is still a lot of work to be done,” said Anna Deryabina, MD, DrPH, MScIH, ICAP regional director in Central Asia. “ICAP in Tajikistan works to address HIV service quality improvement from all levels. This comprehensive approach is essential because it helps address the existing gaps and ensure sustainability of the quality improvement efforts. In the future, we hope to continue building capacity of local clinical teams to provide quality and patient-focused HIV services in order to achieve the UNAIDS 95-95-95 goals.”
https://icap.columbia.edu/news-events/icap-in-tajikistan-helps-catalyze-early-initiation-of-lifesaving-hiv-treatment-for-all/
6 notes
·
View notes
Link
U.S. District Judge Reed O'Connor in Fort Worth, Texas, previously found that the PrEP mandate violated a federal religious freedom law and that other no-cost preventive care mandates were based on recommendations by an illegally appointed task force.
The legal challenge was brought by eight individuals and two businesses, all from Texas. They argued that the free PrEP requirement requires business owners and consumers to pay for services that "encourage homosexual behavior, prostitution, sexual promiscuity and intravenous drug use" despite their religious beliefs.
FUN FACT:
None of the plaintiffs* have standing to sue.
The judge ** has no authority to rule.
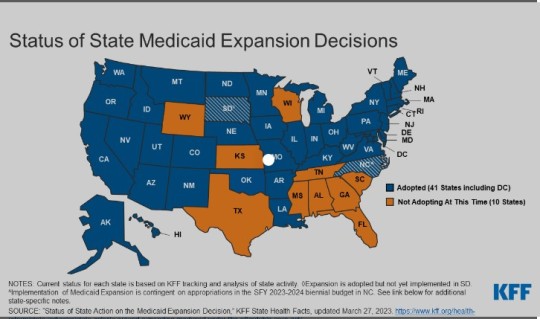
The Affordable Care Act mandates do not apply to states that have not adopted The Affordable Care Act or expanded Medicaid access.
* hate-filled theologically illiterate
** unqualified, emotionally deformed
2 notes
·
View notes
Note
First off, Sad Sack is my new religion. Second, in A.M.F., I noticed in one panel that Stone had some pill bottles on his seat, Macrobid for UTIs, I remembered reading he has those 24/7, but Isentress and Truvada…is he HIV positive? If so, how did he come around to having it?
THANK YOU LOL and good eye! he’s actually not HIV positive, those 2 HIV medications are also prescribed as post exposure prophylaxis (aka PEP) which he’d picked up from the pharmacy to prevent any possible HIV infection because he got so much of the vic’s blood on/in him & once he sobered up the next day he realized that he had no idea about the guy’s HIV status. stone keeps saying he’s gonna get on PrEP (pre exposure prophylaxis hehe) but never gets around to it. also there was so much slime involved during the happenings of A.M.F. that he got a uti near instantaneously LOL
on that note also if you folks out there are ever in a scenario where youre concerned about HIV exposure, talk to your doctor or go to urgent care immediately to get on PEP to prevent any infection!!!! the sooner you start it the better!!!!!!!!!!!
8 notes
·
View notes
Text
Pre-exposure prophylaxis (or PrEP) is medicine taken to prevent getting HIV.
__________
“The PrEP mandate forces religious employers to provide coverage for drugs that facilitate and encourage homosexual behavior, prostitution, sexual promiscuity, and intravenous drug use,” the lawsuit states. “It also compels religious employers and religious individuals who purchase health insurance to subsidize these behaviors as a condition of purchasing health insurance.”
95 notes
·
View notes