#but it DOES highlight the disparity that much more in a country where healthcare is tax paid and (supposedly) about patient needs
Text
me and my mum were listening to danish news about how rigshospitalet (basically the largest hospital in denmark) was cutting back on costs by no longer covering the costs of tattooing nipples on breast-cancer cis women patients who have had breast re-construction, which is paid by tax payer money/free on the hospital
and that's all a discussion about gender reaffirming care!
whether or not the nipple counts as "distressing enough" is a thing I won't get into (I am personally getting mine removed -- opposite gender affirming care!!! same-but-different) -- what is interesting here to me, is firstly that what is being argued -- the big fascinating hypocrisy at the centre -- is notably not whether or not cis women need to prove a significant amount of psychological distress by speaking to psychiatrists and jumping through segregated healthcare hoops
and yet in denmark trans people do have to do this in order to access care -- not to the same amount as in some countries (notably it is done at the hospitals, but as far as I'm aware it's only the two main hospitals in Denmark that offer it, and it's not legal to go private within the country), but that is still the process and was until not-so-many-years also including forced sterilisation
the idea that a cisgender woman might feel significant gender-based distress at not having breasts was not in question in the discussion my mum and I were listening to
the other thing that is interesting is that the person at the rigshospitalet who was arguing that the nipples was too much cost was a cis dude. and of course cis dudes can have breast-cancer, but I have a feeling this guy was not speaking from that kind of thinking + of course the weight of "being a woman who has breasts that look like people think breasts should look" is an issue that he would never have to deal with, and so there was indeed an example there of a doctor who was not taking cis women's dysphoria seriously and arguing a (partial) rolling back of care on this basis
to what extent do cis women have to contend with looking "enough" like a woman because of misogyny? to what extent can one argue the dysphoria they feel is an innate idea of the self that doesn't match with what they see? to what extent is it a reaction to a different traumatic event (the scars a reminder of having been sick)? to what extent is there a cultural disgust against scarring that ought to be unlearned?
I'd argue that for the particular question of whether they deserve the care right now, those questions aren't going to help. offer the care and we can dismantle harmful notions about "correct" womanhood next to it (putting the ball in the court of a far bigger sandpit of societal work we need to do), and at the same time be cognizant of how that hits trans women 100 times over just for existing and having to perform hyper-femininity or else it doesn't count but is also demonised for being a performance, and in a different-but-similar way hits anyone who is assigned female at birth who is trying to build a space of non-conformity and/or masculinity and being scrutinised for "always" being a female while also being masculine traitors (just look at responses to elliot page) (just look at butches regardless of AGAB full stop)
I am supportive of cis women (and cis men) receiving gender affirming care. now they need to be supportive of me and mine receiving the same
#sorry to all americans reading this post i know that healthcare just sucks full stop regardless of gender over there#so the idea of whether to get a breast reconstruction or not is a wild hypothetical in some places#but it DOES highlight the disparity that much more in a country where healthcare is tax paid and (supposedly) about patient needs#and there is an implicit understanding there of certain kinds of gender-based affirmations that doesn't extend across#but also this was a FASCINATING example of gender affirming care that i just had never thought about before#like never mind the nipple tattoos you're getting breasts for free???#that one meme#queer stuff#trans stuff#gender affirming healthcare#trans rights#womens rights#trans healthcare
23 notes
·
View notes
Text
Is Australia on track to eliminate cervical cancer?
Australia is aiming to officially eliminate cervical cancer by 2028, but more work needs to be done to bring Indigenous communities in line with that goal, according to a new report.
The NHMRC’s Centre of Research Excellence in Cervical Cancer Control has released a 2021 progress report, detailing Australia’s movement towards a target of fewer than four cervical cancer cases per 100,000 people. The report is being released at today’s Preventing Cervical Cancer conference.
The report is based on a global strategy by the World Health Organization (WHO) released in November 2020, outlining goals for screening and vaccinating against cervical cancer across the world by 2030.
According to Julia Brotherton, medical director of VCS Population Health and lead author of the report, the WHO strategy reflects advances in the last 15 years in HPV vaccinations and cervical screenings.
“HPV based screening methods [have] much better sensitivity and [provide] much better long-term protection to women, to the extent that even one or two tests in our lifetime can make a staggering difference to a woman’s risk of ever developing cervical cancer,” says Brotherton.
“Australia’s obviously been a world leader by being the first country to roll out a massive HPV vaccine program, and in our long-standing cervical screening program that’s been going since 1991.”
While the country is on track on a population-wide scale, there is a glaring disparity: Australian Indigenous women are dying from cervical cancer at four times the rate of other women.
Better data collection and advances in cervical screenings are likely to be key tools to closing this devastating gap.
One of the biggest challenges researchers have faced, according to Brotherton, is a lack of data to explain why Indigenous women have higher rates of cervical cancer.
“Having had a program for 30 years that couldn’t tell us if Indigenous women were participating but knew they were dying at higher rates is truly unacceptable,” she says. “It’s really well overdue that we are able to know what’s happening.”
Work is now being carried out with Indigenous people to gather this data more effectively. A recently published study from ANU, for instance, highlighted the cervical cancer disparity not just in Australia but around the world.
“Probably by the next report, we’ll be able to look at Indigenous participation nationally,” says Brotherton. “But it’s still in the development phase of consultation with Indigenous people, which is completely appropriate, as to how best that is reported.”
The next challenge is screening for and thus diagnosing cervical cancer.
“Screening is what we need to do to make elimination happen faster,” says Megan Smith, a senior research fellow with the Cancer Council.
“Vaccination’s doing well in Indigenous girls, and so that’s great news, but if we rely on that to get us to elimination in Indigenous women, we’re going to be waiting decades and then they’re going to be decades behind everybody else, which is completely unacceptable.”
She adds that “the only way we can change this is to increase participation in screening”.
Smith highlights that the uncomfortable cervical screening procedure – the speculum exam – is a major barrier to testing for Indigenous people.
“Many women find it unacceptable, but for Indigenous women there are just these extra layers around systemic racism, about feeling uncomfortable in healthcare settings, being in remote areas, perhaps not having access to a female provider or a provider that they trust,” she says.
Self-conducted screenings are a potential solution. Instead of the clinical speculum exam, people could instead take their own cervical swab or have a trusted nurse do it for them in a private setting. This option is already part of the Australian screening program but in a more limited way – women need to be over 30 and overdue for screenings before they’re offered a self-examination swab.
The swabs, very similar to the ones used in COVID-19 tests, look like long cotton tips, and Smith notes that pilot studies suggest that women find them easy to use.
“Certainly we’re not advocating that anybody take away the opportunity for women to have a doctor collect a sample if that’s what she prefers,” says Smith. “It’s all about offering choice. But these pilots really do demonstrate that if you provide women with the appropriate support that they do find it really easy to do, and that does of course mean you don’t need to be in a clinic.”
The tests are similar in accuracy to the traditional speculum exam.
“There is now strong evidence to show that it is just as good,” says Smith, but even if accuracy was reduced, a higher uptake of self-conducted exams would still be overall beneficial for public health.
So do we need to book in-person screenings at all? Could cervical screening tests come in the mail, like bowel cancer tests?
“It’s not impossible, but I think that’s not how we see our way forward in Australia,” says Smith. “We’ve seen trials doing that and they haven’t had nearly as good results.”
In-person healthcare providers form an important part of the cervical screening program, even if they’re not performing speculum exams. This is particularly important in Indigenous communities, where local understanding is critical to encourage people to get vaccinations and screenings. “I think what we’ll see will be tailoring the self-collection to individual communities,” says Smith. They’re also needed for following up with people who receive a positive result on their test.
With other initiatives outlined in the report, it could be possible for Australia to reach the official target of four cervical cancer cases per 100,000 people by the end of the decade.
Brotherton says the official elimination target is based on what the WHO believes to be possible.
“The definition of a rare cancer is usually less than six per 100,000 cases,” she says. Cervical cancer could become slightly less common than that, though it would be impossible to eradicate it entirely.
“Some rare types of cervical cancer are not caused by HPV, and may not be screen detectable,” Brotherton says.
“My understanding is that it’s a feasible, agreed goal.”
See more:
Cancer risk for First Nations women
Elizabeth Stern, women’s health pioneer
Human papilloma virus: a gift from the Neanderthals
Is Australia on track to eliminate cervical cancer? published first on https://triviaqaweb.weebly.com/
0 notes
Text
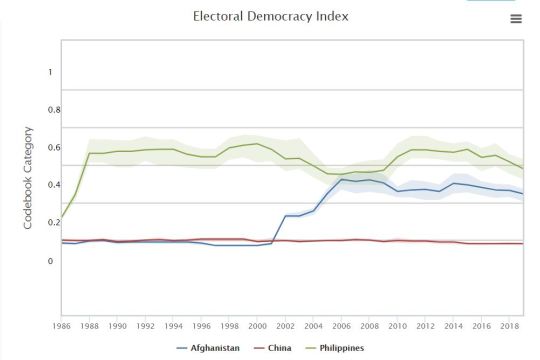
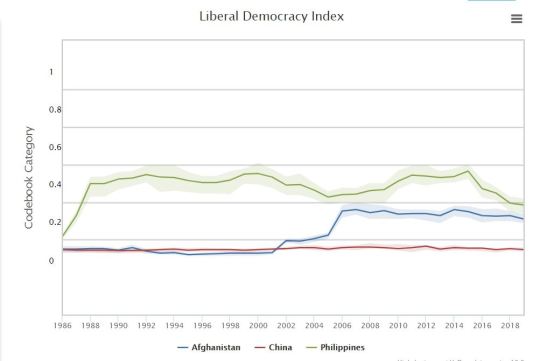
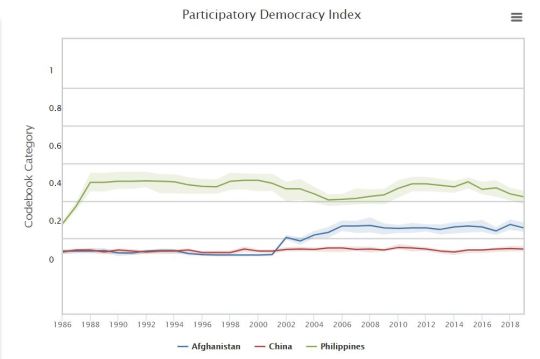
V-Dem Democracy Report
“Democracy is the rule of the people” and as it should. This is considered to be one of the most known and utilized system of government in which is formed through a voting system of certain representatives elected by the country’s common people. For this blog, the 5 principles of approaching democracy will be mainly discussed. Data collected between Afghanistan, China, and the Philippines will also be compared as to depict the difference of being democratic between a less developed country, the most developed one, and our very own country.
1. Electoral
This is considered to be the main essence of democracy in which highlights the importance of relationship and agreements between elected representatives and the citizens especially during elections where competency for obtaining votes is very much observed.
2. Liberal
Although, the Majority Rule is commonly practiced during electoral periods, this is now being limited through a liberal approach in which primarily focuses on protecting individuals and minority rights as to avoid the rise of tyranny among the system. This is done through the establishment of such rule of law and fair distributions of power.
3. Participatory
As mentioned earlier, “democracy is the rule of the people”, hence greatly values the constant participation of the citizens and their exertion of power in every political procedures. Such participation does not only mean during elections but also in political operations such as in addressing social issues present in the community or in the country as a whole.
4. Deliberative
This approach deeply values the importance of political decisions in circumstances where such coercion or emotional appeals cannot be simply recognized as settlements. Such claims during the deliberative discussion between the citizens should be for the society’s sake and must be substantial as logical reasonings and arguments must be presented.

5. Egalitarian
A democratic approach in which primarily values one’s rights especially their access to resources such as clean water, education, and healthcare. This approach includes ensuring the state of being equal between social classes with regards to treatments and the fair distribution of materialistic goods

Democracy in Afghanistan, China, and Philippines
In Afghanistan, democracy and a new system of government has been established in 2001 as a result of the civilian war against the Taliban government which lasted for 9 years. Though this has become a phrase in which the country struggled with as conflicts and terrorism, such as the 9/11 terrorist attack in United States, arise. It is the year 2004 in which Afghanistan started to adapt to a more democratic approach in which it is believed when political participatory had greatly risen as Afghanistan women were granted the right to vote. China, on the other hand, have continuously been a communist country over the past 70+ years. Though despite being a non-democratic system, China is very much known to be -- if not the most -- one of the fastest and largest developing country. It is believed that is due to the “wide range of indicators such as per capita levels, industrial structure, employment, innovation ability and balance of development, among others“ (”China’s status as developing country undeniable
“). And lastly, Philippines has continuously been a democratic country ever since the fall of the late president Marcos’ Martial Law. Though there are still conflicts being reflected in the system, including the presence of social class disparity and extrajudicial killings such as in Gloria Arroyo’s administration (2001-2010) and the current Duterte administration (2016-).
References
Coppedge, M. Lindberg, S. Skaaning, S. Teorell, J. (2005). Measuring high level democratic principles using the V-Dem data. International Political Science Review. https://journals.sagepub.com/doi/abs/10.1177/0192512115622046
Eagan, J. (n.d.). Deliberative democracy. Encyclopædia Britannica. https://www.britannica.com/topic/deliberative-democracy.
Haidary, M. S. (2018, August 15). By the Numbers: Is Afghanistan's Democracy at Risk? The Asia Foundation. https://asiafoundation.org/2018/08/15/by-the-numbers-is-afghanistans-democracy-at-risk/.
Struggle for democracy. (n.d.). Encyclopædia Britannica. https://www.britannica.com/place/Afghanistan/Struggle-for-democracy.
China's status as developing country undeniable. (2019, December 11). Global Times. https://www.globaltimes.cn/content/1173184.shtml#:~:text=China%20remains%20the%20largest%20developing,balance%20of%20development%2C%20among%20others.
What is Participatory Citizen. (n.d.). IGI Global. https://www.igi-global.com/dictionary/participatory-citizen/55423.
0 notes
Text
Femtech poised for growth beyond fertility
The market for female-focused health products (aka ‘femtech’) is set for growth via segmentation, per an analyst note from PitchBook which identifies opportunities for entrepreneurs to target a growing number of health issues that specifically affect women or affect women in a specific way — broadening out from a traditional focus on reproductive health.
Femtech remains a “significantly underdeveloped” slice of healthtech, according to the analysis, which highlights the disparity between how much women spend annually on medical expenses — estimated at ~$500BN — vs how little healthcare R&D is targeted specifically at women’s health issues (a mere 4%).
Last year the global market for female-focused health products generated $820.6M, per the note, and is estimated to reach at least $3BN by the end of 2030. While it says femtech posted $592.1M in VC investment in 2019, slightly down on 2018’s $620.3M. But so far this year it’s racked up $376.2M in VC across 57 deals — putting it on pace to match 2019’s funding levels.
Areas of growth opportunity PitchBook sees for femtech outside its traditional focus on reproductive health are: Endometriosis, a painful disorder of the womb lining affecting one in 10 women; what it calls “personalized and female-oriented approaches to general health & disease management”, with a specific focus on heart health, pain management, and diabetes and weight management within that; and the life-stage transition of the menopause.
“While we still view femtech as a niche industry, we believe secular drivers could help propel new growth opportunities in the space,” write analysts Kaia Colban and Andrew Akers. “These include the increasing representation of women in the venture-backed technology community, rising awareness and acceptance of women’s health issues, and the growing prevalence of infectious diseases among women in some countries in Africa and Asia.
“Furthermore, while the majority of femtech products have traditionally focused on reproductive health, we believe new approaches to women’s health research will help open the door to new products and services.”
Expansion of the vertical is being driven by universal growth of the personalized medicine industry — which PitchBook notes is expected to reach $3.2TR by 2025, registering a CAGR of 10.6% over the forecast period.
While the massive underrepresentation of women in the venture community goes a long way to explaining the relative lack of attention investors have paid to products addressing women’s health — with the note acknowledging pitching to male investors remains a challenge for femtech startups — it suggests investors have also been cool on the subcategory because of a relatively poor track record of “sizable” exits.
“Only six femtech exits were completed in 2019; however, this still represents a 64% increase in exit value compared to 2018,” it writes. “The largest exits in recent years include Progyny’s $130M IPO and Procter & Gamble’s acquisition of This is L. for $100M. Progyny’s stock has roughly doubled in the eight months since it went public.”
PitchBook says it expects just 14% of VC to go toward female-founded startups this year — further noting that only 17% of startups have at least one female founder. (For femtech startups the figure is considerably higher — yet still only 69% of those PitchBook tracks; NB, this does not include startups building products targeted at women where there isn’t a medical need, such as skincare & beauty etc.)
“However, we believe these barriers may be subsiding as male investors begin to recognize the femtech market opportunity and as the VC world becomes more gender-diverse,” it adds, noting that female-founded companies deliver over twice as much per dollar invested than their male-owned counterparts which it reckons could help to turn more investors’ heads.
Other key industry growth drivers the note points to are a conducive regulatory environment; a rise in preventative medicine & holistic health; and advancements in health technology that have made personalized products more accessible and affordable, such as AI and “cloud-based infomatics”.
On the M&A front, PitchBook notes this is most common for femtech startups in the general health & wellness category. And while most remain single-product companies it says it expects a maturing femtech industry to lead to product diversification — “potentially driven by M&A” — noting recent examples of pregnancy-focused apps tapping into the menopause market, which it says suggests an expanding opportunity for fertility startups.
0 notes
Text
Buried in “Hilariously Stupid” White House Attack on Socialism, An Accidentally Strong Argument for Medicare for All
This is Naked Capitalism fundraising week. 1540 donors have already invested in our efforts to combat corruption and predatory conduct, particularly in the financial realm. Please join us and participate via our donation page, which shows how to give via check, credit card, debit card, or PayPal. Read about why we’re doing this fundraiser and what we’ve accomplished in the last year, and our current goal, more original reporting
Yves here. It appears Republicans have noticed how popular socialism is with the young and felt compelled to Do Something about that, in the form of a 72 page soi disant report by the Council of Economic Advisers on the “Opportunity Costs of Socialism”. Apparently no one told them that Basque region of Spain, dominated by the worker-owned Mongragon, which has strict curbs on executive pay, had the lowest post-crisis level of unemployment in the country.
Even this post, however, misses the idea that there are different types of property rights, even with supposedly private property, as Jerri-Lynn’s discussion of the “right to repair” illustrates. Sandwichman at Econospeak made a similar point by hoisting this matrix from Elinor Olstrom:
By Jake Johnson, staff writer at Common Dreams. Originally published at Common Dreams
From its heavy-handed comparisons between mild-mannered democratic socialist Sen. Bernie Sanders and militant communist revolutionary Mao Zedong to its bizarre assertion that the Scandinavian economic model is a failure due to the high weekly costs of owning a pickup truck in Finland and Sweden (seriously), a White House attack on socialism was roundly mocked almost as soon as it was released on Monday, with informed critics arguing that the report reads as if it was plagiarized from a college freshmanwith a serious Ayn Rand obsession.
Titled “The Opportunity Costs of Socialism,” the Council of Economic Advisers’ (CEA) new 72-page paperpurports to offer an empirical analysis of socialist policies—but what it actually does is make what analysts described as “hilariously stupid” and “intellectually embarrassing” claims accompanied by charts and footnotes that give off the appearance of scholarly diligence.
Characterizing the CEA’s report as a “truly bizarre document,” Vox‘s Dylan Matthews notes that the paper’s bibliography contains “a mix of books about mass atrocities in Communist regimes, economics papers on the distortionary effects of taxation, and works by socialists, like the essay Voxpublished by Jacobin staff writer Meagan Day defending democratic socialism.”
But a look beyond the CEA’s hysterical rants against socialism’s supposedly totalitarian nature reveals that the White House accidentally makes a strong case for Medicare for All, which the paper describes as the “headline American socialist proposal.”
After attempting to discredit single-payer healthcare programs—which multiple polls now show most Republicanvoters support—as “similar in spirit to Lenin and Mao,” the CEA produced a chart showing short wait times for seniors under the current U.S. healthcare system compared to those under the Canadian and Nordic systems.
As Vox‘s Sarah Kliff notes, the CEA conveniently omits the fact that “America’s seniors are essentially in a single-payer system”: it’s called Medicare.
“The Trump chart doesn’t say what the White House seems to think it says,” Kliff concludes. “It isn’t telling us that single-payer healthcare has long wait times. If anything, it says that it is possible to build a single-payer system with short wait times—and our Medicare program has already done it.”
So, um, a new @WhiteHouseCEA report ostensibly written to argue against Medicare for All uses… the success of Medicare (!) to argue against it. https://t.co/irnkIlNzbh pic.twitter.com/RhndXzAHzE
— Steve Goldstein (@MKTWgoldstein) October 23, 2018
In a tweet, Sanders offered Trump his congratulations for making such a good argument in favor of Medicare for All:
Congratulations to Donald Trump for unintentionally making the case for Medicare for All. https://t.co/De09BEVq2s
— Bernie Sanders (@SenSanders) October 23, 2018
The CEA’s Medicare for All faceplant was just one of many ludicrous components of the White House’s latest effort to ratchet up fear of the coming socialist menaceahead of next month’s midterm elections. According to recent survey data, a growing number of American voters prefer socialism to capitalism—hardly a surprising finding, given that just five men own almost as much wealth as half the world’s population and tens of millions of Americans are just one emergency away from economic peril.
In a Twitter thread, Public Citizen highlighted a couple more of the report’s egregious lies:
Here’s one embarrassing claim from the report: Restraining drug prices will lower life expectancy. Yes, that’s right – in the country where 1 in 6 ration drugs because of price – they argue that restraining price gouging would cost lives. 5/
— Public Citizen (@Public_Citizen) October 23, 2018
The report is dead wrong on the cost of Medicare for All. Medicare for All is MORE efficient than wasteful private insurers. We would spend the same or less on health care while providing better treatment to all. 6/
— Public Citizen (@Public_Citizen) October 23, 2018
The report twists and turns to claim that US health care is superior. But we do worse than other rich nations on infant mortality, access to care, lifespan, overall health and quality. Private insurance makes things worse in each dimension. 7/
— Public Citizen (@Public_Citizen) October 23, 2018
But as the left-wing magazine CurrentAffairs pointed out on Twitter, no detailed breakdown is necessary to recognize that the CEA’s paper is total bunk.
“The White House paper on socialism can be dismissed in a sentence: it defines socialism as state ownership rather than worker control, and therefore does not have anything to say about socialism,” the publication noted. “Sorry that you wasted 72 pages and a bunch of hours, White House CEA.”
This entry was posted in Free markets and their discontents, Guest Post, Income disparity, Politics, Social policy, Social values, The dismal science on October 24, 2018 by Yves Smith.
Post navigation
← Brexit: The Forward March of Remain? It Still Hasn’t Got Out of the Starting Blocks Standoff Between Italy and European Commission Escalates as Commission Rejects Italian Budget →
Source: https://www.nakedcapitalism.com/2018/10/buried-hilariously-stupid-white-house-attack-socialism-accidentally-strong-argument-medicare.html

0 notes
Text
Testing In California Still A Frustrating Patchwork Of Haves And Have-Nots
Months into the spread of the coronavirus in the United States, widespread diagnostic testing still isn’t available, and California offers a sobering view of the dysfunction blocking the way.
It’s hard to overstate how uneven the access to critical test kits remains in the nation’s largest state. Even as some Southern California counties are opening drive-thru sites to make testing available to any resident who wants it, a rural northern county is testing raw sewage to determine whether the coronavirus has infiltrated its communities.
County to county, city to city — even hospital to hospital within a city — testing capacity varies widely, as does the definition of who qualifies for testing.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Testing deserts, stemming from an overwhelmed supply chain and a disjointed public health system, have hit hardest in California’s rural north and in lower-income urban neighborhoods with concentrations of residents who already were struggling to get quality medical care. In the absence of a coordinated federal response, local health departments, hospitals and commercial labs across the state have been competing for the same scarce materials. Whether they are “haves” — or have-nots — is determined largely by how deep their pockets are, their connections to suppliers and how the state is allocating emergency supplies.
Compounding these problems is the lack of a state or federal public health infrastructure empowered to acquire and allocate resources on a grand and equitable scale. Hospitals and health systems where many people go for care are, by design, set up to focus resources on their own patients and workers. Their bureaucracies can’t readily adapt to do the community outreach and education that could bring testing to the masses; nor are they set up to do the contact tracing that ensures that people who have been exposed to COVID-19 patients are tested and monitored.
Those roles typically fall to county health departments, which in much of California operate on bare-bones budgets that make it a struggle to contain perennial STD outbreaks, let alone a deadly pandemic.
Over the past two months, the state has triaged one testing disaster after another, but it is finally making headway on making tests more widely available, in part by cutting its own deals for supplies and expanding testing sites in underserved areas, said Dr. Bob Kocher, one of three people on a testing task force convened by California Gov. Gavin Newsom.
But conversations with dozens of local health officials, hospital systems, scientists and elected officials reveal just how complicated a task it will be.
Take Lake County, a recreational mecca just over two hours north of San Francisco. With 65,000 residents, it has had so few testing supplies that officials have resorted to buying swabs on Amazon and pilfering chlamydia testing kits for swabs and the liquid used to transport specimens to labs. Through what the county has cobbled together, it has identified six cases of COVID-19, all found via nurses or volunteers who have gone out looking for patients. “We’re basically having to do tea leaves to figure out what’s going on,” said Dr. Gary Pace, the county’s health officer.
He knows the county has community transmission, both from the cases they’ve identified and because they’ve started running tests on raw sewage to check for the COVID-19 virus; samples from four treatment plants have come back positive. “It is a way to just get more information because we can’t do testing,” he said. Unlike the diagnostic kits — which make use of supplies every health department in the country is competing for — the sewage sampling is done pro bono by a technology startup.
While announcing an ambitious program to increase testing last week, Newsom highlighted the rural-urban divide. “One of the big struggles we have had in the last few weeks of this pandemic is getting to rural and remote parts of this state and getting up testing sites and making them available,” he said.
Newsom is promising to dramatically increase the level of coronavirus testing, with a focus on rural towns and communities of color. California currently tests about 25,000 people a day but has a strategy to raise that to 60,000 to 80,000 per day. The state has opened the first of 86 pop-up testing sites targeted for areas in need. It is launching a program to train 10,000 workers to serve as temporary disease investigators who can do the contact tracing considered fundamental in stemming the spread of the virus.
Pace said he wrote the governor to ask for one of the pop-up sites. “Statewide, there’s a situation where there’s not enough testing, and if you’re trying to demonstrate progress, the way you do that is numbers,” he said. “We are interested in equity, though, and in my view, we need some horizontal coverage instead of just lots of numbers.”
In Mendocino County, situated along California’s rugged North Coast, officials expressed similar frustration. In late April, a health center on the Round Valley Indian Reservation got a rapid test machine made by Abbott Laboratories, distributed via the Indian Health Service. That same day, a tribal member came in feeling sick. That person tested positive for COVID-19, as did five family members. The county previously had identified just five cases, all linked to travel.
Dr. Noemi Doohan, the Mendocino County public health officer, fears a broader outbreak among the six tribes who live on the reservation. The state since has provided 2,000 test kits for people who live or work around the reservation. Doohan’s office will have to hire couriers to drive 2½ hours to a public lab in Sonoma County, which also has limited supplies, to get them processed.
It’s Every Lab — And County — For Itself
A mix of commercial and public labs are responsible for testing in California, and supply chain limitations have plagued them all. But those with deeper pockets and stronger commercial relationships have been out-competing counties and public labs with limited resources.
Rural Tulare County, spanning the peaks and foothills of the Sierra Nevada, is home to half a million people. It also has one of the highest per capita death counts of COVID-19 in California. Until recently, the local public lab was the only place in the county that could test for the disease. After borrowing staff from another county, buying additional machines, and suspending testing for most other diseases, they are now able to process 85 tests a day. Officials also can send specimens to commercial labs in other parts of the state, but say days-long turnarounds create bottlenecks for tracking patients and finding contacts.
Monterey County, in the heart of the state’s “salad bowl” coastal farming region, has relied on donations — and horse-trading — to meet demand. A local hospital found the expensive materials needed to make a missing reagent and mixed a batch for the public lab, said lab director Donna Ferguson. The hospital also gave the county 1,000 swabs, which Ferguson used to barter with Riverside County for extraction kits.
And through the kindness of strangers, she found a stopgap for limits on another important resource: lab workers.
During an interview with a local public radio station in March, Ferguson mused that if one of the three microbiologists working in her lab got sick, it could be disastrous for the county’s ability to process tests. The next day, she got a call from a graduate student at Stanford’s nearby Hopkins Marine Station. He’d heard the interview. Could he and his colleagues help? The crew of six graduate students from three universities has been volunteering at the lab since, tripling its capacity to 120 tests a day.
Though the supply chain is a concern for labs of all sizes, manufacturers appear to be prioritizing orders from commercial labs and big health systems over public health labs, said Eric Blanks, chief program officer for the Association of Public Health Laboratories, which represents most of the labs run by public health departments in the nation.
Quest Diagnostics, the medical testing giant headquartered in New Jersey, is running 350,000 coronavirus tests a week in its facilities around the nation. But it is being inundated with samples from across the country, and even as it has worked to ease backlogs, counties and private hospitals are waiting days for results.
Kaiser Permanente says it can test 2,000 to 2,500 people throughout the state each week. Sutter Health, a major provider in Northern California, tests around 650 people each day across its hospitals. CommonSpirit Health, which includes Dignity Health hospitals, says it could process 50,000 samples a week if it had to. As of last week, Stanford had run more than 20,000 tests for Bay Area residents. (Kaiser Health News, which produces California Healthline, is not affiliated with Kaiser Permanente.)
But even the giants don’t have unlimited supplies. “It really is the manufacturing lines. They’re the ones that right now are the limiting factor,” said Karen Smith, system vice president of laboratory services at CommonSpirit Health.
Moreover, hospitals are not set up to solve the broader issue of statewide disparities in access. They can generally handle the patients sick enough to seek out their ERs. But it hasn’t historically been their role to arrange community-wide supplies and testing.
“You’re not going to go to an emergency room if you’re asymptomatic. That’s the last place in the world you want to be right now,” said Dr. Omid Bakhtar, medical director for outreach laboratory services at Sharp HealthCare in San Diego. “It’s frustrating for me. I have the ability to do more [specimens], but how do I get them?”
Tests But No Takers
In pockets around the state, some counties have been able to stabilize their flow of supplies, in some cases because they have more financial means, in others because of their relationships with major hospital systems and research institutions.
With more confidence in their supply chains, Los Angeles and Riverside counties say they are ready to offer testing to any resident. Several other counties, including much of the Bay Area, are asking more people, including workers deemed essential without COVID symptoms, to get tested.
But some counties that have managed to ramp up testing are wrestling with yet another problem: not enough people to test. The reasons are twofold. After weeks of being told they shouldn’t go for testing because of shortages, the public seems to be adhering to that message even now that more testing is available. And the public health workforce tasked with locating those in need of testing is depleted.
San Francisco can test 4,300 people each day in its publicly supported labs but was receiving just 500 samples a day as of late April. Los Angeles is testing roughly 10,000 people daily but says it needs to double that to lift the shelter-in-place orders. Its focus in coming weeks is to increase testing among the uninsured and those in at-risk living environments such as homeless encampments and skilled nursing facilities.
Health officials say part of the challenge is they aren’t getting the word out to poorer residents and communities of color, even as those same groups are being hit harder by the virus in many cities. In San Francisco, for example, Latino residents make up 16% of the population but 25% of COVID-19 cases. In Los Angeles, black people are 9% of the county’s population but represent 15% of the deaths from COVID-19 for which race and ethnicity data is available.
Kocher, of the state testing task force, acknowledged the state has more work to do. But, he argued, there’s also a sufficient amount of testing capability available today, especially via high-capacity commercial labs where the state says the vast majority of specimens should be processed.
“Right now, we’re concerned with not having enough samples collected,” he said.
When officials do slowly begin to let people return to work and school, experts agree that cases will go up, creating even more need for labs, testing and contact tracers. Preparing for that future will require even more resources.
“We need money,” said Santa Barbara County Health Officer Dr. Henning Ansorg. “Lots of money. Lots and lots of it.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation.
Testing In California Still A Frustrating Patchwork Of Haves And Have-Nots published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
Testing In California Still A Frustrating Patchwork Of Haves And Have-Nots
Months into the spread of the coronavirus in the United States, widespread diagnostic testing still isn’t available, and California offers a sobering view of the dysfunction blocking the way.
It’s hard to overstate how uneven the access to critical test kits remains in the nation’s largest state. Even as some Southern California counties are opening drive-thru sites to make testing available to any resident who wants it, a rural northern county is testing raw sewage to determine whether the coronavirus has infiltrated its communities.
County to county, city to city — even hospital to hospital within a city — testing capacity varies widely, as does the definition of who qualifies for testing.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Testing deserts, stemming from an overwhelmed supply chain and a disjointed public health system, have hit hardest in California’s rural north and in lower-income urban neighborhoods with concentrations of residents who already were struggling to get quality medical care. In the absence of a coordinated federal response, local health departments, hospitals and commercial labs across the state have been competing for the same scarce materials. Whether they are “haves” — or have-nots — is determined largely by how deep their pockets are, their connections to suppliers and how the state is allocating emergency supplies.
Compounding these problems is the lack of a state or federal public health infrastructure empowered to acquire and allocate resources on a grand and equitable scale. Hospitals and health systems where many people go for care are, by design, set up to focus resources on their own patients and workers. Their bureaucracies can’t readily adapt to do the community outreach and education that could bring testing to the masses; nor are they set up to do the contact tracing that ensures that people who have been exposed to COVID-19 patients are tested and monitored.
Those roles typically fall to county health departments, which in much of California operate on bare-bones budgets that make it a struggle to contain perennial STD outbreaks, let alone a deadly pandemic.
Over the past two months, the state has triaged one testing disaster after another, but it is finally making headway on making tests more widely available, in part by cutting its own deals for supplies and expanding testing sites in underserved areas, said Dr. Bob Kocher, one of three people on a testing task force convened by California Gov. Gavin Newsom.
But conversations with dozens of local health officials, hospital systems, scientists and elected officials reveal just how complicated a task it will be.
Take Lake County, a recreational mecca just over two hours north of San Francisco. With 65,000 residents, it has had so few testing supplies that officials have resorted to buying swabs on Amazon and pilfering chlamydia testing kits for swabs and the liquid used to transport specimens to labs. Through what the county has cobbled together, it has identified six cases of COVID-19, all found via nurses or volunteers who have gone out looking for patients. “We’re basically having to do tea leaves to figure out what’s going on,” said Dr. Gary Pace, the county’s health officer.
He knows the county has community transmission, both from the cases they’ve identified and because they’ve started running tests on raw sewage to check for the COVID-19 virus; samples from four treatment plants have come back positive. “It is a way to just get more information because we can’t do testing,” he said. Unlike the diagnostic kits — which make use of supplies every health department in the country is competing for — the sewage sampling is done pro bono by a technology startup.
While announcing an ambitious program to increase testing last week, Newsom highlighted the rural-urban divide. “One of the big struggles we have had in the last few weeks of this pandemic is getting to rural and remote parts of this state and getting up testing sites and making them available,” he said.
Newsom is promising to dramatically increase the level of coronavirus testing, with a focus on rural towns and communities of color. California currently tests about 25,000 people a day but has a strategy to raise that to 60,000 to 80,000 per day. The state has opened the first of 86 pop-up testing sites targeted for areas in need. It is launching a program to train 10,000 workers to serve as temporary disease investigators who can do the contact tracing considered fundamental in stemming the spread of the virus.
Pace said he wrote the governor to ask for one of the pop-up sites. “Statewide, there’s a situation where there’s not enough testing, and if you’re trying to demonstrate progress, the way you do that is numbers,” he said. “We are interested in equity, though, and in my view, we need some horizontal coverage instead of just lots of numbers.”
In Mendocino County, situated along California’s rugged North Coast, officials expressed similar frustration. In late April, a health center on the Round Valley Indian Reservation got a rapid test machine made by Abbott Laboratories, distributed via the Indian Health Service. That same day, a tribal member came in feeling sick. That person tested positive for COVID-19, as did five family members. The county previously had identified just five cases, all linked to travel.
Dr. Noemi Doohan, the Mendocino County public health officer, fears a broader outbreak among the six tribes who live on the reservation. The state since has provided 2,000 test kits for people who live or work around the reservation. Doohan’s office will have to hire couriers to drive 2½ hours to a public lab in Sonoma County, which also has limited supplies, to get them processed.
It’s Every Lab — And County — For Itself
A mix of commercial and public labs are responsible for testing in California, and supply chain limitations have plagued them all. But those with deeper pockets and stronger commercial relationships have been out-competing counties and public labs with limited resources.
Rural Tulare County, spanning the peaks and foothills of the Sierra Nevada, is home to half a million people. It also has one of the highest per capita death counts of COVID-19 in California. Until recently, the local public lab was the only place in the county that could test for the disease. After borrowing staff from another county, buying additional machines, and suspending testing for most other diseases, they are now able to process 85 tests a day. Officials also can send specimens to commercial labs in other parts of the state, but say days-long turnarounds create bottlenecks for tracking patients and finding contacts.
Monterey County, in the heart of the state’s “salad bowl” coastal farming region, has relied on donations — and horse-trading — to meet demand. A local hospital found the expensive materials needed to make a missing reagent and mixed a batch for the public lab, said lab director Donna Ferguson. The hospital also gave the county 1,000 swabs, which Ferguson used to barter with Riverside County for extraction kits.
And through the kindness of strangers, she found a stopgap for limits on another important resource: lab workers.
During an interview with a local public radio station in March, Ferguson mused that if one of the three microbiologists working in her lab got sick, it could be disastrous for the county’s ability to process tests. The next day, she got a call from a graduate student at Stanford’s nearby Hopkins Marine Station. He’d heard the interview. Could he and his colleagues help? The crew of six graduate students from three universities has been volunteering at the lab since, tripling its capacity to 120 tests a day.
Though the supply chain is a concern for labs of all sizes, manufacturers appear to be prioritizing orders from commercial labs and big health systems over public health labs, said Eric Blanks, chief program officer for the Association of Public Health Laboratories, which represents most of the labs run by public health departments in the nation.
Quest Diagnostics, the medical testing giant headquartered in New Jersey, is running 350,000 coronavirus tests a week in its facilities around the nation. But it is being inundated with samples from across the country, and even as it has worked to ease backlogs, counties and private hospitals are waiting days for results.
Kaiser Permanente says it can test 2,000 to 2,500 people throughout the state each week. Sutter Health, a major provider in Northern California, tests around 650 people each day across its hospitals. CommonSpirit Health, which includes Dignity Health hospitals, says it could process 50,000 samples a week if it had to. As of last week, Stanford had run more than 20,000 tests for Bay Area residents. (Kaiser Health News, which produces California Healthline, is not affiliated with Kaiser Permanente.)
But even the giants don’t have unlimited supplies. “It really is the manufacturing lines. They’re the ones that right now are the limiting factor,” said Karen Smith, system vice president of laboratory services at CommonSpirit Health.
Moreover, hospitals are not set up to solve the broader issue of statewide disparities in access. They can generally handle the patients sick enough to seek out their ERs. But it hasn’t historically been their role to arrange community-wide supplies and testing.
“You’re not going to go to an emergency room if you’re asymptomatic. That’s the last place in the world you want to be right now,” said Dr. Omid Bakhtar, medical director for outreach laboratory services at Sharp HealthCare in San Diego. “It’s frustrating for me. I have the ability to do more [specimens], but how do I get them?”
Tests But No Takers
In pockets around the state, some counties have been able to stabilize their flow of supplies, in some cases because they have more financial means, in others because of their relationships with major hospital systems and research institutions.
With more confidence in their supply chains, Los Angeles and Riverside counties say they are ready to offer testing to any resident. Several other counties, including much of the Bay Area, are asking more people, including workers deemed essential without COVID symptoms, to get tested.
But some counties that have managed to ramp up testing are wrestling with yet another problem: not enough people to test. The reasons are twofold. After weeks of being told they shouldn’t go for testing because of shortages, the public seems to be adhering to that message even now that more testing is available. And the public health workforce tasked with locating those in need of testing is depleted.
San Francisco can test 4,300 people each day in its publicly supported labs but was receiving just 500 samples a day as of late April. Los Angeles is testing roughly 10,000 people daily but says it needs to double that to lift the shelter-in-place orders. Its focus in coming weeks is to increase testing among the uninsured and those in at-risk living environments such as homeless encampments and skilled nursing facilities.
Health officials say part of the challenge is they aren’t getting the word out to poorer residents and communities of color, even as those same groups are being hit harder by the virus in many cities. In San Francisco, for example, Latino residents make up 16% of the population but 25% of COVID-19 cases. In Los Angeles, black people are 9% of the county’s population but represent 15% of the deaths from COVID-19 for which race and ethnicity data is available.
Kocher, of the state testing task force, acknowledged the state has more work to do. But, he argued, there’s also a sufficient amount of testing capability available today, especially via high-capacity commercial labs where the state says the vast majority of specimens should be processed.
“Right now, we’re concerned with not having enough samples collected,” he said.
When officials do slowly begin to let people return to work and school, experts agree that cases will go up, creating even more need for labs, testing and contact tracers. Preparing for that future will require even more resources.
“We need money,” said Santa Barbara County Health Officer Dr. Henning Ansorg. “Lots of money. Lots and lots of it.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation.
from Updates By Dina https://khn.org/news/testing-in-california-still-a-frustrating-patchwork-of-haves-and-have-nots/
0 notes
Text
Testing In California Still A Frustrating Patchwork Of Haves And Have-Nots
Months into the spread of the coronavirus in the United States, widespread diagnostic testing still isn’t available, and California offers a sobering view of the dysfunction blocking the way.
It’s hard to overstate how uneven the access to critical test kits remains in the nation’s largest state. Even as some Southern California counties are opening drive-thru sites to make testing available to any resident who wants it, a rural northern county is testing raw sewage to determine whether the coronavirus has infiltrated its communities.
County to county, city to city — even hospital to hospital within a city — testing capacity varies widely, as does the definition of who qualifies for testing.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Testing deserts, stemming from an overwhelmed supply chain and a disjointed public health system, have hit hardest in California’s rural north and in lower-income urban neighborhoods with concentrations of residents who already were struggling to get quality medical care. In the absence of a coordinated federal response, local health departments, hospitals and commercial labs across the state have been competing for the same scarce materials. Whether they are “haves” — or have-nots — is determined largely by how deep their pockets are, their connections to suppliers and how the state is allocating emergency supplies.
Compounding these problems is the lack of a state or federal public health infrastructure empowered to acquire and allocate resources on a grand and equitable scale. Hospitals and health systems where many people go for care are, by design, set up to focus resources on their own patients and workers. Their bureaucracies can’t readily adapt to do the community outreach and education that could bring testing to the masses; nor are they set up to do the contact tracing that ensures that people who have been exposed to COVID-19 patients are tested and monitored.
Those roles typically fall to county health departments, which in much of California operate on bare-bones budgets that make it a struggle to contain perennial STD outbreaks, let alone a deadly pandemic.
Over the past two months, the state has triaged one testing disaster after another, but it is finally making headway on making tests more widely available, in part by cutting its own deals for supplies and expanding testing sites in underserved areas, said Dr. Bob Kocher, one of three people on a testing task force convened by California Gov. Gavin Newsom.
But conversations with dozens of local health officials, hospital systems, scientists and elected officials reveal just how complicated a task it will be.
Take Lake County, a recreational mecca just over two hours north of San Francisco. With 65,000 residents, it has had so few testing supplies that officials have resorted to buying swabs on Amazon and pilfering chlamydia testing kits for swabs and the liquid used to transport specimens to labs. Through what the county has cobbled together, it has identified six cases of COVID-19, all found via nurses or volunteers who have gone out looking for patients. “We’re basically having to do tea leaves to figure out what’s going on,” said Dr. Gary Pace, the county’s health officer.
He knows the county has community transmission, both from the cases they’ve identified and because they’ve started running tests on raw sewage to check for the COVID-19 virus; samples from four treatment plants have come back positive. “It is a way to just get more information because we can’t do testing,” he said. Unlike the diagnostic kits — which make use of supplies every health department in the country is competing for — the sewage sampling is done pro bono by a technology startup.
While announcing an ambitious program to increase testing last week, Newsom highlighted the rural-urban divide. “One of the big struggles we have had in the last few weeks of this pandemic is getting to rural and remote parts of this state and getting up testing sites and making them available,” he said.
Newsom is promising to dramatically increase the level of coronavirus testing, with a focus on rural towns and communities of color. California currently tests about 25,000 people a day but has a strategy to raise that to 60,000 to 80,000 per day. The state has opened the first of 86 pop-up testing sites targeted for areas in need. It is launching a program to train 10,000 workers to serve as temporary disease investigators who can do the contact tracing considered fundamental in stemming the spread of the virus.
Pace said he wrote the governor to ask for one of the pop-up sites. “Statewide, there’s a situation where there’s not enough testing, and if you’re trying to demonstrate progress, the way you do that is numbers,” he said. “We are interested in equity, though, and in my view, we need some horizontal coverage instead of just lots of numbers.”
In Mendocino County, situated along California’s rugged North Coast, officials expressed similar frustration. In late April, a health center on the Round Valley Indian Reservation got a rapid test machine made by Abbott Laboratories, distributed via the Indian Health Service. That same day, a tribal member came in feeling sick. That person tested positive for COVID-19, as did five family members. The county previously had identified just five cases, all linked to travel.
Dr. Noemi Doohan, the Mendocino County public health officer, fears a broader outbreak among the six tribes who live on the reservation. The state since has provided 2,000 test kits for people who live or work around the reservation. Doohan’s office will have to hire couriers to drive 2½ hours to a public lab in Sonoma County, which also has limited supplies, to get them processed.
It’s Every Lab — And County — For Itself
A mix of commercial and public labs are responsible for testing in California, and supply chain limitations have plagued them all. But those with deeper pockets and stronger commercial relationships have been out-competing counties and public labs with limited resources.
Rural Tulare County, spanning the peaks and foothills of the Sierra Nevada, is home to half a million people. It also has one of the highest per capita death counts of COVID-19 in California. Until recently, the local public lab was the only place in the county that could test for the disease. After borrowing staff from another county, buying additional machines, and suspending testing for most other diseases, they are now able to process 85 tests a day. Officials also can send specimens to commercial labs in other parts of the state, but say days-long turnarounds create bottlenecks for tracking patients and finding contacts.
Monterey County, in the heart of the state’s “salad bowl” coastal farming region, has relied on donations — and horse-trading — to meet demand. A local hospital found the expensive materials needed to make a missing reagent and mixed a batch for the public lab, said lab director Donna Ferguson. The hospital also gave the county 1,000 swabs, which Ferguson used to barter with Riverside County for extraction kits.
And through the kindness of strangers, she found a stopgap for limits on another important resource: lab workers.
During an interview with a local public radio station in March, Ferguson mused that if one of the three microbiologists working in her lab got sick, it could be disastrous for the county’s ability to process tests. The next day, she got a call from a graduate student at Stanford’s nearby Hopkins Marine Station. He’d heard the interview. Could he and his colleagues help? The crew of six graduate students from three universities has been volunteering at the lab since, tripling its capacity to 120 tests a day.
Though the supply chain is a concern for labs of all sizes, manufacturers appear to be prioritizing orders from commercial labs and big health systems over public health labs, said Eric Blanks, chief program officer for the Association of Public Health Laboratories, which represents most of the labs run by public health departments in the nation.
Quest Diagnostics, the medical testing giant headquartered in New Jersey, is running 350,000 coronavirus tests a week in its facilities around the nation. But it is being inundated with samples from across the country, and even as it has worked to ease backlogs, counties and private hospitals are waiting days for results.
Kaiser Permanente says it can test 2,000 to 2,500 people throughout the state each week. Sutter Health, a major provider in Northern California, tests around 650 people each day across its hospitals. CommonSpirit Health, which includes Dignity Health hospitals, says it could process 50,000 samples a week if it had to. As of last week, Stanford had run more than 20,000 tests for Bay Area residents. (Kaiser Health News, which produces California Healthline, is not affiliated with Kaiser Permanente.)
But even the giants don’t have unlimited supplies. “It really is the manufacturing lines. They’re the ones that right now are the limiting factor,” said Karen Smith, system vice president of laboratory services at CommonSpirit Health.
Moreover, hospitals are not set up to solve the broader issue of statewide disparities in access. They can generally handle the patients sick enough to seek out their ERs. But it hasn’t historically been their role to arrange community-wide supplies and testing.
“You’re not going to go to an emergency room if you’re asymptomatic. That’s the last place in the world you want to be right now,” said Dr. Omid Bakhtar, medical director for outreach laboratory services at Sharp HealthCare in San Diego. “It’s frustrating for me. I have the ability to do more [specimens], but how do I get them?”
Tests But No Takers
In pockets around the state, some counties have been able to stabilize their flow of supplies, in some cases because they have more financial means, in others because of their relationships with major hospital systems and research institutions.
With more confidence in their supply chains, Los Angeles and Riverside counties say they are ready to offer testing to any resident. Several other counties, including much of the Bay Area, are asking more people, including workers deemed essential without COVID symptoms, to get tested.
But some counties that have managed to ramp up testing are wrestling with yet another problem: not enough people to test. The reasons are twofold. After weeks of being told they shouldn’t go for testing because of shortages, the public seems to be adhering to that message even now that more testing is available. And the public health workforce tasked with locating those in need of testing is depleted.
San Francisco can test 4,300 people each day in its publicly supported labs but was receiving just 500 samples a day as of late April. Los Angeles is testing roughly 10,000 people daily but says it needs to double that to lift the shelter-in-place orders. Its focus in coming weeks is to increase testing among the uninsured and those in at-risk living environments such as homeless encampments and skilled nursing facilities.
Health officials say part of the challenge is they aren’t getting the word out to poorer residents and communities of color, even as those same groups are being hit harder by the virus in many cities. In San Francisco, for example, Latino residents make up 16% of the population but 25% of COVID-19 cases. In Los Angeles, black people are 9% of the county’s population but represent 15% of the deaths from COVID-19 for which race and ethnicity data is available.
Kocher, of the state testing task force, acknowledged the state has more work to do. But, he argued, there’s also a sufficient amount of testing capability available today, especially via high-capacity commercial labs where the state says the vast majority of specimens should be processed.
“Right now, we’re concerned with not having enough samples collected,” he said.
When officials do slowly begin to let people return to work and school, experts agree that cases will go up, creating even more need for labs, testing and contact tracers. Preparing for that future will require even more resources.
“We need money,” said Santa Barbara County Health Officer Dr. Henning Ansorg. “Lots of money. Lots and lots of it.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation.
Testing In California Still A Frustrating Patchwork Of Haves And Have-Nots published first on https://smartdrinkingweb.weebly.com/
0 notes
Text
How technology can save the NHS
The NHS turned 70 this year. Much of the coverage of the anniversary highlighted how the health service is facing unprecedented challenges: a shortage of clinicians, an ageing population prone to ever more ailments, and ongoing public health challenges from poor nutrition to air pollution.
More on innovation
And all of this is set against a background of the vagaries of politicians, including pledges to deliver a seven-day NHS, attacks on junior doctors, and various health service ‘reforms’.
When an organisation is stressed in this way, it’s not unusual to hear calls for greater efficiencies to be made, for staff to start working smarter, not harder — and technology is often seen as an enabler of such productivity gains.
The NHS has had a difficult relationship with technology in the past: indeed some of the worst failures in public sector IT have been associated with the health service, like the costly problems of the NHS National Programme for IT. More recent WannaCry ransomware attacks, which took swathes of NHS services offline, shows that the organisation is still lagging when it comes to basic IT hygiene.
That said, it’s hard not to come to the conclusion that there are areas where technology could help the NHS deal with its challenges: experiments with artificial intelligence are showing early promise, indicating that there are areas of routine work, such as reviewing various types of medical scans, that could one day be handed over to AIs.
SEE: How to implement AI and machine learning (ZDNet special report) | Download the report as a PDF (TechRepublic)
Similarly, it’s easy to see how Internet of Things deployments could be used to improve patient safety and resource management. Other technologies, such as robotics or virtual reality, could have smaller, but potentially equally interesting, roles within the health service in future. Connected devices, both for use in hospitals and in the home, will also help drive insight into public health at a population level. Some of the pressure here will come from patients themselves who have bought a new gadget like the new Apple Watch.
However, the more clouds hang over other emerging technologies. For a permanently cash-strapped NHS, any technology that requires a significant financial outlay — such as a new surgical robot — is likely to only make its way into the NHS slowly, particularly if it’s a more esoteric piece of kit. One example of the honest realities of funding: while charities may be willing to fundraise for a new surgical robot for a children’s ward, will they feel the same about IoT kit for tracking (expensive and easy to misplace) hospital beds? That’s always going to be a harder sell.
Still, the trend for technology to become dramatically cheaper and more powerful over time, particularly when there’s increased competition, will likely see certain technologies like AI and robotics spread relatively quickly once a certain price point is reached.
But questions over responsibility will also need to be solved before some emerging tech is used to its full potential. Take AI, for example, or any other systems that become automated: if something goes wrong, who should take the blame?
If an AI reads a scan and makes the wrong call, sending the patient home with an all-clear rather than for treatment due to a recurrence of cancer, working out how to apportion blame will be tricky. Will we blame the NHS, for using a system that can make such mistakes, the hospital for not reviewing the AI’s decisions, or any of the technology providers involved in the health service’s AI stack? How does healthcare ensure that the algorithms behind these services are tested and fair to the whole community, not just a subset?
These are harder problems to resolve than questions of cost, bringing with them issues of patient safety and litigation. The NHS will have to decide what is an acceptable error rate for autonomous tech systems, just as it has to with human medical professionals.
A related issue that must also be dealt with is that of trust. From consumer wearables to AI systems, the health service’s users need to feel that any data they provide to emerging tech should be treated with the same level of confidentiality as if they had shared it with their family GP.
The NHS has already made some missteps in this area: the tin-eared attitude to data sharing with Care.data, and the clumsy handling of patient information with the pilot of DeepMind’s Streams app, have shown the health service still has a way to go before it reaches the necessary level of trust for wider data sharing.
That’s not only a shame because it could hold back the rollout of useful technology, but also because it prevents the NHS from gathering vital data that could be used for public health research to improve healthcare across the country.
Of course, NHS-wide data gathering is something of a pipe-dream right now. To gather and share data between organisations within the NHS would require interoperability between the disparate IT systems that the NHS uses. As IT procurement is done piecemeal, NHS IT is not standardised, meaning that it’s far too hard to piece together data across the health service as whole — a real shame given how useful such data would be in training those AI systems which could do so much good.
What’s more, a significant chunk of the NHS, particularly in secondary care, is firmly attached to good old undigitized paper. For many patients admitted to hospital, every interaction with a doctor will be recorded on a bundle of paper notes in the doctor’s famously terrible handwriting.
SEE: Digital transformation: A CXO’s guide (ZDNet special report) | Download the report as a PDF (TechRepublic)
Pages of notes that fall out with age, which are often kept separately to the patient’s drug chart, and can only be viewed by one healthcare professional at a time. Pages that more junior members of the ward team will spend a not insignificant amount of time chasing around the ward on a daily basis.
Those drug charts, too, are paper — a dreadful anachronism in a world where e-prescribing schemes would cut the mistakes due to handwriting.
Similarly, fax machines and transferring images on physical CDs still occur in some modern hospitals — while there’s a certain security argument for such systems, equally secure all-digital alternatives exist, and would greatly speed the time it takes to send, say, a discharge letter detailing a new medication regime from a hospital ward to the patient’s GP.
Even basic mobile tech is something of a rarity, although more understandable given security reasons. You can’t help but think of the simple productivity benefits mobile would bring — the ability for a consultant to check a patient’s notes when they get a 2am call about an emergency, for example — and wonder how much consumer tech is already taking the strain: when WannaCry took email systems online, it was WhatsApp that let health professionals carry on communicating with each other.
While emerging tech from AI to VR, robotics to IoT could bring clear improvements to the NHS, it seems like there are greater, systemic benefits to be had from just getting the basics right: a paperless NHS, electronic prescribing, data sharing between primary and secondary care, a central body to guide NHS procurement to ensure health service-wide interoperability.
Such a wish list may sound ridiculously simple, but it would be both costly and grossly time consuming, and unlikely to capture either public imagination or political enthusiasm in the same way as more cutting-edge tech. And yet, it’s these ‘simple’ changes that could not only bring greater efficiency and better productivity for the NHS, but lay the foundations for the next generation of emerging technologies.
RECENT AND RELATED COVERAGE
NHS IT: Using the open standards and the cloud to drive digital transformation
How one of the UK’s largest NHS trusts is developing its own infrastructure to put patients at the centre of healthcare.
NHS IT: Can better use of tech give healthcare a shot in the arm?
Is improving tech the key to to making healthcare more efficient?
How smart contact lenses will help keep an eye on your health
Health tech: Researchers are working on combining sensors with off-the-shelf contact lenses for a range of medical applications.
DeepMind’s AI spots early signs of eye disease
Initial results of DeepMind’s partnership with Moorfield’s Eye Hospital in London suggest that a scanning method that uses artificial intelligence could provide quicker diagnoses and help prevent sight loss.
Healthcare security nightmare: UK’s NHS lost nearly 10K patient records last year (TechRepublic)
Despite having electronic record systems in place, 94% of NHS Trusts still use handwritten notes for patient record keeping, according to a report from Parliament Street.
This swallowable chip uses glowing bacteria to spot hidden illnesses
MIT researchers have created swallowable chips that can help identify blood in the gastrointestinal tract.
Government websites hijacked by cryptocurrency-mining malware (CNET)
Over 4,000 websites worldwide were affected by the malware.
Source: https://bloghyped.com/how-technology-can-save-the-nhs/
0 notes
Text
What is big data?
http://www.internetunleashed.co.uk/?p=23856
What is big data? - http://www.internetunleashed.co.uk/?p=23856 While the origins of the term are elusive, and even debated, big data is one of those concepts that many know about, yet it defies a simple definition. At the heart of big data, as the term directly suggests, is an extremely large volume of data. This is often drawn from diverse sources and even different types of data, which is then crunched through advanced analytic techniques which hopefully pick out patterns that can lead to useful conclusions.Big data also infers the three Vs: Volume, Variety and Velocity. Volume refers to the size of the data, variety indicates that the datasets are non-homogenous, and velocity is the speed at which the analysis takes place, often with the goal of achieving real-time analysis.The datasets involved are indeed seriously large – we’re talking terabytes to zettabytes (1ZB is equivalent to 909,494,701TB, for the curious). In addition to the size of these datasets, the data can be of different types: structured, semi-structured and unstructured, plus it can be drawn from multiple sources.This does beg the question as to where all this data is being generated from. It comes from all types of places, including the web, social media, networks, log files, video files, sensors, and from mobile devices.The latter are particularly important as most of us keep our phones with us and on 24/7, and they have an array of sensors, including GPS, cameras, a microphone, and a motion sensor. Furthermore, the majority of smartphone use is not voice communication, but rather other activities, including emails, games, web browsing, and social apps – which ultimately translates to 90% of use being mobile apps. A large driver of big data is this mobile data, which gets generated at a breakneck pace. Data mining But data without any analysis is hardly worth much, and this is the other part of the big data process. This analysis is referred to as data mining, and it endeavors to search for patterns and anomalies within these large datasets. These patterns then generate information that is used for a variety of purposes, such as improving marketing campaigns, increasing sales or cutting costs. The big data and data mining approach not only has the power to transform entire industries, but it has already done so.For example, Trainline is a leading European independent train ticket retailer, selling domestic and cross-border tickets in 173 countries, with approximately 127,000 journeys taken daily by customers. The company utilized big data to modernize its approach to travel, with a focus on improving the customer experience via innovation through its app.The results are that now customers receive enhanced disruption notifications through the app. More than just notifications of delays, these enhanced notifications are specific to each traveler’s journey, a first for the UK rail industry. The firm has also innovated in terms of predictive pricing, which is able to predict when advance fares will rise from the initial discounted rate, allowing passengers to purchase fares at lower prices.Big data has also been used in restaurants, and in particular the fast food industry. McDonald’s is the world’s largest restaurant chain by revenue, and serves over 69 million customers daily at over 36,900 locations in over 100 countries.Due to sheer volume alone, tons of data is generated, and therefore McDonald’s has adopted a data-driven culture, with the goal of improving its understanding on the level of each individual location, with the overall goal of a better chain of restaurants.Through big data, McDonald’s has optimized its drive-through experience, for example taking note of the size of the cars coming through, and preparing for a spike in demand when larger cars join the queue.Another big data innovation has been those digital menu displays that can flexibly show menu items based on a real-time analysis of the data. The menus shift the highlighted items based on data including the time of day and the weather outside, specifically promoting cold drinks when it is hot outside, and more comfort foods on cooler days. This approach has boosted sales at Canadian locations by a reported 3% to 3.5%. Health matters This big data approach has also been applied to healthcare. An obvious example is the major shift away from ‘pen and paper’ charting where your physician’s data is locked away in a filing cabinet in the office, to Electronic Health Records (EHR), which now have all patient information neatly entered into a computer database, ready to be mined.This approach promises to be disruptive, with a recent publication in the European Heart Journal promising the “potential to improve our understanding of disease causation and classification relevant for early translation and to contribute actionable analytics to improve health and healthcare”.The benefits of big data in healthcare will go beyond data mining the EHR. A significant challenge for hospitals is staffing, which has to be adequate at all times, with the potential to ramp up during peak periods.At a group of four Paris hospitals that comprise the Assistance Publique-Hôpitaux de Paris (AP-HP), they are looking to improve flexibility in staffing. They used a dataset of 10 years of hospital admission records, down to a granular level of the number of admissions by the day, as well as the hour of the day, and combined it with weather data, flu patterns, and public holidays.Using machine learning, they then honed their algorithms for future trends to predict the number of upcoming admissions for different days and times. The result is that they now have an easy to use, browser-based interface for hospital administration, as well as clinical staff who are able to forecast admission rates over the next 15 days, which is used to obtain extra staff at times when a larger number of admissions is anticipated.With data, and in particular mobile data being generated at a ridiculously fast rate, the big data approach is needed to turn this massive heap of information into actionable intelligence. In the examples we’ve cited above, the challenge has been met, and as even more data is collected, there will be more opportunities to increase quality and efficiency across a number of diverse industries via faster and better analysis of these disparate sprawling datasets. We also ask: Is big data a big failure? Source link
0 notes
Text
Being a registered nurse in Philippines: Scope & Prospects
Nursing as a profession is versatile with endless scope of improvement and gaining knowledge. Making a career as a nurse includes much more than patient care as nurses make a very important pillar of healthcare without which the healthcare sector can be on the verge of collapsing. The decision of choosing a career as a nurse requires constantly competent performance, adherence to code of ethics, and above all, the sense of empathy towards patients, their families and co-workers. It is always said that healthcare workers never stop learning and the deeper they delve into the field, the better they get at the art of multitasking. Managing personal life along with your professional commitments can be a big concern as a nurse but if the priorities and goals are set straight, then pulling all of it together shouldn’t be a botheration. In order to be a successful nurse one needs to qualify multiple levels of education and attain sufficient practical exposure before treating intense cases.
Before proceeding further, ask yourself the most oft stated question “Who is a nurse”? Once you have your thoughts channelized about it, you might want to look at the video below which details the concept of nursing in regards to the experiences offered by the practical learning.
VIDEO: What It Means To Be A Nurse
The video above is an original concept of Stanford Health Care and it highlights the different views of multi-cultural nurses at the hospital and what according to them constitutes to be a part of nursing as a concept.
Without a doubt, nursing is the most trusted profession as it’s the basic element of trust on which the patient care thrives and with establishing faith, one can transform healthcare. There can be many ways of building a trustful relationship with your patient. It can begin with a simple communication, the ability to be a good listener and lastly by the way you exercise your medical powers in patient’s best interest. Mostly, patients and family members when enter the healthcare system, get in touch with their nurses, they are vulnerable and seeking hidden answers, so winning their unshakable faith is a victory above all others.
Compassion and thoughtfulness are certainly two more parameters on which your career as a nurse can be evaluated. Persuading the patients to take care of their eating habits, withdrawing their attention subtly from a botheration, and convincing them to make the right call for their health are a few things which go unnoticed but often play the most essential role in maintaining a positive patient-nurse relationship.
HOW TO BE A REGISTERED NURSE IN PHILIPPINES
Being a nurse brings loads of responsibility, irrespective of the country you’re working in. However, the demographic structure does affect the working style and living conditions which eventually leaves an impact on your professional space too. If you’re planning to be a registered nurse in Philippines, then you must know a few prerequisites about being a nurse in Philippines.
1. In order to be a registered nurse in Philippines, you must graduate in a credible nursing program like Bachelors of Science in Nursing.
2. Usually, the courses are 3-4 years long and provide you with the much required and detailed knowledge about nursing skills, health promotion, disease prevention, risk reduction, patient care and much more that you need to know in order to be practically treating a patient.
3. Once you have graduated a nursing program and passed the examination conducted by the country board, you are entitled to be a Registered Nurse (RN) in Philippines.
4. After being a registered nurse, you can explore a variety of employment opportunities around you. One can also apply for global nursing programs as studying courses with international recognition further helps to broaden the scope of getting better job opportunities.
5. A registered nurse is eligible to apply for jobs in public and private hospitals, nursing institutions, and one can also be an independent nurse practitioner and open up a clinic of their own.
However, as important as it gets to know about the criteria of being an RN, it is equally important to know the repercussions which come along if any candidate or a student violates the law and carries out nursing as a profession without confirming to be a registered nurse in the country.
The General Practice Board of Nursing states that a fine of minimum ten thousand pesos (P10, 000.00) and a maximum of forty thousand pesos (P40, 000.00) can be levied on any defaulter who:
• Uses an expired certificate of registration to practice nursing
• Uses his/her certificate of registration for any third party
• Uses a forged certificate of being registered as a nurse and
• Takes multiple classes for domestic and foreign programs at the same time without a permit.
*Source: Professional regulation commission Philippines
Also, in some of the cases, there is a clear possibility of being imprisoned for 1-6 years for violating the provisions of the professional regulation commission.
CAREER PROSPECTS FOR REGISTERED NURSES
Being a nurse in Philippines can open a gateway of opportunities both on domestic and global front. Once you get an examination clearance and practice license from the board, you can explore end number of job opportunities in your choice of specialization. However, the fact remains intact that on a domestic front, approximately 2, 00,000 registered Filipino nurses are struggling to find jobs due to the saturating markets in the country. The international standards set by the developed nations have massively impacted the job opportunities and scope of growth in countries like Philippines and India.
On a comparative note, a registered nurse in Philippines is entitled to receive an annual sum of PHP 170,723 while the annual salary of an RN in a developed nation like Canada amounts to $58,832. Mentioned below are a few payrolls from different nations having a high demand for nurses. The differences in payrolls are impactful and convincing enough to make nurses migrate to the developed nations in search of better employment opportunities.
Source: Payscale.com
Apart from the fixed salaries stated above, there is a potential chance of making additional money on your busy months where you tend to report for extra hours than your routine shifts. Nurses are often asked to work in extra shifts due to the unavailability of sufficient trained nurses.
Well, apart from the financial prospects being thoroughly considered, it is important to understand that a nurse can help in improving the patient care only if he/she is satisfied with their job roles and the status being provided to them. In certain developing nations, many a times, nurses are seen facing a tough time in order to attain the much deserved recognition and respect from patients and co-workers. This can be one of the prime reasons for nurses to look opportunities abroad. There comes a point of stagnation where every field of specialization faces a situation of disparity between the demand and supply of nurses. Usually, excessive demand creates a shortage of nurses and when the supply shoots up to fill the gap, it overpowers the demand in consideration.
INTERNATIONAL OPPORTUNITIES
Moving on to the international employment scope for Filipino nurses, it is extremely important to know that till date Philippines is one of the leading supplier of nurses to the developed nations. Pick the data reports of Australia, USA, Canada, New Zealand or any other developed nation for that matter and you will find a bunch of Filipinos making a majority of the nursing population. Majorly, nurses from Philippines consider moving to Canada for better opportunities and an improved quality of lifestyle. There can be different routes towards reaching the end goal but one of the most though of and simple way is to study specialized nursing programs in Canada and learn the importance of different nursing techniques and their requirement in the country. Once you study the practices of patient care being followed in a country, you become well-equipped and trained to treat the patients in the best of their interests.
However, one thing which remains intact is the need to have a fluency in speaking, writing and understanding English language so that the barriers of communication between the nurse and patient don’t affect the treatment process.
Apart from the language proficiency there are also a few things which affect the eligibility of a nurse from Philippines to study nursing programs in Canada. It is important to be a university graduate from a recognized university board/college of your country and also one must clear the RN exam from Philippines in order to be able to move to Canada and practice nursing. The reason why Canada is the most preferred location to relocate for Filipino nurses is because this year Canada will accept 250,000 applications, along with a special consideration for those making an addition to the healthcare sector.
Apart from Canada, UK too has emerged to be a preferred choice for nurses planning to migrate from Philippines. The country has been falling short of nurses and healthcare personnel which has widened the scope of employment for nurses coming from India, Philippines and South Africa. The fact that the population of old people with multiple long term illnesses has increased in the country is a major contributing factor to the high demand of nurses in UK. However, the exact details about working as a nurse in UK can be made clear once a person actually experiences it themselves but for now, here we have a quick video of three Filipino nurses who share their working experience straight from Surrey and Sussex Healthcare NHS Trust. The video explains about the difference in wages, working environment, sense of respect for the profession and a lot many things which one needs to keep in mind before making a move.
VIDEO: Nursing Recruitment in the Philippines 2015
If a decision of migrating to a foreign land in search of opportunities is made with all the just and fair points being considered then it can be highly fulfilling and inch you closer to the vision of being a global nurse. In terms of financial benefits for nurses in their native country and those in foreign lands, it is an openly accepted fact that nurses in Philippines are underpaid as per the efforts and services they put in their job. In spite of the challenging studies and curricular, there is no guaranteed employment opportunities in their homeland which justifies their calling to move abroad. Licensed healthcare professionals in developed nations are given a much needed recognition for their services and also the compensations granted are more than satisfactory.
MAKE THE RIGHT CHOICE
In situations related to choosing a career path for yourself, there is no clearly ”right” or “wrong” path to be chosen as each one of these paths come with their own set of limitations and advantages. What matters is that how you prioritize the different aspects of growth and development which could help you in the long run. So here’s a quick piece of advice about making the right decision.
Just think about what you want to do and then put a little more stress on “WHY” you want to do it and you shall find the weightage of your opinions lying right there. So, in terms of considering the gateway of opportunities one can open by being a registered nurse in Philippines, it is important to make the right choices ahead of you as it’s with these choices of yours that your identity as a nurse will shape up. In the field of nursing, the more you grow the critical are the cases you have to deal with. So, make a strong mind an uninterrupted focus and continue to work towards finding the ideal opportunities for yourself. Whether it is your native land or it is an array of opportunities in a foreign land, analyze all the prospects it has to offer and make the right choice.
0 notes
Quote
In the Humanities, the phrase ‘the part is a mirror of the whole’ is a very popular maxim. Okeho, in very many respects mirrors what is going on in Nigeria and in many other countries in Africa. What has just been stated is not a hyperbole but a fact as would be demonstrated very shortly.
As stated in the blurb and Preface of the book under review, Okeho in History‘was commissioned to celebrate the centenary of the relocation of Okeho back to its original site in 1917’. Besides educating everyone about the background of the town, the underlining motive of the book is to call the attention of the indigenes to the hopes and developmental challenges of their community. The extent to which it lives up to this intendment would be gleaned from an excursion we are now taking into the landscape of the 232 page publication.
The book is divided into four parts. Part One is appropriately titledIn the Beginning.Part Two contains items that deal with Governance Institutions. In Part Three, issues treated come under the collective title:Religion and Spirituality. Issues pertaining to Education are treated in Part Four while Parts Five and respectively deal with The Economy and Health.Communal Life makes up Part Seven.
The final part which carries the titleConclusiondiscusses the various ways by which Okeho can be ‘taken to greater heights’. There are ten Appendixes. Contained in these Appendices are Traditional Political Institutions, 2. Compounds in Okeho Quarters 3. Modern Political Institutions 4. Education 5. Health Facilities 6. Major Businesses 7. Religion 8.Major Social Organisations 9. Entertainers and 10. An Anthem.
Special pages are also devoted to Bibiliography, Picture Gallery and Index.
Let me state from the onset that the author of this book, Professor Segun Gbadegesin, although a philosopher by training and vocation, demonstrates a good knowledge of historical ethos. This should not be surprising since no one can be a good philosophy scholar without having a good knowledge of some historical figures and ideas. Beyond the call of duty as a philosophy scholar, the authoris also an individual with veritable interest in historiography/history. An accomplished scholar, Prof Gbadegesin is also exemplary in community service. No wonder, he was bestowed with the title of Asiwaju of Okeholand. He has certainly been living up to the demands of this office as attested to, among others, the publication of this book.
The book appropriately opens with the location of the subject-matter: Okeho. The town is found in the heartland of the Yoruba nation. Research carried out established a notion that has always been in the public domain to wit: Okeho is an amalgamation of eleven villages. The villages voluntarily decided to come together for protection and self-survival; a very smart move indeed.
The villages that came together are Isia, Olele, Isemi, Imoba, Gbonje, Oke-Ogun, Ogan, Bode, Pamo, Alubo and Ijo.
The Baale of Ijo whose domain is more strategically located was the one that invited others at different times. For this reason, it was conceded that he assumed the overall leadership of the new settlement. Two points are important to be made at this juncture. The first is the mindset of the then Onjo – an insight into the temperament of the people of yore. For the fear of possible challenge to his leadership position, someone else might demur in having others come near him – especially equally powerful personalities. It is natural for one to want to be protective of one’s ‘privileged’ position. Thus, it was not impossible that such a fear was entertained by the then head of Ijo, Arilesire. Reading between the lines of this insightful book along with its predecessor,
1 Itan Ilu Okeho[i]he overall interest of the people, their safety particularly, was uppermost in the minds of not only OnijoArilesire, but heads of the communities that decided to amalgamate with Ijo. This was around 1800.[ii]
The second point relates to what I mentioned earlier – how Okehomirrors Nigeria. We are aware that Nigeria is an amalgamation of several nations.But while Okeho was able to forge a town out of several hitherto separate settlements within a short time, the more the years advanced, the more Nigeriais falling apart.As stated in the Preface of the book under review, ‘in the voluntary merger and preservation of the heritage of each of the constituents, Okeho also taught us a great lesson in the management of diversity’ Page xvii.
Considering the fact that in an occasion like this, there would not be enough time to go into long treatise, permit me to just highlight salient issues raised in this book.
As stated on Page 95, the economy of the community was built on communalism in which people co-operated with a view to advancing the interest of the individual and that of the community as a whole.
What kept this system thriving then was the honesty and trust that abounded. On page 101 for instance, it was stated that traders used to go to markets in many towns outside Okeho in those days. “Those who could not go gave their products to the market delegates with the confidence that their interest would be well-represented. This was the precursor to the cooperative movement of later years”. (P101).
A maxim in Yoruba language has it that Bi a kobarieniba la, olakiiya. Another says Owolaa fi peenaowo. The first means that to make it in life, one needs the support of other(s) while the second posits that one has to invest in order to reap some dividends. What these means when taken together is that there is the need to have sources from which people with entrepreneurial skills can tap so as to grow their businesses. In several of his articles in his Weekly Column in The Nation newspaper, the author of the book under review, Prof Segun
Gbadegesin,always clamoursfor the need to implement policies that are pro-people. In Okeho in History, he underscores this same point very much by calling on patriotic and well-off indigenes to pull resources together to assist ambitious but less endowed natives. This is in line with the age-old notion of ‘agbajoowoni a fi n soya’. His advocacy is supported by Asiwaju Bola Tinubu who in his recent public speech[iii] asserts that “The long-term economic strength of the nation is dependent on how we deploy idle men, material and machines into productive endeavour.”
What the JagabanTinubu says of the Nigerian nation is true of Okeho. The interesting thing is that what is advocated here is not strange to Okeho, our beloved town. Apart from the eesu, aro, owe[iv]tc traditions, Gbadegesin makes it known to us that such a practice has taken place before. On page 103, he recalled that there was an explosion in transport business as a result of credit facilities provided by AlhajiShittu Oladejo a.k.a. Asao Motors. The challenge is thrown to EgbeOmoIbileOkeho, Okeho Strategic Development Foundation(OSRADEF) and elites of Okeho is to pull their resources together with a view to lifting the town up. Although eleven communities came together to form Okeho, although there are over 240 Compounds (Agbo-ile), although there are various political, religious, professional and sundry other groups in Okeho, there is the need to have patriotism, love for one another and development of the town at heart. Echoing one of the exhortations of late Onjo, Oba Ereola Adedeji where he reminded everyone that there is only one Okeho, Gbadegesin urges everyone to join hands together in uplifting the town by “investing our intellectual, moral, spiritual and material resources in its development and resources” p. 157.
At the beginning of this short Review, I talked about how Okeho is a microcosmof Nigeria, especially in regard to the plurality of religious faiths, historical background, politically-motivated violence as well as failure to properly exploit available potentials for the good of all. The only major area of difference betweenOkeho and the Nigeria nation was in how the two were respectively amalgamated and how there is no known religious-induced violence in Okeho – thank God! While the coming together ofOkeho was voluntary, the coming together ofNigeria was forced. The Nigeria nation has something to learn in how Okeho elders, more than a century ago, forged unity among disparate communities. Nigeria leaders also have something to learn from how the present Okeho leadership and the elites are trying to overcome their shortcomings and build a new society that will continue to serve the best interest of its people. They are doing this by re-examining their past, learn from their mistakes and enhance their areas of strength. Nigeria should take a cue by listening to the agitators of Restructuring so that components of the country can, just as Okeho Eleven did over one hundred years ago, sit down to discuss the terms of staying together.
2 keho in History teaches a lot of lessons. I will mention just a few. Strength in unity p vi, how power or wealth makes some people to misbehave (bi aye ba ye won tan, iwaibajeni won ma n hu) p71, how treachery or undue rebellion does not pay pp 8, 47, 59.
The personal experiences narrated by the author on pages 111 and 112/113 are quite instructive regarding the immense benefit that we can derive from a proper co-operation between traditional and western ideas. Incantations by a knowledgeable elder literally neutralized the venom of a scorpion that stung the author while at school. The second experience was that of how the western method of healthcare came to the rescue. This was how Pa Bamimeke used a vacuum to bring out the cockroach that sneaked into the writer’s ear, p112.
Before rounding off, it would be remiss of me if I failed to mention areas that would need edification or emendation in the next edition of this historical book. Translation of the Yoruba expressions on pp 24 and 29 is desirable as was done for those on pages 40, 57, 67,130 etc. Also, ‘house fire’ on page 71 in reference to Sango ought to be ‘thunderbolt (ara)’. A person who is not familiar with Oyo State may not realize that the School of Hygiene being referred to on P 90 is the one in Ibadan as only Eleyele was mentioned. ‘Ward off’ should replace ‘wade off’ on page 6. Efforts should also be made to ensure that the missing letters in such words as Isemi, 6, 13, 23 Alase 13, Ayoola 45 to mention a few are inserted. The phrase “There, Olujumo, Olujide, and Adeniyi” p42 is hanging. In the same vein, I hope that the name of notable Okeho professionals like LereShittu will find a place among Journalist/Broadcasters (p179). Luckily, the author promises that the missing ones will be included in subsequent editions.
A few words on the role normally played by Ifa in the choice of a king would be helpful (p42). Readers would be better informed by knowing who the first Onibode is P30.
In his concluding remarks, Gbadegesin states “We need others as they need us to make the world a habitable and better place for all people.” (P157). This message is for Okeho people as it is for the people of Okeogun as well as Nigeria as a whole.
I like to end this Review by echoing His Royal Highness, Oba RafiuOsuolale Mustapha Adeitan II in his Foreword to this book. He commends the book to all sons and daughters of Okeholand because “There is a wealth of information there for everyone to cherish” pxiv. Except that the book is recommended not just to indigenes of Okeholand but to all Nigerians and several others across the world due to the universal messages contained therein.
Thanks for your attention.
*JareAjayi, a poet, novelist and playwright is a journalist and social worker dedicated to community service among others.
http://icechuks2.blogspot.com/2017/11/okeho-in-history-clarion-call-to.html
0 notes
Text
6 Key Highlights From iMoney’s Pre-Budget Forum
With Budget 2018 around the corner, iMoney invited a panel of experts to discuss and share their views on a number of topics related to the Malaysian economy. The panel reviewed the policies from the previous Budget 2017 to see if Malaysia is on track economically, and also discussed what could be announced in the next Budget. If you’ve missed the Facebook live discussion, here are five key highlights from the forum:
1. The disparity between consumer perception and economic growth
Malaysia’s economy expanded at the fastest pace in more than two years in the second quarter of 2017 due to domestic demand and robust exports. According to World Bank, the gross domestic product (GDP) growth rate is predicted to rise to 4.9% for the year, which is slightly higher than the current projection range of 4.3% to 4.8%. Despite the positive growth in numbers, the sentiment is not echoed by the consumers. During the live forum, there were a few contributing factors brought up by the panellists. According to one of the panellists, Professor Dr. Jomo Kwame Sundaram, the former assistant secretary-general for economic development at the United Nations, the three main factors contributing to the negative sentiment on the ground are the implementation of the Goods and Services Tax (GST), the declining ringgit and also political scandals such as 1MDB and the fiasco surrounding Felda Global Ventures. These were initially countered by measures such as the introduction of 1Malaysia People's Aid (BR1M) and minimum wage and also alleviated by the higher commodity prices. However, in recent years, these are no longer effective to help with the rising cost of living. This was echoed by Dr. Muhammed Abdul Khalid, founder and chief economist from DM Analytics, adding that other than GST and the declining ringgit, the reduction of subsidies also played a role. “If ringgit drops, the prices of all these items [food] go up. It’s worse for low-income because they spend the bulk of their income on food,” Muhammed explained. This is further exacerbated with wage increment at a slower pace, said Lee Ching Wei, CEO of iMoney Group. Muhammed agreed, saying wage, after inflation adjustment, only grew by 0.9% last year, which in absolute value is only RM17. “The worst thing is, which is quite surprising, at the mean level, the lowest income growth was for the B40 group. Usually this group of the population has the highest income growth compared to T20 and M40,” Muhammed added.
2. Malaysia’s taxation system needs to be more progressive
Malaysia tax system is inequitable. This is the sentiment echoed by the panellists during the iMoney live forum last Tuesday. “After taxation, income distribution is worse than before taxation,” said Jomo. This is due to the regressive nature of certain taxes, such as GST. However, scrapping GST now is not a good idea because it will create a revenue gap which the government will need to fill from other channels so deficit in the budget does not increase. The view among the economists is, the country should move to a more progressive tax structure, and this goes beyond reviewing, reducing or repealing GST. Despite criticism, the government does not plan to repeal GST, and according to the Prime Minister Datuk Seri Najib Razak, GST helped the government offset the losses from the falling fuel price. The revenue from GST was recorded at RM39 billion in 2016. The current tax system is regressive because it does not tax sources of earning fairly, Muhammed added. The Malaysian tax system also gives the affluent and corporations too many tax exemptions. If you’re a wage earner, you get taxed, but if you buy or sell shares, or if you receive an inheritance, you don’t get taxed in Malaysia. Even for property flippers, the Real Property Gains Tax (RPGT) is only up to five years for Malaysians. Other countries tax these on top of individual and corporate income tax. Another fallacy that we believe in is the theory of reducing corporate income tax to create more job opportunities and increase wage, said both economists. Instead, there should be more incentives to enhance the productivity of the corporate sector. “The country needs a sustainable revenue base for the country rather than just tinkering with the consumption tax,” said Jomo.
3. Budget 2018 should not cut investment in education and healthcare
In the previous Budget, the funding for the higher education ministry was set at RM6.117 billion, down from the RM7.575 billion allocated for 2016. As a result, 10 out of 20 public universities are now 70% dependent on public funds, ahead of the 2020 target. “What this Budget should not do is: Do not cut spending, especially development expenditure, for education and health,” said Muhammed, adding that these are not expenditure but investments which will bring returns to the country. Research and resources will suffer when these expenditures are cut. The current spending of RM6 billion is not huge if compared to the interest on national debt at RM24 billion. “We have the highest household debt in Asia, and much of it is from housing, but education is fast catching up,” said Jomo. “We spend a lot on education but we don’t have much to show for it, but for healthcare, we don’t spend a lot but we have an impressive record.” He further added that Malaysia should spend more on preventive healthcare and lauded the recent announcement by Health Minister Datuk Seri Dr S. Subramaniam on the reduction of cost for Hepatitis C treatment to RM500. “We must be committed towards achieving universal health coverage,” said Jomo.
4. PR1MA and affordable housing
As of March 2017, a total of 6.3 million applications for the BR1M 2017 have been approved, with total allocation of RM5.41 billion. Assuming only 1 million of these applicants need affordable housing, it seems pretty impossible for the government to provide affordable housing such as PR1MA to everyone, Wong Chen, Kelana Jaya MP said. “Assuming we can build 10,000 houses a year, it can only serve 1% of those who need. This creates the ‘lucky draw’ mentality which encourages corruption,” said Wong. With RM10 billion, Wong said he would rather use it for wage increase to reduce poverty rather than building affordable housing. However, Jomo disagreed with the idea, saying that affordable housing is not an insoluble problem because there are countries which had successfully done it such as Singapore. “The problem in Malaysia is the access to land is controlled and abused by politicians, and the politicians are often in bed with the developers,” added Jomo. Although the current system is imperfect and it does lead to substandard housing, but it doesn’t mean these problems are insoluble.
5. Should we reinstate fuel subsidy?
It has been almost three years since Malaysia scrapped fuel subsidy back in December 1, 2014, and the current managed float system was introduced. This was during a time when crude oil prices fell to US$62 per barrel. In May, Pandan MP Rafizi Ramli suggested that fuel subsidies could be reinstated once Pakatan Harapan was installed as the new government. During the discussion, a Facebook user asked Wong to justify the return of fuel subsidies. “As an oil producing country, we are morally obligated to subsidise fuel, and at the same time, decelerate our dependency on oil,” said Wong, adding that at one point, the question of fuel subsidies would not even arise as consumption of oil drops. “It is our moral duty to subsidy the poorest,” Wong added. This was labelled impractical and the worst thing to do for the country by both Jomo and Muhammed. “We all know that the fuel subsidy is largely enjoyed by the middle class and not by the poorest,” Jomo said, adding that subsidy should be channelled towards public transportation. [caption id="attachment_31669" align="alignnone" width="743"] Image from Bank Negara Malaysia[/caption] A Bank Negara Malaysia report revealed, “It is estimated that the bottom 20% of households in Malaysia only receive 4% of the fuel subsidy, while the richest 20% receive 42% of the subsidy.” This was also echoed by Muhammed who said fuel subsidy is the worst thing to do to help the poor. We also need to relook at the definition of poverty. As a developing country, we should look at the relative term of what being poor means, it is not just merely looking at the income. So, will the budget deficit for Malaysia be reduced to the point where we achieve a balance budget? An annual balanced budget should not be the target, but rather to balance the budget over the medium term. “When the economy is doing well, the country should do some belt tightening and cut down expenses to pay down the deficit. When the economy is in bad shape, the country needs more productive government spending to counter the effect of the private sector declining,” said Jomo. The country has been running a deficit since 1997. It made sense during the 1997 crisis, but it no longer makes sense now. Wong agreed, “For developing country, it is reasonable to have an average deficit of 2% to 3%. However, in a 10-year cycle, we should try to record a two-year surplus.” If you’ve missed the live forum, watch the full discussion below:
youtube
The post 6 Key Highlights From iMoney’s Pre-Budget Forum appeared first on iMoney Malaysia.
0 notes
Text
Important Things to Know About Diabetes in the Developing World
New Post has been published on http://type2diabetestreatment.net/diabetes-mellitus/important-things-to-know-about-diabetes-in-the-developing-world/
Important Things to Know About Diabetes in the Developing World
Last month, I attended a meeting with the Helmsley Charitable Trust folks in New York, brainstorming with some community leaders on how we can best work together to make life better for people with type 1 diabetes everywhere. One of the folks I met on that trip was Merith Basey, the young, enthusiastic Director of International Operations at the Virginia-based non-profit organization AYUDA (American Youth Understanding Diabetes Abroad). Some things that Merith told me about diabetes in the Third World were eye-opening, to say the least. Not just how much they need help, but how help often comes in the wrong forms.
Don't miss today's inside look from Merith on what's happening with diabetes advocacy in the neediest countries:
A Guest Post by Merith Basey, AYUDA
As we all know, diabetes today is a global epidemic — affecting an estimated 366 million people on the planet. Readers of this blog will be no strangers to the challenges of managing diabetes wherever in the world they may live. These challenges can be greatly exacerbated in low and middle income countries, where an overwhelming 80% of people with diabetes live and where a lack of education at the primary health care level is often coupled with poor access to medical supplies (due to poor access to health services, inequities within the health system, insufficient or non-existent drug supply system and inability to pay).
Given the current global economic crisis, the dual burden of diabetes combined with unemployment can push people more deeply into poverty and poor health wherever in the world they live. For young people aged 15-24, who in 2009 made up almost 40% of those without work, living with or being at risk for diabetes in these countries can be particularly burdensome. They can often live for extended periods with undiagnosed diabetes and their decreased quality of life and lost productivity can remain unrecognized by many, including their governments.
Over the past eight years with AYUDA, living and working in type 1 diabetes communities across Latin America, I have witnessed first-hand the everyday realities that many children, young people and their families face when trying to manage the condition, particularly when confronted with the dual challenges of access to affordable medication and supplies, and access to appropriate education and support. Two main challenges remain at the core:
A lack of insulin and diabetes supplies
Despite what people may believe, more than 90 years after the discovery of insulin, children and young people in many parts of the world still die or suffer preventable complications as a result of a lack of insulin. Even though insulin is listed in the World Health Organization (WHO) Essential Medicines List, the IDF recognizes that, "it is still not available on an uninterrupted basis in many parts of the developing world."
Furthermore, the cost of insulin and test strips is often disproportionate to the average monthly income for a local family, i.e. in developing countries, paying for insulin and testing supplies each month represents a much more significant proportion of a family's paycheck than it would elsewhere. Since test strips alone can cost up to $1 each, testing even a couple of times per day can be almost impossible in countries where a large proportion of the population live on less than $2 per day. There are also vast inequities within countries, for example a person diagnosed with type 1 diabetes in rural Mozambique has a life expectancy of less than 2 years, whereas someone living in the country's capital Maputo, would have a life expectancy closer to 20 years.
That said, many people without health insurance in high-income countries like the United States can also end up paying high prices for their insulin and testing supplies, particularly at a moment in the country's history where 46.2 million are now living below the poverty line. As a result, increasing numbers of people cannot afford to correctly adhere to their insulin therapy and consequently are at increased risk of hospitalization with DKA. A recent study in the U.S. reported that a "lack of money or transportation to obtain insulin" was the reason that a third of patients entering hospital with DKA had halted their own insulin therapy.
With the growing numbers of people living with insulin-dependent diabetes, including an estimated rate of 78,000 new cases of type 1 diabetes per year, the global need for insulin (and other diabetes supplies) will continue to increase.
Over the past decade in the field of HIV/AIDS, strong pressure from HIV activists and NGOs meant that life-saving anti-retroviral drugs were reduced from more than $10,000 per person per year to less than $100 per year, due in part to a price war between branded pharmaceutical drugs and significantly cheaper generic drugs. Activist pressure helped to shift government policy so that pharmaceutical companies were forced to run things differently, making drugs much more affordable for both people and governments.
In diabetes, the leap to affordability is still yet to come. Despite human insulins such as NPH and R being off-patent (i.e. being available as a generic, or non-brand name version), newer branded analogue insulin (eg. Lantus, Humalog, Novorapid etc), is still on-patent, which means that although the WHO recognizes that analogue insulin provides "no clear advantage over human insulin," the higher costs of analogue insulin are considered to inflate the cost of all insulins.
Myths create cost disparities
In addition to high costs of insulin and diabetes supplies in general, there are often many myths surrounding diabetes, including the widespread misconception that simply the use of more expensive insulin will translate into better health. As David Beran, Advisor to the Board for the International Insulin Foundation highlights, "in government tendering schemes, generic companies have the added disadvantage of no brand recognition."
There is understandably a desire and pressure amongst parents to seek what is perceived to be the best diabetes care for their children. In some of the type 1 diabetes communities in which I have worked in Latin America, you can often see the repercussions that the high prices of some branded drugs and supplies can have for families who cannot afford them. While many families or young people can manage their child's or their own diabetes well on a non-branded regimen of NPH and R (without the additional expense of branded insulin), others struggle to pay for branded insulin unnecessarily. It is not uncommon in some communities to see siblings of children with type 1 diabetes refuse food at home from time to time through concern that the money would be better spent on their brother or sister's diabetes supplies.
A lack of education is just as dangerous as a lack of insulin
For diabetes, access to insulin and other diabetes supplies is both obvious and critical, but living a full and productive life with diabetes is not assured without appropriate diabetes education and support. Unfortunately, over the years I have continued to witness the tragic and preventable consequences of a lack of diabetes education that can be equally debilitating as a lack of insulin.
The founding of AYUDA was in fact inspired by a young boy in Quito, Ecuador, who despite having access to insulin, was never in control of his diabetes. What was missing from the equation was the diabetes education component and just as importantly, a community for him and his family to connect to and learn from. Today, through partnerships with transparent local diabetes organizations, AYUDA is dedicated to developing and implementing sustainable diabetes programs using a youth-to- youth model. Through increasing access to diabetes supplies, coupled with locally appropriate, culturally sensitive diabetes education, our goal is to ensure no child dies or suffers preventable complications as a result of type 1 diabetes and furthermore that he or she is empowered to live a healthy and happy life with diabetes. As an organization AYUDA is dedicated to collaborating with local diabetes communities to develop and implement sustainable diabetes programs. AYUDA's peer learning model uses international volunteers as catalysts for motivating local young people with diabetes to live happy and healthy lives.
Despite the many advances that we see every day in medicine, the disparities in global healthcare spending for diabetes continue to be vast, with only 20% of global healthcare expenditures for diabetes going to low and middle income countries. As a result, it is fundamental that urgent action is taken with regard to increasing affordable access to diabetes treatment, education and support, in a sustainable and locally appropriate manner.
Wow. Thank you, Merith! For more on what AYUDA does, watch this video:
youtube
Disclaimer: Content created by the Diabetes Mine team. For more details click here.
Disclaimer
This content is created for Diabetes Mine, a consumer health blog focused on the diabetes community. The content is not medically reviewed and doesn't adhere to Healthline's editorial guidelines. For more information about Healthline's partnership with Diabetes Mine, please click here.
Type 2 Diabetes Treatment
Type 2 Diabetes Diet
Diabetes Destroyer Reviews
Original Article
0 notes
Text
The Startlingly High Cost Of The ‘Free’ Flu Shot
In the Byzantine world of health care pricing, most people wouldn’t expect that the ubiquitous flu shot could be a prime example of how the system’s lack of transparency can lead to disparate costs.
The Affordable Care Act requires health insurers to cover all federally recommended vaccines at no charge to patients, including flu immunizations. Although people with insurance pay nothing when they get their shot, many don’t realize that their insurers foot the bill — and that those companies will recoup their costs eventually.
In just one small sample from one insurer, Kaiser Health News found dramatic differences among the costs for its own employees. At a Sacramento, Calif., facility, the insurer paid $85, but just a little more than half that at a clinic in Long Beach. A drugstore in Washington, D.C., was paid $32.
The wide discrepancy in what insurers pay for the same flu shot illustrates what’s wrong with America’s health system, said Glenn Melnick, a health economist at the University of Southern California.
“There is always going to be some variance in prices, but $85 as a negotiated price sounds ridiculous,” he said.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
Flu shots are relatively cheap compared with most health services, but considering the tens of millions of Americans who get vaccinated each year, those prices add up.
Health plans pass those expenses to consumers through higher premiums, economists say.
“The patient is immune from the cost, but they are the losers because eventually they pay a higher premium,” said Ge Bai, an accounting and health policy professor at Johns Hopkins University’s campus in Washington, D.C.
Bai said the variation in payments for flu shots has nothing to do with the cost of the drug but is a result of negotiations between health plans and providers.
Typically, health insurers’ reimbursements to private health providers are closely guarded secrets. The insurers argue secrecy is needed for competitive business reasons.
But there’s one place those dollar figures appear for anyone to see: the “explanation of benefit” forms that insurers send to members after paying a claim.
KHN reviewed forms that one of its insurers, Cigna, paid for some colleagues to get flu shots this fall in Washington, D.C., and California.
Cigna paid $32 to CVS for a flu shot in downtown Washington and $40 to CVS less than 10 miles away in Rockville, Md.
In Southern California, Cigna paid $47.53 for a flu shot from a primary care doctor with MemorialCare in Long Beach. But it paid $85 for a shot given at a Sacramento doctors’ office affiliated with Sutter Health, one of the biggest hospital chains in the state.
Health experts were not surprised insurers paid Sutter more, though they were stunned just how much more.
“Sutter has huge clout in California, and insurers have no other option than to pay Sutter the price,” Bai said.
For years, Sutter has faced criticism that is uses its market dominance to charge higher rates. In October, it settled a lawsuit brought by the state attorney general, employers and unions that accused the hospital giant of illegally driving up prices.
The $85 was not just far more than what Cigna paid elsewhere but also more than triple the price Sutter advertises on its website for people without insurance: $25.
How does Sutter justify its higher prices as well as different prices for the same shot at the same location?
Sutter officials had no simple explanation. “Pricing can vary based on a number of factors, including the care setting, a patient’s insurance coverage and agreements with insurance providers,” Sutter said in a statement.
Cigna also said many issues are considered when determining its varied payments.
“What a plan reimburses a pharmacy/clinic/medical center for a flu vaccine depends on the plan’s contracted rate with that entity, which can be affected by a number of factors including location, number of available pharmacies/facilities in that area (a.k.a. competition), and even the size of the plan (a.k.a. potential customers),” Cigna said in a statement. “It is important to keep in mind that hospitals and pharmacies have different economics, including the cost to administer.”
It’s also noteworthy that Medicaid, the state-federal health insurance program covering more than 72 million low-income Americans, pays providers far less for a flu shot. In Washington, D.C., Medicaid pays $15. In Connecticut, $19.
Nationally, self-insured employers and insurers paid between $28 and $80 for the same type of flu shot administered in doctors’ offices in 2017, according to an analysis of more than 19 million claims of people under 65 years old by the Kaiser Family Foundation in partnership with the Peterson Center on Healthcare. (Kaiser Health News is an editorially independent program of the foundation.)
“Your health plan could end up paying more than double the cost for the same flu shot depending on where you get it,” said Cynthia Cox, a vice president at the foundation.
“We see the same pattern for more expensive services like MRIs or knee replacements,” she said. “That variation in prices is part of what’s driving insurance premiums higher in some parts of the country.”
The wide discrepancy in costs for the same service highlights a major problem in the U.S. health care system.
“We don’t have a functioning health care market because of all this lack of transparency and opportunities for price discrimination,” Melnick said.
“Prices are inconsistent and confusing for consumers,” he said. “The system is not working to provide efficient care, and the flu shot is one example of how these problems persist.”
An unintended consequence of the health law making flu shots free for insured patients is that health plans have little ability to direct patients to providers that offer the vaccine for less cost because patients have no reason to care, Bai said.
Around the country, retailers like Target and CVS offer various incentives such as gift cards and coupons to entice consumers to come in for their free flu shots in hopes they shop for other goods, too. Some hospital systems such as Baptist Health in South Florida have also started providing free flu shots for people without insurance.
Bai said that while hospitals like Baptist should be praised for helping improve the health of their communities, there are other factors in play.
“There is a hidden motivation to use free flu shots as a marketing tool to improve the hospital’s reputation,” she said. “If people come to the hospital for a flu shot, they may like the facility and come again.”
from Updates By Dina https://khn.org/news/the-startlingly-high-cost-of-the-free-flu-shot/
0 notes