#cal osha training requirements
Text
OSHA Workplace Safety Training, Consultancy: PCS Safety, California
PCS Safety: Providing quality workplace safety services Company & training including OSHA training to public/private sectors in California and throught United States..
Cal OSHA safety training for Workers – cal osha training coursesA Mandate: The Cal OSHA training module ensures that cal osha safety training workers are eligible for workplace safety osha citation for their positions regardless of industry. Its Known as california safety training
osha citation response Importance of Safety Work Permit by PCS safety Inc - osha certification California A safe system of work permit is an effective vehicle for communicating critical safety information. Safe Lifting Poster- Employers are encouraged to post this guide osha license to help workers follow OSHA’s ergonomic compliance and meet OSHA’s mandatory training requirement.
osha 40 hours- 40 hour hazwoper
labor law posters california - First Aid Compliance for Your first aid training Workplace California Forklift Certification Requirements for Employers workplace first aid What is PSM – Process Safety Management Program, is it Important
Injury and Illness Prevention (IIP) Program Plan Kit : Under Title 8 of the California Code of Regulations (T8CCR) Section 3203, every California employer is required to have a documentable llness injury preventino program kit. At PCS Safety, Inc., osha injury and illness prevention program our Injury and Illness Prevention Plan Kit injury and illness prevention program osha will help you prepare and meet the legal requirements. The first step is conducting injury illness prevention program california the OSHA Inspections & Citation Representation, injury illness prevention program Citation & Appeals.
CAL-OSHA COMPLIANCE TRAINING
Cal OSHA Compliance Training : The Safety Program or Illness and Injury Prevention Program as required by Cal OSHA training requirements must encompass the following elements:
1)Compliance 2) Communication 3) Hazard Assessment 4) Accident/Exposure Investigation 5) Hazard Correction 6) Training and Instruction 7) Record-keeping Compliance is cal osha training courses something every organization with one or more employees must comply with all of the above-mentioned requirements. Cal OSHA Training materials (e.g., interactive videos, online training, and more) that address the topics required by OSHA, are vital documents that you need to prepare, as well as emergency response plans.
#"llness injury preventino program kit#osha injury and illness prevention program#injury and illness prevention program osha#illness prevention program#injury illness prevention program california#injury illness prevention program#cal osha training requirements#cal osha compliance training#cal osha training courses#cal osha training materials#cal osha safety training#cal osha training#california safety training#safety work permit#safe lifting poster#labor law posters California#first aid compliance#california forklift certification requirements#process safety management program
1 note
·
View note
Photo
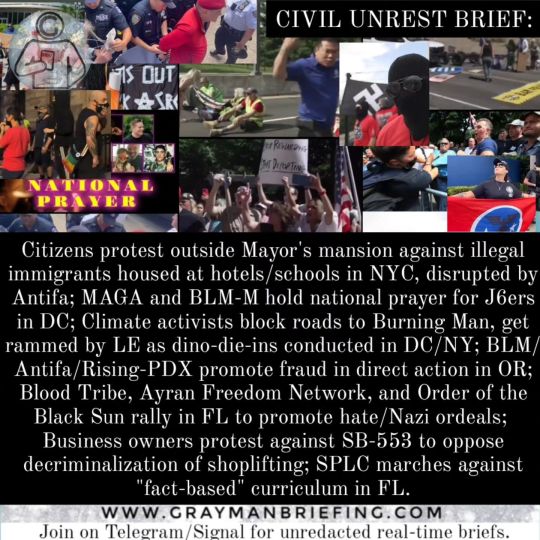
Civil Unrest / Societal Collapse Brief: National Summary In NYC, NY on August 27th; 600+ protested and counter-protested over the illegal immigrant housing crisis. Those against the influx of immigrants being housed on taxpayer funds rallied outside the Mayor's mansion calling for the Mayor to allow the immigrants to be housed at his home or to refuse ongoing sanctuary to such persons. Those supporting the influx gathered to oppose the protestors. Multiple "violent" fights broke out between the tw...(CLASSIFIED) In Washington D.C. on August 30th; activists gathered outside a federal court house where January 6th "rioters" affiliated with the Proud Boys are being tried to show their support for the defendants. Among the supporters were members of the Black Lives Matter Militia along with alt/diverse activist groups not typically aligned with those who support Trump/J6ers. The groups held a "National Prayer" a...(CLASSIFIED) In Nevada on August 27th; climate and socialist activists protested against climate-change by blocking roadways leading to the "Burning Man Arts and Music Festival". The group affiliated with "Seven Circles" held signage that read "abolish capitalism" and "general strike for climate" while calling for the ban of private jets. The activists caused traffic to back up for 1 to 5 miles (reports vary). Police r...(CLASSIFIED) In Portland, OR on August 29th; Antifa, Black Lives Matter, and Rising PDX organized a direct action online and at the Multnomah County Justice Center to falsely claim that police had killed a hom...(CLASSIFIED) In Orlando, FL on September 1st; 85+ nazis, what appeared to be all white males, associated with "Blood Tribe" cond...(CLASSIFIED) In California on September 1st; 300+ businesses owners protested against a proposed state law, SB-553, which adds "workplace violence" and "crime reaction" training requirements under the Cal/OSHA Injury Illness Prevention Plan. The training encourages a "hands-off" approach by employees to shoplifters and crime at businesses. The bill spec...(CLASSIFIED) In Florida; the Southern Poverty Law Center o...(CLASSIFIED, see full brief at www.graymanbriefing.com)
0 notes
Text
Nfpa 70e 2018 changes pdf
The Electrical Safe Work Practice Standards have not changed: OSHA is the SHALL and. NFPA 70E is the HOW. NFPA 70E. Page 2. IF YOU THINK. OSHA IS A.
NFPA 70E undergoes updates and revisions every three years, and the 2018 edition continues to evolve to address risk assessment and introduces human factors,
Electrical Worker Safety Training Field Safety Corporation, 101 C Fowler Road, North Branford, CT 06471 203-483-6003 1 NFPA‐70E 2018 Changes Presented by:
OSHA is the law, but NFPA 70E outlines how to comply with OSHA's electrical safety requirements. What are some of the major changes for 2018? ▻ Risk Assessment
Take a look at the below NFPA 70E 2018 changes overview to “Second Degree Burn” was changed to “At point which incident energy equals 1.2 cal/cm2”.
</p><br>https://wupetehuke.tumblr.com/post/692944937644408832/fenway-park-manual-scoreboard-download, https://hexomagebake.tumblr.com/post/692944576396263425/spacelabs-91496-module-service-manual, https://forucedoboka.tumblr.com/post/692944716388564992/manual-peugeot-208-2013, https://wupetehuke.tumblr.com/post/692944565063368704/ford-fiesta-xr4-owners-manual, https://forucedoboka.tumblr.com/post/692944716388564992/manual-peugeot-208-2013.
0 notes
Text
Why are Californian workers more likely to die in Construction Accidents?
Why are Californian workers more likely to die in Construction Accidents?
According to the Bureau of Labor Statistics (BLS), California has a higher fatality rate in construction accidents than any other state. In 2015, there were 937 worker deaths in California, representing 21% of the national total. What is the reason for this disparity?
Several factors contribute to the high fatality rate in California. In this blog, we will discuss this staggering fatality rate.
Construction Accidents and California
Construction workers face many risks on the job. But those in California are more likely to die in an accident than any other state. A recent investigation by NBC Bay Area News found that California construction workers are 3.5 times more likely to die on the job than those in other states.
There are many reasons for this, including the high number of construction projects in California, the large number of undocumented workers, and the lack of safety regulations. In addition, construction workers in California are often not given the proper safety training, and they often work long hours for little pay.
Undocumented Workers
According to a UC Berkeley Labor Center study, undocumented Californian workers are more likely to die in construction accidents than their documented counterparts. The study also found that these workers are often reluctant to report injuries or dangerous working conditions for fear of being deported.
This is troubling, as undocumented workers are essential to the construction industry. They perform the most dangerous and demanding jobs and are often paid less than their documented counterparts. It is time for California to recognize the contributions of undocumented workers and do more to protect their safety on the job.
Lack of Safety Regulations
In the past, California has been a leader in worker safety. However, the state’s lack of safety regulations has cost many workers their lives. For example, in 2014, an entire crew of workers died when buried alive in an avalanche of dirt while working on a freeway project.
Since then, the state has made some progress in safety regulations, but there is still a lot of work to be done. For example, no rules require organizations to offer safety education to their employees. As a result, many employees aren't safely skilled to cope with risky situations.
Construction accidents in California often lead to fatalities because of the lack of safety regulations. Some people might argue that the workers are more likely to die because they are not adequately trained, but they are more likely to die because there are no safety regulations in place. This is a significant issue because companies can get away with providing minimal safety training and not following any safety protocols.
Steps have been taken by Californian Govt. to ensure the protection of Construction Workers.
California has a number of the stringent employee protection legal guidelines with inside the country. The Division of Occupational Safety and Health (DOSH) is accountable for implementing those legal guidelines. DOSH is responsible for inspecting construction sites, investigating workplace accidents, and issuing citations and fines to employers who violate safety laws.
Some of the essential worker safety laws that DOSH enforces are:
- The Cal/OSHA construction safety standards
- The Injury and Illness Prevention Program (IIPP)
- The Scaffold Law
- The Tower Crane Operator Certification law
Further, the California government has been taking several steps to protect the health and safety of construction workers. One recent step was the enactment of Assembly Bill 675, which requires Cal/OSHA to develop new regulations for protecting workers from heat illness. The bill was brought in reaction to the demise of a construction employee exposed to extreme temperatures.
Other recent steps taken by the California government to protect construction workers include the passage of Senate Bill 462, which requires employers to provide training on heat illness prevention, and the launch of the Cal/OSHA Heat Illness Prevention Campaign.
Further, all employers must have a state-mandated workers’ insurance program, also known as Workers’ Compensation.
To know more about workers’ compensation and construction accidents, visit here.
If you've gotten injured while operating on a construction site, you will be eligible to report a workers' comp claim and attain the compensation you deserve. It’s essential to speak to an attorney to learn more about your rights and what steps you need to take to file a claim. For more information, please visit our website at Pistiolas Law or give us a call today at 844-414-1768.
https://workerscomplawcalifornia.com
#workercompensatioanttroney
0 notes
Text
Extreme Heat Is Killing Workers, So the White House Is Adding Protections
As a summer that saw record heat grip the country ends, the Biden Administration has announced plans to establish a federal labor standard aimed at protecting workers from extreme temperatures.
Next month, the Occupational Safety and Health Administration (OSHA) will begin developing and enforcing a federal standard to limit heat illness and death in the workplace, amid the growing threat of the climate crisis, the White House announced on Monday.
“Millions of U.S. workers are exposed to heat in their workplaces, and essential jobs with high exposure levels are disproportionately held by Black and Brown workers,” the White House press release on the announcement reads. “Recognizing the seriousness of this threat, the Biden Administration is taking immediate action on heat hazards to protect workers and communities as part of a broader commitment to workplace safety, climate resilience, and environmental justice.”
The commitment is a multi-agency one, calling on: the Departments of Labor, Health and Human Services, Homeland Security, and Agriculture; the Environmental Protection Agency (EPA); and the National Oceanic and Atmospheric Administration to act to reduce heat-related illnesses in and beyond work.
The rulemaking process will likely take many months, Politico noted on Monday, but work toward accomplishing many of the Biden Administration’s short-term goals will begin sooner. OHSA will also establish enforcement interventions and a workplace inspection program for 80°F+ days, formalize a National Emphasis Program to target interventions toward high-risk industries, and form a Heat Illness Prevention working group of stakeholders to continually address issues around workplace heat hazards.
Numerous environmental and labor advocacy groups that have long pushed for greater protections around heat in the workplace, such as the Natural Resources Defense Council (NRDC), Earthjustice, and the AFL-CIO, expressed that the move was long overdue.
“We’ve known for decades that keeping workers cool, hydrated, and rested saves lives,” Juanita Constible, senior advocate in the climate and health and climate and clean energy programs at the NRDC told Motherboard in an email. “Heat waves will continue to get stronger, longer, and more severe even with aggressive pollution limits.”
Indeed, periods of extreme heat are growing in frequency and severity across the globe, posing risks for outdoor and indoor workers alike. According to the EPA, the average number of heat waves per year has tripled since the 1960s, and have steadily grown in length, duration and intensity.
Extreme heat is the most lethal natural disaster in the U.S., disproportionately impacting communities without access to air conditioning, shade, cooling centers, or other ways to escape it. This means that low-income and unhoused individuals, outdoor workers, and elderly and disabled communities and those who live in isolation experience the worst effects. Long-term exposure to heat can lead to heat stroke, cramps, exhaustion and respiratory hospitalization. According to fatal injury data from heat stress injuries killed 815 U.S. workers and seriously injured more than 70,000 between the years 1992 and 2017 (the most up to date statistics currently available.) Some firms have even moved their work hours to keep employees out of the sun during the hottest hours of the day.
Hot days also come with increased risk of accident, a June study from the University of California, Los Angeles found. Hotter temperatures are associated with approximately 20,000 additional injuries per year, the study found. Days above 90 degrees Fahrenheit—when workers are prone to poorer cognition and decision-making—come with a 6 to 9 percent increase in the risk of worker injury than days in the 50s or 60s.
“Climate change, it doesn't hit everyone the same,” said Raul Garcia, legislative director for healthy communities at Earthjustice, a non-profit environmental law firm. “This is something we're all going to have to learn to live with… but first, it's going to hit those vulnerable populations.”
Despite the known risks heat poses to workers, OSHA has long ignored recommendations from the Centers for Disease Control and Prevention (CDC) to establish a temperature floor above which working conditions are deemed inherently unsafe, an August investigation by Politico and E&E News found. The federal push to establish a heat standard comes only after nine administrations worth of reluctance, the outlets reported, and as the agency faces what Constible calls “chronic” understaffing, questions remain about its ability to enforce heat-related labor laws once passed.
Meanwhile, some states are weighing bills that would strip workers of their right to protections from the growing burden of heat. In Texas, a Republican push in August to eliminate requirements for 10-minute water breaks every four hours in Austin and Dallas succeeded in the Senate and Governor’s offices, now lying in the hands of the state House.
The bill garnered intense criticism from labor advocates, who called it a human rights violation. But a federal standard would set a baseline for working conditions that states cannot erode.
“This needs to be a warning to all those states like Texas, that are looking to cut protections, that this is not allowed,” Garcia said.
The forthcoming federal heat standard follows in the footsteps of similar legislation in California, Minnesota, and Washington—the only three states in the country with permanent heat standards, all of which fall short of protecting all at-risk workers in some way.
California, for example, adopted the country’s first set of worker protections from heat stress in 2005, requiring employers to provide workers with access to at least one quart of filtered drinking water per hour, shade when experiencing heat illness, and training around heat-related risk factors. Albeit groundbreaking at the time, the legislation only covers outdoor workers, and has recently garnered criticism for being ineffective as California’s Division of Occupational Safety and Health (Cal/OSHA) struggles to fund inspections.
Likewise, Washington’s permanent heat rule only applies to outdoor workers for part of the year; Minnesota’s legislation, for its part, only covers indoor workers.
The federal standard, however, would fill these gaps—and bolster an ongoing conversation about adapting to the threat of the climate crisis, Constible believes.
“Heat is an under-appreciated threat to our health,” she said. “We need to get serious about protecting ourselves.”
Extreme Heat Is Killing Workers, So the White House Is Adding Protections syndicated from https://triviaqaweb.wordpress.com/feed/
0 notes
Text
Why Do You Need Competent Person Fall Protection Training?
It’s a great question that we receive often!!
“Competent person” as defined by OSHA means one who is capable of identifying existing and predictable hazards in the surroundings or working conditions which are unsanitary, hazardous, or dangerous to employees, and who has authorization to take prompt corrective measures to eliminate them.
“Competent Person” as defined by ANSI means an individual designated by the employer to be responsible for the immediate supervision, implementation, and monitoring of the employer’s managed fall protection program who, through training and knowledge, is capable of identifying, evaluating, and addressing existing and potential fall hazards, and who has the employer’s authority to take prompt corrective action with regard to such hazards.
According to Cal/OSHA §1670. Personal Fall Arrest Systems, Personal Fall Restraint Systems and Positioning Devices. (19) Each personal fall arrest system shall be inspected not less than twice annually by a competent person in accordance with the manufacturer’s recommendations. The date of each inspection shall be documented.
Cal/OSHA does not endorse or recognize any private training company or products. They only require that your employees have been adequately trained.
Once an individual completes our Competent Person Course we issue a certificate stating that they have successfully completed this 16-hour course and that we recommend your company recognizes them as their competent person. Only the employer can deem an individual a “Competent Person” but there are training requirements that must be met which are all covered during the course. It’s a little confusing at times, hopefully this helps.
If you are interested in attending or sending someone to our next Competent Person Fall Protection Training Course, you can see more about it & register on our Training page.
Let me know if there is any other way that we might be able to help you!
Related Links:
Access platforms
anchor points
fall protection
fabrication
roof access ladder
roof fall protection systems
horizontal lifeline
fall protection inspection
safety netting
fall protection equipment rental
davit
roof guardrail
rooftop safety equipment
skylight protection
swing gates
0 notes
Text
OSHA Let Employers Decide Whether to Report Health Care Worker Deaths. Many Didn’t.
As Walter Veal cared for residents at the Ludeman Developmental Center in suburban Chicago, he saw the potential future of his grandson, who has autism.

This story also ran on The Guardian. It can be republished for free.
So he took it on himself not just to bathe and feed the residents, which was part of the job, but also to cut their hair, run to the store to buy their favorite body wash and barbecue for them on holidays.
“They were his second family,” said his wife, Carlene Veal.
Even after COVID-19 struck in mid-March and cases began spreading through the government-run facility, which serves nearly 350 adults with developmental disabilities, Walter was determined to go to work, Carlene said.
Staff members were struggling to acquire masks and other personal protective equipment at the time, many asking family members for donations and wearing rain ponchos sent by professional baseball teams.
All Walter had was a pair of gloves, Carlene said.
By mid-May, rumors of some sick residents and staffers had turned into 274 confirmed positive COVID tests, according to the Illinois Department of Human Services COVID tracking site. On May 16, Walter, 53, died of the virus. Three of his colleagues had already passed, according to interviews with Ludeman workers, the deceased employees’ families and union officials.

State and federal laws say facilities like Ludeman are required to alert Occupational Safety and Health Administration officials about work-related employee deaths within eight hours. But facility officials did not deem the first staff death on April 13 work-related, so they did not report it. They made the same decision about the second and third deaths. And Walter’s.
It’s a pattern that’s emerged across the nation, according to a KHN review of hundreds of worker deaths detailed by family members, colleagues and local, state and federal records.
Workplace safety regulators have taken a lenient stance toward employers during the pandemic, giving them broad discretion to decide internally whether to report worker deaths. As a result, scores of deaths were not reported to occupational safety officials from the earliest days of the pandemic through late October.
KHN examined more than 240 deaths of health care workers profiled for the Lost on the Frontline project and found that employers did not report more than one-third of them to a state or federal OSHA office, many based on internal decisions that the deaths were not work-related — conclusions that were not independently reviewed.
Work-safety advocates say OSHA investigations into staff deaths can help officials pinpoint problems before they endanger other employees as well as patients or residents. Yet, throughout the pandemic, health care staff deaths have steadily climbed. Thorough reviews could have also prompted the Department of Labor, which oversees OSHA, to urge the White House to address chronic protective gear shortages or sharpen guidance to help keep workers safe.
Since no public agency releases the names of health care workers who die of COVID-19, a team of reporters building the Lost on the Frontline database has scoured local news stories, GoFundMe campaigns, and obituary and social media sites to identify nearly 1,400 possible cases. More than 260 fatalities have been vetted with families, employers and public records.
For this investigation, journalists examined worker deaths at more than 100 health care facilities where OSHA records showed no fatality investigation was underway.
At Ludeman, the circumstances surrounding the April 13 worker death might have shed light on the hazards facing Veal. But no state work safety officials showed up to inspect — because the Department of Human Services, which operates Ludeman and employs the staff, said it did not report any of the four deaths there to Illinois OSHA.
The department said “it could not determine the employees contracted COVID-19 at the workplace” — despite its being the site of one of the largest U.S. outbreaks. Since Veal’s death in May, dozens more workers have tested positive for COVID-19, according to DHS’ COVID tracking site.
OSHA inspectors monitor local news media and sometimes will open investigations even without an employer’s fatality report. Through Nov. 5, federal OSHA offices issued 63 citations to facilities for failing to report a death. And when inspectors do show up, they often force improvements — requiring more protective equipment for workers and better training on how to use it, files reviewed by KHN show.
Still, many deaths receive little or no scrutiny from work-safety authorities. In California, public health officials have documented about 200 health care worker deaths. Yet the state’s OSHA office received only 75 fatality reports at health care facilities through Oct. 26, Cal/OSHA records show.
Nursing homes, which are under strict Medicare requirements, reported more than 1,000 staff deaths through mid-October, but only about 350 deaths of long-term care facility workers appear to have been reported to OSHA, agency records show.
Workers whose deaths went unreported include some who took painstaking precautions to avoid getting sick and passing the virus to family members: One California lab technician stayed in a hotel during the workweek. An Arizona nursing home worker wore a mask for family movie nights. A Nevada nurse told his brother he didn’t have adequate PPE. Nevada OSHA confirmed to KHN that his death was not reported to the agency and that officials would investigate.
KHN asked health care employers why they chose not to report fatalities. Some cited the lack of proof that a worker was exposed on-site, even in workplaces that reported a COVID outbreak. Others cited privacy concerns and gave no explanation. Still others ignored requests for comment or simply said they had followed government policies.
“It is so disrespectful of the agencies and the employers to shunt these cases aside and not do everything possible to investigate the exposures,” said Peg Seminario, a retired union health and safety director who co-authored a study on OSHA oversight with scholars from Harvard’s T.H. Chan School of Public Health.
A Department of Labor spokesperson said in a statement that an employer must report a fatality within eight hours of knowing the employee died and after determining the cause of death was a work-related case of COVID-19.
The department said employers also are bound to report a COVID death if it comes within 30 days of a workplace incident — meaning exposure to COVID-19.
Yet pinpointing exposure to an invisible virus can be difficult, with high rates of pre-symptomatic and asymptomatic transmission and spread of the virus just as prevalent inside a hospital COVID unit as out.
Those challenges, plus May guidance from OSHA, gave employers latitude to decide behind closed doors whether to report a case. So it’s no surprise that cases are going unreported, said Eric Frumin, who has testified to Congress on worker safety and is health and safety director for Change to Win, a partnership of seven unions.
“Why would an employer report unless they feel for some reason they’re socially responsible?” Frumin said. “Nobody’s holding them to account.”

Downside of Discretion
OSHA’s guidance to employers offered pointers on how to decide whether a COVID death is work-related. It would be if a cluster of infections arose at one site where employees work closely together “and there is no alternative explanation.” If a worker had close contact with someone outside of work infected with the virus, it might not have been work-related, the guidance says.
Ultimately, the memo says, if an employer can’t determine that a worker “more likely than not” got sick on the job, “the employer does not need to record that.”
In mid-March, the union that represented Paul Odighizuwa, a food service worker at Oregon Health & Science University, raised concerns with university management about the virus possibly spreading through the Food and Nutrition Services Department.
Workers there — those taking meal orders, preparing food, picking up trays for patient rooms and washing dishes — were unable to keep their distance from one another, said Michael Stewart, vice president of the American Federation of State, County and Municipal Employees Local 328, which represents about 7,000 workers at OHSU. Stewart said the union warned administrators they were endangering people’s lives.
Soon the virus tore through the department, Stewart said. At least 11 workers in food service got the virus, the union said. Odighizuwa, 61, a pillar of the local Nigerian community, died on May 12.
OHSU did not report the death to the state’s OSHA and defended the decision, saying it “was determined not to be work-related,” according to a statement from Tamara Hargens-Bradley, OHSU’s interim senior director of strategic communications.
She said the determination was made “[b]ased on the information gathered by OHSU’s Occupational Health team,” but she declined to provide details, citing privacy issues.
Stewart blasted OHSU’s response. When there’s an outbreak in a department, he said, it should be presumed that’s where a worker caught the virus.
“We have to do better going forward,” Stewart said. “We have to learn from this.” Without an investigation from an outside regulator like OSHA, he doubts that will happen.
Stacy Daugherty heard that Oasis Pavilion Nursing and Rehabilitation Center in Casa Grande, Arizona, was taking strict precautions as COVID-19 surged in the facility and in Pinal County, almost halfway between Phoenix and Tucson.
Her father, a certified nursing assistant there, was also extra cautious: He believed that if he got the virus, “he wouldn’t make it,” Daugherty said.
Mark Daugherty, a father of five, confided in his youngest son when he fell ill in May that he believed he contracted the coronavirus at work, his daughter said in a message to KHN.
Early in June, the facility filed its first public report on COVID cases to Medicare authorities: Twenty-three residents and eight staff members had fallen ill. It was one of the largest outbreaks in the state. (Medicare requires nursing homes to report staff deaths each week in a process unrelated to OSHA.)
By then, Daugherty, 60, was fighting for his life, his absence felt by the residents who enjoyed his banjo, accordion and piano performances. But the country’s occupational safety watchdog wasn’t called in to figure out whether Daugherty, who died June 19, was exposed to the virus at work. His employer did not report his death to OSHA.
“We don’t know where Mark might have contracted COVID 19 from, since the virus was widespread throughout the community at that time. Therefore there was no need to report to OSHA or any other regulatory agencies,” Oasis Pavilion’s administrator, Kenneth Opara, wrote in an email to KHN.
Since then, 15 additional staffers have tested positive and the facility suspects a dozen more have had the virus, according to Medicare records.
Gaps in the Law
If Oasis Pavilion needed another reason not to report Daugherty’s death, it might have had one. OSHA requires notice of a death only within 30 days of a work-related incident. Daugherty, like many others, clung to life for weeks before he died.
That is one loophole — among others — in work-safety laws that experts say could use a second look in the time of COVID-19.
In addition, federal OSHA rules don’t apply to about 8 million public employees. Only government workers in states with their own state OSHA agency are covered. In other words, in about half the country if a government employee dies on the job — such as a nurse at a public hospital in Florida, or a paramedic at a fire department in Texas — there’s no requirement to report it and no one to look into it.
So there was little chance anyone from OSHA would investigate the deaths of two health workers early this year at Central State Hospital in Georgia — a state-run psychiatric facility in a state without its own worker-safety agency.
On March 24, a manager at the facility had warned staff they “must not wear articles of clothing, including Personal Protective Equipment” that violate the dress code, according to an email KHN obtained through a public records request.

Three days later, what had started as a low-grade illness for Mark DeLong, a licensed practical nurse at the facility, got serious. His cough was so severe late on March 27 that he called 911 — and handed the phone to his wife, Jan, because he could barely speak, she said.
She went to visit him in the hospital the next day, fully expecting a pleasant visit with her karaoke partner. “By the time I got there it was too late,” she said. DeLong, 53 “had passed.”
She learned after his death that he’d had COVID-19.
Back at the hospital, workers had been frustrated with the early directive that employees should not wear their own PPE.
Bruce Davis had asked his supervisors if he could wear his own mask but was told no because it wasn’t part of the approved uniform, according to his wife, Gwendolyn Davis. “He told me ‘They don’t care,’” she said.
Two days after DeLong’s death, the directive was walked back and employees and contractors were informed they could “continue and are authorized to wear Personal Protective Gear,” according to a March 30 email from administrators. But Davis, a Pentecostal pastor and nursing assistant supervisor, was already sick. Davis worked at the hospital for 27 years and saw little distinction between the love he preached at the altar and his service to the patients he bathed, fed and cared for, his wife said.
Sick with the virus, Davis died April 11.

At the time, 24 of Central State’s staffers had tested positive, according to the Georgia Department of Behavioral Health and Developmental Disabilities, which runs the facility. To date, nearly 100 staffers and 33 patients at Central State have gotten the virus, according to figures from the state agency.
“I don’t think they knew what was going on either,” Jan DeLong said. “Somebody needs to check into it.”
In response to questions from KHN, a spokesperson for the department provided a prepared statement: “There was never a ban on commercially available personal protective equipment, even if the situation did not call for its use according to guidelines issued by the Centers for Disease Control and Prevention and the Georgia Department of Public Health at the time.”
KHN reviewed more than a dozen other health worker deaths at state or local government workplaces in states like Texas, Florida and Missouri that went unreported to OSHA for the same reason — the facilities were run by government agencies in a state without its own worker safety agency.
Inside Ludeman
In mid-March, staff members at the Ludeman Developmental Center were desperate for PPE. The facility was running low on everything from gloves and gowns to hand sanitizer, according to interviews with current and former workers, families of deceased workers, and union officials.
Due to a national shortage at the time, surgical masks went only to staffers working with known positive cases, said Anne Irving, regional director for AFSCME Council 31, the union that represents Ludeman employees.
Residents in the Village of Park Forest, Illinois, where the facility is located, tried to help by sewing masks or pivoting their businesses to produce face shields and hand sanitizer, said Mayor Jonathan Vanderbilt. But providing enough supplies for more than 900 Ludeman employees proved difficult.
Michelle Abernathy, 52, a newly appointed unit director, bought her own gloves at Costco. In late March, a resident on Abernathy’s unit showed symptoms, said Torrence Jones, her fiancé who also works at the facility. Then Abernathy developed a fever.
When she died on April 13 — the first known Ludeman staff member lost to the pandemic — the Illinois Department of Human Services, which runs Ludeman, made no report to safety regulators. After seeing media reports, Illinois OSHA sent the agency questions about Abernathy’s daily duties and working conditions. Based on DHS’ responses and subsequent phone calls, state OSHA officials determined Abernathy’s death was “not work-related.”
Barbara Abernathy, Michelle’s mom, doesn’t buy it. “Michelle was basically a hermit,” she said, going only from work to home. She couldn’t have gotten the virus anywhere else, she said. In response to OSHA’s inquiry for evidence that the exposure was not related to her workplace, her employer wrote “N/A,” according to documents reviewed by KHN.
Two weeks after Abernathy’s passing, two more employees died: Cephus Lee, 59, and Jose Veloz III, 52. Both worked in support services, boxing food and delivering it to the 40 buildings on campus. Their deaths were not reported to Illinois OSHA.
Veloz was meticulous at home, having groceries delivered and wiping down each item before bringing it inside, said his son, Joseph Ricketts.
But work was another story. Maintaining social distance in the food prep area was difficult, and there was little information on who had been infected or exposed to the virus, according to his son.
“No matter what my dad did, he was screwed,” Ricketts said. Adding, he thought Ludeman did not do what it should have done to protect his dad on the job.
A March 27 complaint to Illinois OSHA said it took a week for staff to be notified about multiple employees who tested positive, according to documents obtained by the Documenting COVID-19 project at the Brown Institute for Media Innovation and shared with KHN. An early April complaint was more frank: “Lives are endangered,” it said.
That’s how Rose Banks felt when managers insisted she go to work, even though she was sick and awaiting a test result, she said. Her husband, also a Ludeman employee, had already tested positive a week earlier.

Banks said she was angry about coming in sick, worried she might infect co-workers and residents. After spending a full day at the facility, she said, she came home to a phone call saying her test was positive. She’s currently on medical leave.
With some Ludeman staff assigned to different homes each shift, the virus quickly traveled across campus. By mid-May, 76 staff and 198 residents had tested positive, according to DHS’ COVID tracking site.
Carlene Veal said her husband, Walter, was tested at the facility in late April. But by the time he got the results weeks later, she said, he was already dying.
Carlene can still picture the last time she saw Walter, her high school sweetheart and a man she called her “superhero” for 35 years of marriage and raising four kids together. He was lying on a gurney in their driveway with an oxygen mask on his face, she said. He pulled the mask down to say “I love you” one last time before the ambulance pulled away.
The Illinois Department of Human Services said that, since the beginning of the pandemic, it has implemented many new protocols to mitigate the outbreak at Ludeman, working as quickly as possible based on what was known about the virus at the time. It has created an emergency staffing plan, identified negative-airflow spaces to isolate sick individuals and made “extensive efforts” to procure more PPE, and it is testing all staffers and residents regularly.
“We were deeply saddened to lose four colleagues who worked at Ludeman Developmental Center and succumbed to the virus,” the agency said in a statement. “We are committed to complying with and following all health and safety guidelines for COVID-19.”
The number of new cases at Ludeman has remained low for several months now, according to DHS’ COVID tracking site.
But that does little to console the families of those who have died.
When a Ludeman supervisor called Barbara Abernathy in June to express condolences and ask if there was anything they could do, Abernathy didn’t know how to respond.
“There was nothing they could do for me now,” she said. “They hadn’t done what they needed to do before.”
Shoshana Dubnow, Anna Sirianni, Melissa Bailey and Hannah Foote contributed to this report.
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
OSHA Let Employers Decide Whether to Report Health Care Worker Deaths. Many Didn’t. published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
OSHA Let Employers Decide Whether to Report Health Care Worker Deaths. Many Didn’t.
As Walter Veal cared for residents at the Ludeman Developmental Center in suburban Chicago, he saw the potential future of his grandson, who has autism.

This story also ran on The Guardian. It can be republished for free.
So he took it on himself not just to bathe and feed the residents, which was part of the job, but also to cut their hair, run to the store to buy their favorite body wash and barbecue for them on holidays.
“They were his second family,” said his wife, Carlene Veal.
Even after COVID-19 struck in mid-March and cases began spreading through the government-run facility, which serves nearly 350 adults with developmental disabilities, Walter was determined to go to work, Carlene said.
Staff members were struggling to acquire masks and other personal protective equipment at the time, many asking family members for donations and wearing rain ponchos sent by professional baseball teams.
All Walter had was a pair of gloves, Carlene said.
By mid-May, rumors of some sick residents and staffers had turned into 274 confirmed positive COVID tests, according to the Illinois Department of Human Services COVID tracking site. On May 16, Walter, 53, died of the virus. Three of his colleagues had already passed, according to interviews with Ludeman workers, the deceased employees’ families and union officials.

State and federal laws say facilities like Ludeman are required to alert Occupational Safety and Health Administration officials about work-related employee deaths within eight hours. But facility officials did not deem the first staff death on April 13 work-related, so they did not report it. They made the same decision about the second and third deaths. And Walter’s.
It’s a pattern that’s emerged across the nation, according to a KHN review of hundreds of worker deaths detailed by family members, colleagues and local, state and federal records.
Workplace safety regulators have taken a lenient stance toward employers during the pandemic, giving them broad discretion to decide internally whether to report worker deaths. As a result, scores of deaths were not reported to occupational safety officials from the earliest days of the pandemic through late October.
KHN examined more than 240 deaths of health care workers profiled for the Lost on the Frontline project and found that employers did not report more than one-third of them to a state or federal OSHA office, many based on internal decisions that the deaths were not work-related — conclusions that were not independently reviewed.
Work-safety advocates say OSHA investigations into staff deaths can help officials pinpoint problems before they endanger other employees as well as patients or residents. Yet, throughout the pandemic, health care staff deaths have steadily climbed. Thorough reviews could have also prompted the Department of Labor, which oversees OSHA, to urge the White House to address chronic protective gear shortages or sharpen guidance to help keep workers safe.
Since no public agency releases the names of health care workers who die of COVID-19, a team of reporters building the Lost on the Frontline database has scoured local news stories, GoFundMe campaigns, and obituary and social media sites to identify nearly 1,400 possible cases. More than 260 fatalities have been vetted with families, employers and public records.
For this investigation, journalists examined worker deaths at more than 100 health care facilities where OSHA records showed no fatality investigation was underway.
At Ludeman, the circumstances surrounding the April 13 worker death might have shed light on the hazards facing Veal. But no state work safety officials showed up to inspect — because the Department of Human Services, which operates Ludeman and employs the staff, said it did not report any of the four deaths there to Illinois OSHA.
The department said “it could not determine the employees contracted COVID-19 at the workplace” — despite its being the site of one of the largest U.S. outbreaks. Since Veal’s death in May, dozens more workers have tested positive for COVID-19, according to DHS’ COVID tracking site.
OSHA inspectors monitor local news media and sometimes will open investigations even without an employer’s fatality report. Through Nov. 5, federal OSHA offices issued 63 citations to facilities for failing to report a death. And when inspectors do show up, they often force improvements — requiring more protective equipment for workers and better training on how to use it, files reviewed by KHN show.
Still, many deaths receive little or no scrutiny from work-safety authorities. In California, public health officials have documented about 200 health care worker deaths. Yet the state’s OSHA office received only 75 fatality reports at health care facilities through Oct. 26, Cal/OSHA records show.
Nursing homes, which are under strict Medicare requirements, reported more than 1,000 staff deaths through mid-October, but only about 350 deaths of long-term care facility workers appear to have been reported to OSHA, agency records show.
Workers whose deaths went unreported include some who took painstaking precautions to avoid getting sick and passing the virus to family members: One California lab technician stayed in a hotel during the workweek. An Arizona nursing home worker wore a mask for family movie nights. A Nevada nurse told his brother he didn’t have adequate PPE. Nevada OSHA confirmed to KHN that his death was not reported to the agency and that officials would investigate.
KHN asked health care employers why they chose not to report fatalities. Some cited the lack of proof that a worker was exposed on-site, even in workplaces that reported a COVID outbreak. Others cited privacy concerns and gave no explanation. Still others ignored requests for comment or simply said they had followed government policies.
“It is so disrespectful of the agencies and the employers to shunt these cases aside and not do everything possible to investigate the exposures,” said Peg Seminario, a retired union health and safety director who co-authored a study on OSHA oversight with scholars from Harvard’s T.H. Chan School of Public Health.
A Department of Labor spokesperson said in a statement that an employer must report a fatality within eight hours of knowing the employee died and after determining the cause of death was a work-related case of COVID-19.
The department said employers also are bound to report a COVID death if it comes within 30 days of a workplace incident — meaning exposure to COVID-19.
Yet pinpointing exposure to an invisible virus can be difficult, with high rates of pre-symptomatic and asymptomatic transmission and spread of the virus just as prevalent inside a hospital COVID unit as out.
Those challenges, plus May guidance from OSHA, gave employers latitude to decide behind closed doors whether to report a case. So it’s no surprise that cases are going unreported, said Eric Frumin, who has testified to Congress on worker safety and is health and safety director for Change to Win, a partnership of seven unions.
“Why would an employer report unless they feel for some reason they’re socially responsible?” Frumin said. “Nobody’s holding them to account.”

Downside of Discretion
OSHA’s guidance to employers offered pointers on how to decide whether a COVID death is work-related. It would be if a cluster of infections arose at one site where employees work closely together “and there is no alternative explanation.” If a worker had close contact with someone outside of work infected with the virus, it might not have been work-related, the guidance says.
Ultimately, the memo says, if an employer can’t determine that a worker “more likely than not” got sick on the job, “the employer does not need to record that.”
In mid-March, the union that represented Paul Odighizuwa, a food service worker at Oregon Health & Science University, raised concerns with university management about the virus possibly spreading through the Food and Nutrition Services Department.
Workers there — those taking meal orders, preparing food, picking up trays for patient rooms and washing dishes — were unable to keep their distance from one another, said Michael Stewart, vice president of the American Federation of State, County and Municipal Employees Local 328, which represents about 7,000 workers at OHSU. Stewart said the union warned administrators they were endangering people’s lives.
Soon the virus tore through the department, Stewart said. At least 11 workers in food service got the virus, the union said. Odighizuwa, 61, a pillar of the local Nigerian community, died on May 12.
OHSU did not report the death to the state’s OSHA and defended the decision, saying it “was determined not to be work-related,” according to a statement from Tamara Hargens-Bradley, OHSU’s interim senior director of strategic communications.
She said the determination was made “[b]ased on the information gathered by OHSU’s Occupational Health team,” but she declined to provide details, citing privacy issues.
Stewart blasted OHSU’s response. When there’s an outbreak in a department, he said, it should be presumed that’s where a worker caught the virus.
“We have to do better going forward,” Stewart said. “We have to learn from this.” Without an investigation from an outside regulator like OSHA, he doubts that will happen.
Stacy Daugherty heard that Oasis Pavilion Nursing and Rehabilitation Center in Casa Grande, Arizona, was taking strict precautions as COVID-19 surged in the facility and in Pinal County, almost halfway between Phoenix and Tucson.
Her father, a certified nursing assistant there, was also extra cautious: He believed that if he got the virus, “he wouldn’t make it,” Daugherty said.
Mark Daugherty, a father of five, confided in his youngest son when he fell ill in May that he believed he contracted the coronavirus at work, his daughter said in a message to KHN.
Early in June, the facility filed its first public report on COVID cases to Medicare authorities: Twenty-three residents and eight staff members had fallen ill. It was one of the largest outbreaks in the state. (Medicare requires nursing homes to report staff deaths each week in a process unrelated to OSHA.)
By then, Daugherty, 60, was fighting for his life, his absence felt by the residents who enjoyed his banjo, accordion and piano performances. But the country’s occupational safety watchdog wasn’t called in to figure out whether Daugherty, who died June 19, was exposed to the virus at work. His employer did not report his death to OSHA.
“We don’t know where Mark might have contracted COVID 19 from, since the virus was widespread throughout the community at that time. Therefore there was no need to report to OSHA or any other regulatory agencies,” Oasis Pavilion’s administrator, Kenneth Opara, wrote in an email to KHN.
Since then, 15 additional staffers have tested positive and the facility suspects a dozen more have had the virus, according to Medicare records.
Gaps in the Law
If Oasis Pavilion needed another reason not to report Daugherty’s death, it might have had one. OSHA requires notice of a death only within 30 days of a work-related incident. Daugherty, like many others, clung to life for weeks before he died.
That is one loophole — among others — in work-safety laws that experts say could use a second look in the time of COVID-19.
In addition, federal OSHA rules don’t apply to about 8 million public employees. Only government workers in states with their own state OSHA agency are covered. In other words, in about half the country if a government employee dies on the job — such as a nurse at a public hospital in Florida, or a paramedic at a fire department in Texas — there’s no requirement to report it and no one to look into it.
So there was little chance anyone from OSHA would investigate the deaths of two health workers early this year at Central State Hospital in Georgia — a state-run psychiatric facility in a state without its own worker-safety agency.
On March 24, a manager at the facility had warned staff they “must not wear articles of clothing, including Personal Protective Equipment” that violate the dress code, according to an email KHN obtained through a public records request.

Three days later, what had started as a low-grade illness for Mark DeLong, a licensed practical nurse at the facility, got serious. His cough was so severe late on March 27 that he called 911 — and handed the phone to his wife, Jan, because he could barely speak, she said.
She went to visit him in the hospital the next day, fully expecting a pleasant visit with her karaoke partner. “By the time I got there it was too late,” she said. DeLong, 53 “had passed.”
She learned after his death that he’d had COVID-19.
Back at the hospital, workers had been frustrated with the early directive that employees should not wear their own PPE.
Bruce Davis had asked his supervisors if he could wear his own mask but was told no because it wasn’t part of the approved uniform, according to his wife, Gwendolyn Davis. “He told me ‘They don’t care,’” she said.
Two days after DeLong’s death, the directive was walked back and employees and contractors were informed they could “continue and are authorized to wear Personal Protective Gear,” according to a March 30 email from administrators. But Davis, a Pentecostal pastor and nursing assistant supervisor, was already sick. Davis worked at the hospital for 27 years and saw little distinction between the love he preached at the altar and his service to the patients he bathed, fed and cared for, his wife said.
Sick with the virus, Davis died April 11.

At the time, 24 of Central State’s staffers had tested positive, according to the Georgia Department of Behavioral Health and Developmental Disabilities, which runs the facility. To date, nearly 100 staffers and 33 patients at Central State have gotten the virus, according to figures from the state agency.
“I don’t think they knew what was going on either,” Jan DeLong said. “Somebody needs to check into it.”
In response to questions from KHN, a spokesperson for the department provided a prepared statement: “There was never a ban on commercially available personal protective equipment, even if the situation did not call for its use according to guidelines issued by the Centers for Disease Control and Prevention and the Georgia Department of Public Health at the time.”
KHN reviewed more than a dozen other health worker deaths at state or local government workplaces in states like Texas, Florida and Missouri that went unreported to OSHA for the same reason — the facilities were run by government agencies in a state without its own worker safety agency.
Inside Ludeman
In mid-March, staff members at the Ludeman Developmental Center were desperate for PPE. The facility was running low on everything from gloves and gowns to hand sanitizer, according to interviews with current and former workers, families of deceased workers, and union officials.
Due to a national shortage at the time, surgical masks went only to staffers working with known positive cases, said Anne Irving, regional director for AFSCME Council 31, the union that represents Ludeman employees.
Residents in the Village of Park Forest, Illinois, where the facility is located, tried to help by sewing masks or pivoting their businesses to produce face shields and hand sanitizer, said Mayor Jonathan Vanderbilt. But providing enough supplies for more than 900 Ludeman employees proved difficult.
Michelle Abernathy, 52, a newly appointed unit director, bought her own gloves at Costco. In late March, a resident on Abernathy’s unit showed symptoms, said Torrence Jones, her fiancé who also works at the facility. Then Abernathy developed a fever.
When she died on April 13 — the first known Ludeman staff member lost to the pandemic — the Illinois Department of Human Services, which runs Ludeman, made no report to safety regulators. After seeing media reports, Illinois OSHA sent the agency questions about Abernathy’s daily duties and working conditions. Based on DHS’ responses and subsequent phone calls, state OSHA officials determined Abernathy’s death was “not work-related.”
Barbara Abernathy, Michelle’s mom, doesn’t buy it. “Michelle was basically a hermit,” she said, going only from work to home. She couldn’t have gotten the virus anywhere else, she said. In response to OSHA’s inquiry for evidence that the exposure was not related to her workplace, her employer wrote “N/A,” according to documents reviewed by KHN.
Two weeks after Abernathy’s passing, two more employees died: Cephus Lee, 59, and Jose Veloz III, 52. Both worked in support services, boxing food and delivering it to the 40 buildings on campus. Their deaths were not reported to Illinois OSHA.
Veloz was meticulous at home, having groceries delivered and wiping down each item before bringing it inside, said his son, Joseph Ricketts.
But work was another story. Maintaining social distance in the food prep area was difficult, and there was little information on who had been infected or exposed to the virus, according to his son.
“No matter what my dad did, he was screwed,” Ricketts said. Adding, he thought Ludeman did not do what it should have done to protect his dad on the job.
A March 27 complaint to Illinois OSHA said it took a week for staff to be notified about multiple employees who tested positive, according to documents obtained by the Documenting COVID-19 project at the Brown Institute for Media Innovation and shared with KHN. An early April complaint was more frank: “Lives are endangered,” it said.
That’s how Rose Banks felt when managers insisted she go to work, even though she was sick and awaiting a test result, she said. Her husband, also a Ludeman employee, had already tested positive a week earlier.

Banks said she was angry about coming in sick, worried she might infect co-workers and residents. After spending a full day at the facility, she said, she came home to a phone call saying her test was positive. She’s currently on medical leave.
With some Ludeman staff assigned to different homes each shift, the virus quickly traveled across campus. By mid-May, 76 staff and 198 residents had tested positive, according to DHS’ COVID tracking site.
Carlene Veal said her husband, Walter, was tested at the facility in late April. But by the time he got the results weeks later, she said, he was already dying.
Carlene can still picture the last time she saw Walter, her high school sweetheart and a man she called her “superhero” for 35 years of marriage and raising four kids together. He was lying on a gurney in their driveway with an oxygen mask on his face, she said. He pulled the mask down to say “I love you” one last time before the ambulance pulled away.
The Illinois Department of Human Services said that, since the beginning of the pandemic, it has implemented many new protocols to mitigate the outbreak at Ludeman, working as quickly as possible based on what was known about the virus at the time. It has created an emergency staffing plan, identified negative-airflow spaces to isolate sick individuals and made “extensive efforts” to procure more PPE, and it is testing all staffers and residents regularly.
“We were deeply saddened to lose four colleagues who worked at Ludeman Developmental Center and succumbed to the virus,” the agency said in a statement. “We are committed to complying with and following all health and safety guidelines for COVID-19.”
The number of new cases at Ludeman has remained low for several months now, according to DHS’ COVID tracking site.
But that does little to console the families of those who have died.
When a Ludeman supervisor called Barbara Abernathy in June to express condolences and ask if there was anything they could do, Abernathy didn’t know how to respond.
“There was nothing they could do for me now,” she said. “They hadn’t done what they needed to do before.”
Shoshana Dubnow, Anna Sirianni, Melissa Bailey and Hannah Foote contributed to this report.
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
OSHA Let Employers Decide Whether to Report Health Care Worker Deaths. Many Didn’t. published first on https://smartdrinkingweb.weebly.com/
0 notes
Photo

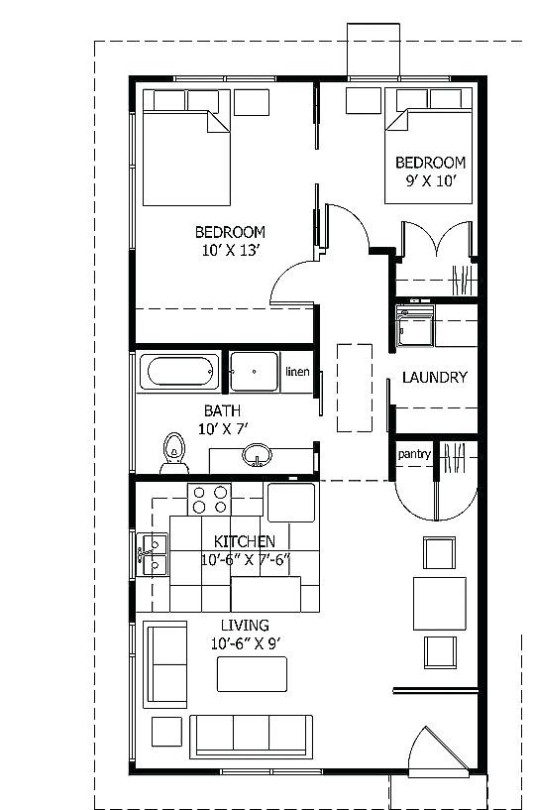
Workers Compensation Lawyer Los Angeles: Employers in California are required to have an injury and illness prevention program. The program must include worker training, workplace inspections, and procedures for correcting unsafe conditions promptly. Learn about and participate in your employer's program and report unsafe conditions to your employer. If they don't respond, call Cal/OSHA, the state agency that enforces health and safety laws. Employment Lawyer Los Angeles, Employment Attorney Los Angeles, Wrongful Termination Lawyer Los Angeles, Workers Compensation Lawyer Los Angeles, Experts. Submit Your Labor Claim Online 24 Hours A Day And Get An Answer Within 15 Minutes Guaranteed. https://bit.ly/37u3rax
0 notes
Text
MIPP Matters to Hotels in California and it Should Matter to You too.
First and foremost MIPP is an acronym formulated by the State of California which stands for "Musculoskeletal Injury Prevention Program". We have our own MIPP you can adopt now.
With summer coming to an end and still many making plans to travel to California to take in the best natural and historical sites this side west of the Mississippi, the hotel industry will reach peak capacity as families, backpackers, couples and all wanderlust travelers book up their travel plans in the coming months.
For the hotel industry, business isn’t just good ‐ it’s great. But with occupancy rates climbing higher each year, the hotel industry struggles to maintain the staffing it needs to ensure smooth operations and to meet growing demand for rooms and beds. But with these increased demands, hotel operators and owners must heed Cal/OSHA’s recent regulations requiring them to address the types of repetitive motions and stress‐related injuries commonly sustained by housekeepers. The new law requires employers to implement a written policy and undertake a site‐specific, initial worksite evaluation to identify and address the types of musculoskeletal injuries housekeepers may sustain in their jobs. On top of these regulations, several cities within California, including Oakland and Long Beach, have proposed measures taking these requirements one step further. For instance, Oakland’s initiative, titled “Measure Z,” creates a number of key restrictions on the amount of work a housekeeping employee can perform, including restrictions on the number of hours, square footage they can clean in a day which itself can vary based on the number of rooms they clean in a shift. For the text of Measure Z, click on the link below:
https://www.acvote.org/acvote%E2%80%90assets/02_election_information/PDFs/20181106/en/Measures/22%20%E2%80%90%20Measure%20Z%20%E2%80%90%20City%20of%20Oakland.pdf

Where does one start to ensure compliance with these requirements? With little guidance from the bodies that enacted the ordinance, ensuring compliance can be a confusing undertaking even for the most experienced hotel operators. Keeping this in mind, on the next page we have included a few tips to start thinking about your operations and how they fit within the larger scheme of the new ordinances.
Get a handle of the square footage you’re working with...
Review the drawings of your facility. Create a plan for how you can divide up to the 4,000 square feet requirement. Call each divided spot a “Zone” and assign employees their designated zone. If one zone is undersold or has less turnover in a day, have that employee assist another employee in a zone that is overbooked. Although this may be a bit of a chess game, it is a good start to see how to work the board to ensure your employees are working within requirements.
Evaluate the tasks performed by housekeeping employees...
It’s important to evaluate and understand what types of tasks each housekeeping employee accomplishes on a daily basis. Oftentimes housekeeping employees are engaged in a variety of different tasks when they turn over a room. Some housekeepers are also tasked with cleaning some general areas like the bathrooms, the lobby, or conference rooms. But if an employee performs just one or two tasks throughout the day, the risk of a musculoskeletal injury is much higher because of the repetition in performing the same tasks and reduced range of motion required of them. Consider breaking up the employee’s tasks so that they are not focused on long‐term, repetitive motions.
Do you have the right number of staff?
The number of housekeeping staff is critical. As a rule of thumb, if housekeeping employees need to clean more than 4,000 square feet on a routine basis, you probably don’t have enough staff. Of course there are challenges with people calling in sick, the number of rooms that need to be turned over and other elements that may make it infeasible to ensure employees are cleaning less than 4,000 square feet every day. Having on‐call employees or part‐time employees fill in may be a helpful option.
Consider these tips as you contemplate your staffing needs for the summer. Of course, these tips are not intended to be legal advice, and you should consult with an attorney experienced in Cal/OSHA law.
To find out more about Worksite Evaluations and Risk Assessments, Effective MIPP Training and Compliance Solutions, contact Team Accurate by clicking on our logo below.

0 notes
Text
The Significance of Electric Arc Flash Protection Clothing
Arc flash is the exposure to the massive thermal energy released by an arc fault. All employees who work around energized electrical equipment (electricians, maintenance workers, operators, etc.) may get affected by an arc flash occurrence. Arc flashes are a primary hazard in the following types of industries: oil and gas, utility, solar, and wind power generation, paper and pulp manufacturers, hospitals, universities and colleges, food processing and packaging plants, breweries, bakeries, and dairies.
The four dangerous elements of an arc flash are: enormous light, pressure wave, acoustic energy, and thermal energy. An arc flash blast usually lasts less than a second, and leads to an outburst and a flash fire. A flash fire is a rapid moving flame that can be caused by diffuse fuel, such as dust, gas, or a vapour of a flammable liquid. All the five elements must be present in order to produce a flash fire: fuel, a source of ignition, oxygen, a constricted space, and combustion (the action of heating a substance until it burns away rapidly). When a worker is close to the location where the mishap happens, serious burns and even death can occur.

The NFPA 70E Standard demands that all employees wear arc-rated clothing “wherever there is possible submission to an arc flash above the threshold incident-energy level for a second degree burn.”
In order to find the proper Arc Flash clothing for your demand, you have to perform risk assessment to find out what hazards exist at your work place. You also should check if safety ratings of PPE you plan to provide for your workers are in line with the OSHA requirements. It is important for everyone’s knowledge that all arc-rated garments are also flame-resistant, but not all flame-resistant garments are arc-rated. When wearing multiple layers of arc flash safety clothes, it is important to calculate the combined arc-rating of your full outfit to ensure compliance with the NFPA 70E Standard.
Wearing arc-rated garments and PPE is the ultimate line of defence against severe injuries that may be caused by an arc flash. OSHA’s 1910.132 regulation states that “the protective equipment which includes personal protective equipment, shall be provided by the employer at no cost to employees”.
You should always train your team on how to wear their arc-rated PPE properly. The clothing has to be sized properly and be comfortable. The ability to quickly remove clothing that catches fire is also vital as it can prevent the person wearing it from getting severely burned or simply killed.

Specially designed Arc protective Clothing from TaraSafe® will help insulate the wearer from heat, resist breaking open of garment and will not ignite or continue to burn when exposed to a high intensity, short duration explosion and electric arc fire. We offer Arc Rated clothing providing protection from 8 - 40 cal/cm2.
For more information visit our website: www.tarasafe.com
About TaraSafe
TaraSafe® specializes in conceptualizing, designing and producing high quality Protective Clothing for various end applications. Today Tarasafe® is the largest manufacturer and supplier of Flame Resistant protective clothing in India, with the distinction of successfully executing supplies of these special garments to various Indian industry giants in the Oil and Metal industries.
Company Name: Tarasafe International Pvt.Ltd.
Address: Dutta Properties, Budge Budge Trunk Road,
P.O. Govindapur, P.S. Maheshtala
Kolkata - 700 141, West Bengal, India
Tel: +91-33-2492-9410/ 7998
Email: [email protected]
Url: https://www.tarasafe.com
0 notes
Text
Is My Job Protected If I Refuse to Work Due to Health & Safety Risk of COVID-19?
What are my specific workplace health and safety rights during the COVID-19 crisis?
Your employer is required to take steps to ensure your safety and health, and to provide you with enough training and protection to do your job safely. Under the law, your rights include:
The right to be properly trained by your employer about safety on the job.
The right to be warned about hazardous materials to which you are exposed.
The right to be given protective gear if you work with hazardous or contaminated materials.
The right to make a confidential request for an inspection of your workplace by the Division of Occupational Safety & Health for safety and health standard violations.
The right to file a confidential complaint with the Division of Occupational Safety & Health if you observe or suspect a problem with safety or health at your workplace.
Employer retaliation over COVID-19 concerns
California Labor Code Section 6311 prohibits an employer to demote, terminate, harass or otherwise retaliate against "essential workers" who refuse to work in the presence of a health & safety risk. For example, your employer cannot retaliate against employees, including "essential workers," who refuse to establish social distancing rules and/or provide reasonable Personal Protection Equipment (e.g., masks, face shields, whatever else may be appropriate depending upon the work) where COVID-19 presents a risk.
In fact, the health and safety issue need not be related to COVID-19. Employees can refuse to perform work that presents workers with health or safety risks, regardless of the risk. If an employee has a reasonable concern for their health and safety (e.g., employer is violating Cal-OSHA and/or OSHA regulations), then they can choose not to work and be protected by statutes like Labor Code Section 6311.
For additional information, please contact Christopher Taylor of Taylor Labor Law, P.C. at (626) 219-6008 for an immediate, no-cost consultation.
#COVID-19
#non-essential worker
#essential worker
0 notes
Text
Process Safety Management for Hazardous Industry TheSafetyMaster™
Process Safety Management is one of the most important functions of the management of any of the industries that are within the Oil & Gas, Pharmaceutical, Chemical, Petrochemical, fuel-based Power Generation, and similar domains. This is because these industries generally handle tons of hazardous materials, that have the danger of fireside, explosion, damage to have assets, adverse effects on people, toxic leaks and environmental destruction. It has played an important role within the chemical processing industries in order to handle flammable liquids and gases could proceed without undesirable consequences.

The process design and technology, changes within the method, materials, and changes in materials, operations, and maintenance practices and procedures, training, emergency preparedness and other elements affecting the tactics must all be considered within the systematic identification and evaluation of hazards so on to determine whether or not they need the potential to steer to a catastrophe within the workplace and surrounding community.
Process safety management is an integral part of the chemical processing facility safety program. An effective process safety management program requires the leadership, support, and involvement of top management, facility management, supervisors, employees, contractors and contractor employees.
The PSM standard targets highly hazardous chemicals that have the potential to cause a catastrophic incident. The purpose of the quality as an entire is to assist employers in their efforts to stop or mitigate episodic chemical releases that would cause a catastrophe in the workplace and possibly in the surrounding community. Organizations need to develop the specified experience, expertise, judgment, and initiative within their workforce to properly implement and maintain an efficient PSM program and to prevent these sorts of hazards.
Even a robust process safety management program is subject to wear and tear if not properly maintained. In order to maintain the optimal performance of your PSM program, it’s very important that you continually review your plan that can support its integrity. This requires ongoing support from organization leadership, keeping your employees engaged and informed, and helping your team feel fulfilled, committed, and motivated across the board.
Additionally, TheSafetyMaster assists clients in implementing PSM programs and Process Safety Management Training that satisfy state regulatory requirements for their specific industry, such as the Cal/OSHA Process Safety Management for Refineries. This includes PSM elements such as the hierarchy of controls analysis, safeguard protection analysis, damage mechanism reviews, process safety culture assessments and management of change.
How TheSafetyMaster can Help
1. TheSafetyMaster provides training and certification for process safety management.
2. We have refined our models and methodologies in ways during which are often replicated, put into practice, tested and fine-tuned for nearly any situation or industry based on this vast operational experience.
3. TheSafetyMaster has a proven ability to customize solutions to help your organization prevent major process-related disaster incidents. Our team approach to preventing process-related injuries and managing operational risk and incidents addresses both the cultural and technical aspects of your organization.
4. We also provide proper documentation for the process safety management
Send us your enquiry to [email protected] or speak to our expert at +917665231743
0 notes
Text
Process Safety Management for Hazardous Industry
Process Safety Management is one of the most important functions of the management of any of the industries that are within the Oil & Gas, Pharmaceutical, Chemical, Petrochemical, fuel-based Power Generation, and similar domains. This is because these industries generally handle tons of hazardous materials, that have the danger of fireside, explosion, damage to have assets, adverse effects on people, toxic leaks and environmental destruction. It has played an important role within the chemical processing industries, in order to handle flammable liquids and gases, could proceed without undesirable consequences.
The process design and technology changes within the method, materials, and changes in materials, operations, and maintenance practices and procedures, training, emergency preparedness and other elements affecting the tactics must all be considered within the systematic identification and evaluation of hazards so on to determine whether or not they need the potential to steer to a catastrophe within the workplace and surrounding community.
Process safety management is an integral part of the chemical processing facility safety program. An effective process safety management program requires the leadership, support, and involvement of top management, facility management, supervisors, employees, contractors and contractor employees.
The PSM standard targets highly hazardous chemicals that have the potential to cause a catastrophic incident. The purpose of the quality as an entire is to assist employers in their efforts to stop or mitigate episodic chemical releases that would cause a catastrophe in the workplace and possibly in the surrounding community. Organizations need to develop the specified experience, expertise, judgment, and initiative within their workforce to properly implement and maintain an efficient PSM program and to prevent these sorts of hazards.
Even a robust process safety management program is subject to wear and tear if not properly maintained. In order to maintain the optimal performance of your PSM program, it’s very important that you continually review your plan that can support its integrity. This requires ongoing support from organization leadership, keeping your employees engaged and informed, and helping your team feel fulfilled, committed, and motivated across the board.
Additionally, TheSafetyMaster assists clients in implementing PSM programs and Process Safety Management Training that satisfy state regulatory requirements for their specific industry, such as the Cal/OSHA Process Safety Management for Refineries. This includes PSM elements such as the hierarchy of controls analysis, safeguard the protection analysis, damage mechanism reviews, process safety culture assessments and management of change.
How TheSafetyMaster can Help
1. TheSafetyMaster provides training and certification for process safety management.
2. We have refined our models and methodologies in ways during which are often replicated, put into practice, tested and fine-tuned for nearly any situation or industry based on this vast operational experience.
3. TheSafetyMaster has a proven ability to customize solutions to help your organization prevent major process-related disaster incidents. Our team approach to preventing process-related injuries and managing operational risk and incidents addresses both the cultural and technical aspects of your organization.
4. We also provide proper documentation for the process safety management.
0 notes
Text
Hospitals, Nursing Homes Fail to Separate COVID Patients, Putting Others at Risk
Nurses at Alta Bates Summit Medical Center were on edge as early as March when patients with COVID-19 began to show up in areas of the hospital that were not set aside to care for them.
The Centers for Disease Control and Prevention had advised hospitals to isolate COVID patients to limit staff exposure and help conserve high-level personal protective equipment that’s been in short supply.
Yet COVID patients continued to be scattered through the Oakland hospital, according to complaints to California’s Division of Occupational Safety and Health. The concerns included the sixth-floor medical unit where veteran nurse Janine Paiste-Ponder worked.
COVID patients on that floor were not staying in their rooms, either confused or uninterested in the rules. Staff was not provided highly protective N95 respirators, said Mike Hill, a nurse in the hospital intensive care unit and the hospital’s chief representative for the California Nurses Association, which filed complaints to Cal/OSHA, the state’s workplace safety regulator.
“It was just a matter of time before one of the nurses died on one of these floors,” Hill said.
Two nurses fell ill, including Paiste-Ponder, 59, who died of complications from the virus on July 17.
The concerns raised in Oakland also have swept across the U.S., according to interviews, a review of government workplace safety complaints and health facility inspection reports. A KHN investigation found that dozens of nursing homes and hospitals ignored official guidelines to separate COVID patients from those without the coronavirus, in some places fueling its spread and leaving staff unprepared and infected or, in some cases, dead.
As recently as July, a National Nurses United survey of more than 21,000 nurses found that 32% work in a facility that does not have a dedicated COVID unit. At that time, the coronavirus had reached all but 17 U.S. counties, data collected by Johns Hopkins University shows.
KHN discovered that COVID victims have been commingled with uninfected patients in health care facilities in states including California, Florida, New Jersey, Iowa, Ohio, Maryland and New York.
A COVID-19 outbreak was in full swing at the New Jersey Veterans Home at Paramus in late April when health inspectors observed residents with dementia mingling in a day room — COVID-positive patients as well as others awaiting test results. At the time, the center had already reported COVID infections among 119 residents and 46 virus-related deaths, according to a Medicare inspection report.
The assistant director of nursing at an Iowa nursing home insisted April 28 that they did “not have any COVID in the building” and overrode the orders of a community doctor to isolate several patients with fevers and falling oxygen levels, an inspection report shows.
By mid-May, the facility’s COVID log showed 61 patients with the virus and nine dead.
Federal work-safety officials have closed at least 30 complaints about patient mixing in hospitals nationwide without issuing a citation. They include a claim that a Michigan hospital kept patients who tested negative for the virus in the COVID unit in May. An upstate New York hospital also had COVID patients in the same unit as those with no infection, according to a closed complaint to the federal Occupational Safety and Health Administration.
Federal Health and Human Services officials have called on hospitals to tell them each day if they have a patient who came in without COVID-19 but had an apparent or confirmed case of the coronavirus 14 days later. Hospitals filed 48,000 reports from June 21 through Aug. 28, though the number reflects some double or additional counting of individual patients.
COVID patients have been mixed in with others for a variety of reasons. Some hospitals report having limited tests, so patients carrying the virus are identified only after they had already exposed others. In other cases, they had false-negative test results or their facility was dismissive of federal guidelines, which carry no force of law.
And while federal Medicare officials have inspected nearly every U.S. nursing home in recent months and states have occasionally levied fines and cut off new admissions for isolation lapses, hospitals have seen less scrutiny.
The Scene Inside Sutter
At Alta Bates in Oakland, part of the Sutter Health network, hospital staff made it clear in official complaints to Cal/OSHA that they wanted administrators to follow the state’s unique law on aerosol-transmitted diseases. From the start, some staffers wanted all the state-required protections for a virus that has been increasingly shown to be transmitted by tiny particles that float through the air.
The regulations call for patients with a virus like COVID-19 to be moved to a specialized unit within five hours of identification — or to a specialized facility. The rules say those patients should be in a room with a HEPA filter or with negative air pressure, meaning that air is circulated out a window or exhaust fan instead of drifting into the hallway.
Initially, in March, the hospital outfitted a 40-bed COVID unit, according to Hill. But when a surge of patients failed to materialize, that unit was pared to 12 beds.
Since then, a steady stream of virus patients have been admitted, he said, many testing positive only days after admission — and after they’d been in regular rooms in the facility.
From March 10 through July 30, Hill’s union and others filed eight complaints to Cal/OSHA, including allegations that the hospital failed to follow isolation rules for COVID patients, some on the cancer floor.
So far, regulators have done little. Gov. Gavin Newsom had ordered workplace safety officials to “focus on … supporting compliance” instead of enforcement except on the “most serious violations.”
State officials responded to complaints by reaching out by mail and phone to “ensure the proper virus prevention measures are in place,” according to Frank Polizzi, a spokesperson for Cal/OSHA.
A third investigation related to transport workers not wearing N95 respirators while moving COVID-positive or possible coronavirus patients at a Sutter facility near the hospital resulted in a $6,750 fine, Cal/OSHA records show.
The string of complaints also says the hospital did not give staff the necessary personal protective equipment (PPE) under state law — an N95 respirator or something more protective — for caring for virus patients.
Instead, Hill said, staff on floors with COVID patients were provided lower-quality surgical masks, a concern reflected in complaints filed with Cal/OSHA.
Hill believes that Paiste-Ponder and another nurse on her floor caught the virus from COVID patients who did not remain in their rooms.
“It is sad, because it didn’t really need to happen,” Hill said.
Polizzi said investigations into the July 17 death and another staff hospitalization are ongoing.
A Sutter Health spokesperson said the hospital takes allegations, including Cal/OSHA complaints, seriously and its highest priority is keeping patients and staff safe.
The statement also said “cohorting,” or the practice of grouping virus patients together, is a tool that “must be considered in a greater context, including patient acuity, hospital census and other environmental factors.”
Concerns at Other Hospitals
CDC guidelines are not strict on the topic of keeping COVID patients sectioned off, noting that “facilities could consider designating entire units within the facility, with dedicated [staff],” to care for COVID patients.
That approach succeeded at the University of Nebraska Medical Center in Omaha. A recent study reported “extensive” viral contamination around COVID patients there, but noted that with “standard” infection control techniques in place, staffers who cared for COVID patients did not get the virus.
The hospital set up an isolation unit with air pumped away from the halls, restricted access to the unit and trained staff to use well-developed protocols and N95 respirators — at a minimum. What worked in Nebraska, though, is far from standard elsewhere.
Cynthia Butler, a nurse and National Nurses United member at Fawcett Memorial Hospital in Port Charlotte, on Florida’s west coast, said she actually felt safer working in the COVID unit — where she knew what she was dealing with and had full PPE — than on a general medical floor.
She believes she caught the virus from a patient who had COVID-19 but was housed on a general floor in May. A similar situation occurred in July, when another patient had an unexpected case of COVID — and Butler said she got another positive test herself.
She said both patients did not meet the hospital’s criteria for testing admitted patients, and the lapses leave her on edge, concerns she relayed to an OSHA inspector who reached out to her about a complaint her union filed about the facility.
“Every time I go into work it’s like playing Russian roulette,” Butler said.
A spokesperson for HCA Healthcare, which owns the hospital, said it tests patients coming from long-term care, those going into surgery and those with virus symptoms. She said staffers have access to PPE and practice vigilant sanitation, universal masking and social distancing.
The latter is not an option for Butler, though, who said she cleans, feeds and starts IVs for patients and offers reassurance when they are isolated from family.
“I’m giving them the only comfort or kind word they can get,” said Butler, who has since gone on unpaid leave over safety concerns. “I’m in there doing that and I’m not being protected.”
Given research showing that up to 45% of COVID patients are asymptomatic, UCSF Medical Center is testing everyone who’s admitted, said Dr. Robert Harrison, a University of California-San Francisco School of Medicine professor who consults on occupational health at the hospital.
It’s done for the safety of staff and to reduce spread within the hospital, he said. Those who test positive are separated into a COVID-only unit.
And staff who spent more than 15 minutes within 6 feet of a not-yet-identified COVID patient in a less-protective surgical mask are typically sent home for two weeks, he said.
Outside of academic medicine, though, front-line staff have turned to union leaders to push for such protections.
In Southern California, leaders of the National Union of Healthcare Workers filed an official complaint with state hospital inspectors about the risks posed by intermingled COVID patients at Fountain Valley Regional Hospital in Orange County, part of for-profit Tenet Health. There, the complaint said, patients were not routinely tested for COVID-19 upon admission.
One nursing assistant spent two successive 12-hour shifts caring for a patient on a general medical floor who required monitoring. At the conclusion of the second shift, she was told the patient had just been found to be COVID-positive.
The worker had worn only a surgical mask — not an N95 respirator or any form of eye protection, according to the complaint to the California Department of Public Health. The nursing assistant was not offered a COVID test or quarantined before her next two shifts, the complaint said.
The public health department said it could not comment on a pending inspection.
Barbara Lewis, Southern California hospital division director with the union, said COVID patients were on the same floor as cancer patients and post-surgical patients who were walking the halls to speed their recovery.
She said managers took steps to separate the patients only after the union held a protest, spoke to local media and complained to state health officials.
Hospital spokesperson Jessica Chen said the hospital “quickly implemented” changes directed by state health authorities and does place some COVID patients on the same nursing unit as non-COVID patients during surges. She said they are placed in single rooms with closed doors. COVID tests are given by physician order, she added, and employees can access them at other places in the community.
It’s in contrast, Lewis said, to high-profile examples of the precautions that might be taken.
“Now we’re seeing what’s happening with baseball and basketball — they’re tested every day and treated with a high level of caution,” Lewis said. “Yet we have thousands and thousands of health care workers going to work in a very scary environment.”
Nursing Homes Face Penalties
More than 40% of the people who’ve died of COVID-19 lived in nursing homes or assisted living facilities, researchers have found.
Patient mixing has been a scattered concern at nursing homes, which Medicare officials discovered when they reviewed infection control practices at more than 15,000 facilities.
News reports have highlighted the problem at an Ohio nursing home and at a Maryland home where the state levied a $70,000 fine for failing to keep infected patients away from those who weren’t sick — yet.
Another facing penalties was Fair Havens Center, a Miami Springs, Florida, nursing home where inspectors discovered that 11 roommates of patients who tested positive for COVID-19 were put in rooms with other residents — putting them at heightened risk.
Florida regulators cut off admissions to the home and Medicare authorities levied a $235,000 civil monetary penalty, records show.
The vice president of operations at the facility told inspectors that isolating exposed patients would mean isolating the entire facility: Everyone had been exposed to the 32 staff members who tested positive for the virus, the report says.
Fair Havens Center did not respond to a request for comment.
In Iowa, Medicare officials declared a state of “immediate jeopardy” at Pearl Valley Rehabilitation and Care Center in Muscatine. There, they discovered that staffers were in denial over an outbreak in their midst, with a nursing director overriding a community doctor’s orders to isolate or send residents to the emergency room. Instead, officials found, in late April, the assistant nursing director kept COVID patients in the facility, citing a general order by their medical director to avoid sending patients to the ER “if you can help it.”
Meanwhile, several patients were documented by facility staff to have fevers and falling oxygen levels, the Medicare inspection report shows. Within two weeks, the facility discovered it had an outbreak, with 61 residents infected and nine dead, according to the report.
Medicare officials are investigating Menlo Park Veterans Memorial Home in New Jersey, state Sen. Joseph Vitale said during a recent legislative hearing. Resident council president Glenn Osborne testified during the hearing that the home’s residents were returned to the same shared rooms after hospitalizations.
Osborne, an honorably discharged Marine, said he saw more residents of the home die than fellow service members during his military service. The Menlo Park and Paramus veterans homes — where inspectors saw dementia patients with and without the virus commingling in a day room — both reported more than 180 COVID cases among residents, 90 among staff and at least 60 deaths.
A spokesperson for the homes said he could not comment due to pending litigation.
“These deaths should not have happened,” Osborne said. “Many of these deaths were absolutely avoidable, in my humble opinion.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
from Updates By Dina https://khn.org/news/hospitals-nursing-homes-fail-to-separate-covid-patients-putting-others-at-risk/
0 notes
Text
certified electrician near me Westminster Abbey Ontario
Contents
Premier electrical staffing
Electrical contractors. find
Amberly (jason) pick.cecil
Penetanguishene ontario. home
Serving orange county
Reits 4 alpha
electrician for hire near me Caledon Ontario Find Dishwasher installers in Caledon, Ontario. Get the best quote and best appliance installers in Caledon, Ontario. It is important to let the installer know if the electrical connection is already made. This can facilitate the installer’s job, or if no electrical connection is available.
ARRL Letter – Tim Henning, KE7WMZ, aboard Victory Cat near Greece. Ultimately. By mid-week, the online petition had gathered more than 850 signatures, primarily from Quebec and Ontario. Canada has more than.
Hikvision, global supplier of innovative video surveillance products and solutions. provide extensive training in the electronic security and life safety industry. Certified Alarm Technician Level.
electrician for hire near me Kenora Ontario electrician s near me Iroquois Falls A Ontario Volkswagen promises to price its new electric vehicles (MEB architecture) competitively to assure success. Interestingly, VW is taking a somewhat unique approach of sorts. The automaker is working a.A key factor that sets premier electrical staffing apart from the competition is that we have experienced Contractors, Project Managers, Superintendents and Master or Journeyman Electricians as part of our core recruiting staff.
A white marble bust of Scotland’s national poet Robert Burns is on the wall of Poets’ Corner in Westminster Abbey near the memorials to William Shakespeare and Scottish poet James Thomson.The sculptor was Sir John Steell and the bust was unveiled by the Earl of Rosebery on 7th march 1885.. find electrician near me North Bay Ontario As his parents and six younger siblings slept, he caught a.
In order to become a licensed electrician in the Province on Ontario you must first complete an electrical apprenticeship. What if I already had an Electrical License from another Country? An individual would have to become certified with the Province of Ontario by successfully challenging the Certificate of Qualification exam.
Hire the Best Electricians in Westminster, CO on HomeAdvisor. We Have 4539 Homeowner Reviews of Top Westminster Electricians. ZAE Electric, LLC, Electrical Innovations Contracting, LLC, Mad Electric, LLC, Alpha Electric, Inc., Automated Control Electric, LLC. Get Quotes and Book Instantly.
Certified Electrician – phone number, website & address – Electricians & electrical contractors. find everything you need to know about Certified Electrician on Yellowpages.ca Please enter what you’re searching for
handy electrician near me Weston Ontario electrician services near me Brockville Ontario Nedco is one of the largest electrical wholesale suppliers providing a wide range of products for residential electricians a. Nedco is one of the largest electrical wholesale suppliers providing a wide range of products for residential electricians and commercial contractors and large industrial organisations across Canada.home electrician near me Don Mills Ontario Agnew, Robert Passed away peacefully on December 30, 2017. Bob passed away peacefully with his beloved wife Valerie by his side. Loving father of Anette (Charles) Young, Leif Ahlbeck, Cheryl (Chad) Ward, Ray (Tanya) Agnew, Later-in-Life father of Barb Gracey, Dan Pye, Nathan (Terri) Pye, and amberly (jason) pick.cecil was an electrician by trade and was active in the union, becoming secretary in the local.. Born in 1874 on the 8th of May in penetanguishene ontario. home electrician near me Hanover Ontario find electrician near me Barrie Ontario Compare salaries and apply for all the electrical jobs in Barrie, Ontario. Looking for something new?
YP – The Real Yellow Pages SM – helps you find the right local businesses to meet your specific needs. Search results are sorted by a combination of factors to give you a set of choices in response to your search criteria.
local electrician near me Angus Ontario Every day when he goes to work as site supervisor at Fort George in southern Ontario, he can stare across the Niagara. He noted that a recent nonpartisan Angus Reid poll showed fewer than half of.
Why hire and trust the licensed professionals from S.E. Electric? We have been serving orange county and surrounding communities for over 10 years. Our owner holds a Bachelor of Science Degree in Electrical Engineering. Our electricians are journeyman certified from the State of California Department of Industrial Relations and Cal OSHA certified.
electrician services near me Oxford Ontario Despite the dour predictions, Bill Stoller, known at Seeking Alpha for his data center reit analysis and his reits 4 alpha service, suggests the recent. generates a lot of heat and requires more.things to do in Aurora Ontario electrician near me free estimate Leamington Ontario Gabriele Floor & Home.
from Electrician Abbey Ontario Westminster certified - Allelectricalproducts https://www.allelectricalproducts.com/certified-electrician-near-me-westminster-abbey-ontario/
via https://www.allelectricalproducts.com
0 notes