Conversation
table rounding w hangry
Me: Alrighty, in Room 1, we have Mr. Smith. He is a 63y/o male with a history of Afib and Takotsubo cardiomyopathy who presented with flash pulmonary edema and DVT. Cardiology is following. Following extensive diuresis and an increase in his home metoprolol, he is no longer in RVR and now satting mid-90s on room air. Once we get the prior auth on his Lovenox, he can go home.
Attending: Perfect.
Me: He also has an adorable bulldog at home.
Attending: Ah.
Me: Okay, next up in Room 2, we have Ms. Jones. She is a 74y/o female who received allogeneic stem cell transplant about 2 months ago and presented with rash and diarrhea suspicious for diarrhea. Heme/Onc is following. She is on Methylprednisolone with significant improvement in stool volume, now putting less than 500ml out. Her rash originally was ~50% BSA and is now about 20%. She will be discharged on Prednisone taper, pending Heme/Onc recs.
Attending: Good.
Me: And she has a little goldendoodle at home.
Attending: Nice.
Me: All right. Then in Room 3 is Ms. Williams. She is a 67y/o female who presented with urosepsis secondary to new kidney stone. She's had a wild hospital course and was extubated just 2 days ago. It appears that she also is now deaf. We've consulted ENT, and they suspect vestibular neuritis. I reached out to them to ask about starting steroids. She likely will not be returning home for at least another 48hrs while we sort this out.
Attending: I see.
Me: She has a giant derpy mutt at home.
Attending: I take it that you like dogs.
Surrounding coworkers: [in unison] YEP!
48 notes
·
View notes
Photo
@populationpensive










Chris Evans + instagram highlights 2020
5K notes
·
View notes
Photo
14 Hilariously Flawless Responses To Dudes Asking For Nudes
2K notes
·
View notes
Text
s/p first year as a PA
I was hired as a hospitalist primarily for the transplant service. However, in the setting of the pandemic and staffing shortages, I am all over the place now and work in almost everything non-pediatric and non-surgical.
In my first few months as a PA, I was incredibly overwhelmed. I went from being a learner who switches specialties every month to a fully-fledged provider making life-or-death decisions on an hourly basis. Oftentimes I’d find myself in the room of a patient actively crumping, surrounded by the patient’s family and multiple nurses awaiting instructions on what to do to save the patient. I thought that I faced a lot of pressure in school, but it was nothing compared to this.
And just when I started to get a hang of it all, the pandemic hit. What a nightmare. As mentioned above, I was hired to work with with transplant patients. Prior to the pandemic, my transplant colleagues and I were masking and gowning for almost every patient: 1 surgical mask and 1 gown per patient and per patient encounter. But once COVID hit, we were rationing PPE. 1 N95, 1 pair of goggles, and 1 face shield for the pandemic. 1 surgical mask per week, and 1 gown only if a patient had Cdiff or a history of MDRO bacteremia.
What did the pandemic mean for our transplant patients?
Our patients are on immunosuppressant medications to prevent transplant rejection. Unfortunately, this makes it difficult for them to fight infections.
Our department did what it could to prevent COVID. We'd test patients on admission for COVID, regardless of symptoms or exposure history. If they were positive, they went to the COVID team and quarantined on their unit for a period of time and had to test negative before returning to our unit and being transplanted. We took many other measures to reduce COVID risk to the best of our ability.
People still died. To see someone get transplanted successfully and then die of a virus is horrifying. Unfortunately, despite our admission tests, sometimes patients contracted COVID within the hospital. Patients would be happily FaceTiming their family one moment, telling them all of their plans for once they were discharged- then the next day they'd be intubated. We tried Remdesivir, Dexamethasone, prone positioning, etc. But the virus moved through them quickly, and these efforts often were too late. No amount of hoping and praying brought them back.
As a first year PA, I learned to go to an empty conference room, close the door, and remove my mask before calling to the family of the deceased. This way, as they gathered around the phone in their homes, the family could hear me unmuffled as I delivered the news. Also, this way my tears didn't ruin my mask for the rest of the week.
I learned a lot this year. It's been a mixture of crying and laughing. There are times that I question why I ever became a PA, and then there are times when this career feels like home. In addition to transplant, I’ve also been working in the ED, IMC, ICU, inpatient hospice, clinic, and infusion center these past 6 months. I’ve learned quite a lot along the way.
Lessons learned as a first year PA:
1. Check your pager hourly: This is in addition to checking it whenever you get paged. Sometimes I’ll get paged while I’m rounding, read it, and then forget about it. Now I go through my pager at every hour to ensure that I already responded to all my pages and then answer ones that I missed/forgot. On a semi-related note, a while back I wrote about good paging etiquette.
2. Let people know when you're out: I work a rotating schedule. As a result, it’s hard to predict when I’m in or out of the hospital. Sometimes I’ll come back on service and find urgent emails or texts that are a few days old. Now I leave an away message with my return date and my supervisor’s contact information on both email and hospital text. If someone really needs to get a hold of me, my supervisor has my personal cell phone number.
3. Be conscientious of what time you consult: I generally try to get all of my nonurgent consults done before 3pm. Many services have only 1 resident covering after 3pm, so I try not to page/call unless I have an emergency.
4. Call the nurse if something needs to be done urgently: Being a nurse means being the ultimate multitasker. Room 5 is due for his IV Amphotericin, Room 2's Foley is supposed to come out prior to void trial with Urology, Room 1's infusion completed and is beeping, and Room 4 is a bit altered and yanked out her PICC. Now I’m placing an order for Room 3 to get IV Lasix due to concern for pulmonary edema. However, the nurse may be preoccupied with Room 4 and not see the order in the computer for some time. If I really need to the patient to get the Lasix right way, I’ll place the order through EMR and then call the nurse and see what their situation is. If they’re crazy busy with Room 4 and likely to be unable to get to the Lasix within the next 15min, I ask whether they’re okay with me asking another nurse to give the Lasix now. Usually the answer is yes.
5. Value your nurses: Nurses know the patient best. They’re the ones answering call bells, giving meds, doing dressing changes, etc. Unfortunately they oftentimes bear the brunt of everyone’s frustrations, from patients to patients’ families to attendings to managers. Not to mention, they’re the ones doing the dirty work. Bedside nurses are the heartbeat of healthcare, but they also are high risk for burnout. Always support your nurses, whether that’s volunteering to answer a patient’s family member’s 17th phone call of the day or responding to a patient’s call bell yourself.
6. Know how to get a hold of someone quickly: It’s less than ideal to page someone repeatedly. At my hospital, if I need to talk to an attending urgently, I call the operator and ask them to connect me directly to the attending’s cell phone. If a patient is crashing and we’re not in the ICU, I dial the emergency number and call a rapid response, which sends people running into my patient’s room.
7. Plan your discharge meds from Day 1: The goal of every admission is to treat the patient and then discharge them safely. Send medications early for prior auth and call the pharmacy to make sure that they have medications in stock. (One time a patient’s insurance didn’t cover Levofloxacin, of all things.)
8. Keep social work and care coordination aware of all needs from the start: Does your patient looks unsteady? Place a PT/OT consult and let social work and care coordination know that the patient might require home therapy services and/or DME so that they can start looking at services and companies that may be covered by insurance. Does your patient have a central line? They’ll likely need a home health service to teach them how to care for it daily at home. Do they seem to require frequent transfusions? They’ll probably need labs on discharge. Is the patient’s living situation safe (no heat/AC, possible abuse at home, financial difficulties, etc)? They may need alternative housing.
9. The attending is not always right: Generally speaking, the attending has the last say on how the team manages a patient. However, I’ve come across situations in which an attending’s decision put a patient in more danger. Sometimes asking them about their decision can help steer the care plan toward better patient care. Other times you just have to stand your ground and be okay with being on the receiving end of an attending’s misdirected rant. Report these instances to your manager and to other higher-ups.
10. Always have gloves in your pocket: You never know when you’ll find a mess. Or which part of the body someone asks you to examine. Or how hygienic a person is (or is not).
11. Verify weird vitals: I was very new when I walked into work, opened a patient’s chart, and promptly bolted down the hallway when I saw a patient’s O2 sats recorded as 15-20s. I found the patient sitting up in bed, eating breakfast, and bewildered by me bursting into the room. Turns out that overnight someone mistakenly recorded his respirations as the O2 sats.
12. Remove whatever tubes you can: Anything entering the body is an infection risk. Does your patient still need that Foley placed by the surgery team? No? Yank it (don’t actually yank because ouch). Is your patient A&O and able to eat without aspirating? Remove the NG tube. Does your patient have good veins and require infrequent transfusions/labwork? Pull their central line.
13. Take a buddy with you to emergencies: Two heads are better than one. Even if you’re a seasoned provider and well-equipped to manage an emergency, you might need another body to help with performing CPR, making urgent calls, grabbing supplies, etc.
14. Ask your patients about premeds for procedures: We all have different levels of pain tolerance. A procedure goes far more smoothly if your patient is comfortable. Note: if you’re going to premed with Ativan or an opiate in the outpatient setting, make sure they have a driver.
15. Be good to your charge nurse and unit secretary: I don’t know how they do it. If I had to manage the unit’s signout, patient complaints, calls from other floor, being yelled at by providers, verifying paper orders, and finding beds for incoming patients- all at the same time - I’d lose my mind.
16. If your patient is mad, just shut up and listen: There are many things that you can’t control: the time it takes for a patient to get a room, the temperature of hospital food, the dismissive attitude of your attending, etc. And oftentimes the patient knows this. My reflex is to want to apologize for things and overexplain why different things are happening. But sometimes the patient just needs to rant. Take a step back and just listen. That can make all the difference.
17. Fact check your notes: The framework for your progress note often is the note from the day prior. It sounds obvious, but make sure that you go through the note and make updates and changes accordingly. If today is 01/15, there’s a good chance that the Fungitell from 12/31 is not still pending.
18. Try to learn some nursing skills: This is one of the areas in which I most envy my NP colleagues. If a patient’s IV pump is beeping or their central line need to be flushed, I oftentimes awkwardly step out of the room and look vacantly into the distance for a nurse. I’ve finally figured out how to spike a bag (albeit I do so very slowly, and it certainly makes the RNs giggle some). I talked to our unit’s nurse manager, and she’s willing for me to learn some nursing skills from the staff during a slow day- we’ll see when thing slow down!
19. Be kind: Generally speaking, being in a hospital is stressful. Patients are feeling out of sorts, and staff are working with constant dinging in the background. I rant plenty on this website, but I’m kind to everyone at work (with few exceptions) because it makes things more comfortable for everyone. Additionally, if you are always kind to your patients and colleagues, your reputation will speak for itself. One time I was walking down a hall with poor reception while on my ASCOM with a notoriously standoffish nurse from another unit. My phone cut out. She called my unit’s nurse manager to complain, and the nurse manager told her that I would never hang up on purpose. My interactions with the nurse going forward were always more pleasant in nature.
20. Support your team: The best colleagues are not the smartest colleagues; the best coworkers are the ones who have your back. Whether it’s a medical emergency or just a strange situation, it’s important to be supported and to give support.
I know that I’ve learned a lot more than this, so I’ll likely be adding to this throughout the year. Happy Snow Day, all!
25 notes
·
View notes
Text
To all the parents out there who bundle their babies up in the winter time with those little hats with the little ears that make them look like little teddy bears: You are doing the lord’s work. Seeing tiny ewoks toddle across the grocery store parking lot is just what we all need sometimes. My joy is immeasurable and my day is restored.
178K notes
·
View notes
Photo
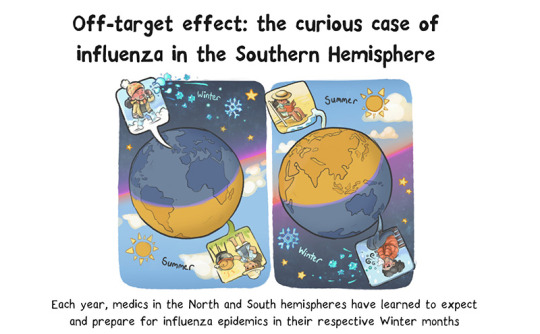
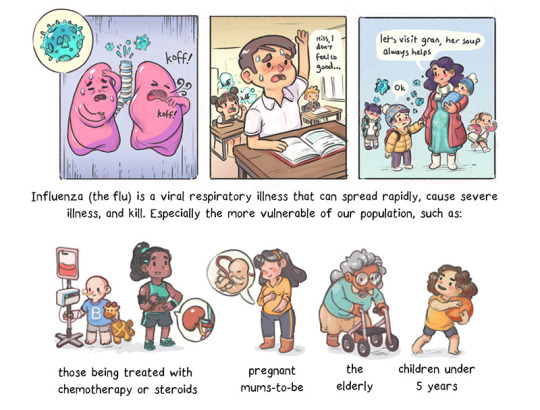
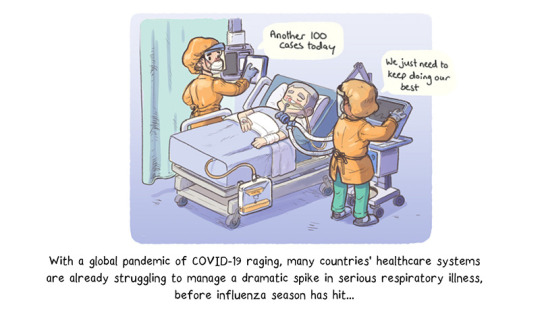
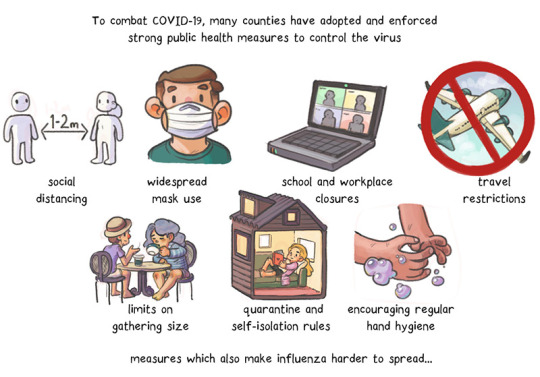
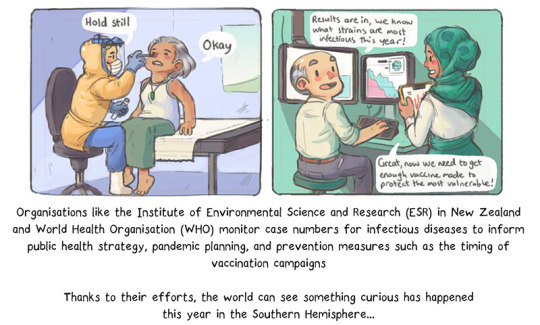

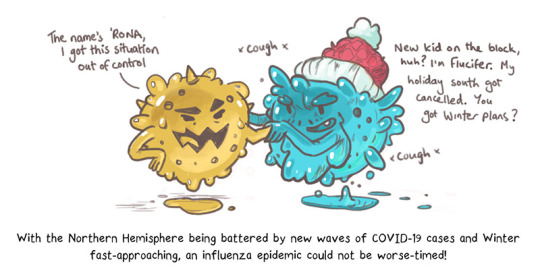

A comic about how New Zealand avoided a flu epidemic this year, likely thanks to COVID-19 precautions like social distancing and travel restrictions.
I am grateful to the MRINZ for embracing my art and research exploring the medium of comics. Would you like to see more research explained in this format?
More of my work: https://artibiotics.com/
Support: https://artibiotics.com/support
#graphicMedicine #caretoon #caretoons #comic #flu #COVID19
232 notes
·
View notes
Text
I tried pole for the first time.

0 notes
Note
Hi, I hope you are doing ok.
Umm I actually feel weird asking this, so it's ok if you just ignore this.
Is mask not compulsory anymore on public events in NZ? This video got around in my local tattoo community and people are of course debating if the pandemic is real. 🙄
https://m.facebook.com/story.php?story_fbid=10218801986310427&id=1523823067&ref=content_filter
The video seem to be from Christchurch Tattoo Expo.
https://instagram.com/chchtattooexpo
https://www.chchtattooexpo.com/faq
I totally don’t mind answering this, it’s good to be able to clear up some misinformation about the pandemic!
I haven’t been living in NZ since June 2020, but my family are all still there so I have a decent idea what’s going on. And this is the scoop:
Mask wearing has never been compulsory in NZ. Now, that’s not because mask wearing doesn’t work, and isn’t a useful tool in fighting the pandemic. It’s because NZ used different tools effectively and now has no community transmission (and hasn’t for several months).
Life in NZ is pretty much back to normal - we were in lockdown for a couple of months back around April 2020, during which time strict social distancing policies were enforced. These were universally enforced throughout the country. That was easier because the NZ government provided wage subsidies to ensure that people could work from home, keep their jobs, and still survive. It’s also easier in NZ because the country is only 5 million people under one government (I say this because NZ has done an excellent job but I don’t like people saying that other countries are doing worse simply because the people are selfish - NZ had a lot going for it in terms of pandemic control).
Once the presence of covid-19 was eradicated from the community, New Zealanders were able to gradually return to normal life. There are still strict border controls being enforced there - only NZ citizens or permanent residents can enter the country, and even then there is a government mandated and run 14 day quarantine, in managed hotels, with daily testing. The only cases being reported in NZ for a while now have been in that quarantine, effectively eliminating community spread and allowing life within the country to largely return to normal. Anyone in NZ who has any respiratory signs is still encouraged to get a covid-19 test - my Dad got one a few weeks ago because he had cold symptoms. So they’re still being vigilant, but the data is showing that it’s safe for them to operate more normally than when the virus was actively circulating within communities.
So that’s why you’ll see pictures of people in NZ at big events, within 6 feet of each other, and not wearing masks. Covid-19 isn’t circulating there, so it’s not necessary. And that has been determined through careful and widespread testing and monitoring. But that absolutely does not mean that the pandemic isn’t very real in many other countries - I’m in the US right now horrified at how many people are dying, I’m wearing my mask whenever I’m in public, I’m only going out because I do an essential job (and there I am wearing my mask, washing my hands, and keeping my distance). I am getting tested regularly because of my work, and I am very grateful to be getting vaccinated next week.
I hope that clears things up for you! In summary - it is safe right now to be in NZ and not wearing a mask. In other places such as the US and the UK it is not. Please take precautions. Please do not take the situation in NZ to be representative of any other country. Please, please follow the guidelines where you live, as they should reflect your situation most accurately. Or if you are concerned, be MORE careful. If in doubt, wear a mask, keep your distance, and always stay home if you are sick. The pandemic is very real and very dangerous. Stay safe out there x
13 notes
·
View notes
Conversation
Attending: Here's our situation. The CT scanner is down, and we're out of Dilaudid.
Nurse: Oh, wow.
PA: Does this mean we get to go home?
Attending: Well, WE know that we have no CT or Dilaudid, but none of our incoming patients know that.
Me: If you lend me some snow boots and promise me a good eval, I'll stand next to the highway with a sign.
19 notes
·
View notes
Text
If I was Elizabeth Bennet my entire family abandoning me at the dinner table when Mr. Collins requested a private audience would have been my villain origin story.
56K notes
·
View notes
Text
get the fuck over yourself
This is the story of two patients.
And they have all my sympathy.
My anger is not directed at them.
But at their spouses.
Patient 1:
Chronic pelvic pain
Has tried multiple pain meds, other meds, PT
Fearful of surgery
But asked us about undergoing surgery…
Our team: “It probably will make your problem worse, but why do you ask?”
Patient: “My husband really wants to have sex, and he thinks surgery is the answer.”
Our team: “How about couples counseling and sex therapy?”
Patient: “I don’t think he’d want to go…”
Patient 2:
Continuous vaginal bleeding for the past few years
Almost outside the “ideal” childbearing age range
Has tried hormone therapy among other things
Textbook solution: hysterectomy
Our team: “Would you be interested in a hysterectomy?”
Patient: “I would, but…”
Our team: “What concerns do you have?”
Patient: “I don’t want anymore kids. I already had enough trouble with my other pregnancies. But my husband still wants more.”
Hangry’s initial thoughts during these conversations:
Hangry after thinking more about what these women go through at home:

Attention Spouses:
If your loved one is struggling with her health,
That is your priority.
I don’t give a fuck if you want to have sex.
I don’t give a fuck if you want more kids.
You declared that you’d love her in sickness and in health.
Don’t be crying about “blue balls.”
Don’t be asking that she put her body through even more hell just because you want more offspring.
Your job is to make her feel better.
Your duty is to make her feel her best.
Get the fuck over your “needs.”
Be supportive.
Look after her health.
BE A GOOD SPOUSE AND DO YOUR FUCKING JOB.
103 notes
·
View notes
Text
ECG: quick and dirty
I’ve had countless sessions and lectures on ECGs. I don’t know how many websites I have bookmarked, or how many times my eyes glazed over reading Dubin. I’m also terrible at cardiology. I was on my way to accepting my fate of being horrible at ECGs forever, until I had a life changing session on ECGs taught by a great ER doc. I want to post it here because it was probably the most useful thing I learned in med school, and it will stick with me for the rest of my career.
WHEN LOOKING AT ECGs FOR THE FIRST TIME:
1. One ECG is never enough. Always get old ones for comparison. If none available, do another one. Because. One ECG is never enough.
2. RATE. Look at the number on top of the printed ECG. It’s stupid not to use that number. Yes, you should know the rule, 300-150-100-75-60-50. People say you shouldn’t trust the machine because… well, it’s a machine, and it can make mistakes. This is true. I don’t like to look at their “diagnosis” until I have gone through it myself. But the rate is just a number. Plus you should be able to eyeball it and be able to tell if it’s tachy, brady, etc. If the machine is telling you it’s 200 and if it looks tachy, then it’s probably the right number.
3. RHYTHM. Is there a p-wave for every QRS and a QRS for every p-wave? Is the p-wave upright in lead II and down in aVR? Good. Done. BOOM. It’s sinus rhythm. ***if you cannot clearly see the p-waves then you cannot call sinus. move on.
4. AXIS. Again, look at the number at the top of the page. If it’s between 0 and +90, then it’s normal axis. If the number isn’t provided, or if your preceptor doesn’t believe in the convenience of machines/technology, look at the QRS complex of lead I and lead II.
up in lead I, up in lead II: normal axis
up in lead I, down in lead II: left axis deviation (most common causes are left anterior hemi block and left ventricular hypertrophy)
down in lead I, up in lead II: right axis deviation (most common causes are right ventricular hypertrophy…PE)
5. did someone say HYPERTROPHY?
look at V1
is the R wave tall? (greater than 7mm?) right ventricular hypertrophy.
is the S wave tall? (greater than 11mm?) left ventricular hypertrophy.
6. P-waves
look at lead II
is it wide? left atrial enlargement.
is it tall? right atrial enlargement.
7. PR interval
should be between 0.12 sec and 0.2 sec (3-5 small boxes). I used to always get this interval and QRS complex (less than 0.12 sec) mixed up. Think: atria depolarizing + shit getting to ventricles is gonna take longer than ventricles depolarizing. [2 things happening] versus [1 thing happening]. [0.12 sec-0.2 sec] versus [<0.12 sec].
long PR interval means there’s some sort of block at the AV node.
1st deg block. PR interval is long. everything else is normal. cool.
2nd deg block
type I: PR interval progressively gets long. eventually a dropped QRS.
type II: PR interval is constant, but randomly dropped QRS.
3rd deg block “complete block”
there is no association between P waves and QRS. they run separately. **QRS does NOT have to be wide. Just look for P wave/QRS complex disassociation. I sometimes get this and 2nd deg type II mixed up. The only difference I try to remember is that PR interval is constant in 2nd deg type II, but is variable in 3rd deg.
8. QRS complex
narrow or wide?
narrow: good. signal coming from somewhere above ventricles.
wide: think BBB (bundle branch block)
LOOK AT V1 ONLY.
if the last deflection of QRS is DOWN, then it’s a left BBB
if the last deflection of QRS is UP, then it’s a right BBB. super easy. no more of this bunny ears crap.
9. ST segment
always look from J point, and compare with the isoelectric line of T-P segment (NOT PR interval).
elevated/depressed… STEMI… duh. indicates ACUTE ischemic changes.
look for reciprocal changes of the heart. if ST elevation in lateral leads, could see ST depression in the septal leads. PAILS:
posterior up, anterior down
anterior up, inferior down
inferior up, lateral down
lateral up, septal down.
LBBB can look like STEMI. How to tell?
disconcordant changes is normal. (QRS and STEMI on opposite sides of the isoelectric line.)
concordant changes is abnormal.
massive discordance is abnormal. (STEMI is greater than 5mm)
this isn’t that important. Moving on.
Inferior STEMI. Could right ventricle be involved?
DO NOT GIVE NITRO DO NOT GIVE NITRO DO NOT GIVE NITRO.
order a 15 lead
is STE in lead III > lead II? likely RV involvement
INFERIOR MI? 15 LEAD NO NITRO
INFERIOR MI? 15 LEAD NO NITRO
INFERIOR MI? 15 LEAD NO NITRO
10. T waves
is it inverted? indicates recent ischemic changes.
11. Q waves
is it significant? indicates old ischemic changes. will likely be present if followed rule number 1 of reading ECGs. (1 ECG is never enough= look at old ECGs).
I literally go through this list of 11 points in my head when I’m reading an ECG, regardless of whether or not I have an atrial flutter jumping at my face or if I see a massive anterolateral STEMI. Obviously I needed background knowledge on ECGs and the physiology of the heart before constructing this list, but this basic checklist has been very, very useful to me so far. It might look lengthy, but it doesn’t take a lot of time at all- a patient is not likely going to have all these issues with their heart.
Anyway. I still don’t love ECGs, but it feels pretty wonderful to be able to be able to evaluate it in a systematic manner, and get the theory behind interpreting the scribbles of an ECG reading. I don’t get these moments as much as I would like to, but it’s that crosspoint where my classroom learning actually meets real-life applications that gives me happy brain-gasms for days. I love knowing things and more importantly, knowing why.

6K notes
·
View notes
Video
“Umm honey, I’ll be late today. I’m stuck in traffic.”
(Source)
50K notes
·
View notes