#JCMICR
Text
Acute appendicitis in an incarcerated hernia sac at the laparoscopic trocar entrance by Hasan Cantay in Journal of Clinical and Medical Images, Case Reports

Abstract
Rarely, appendix vermiformis can be detected in abdominal wall hernias such as inguinal, obturator, umbilical and incisional hernias. Detection of the appendix in the hernia formed at the laparoscopic trocar entrance is extremely rare. We treated a 58-year-old female patient with acute appendicitis in an incarcerated hernia sac at the laparoscopic trocar entrance with laparoscopic appendectomy and laparoscopic mesh hernioplasty. In order to prevent the development of hernia at the trocar entrance, the fascia at this place should be sutured in laparoscopic operations.
Introduction
Adipose tissue, omentum, small intestine, colon and sometimes different organs are most commonly obtainable in the hernia sac [1, 2]. Acute appendicitis is accepted as a common surgical emergency. Appendix vermiformis can be detected in abdominal wall hernias such as inguinal, obturator, umbilical and incisional hernias, with an incidence of 0.008-1% [3]. If the appendix is located in the inguinal hernia sac or in the femoral hernia sac, they are specially named as Amyand and Garengeot, respectively [1-3]. In this case report, we aimed to evaluate acute appendicitis detected in an incarcerated hernia sac at the trocar entrance, in light of the literature.
Case presentation
A 58-year-old female patient who underwent laparoscopic total abdominal hysterectomy and bilateral salpingo-oophorectomy with the diagnosis of myoma uteri 4 months ago was admitted to the emergency service with complaints of swelling, redness and abdominal pain at the old trocar entrance in the right lower quadrant, which had been going on for 2 days. The patient had no comorbidity, and she had nausea and gas-stool discharged. During the physical examination, incarcerated incisional hernia at the trocar entry site in the right lower quadrant and widespread tenderness in this region. Laboratory results were unremarkable except for the fact that WBC (leukocyte) was 12.800 cell/μL. There was minimal air-fluid level in the standing abdominal X-ray of the patient (Figure 1). In the superficial USG examination of the right lower quadrant of the abdomen, a fascia defect and a herniated intestinal loop in it were observed. It was decided to operate on the patient. Under intratracheal general anaesthesia, pneomoperitoneum was created with a 10-mm trocar inserted through the umbilicus, and the abdomen was entered with a camera. It was observed that the appendix and part of the cecum were in the incarcerated hernia sac (Figures 2 and 3). Subsequently, 2 more 5-mm trocars were inserted. The cecum was removed from the defect with the aid of a Grasper. It was observed that the appendix was adherent, inflamed and erectile within the hernia wall. The appendix was carefully separated from the hernia with the aid of a harmonic device. Laparoscopic appendectomy was performed by double ligating the appendix radix with 2/0 VICRYL suture. Then, the appendix was removed from the abdomen through the trocar. After that, mesh hernioplasty was performed laparoscopically and a drain was placed and the layers were closed anatomically and the operation was completed. The patient’s drain was removed on the second postoperative day, and the patient was discharged with full recovery. In the postoperative outpatient clinic controls, it was not detected any surgical site infection or recurrence.

Figure 1: Abdominal X-ray of the patient.

Figure 2: Laparoscopic view of acute appendicitis in hernia sac.
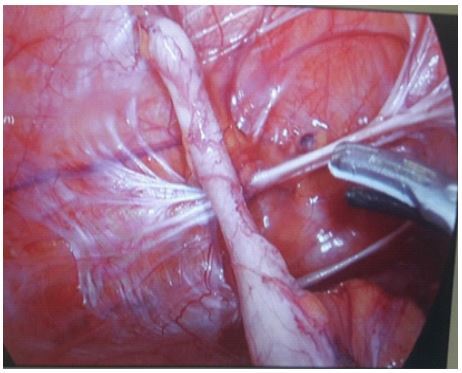
Figure 3: Appearance of appendix in hernia sac (adhesive to the hernia sac wall).
Discussion
The treatment of acute appendicitis is surgery, but conservative treatment with antibiotics can be applied in selected patients for whom surgery is contraindicated [4]. Treatment of incarcerated hernia is also exploration of the hernia sac and emergency repair of the defect with or without mesh [5]. Anterior abdominal wall hernias including appendix, which are rarely seen, are usually detected in the right side inguinal region and femoral canal. Although it is encountered by chance during elective repairs, it can also be encountered with appendicitis [6]. Encountering with the appendix is rare in incisional hernias. In most of these cases, the appendix is detected in Phannenstiel incision, and upper midline incisions of the abdomen such as open cholecystectomy [3, 7]. Detection of appendix is much rarer in hernias at the laparoscopic port site, and when we search at the literature, we encounter only three cases similar to our study. In the first case, appendix was found at the umbilical trocar entrance after laparoscopic sterilization on the 12th postoperative day; in the second case, it was found at the 5-mm trocar entrance after laparoscopic cholecystectomy, and in the third case, it was found in the incisional hernia sac at the right iliac fossa level where a 5-mm trocar drain was placed [3, 8, 9].
Conclusion
In conclusion, it is possible to detect the appendix in the hernia sac formed at the laparoscopic trocar entrance. In order to prevent the development of hernia at the trocar entrance, the facia at this region should be sutured in laparoscopic operations.
Declarations
Funding: This work did not benefit from any financial support.
Conflict of interest: All authors declare no conflict of interest.
Patient consent statement: A written permission to publish has been obtained from the patient.
For more details : https://jcmimagescasereports.org/author-guidelines/
#appendix vermiformis#laparoscopic#Rarely#appendectomy#hernioplasty#Garengeot#abdominal hysterectom#leukocyte#inguinal region#Hasan Cantay#JCMICR
0 notes
Text
Role of Alpha Fetoprotein in hepatocellular carcinoma by MuhammadWaqar Mazhar in Journal of Clinical and Medical Images, Case Reports

Abstract
Hepatocellular carcinoma prevelance rate is higher in Pakistan due to HCV mortality rate, consumption of Alchol, and regular smoking, higher level of AFP progression normal liver cells into fatty liver cells, after inflammation it convert into HCC.In this study, we find the correlation between AFP and hepatocellular carcinoma. AFP involve in development of liver cancer, LFT’s test elevation and HCV also cause of cancer.
Keywords: Hepatocellular Carcinoma; Alpha Fetoprotein; alanine amino transferases; aspartate aminotransferases.
Introduction
Hepatocellular carcinoma is the 4th most common malignancy in worldwide and it is leading cause of cancer like disease in liver, and it exceed more than 1 million deaths per year by 2030 [1]. Acute hepatitis and acute liver failure are the most serious medical condition that require early diagnosis by release of IL-6, TNF-α and elevated alanine amino transferases, aspartate aminotransferases, alkaline phosphatase and α -Fetoprotein that progress healthy liver in to fatty liver known as steatosis and then inflammation occur in this and leads to hepatocellular carcinoma [2]. Most cases of HCC due to the virus like HCV and HBV, Diabetic and obesity, alcohol related diseases, non- alcohol related diseases, carcinogens like aflatoxins compounds [3]. HCC is the most common cancer that have high mortality rate in cancers due to mortality of HCV and NLFD. In Pakistan HCC ratio high due to prevalence and mortality rate of HCV [4]. The major treatment of HCC are chemotherapy, radiotherapy, transplantation and surgery. Because the most cases diagnose at the late stage, surgery cannot be performed and drugs are the only treatment of HCC [5]. Most patients in HCC become more drug resistance drug resistance. Drug treatment is the best choice of patients who are not edible for surgery. HCC is usually resistance to chemotherapeutic drugs. Because it hinders liver cancer treatment. In recent years targeted drugs use as medication and immune checkpoint inhibitors are introduce for treatment [6].
In the previous research evidence indicates that alpha-fetoprotein has high false-positive rate in diagnosis of early stage of HCC. The EASL clinic practices shows that AFP as a biomarker for liver transplantation and drug indicator [7]. The AFP level increased in many patients’ ad its risk for progression of HCC. AFP, currently the only biomarker available for HCC drug treatment, function as immune suppressor and promote malignancy transformation in HCC [8]. HCC is resistant to traditional chemotherapeutic agents such as doxorubicin, tetrahydrofolate, oxaliplatin, cisplatin, and gemcitabine. currently the recommended drugs include such as targeted therapeutics and immune checkpoint inhibitors [9].
AFP is a glycoprotein that secreted by endoderm embryonic tissue. The lower level of AFP in blood due to AFP is decrease in mature hepatocytes and that AFP gene expression is blocked. It is possible that AFP involved in HCC development and progression become an important factor affecting HCC diagnosis and treatment. AFP plays an important role in promoting cancer cell proliferation and, inhibition cancer cell apoptosis.
LFT’s test performed for liver injury, alanine aminotransferases, aspartate aminotransferases and alkaline phosphatase. These enzymes are commonly elevated in liver disease patients. Alkaline phosphatase and AFP play important role in the diagnosis of cancer.
Case Study
The patient name was sikandar, age 56 patient feel pain in their abdomen and sudden loss of weight. The patient has already hepatitis C infection and their PCR results were positive with high viral load. Due to serious illness it admitted in emergency ward 12, Nishter Hospital Multan. The doctors panel referred some test and kept in observations for better health condition.
The total bilirubin level was 2.05mg/dl in their blood and their normal values 0.6 - 1.2. The serum glutamate-pyruvate transaminase level is 43U/L and normal values up to 40. Aspartate amino transferases and alkaline phosphatase level were high in blood respectively 151 U/L and 493 U/l show in (Figure 1). Its indicate liver injury and cirrhosis. The AFP test indicates correlation with Hepatocellular carcinoma. The AFP level in patient was 6101ng/ml and normal values were 0.1 – 10. Higher level of AFP indicates that HCC have positive relation with AFP to proliferate cancer. The test formed by fully automated state of the Art analyzer Beckman Coulter 700 AIJ.

Figure 1: Liver function and Alpha Feto Protein test in patient.
After blood reports, doctor suggest ultarosund Computrised Tomography whole abdominal view. In view, spleen size becomes enlarged 6cm, calculi in gall bladder, heterogeneous patchy atrial enhancement of right lobe, and some nodules seen in both lobes of liver. The doctor findings the AFP correlation with HCC, splenomegaly, ascites, cholelithiasis and protosystematic collaterals.

Figure 2: Ultrasound Computrised Tomography whole abdomen.
The patient diagnosed with hepatocellular carcinoma at last stage, and doctor reffered to liver transplantation in india. But after 4 weeks he cannot survive.
Conclusion
Hepatitis C was the major risk of hepatocellular carcinoma in Pakistan. Smoking and alcohol have big problem to influence HCC in humans. The case study show that alpha fetoprotein has correlation with HCC. Higher Alkaline phosphatase and serum Bilirubin level enhance the liver carcinoma. AFP play role in cell proliferation, cancer cell differentiation and cell cycle arrest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Hepatocellular Carcinoma#Alpha Fetoprotein#alanine amino transferases#aspartate aminotransferases#malignancy#HCV#HCC#doxorubicin#tetrahydrofolate#oxaliplatin#Tomography#MuhammadWaqar Mazhar#JCMICR
0 notes
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Amal in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
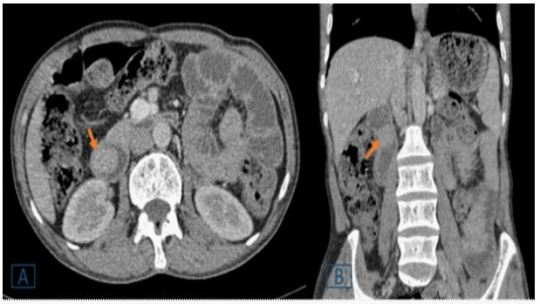
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#ATCD#frequent vomiting#dyspepsia#abnormalities#Peutz-Jeghers syndrome#polyposis syndromes#gastrointestinal#EGD#Lahfidi Amal#JCMICR
0 notes
Text
Zinner Syndrome: A Rare Case of the Mesonephricduct Anomaly by Balagobi B in Journal of Clinical and Medical Images, Case Reports

Abstract
The present article reports 18-year-old boy came to the urology clinic with perineal discomfort and few episodes of incomplete emptying of the bowel for two months. He did not claim any symptoms related to his voiding or ejaculation. The abdominal and external genitalia examination was regular. He had average prostate size on digital rectal examination with a palpable painless cystic mass just above the prostate gland. Zinner's syndrome should be a differential diagnosis in young patients with urinary symptoms and unilateral renal agenesis. A detailed review of the relevant literature is also presented.
Keywords: Zinner's syndrome; congenital malformation; seminal vesicle cyst; renal agenesis; infertility.
Introduction
Zinner's syndrome is one of the rarest congenital malformations present with cysts in the seminal vesicle, ejaculatory duct obstruction, and ipsilateral renal agenesis [1]. Its origins in the development abnormality of the Wolffian duct at embryogenesis. Some of the patients with Zinner's syndrome may remain asymptomatic and discovered incidentally, while others present with clinical signs of bladder outlet obstruction, nonspecific pelvic pain, and symptoms related to ejaculatory dysfunction [2]. Herein, we present a case of Zinner's syndrome in which the patient presents with perineal pain and discomfort with a few episodes of incomplete defecation as an initial complaint.
Case presentation
An 18-year-old boy came to the urology clinic with perineal discomfort and few episodes of incomplete emptying of the bowel for two months. At the same time, he did not claim any symptoms related to his voiding or ejaculation. The abdominal and external genitalia examination was regular. He had average prostate size on digital rectal examination with a palpable painless cystic mass just above the prostate gland. The initial laboratory investigations did not reveal any abnormal values, including renal function tests and hormone analysis (LH, FSH, and testosterone). The ultrasound kidney, ureter, and bladder (KUB) showed the right side renal agenesis and homolateral seminal vesicle cyst (Figure 1). Subsequently, the urinary tract's magnetic resonance imaging (MRI) was requested, which diagnosed Zinner's syndrome by visualizing the seminal vesicle cyst on T1 and T2 weighted images as hypo intensity and hyper intensity signals, respectively (Figure 2). Furthermore, his sperm parameters were normal in limit and excluded the risk of future infertility. We offered simple nonopioid analgesics for the perineal pain and laxatives for the defecation issues. We did not do any invasive treatment for him as he is asymptomatic after initial treatment. Therefore, he is under surveillance at our urology clinic for more than one year.
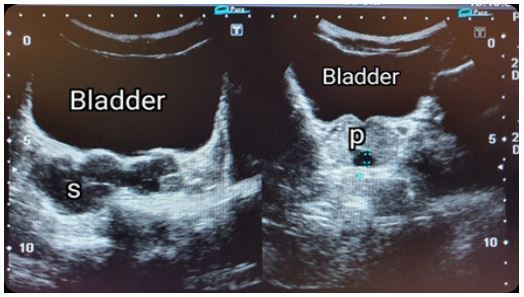
Figure 1: Ultrasound pelvis showing the multiple cysts within the right seminal vesicle(S) and dilated distal part of seminal vesicle within prostate gland (P).

Figure 2: (A) Coronal image of MRI abdomen showing absent right kidney with enlarged normal left side kidney. (B & C) Pelvic MRI. T1 and T2 – weighted axial images show the right side dilated cysts within the seminal vesicle, and it shows hyperintensity in T1 and hypointensity in T2-weighted images.
Discussion
Zinner's syndrome occurs due to abnormal growth of the Wolffian duct during embryogenesis, and it is marked by ejaculatory duct obstruction, cysts in seminal vesicles, and same-side renal agenesis [3]. In history, the seminal vesicle cysts were identified first by Smith in 1872, and later the association between unilateral renal agenesis and seminal vesicle cyst was first described by Zinner in 1914 [2]. Since that, more than 100 case reports in Zinner's syndrome reported in the English literature and this is the first reported case in Sri Lanka in this entity [4]. The ureteric bud originates from the distal part of the mesonephric duct and ascends cranially to meet the metanephric blastema, which will form the future kidney. Maldevelopment of the distal mesonephric duct occurs due to various insults during the first trimester that leads to ejaculatory duct atresia and abnormality of ureteral budding. Atresia of the ejaculatory duct causes obstruction and cystic dilatation of seminal vesicles and anomaly in the ureteral budding results in renal agenesis [5]. Patients with this congenital anomaly are usually asymptomatic until their second to the third decade of life [6]. The symptoms develop due to bladder irritation, bladder outlet obstruction, cyst distension, and obstruction of the ejaculatory duct. Therefore, the Patients may present with unspecific and various clinical manifestations, including voiding symptoms (frequency, dysuria, urgency, poor flow), haematuria, pelvic pain, perineal or scrotal pain or discomfort, urinary tract infection, painful ejaculation, and haematospermia [5].
The diagnostic evaluation of a Zinner's syndrome includes biochemical investigations, radiological imaging, and cystoscopic examination. Urinalysis and culture, blood analysis, renal function tests, and hormone profile (FSH, LH, Testosterone) is proper initial biochemical investigations. Transrectal ultrasonography is the most widely used tool for identifying and initial evaluating seminal vesicle cysts, and it reveals anechoic cystic pelvic lesions with a thick, irregular wall and calcifications [7]. Besides, the computed tomogram also can demonstrate the cysts in the seminal vesicle and renal agenesis, but it is not adequate to make the final diagnosis. Therefore, magnetic resonance imaging is the definitive diagnostic imaging of Zinner's syndrome without the need for additional invasive investigations. Typically, the cysts in seminal vesicles appear as hyperintensity lesions on T2- weighted images andhypointensity in T1- weighted images. Besides, an MRI scan reveals excellent soft-tissue anatomy between the cysts and surroundings in the pelvis, which is helpful for surgical management [3]. Urethrocystoscopy may show trigonal abnormality or bulge inside the bladder due to external compression [8].
The management of Zinner's syndrome should be planned according to the clinical presentation. The Conservative approach is helpful in mild symptomatic or asymptomatic cases with normal biochemical parameters [6]. Aspiration of the seminal vesicles and combined instillation of substances such as alcohol or minocycline and antibiotics are also tried in mild symptomatic group 3. Surgical treatment options should restrict to symptomatic cases or patients who failed conservative measures. Surgical treatment options can be a transurethral resection of the ejaculatory duct (TURED) or seminal vesiculectomy. TURED procedure includes the resection of the prostate at the level of verumontanum until the opening of the ejaculatory ducts. A study reported a remarkable improvement of semen volume, pH, and sperm count, increasing carnitine and fructose concentration after TURED in seven patients. Therefore, they recommended that TURED surgery be tried first to resumption natural fertility before trying other infertility treatments [9]. Open excision of the cyst was the most effective procedure for symptomatic patients until recently, and it was replaced by laparoscopic and robotic surgeries in the current era. Minimally invasive surgeries ensure retrovesical anatomy during surgery with minimal blood loss and minimal postoperative morbidity. Unfortunately, some of the patients with infertility fail to recover from poor sperm parameters despite all these efforts, and assisted reproduction techniques become the only hope for them [10].
Conclusion
Zinner's syndrome should be a differential diagnosis in young patients with urinary symptoms and unilateral renal agenesis. Even though transrectal ultrasonography is used as an initial screening tool, the MRI pelvis makes the final diagnosis, and surgical treatment options resolve the complaints in symptomatic patients except for the poor sperm parameters.
Acknowledgement
The authors wish to thank, S.Thiruvarangan, Research Assistant who assisted to this manuscript preparation and submission process in the final stage of this article.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Zinner's syndrome#congenital malformation#seminal vesicle cyst#renal agenesis#infertility#LH#FSH#urology clinic#nonopioid analgesics#Balagobi B#JCMICR
0 notes
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Ama in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
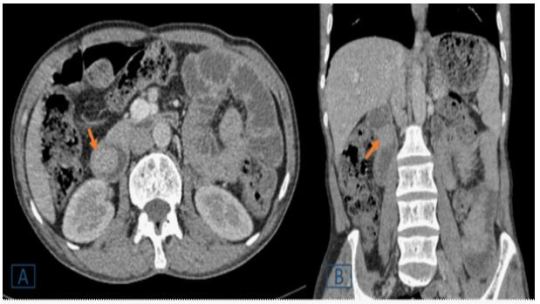
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Peutz-Jeghers syndrome#juvenile polyposis#computed tomography#gastrointestinal bleeding#vomiting#endoscopy#enteroscopic#Lahfidi Ama#JCMICR
0 notes
Text
Spontaneous Rupture of Wandering Spleen: Case Report by Mina Alvandipour in Journal of Clinical and Medical Images, Case Reports

Abstract
Keywords: Spleen; wandering spleen; ectopic spleen; splenic rupture.
Introduction
A wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [1]. wandering spleen is caused by either extreme laxity or absence of the normal ligaments that anchor the spleen to the left upper quadrant. Gravity also plays a role by allowing the spleen to descend into the lower abdomen attached by its vascular pedicle [2]. Symptoms depend on the degree of torsion and range from chronic abdominal pain in mild torsion to acute pain in severe torsion and infarction. Accurate clinical diagnosis is difficult because of the rarity of the condition and non-specific symptoms. Radiological evaluation includes usage of ultrasound, Doppler, abdominal CT or MRI depending upon availability or preference [3]. A wandering spleen can be either congenital or acquired. In the congenital condition the ligaments fail to develop properly, whereas in the acquired form the hormonal effects of pregnancy and abdominal wall laxity are proposed as determining factors .However, the precise etiology of the wandering spleen is not known [1]. We present a spontaneous rupture of a wandering spleen with severe torsion and infarction and abdominal pain without any history of trauma.
Case Report
A 25 years old female present to emergency unit with 2 week history of progressive abdominal pain, recurrent constipation ,vomiting and loss of appetite. There was no history of melena, fever, and hematochezia and weight loss. On examination there was periumbilical and epigastria tenderness and a firm and tender mass in the right side of the abdomen without muscle guarding and rebound tenderness. The vital sign and laboratory results were all within the normal ranges, except decreased hematocrit (hemoglobin-8.4). The plain abdominal radiograph was un-remarkable while abdominal ultrasonography with color Doppler showed absence of spleen in its normal location in the left upper abdomen. Also it detects a heterogeneous hypoechoic capsulated mass with diameter of 175mm in right lower abdomen. Other organs of the abdomen were normal. Abdominal pelvic CT scan with and without contrast was recommended and findings was Absence of the spleen in its normal position in the left hypochondrium, and presence of large diameter mass (splenomegaly)in the right sub hepatic area(Wandering spleen) . Other organs of the abdomen were normal. Contrast-enhanced computed tomography (CECT) of the abdomen revealed whirlpool sign near the umbilicus. The splenic parenchyma showed abnormal enhanced areas, suggestive of splenic torsion and infarction.
A final diagnosis was wandering spleen with torsion of the vascular pedicle and infarction. The patient underwent a total splenectomy. During the laparotomy, an enlarged and infarcted mass was seen in right side of abdomen. The characteristic “whirlsign” can be seen in the area of the splenic vascular pedicle, indicative of torsion. Histological examination confirmed total infraction of the wandering spleen. The postoperative course was uneventful, and the patient was discharged on the 4th day after the operation.
Discussion
A wandering spleen is a rare but well-known entity. The incidence is < 0.2%. It is more common in females than males between the second to fourth decade of life and children [4]. Splenic weight >500 g in more than 8 out of 10 cases [5]. Interestingly, it has been reported that one out of three cases of wandering spleen appears in children bellow the age of 10 years old [7].
Wandering is characterized by splenic hyper mobility that results from elongation or mal-development of its suspensory ligaments. It is also known as aberrant, floating, displaced, prolapsed, ptotic, dislocated or dystopic spleen. Ectopic spleen, splenosis and accessory spleens are separate clinical entities and must be distinguished from it [5]. If the pedicle is twisted in the course of movement of the spleen, blood supply may be interrupted or blocked, resulting in severe damage to the blood vessels .Acute splenic torsion compromises venous outflow, which causes congestion and impairment of arterial inflow. Pain is originated from the splenic capsular stretching with rapid splenic enlargement and localized peritonitis [6]. Etiology is congenital or acquired. In case of congenital anomaly, a failure occur in fusion of the dorsal mesogastrium with the posterior abdominal wall during the second month of embryogenesis. Acquired risk factors that predispose to wandering spleen include pregnancy, trauma and splenomegaly [7]. Splenic torsion is usually clockwise. Complications of splenic torsion include: gangrene, abscess formation, local peritonitis, intestinal obstruction and necrosis of the pancreatic tail, which can lead to recurrent acute pancreatitis [8].
Wondering spleen had nonspecific symptoms such as abdominal pain that make diagnosis extremely challenging. As a result, radiologists play a major role in the diagnosis of this condition and its complications. Torsion may occur acutely and present with infarction or peritonitis. Chronic intermittent torsion can lead to pain, splenomegaly, and functional splenectomy. Contrast-enhanced computed tomography (CT) is the best imaging tool to make this diagnosis, although ultrasound may be used as well. Imaging findings on CT include identification of a spleen in an abnormal location, or with an abnormal orientation in the left upper quadrant. Often the wandering spleen is identified as a “comma” shaped mass in abdomen, with no normal left upper quadrant spleen [9].
Laboratory investigations are non-specific. Thrombocytopenia, through a mechanism of spleen enlargement secondary to compression of the splenic pedicle is rarely found [7]. The clinical presentation of wandering spleen is variable; it is either asymptomatic or noted incidentally during physical and radiographic examination or presents as acute abdomen due to torsion with subsequent infarction. The most common presentation is a mass with non-specific abdominal symptoms or intermittent abdominal discomfort due to congestion resulting from torsion and spontaneous detorsion [10]. Today, the only recommended treatment for wandering spleen is operation [7]. Splenectomy is indicated for infracted spleen and sometimes for huge splenomegaly precluding splenopexy. Splenopexy is the choice of treatment if the spleen is not infarcted [6]. Splenic preservation is highly recommended for young patients—those under one year of age up to those in their thirties—who are at particular risk for overwhelming post-splenectomy sepsis [10]. This should be appropriately followed up by the prophylactic vaccines against post-splenectomy sepsis syndrome. Ideally they should be administered before surgery; however, in emergencies this is not always possible [1].
Conclusion
In this case, splenectomy was done due to spleen infarction. Laparotomy was done in this case because of low experience at laparoscopy splenectomy. This report highlights the investigations and management necessary for a patient who presents with an ischaemic torted wandering spleen.
Acknowledgement: None.
Conflict of Interest: None.
Funds: None.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Spleen#wandering spleen#ectopic spleen#splenic rupture#Radiological#ultrasonography#Contrast-enhanced computed tomography#laparotomy#laparoscopy#Mina Alvandipour#JCMICR
0 notes
Text
Laser therapy and application of Aloe vera for wound treatment after mastopexy complications: A case report by Emerson Barbosa da Silva in Journal of Clinical and Medical Images, Case Reports

Abstract
Mammoplasty is a surgery aimed at reducing breasts, being an invasive procedure and with the possibility of post-surgical complications. In the case presented, the patient had healing difficulties which progressed to an intense inflammatory process that evolved to necrosis of the areolas, laser therapy sessions were applied using lasers with red LED and blue LED in order to treat the inflammatory process, stimulate regeneration of tissue and collagen synthesis, treat the patient's pain, hydrate the tissues, fight infections and skin diseases and whiten the area. It was associated with the application of Aloe vera in natura to treat wounds and heal the local. It was observed that after treatment there was a significant improvement in areola necrosis, healing of the injured part and improvement in collagen production. Making an evaluation during the 24 sessions, we were able to assess that in synergy between the Red Laser, Infrared, Blue LED and the use of the active ingredient Aloe vera corroborate the evolution of tissue healing.
Keywords: Aloe vera; laser therapy; mastopexy; surgical complications.
Introduction
Mastopexy or reduction mammoplasty is a surgery performed to reduce the breasts are usually more invasive because it involves larger incisions, tissue, skin, fat and repositioning of the areolas. These patients have back and neck pain due to the weight of the breasts, in some cases, the clinical picture even presents curvature of the back, some patients seek this type of surgery because they are unhappy with their aesthetic appearance [1]. Necrosis occurs when cells in a particular region of the body fail to receive enough oxygen. There are risks that are managed by the patient and risks inherent to the surgery technique itself. There are more common factors after surgery, which are headaches and in the surgery itself, bleeding at the site, keloids, infection, necrosis and thrombosis. It is not common to happen necrosis in the breast after mammoplasty, the probability is around 1%, factors that interfere with healing are smoking and diabetes [2, 3]. In performing this type of surgery, it is necessary to raise the areola, due to a structure called the Areolocapillary Complex - CAP, it can suffer some injury, when this tissue does not receive oxygen causing necrosis [3, 4].
The doctor responsible for the surgery cannot observe if there is any type of injury in the NAC, this usually occurs in breasts with ptosis because the greater the distance that the areola will travel during the surgery, the greater the chances of any injury to the NAC. Several authors sought to describe studies that showed assessments regarding complications in breast reduction surgery. The most common complications found in the literature were described, related to blood perfusion of the nipple-areola complex (NAC), operative site infection, dehiscence, asymmetries and changes in sensitivity secondary to the surgical procedure. The type of injury that occurred was scarring below the right areola in the stitches and tissue necrosis in the left areola, the probable cause may have been because of the NAC injury. Each author in the literature as well as those present on the table describes the safety of each flap, with its particularities, but without comparing the different techniques with each other1. The treatment performed was Red, Infrared, Blue Led laser therapy and the Aloe and vera plant [4].
The laser performs an amplification of light by stimulated emission of electromagnetic radiation that emits coherent and collimated light that can have different powers, for therapeutic use, we use low power laser that increase lymphocytes and phagocytosis, increasing fibroblasts and intensifying reabsorption of fibrin and due to the characteristics Biostimulators accelerating tissue repair, due to mitotic activation of epithelial cells, produces collagen and decreases the synthesis of inflammatory meters.
Treatment Red and infrared laser therapy (light amplification by stimulated emission of radiation) Red Light (660nm): Red light treats inflammatory processes, stimulates tissue regeneration and collagen synthesis, improves vascularization and angiogenesis, increases ATP production. It acts on the epidermis, dermis, hypodermis, muscle fascia, muscle tissue, tendinous ligament [5]. Infrared Light (808nm): Infrared light has the analgesic function (pain treatment) as the main point, acts in lymphatic drainage and edema, has an anti-inflammatory effect and increases the absorption of products by 40 %. It acts on the epidermis, dermis, hypodermis, muscle fascia, muscle, ligament, tendon, nervous and bone tissue [6]. Blue Light (470nm): Blue light has bactericidal and fungicidal action, promotes tissue hydration, fights infections and skin diseases and has a whitening effect. It acts mainly on the epidermis and on open lesions in the dermis [5, 6]. The healing caused by the blue LED is a mechanism of molecular events divided into three phases: inflammatory, proliferative and remodeling. It is in the remodeling phase that the recovery of tissue structure occurs through maturation of elements and changes in the extracellular matrix, where the deposit of proteoglycans and collagen occurs.
Case Presentation
Patient 27 years old, female, denies smoking and alcohol consumption, denies diabetes mellitus, underwent mastopexy surgery to reduce and improve the sagging of the breasts, after performing the surgery below the right areola, she presented difficulty in healing in the stitches and in the left areola necrosis and difficulty healing the stitches. Patient underwent breast reduction surgery, after surgery the breasts present exudate thickening of the skin in the right areola in the stitches it began to show difficulty in healing, in the left areola that was not healing, there was a darkening of the areola and after two weeks the tissue it was already completely necrotic. The plastic surgeon who performed the surgery indicated the use of Kollagenase (collagenase) Cristália®, intended for the treatment of skin lesions when debridement is indicated in wounds, ulcers and necrotic lesions. Without evolution, the professional indicated Lasertherapy to the patient. The methodologies applied during the first 20 sessions were performed 3 sessions per week, red and infrared laser therapy doses of 8 J/cm2 and blue LED using the Laser Therapy EC - DMC® equipment. 24 laser therapy sessions were carried out, in all of them both blue and red led were used. The first 20 sessions were held 3 times a week, after which 4 sessions were held, one per week. The patient applied Aloe vera in natura 3 times a day on the lesion, before application, asepsis of the lesion was recommended.
The patient underwent anchor mastopexy with the desire to improve the aesthetic aspect of the breast, in addition to improving physical aspects such as pain in the spine, after a week of the surgical procedure the patient noticed that the left breast took longer to heal when compared to on the right. The lesion turned red and began to produce fluid, the shape of the areola was changing due to the intense inflammatory process. After a few days, a blackened stain began to appear, which characterized a necrosis process that soon extended, the incision became swollen and without the possibility of healing as seen in (Figure 1).

Figure 1: Left breast with extensive necrotic ulceration in the areola.
In the first consultation, skin debridement was performed, which aims to remove the largest amount of dead tissue, in order to reduce the process of tissue necrosis and reduce the possibility of infection by opportunistic pathogens, which would complicate the situation. The lesion was now cleaner (Figure 2) and it was possible to carry out an effective treatment plan.

Figure 2: Left breast after debridement and cleaning of the lesion.
The application of Infrared and Blue LED was started, three times a week until completing the twenty sessions, during the treatment the patient performed the topical application of Aloe vera in natura to assist in the healing process in the skin and enhance the treatment. The lesions became redder, since the treatment increases tissue perfusion, improving nutrient delivery and access to defense cells that help in the healing process (Figure 3).

Figure 3, A-F: Evolution of the lesion between the first 5 sessions.
After the tenth session, the tissue improvement in relation to necrosis was already noticed and until the twentieth session, areas of necrosis in the breast were no longer seen, which showed the efficiency of the treatment (Figure 4).
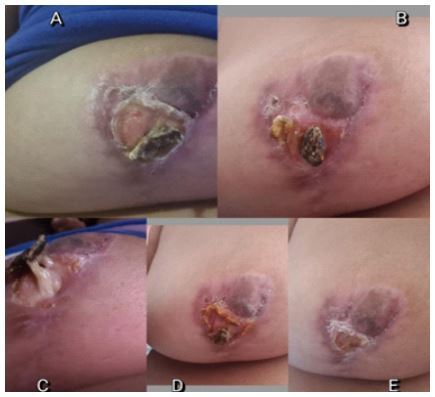
Figure 4, A-E: Aspect of the lesion from the tenth and twentieth sessions.
After the twenty-fourth session, the tissue has already been fully recovered and fibrosis at the site where the lesion was, showing the tissue completely healed, without bleeding and without production of fluids from the inflammatory process as seen in (Figures 5 and 6), leaving the optimistic patient and with improved self-esteem and non-psychological trauma suffered after the surgical complication.

Figure 5, A-B: Result of the twenty-fourth session.

Figure 6: Aspect in the breast at the end of treatment.
Aloe vera, popularly known as aloe, is a medicinal plant that brings benefits to skin health. The hydrating action of the plant has already been proven in several studies. However, there is still not enough scientific evidence to confirm its healing effect [7]. Pyrocatechol, cinnamic acid, ascorbic acid and p-coumaric acid are some of the substances involved in the bactericidal (destroying bacteria) and bacteriostatic (preventing the proliferation of bacteria) effect of Aloe vera. The plant has antimicrobial action and fights some types of fungi, viruses and bacteria [7, 8, 9].
The use of Aloe vera can aid in healing and re-epithelization (repair of skin tissue) in a short period, if properly indicated, in case of burns [10]. Infrared density therapy has an anti-inflammatory effect, through vasodilation, it also has a beneficial effect on nerve cells, decreasing sensitivity and blocking the pain transmitted by these cells to the brain [9]. The laser penetrates deep into tissue and accelerates cell reproduction and growth. In this way, it increases the energy available to the cell so that it can absorb nutrients more quickly and get rid of waste products. As a result of laser exposure, damaged cells are repaired more quickly [10, 11].
Blue light laser therapy stimulates the development of fibroblasts in the damaged tissue. Fibroblasts are the building blocks of collagen, which is the essential protein needed to replace old tissue to repair tissue damage. Thus, the technique is effective in improving the aesthetic appearance of surgical scars and in the treatment of open wounds and burns, reducing the formation of fibrous tissue and keloids [12]. Thus, we noticed that the therapy associated with laser brings several benefits, mainly by accelerating the healing process of the skin, leading to the best appearance of the tissue and reducing the lesion, being in this situation the best treatment available for the conditions and access to the technologies that the patient can enjoy [13].
Conclusion
Although mammoplasty is a surgery aimed at improving not only the quality of life of the patient, also helps in self-esteem. Is important stress the necessary care during these procedures so that no negative side effect occurs, as in the case presented? When the patient goes through this situation, she has a worsening in her health and self-esteem, because there may be cases where recovery is not possible, affecting that person's life permanently. Fortunately, with the technologies we currently have, it is possible to perform treatments for help with the problem. It was observed that the synergistic treatments that were performed corroborate the improvement in the recovery of breast tissue.
Acknowledgments
The Sara Magna Clinic – Dermatologist and Naturopath, the Coordination of the Biomedicine and Pharmacy Course at the Centro Universitário Ítalo Brasileiro and the Centro Universitário FMABC.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Mammoplasty#Aloe vera#laser therapy#mastopexy#surgical complications#Necrosis occurs#hypodermis#FMABC#Emerson Barbosa da Silva#JCMICR
0 notes
Text
Spontaneous Rupture of Wandering Spleen: Case Report by Mina Alvandipour in Journal of Clinical and Medical Images, Case Reports

Abstract
Keywords: Spleen; wandering spleen; ectopic spleen; splenic rupture.
Introduction
A wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [1]. wandering spleen is caused by either extreme laxity or absence of the normal ligaments that anchor the spleen to the left upper quadrant. Gravity also plays a role by allowing the spleen to descend into the lower abdomen attached by its vascular pedicle [2]. Symptoms depend on the degree of torsion and range from chronic abdominal pain in mild torsion to acute pain in severe torsion and infarction. Accurate clinical diagnosis is difficult because of the rarity of the condition and non-specific symptoms. Radiological evaluation includes usage of ultrasound, Doppler, abdominal CT or MRI depending upon availability or preference [3]. A wandering spleen can be either congenital or acquired. In the congenital condition the ligaments fail to develop properly, whereas in the acquired form the hormonal effects of pregnancy and abdominal wall laxity are proposed as determining factors .However, the precise etiology of the wandering spleen is not known [1]. We present a spontaneous rupture of a wandering spleen with severe torsion and infarction and abdominal pain without any history of trauma.
Case Report
A 25 years old female present to emergency unit with 2 week history of progressive abdominal pain, recurrent constipation ,vomiting and loss of appetite. There was no history of melena, fever, and hematochezia and weight loss. On examination there was periumbilical and epigastria tenderness and a firm and tender mass in the right side of the abdomen without muscle guarding and rebound tenderness. The vital sign and laboratory results were all within the normal ranges, except decreased hematocrit (hemoglobin-8.4). The plain abdominal radiograph was un-remarkable while abdominal ultrasonography with color Doppler showed absence of spleen in its normal location in the left upper abdomen. Also it detects a heterogeneous hypoechoic capsulated mass with diameter of 175mm in right lower abdomen. Other organs of the abdomen were normal. Abdominal pelvic CT scan with and without contrast was recommended and findings was Absence of the spleen in its normal position in the left hypochondrium, and presence of large diameter mass (splenomegaly)in the right sub hepatic area(Wandering spleen) . Other organs of the abdomen were normal. Contrast-enhanced computed tomography (CECT) of the abdomen revealed whirlpool sign near the umbilicus. The splenic parenchyma showed abnormal enhanced areas, suggestive of splenic torsion and infarction.
A final diagnosis was wandering spleen with torsion of the vascular pedicle and infarction. The patient underwent a total splenectomy. During the laparotomy, an enlarged and infarcted mass was seen in right side of abdomen. The characteristic “whirlsign” can be seen in the area of the splenic vascular pedicle, indicative of torsion. Histological examination confirmed total infraction of the wandering spleen. The postoperative course was uneventful, and the patient was discharged on the 4th day after the operation.
Discussion
A wandering spleen is a rare but well-known entity. The incidence is < 0.2%. It is more common in females than males between the second to fourth decade of life and children [4]. Splenic weight >500 g in more than 8 out of 10 cases [5]. Interestingly, it has been reported that one out of three cases of wandering spleen appears in children bellow the age of 10 years old [7].
Wandering is characterized by splenic hyper mobility that results from elongation or mal-development of its suspensory ligaments. It is also known as aberrant, floating, displaced, prolapsed, ptotic, dislocated or dystopic spleen. Ectopic spleen, splenosis and accessory spleens are separate clinical entities and must be distinguished from it [5]. If the pedicle is twisted in the course of movement of the spleen, blood supply may be interrupted or blocked, resulting in severe damage to the blood vessels .Acute splenic torsion compromises venous outflow, which causes congestion and impairment of arterial inflow. Pain is originated from the splenic capsular stretching with rapid splenic enlargement and localized peritonitis [6]. Etiology is congenital or acquired. In case of congenital anomaly, a failure occur in fusion of the dorsal mesogastrium with the posterior abdominal wall during the second month of embryogenesis. Acquired risk factors that predispose to wandering spleen include pregnancy, trauma and splenomegaly [7]. Splenic torsion is usually clockwise. Complications of splenic torsion include: gangrene, abscess formation, local peritonitis, intestinal obstruction and necrosis of the pancreatic tail, which can lead to recurrent acute pancreatitis [8].
Wondering spleen had nonspecific symptoms such as abdominal pain that make diagnosis extremely challenging. As a result, radiologists play a major role in the diagnosis of this condition and its complications. Torsion may occur acutely and present with infarction or peritonitis. Chronic intermittent torsion can lead to pain, splenomegaly, and functional splenectomy. Contrast-enhanced computed tomography (CT) is the best imaging tool to make this diagnosis, although ultrasound may be used as well. Imaging findings on CT include identification of a spleen in an abnormal location, or with an abnormal orientation in the left upper quadrant. Often the wandering spleen is identified as a “comma” shaped mass in abdomen, with no normal left upper quadrant spleen [9].
Laboratory investigations are non-specific. Thrombocytopenia, through a mechanism of spleen enlargement secondary to compression of the splenic pedicle is rarely found [7]. The clinical presentation of wandering spleen is variable; it is either asymptomatic or noted incidentally during physical and radiographic examination or presents as acute abdomen due to torsion with subsequent infarction. The most common presentation is a mass with non-specific abdominal symptoms or intermittent abdominal discomfort due to congestion resulting from torsion and spontaneous detorsion [10]. Today, the only recommended treatment for wandering spleen is operation [7]. Splenectomy is indicated for infracted spleen and sometimes for huge splenomegaly precluding splenopexy. Splenopexy is the choice of treatment if the spleen is not infarcted [6]. Splenic preservation is highly recommended for young patients—those under one year of age up to those in their thirties—who are at particular risk for overwhelming post-splenectomy sepsis [10]. This should be appropriately followed up by the prophylactic vaccines against post-splenectomy sepsis syndrome. Ideally they should be administered before surgery; however, in emergencies this is not always possible [1].
Conclusion
In this case, splenectomy was done due to spleen infarction. Laparotomy was done in this case because of low experience at laparoscopy splenectomy. This report highlights the investigations and management necessary for a patient who presents with an ischaemic torted wandering spleen.
Acknowledgement: None.
Conflict of Interest: None.
Funds: None.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Spleen#wandering spleen#ectopic spleen#splenic rupture#ligaments#Radiological#abdominal pain#CECT#splenopexy#Mina Alvandipour#JCMICR
0 notes
Text
Role of Alpha Fetoprotein in hepatocellular carcinoma by MuhammadWaqar Mazhar in Journal of Clinical and Medical Images, Case Reports

Abstract
Hepatocellular carcinoma prevelance rate is higher in Pakistan due to HCV mortality rate, consumption of Alchol, and regular smoking, higher level of AFP progression normal liver cells into fatty liver cells, after inflammation it convert into HCC.In this study, we find the correlation between AFP and hepatocellular carcinoma. AFP involve in development of liver cancer, LFT’s test elevation and HCV also cause of cancer.
Keywords: Hepatocellular Carcinoma; Alpha Fetoprotein; alanine amino transferases; aspartate aminotransferases.
Introduction
Hepatocellular carcinoma is the 4th most common malignancy in worldwide and it is leading cause of cancer like disease in liver, and it exceed more than 1 million deaths per year by 2030 [1]. Acute hepatitis and acute liver failure are the most serious medical condition that require early diagnosis by release of IL-6, TNF-α and elevated alanine amino transferases, aspartate aminotransferases, alkaline phosphatase and α -Fetoprotein that progress healthy liver in to fatty liver known as steatosis and then inflammation occur in this and leads to hepatocellular carcinoma [2]. Most cases of HCC due to the virus like HCV and HBV, Diabetic and obesity, alcohol related diseases, non- alcohol related diseases, carcinogens like aflatoxins compounds [3]. HCC is the most common cancer that have high mortality rate in cancers due to mortality of HCV and NLFD. In Pakistan HCC ratio high due to prevalence and mortality rate of HCV [4]. The major treatment of HCC are chemotherapy, radiotherapy, transplantation and surgery. Because the most cases diagnose at the late stage, surgery cannot be performed and drugs are the only treatment of HCC [5]. Most patients in HCC become more drug resistance drug resistance. Drug treatment is the best choice of patients who are not edible for surgery. HCC is usually resistance to chemotherapeutic drugs. Because it hinders liver cancer treatment. In recent years targeted drugs use as medication and immune checkpoint inhibitors are introduce for treatment [6].
In the previous research evidence indicates that alpha-fetoprotein has high false-positive rate in diagnosis of early stage of HCC. The EASL clinic practices shows that AFP as a biomarker for liver transplantation and drug indicator [7]. The AFP level increased in many patients’ ad its risk for progression of HCC. AFP, currently the only biomarker available for HCC drug treatment, function as immune suppressor and promote malignancy transformation in HCC [8]. HCC is resistant to traditional chemotherapeutic agents such as doxorubicin, tetrahydrofolate, oxaliplatin, cisplatin, and gemcitabine. currently the recommended drugs include such as targeted therapeutics and immune checkpoint inhibitors [9].
AFP is a glycoprotein that secreted by endoderm embryonic tissue. The lower level of AFP in blood due to AFP is decrease in mature hepatocytes and that AFP gene expression is blocked. It is possible that AFP involved in HCC development and progression become an important factor affecting HCC diagnosis and treatment. AFP plays an important role in promoting cancer cell proliferation and, inhibition cancer cell apoptosis.
LFT’s test performed for liver injury, alanine aminotransferases, aspartate aminotransferases and alkaline phosphatase. These enzymes are commonly elevated in liver disease patients. Alkaline phosphatase and AFP play important role in the diagnosis of cancer.
Case Study
The patient name was sikandar, age 56 patient feel pain in their abdomen and sudden loss of weight. The patient has already hepatitis C infection and their PCR results were positive with high viral load. Due to serious illness it admitted in emergency ward 12, Nishter Hospital Multan. The doctors panel referred some test and kept in observations for better health condition.
The total bilirubin level was 2.05mg/dl in their blood and their normal values 0.6 - 1.2. The serum glutamate-pyruvate transaminase level is 43U/L and normal values up to 40. Aspartate amino transferases and alkaline phosphatase level were high in blood respectively 151 U/L and 493 U/l show in (Figure 1). Its indicate liver injury and cirrhosis. The AFP test indicates correlation with Hepatocellular carcinoma. The AFP level in patient was 6101ng/ml and normal values were 0.1 – 10. Higher level of AFP indicates that HCC have positive relation with AFP to proliferate cancer. The test formed by fully automated state of the Art analyzer Beckman Coulter 700 AIJ.
https://jcmimagescasereports.org/wp-content/uploads/2022/10/fig-1-10.jpg
Figure 1: Liver function and Alpha Feto Protein test in patient.
After blood reports, doctor suggest ultarosund Computrised Tomography whole abdominal view. In view, spleen size becomes enlarged 6cm, calculi in gall bladder, heterogeneous patchy atrial enhancement of right lobe, and some nodules seen in both lobes of liver. The doctor findings the AFP correlation with HCC, splenomegaly, ascites, cholelithiasis and protosystematic collaterals.
https://jcmimagescasereports.org/wp-content/uploads/2022/10/fig-2-10.jpg
Figure 2: Ultrasound Computrised Tomography whole abdomen.
The patient diagnosed with hepatocellular carcinoma at last stage, and doctor reffered to liver transplantation in india. But after 4 weeks he cannot survive.
Conclusion
Hepatitis C was the major risk of hepatocellular carcinoma in Pakistan. Smoking and alcohol have big problem to influence HCC in humans. The case study show that alpha fetoprotein has correlation with HCC. Higher Alkaline phosphatase and serum Bilirubin level enhance the liver carcinoma. AFP play role in cell proliferation, cancer cell differentiation and cell cycle arrest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Hepatocellular Carcinoma#Alpha Fetoprotein#alanine amino transferases#aspartate aminotransferases#AFP#HCC#HCV#aminotransferases#enzymes#MuhammadWaqar Mazhar#JCMICR
0 notes
Text
Sub-Clavicular Hibernoma: A Rare Diagnosis of Lipomatous Tumor by Zaïd Boughaleb in Journal of Clinical and Medical Images, Case Reports

Abstract
Lipomatous tumors are the most common soft tissue tumors, including a large variety of benign and malignant lesions. Hibernoma is a benign lipomatous tumor originating from the brown adipose tissue inherited from the fetus. The diagnosis is often incidental, since the large majority are asymptomatic or very slow growing. Differential diagnosis with other lipomatous tumors is often challenging. Hence the diagnostic work-up is large and must be multidisciplinary. Biopsy and large resection with sane margins are the standard of care. We describe a 48-year-old male patient with a history of a painless, mobile, slow growing right sub-clavicular mass apparently evolving for eleven years. This patient underwent ultrasound, mammography, MRI, CT Scan and ultrasound guided large core biopsy at different points in time. We describe this case of a well-documented hibernoma of the sub-clavicular region in line with the current literature.
Keywords: CT scan; hibernoma; lipomatous tumor; MRI; ultrasound.
Introduction
Lipomatous tumors including a large variety of benign and malignant lesions are the most common soft tissue tumors, their prevalence increasing with age [1]. Sometimes, overlapping imaging features can be misleading in diagnosis [2]. Since the distinction between benign and malignant lipomatous tumor is challenging, especially when based on clinical and superficial work-up, the differential diagnosis of lipomatous tumors includes hibernoma [3]. Hibernoma is a rare, heterogeneous, slow growing fatty tumor of good prognosis [1], arising from brown fat precursors, representing approximatively 1% of all tumors derived from lipomatous tissues [1]. Usually, no symptoms are associated except when the enlarging mass impinges on local tissues4. To date a few thousand cases worldwide have been described [1].
Case Presentation
A 48-year-old male patient was referred to our mammography unit with a history of a painless, mobile, slow growing right sub-clavicular mass apparently evolving for eleven years. No skin redness, fever or signs of nerve or vascular compression were related. Previous ultrasound examinations reported a fatty mass with a diagnosis of lipoma (well-differentiated fatty tumor without suspicious radiological signs of malignancy [3]). Mammography showed a radiolucent mass consistent with a lipomatous origin on a targeted modified medio-lateral oblique view [5]. Ultrasound revealed a hyperechoic, homogeneous mass compared to the subcutaneous fatty tissue, measuring 11,5 x 3,6 x 10 cm, with vascular hyperemia on color-doppler ultrasound (Figure 1). MRI examination was performed to assess the precise extent and possible invasion of the underlying tissues. MRI described a mass measuring 10 x 3,9 x 9 cm with hypersignal on T2 sequence (but slightly lower than the subcutaneous fat signal [3]), hyposignal on T1 sequence compared to muscle structure (but slightly higher than subcutaneous fat signal [3]), very low signal on a fat suppression sequence and moderate enhancement on the post-contrast T1 sequence. No invasion of the adjacent soft tissues, muscles or bones was described (Figure 2). A CT scan without contrast media injection recently performed for other reasons showed a pre-pectoral low attenuation mass without involvement of the underlying tissues. In our case, density of the lesion was slightly higher than subcutaneous fat [5]. Eventually, diagnostic large core needle biopsies under ultrasound control were performed yielding the histological diagnosis of adipocytes with a microvacuolar and eosinophilic cytoplasm without signs of mitosis or necrosis. The diagnosis of hibernoma was raised. For aesthetic reasons, this patient was referred to our oncologic plastic surgeon; preoperative laboratory testing reported no evidence of metabolic disorder or infectious component [6]. Surgery showed a mass alongside the pectoral fascia, without muscle or vessel invasion. Histology confirmed the diagnosis of hibernoma.
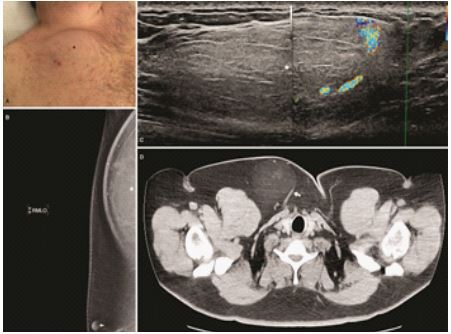
Figure 1: (A) Subclavicular swelling due to the clinical mass (black star). (B) Mediolateral modified oblique mammographic view showing a radiolucent mass (white star), nipple (with arrow). (C) Ultrasound: hyperechoic mass with peripheral vessels on color ultrasound (white star). (D) Axial non-enhanced CT scan showing the mass (white arrow).

Figure 2: (A) T2-weighted axial MRI image revealing a slightly hypointense mass compared to subcutaneous fatty tissue (black star). (B) Axial T1-weighted non-enhanced MRI image with fat suppression: hibernoma undistinguishable from adjacent fatty tissue. (C) Gross macroscopic specimen showing a lipomatous mass. (D) Axial T1-weighted MRI image with fat-suppression post Gadolinium injection demonstrating a slight enhancement of the mass (white arrow).
Discussion
Huge progress has been made since the descriptions by Merkel in 1906 and Gery in 1914 [7, 8]. Brown fat is a particular form of fat found in the hibernating and non-hibernating animals [9]. Representing approximatively 1,6% of all benign lipomatous tumors, hibernomas are very slow growing tumors usually occurring between the age of 20 and 50 years [11, 12]. Average age at diagnosis is 38 years and various gender predominance have been described in the literature. Intraosseous hibernomas are found in older patient [13]. The most common location, as the majority of fat tumors, are neck, shoulder and periscapular regions which are areas with possible remaining brown fat tissue [14]. However, hibernomas can occur anywhere in the body [15]. The clinical manifestations are rare, but might occur as a painless soft tissue mass, with a locoregional irritation or neurovascular compression [16]. Conventional radiography demonstrates a radiolucent mass with no adjacent osseous abnormalities or mineralization [17]. Ultrasound describes a rather uniformly hyperechoic mass [5], with increased vascular flow [17] generally unspecific, like other soft tissue tumors. In our case, the diagnosis of a typical lipoma [5] was ruled out due to vascular hyperemia on color doppler ultrasound. On CT scan, hibernoma presents as a homogenous low-density mass of lipidic composition between the attenuation of subcutaneous fat and skeletal muscle [5]. Contrast enhanced CT scan usually shows variable degree of enhancement [16] and intra-tumoral septas [10]. Diagnosis of hibernoma cannot be excluded based on the lack of intra-tumoral vessels [10]. On MRI, the imaging modality of choice [3], hibernoma shows an hypoT1 and hyperT2 signal because of the fatty component alike our case but differs slightly from the fat signal. On a fat-suppressed sequence, attenuation is similar to fatty tissue. After Gadolinium contrast media injection, enhancement is variable but predominantly present and rather heterogeneous [5]; a common sign are large flow voids indicating fast flowing flood in intratumoral vessels. Internal septation, one of the features of hibernoma [3], was absent in our case. High level of FDG uptake has been described in brown adipose tissue [16], sometimes even higher than liposarcoma [10] but overlapping results [2] prevent clear distinction between both tumors. Four types of hibernomas have been described, based on a histological classification [15]: the typical variant, the most common one like our case, the “myxoid” variant, the “lipoma-like” variant and the “spindle-cell” variant. Differences in imaging characteristics among these different histological subtypes of hibernomas are due to the variable amounts of water and fat content. One study distinguished between “lipoma-like” and “non lipoma-like” hibernoma [18]. Non-lipomatous hibernomas are probably indistinguishable from other liposarcomas [17]. Differential diagnosis of hibernoma is very large and may include benign tumors (lipoma, angiolipoma, hemangioma, hemangiopericytoma, hemangioblastoma, xanthoma, granular cell tumor, adult rhabdomyoma, lipoblastoma…) [16, 19] and malignant tumors (liposarcoma, clear cell sarcoma,…) 5, 10, 16. Clinical and imaging features as previously described may guide the diagnosis, but the histological examination gives the final diagnostic. In the absence of treatment, hibernoma continues to grow and leads to functional or cosmetic consequences 2. Tumor regrowth has been reported with incomplete excision of hibernoma 19. The standard of care of hibernoma is surgical removal with clear margins. Surgical excision is advised to rule out a possible malignant lesion with hibernoma-like differentiation which could be missed by core needle biopsy 1. No risk factor has been described [1]. Multiple lesions in a single patient are possible 21. After resection, the tumor generally does not recur. Since no malignant transformation or metastatic (22) spread have been described in the current literature, hibernoma can be considered as a benign tumor 1 for patients is 20.
In conclusion, the diagnosis of fatty tumors, often challenging especially with rare tumors like hibernomas, should comprise ultrasound, MRI and large core needle biopsies. Since hibernomas are benign tumors with no tendency to recur or metastasize, surgical resection with clear margins is recommended 17.
Declarations
Funding
This work did not benefit from any financial support
Conflict of interest
All authors declare no conflict of interest.
Ethical approval statement
The study has been approved by the Ethical Committee of the institution (76/2021).
Patient consent statement
A written permission to publish has been obtained from the patient.
For more details : https://jcmimagescasereports.org/author-guidelines/
#CT scan#hibernoma#lipomatous tumor#MRI#ultrasound#asymptomatic#sub-clavicular#hyposignal#Subclavicular#mammographic#Zaïd Boughaleb#JCMICR
0 notes
Text
Publications trends in major anesthesiology journals: A 20-year analysis of five top-ranked journals in the field by Stefan Koppert in Journal of Clinical and Medical Images, Case Reports

Abstract
Background: With the intention to quantify the importance of a medical journal, the impact factor (IF) was introduced. It has become a de facto fictive rating instrument of the importance of medical journals. Also, it is often used to assess the value of the individual publications within the specific journal. The aim of the present study was to analyze publication trends over 20 years in five high-ranked anesthesiology journals.
Methods: The Medline (NCBI) database PubMed was used for analysis which was restricted to the following journals: 1. Anesthesiology; 2. British Journal of Anaesthesia; 3. Journal of Neurosurgical Anesthesiology; 4. Anesthesia & Analgesia; and 5. Anaesthesia. Specific publication parameters (IFs, number of pages and authors, etc.) were retrieved using the PubMed download function and imported into Microsoft Excel for further analysis.
Results: The mean IF of the five journals analyzed increased significantly within the study period (1991 vs. 2010; +61.81%). However, the absolute number of case reports decreased significantly by 54.7% since 1991. The journals Br J Anaesth (12.2%), J Neurosurg Anesthesiol (51.9%), and Anesth Analg (57.2%) showed significant increases in the number of publications per year. The mean number of authors increased significantly in all the journals from 1991 to 2010 (3.0 vs. 4.3; +43.3%).
Conclusions: The IF, as well as the number of articles per year and the number of authors per article, increased significantly. In contrast, the number of pages per article remained comparable during the period analyzed.
Keywords: Impact factor; scientific publication; scientific journal; publication trend.
Introduction
The scientific productivity of a institution or person in medical research is reflected by the number of published articles [1]. However, both medical science and publication options have changed dramatically over the last several years. Publishing medical data in the new open access journals (OAJs) and via the World Wide Web (WWW) has gained significant importance recently. Although the classic printed journal was the standard for any years, it is now easily possible to publish peer-reviewed medical work without printing on paper. Publishing scientific medical papers remains the standard in medicine with regard to scientific reputation.
To quantify the importance of a medical paper, the impact factor (IF) was introduced by the Institute for Scientific Information (ISI, Thomson Scientific/Thomson Corporation, New York, NY, USA) in the 1960s [2]. The IF is a citation index calculated for a specific journal by dividing the number of citations within the last two years by the number of articles published [3, 4]. Therefore, it is a fictive instrument to rate the quality of a journal and the importance of an article because it is published within a specific journal [5]. The IF is relevant in medical research because it significantly impacts publication practice [6] and it has also gained enormous significance for research department funding [3]. The aim of the present study was to analyze the publication trends over 20 years in five high-ranked anesthesiology journals in Medline/PubMed [7]. We focused primarily on delineating trends in the IFs of each journal, as well as the numbers, types, and characteristics of each publication.
Material and Methods
Journals
The Medline (National Center for Biotechnology Information, NCBI, Rockville Pike, MD, USA) database PubMed (http://www.pubmed.com) was used for analysis [7]. Five high-ranked anesthesiology journals (excluding pain medicine), according to the Institute for Scientific Information (ISI, Thomson Scientific, Rockville Pike, MD, USA), were identified using InCites™ [2]. These top-ranked journals were selected by the highest IF in 2010. The IFs of these journals were gathered to analyze the trend in IF for each journal during the period from 1991 to 2010 [2]. Further analysis was restricted to the following journals: 1. Anesthesiology; 2. British Journal of Anaesthesia (Br J Anaesth); 3. Journal of Neurosurgical Anesthesiology (J Neurosurg Anesthesiol); 4. Anesthesia & Analgesia (Anesth Analg); and 5. Anaesthesia.
Data acquisition
For specific data analysis, the following publication information was recorded in the following data sets:
country of origin;
article type (i.e., randomized, controlled trial [RCT], clinical trial, comparative study, or case report);
number of articles per year and journal [n];
number of pages per article [n]; and
number of authors per article [n].
Letters to the editor, editorials, and comments were excluded from the analysis because they are not necessarily based on scientific, peer-reviewed data. All published articles from these journals were gathered by direct data import from PubMed via Microsoft Excel® 2003 (Microsoft, Redmond, WA, USA) for each year (1991-2010) and for each of the five journals (search string; e.g., "Anesthesiology"[Journal] AND ("2006/01/01"[PDAT]: "2006/12/31"[PDAT]). Data were retrieved using the PubMed download function (XML data format; “Extensible Markup Language“) and were imported into Microsoft Excel for further analysis.
Statistical analysis
Descriptive statistics were performed by using Microsoft Excel® 2003. The t-test and the Chi²-test were used for the statistical analysis. A value of p<0.05 was considered statistically significant.
Results
Impact factor analysis
Trends in the IF for each journal and year over the 20-year time frame (1991-2010) were gathered (Figure 1). During this period, the IFs of all journals increased (2.249 in 1991 vs. 3.639 in 2010; i.e., +61.81%). The IF of J Neurosurg Anesthesiol increased from 0.638 in 1992 to 2.205 in 2010, i.e., +245%. The smallest increase was +46.03% for Anesth Analg (from 1991 to 2010)

Figure 1: The trend in impact factors (IF) among the top five anesthesiology journals [2]. x-axis shows the years analyzed and the y-axis shows the impact factor (IF) during that time.
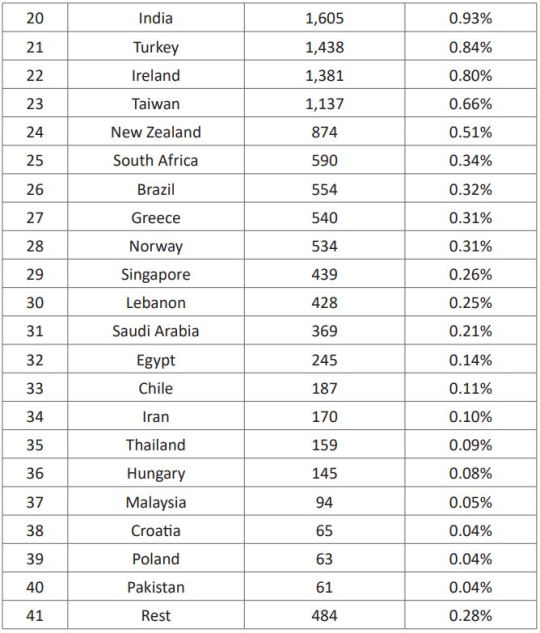
Country of origin
A total of 42,549 articles, containing 183,763 pages written by 154,437 authors, were found between January 1, 1991, and December 31, 2010, in the five journals. Among these articles, the greatest numbers of publications were submitted from the US (31.05%; Table 1), followed by the UK (13.64%), Japan (9.24%), Germany (7.68%), and France (6.22%).
Table 1: Country of origin, number of publications, and resulting rank (1991 to 2010).

Article type
The absolute number of comparative studies and randomized, controlled trials (RCT) was comparable between 1991 and 2010 (Figure 2) with minor changes during that time-frame. The number of case reports also varied from year to year; however, the absolute number of case reports decreased significantly by 45.8% between 2003 and 2010 and by 54.7% between 1991 and 2010 (p<0.0001; Figure 2).

Figure 2: Publication types (case reports, comparative studies, and randomized controlled trials [RCTs]).
Articles per year
During the time frame analyzed, the mean number of articles per year in each journal [n] was 425±226. Altogether, 42,549 articles were published in the five journals. Anesth Analg (n=14,085 of 42,549; 33.1%) published the most articles, followed by Anesthesiology (23.4%), Anaesthesia (22.5%), Br J Anaesth (18.6%), and J Neurosurg Anesthesiol (2.4%). In Anesthesiology, the mean number of articles published per year was 498.8±67.6 (maximum n=628 in 1999; Figure 3). Compared to 1991, the number of articles per year decreased by 5.0% in this journal until 2010 (p=0.009). In Anaesthesia, a decrease of 45.1% (p<0.0001) in the mean number of articles published was also observed between 1991 and 2010. In contrast, the journals Br J Anaesth (+12.2%; p=0.816), J Neurosurg Anesthesiol (+51.9%; p<0.0001), and Anesth Analg (+57.2%; p<0.0001) all showed increases in the numbers of publications per year.

Figure 3: Number of articles per year [n] in the top five anesthesia journals.
Pages per article
Although the mean number of pages per article (4.3±1.4) did not change between 1991 and 2010 (Figure 4; p>0.05), there were variations among the years. In the Br J Anaesth only, the pages per article remained stable during the time frame analyzed (p>0.05). In the other journals, the pages per article increased (Anesthesiology, Anesth Analg, Anaesthesia) or decreased (J Neurosurg Anesthesiol).
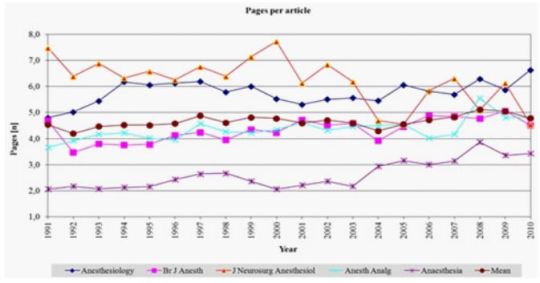
Figure 4: Pages per article [n] in the top five anesthesia journals.
Number of authors per article
The mean number of authors per article [n] was 3.6±0.7, which increased significantly in all journals from 1991 to 2010 (3.0 vs. 4.3, a relative increase of 43.3%; p<0.0001; Figure 5). Anesthesiology showed the smallest increase (1991 vs. 2010, 3.43 vs. 4.28 authors; relative increase of 24.8%), followed by Anaesthesia (2.3 vs. 3.2; +39.1%), Anesth Analg (3.35 vs. 4.67; +39.4%), and Br J Anaesth (3.08 vs. 4.62; +50%); the greatest increase was observed in the J Neurosurg Anesthesiol (3.0 vs. 4.8; +62.5%).
Discussion
The aim of the present study was to analyze publication parameters in five top-ranked anesthesia journals over a 20-year time frame. The following journals were analyzed: 1. Anesthesiology; 2. Br J Anaesth; 3. J Neurosurg Anesthesiol; 4. Anesth Analg; and 5. Anaesthesia. The absolute number of scientific publications has been rising since the 18th century [8]. Since then, the number of publications has doubled every 10 to 15 years [8]. This trend has been especially true in Anesthesiology, which has gained relevance recently, thereby resulting in a concomitant increase in scientific publications [9-11]
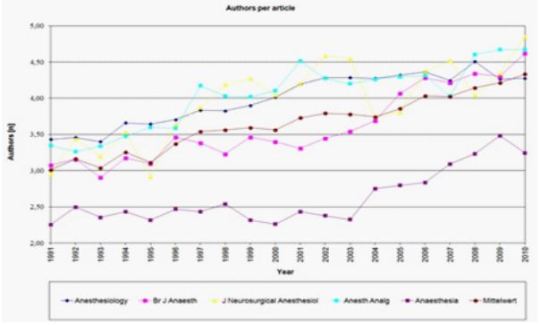
Figure 5: Number of authors per article [n] in the top five anesthesia journals (1991 to 2010).
Country of origin
In the present study, the vast majority of publications were submitted from the US, followed by Western Europe and Japan (Table 1). These data are in concordance with Li et al.’s study, analyzing journals between 2000 and 2009 [12]. The top five countries in the present investigation were among the top seven countries in the study by Li et al. [12]. Figueredo and colleagues also found that the USA, the UK, Japan, Germany, Canada, and France published the most articles in anesthesia journals between 1997 and 2001 [13]. In their study, the largest increase in scientific production in anesthesiology was observed in Germany [13]. However, they concluded that the geographical distribution of scientific production must not only be analyzed in absolute terms but should also be evaluated relative to other variables, such as financial spending on research and development, as well as population growth [13].
Articles per year
Altogether, 42,549 articles were published in the five journals within the time frame analyzed. In Anesthesiology, the mean number of articles published per year was 498.8±67.6. Compared to 1991, the number of articles per year decreased by 5.0% until 2010. In Anaesthesia, a decrease of 45.1% in the mean number of articles published was observed in the same period. In order to attain higher quality in journal articles and consequently a higher IF, several prerequisites for article acceptance have been developed in recent years. Currently, clinical trial registration, as well as plagiarism checks and ethical committee approvals, is a standard practice. Although this practice ensures higher-quality articles, it also could result in a decrease in the number of accepted publications.
Li et al. [14] confirmed these results in 18 different anesthesiology journals. The authors postulated that this decrease might be associated with an increasing IF. Feneck and colleagues also found a decrease in research publications from the UK in anesthesia journals from 1997 to 2006 [15]. In our study, the journals Br J Anaesth, J Neurosurg Anesthesiol, and Anesth Analg showed significant increases in the numbers of publications per year (1991 to 2010). Another study published by Li et al. [14] showed that these journals have decreasing numbers of articles while analyzing the period of 2000-2009 only. However, it is accepted that the absolute number of scientific publications is less important due to the difficulties that can occur in quality assessments of studies [16].
Impact factor analysis
Among the many surrogate parameters, the IF from the Institute for Scientific Information [2] has achieved the greatest popularity, especially in government research and medical schools [3, 4]. It is a common, but fictive, instrument for quantifying the importance of a medical paper based on citations [17] and it is used to rate the quality of a (medical) journal [4, 5]. Today, the IF also has enormous significance for research department funding [3, 18]. The IF was originally designed and sold as a product for advertisers, i.e., it was sold to advertisers, at very high costs for the purpose of helping them target their advertisements to the most widely read journals within the set of journals that were read by potential buyers of their products [19]. Although the IF is not an absolute measurement of the quality of a journal [3], it can quantify the influence of a journal in the medical field [4]. Because the IF influences medical research and funding [18], changes in the IF can significantly affect publication practice [6]. During the time frame analyzed, the IF of all journals in the present study increased (2.249 in 1991 vs. 3.639 in 2010; i.e., +61.81%). This phenomenon is not new and has been observed for several years also by other authors [20]. The median and highest IF in the present study have increased since 2005 [3]. This increase in IF has been observed for years [3, 20]. One main reason for the IF boom is the growth of research production [4, 20, 21]. More researchers are writing more contributions in more journals [22, 23] with more references [3]. In contrast, several journals have decreasing IFs, especially those in non-English languages and those that are difficult to access.
However, IFs can be manipulated by many strategies: self-citation; increasing editorials and reviews (more likely to be cited); and a reduction of the number of case reports (less likely to be cited) [4, 16, 18]. Therefore, the importance of the IF remains controversial [24] and there is no established current alternative available to rate the quality of scientific publications [4].
As the main factor that could lead to overestimate the IF is the amount of self-citations within a journal, in 2010 Landoni et al. [25] have suggested to apply a new metric called “new IF 20%”. This instrument, accounting the weight of self-citation with the aim of limiting their influence on the final result, is employed when the self-citation percentage is more than 20% of the total. Other authors present innovative journal metrics as IF substitute, e.g. the CAPCI factor (Citation Average per Citable Item) by E.P. Diamandis [26]. In addition, the International Committee of Medical Journal Editors (ICMJE) has outlined guidelines for the authorship of scientific papers [27], but it remains unclear whether authors comply with these prerequisites when submitting manuscripts. Therefore, the contributions of each author should not only be judged by the authors themselves but also by the editors to prevent misconduct by researchers and inadequate authorship.
Article type
Although the absolute numbers of comparative studies and RCTs were comparable between 1991 and 2010, there were significant variations per year. In contrast, the absolute number of case reports decreased significantly by 45.8% between 2003 and 2010 and by 54.7% between 1991 and 2010. Li et al. [14] also found a decreasing number of articles per year (both clinical studies and RCTs) when analyzing several different journals. Because case reports are cited less frequently in the years after their publication, publishing them can be counterproductive for a journal striving to obtain a higher IF. Therefore, publishing fewer case reports to enhance the IF might have motivated the major anesthesiology journals that were analyzed in the present study.
Pages per article
The mean number of pages per article was 4.3±1.4 and did not change between 1991 and 2010 (Figure 4; p>0.05). However, only in the Br J Anaesth the pages per article remained stable during the time frame analyzed (p>0.05). For Anesthesiology, Anesth Analg, and Anaesthesia the pages per article increased but decreased significantly for J Neurosurg Anesthesiol. However, due to lower publications costs and the availability of electronic publication [28], restrictions on the length of articles might not have been as relevant as such restrictions previously were.
Number of authors per article
The mean number of authors per article was 3.6±0.7 in the present study, and it increased significantly in all journals analyzed between 1991 and 2010 (3.0 vs. 4.3; relative increase of 43.3%). This increase was the lowest in Anesthesiology (+24.8%) and was significantly higher in the other journals (+62.5%). The increase in the number of authors per articles has also been a commonly observed phenomenon in other medical journals and in different countries [29, 30]. This phenomenon has been observed even in the most highly ranked journals (N Engl J Med, J Am Med Assoc, and The Lancet) [29, 30]. Kumar et al. [30] reported a gradual increase in the average number of authors over the past three decades [30]. Drenth et al. also found an increasing number of authors in the Br Med J [31]. These findings are congruent with the results of the present study, although different medical fields were analyzed. A number of reasons could be responsible for this phenomenon [30]. There has been an increasing trend toward cooperation among researchers in multiple disciplines and an increase in multi-center studies, as well as an increase in the complexity of research projects, which could facilitate collaboration and result in an increase in the number of authors per article [30, 32]. Additionally, it has been shown that studies with many authors are cited more often than studies with fewer authors, thereby contributing to the IF of the journal [23].
Limitations
The analysis in the present study was restricted to only five high-ranked anesthesiology journals listed in the Medline and PubMed database. All these journals are published in English. Due to the descriptive character of this study, it was possible to delineate variations in the specific publications measured, but it was not possible to provide definitive answers why these changes occurred. However, we used a 20-year time frame to compensate for variations in specific years. Although the journals were selected from the anesthesiology category of JCR, a few of the selected journals cover disciplines beyond anesthesia research.
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Granted by all authors.
Availability of data and material
On request.
Funding
None of the authors received financial or other support for the data analysis or for the writing of this manuscript. This study was not funded and did not require outside writing assistance.
Authors' information (optional)
All authors contributed significantly to the data analysis and to the writing of the manuscript.
Acknowledgements
None
Conclusions
The present study could provide some interesting insight into the trends in several specific publication measurements. When interpreted in the global context of biomedical publishing, the present study identified the potential publication strategies used to enhance the prominence of anesthesia journals. The IF (mean: +61.81%), as well the number of articles per year (+57.2%) and the numbers of authors per article (+43.3%) increased significantly between 1991 and 2010. In contrast, only the number of pages per article remained comparable during the period analyzed. It is impossible to offer definitive answers explaining why these measures changed, but these changes could partially be due to the authors (e.g., number of authors per article). In our opinion, the publication process would have greater transparency if journals would provide such data at the end of each year.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Impact factor#scientific publication#scientific journal#publication trend#Neurosurgical Anesthesiology#IF#anesthesiology#anesthesiology category#biomedical#Stefan Koppert#JCMICR
0 notes
Text
A 12 Day- Old Female Infant Diagnosed with Pelvic Osteomyelitis in the Pediatric Emergency Department by Mehmet Ali Oktay in Journal of Clinical and Medical Images, Case Reports

Abstract
Osteomyelitis (OM) is a bacterial disease that is very rare in newborns and has devastating consequences. Neonatal OM is seen in 1-3 in 1000 babies. We presented a 12-day-old female baby who was brought to the Pediatric Emergency Department (PED). Because she could not move her leg. She did not have fever and septic appearance and had a history of hospitalization in Neonatal Intensive Care Unit; acute phase reactants were high and radiological imaging performed gradually was consistent with OM. Our patient is the youngest patient who was diagnosed with pelvic OM upon admission to the PED. Earlydiagnosis and treatment prevent complications and sequels.
Keywords: Osteomyelitis; newborn; pediatric emergency
Introduction
Osteomyelitis often occurs secondary to the hematogenous spread of microorganisms into the blood-rich metaphysis of the developing bone. When left untreated, it leads to complications such as joint destruction and decreased range of motion [1]. Osteomyelitis (OM) of the hip is rare in newborns. Signs and symptoms are quite different compared to older children. This may cause difficulties/delays in diagnosis and permanent disability [2]. Successful management of OM in the neonatal period has been associated with rapid correct diagnosis and adequate correct treatment [2, 3]. The incidence of OM in the pediatric age group is 1/5000 cases. About 50% of pediatric OM cases are under the age of five. The incidence of neonatal OM is 1-3/1000 cases [3]. Although there are studies on patients diagnosed with osteomyelitis while staying in neonatal intensive care unit (NICU) [1, 4, 5], cases diagnosed upon PED (Pediatric Emergency Department) admission are very rare [6]. In this article, the youngest case in literature who went to the PED and was diagnosed with pelvic and acetabulary OM is presented.
Case Report
A 12-day-old girl, born from the first pregnancy of a 28-year-old mother, was admitted to the PED with complaints of restlessness and inability to move her right leg. The day before the application, it was stated by her mother that she did not move her leg, that she was agitated when forced to move, and could not be consoled. The baby did not have a history of fever or trauma, her feeding was good, and her urine and defecation were normal. From her history, it was learned that she was born at 36 weeks and 3 days of gestation and had intrauterine growth retardation compatible with 31 weeks gestational age, and she was born by emergency cesarean section due to preeclampsia. The patient, who was hospitalized in the NICU due to temporary tachypnea of the newborn after birth, was discharged on the sixth postnatal day. During the follow-up in the NICU, umbilical catheterization was not applied to the patient. She had not received antibiotic treatment and no growth was detected in blood cultures taken before discharge.
At her evaluation in the Pediatric Emergency Department triage area, she was a restless baby with a good general appearance. Vital signs; body temperature was 37°C, heart rate was 140/min, respiratory rate was 42/min, pulse oximetry was 98%, and mean arterial pressure was 45 mmHg. There was no pathological finding in the physical examination, and it was observed that the patient's discomfort increased due to the position given to the hip and leg while changing the diaper. While abducting the right thigh from the hip in the supine position, there was limited range of motion compared to the left. No swelling or redness was detected on the joint surface.
Laboratory and radiological examinations were planned for the patient with a preliminary diagnosis of septic arthritis. In laboratory tests: hemoglobin (Hb) 14.6 g/dL, RBC (Erythrocyte) - 3.361 x10.e6/uL, hematocrit (Hct) 40.04%, white blood cell (WBC) 16.82 x10.e3/uL, neutrophil percentage 59.8%, C-reactive protein (CRP) 25.9 mg/L, erythrocyte sedimentation rate (ESR) 51 mm/hr, procalcitonin (PCT) 2.95 ng/mL, IL-6 145.6 pg /mL detected. On direct radiographs of the lower extremity and pelvis, the right femoro-acetabular distance was observed to be increased (Figure 1). Long bone radiographs were normal. In the superficial tissue ultrasound (US) performed for the right hip joint, bilateral hip joints were compared with each other, and no significant effusion was observed on the right side. The patient was consulted to the Orthopedics and Traumatology department with a preliminary diagnosis of septic arthritis. MRI was requested from the patient for the differential diagnosis of septic arthritis.

Figure 1: There is an increase in the right acetofemoral distance compared to the left.
Bilateral hip MR imaging showed “The right femoral head is small and irregular in appearance, and an area of pathological signal change in the right femur proximal metaphysis, medullary bone marrow, and solid periosteal reaction in the lateral proximal section is observed. Widespread edema was observed in the surrounding muscle planes, fascial surface and subcutaneous adipose tissue adjacent to the hip joint. In addition, medullary bone marrow edema was observed in the right acetabulum (osteomyelitis). Areas of pathological signal changes consistent with diffuse edema are observed in the right obturator externus, pectineus, quadriceps muscles, gluteal muscle planes and iliacus muscle (myositis). Minimal free fluid was observed in the right hip joint space. Findings were primarily evaluated as compatible with osteomyelitis and myositis.” (Figure 2).

Figure 2: Osteomyelitis in the proximal metaphysis of the femur
Due to the history of hospitalization in the intensive care unit, the patient was diagnosed with OM secondary to hematogenous spread and, according to the age, to include possible infectious agents, vancomycin (15mg/kg/dosex3), ceftazidime (30 mg/kg/dose x 3), fluconazole loading (12 mg/kg/dose)) and maintenance (6 mg/kg/dose) treatment was started. Blood culture was taken before antibiotic treatment. Our patient, who received antibiotic doses only one day before the operation, was operated on the postnatal 13th day.
The patient was operated by the Orthopedics and Traumatology department and the intra-articular pus was drained. From the material; joint fluid culture, fungal culture, tuberculosis PCR, ARB staining, fungus search was sent. There was no growth in the blood culture, but because of the growth of ceftazidime-resistant Klebsiella pneumoniae in the joint fluid culture, ceftazidime was discontinued and meropenem (20 mg/kg/dosex3) treatment was started. Fluconazole was discontinued on the 8th day because there was no growth in the fungal culture. The patient was discharged with oral trimethoprim-sulfamethoxazole treatment after 25 days of vancomycin and 27 days of meropenem treatment. Trimethoprim-sulfamethoxazole was discontinued 22 days after discharge. The regression of the inflammation was seen in the MRI taken under the control of the outpatient clinic. verbal consent was obtained from the patient's parents for the publication of the article.
Discussion
This case demonstrates the importance of detailed investigation of newborn infants admitted to PED. Although OM in newborns is rare, there are difficulties in diagnosing and treating it. High suspicion is required for early diagnosis and observation of clinical signs is very important.
Risk factors for osteomyelitis in newborns are stated as immature host-defense mechanisms, invasive intervention such as umbilical catheterization. It has been shown that half of the cases diagnosed with neonatal OM have a history of umbilical catheterization. It has been observed that the pregnancy and delivery history of the mother is also important in the development of OM, and maternal complications such as maternal hypertension, preeclampsia, ablatio placentae, infection are present in approximately half of the infants who develop OM [7]. Particular attention should be paid to the evaluation of newborn cases, especially in PEDs where is crowded and the number of patient admissions is high. Newborns are among the patients at risk for PED and require special care. Application complaints and prenatal, natal and postnatal history should be questioned in detail. It was observed that the mother of our case had preeclampsia during pregnancy, but umbilical catheterization was not applied to the baby.
In studies conducted in newborns with neonatal osteomyelitis, the most common sites of involvement were reported as femur, humerus, and tibia, respectively [1, 4, 8]. The pelvis is a rare site of hematogenous disseminated OM for neonates. Pelvic OM constitutes 2.3% of all childhood osteomyelitis cases [3]. Our case also had pelvic (acetabular) OM, which is a rare site of OM involvement. Involvement was also demonstrated in the proximal region of the right femur.
Pelvic OM was defined in three cases at 5, 15, and 18 days in the neonatal period [3, 9, 10]. In the literature, it has been observed that mostly cases hospitalized in the NICU were diagnosed with osteomyelitis [1, 3, 4, 8-10]. As far as we can find in the literature, a 4-week-old case with a diagnosis of distal tibial OM and culture of GBS has been reported, just like our case [6]. Our case is the youngest OM case diagnosed in the emergency department, except for the case in the literature. The clinical features, presentation symptoms, cultures and risk factors of cases diagnosed with neonatal osteomyelitis in the literature are shown in (Table 1)
Table 1: Comparison of cases with neonatal osteomyelitis in the literature.
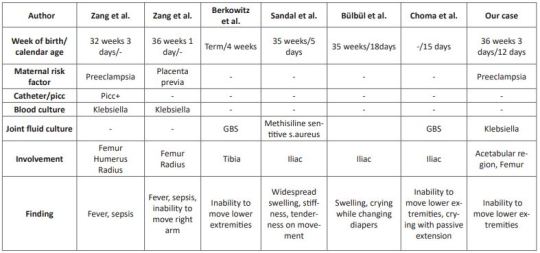
Clinical symptoms are related to the bone or joint area involved in newborns. Swelling and local inflammation findings are common findings in the neonatal osteomyelitis group. Systemic findings such as fever are seen in fewer of these cases. A highly variable rate of fever was found in 9.1-76.5% of patients with extensive neonatal osteomyelitis. In addition, it has been shown that the WBC count, CRP and ESR levels are high in the cases [1, 4, 8, 11]. In our case, there was no fever, but there were complaints of inability to move her right leg and restlessness. Laboratory parameters were high and consistent with the literature. In cases with osteomyelitis, direct radiographs can guide the correct diagnosis, exclude other diagnostic possibilities, or provide clues for underlying pathological conditions [12]. Soft tissue swelling on plain radiographs can be seen within days of the onset of infection. It can also show periosteal reaction, lytic lesions, joint effusions and destructive bone changes 7-10 days after the onset of infection [13]. US findings begin with nonspecific swelling in the soft tissues adjacent to the bone. US can show thickening and elevation of periosteal and subperiosteal fluid collections as early as 3 days [14]. In a study comparing osteomyelitis groups, it was shown that the diagnostic value of US was statistically higher in the newborn group compared to the other groups, regarding the capacity of detecting subperiosteal abscesses [11]. In our case, however, an increased femoro-acetabular distance was observed on direct X-ray, but no finding was found on US. This supports the view that the primary step in the pediatric emergency department in patients with suspected osteomyelitis should be started with direct X-ray as recommended in the literature.
MR imaging is the most useful imaging technique for evaluating suspected OM, allowing early detection of osteomyelitis and assessment of the extent of involvement and disease activity. MRI is very sensitive in detecting OM 3-5 days after the onset of infection [12]. As seen in our case, it still remains the gold standard. However, we recommend hospitalization in order not to miss the newborn cases because MRI is difficult in emergency conditions.
In infants, osteomyelitis and septic arthritis often coexist. While Staphylococcus aureus is the most common organism causing osteomyelitis at all ages, GBS and Escherichia Coli are important pathogens to be considered in newborns [6]. Culture is found to be negative in 22-50% of the cases [15]. Antibiotics to be used in neonatal OM should be effective against these pathogens [16]. In our case, treatment with antibiotics covering these pathogens was applied and Klebsiella pneumoniae growth was observed in the pus culture.
We think that even with rapid diagnosis and aggressive treatment, there are orthopedic sequelae and inadequate treatment increases the risk of chronic osteoma [16], therefore, in cases who apply to the pediatric emergency department with these complaints, early diagnosis and treatment of neonatal OM should be planned in a timely manner to minimize long-term sequelae.
In conclusion, a detailed anamnesis should be taken and a careful physical examination should be performed in newborns who present to the PED with limited range of motion at joints. Neonatal OM cases mostly consist of cases diagnosed while staying in the NICU. Pelvic involvement is rare and our case is the youngest pelvic OM case diagnosed in the PED.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Osteomyelitis#newborn#pediatric emergency#Pediatric Emergency Department#OM#PED#catheterization#RBC#C-reactive protein#hematocrit#Traumatology#Mehmet Ali Oktay#JCMICR
0 notes
Text
Depression among university students during Vietnam’s fourth wave of the COVID-19 pandemic by Le Minh Tu Phan in Journal of Clinical and Medical Images, Case Reports

Abstract
The novel human coronavirus disease COVID-19 has been continuing to spread around the world, causing serve economic and social consequences worldwide. From the fourth wave of COVID-19 pandemic, thousands of Vietnamese people have been infected every day, making it the biggest outbreak of COVID-19 in Vietnam. Due to the most serve wave of COVID-19 in Vietnam, the concerns about a rising mental health burden have been grown. University students who are still suffering are one of the hardest-hit subjects of the pandemic. This study aims to determine the level of depression, attitudes, and behaviours of university students in Vietnam under these circumstances. A cross-sectional online survey was conducted on nationwide students from August to September 2021. The Patient Health Questionnaire-9 (PHQ-9) scale was used to evaluate the level of depression. The difference between the percentages of qualitative variables was tested using the Chi-square test. Out of a total of 302 university students, 46.0% had depression symptoms, 6.0% and 3.6% for moderately severe and severe, respectively. 80.5% of university students adhered to the Vietnamese 5K guideline. However, 33.4% of students did not wash their hands after coughing and sneezing. Additionally, 44.7% of university students increased physical activity at home; 36.8% used electronic devices over 8 hours/day for sedentary entertainment. The findings indicate a high risk of depression and decreased physical activity among university students during the COVID-19 pandemic. It is expected that the mental health problems of Vietnamese university students during and after the pandemic should be paid an intense attention from both the government and universities to eliminate the depression of university students.
Keywords: Depression; vietnamese student; mental health; mental disorder; physical activity; 5k vietnamese guideline.
Introduction
The novel coronavirus (SARS-CoV-2), which causes acute respiratory distress syndrome, was first reported in December 2019 in Wuhan City, Hubei Province, China [1]. In Vietnam, the first case recorded on January 17, 2020, was a woman returning from Wuhan city, China [2]. As of November 4, 2021, Vietnam has experienced four waves of COVID-19, with the total number reaching 946,043 cases [3]. During the fourth wave, from April 27 to November 4, 2021, the number of COVID-19 infections in Vietnam was 941,159, resulting in a variety of economic and social consequences [3]. During the pandemic, Vietnam has been facing high number of infections, economic recession, and limited social interactions, contributing to risk for mental health issues.
In recent years, depression has impacted 264 million people globally, about half of whom experience symptoms at the age of 14. This condition may lead to suicide - a second leading cause of death among young adults (15-29 years old) [4]. Due to the COVID-19 pandemic outbreak in Wuhan City, Hubei Province, China, 17.9% of depressive cases and 8.5% of cases with the risk of suicide and self-injury were recorded [5]. Based on the negative impacts on the increased mental health problems in general populations, concerns have been raised about the potential impact on the students’ psychology, attitudes, and behaviour. According to the survey in China, 41.52% of students were depressed, and 2.03% had suicidal behaviour [6]. Along with psychological effects, the COVID-19 pandemic had an impact on students' lives, social relationships, and daily routines [7]. During the quarantine period, physical activity decreased while spending time on electronic devices for sedentary entertainment increased [8]. Despite the fact that face masks and hand washing are effective methods of infection prevention [9], Vietnamese students had low adherence to these preventive measures, with only 48.9% washing their hands after coughing or sneezing and 72.8% wearing a mask with a positive attitude [10, 11]. It might not only increase the risk of disease transmission but decrease the effectiveness of disease prevention strategies.
University students account for a considerable proportion of the Vietnamese population and will be the country’s future labour force. However, they have been suffering the serve impacts during the ongoing pandemic, such as being unable to physically interact with teachers and friends, suffering from an increased level of depression, having fewer physical activities. To our knowledge, there is still not a specific study in Vietnam that could evaluate the impact of the fourth outbreak on university students' mental health. Therefore, this study has been conducted to determine the level of depression, the changes in attitude and behaviour of university students in Vietnam during the COVID-19 pandemic.
Method
Students studying at universities/colleges in Vietnam.
Place and time
From August to September 2021 in Vietnam.
Study design
Descriptive cross-sectional study.
Sampling size
This study collected by convenience sampling technique. University students over 18 years old who reside in Vietnam are recorded. The sample size was calculated using the popularity estimating formula with the following assumptions. The rate of mild to severe student depression in Bangladesh was 82.4% [12], with a 95% confidence level, a precision error of 5%, and a non-response rate of 10%. The required sample size was calculated about 246 people; hence, this survey collected the information of 308 Vietnamese students.
Sampling methods
An online survey was conducted via google form. The questionnaire link was sent to student at nationwide universities through forums, study groups, clubs on social networks (Zalo, Facebook...), students were introduced to the research objectives and invited to participate in the survey.
Variables
Qualitative variables such as demographics, levels of depression (minimal, mild, moderate, moderately severe, and severe), attitudes towards the 5K Vietnamese guideline (including Declaration - Distance - Disinfection - Mask – No gathering), changes in physical activity behaviour (increase, decrease, unchanged), and spending time on electronic devices. Attitude is described as a person's mental propensity that governs how they think about executing the 5K Vietnamese guideline. Behaviour refers to their activities, such as strictly following the 5K Vietnamese guideline or engaging in other physical activities during the ongoing pandemic.
Data collection
The data was collected through a questionnaire consisting of three main parts: (1) Demographic information: age, gender, quarantine status, number of family members, access to information on disease prevention. (2) Assessment of the depressive level through the Patient Health Questionnaire-9 scale (PHQ-9): Through 4 corresponding levels (0-Not at all; 1- Several days; 2- More than half of the days; 3- Nearly every day). Thus, the total score to determine depression is based on 5 levels: minimal (0-4 points), mild (5-9 points), moderate (10-14 points), moderately severe (15-19 points), severe (20-27 points) [13]. This part of the question was translated into Vietnamese and validated for Vietnamese people. (3) Evaluation of the changes in attitudes and behaviours: level of physical activities at home during the pandemic (increase/decrease/unchanged), wear a mask, wash hands frequently with soap or antiseptic solution, keep a distance from others, make health declarations, and other factors.
Statistical analysis
Data was imported and cleaned by Microsoft Excel 2019. Descriptive statistics were reported in frequency and percentage. A Chi-square test was applied to compare percentages between groups. Statistical analysis was performed using MedCalc version 20 software.
Ethical issues
All participants were introduced to the survey. If they agreed, they would answer "Yes" to the first question indicating their consent to participate in the study and they are not bound by anything. The data collection was completely anonymous and used for research purposes only.
Table 1: Demographic characteristics.
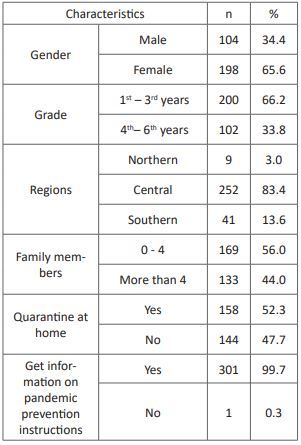
Result
Demographic characteristics
A total of 308 participants were recorded. Six cases were excluded for not residing in Vietnam (n = 4), not agreeing to participate in the study (n = 1), and not completing the questionnaire (n = 1), resulting in a total of 302 samples being used for analysis. Most students are female (n = 198; 65.6%) and 1st to 3rd year students (n = 200; 66.2%), mainly living in the central Vietnam (n = 252; 83.4%). The common members of their family are less than 4 people (n = 169; 56.0%). Almost all university students have received instructions on pandemic prevention measures (n = 301; 99.7%). The detailed demographic characteristics are presented in (Table 1).
Correlation of student depression and related issues
The PHQ-9 scale was used to assess the level of depression. Nearly half of university students have depression (46.0%), 6.0% for moderately severe and 3.6% for severe depression, respectively (Figure 1).
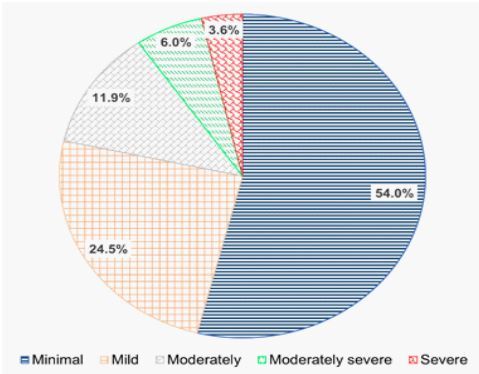
Figure 1: Level of depression among the students.
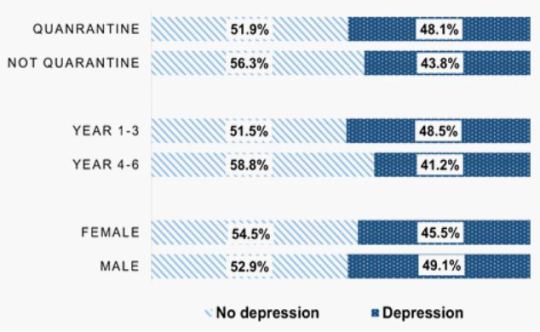
Figure 2: The percentage of depression and related issues.
(Figure 2) shows the proportion of depression among male students at 49.1% and among students from year 1 to year 3 at 48.5%. The rate of depression varies according to quarantine status, with higher proportion (48.1%) of individuals who have been quarantined experiencing depression compared to 43.8% of participants who have not been quarantined.
The correlation between demographics and the degree of depression factors was evaluated using the Chi-square test. The results show that depression proportion among female students is higher than that among male students. Among the students with severe depression, up to 81.8% are female, and the difference is statistically significant (p = 0.004). In addition, depression mainly occurs among 1st to 3rd-year students with the rates of moderate and moderately severe depression at 69.4% and 66.7%, respectively. Other differences are presented in detail in (Table 2).
Table 2: Correlations of depression and related factors.

Students' attitudes and behaviours during the COVID-19 outbreak
People who increased physical activities at home account for a larger portion (44.7%) than those who reduced physical activities (27.2%) as shown in (Figure 3A & Figure 3B) displays that 36.8% of university students used electronic devices for sedentary entertainment over 8 hours/day, higher than that before the pandemic occurred (11.6%). The percentage of people used electronic devices from 0 to 2 hours per day decreases by more than half compared to that before the pandemic (10.9%).

Figure 3: A - Level of physical activity at home; B - Comparison of spending time on electronic devices among students for sedentary entertainment before and during the pandemic.
Most university students have a positive attitude to adhere to the 5K Vietnamese guidelines of the Ministry of Health, 95.4% wear masks, 89.7% wash their hands regularly, and 90.1% do not gather in crowds. But the proportion of students who do not fully follow the 5K guidelines is still quite high at 19.5% (Figure 4A). Most of student reported that they have been wearing mask when leaving home (94.4%), including places such as medical facilities (98.3%), schools/workplaces (96.4%), residential areas (96.4%) as shown in Figure 4B. Regarding hand-washing behaviour, 90.4% of students reported to wash their hands after returning from public locations, whereas 24.2% and 33.4% of students reported not to wash their hands after close contact with others and not to wash their hands after coughing or sneezing, respectively (Figure 4C).

Figure 4: A - Students' attitude towards adherence regarding the 5K Vietnamese guideline; B - Mask-wearing habits of university students; C – Hand-washing habits of university students.
Discussion
The COVID-19 pandemic has had a negative impact on the mental health of the community in general and students in particular. Our study has assessed the impact of the pandemic on mental health, attitude, and behaviour of Vietnamese university students during the fourth COVID-19 wave. 46% of the students have a high level of depression with 9.6% of moderately severe and severe levels of depressive symptoms. Depression affects an individual's health, increases the risk of coronary heart disease and of suicidal ideation [14, 15]. We found that the depression proportion among Vietnamese university students is similar to that of Bangladeshi students (46.92% depressed) [16] but higher than that of students in Saudi Arabia (25.4% depressed) [17]. Compared to Spanish students, Vietnamese university students also have a higher rate of depression [18]. In Vietnam, when the community first practiced social distancing, there was a study to assess the level of psychological trauma among people with depression [19]. These percentages are lower than that of the results (46.0%) in our study, indicating that university students have been among the most heavily affected people during the pandemic. The findings also show that the rate of depression among 1st to 3rd-year students (48.5%) is higher than that of 4th-6th year students (41.2 %). The number of students in 1st to 3rd years with both moderate and moderately severe symptoms (69.7% and 66.7%, respectively) is twice as much as that of the students in 4th to 6th years (30.6% and 33.3%, respectively). One possible reason is that students in their 4th to 6th years have more stable mentality than students in their first years owing to higher level of emotional maturity. They are more psychologically stable when confronted with mental health conditions. Therefore, evaluating students’ perceptions, knowledge, and attitudes may aid in identifying characteristics that form healthy practices and responsive behaviours, as well as strengthening prevention efforts against significant mental health problems [20]. To help students improve this condition, we should encourage them to increase social interaction or introduce them to skill courses on emotional control, nurturing and healing from within, especially for first-year students. Additionally, meditation can be good therapy for the stress caused by the COVID-19 pandemic [21]. Other findings demonstrate that girls have a higher proportion of depression than boys, as up to 81.8% of depression cases are among female students. This shows that women are more susceptible to psychological trauma than men, suggesting that it is necessary to pay intense attention to women's mental health. On the other hand, the proportion of students experiencing depression is mainly recorded among students living in the central region, where the pandemic outbreak is not as strong as that in the southern region. Thus, when the scope of the study is expanded to areas where the outbreak is more intense, the incidence of depression might reach much higher levels, leading to an alarming situation. Apart from reviewing and tracking the number of infected cases, it is essential for Vietnamese government to focus on mental health care to minimize negative consequences for people, the economy and society.
When implementing social distancing measures for a long time, schools are closed, making the changes in students' daily habits, with 22.5% of students using electronic devices for sedentary entertainment from 6 to 8 hours and 36.8% for more than 8 hours a day. Increased spending time on electronic devices can cause sleep disturbances and increase the risk of cardiovascular diseases such as high blood pressure and coronary heart disease. Additionally, it also affects mental health by causing depression, even suicide [22]. Our study also recorded an increase in physical activities at home during social distancing (44.7%). In this survey, the non-depression rate in students is 54%, with attitudes of compliance with 5K guidelines (95.4%), 89.7% washing their hands on a regular schedule, and 90.1 % not gathering over 5 people. These results exhibit the positive attitude of university students that might help them avoid depression. Wearing a mask and washing hands are both highly prevalent in this study (except at home: 49.3 %), which may be associated with a higher proportion of non-depression. Many students have a good attitude towards the 5K guidelines, 94.4% of which wear masks anywhere outside their home. Nevertheless, one fifth of university students (19.5%) have not strictly followed the 5K guidelines of the Vietnam Ministry of Health. This may bring about consequences including the increase of infection risk and disease transmission in the population. Viruses are spread by the respiratory tract when mucus or respiratory secretions containing the virus enter the body from the eyes, nose, or throat, mainly through the hands. Therefore, hands are also a common way for viruses to spread from person to person [23]. Thus, frequent hand washing is an effective measure to reduce the risk of infection and spread to the community. Our study shows that 33.3% of the students did not wash their hands after coughing and sneezing, exhibiting the increase of the infection risk. Thus, it is necessary to intensively propagandize the preventive measures to the population. Besides, the further study needs to be conducted with the enlargement of sample size to more accurately evaluate the level of psychological vulnerability, attitude, and behaviour of Vietnamese university students.
Conclusions
In conclusion, this study gives the evidence that nearly half of Vietnamese university students show signs of depression, exhibiting a relatively high percentage of students’ depression during the Vietnam’s fourth wave of the COVID-19 pandemic. Most students strictly adhered to the 5K guidelines, but it still remains a high percentage of students who have not practised hand washing after coughing and sneezing. Due to the increase of spending time on electronic devices for sedentary entertainment, students' dependence on electronic devices has become higher during the pandemic. We highlight the risk of mental health issues among students during the ongoing pandemic, which can have serious and long-term consequences on their life. Further, the study with larger sample size is highly required to assess more accurately the level of psychological vulnerability, attitude, and behaviour of Vietnamese students. It is essential to develop the government policy to help university students reduce the depression among the university students. Both the government and universities could cooperate to reduce the mental health problems, improve the fitness, and build a healthy lifestyle for the better life quality of university students.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Depression#vietnamese student#mental health#mental disorder#physical activity#5k vietnamese guideline#Le Minh Tu Phan#JCMICR
0 notes
Text
A mysterious intra-cardiac needle discovered accidentally during pericardiothentesis under fluoroscopy by Hesham Alkady in Journal of Clinical and Medical Images, Case Reports
Abstract
Due to the rarity of retained intra-cardiac sewing needles, no clear guidelines exist regarding the indication for their extraction. In this study we report a case of a sewing needle extracted from the right atrium of an adult female presenting with recurrent pericardial effusion after one year of accidental penetration.
Keywords: Intra-cardiac needles; pericardiothentesis; echocardiography; cardiopulmonary bypass; sternotomy.
Introduction
Intra-cardiac sewing needles detected in adults and children may be due to accidental penetration e.g. while sleeping, self-inflicted as a result of mental and psychic disorders or domestic abuse [1, 2]. Due to the rarity of retained intra-cardiac sewing needles, no clear guidelines exist regarding the indication for their extraction. Conservative or operative options should be individualized according to the timing of presentation (acute or delayed), presence of symptoms (e.g. chest pain, infection, arrhythmia) as well as location [3]. In this study we report a case of a sewing needle extracted from the right atrium of an adult female after one year of accidental penetration
Case report
A 60 year old female patient was referred to our outpatient clinic due to a needle found by the cardiologist during pericardiothentesis under fluoroscopy for increasing pericardial effusion. (Video)
The clinical history, physical examination as well as laboratory studies of the patient were unremarkable apart from recent progressive shortness of breath since 2 months. Therefore the cardiologist decided to do a pericardial aspiration with chemical, bacteriological and cytological examination of the pericardial fluid after increase its amount despite of diuretic therapy. The pericardial aspirate was sero-sanguinous exudative in nature, negative for organisms and malignant cells. The patient had no explanation how a needle reached this place and she did not receive any major procedure before could be the cause. The patient is also well-educated and her mental as well as psychological assessments were within normal. A transthoracic echocardiography showed an echogenic linear object at the wall of right atrium, unclear whether inside or outside the atrial cavity, as well as mild pericardial effusion with thickening of the pericardium. Multi-slice CT chest showed that the needle lies inside the right atrial cavity embedded in its wall (Figure 1).

Figure 1: A Multi-slice CT of the chest showing the needle in the right atrial cavity as well as collected pericardial effusion on its lateral surface. The pericardium appears slightly thickened.
The possible hazards of leaving the needle in the heart were explained to the patient as well as the advantage of biopsying the pericardium during surgical extraction to determine the cause of recurrent effusion. The patient was first terrified from the surgical intervention; however she consented surgery at the end. Through full median sternotomy, the thickened pericardium was opened and sero-sanguinous effusion was evacuated. Some adhesions were found on the anterior surface of the heart especially right atrium. Trials to locate the needle by digital palpitation of the right atrium were unsuccessful. A mobile C-arm X-ray machine was brought to the operation room to confirm the position of the needle inside the right atrial cavity. Cardiopulmonary was then initiated via aorto-bicaval cannulation. After snaring of both cavae, the right atrium was opened transversely along the atrio-ventricular groove and astonishingly a rusty sewing needle was found embedded with its sharp end in the roof of the right atrium near the tricuspid valve (Figure 2).

Figure 2: The rusty sewing needle found in the cavity of the right atrium embedded in its wall.
Upon seeing the sewing needle, the patient remembered that she brought that type of needles one year ago and lost one of them shortly after. So the only available explanation postulated is that the needle went unnoticed into the patient´s chest may be while sleeping nearby the needle or leaving it inside her pocket which then eroded its way through the pericardium onto the right atrium being an anterior structure immediately behind the chest wall. The postoperative recovery went uneventfully and the patient was discharged home safely after one weak. Pathological examination of the thickened pericardium revealed nonspecific chronic inflammation with no signs of malignancy.
Discussion
Upon reviewing the literature, there is a general tendency to remove intra-cardiac needles once diagnosed to avoid potential hazards or prevent further damage [4]. These hazards include embolization, thrombus formation, endocarditis, pericarditis and injury to cardiac structures including cardiac perforation and pericardial tamponade [5]. Hazards are more prone when the needles are located in left-sided chambers and when partially embedded in myocardium [6].
Localization modalities of intra-cardiac needles include echocardiography and more accurately computed tomography. Intra-operative C-Xray is much helpful and time sparing. Interventional extraction using modern radiological facilities would be difficult and may be hazardous. Median sternotomy is much superior than any other approaches e.g. thoracotomies as it allows the best exposure and safest access to cardiopulmonary bypass. Sometimes the needle can be removed without the help of the heart machine and sometimes not [7, 8]. In our study, although the needle penetrated accidentally into the chest wall and then right atrium, yet it did cause some sort of chronic pericarditis and recurrent effusion one year later. This represented, beside the sharp nature of the non-sterile sewing needle, the indications to remove the needle.
Conclusions
Since the fact that no clear guidelines exist regarding the indication for extraction of intra-cardiac needles, therefore management whether conservative or operative should be individualized according to each case. Surgical removal of lately-discovered intra-cardiac needles should be considered if complications occurred like pericarditis causing recurrent pericardial effusion in our case.
Compliance with ethical standards
Conflict of interest: The authors have declared that no conflict of interest exists.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Intra-cardiac needles#pericardiothentesis#echocardiography#cardiopulmonary bypass#sternotomy#fluoroscopy#cardiologist#sero-sanguinous#Hesham Alkady#JCMICR
0 notes
Text
Pseudocoarctation of the aorta by Phong Teck Lee in Journal of Clinical and Medical Images, Case Reports

Introduction
Pseudocoarctation of the aorta was first described in 1951 and remains a relatively rare congenital anomaly [1]. We present a case of pseudocoarctation of the aorta which was detected on magnetic resonance imaging (MRI).
Case Report
A 19-year-old gentleman with suspected coarctation of aorta was referred for magnetic resonance imaging (MRI). Twelve-lead electrocardiogram showed right bundle branch block. On clinical examination, there was a soft ejection systolic murmur in the left parasternal edge. He was asymptomatic with excellent exercise capacity. MRI was performed with Siemens Aera 1.5-Tesla scanner. The entire aorta was reconstructed with three-dimensional rendered imaging from non-contrast aortogram. The aorta appears elongated an unusually “high” aortic arch up to the level of the clavicle. This results in a large distance between the aortic arch and the pulmonary artery bifurcation. The descending aorta is mildly kinked at the level of the ligamentum arteriosum with no significant stenosis (Figure/Video). Phase contrast assessment at the level of the kink demonstrated absence of significant stenosis with a maximal velocity of 1.5 m/s. There was no evidence of collateral artery formation. The left ventricular volumes and systolic function were normal and there was no evidence of myocardial hypertrophy. These findings are consistent with a diagnosis of pseudocoarctation of the aorta.
Discussion
Pseudocoarctation of the aorta consists of elongation and kinking of the aortic arch and narrowing of the aortic isthmus without significant obstruction. The exact etiology of pseudocoarctation of the aorta is unknown. Postulated embryologic cause include failure of the compression of the third through the seventh segments of the dorsal aortic roots and the fourth arch segment [2].
Features of pseudocoarctation of the aorta are best visualized using three-dimensional reconstruction of the aorta by computed tomography (CT) or magnetic resonance imaging (MRI). The elongation of the arch frequently produces an unusually high aortic arch in the mediastinum and increased distance between the origins of left common carotid artery and left subclavian artery [3]. The left subclavian artery also has a more caudal origin [3]. Other features include absence or only a mild degree of luminal stenosis, absence of collateral circulation and absence of left ventricular hypertrophy and ascending aortic dilatation [4]. These features are present in our case. Concomitant congenital heart lesions have been reported in association with pseudocoartation of the aorta [2]. It could also be associated with distal aneurysmal dilatation. While pseudocoarctation of the aorta is usually benign, cases of aneurysm formation and rupture have been reported [2, 3]. As such, surgical treatment is recommended for symptomatic cases, or those associated with aneurysm formation, and regular follow-up for asymptomatic patients.
This case highlights the imaging features of pseudocoarctation of the aorta. We demonstrated the utility of CMR, especially three-dimensional reconstruction imaging and phase contrast assessment in the diagnosis of pseudocoarctation of the aorta.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Pseudocoarctation#magnetic resonance imaging#asymptomatic#aortic#ligamentum#myocardial hypertrophy#embryologic#computed tomography#Phong Teck Lee#JCMICR
0 notes
Text
Primary breast osteosarcoma with pulmonary metastases by Guillaume Fahrni in Journal of Clinical and Medical Images, Case Reports

Abstract
Primary breast osteosarcoma is a rare malignant tumor, with only small series reported. We report the case of an 89-year-old woman presenting with a large calcified tumor of the left breast, associated with calcified lung metastases. After non-conclusive biopsy, osteosarcoma was proven at tumorectomy.
Keywords: Osteosarcoma; breast tumor; calcified cancer; lung metastases; breast surgery.
Background
Breast sarcomas are uncommon malignant tumors. Among them, primary breast osteosarcoma is rare with less than 200 cases reported in the literature, representing 12.5% of all breast sarcomas and 1% of all breast tumors [1]. It is a very aggressive tumor that typically produces bone and osteoid matrix. It usually affects elderly patients, with a median age at diagnosis of 64.5 years [3]. The clinical presentation is a palpable mass sometimes associated with a cutaneous rash. Complete resection is the treatment of choice in case of limited disease extension [4]. Survival rate is poor, under 40% at 5 years [5].
Case Presentation
An 89-year-old woman without relevant past medical history was hospitalized for cardiac failure. While performing routine physical examination, a palpable firm and irregular mass of the left breast was evidenced, seemingly unnoticed by the patient. This finding motivated the realization of a mammography showing a regional area of coarse heterogeneous calcifications in the internal quadrants of the left breast. Correlation with ultrasound demonstrated a subcutaneous mass with posterior acoustic shadowing (Figure 1). A fine needle biopsy was performed, however it was not contributive due to the large calcifications within the sample. Due to the high suspicion of primary breast neoplasm, a thoracoabdominal CT was performed that revealed a large heterogeneous and calcified mass of the left breast associated with diffuse and partially calcified lung nodules (Figure 2).
The patient’s case was discussed at the tumor board and a breast tumorectomy was decided and performed without any immediate complication following surgery. On gross observation, the tumorectomy piece (16.5 x 13.5 x 9.5cm) contained a well-defined mass measuring 10. x 8.5 x 7.5 cm, heterogeneous, partially calcified and containing areas of central necrosis (Figure 3). Microscopic examination showed a peripheral zone containing a dense proliferation of spindle-shaped cells. There was a central zone composed of ossification foci, osteoclastic cells and cartilage, as well as a transition zone with osteoid formations and sclerous tissue (Figure 3). Immunohistochemistry was performed, with spindle-shaped cells showing a strong expression of MYC, a moderate expression of MDM2, a heterogenous expression of p63 and no expression of epithelial markers CKAE1/AE3, CK5/6, EMA, MNF-116, CK7, CK19. An intra-mammary lymph node (2.2 cm) was also identified, containing metastatic tissue. The aforementioned findings were consistent with the diagnosis of high-grade malignant mesenchymal neoplasm compatible with an extraskeletal osteosarcoma of the breast with lung metastasis. Patient outcome was unfavorable with rapid decline and death due to advanced metastatic disease progression.
Figure 1: Mammography with medio-lateral oblique (A) and cranio-caudal (B) incidencesviews of the left breast evidencing a regional area of coarse heterogeneous calcifications at the union of the internal quadrants. Breast ultrasound (C) showing a subcutaneous mass with large posterior acoustic shadowing limiting further analysis.
Figure 2: Thoracoabdominal contrast-enhanced CT revealing a large calcified mass involving the internal quadrants of the left breast (A, arrowhead) and diffuse partially calcified pulmonary nodules consistent with lung metastasis (B-C). Note the calcified aspect of the lung metastasis (C, arrow).
Figure 3: Macroscopic examination (A) evidencing a voluminous calcified mass with central necrosis. Microscopic examination (B-C) showed a peripheral zone containing a dense proliferation of spindle-shaped cells (B), and a central zone composed of ossification foci, osteoclastic cells and cartilage (C).
Discussion
Primary breast osteosarcoma is a type of breast tumor with bone producing osteoid matrix [6]. It is not only a very rare breast malignancy but also an unusual location for an extraskeletal sarcoma [7]. Although rare, its diagnosis is important as the imaging features, treatment and prognosis differ from other breast cancers. As with all sarcomas, it is defined by the underlying type of tissue with the most common subtype including fibrohistiosarcoma, myxofibrosarcoma and angiosarcoma [2].
Primary breast osteosarcoma has to be differentiated from metaplastic carcinoma and cystosarcoma phyllodes, that can both present with similar imaging features [8]. The clinical presentation is a breast mass, with rapid growth but rarely associated with pain [9]. Nodal involvement is uncommon, but metastases are frequent. Lung is the most commonly organ involved, followed by bone. The survival is poor, with an overall 5-year survival rate of 38% [10]. On mammography, the primary lesion is usually a large, dense, calcified mass [11]. However, in some cases, calcifications can be absent [12]. Ultrasound is helpful for lesion characterization, staging and biopsy guidance and usually shows important acoustic shadowing limiting analysis [2]. MRI is useful to assess the extent of the mass within the breast, to search out for other masses, assess for chest wall invasion usually showing a high T2 signal mass with enhancement [1]. Whole-body contrast-enhanced CT scan or 18FDG PET-CT are of interest to detect metastatic extension [6]. The final diagnosis of primary breast osteosarcoma is made on pathology, demonstrating osteosarcomatous matrix and showing that the lesion does not arise from adjacent bone (sternum or ribs) [13]. Immunohistochemistry is helpful to establish the diagnosis, with the use of epithelial markers such as CKAE1/AE3, CK5/6, EMA, SMA, CK7, vimentin, MAC-387 and others [14]. Excisional biopsy (complete tumorectomy), as this was done in our patient, is preferred to fine needle biopsy, as the mass can be very firm due to the presence of calcifications that can lead to inconclusive results as in our case [6]. As with any subtype of sarcoma, the treatment is the complete surgical excision with large margins [11]. Local recurrence rates were reported as high as 67% after tumorectomy and 11% after mastectomy [5, 15]. If no local node involvement is seen, axillary node dissection is not recommended, since this type of sarcoma does not spread via lymphatic route [16]. In this regard, our case was unusual as a pathologic intra-mammary lymph node was found. There is no consensus about the administration of adjuvant chemotherapy. However, it is generally recommended as it evidenced to improve survival rates, but no standard dose has been established yet [10]. For more advanced cases with metastasis, chemotherapy is the main treatment. Drugs used are the same as with other sarcomas and include cisplatin, doxorubicin, ifosfamide and methotrexate [17].
Acknowledgments: The authors declare no conflict of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Osteosarcoma#breast tumor;#calcified cancer#lung metastases#breast surgery#Immunohistochemistry#cystosarcoma#Guillaume Fahrni#JCMICR
0 notes