#medicare advantage plans explained
Text
The 5 Best Medicare Advantage Plans For 2024
5 Best Medicare Advantage Plans: Medicare Advantage plans, also known as Medicare Part C, are popular options for individuals looking for comprehensive coverage beyond what Original Medicare provides.
These plans are offered by private insurance companies approved by Medicare and often include additional benefits such as prescription drug coverage, and dental, vision, and hearing services.
5…

View On WordPress
#best medicare advantage plans#medicare#medicare advantage#medicare advantage cons#medicare advantage plan#medicare advantage plans#medicare advantage plans 2023#medicare advantage plans explained#medicare advantage plans pros and cons#medicare advantage vs medicare supplement#medicare advantage vs medigap#medicare explained#medicare plans#medicare supplement#medicare supplement plans#medigap vs medicare advantage#what is medicare advantage
0 notes
Text

5 Best Medicare Part D Insurance Companies
#medicare part d#medicare supplement#medicare supplemental insurance#medicare#medicare advantage#medicare part c#medicare part d plans#medicare insurance#medicare drug plan#medicare part d donut hole#medicare drug coverage#medicare part d enrollment#medicare advantage plans#medicare supplement plan#medicare supplement insurance#medicare part d explained#medicare drug plans#medicare part a#medicare part b#medicare explained
0 notes
Text
By Jake Johnson
Common Dreams
Oct. 4, 2023
"Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare," says a new report from Physicians for a National Health Program.
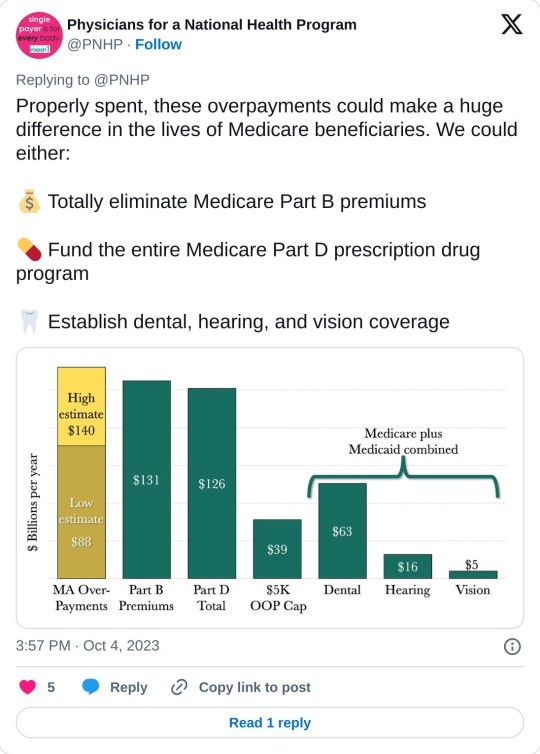
A report published Wednesday estimates that privately run, government-funded Medicare Advantage plans are overcharging U.S. taxpayers by up to $140 billion per year, a sum that could be used to completely eliminate Medicare Part B premiums or fully fund Medicare's prescription drug program.
Physicians for a National Health Program (PNHP), an advocacy group that supports transitioning to a single-payer health insurance system, found that Medicare Advantage (MA) overbills the federal government by at least $88 billion per year, based on 2022 spending.
That lower-end estimate accounts for common MA practices such as upcoding, whereby diagnoses are piled onto a patient's risk assessment to make them appear sicker than they actually are, resulting in a larger payment from the federal government.
But when accounting for induced utilization—"the idea that people with supplemental coverage are likely to use more health care because their insurance pays for more of their cost"—PNHP estimated that the annual overbilling total could be as high as $140 billion.
"This is unconscionable, unsustainable, and in our current healthcare system, unremarkable," says the new report. "Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare, siphoning money from vulnerable patients while delaying and denying necessary and often lifesaving treatment."
Even if the more conservative figure is accurate, PNHP noted, the excess funding that MA plans are receiving each year would be more than enough to expand traditional Medicare to cover dental, hearing, and vision. Traditional Medicare does not currently cover those benefits, which often leads patients to seek out supplemental coverage—or switch to an MA plan.
The Congressional Budget Office has estimated that adding dental, vision, and hearing to Medicare and Medicaid would cost just under $84 billion in the most costly year of the expansion.
"While there is obvious reason to fix these issues in MA and to expand traditional Medicare for the sake of all beneficiaries," the new report states, "the deep structural problems with our healthcare system will only be fixed when we achieve improved Medicare for All."
Bolstered by taxpayer subsidies, Medicare Advantage has seen explosive growth since its creation in 2003 even as it has come under fire for fraud, denying necessary care, and other abuses. Today, nearly 32 million people are enrolled in MA plans—more than half of all eligible Medicare beneficiaries.
Earlier this year, the Biden administration took steps to crack down on MA overbilling, prompting howls of protest and a furious lobbying campaign by the industry's major players, including UnitedHealth Group and Humana. Relenting to industry pressure, the Biden administration ultimately agreed to phase in its rule changes over a three-year period.
Leading MA providers have also faced backlash from lawmakers for handing their top executives massive pay packages while cutting corners on patient care and fighting reforms aimed at rooting out overbilling.
As PNHP's new report explains, MA plans are paid by the federal government as if "their enrollees have the same health needs and require the same levels of spending as their traditional Medicare counterparts," even though people who enroll in MA plans tend to be healthier—and thus have less expensive medical needs.
"There are several factors that potentially contribute to this phenomenon," PNHP's report notes. "Patients who are sicker and thus have more complicated care needs may be turned off by limited networks, the use of prior authorizations, and other care denial strategies in MA plans. By contrast, healthier patients may feel less concerned about restrictions on care and more attracted to common features of MA plans like $0 premiums and additional benefits (e.g. dental and vision coverage, gym memberships, etc.). Insurers can also use strategies such as targeted advertising to reach the patients most favorable to their profit margins."
A KFF investigation published last month found that television ads for Medicare Advantage "comprised more than 85% of all airings for the open enrollment period for 2023."
"TV ads for Medicare Advantage often showed images of a government-issued Medicare card or urged viewers to call a 'Medicare' hotline other than the official 1-800-Medicare hotline," KFF noted, a practice that has previously drawn scrutiny from the U.S. Senate and federal regulators.
PNHP's report comes days after Cigna, a major MA provider, agreed to pay $172 million to settle allegations that it submitted false patient diagnosis data to the federal government in an attempt to receive a larger payment.
Dr. Ed Weisbart, PNHP's national board secretary, toldThe Lever on Wednesday that such overpayments are "going directly into the profit lines of the Medicare Advantage companies without any additional health value."
"If seniors understood that the $165 coming out of their monthly Social Security checks was going essentially dollar for dollar into profiteering of Medicare Advantage, they would and should be angry about that," said Weisbart. "We think that we pay premiums to fund Medicare. The only reason we have to do that is because we're letting Medicare Advantage take that money from us."
13 notes
·
View notes
Text
Guiding Your Medicare Journey: Exploring Medicare Nationwide
Introduction: Accessible Healthcare Solutions with Medicare Nationwide
Medicare Nationwide serves as a guiding light for individuals navigating the complexities of Medicare across the United States. Committed to providing accessible healthcare solutions, Medicare Nationwide offers a comprehensive range of services and resources to empower beneficiaries in making informed decisions about their healthcare options.
Comprehensive Coverage Understanding
Understanding the nuances of Medicare coverage is essential for maximizing healthcare benefits. Medicare Nationwide provides extensive information on each aspect of Medicare. From Medicare Part A, which covers hospital stays and inpatient care, to Medicare Part B, encompassing outpatient services and medical supplies, Medicare Nationwide ensures beneficiaries have a thorough understanding of their coverage options.
Enrollment Assistance
Enrolling in Medicare can be overwhelming, especially for newcomers. Medicare Nationwide offers enrollment assistance to guide beneficiaries through the process with ease. Whether individuals are enrolling for the first time or exploring coverage options during the annual enrollment period, Medicare Nationwide provides guidance and support. By explaining enrollment periods, eligibility criteria, and coverage options, Medicare Nationwide empowers beneficiaries to make well-informed decisions.
Comparing Medicare Advantage Plans
Medicare Advantage plans, or Medicare Part C, provide an alternative way for beneficiaries to receive their Medicare benefits. Medicare Nationwide helps beneficiaries compare available Medicare Advantage plans in their area. By evaluating plan features, costs, and coverage options, beneficiaries can choose the plan that best fits their healthcare needs and financial situation.
Understanding Prescription Drug Coverage
Prescription drug coverage, known as Medicare Part D, is crucial for many beneficiaries. Medicare Nationwide offers valuable insights into Medicare Part D plans, including coverage details, formularies, and costs. Understanding prescription drug coverage options allows beneficiaries to access necessary medications affordably.
Exploring Supplemental Coverage Options
In addition to Original Medicare and Medicare Advantage plans, beneficiaries may consider Medicare Supplement Insurance (Medigap) policies. Medicare Nationwide provides guidance on selecting the appropriate Medigap plan, including coverage options, costs, and enrollment requirements. This supplemental coverage fills gaps in Medicare coverage, providing added peace of mind.
Conclusion: Empowering Healthcare Decision-Making
In conclusion, Medicare Nationwide is a trusted resource for navigating the complexities of Medicare. By providing comprehensive coverage understanding, enrollment assistance, and support in exploring coverage options, Medicare Nationwide empowers beneficiaries to make informed decisions about their healthcare coverage. With Medicare Nationwide's guidance, beneficiaries can confidently navigate the Medicare landscape and access the healthcare they need.
2 notes
·
View notes
Text
For everyone in the notes of the wood glue post asking if they can borrow my dad, please know that this week he spent forty minutes on the phone explaining to me (again) about how cardiologists are all part of a scam to sell Medicare Advantage plans. He had heart surgery this year. He will not go to the cardiologist because they are a scam.
What I'm saying is I'm implementing a "no returns" policy. He's your problem now. He needs his dentures redone. He cannot move away from the Chicago suburbs because Jewel Osco brand lime seltzer is the only thing he will drink. Good luck.
#personal#he is also still holding the Comcast modem hostage until they pay him the $91 they owe him
3 notes
·
View notes
Text
Maximizing Your Coverage: A Guide to Cigna Advantage Medicare Plans
Introduction
As individuals age, access to comprehensive healthcare coverage becomes increasingly important for maintaining health and financial security. Cigna, a reputable healthcare company, offers a range of Advantage Medicare plans designed to provide beneficiaries with extensive coverage and additional benefits beyond traditional Medicare. In this guide, we'll explore Cigna Advantage Medicare plans, explaining their coverage options, benefits, and how beneficiaries can maximize their coverage to meet their healthcare needs.

Understanding Cigna
Cigna is a global health service company dedicated to improving the health, well-being, and peace of mind of its customers. With a focus on innovation, affordability, and customer satisfaction, Cigna offers a wide range of healthcare products and services, including medical, dental, vision, pharmacy, and behavioral health coverage. Cigna's commitment to providing comprehensive, high-quality care makes it a trusted choice for millions of individuals and families worldwide.
Overview of Cigna Advantage Medicare Plans
Cigna Advantage Medicare plans, also known as Medicare Advantage plans or Medicare Part C, are offered as an alternative to traditional Medicare. These plans are available through private insurance companies like Cigna and provide all the benefits of Medicare Part A and Part B, as well as additional benefits such as prescription drug coverage (Part D), dental, vision, hearing, and wellness programs. Medicare Advantage plans may also offer provider networks, with beneficiaries typically required to use network providers for covered services.
Exploring Cigna Advantage Medicare Plans
Cigna Advantage Medicare plans offer a variety of benefits and coverage options designed to meet the diverse healthcare needs of beneficiaries. Some key features of Cigna Advantage plans include:
Comprehensive Coverage: Cigna Advantage plans provide coverage for Medicare Part A and Part B benefits, as well as additional benefits such as prescription drug coverage, dental, vision, hearing, and wellness programs. This comprehensive coverage ensures that beneficiaries have access to a wide range of healthcare services and resources.
Provider Networks: Cigna Advantage plans may utilize provider networks, with beneficiaries often required to use network providers for covered services. This can help ensure coordinated care and access to quality healthcare providers within the Cigna network.
Additional Benefits: In addition to traditional Medicare benefits, Cigna Advantage plans may offer additional benefits such as telehealth services, fitness memberships, transportation assistance, and home-delivered meals. These extra benefits enhance the value of the plan and help beneficiaries access care and support services more conveniently.
Cost-Saving Opportunities: Cigna Advantage plans may offer cost-saving opportunities such as lower premiums, deductibles, and copayments compared to traditional Medicare. Some plans may also include coverage for preventive services at no additional cost, helping beneficiaries stay healthy and avoid costly medical expenses.
Maximizing Your Coverage with Cigna Advantage Medicare Plans
To maximize your coverage with Cigna Advantage Medicare plans, beneficiaries can consider the following strategies:
Assess Your Healthcare Needs: Evaluate your healthcare needs and budget to determine which Cigna Advantage plan best meets your requirements. Consider factors such as prescription medication needs, preferred doctors and hospitals, and anticipated medical expenses.
Understand Plan Options: Familiarize yourself with the different Cigna Advantage plans available in your area, including HMOs, PPOs, and Special Needs Plans (SNPs). Understand the coverage options, benefits, and cost-sharing requirements of each plan to make an informed decision.
Review Provider Networks: If the plan utilizes a provider network, review the network of healthcare providers to ensure that your preferred doctors, specialists, and hospitals are included. Check whether your current providers participate in the plan's network, or if you're willing to switch providers if necessary.
Utilize Additional Benefits: Take advantage of the additional benefits offered by Cigna Advantage plans, such as telehealth services, fitness memberships, transportation assistance, and home-delivered meals. These extra benefits can help you access care and support services more conveniently and affordably.
Conclusion
Cigna Advantage Medicare plans offer a comprehensive solution for beneficiaries seeking extensive coverage and additional benefits beyond traditional Medicare. By assessing healthcare needs, understanding plan options, reviewing provider networks, and utilizing additional benefits, beneficiaries can maximize their coverage and access high-quality healthcare services with Cigna. With Cigna's commitment to innovation, affordability, and customer satisfaction, beneficiaries can trust that they're in good hands when choosing a Cigna Advantage Medicare plan.
0 notes
Text
What Does a Medicare Supplement Insurance Coverage Representative Do?

Medicare Supplement Insurance coverage, also known as Medigap, is a sort of health insurance developed to supplement Original Medicare. It helps pay a few of the healthcare costs that Original Medicare does not cover, such as copayments, coinsurance, and deductibles. As a Medicare Supplement Insurance policy representative, your key duty is to help individuals understand their options, select the best plan for their needs, and enroll in an ideal plan.
One of the key duties of a Medicare Supplement Insurance representative is to educate clients about the differences between Original Medicare and Medicare Supplement strategies. This involves explaining the insurance coverage advantages of each strategy, as well as any type of constraints or restrictions that may apply. Agents have to be fluent in Medicare regulations and standards to supply exact information to customers.
Along with educating clients, Medicare Supplement Insurance coverage representatives help people compare different Medigap plans from numerous insurance provider. The Life Insurance agents near me aid customers in examining costs, coverage options, and company networks to locate a strategy that fits their budget plan and health care demands. Representatives should stay current on changes in the insurance policy market and brand-new plan offerings to best offer their clients.
Furthermore, Medicare Supplement Insurance coverage representatives play a crucial duty in the enrollment process. The Life Insurance from Community First Insurance in Winchester Kentucky agents assist customers full applications, send needed documentation, and make sure that all requirements are fulfilled for registration in a Medigap strategy. Representatives additionally provide ongoing assistance to customers, answering questions, addressing issues, and helping with any concerns that might emerge during the insurance coverage duration.
To conclude, being a Medicare Supplement Insurance policy agent needs knowledge of Medicare policies, superb communication skills, and a commitment to aiding individuals navigate the complicated world of healthcare insurance coverage. By acting as teachers, advisors, and advocates for their clients, Medicare Supplement Insurance policy agents play a vital role in making certain people have accessibility to the insurance coverage they need to maintain their health and health. You can get more enlightened on this topic by reading here: https://en.wikipedia.org/wiki/Insurance.
1 note
·
View note
Text
Medicare explained
Learn about Medicare Advantage plans tailored for Florida, Georgia, Texas, Virginia, South Carolina, North Carolina, Michigan, and Pennsylvania. Discover comprehensive coverage options including dental. Medicare explained
About Company:-
Welcome to Medicare Pro: Your Hassle-Free Medicare Coverage Solution in Your State Are you turning 65 in the next three months? Congratulations on reaching this milestone! Now is the perfect time to secure the best Medicare plan for your needs.
Access any doctor, anywhere in the country with our strong PPO network. Whether you're traveling or relocating, your coverage stays with you.Enjoy peace of mind with our plans that include a Part B giveback of up to $175.00 a month, ensuring you're covered for all your medical needs.
Click Here For More Info:- https://floridamedadvantage.net/
Social Media Profile Links:-
https://www.facebook.com/medicareadvantgeadvisor
0 notes
Text
What to Do If You Missed Medicare Open Enrollment?
If you've missed the Medicare Open Enrollment Period, it's important to take prompt action to address any gaps in your coverage and avoid potential penalties. While certain enrollment periods are limited, there are still options available to help you make necessary adjustments to your Medicare plan.
Here's what to do if you missed Medicare Open Enrollment:
Understand the Consequences: Missing the Medicare Open Enrollment Period may limit your ability to make changes to your coverage until the next enrollment period. Delayed enrollment could lead to gaps in coverage and potential penalties, especially for Medicare Advantage and Part D prescription drug plans.
Review Special Enrollment Period (SEP) Eligibility: Check if you qualify for a Special Enrollment Period (SEP). SEPs are triggered by certain life events, such as moving, losing employer-sponsored coverage, or becoming eligible for Extra Help with prescription drug costs. If you qualify for an SEP, you may be able to make changes to your Medicare plan outside the regular enrollment periods.
Verify Employer-Sponsored Coverage: If you have employer-sponsored health coverage, understand how it coordinates with Medicare. Delaying enrollment in Medicare because you have employer coverage could result in penalties if the employer coverage is not considered credible.
Assess Your Current Coverage: Evaluate your existing Medicare coverage, including Original Medicare, Medicare Advantage, and Part D plans. Ensure that your current plan meets your healthcare needs and consider whether adjustments are necessary. Contact Medicare or Social Security: Reach out to Medicare or the Social Security Administration to explain your situation. In some cases, they may guide available options or assist with resolving specific issues related to your enrollment.
Explore Medigap Policies: If you have Original Medicare and missed the Medigap Open Enrollment Period, consider whether you can still purchase a Medigap policy. While this period offers guaranteed acceptance, some states have additional rules, and eligibility may vary.
Assess Medicare Advantage Plans: If you're enrolled in a Medicare Advantage plan and missed the Open Enrollment Period, check if you qualify for a Special Enrollment Period. Life events, such as moving to a new service area or losing other health coverage, may trigger a SEP.
Part D Prescription Drug Plans: If you missed the Annual Enrollment Period for Part D prescription drug plans, consider your options. You may still be eligible for a SEP or may need to wait until the next Annual Enrollment Period to make changes. Be Aware of Late Enrollment Penalties: Understand the potential for late enrollment penalties. Delayed enrollment in Medicare Advantage or Part D plans may result in higher premiums when you do enroll.
Seek Professional Advice: Consult with a Medicare advisor or counselor to get personalized guidance based on your situation. They can provide insights into available options and help you make informed decisions about your coverage.
Consider Future Planning: If you've missed enrollment periods, use the experience as an opportunity for future planning. Stay informed about upcoming enrollment periods, and proactively assess your healthcare needs to avoid similar issues in the future.
In summary, missing the Medicare Open Enrollment Period requires proactive steps to address potential coverage gaps and penalties. Understanding your eligibility for Special Enrollment Periods, assessing your current coverage, and seeking assistance from Medicare resources or advisors can help you navigate the situation effectively. Be proactive in addressing any missed deadlines to ensure continued access to necessary healthcare services.
0 notes
Text
Medicare Coverage for Adult Day Care Explained
Medicare Coverage for Adult Day Care Explained offers a comprehensive overview of the support provided by Medicare for adult day care services. This informative resource delves into the eligibility criteria, coverage options, and benefits available to seniors seeking assistance with daytime care needs. It explores the types of services covered, such as social activities, meals, transportation, and therapeutic programs, aimed at enhancing seniors' well-being and quality of life. Additionally, the guide addresses the role of Medicare Advantage plans in offering supplemental benefits for adult day care, providing insights into how beneficiaries can maximise their coverage options. By unravelling the complexities of Medicare's support for adult day care, this resource empowers seniors and their caregivers to make informed decisions about accessing these essential services. Whether seeking respite for caregivers or social engagement for seniors, understanding Medicare's coverage for adult day care is crucial for ensuring comprehensive care and support in the ageing process.
Understanding Medicare's Role in Adult Day Care
Introducing Medicare Coverage for Adult Day Care offers an overview of the program's goals and eligibility requirements. Medicare aims to aid seniors by offering daytime care options fostering socialisation, engagement, and assistance with daily activities. This subheading sheds light on Medicare's commitment to enhancing seniors' quality of life, providing essential services for their well-being and ensuring they receive the care and support they need during daytime hours.
Types of Adult Day Care Services Covered by Medicare
Medicare explores the range of services eligible for coverage under Medicare. It delves into the various activities and support provided, including meals, social interactions, health monitoring, transportation, and therapeutic programs. This resource sheds light on Medicare's comprehensive coverage, ensuring seniors have access to diverse services that promote their well-being and independence during daytime hours.
Eligibility Criteria for Medicare Coverage
Outlines the requirements individuals must meet to qualify for Medicare benefits. It explains age criteria, citizenship or legal residency status, and contributions to Medicare through payroll taxes. Additionally, it discusses specific enrollment periods, such as Initial Enrollment, Special Enrollment, and General Enrollment, highlighting the importance of understanding these criteria to ensure timely access to Medicare coverage and benefits.
Delving into Medicare's Coverage Benefits
Here, the focus is on the coverage options and benefits available through Medicare coverage for adult day care. It outlines the various services covered, such as skilled nursing care, personal care assistance, therapy services, and social activities. This section also discusses cost-sharing requirements, including deductibles, coinsurance, and copayments.
Enrolling in Medicare Advantage Plans for Additional Benefits
Explores the option of enhancing Medicare coverage by enrolling in Medicare Advantage plans. This resource delves into the supplemental benefits offered by these plans, such as vision, dental, hearing, and prescription drug coverage, along with additional services like transportation assistance and fitness programs. Understanding the enrollment process and available benefits empowers individuals to make informed decisions about their healthcare coverage.
How to Navigate Medicare's Coverage for Adult Day Care?
Navigating Medicare coverage for adult day care requires understanding eligibility criteria, available benefits, and enrollment options. This process involves evaluating individual healthcare needs, researching plan options, and coordinating care with healthcare providers. By exploring coverage options, accessing available benefits, and understanding cost-sharing requirements, individuals can make informed decisions to ensure comprehensive care and support for adult day care services.
Resources for Seniors and Caregivers in Adult Day Care
The final subheading explores resources and support services available to seniors and caregivers navigating Medicare's coverage for adult day care. It discusses community-based programs, support groups, and online resources that offer information, assistance, and advocacy for individuals seeking adult day care services. Additionally, it highlights the importance of exploring all available options to ensure comprehensive care and support for seniors in need of daytime assistance.
Conclusion
Understanding Medicare coverage for adult day care is crucial for seniors and their caregivers navigating healthcare options. This comprehensive guide has provided insights into the eligibility criteria, types of services covered, and the role of Medicare Advantage plans in providing additional benefits. By exploring these aspects, individuals can make informed decisions about accessing adult day care services that best meet their needs. Moreover, the availability of resources and support services ensures that seniors and caregivers can navigate the complexities of Medicare coverage effectively. Ultimately, Medicare's commitment to providing comprehensive care extends to supporting seniors in maintaining their independence, social engagement, and overall well-being through adult day care services. By leveraging Medicare's coverage options and accessing available resources, seniors can enjoy enhanced quality of life while caregivers receive the support they need to provide compassionate care. Thus, understanding Medicare's coverage for adult day care plays a pivotal role in promoting the health and happiness of seniors in our communities.
0 notes
Text
Navigating Healthcare Excellence: Steve Jones Unveils the Best Medicare Plans in California
In the vast and diverse landscape of healthcare options, finding the best Medicare plan in California can be a daunting task. Enter Steve Jones, a seasoned expert in insurance and financial planning, who brings unparalleled insights to help Californians make informed decisions about their Medicare coverage. In this blog post, we'll explore the intricacies of Medicare plans in California and discover why Steve Jones is the go-to advisor for those seeking excellence in healthcare coverage.
Understanding the California Healthcare Landscape:
California, known for its cultural diversity and innovation, boasts a healthcare landscape that mirrors its dynamic population. When it comes to Medicare plans, the state offers a range of options, each with its unique features and advantages. From Original Medicare to Medicare Advantage and supplemental plans, navigating this array of choices requires expert guidance.
Steve Jones: A Trusted Advisor:
Steve Jones, with his extensive knowledge of the insurance industry and a commitment to personalized service, emerges as a beacon of guidance in the realm of Medicare plans. His approach goes beyond recommending generic solutions; instead, he works closely with individuals to understand their health needs, financial situations, and preferences, ensuring that the recommended plan aligns seamlessly with their unique circumstances.
The Best Medicare Plans in California:
Original Medicare (Part A and Part B):
Steve Jones often starts by explaining the fundamentals of Original Medicare, which includes Part A (hospital insurance) and Part B (medical insurance). This provides coverage for hospital stays, doctor visits, and essential medical services. While comprehensive, some individuals may choose to enhance their coverage further.
Medicare Advantage Plans:
Steve navigates clients through the benefits of Medicare Advantage plans, also known as Part C. These plans, offered by private insurance companies, often include additional coverage beyond Original Medicare, such as vision, dental, and prescription drug coverage. Steve evaluates individual health needs to determine if a Medicare Advantage plan suits their lifestyle.
Medicare Supplement (Medigap) Plans:
For those seeking comprehensive coverage, Steve may recommend Medicare Supplement plans. These plans work alongside Original Medicare to fill the gaps in coverage, such as deductibles and copayments. Steve explains the nuances of various Medigap plans, helping clients choose the one that complements their healthcare needs.
Prescription Drug Plans (Part D):
Understanding the importance of prescription drug coverage, Steve guides clients through Medicare Part D plans. These plans are designed to help cover the costs of prescription medications, ensuring individuals have access to necessary drugs without breaking the bank.
Dual Eligible Special Needs Plans (D-SNPs):
Steve introduces the concept of Dual Eligible Special Needs Plans for individuals qualifying for both Medicare and Medicaid. These plans offer tailored benefits to address the unique needs of dual-eligible individuals, providing a holistic approach to healthcare.
Steve Jones' Approach:
What sets Steve Jones apart is his commitment to a client-centric approach. He emphasizes the importance of considering individual health conditions, preferred healthcare providers, and budget constraints when selecting a Medicare plan. Steve simplifies the complex world of insurance options, providing clarity and confidence to clients as they embark on their healthcare journey.
Conclusion:
In the dynamic landscape of California's healthcare options, Steve Jones emerges as a trusted advisor, guiding individuals towards the best Medicare plans tailored to their unique needs. With a deep understanding of the intricacies of each plan, Steve ensures that clients make informed decisions, securing not just healthcare coverage but peace of mind. For those navigating the complex choices in Medicare plans in California, Steve Jones is the beacon of expertise, leading the way to a healthcare solution that aligns perfectly with individual circumstances and aspirations.
0 notes
Text
Discussing Transformative Changes in Medicare Policies for Behavioural Health Billing in 2024

Dealing with the constantly evolving world of behavioral health billing requires a clear understanding of recent policy updates. In 2024, significant reforms are happening to address long-standing issues with mental health reimbursements. This blog explains these policy changes, emphasizing their practical benefits for psychiatry billing service providers and patients. Let's explore how these modifications can enhance Behavioral health billing services in terms of accessibility, cost, and quality.
Expanding Access to Mental Health Professionals
In a big shift from the past, these policies create a special benefit category for Marriage and Family Therapists (MFTs) and Mental Health Counselors (MHCs). Recognizing their unique skills opens doors for patients to get therapy from qualified professionals, focusing on targeted medical billing and coding practices for specialized services.
Revolutionizing Access to Intensive Outpatient Services
Expanding access to intensive outpatient services (IOPs) is a crucial change in Behavioral Health Billing. This shift breaks down old limitations tied to specific diagnoses. By broadening coverage, more individuals with moderate to severe mental health conditions can now receive intensive care outside of traditional inpatient settings, offering a substantial improvement in overall patient well-being.
Innovations in Crisis Intervention
Acknowledging the critical need for immediate intervention during mental health crises, the policies explore the coverage of mobile crisis services. This forward-thinking approach aims to go beyond physical location limitations, meeting patients at their moments of greatest need. At the same time, it streamlines crisis-related billing and coding procedures, ensuring a swift response to urgent situations.
Optimizing Reimbursement Rates
The proposed increases in reimbursement rates for crucial behavioral health services demonstrate a dedication to excellence. These higher reimbursement rates not only encourage providers to deliver treatment within primary care settings but also pave the way for early intervention and improved accessibility. Remaining informed about rule changes and cultivating collaborative relationships with behavioral health specialists are integral components of successfully navigating these changes.
Shifting Focus: From Illness to Wellness
Going beyond a reactive approach, these policies signal a paradigm shift towards preventative and well-being initiatives. This holistic strategy encompasses the integration of technology, wellness incentives through Medicare Advantage plans, and cooperative efforts with community organizations, faith-based groups, and social service agencies. Addressing broader social and economic factors impacting mental health becomes an essential part of this comprehensive strategy.
Addressing Workforce Shortages
While the transformative policies hold immense promise, overcoming the critical barrier of a shortage of behavioral health care professionals is essential. Innovative solutions, including programs offering loan repayment and expanded telehealth opportunities, become vital steps. Fostering collaboration among healthcare professionals not only optimizes treatment outcomes but also streamlines communication in billing and coding processes within the healthcare system.
Uncovering New Challenges
The evolution of Behavioral Health Billing introduces its own set of challenges varying from technological adaptations, some privacy concerns and changes in compliance requirements. Let's delve into these challenges to assist providers in navigating the changing landscape:
Technological Adaptation
Providers must stay up-to-date with technological advancements and adapt to new systems to ensure a smooth transition without compromising patient care. Addressing issues related to integrating Electronic Health Records (EHRs) and ensuring data security becomes crucial.
Privacy Concerns in Telehealth
While telehealth enhances accessibility, new challenges emerge concerning patient privacy. Providers face hurdles in safeguarding privacy in virtual settings, including potential issues related to illegal access or data breaches.
Regulatory Compliance
Dealing with the intricate web of rules surrounding behavioral health billing requires attention to detail. Providers must stay abreast of the latest changes in compliance requirements to ensure their procedures align with the new legal frameworks.
Conclusion
The landscape of Behavioral Health Billing is undergoing a transformative shift in 2024. These policy changes go beyond mere administrative adjustments. They signify a pivotal turning point, promising enhanced access, affordability, and a redefined approach to psychiatry billing services. As providers adapt to this evolving landscape, the realization of accessible and high-quality behavioral health care becomes a tangible reality. Stay ahead of the curve by partnering with Medcare MSO is a trusted name in medical billing companies in USA, your ally in navigating the complexities of behavioral health billing and coding. Explore the future of behavioral health billing with Medcare MSO and optimize your practice for a new era of psychiatry billing services.
Photo by Marek Levák on Unsplash
Read the full article
0 notes
Text

Your Medicare Coverage Guide for 2023
#medicare#medicare advantage#medicare coverage#medicare part d#medicare drug coverage#medicare supplement#medicare supplement plans#medicare explained#medicare basics#medicare supplemental insurance#medicare part a#medicare part b#medicare part c#medicare coverage guidelines#what does medicare cover#medicare dental coverage#medicare advantage plan#medicare advantage plans#medicare insurance#medicare made clear#medicare and employer coverage
0 notes
Text
Medicare Advantage RADV: Navigating the Landscape for Better Healthcare Outcomes

In today's complex healthcare landscape, understanding the intricacies of Medicare Advantage RADV (Risk Adjustment Data Validation) is crucial for both healthcare providers and beneficiaries. This article aims to shed light on what RADV entails, its impact on Medicare Advantage plans, and the importance of accurate data in ensuring quality healthcare for seniors.
Introduction
Medicare Advantage, a popular alternative to traditional Medicare, offers seniors additional benefits and services through private insurance plans. However, within this framework lies RADV, a process designed to validate the accuracy of data submitted by healthcare providers.
Explaining Medicare Advantage
Medicare Advantage plans provide seniors with a broader range of healthcare coverage, including hospital stays, doctor visits, and preventive care. These plans often include prescription drug coverage, making them an attractive option for many beneficiaries seeking comprehensive care.
RADV: Risk Adjustment Data Validation
RADV, as the acronym suggests, involves the validation of data submitted by healthcare providers to ensure accuracy. This process plays a pivotal role in determining the payments made to Medicare Advantage plans, emphasizing the need for precision in reporting health status information.
The Importance of Accurate Data
Accurate data is the backbone of RADV. The information provided by healthcare providers directly influences the reimbursement received by Medicare Advantage plans. Inaccuracies in data reporting can lead to financial repercussions and impact the quality of healthcare provided to beneficiaries.
How RADV Works
The RADV process involves a meticulous examination of medical records to verify the health conditions reported. Healthcare providers collaborate with Medicare Advantage plans to facilitate this validation, emphasizing the importance of accurate and complete documentation.
Challenges in RADV Implementation
Implementing RADV poses challenges for healthcare providers, including data collection hurdles and navigating complex regulations. Addressing these challenges requires a strategic approach to ensure the efficiency and effectiveness of the validation process.
Impact on Beneficiaries
RADV directly influences the quality of healthcare provided to beneficiaries. Accurate data ensures that Medicare Advantage plans receive appropriate reimbursements, enabling them to deliver comprehensive and tailored healthcare services to seniors.
Compliance and Regulations
Healthcare providers must adhere to stringent compliance standards and regulations when participating in RADV. Understanding these requirements is essential to avoid penalties and maintain a seamless partnership with Medicare Advantage plans.
Strategies for Healthcare Providers
To navigate the RADV landscape successfully, healthcare providers should adopt best practices for data validation. Collaborative efforts between providers and plans contribute to accurate reporting and a streamlined validation process.
The Future of RADV
As the healthcare landscape evolves, so does RADV. Keeping abreast of potential developments and changes in RADV ensures that healthcare providers remain proactive in adapting to industry advancements.
Case Studies
Real-world examples showcase successful RADV experiences, offering insights into effective strategies and highlighting the positive impact of accurate data on healthcare outcomes.
Addressing Common Misconceptions
Misconceptions about RADV can hinder effective participation. This section aims to clarify common myths, providing readers with a clearer understanding of the process.
Engaging Beneficiaries
Empowering beneficiaries in RADV processes is crucial. Encouraging active participation ensures that their health status is accurately represented, contributing to more personalized and effective healthcare.
Continuous Improvement
Adopting a mindset of continuous improvement allows healthcare providers to evolve with changes in the RADV landscape. Proactive measures contribute to enhanced data accuracy and better healthcare outcomes for seniors.
Conclusion
In conclusion, Medicare Advantage RADV is a critical aspect of the healthcare journey for seniors. Navigating this landscape requires a collaborative effort from healthcare providers, plans, and beneficiaries to ensure accurate data reporting and, consequently, improved healthcare quality.
Frequently Asked Questions (FAQs)
What is the primary purpose of RADV in Medicare Advantage?
RADV aims to validate the accuracy of data submitted by healthcare providers, influencing reimbursements and ensuring quality healthcare for beneficiaries.
How can healthcare providers overcome challenges in RADV implementation?
Adopting best practices for data validation and collaborative efforts with Medicare Advantage plans are key strategies for overcoming challenges.
What role do beneficiaries play in the RADV process?
Beneficiaries play a crucial role by actively participating in RADV processes, ensuring that their health status is accurately represented.
Why is accurate data essential in RADV?
Accurate data is essential as it directly impacts the reimbursement received by Medicare Advantage plans, influencing the quality of healthcare provided to beneficiaries.
How can healthcare providers stay informed about changes in RADV?
Staying informed involves continuous learning, monitoring industry developments, and adapting to potential changes in RADV regulations.
1 note
·
View note
Text
Telehealth Providers: A Detailed Review For People
Write-Up Composed By-Barker Bowman
For clients, telehealth solutions enable them to gain access to clinical advice and treatment from anywhere they are, even in the house. People can also talk with clinical experts in a variety of medical settings and specializeds.
This enhanced availability to medical care specialists indicates an individual can get help quickly without putting themselves, their family, or the area in danger (e.g. throughout the COVID-19 pandemic).
What is Telehealth?
Telehealth is a wide term made use of to explain remote health care solutions. It encompasses a range of modern technologies that sustain medical and health-related services, consisting of videoconferencing, streaming media, store-and-forward imaging, terrestrial and wireless communications. The Wellness Resources and Administration (HRSA) specifies telehealth as "using electronic info and telecommunications technologies to support long-distance medical health care, client and specialist health-related education and learning and public health."
The most well-known kind of telehealth is remote treatment by physicians and other healthcare providers utilizing videoconferencing technology. This allows individuals to obtain the very same solutions they would in-person, including physical exams, psychiatric therapy, and diagnosis of disease.
In addition, telehealth can also include remote nonclinical health services such as physician training and administrative conferences. It can even consist of remote monitoring of home health and wellness conditions such as heart rate, blood pressure and glucose levels. Making use of telehealth helps in reducing the need for individuals to travel to facilities, which is specifically helpful for those with limited flexibility and those living in backwoods.
Those that utilize telehealth are typically very satisfied with the experience and ease. Several of the factors for this contentment include expense savings from not needing to travel, increased worker productivity by not needing to take some time off work and having to leave their task website, in addition to accessibility to specialized doctors that may or else not be available.
In terms of the future, there are lots of things that can raise telehealth's appeal and make it a lot more accessible. Some of these variables consist of an expansion of Medicare's telehealth protection, reimbursement parity between telehealth visits and in-person appointments, and raised research study on the cost-effectiveness of telehealth. Additionally, it is important that broadband Internet is extensively readily available in all areas and that the costs of telehealth solutions are cost effective for all people. If these problems are fixed, it is likely that telehealth will certainly come to be a lot more extensive in the coming years.
Advantages of Telehealth
Aside from its incredibly convenient nature, there are numerous methods telehealth services advantage clients. For https://www.verywellhealth.com/treatments-for-loss-of-cartilage-in-knee-5096944 , they save on traveling expenditures. Instead of needing to pay for gas, tolls, and parking, people can merely get in touch with their clinician on-demand from the comfort of their office or home.
An additional advantage is that telehealth consultations are usually much less taxing. A normal check out with a company lasts around 20 mins, whereas the average in-person visit with a medical professional is 45-50 mins. Having shorter gos to suggests that patients do not need to take as much pause work, find a babysitter or caretaker, and even leave your home if they are really feeling ill.
For individuals who need to deal with persistent health problems, telehealth can also make it less complicated for them to manage their treatment plan. As an example, if a person experiences a problem like blepharitis, a typical eye condition that triggers inflammation, irritation, and itching in the top eyelids, they can often obtain a prescription for medicated eye declines or ointments via a telehealth visit with their carrier.
In addition, telehealth solutions help to avoid the spread of diseases. During the COVID-19 pandemic, as an example, permitting patients to communicate with doctor remotely was an essential device to avoid the unneeded spread of microorganisms. The same could be true for future pandemics or various other conditions, as telehealth allows people to contact their doctors without having to place other individuals in jeopardy in their neighborhoods.
#Assisted Living#Senior Care#Elder Care#Retirement Home#Senior Living Communities#Assisted Living Facility#Memory Care#Long Term Care Facilities#Senior Care Centers#Senior Home Care#Nursing Home#Personal Care#Home Care Assistance#Home Care Agency#Telehealth#Telehealth Services#Telehealth Nurse#Senior Telehealth Care
0 notes
Text
youtube
Let's explain the differences between original Medicare, managed by the federal government with set premiums and coverage parameters, and Medicare Advantage, a private health insurance alternative offering additional benefits.
There are similarities in basic medical care coverage, including hospital stays, doctor visits, and diagnostic tests.
Medicare Advantage plans provide additional services, such as dental, vision, and hearing coverage, along with potential extras like gym memberships and transportation.
There is also a difference in the flexibility of choosing doctors under original Medicare compared to Advantage plans, which often have specified networks.
Drug coverage requires plan D under original Medicare while roughly 90% of Advantage plans have this included.
There are cost factors to consider, where Original Medicare has deductibles and potential supplemental policies, while Medicare Advantage plans may have additional premiums, deductibles, or copays.
0 notes