#Bernard Soulier Syndrome
Text
When to worry about thrombosis — Rarely, patients with thrombocytopenia are at risk for thrombosis rather than, or in addition to, bleeding. While most of the implicated disorders are rare, it is important to consider them because urgent treatment may be needed to prevent life-threatening thrombotic events.
Examples include the following:
●Heparin-induced thrombocytopenia – A small percentage of patients exposed to heparin (less than 5 percent) will develop heparin-induced thrombocytopenia (HIT) in which antibodies to a platelet factor 4 epitope induced by heparin can cause thrombocytopenia and platelet activation, leading to life-threatening venous and/or arterial thrombosis. This diagnosis should be considered in a patient recently exposed to heparin who develops thrombocytopenia, thrombosis, anaphylaxis, or skin reactions. Treatment involves immediate discontinuation of heparin and administration of a non-heparin anticoagulant (e.g., dabigatran or bivalirudin).
●Vaccine-induced immune thrombotic thrombocytopenia (VITT) – VITT is a rare syndrome that occurs after vaccination with coronavirus disease 2019 (COVID-19) adenoviral vector vaccines (AstraZeneca and Janssen [Johnson & Johnson]). It resembles spontaneous HIT in that there is no prior heparin exposure, and it is associated with life-threatening venous and/or arterial thrombosis. Individuals with thrombosis and/or thrombocytopenia should be evaluated for recent administration of a COVID-19 vaccine within the preceding 5 to 30 days, and for which specific type of vaccine they received.
●Antiphospholipid syndrome – The antiphospholipid syndrome (APS) can develop in individuals with systemic lupus erythematosus, other medical conditions (eg, infection, medications, cancer), or in individuals without an underlying condition. Patients may have venous and/or arterial thrombosis. Treatment involves anticoagulation or aspirin, and treatment of any underlying condition.
●Disseminated intravascular coagulation – Patients with disseminated intravascular coagulation (DIC) are at risk of bleeding or thrombosis, usually venous. DIC is commonly seen in acutely ill patients with sepsis or malignancy, but it can also be seen in a variety of other conditions.
●Thrombotic microangiopathy – Thrombotic microangiopathies (TMAs) such as thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), or drug-induced TMA (DITMA) are associated with small-vessel platelet-rich thrombi. These microthrombi can occur in any organ and can be life-threatening. Plasma exchange for TTP may be life-saving and should be initiated immediately when TTP is suspected.
●Paroxysmal nocturnal hemoglobinuria – Paroxysmal nocturnal hemoglobinuria (PNH) is a rare condition caused by loss of glycosyl phosphatidylinositol from cell membranes. Thrombosis (often involving unusual locations such as intraabdominal or cerebral veins) can occur, along with hemolytic anemia and/or bone marrow failure. Treatment depends on the degree of cytopenias and the presence of thrombosis.
●ITP with a concomitant thrombotic disorder – Certain conditions can occur in patients with ITP increasing their risk of thrombosis such as atrial fibrillation or recent or previous deep vein thrombosis. Management of anticoagulation in that population can be challenging; however, it is important to note that the low platelet count is not protective against thrombosis, and anticoagulation is often indicated.
Work up:
Peripheral blood smear — Review of the peripheral blood smear is used to exclude pseudothrombocytopenia (eg, falsely low platelet count due to platelet clumping) and to evaluate morphologic abnormalities of blood cells that could be useful in determining the cause of thrombocytopenia. As an example, giant platelets may suggest a congenital platelet disorder (eg, MYH-9-related disorders, Bernard Soulier syndrome [BSS]); these may be counted as red blood cells by some automated counters.
Pseudothrombocytopenia — The possibility of pseudothrombocytopenia (ie, falsely low platelet count) should be eliminated before any further evaluation is undertaken. Pseudothrombocytopenia can occur in a number of settings, all of which can be identified by review of the peripheral blood smear and/or repeating the CBC using a non-EDTA anticoagulant:
●Incompletely mixed or inadequately anticoagulated samples may form a clot that traps platelets in the collection tube and prevents them from being counted.
●In approximately 0.1 percent of individuals, exposure of patient samples to the EDTA anticoagulant in the collection tube can induce platelet clumps or platelet rosettes around white blood cells (WBCs). These may be counted by automated counters as leukocytes rather than platelets. The mechanism is "naturally occurring" platelet autoantibodies directed against a concealed epitope on platelet membrane glycoprotein (GP) IIb/IIIa that becomes exposed by EDTA-induced dissociation of GPIIb/IIIa [45-52].
If platelet clumping is observed, the platelet count is repeated using heparin or sodium citrate as an anticoagulant in the collection tube. If citrate is used, the platelet count should be corrected for dilution caused by the amount of citrate solution; no such correction is needed for heparin. Alternatively, fresh, non-anticoagulated blood can be pipetted directly into platelet-counting diluent fluid.
RBC and WBC abnormalities — Abnormal RBC and WBC morphologies may suggest a specific condition.
Examples include the following:
●Schistocytes suggest a microangiopathic process (eg, DIC, TTP, HUS, DITMA).
●Nucleated RBCs, and Howell-Jolly bodies, may be seen post-splenectomy or occasionally in patients with poor splenic function.
●Spherocytes suggest immune-mediated hemolytic anemia or hereditary spherocytosis.
●Leukoerythroblastic findings, teardrop cells, nucleated RBCs, or immature granulocytes suggest an infiltrative process in the bone marrow.
●Leukocytosis with a predominance of bands and/or toxic granulations suggests infection.
●Immature WBCs (eg, myeloblasts) or dysplastic WBCs suggest leukemia or myelodysplasia.
●Multi-lobed/hypersegmented neutrophils (ie, more than 5 lobes) suggest a megaloblastic process (eg, B12/folate/copper deficiency).
HIV and HCV testing — Thrombocytopenia has been identified as an important "indicator condition" for HIV infection. Thus, adults with new thrombocytopenia should have HIV testing if not done recently.
Thrombocytopenia may also be seen with hepatitis C virus (HCV) infection; testing is appropriate for adults with thrombocytopenia if not done recently. Other laboratory testing — Aside from the testing mentioned above (CBC, review of peripheral smear, HIV and HCV testing), no additional laboratory testing is absolutely required in a patient with isolated thrombocytopenia. However, additional testing may be warranted in patients with other findings.
Examples of findings that may trigger other laboratory testing include the following:
●Symptoms or findings of systemic autoimmune disorders (eg, systemic lupus erythematosus [SLE], anti-phospholipid syndrome [APS]) may prompt testing for anti-nuclear antibodies or anti-phospholipid antibodies, respectively. We do not test for these in patients with isolated thrombocytopenia and no signs or symptoms suggestive of SLE or APS.
●Findings of liver disease should prompt measurements of hepatic enzymes and possibly tests of liver synthetic function (eg, albumin, coagulation testing), depending on the severity of the liver disease.
●Thrombosis should prompt consideration of DIC, heparin-induced thrombocytopenia (HIT) and related syndromes, and APS. Depending on the site of thrombosis and other hematologic findings, paroxysmal nocturnal hemoglobinuria (PNH) may also be a consideration.
●Microangiopathic changes on the peripheral smear should prompt coagulation testing (eg, PT, aPTT, fibrinogen) and measurement of serum lactate dehydrogenase (LDH) and renal function to evaluate for DIC, TTP, or HUS; with subsequent evaluation based on the results.
ADDITIONAL EVALUATION
Hematologist referral/consultation — Referral to a hematologist is appropriate to confirm any new diagnosis of a thrombocytopenic condition or to determine the cause of any unexplained thrombocytopenia. The urgency of referral depends on the degree of thrombocytopenia and other abnormalities, and the stability of the findings.
In hospitalized patients, some conditions are medical emergencies that require immediate action. Immediate hematologist involvement in diagnosis and management is appropriate for the following:
●Suspected thrombotic thrombocytopenic purpura (TTP) or hemolytic uremic syndrome (HUS).
●Suspected heparin-induced thrombocytopenia (HIT).
●Suspected COVID-19 vaccine-induced immune thrombotic thrombocytopenia (VITT).
●Suspected hematologic malignancy (eg, acute leukemia), aplastic anemia, or other bone marrow failure syndrome.
The consulting hematologist can also assist in diagnosis and management of patients with severe thrombocytopenia (ie, platelet count less than 50,000/microL) who have serious bleeding or require an urgent invasive procedure, and in pregnant women with severe thrombocytopenia, regardless of the cause.
Bone marrow evaluation — Bone marrow evaluation (aspirate and biopsy) is not required in all patients with thrombocytopenia. However, it may be helpful in some patients if the cause of thrombocytopenia is unclear, or if a primary hematologic disorder is suspected. A possible exception may be a clinical picture consistent with a nutrient deficiency in which a bone marrow would only be needed if a deficiency could not be documented, or if the hematologic findings did not resolve upon nutrient repletion.
The following bone marrow findings may be helpful:
●Normal or increased numbers of megakaryocytes suggests that the thrombocytopenia is due, at least in part, to a condition associated with platelet destruction (eg, ITP, drug-induced immune thrombocytopenia).
●Decreased megakaryocyte numbers, along with overall decreased or absent cellularity (picture 18 and picture 19), is consistent with decreased bone marrow production of platelets, as in aplastic anemia.
●In rare cases, severe reduction or absence of megakaryocytes with no other abnormalities (also called acquired amegakaryocytic thrombocytopenia or acquired pure megakaryocytic aplasia) may occur. This finding is most often reported in patients with SLE, and is typically due to an autoantibody directed against the thrombopoietin receptor.
●Megaloblastic changes in the RBC and granulocytic series suggest a nutrient deficiency (eg, vitamin B12, folate, copper) (picture 20), while dysplastic changes suggest a myelodysplastic disorder (picture 21 and picture 22).
●Granulomata, increased reticulin or collagen fibrosis (picture 23 and picture 24), or infiltration with malignant cells (picture 25) establishes the diagnosis of bone marrow invasion, especially when a leukoerythroblastic blood picture is also present.
GENERAL MANAGEMENT PRINCIPLES
There are some general management principles that apply to all patients with thrombocytopenia regardless of the cause, and for which questions may arise before a diagnosis has been established.
●Activity restrictions – Patients who are otherwise healthy and have no manifestations of petechiae or purpura may not require activity restrictions.
Individual considerations apply to participation in certain activities. As an example, individuals with severe thrombocytopenia (less than 50,000/microL) generally should not participate in extreme athletics such as boxing, rugby, and martial arts. However, no restrictions are necessary for usual activities or low-impact exercise.
●Anticoagulant and anti-platelet medications – For anticoagulant and anti-platelet medications, the clinical indications and risks associated with discontinuation (eg, thrombosis) are balanced against the bleeding risk associated with the degree of thrombocytopenia and of continuing the anticoagulant and/or anti-platelet medication [7]. Input from the consulting specialist who prescribed the medication and/or the hematologist may be sought. A discussion of anticoagulation in adults with thrombocytopenia is presented separately.
It is also important to note that thrombocytopenia by itself does not protect against venous or arterial thrombosis, and appropriate use of thromboprophylaxis or anticoagulants should not be withheld from a patient with mild to moderate thrombocytopenia (eg, greater than 50,000/microL) if it is indicated (eg, postoperatively). For patients with more severe thrombocytopenia, decisions are made on a case-by-case basis regarding the risks of bleeding and benefits of anticoagulation.
●Over-the-counter remedies – Patients should be educated about which non-prescription remedies interfere with platelet function (eg, aspirin, nonsteroidal anti-inflammatory drugs, ginkgo biloba). In general, these agents are avoided unless there is a specific indication for which equivalent alternatives are lacking.
●Safe platelet count for invasive procedures – Most platelet count thresholds for invasive procedures are based on weak observational evidence at best. In general, procedures with a greater risk of bleeding are performed at higher platelet counts. While there is some flexibility in individual circumstances, anesthesiologists and surgeons performing these procedures will have the last word. A listing of general guidelines used for different procedures is presented separately.
Optimal methods for raising the platelet count in preparation for an invasive procedure depend on the underlying condition (eg, corticosteroids or intravenous immune globulin (IVIG) for presumptive ITP; platelet transfusion for myelodysplastic syndromes). These approaches are discussed in detail in separate topic reviews.
Individuals with impaired platelet function may require platelet transfusions despite adequate platelet counts, depending on the procedure. Attention should also be paid to correcting coagulation abnormalities if present.
●Emergency management of bleeding – Urgent management of critical bleeding in the setting of severe thrombocytopenia requires immediate platelet transfusion, regardless of the underlying cause.
6 notes
·
View notes
Text
Victor McKusick, “Mendelian Inheritance in Man”, 1966, Chromosome #22.
Here I present: Victor McKusick, “Mendelian Inheritance in Man”, 1966, Chromosome #22. This book was printed in twelve (12) editions from 1966 to 1998 shown ABOVE. There are fifty-three (53) alleles of chromosome #22 listed BELOW.
Cat eye syndrome.
Thrombophilia.
Rhabdoid predisposition syndrome, familial.
Schizophrenia susceptibility locus.
Bernard-Soulier syndrome, type B.
Giant platelet…

View On WordPress
0 notes
Photo
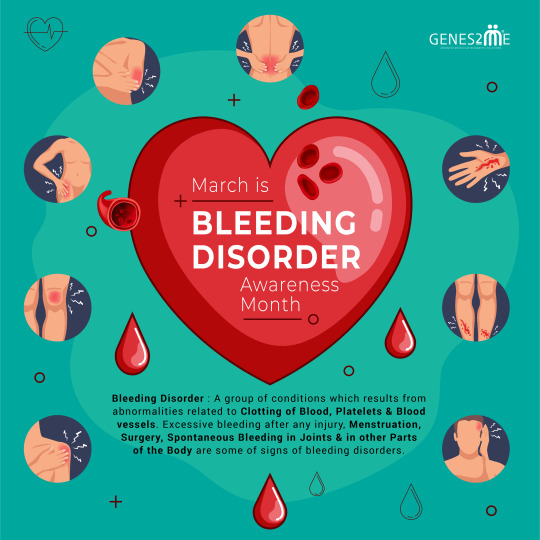
Bleeding Disorder: A group of conditions which results from abnormalities related to clotting of blood, platelets & blood vessels. Excessive bleeding after any injury, menstruation, surgery, spontaneous bleeding in joints & in other parts of the body are some of signs of bleeding disorders.
Hemophilia A & B, Von Willebrand Disease, #FactorXIIIDeficiency, #FactorVIIDeficiency, #FactorXDeficiency, #CongenitalFibrinogenDeficiency, #BernardSoulierSyndrome : some of the common bleeding disorders. Bleeding disorders can either be acquired or inherited.
Lack of awareness about such conditions especially sometimes because of the invisible symptoms makes the life of a person affected with bleeding disorder living with chronic pain really hard. These disorders are rare and oftenly not taken seriously by people. Challenges of people living with rare bleeding disorders shouldn’t be ignored.
#BleedingDisordersAwarenessMonth #HemophiliaA #HemophiliaB #bloodclots #coagulation #inherited #diagnostic #healthcare #health #testing
Connect Today - #GENES2ME
18001214030
#factor SIII Deficiency#Factor VII Deficiency#Factor X Deficiency#Congenital Fibrinogen Deficiency#Bernard Soulier Syndrome#Blood Clots#Hemophilia B#Hemophilia A#health#health care#genetics#genetic testing in delhi
0 notes
Link
We continue the theme of bleeding and clotting with a handful of important genetic conditions. Today: clotting.
The most common inherited *clotting* disorder (thrombophilia="loves to clot") is Factor V Leiden mutation. Deficient or defective Factor V causes a rare variant of hemophilia; by contrast, the FVL mutation makes Factor V resistant to activated Protein C, whose job is to degrade clots. "[Factor V Leiden] is present in 5% of the white population and 1.2% of the black population. Factor V Leiden increases the risk of venous thrombosis 3- to 8-fold for heterozygous and 30- to 140-fold for homozygous individuals." Individuals may present with deep vein thrombosis and/or pulmonary embolism, typically provoked by pregnancy, oral contraceptive pills, surgery, immobilization or old age.
Pro-Tip: Platelet function disorders are rare and include Bernard-Soulier syndrome, a platelet adhesion disorder, and Glanzmann thrombasthenia, a platelet aggregation disorder.
2 notes
·
View notes
Text
Bernard - Soulier syndrome AR
Plt gp1b/IX defect in binding of VWB fail to response to ristocetin
Giant PLT
0 notes
Text
Global Platelet Aggregation Devices Market Trends, Industry Report 2027

New York, NY 14 May 2021: The global platelet aggregation devices market size is expected to reach USD 1,556.8 million by 2027 according to a new study by Polaris Market Research. The report “Platelet Aggregation Devices Market Share, Size, Trends, Industry Analysis Report, By Product (Systems, Reagents, Consumables and Accessories); By Application (Research Applications, Clinical Applications, Others); By End Use (Standalone Hospitals, Diagnostic Laboratories, Research and Academic Institutes, Blood Banks, and Other End Users); By Regions; Segment Forecast, 2020 –2027” gives a detailed insight into current market dynamics and provides analysis on future market growth.
Platelet aggregation is the biological process where the platelet cells are employed in a process to prevent bleeding through vaso-constriction for rapid clot formation. The whole process is mediated via platelet aggregating factor (PAF). The quantitative and qualitative defects of platelets lead to increased bleeding. The high reactivity of platelets in the patients having anti-platelet therapy results in thromboembolic complications.
Platelet function related disorders can be either inherited or acquired. The inherited platelet function disorders include Von Willebrand disease, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Storage pool disease. The acquired platelet dysfunction may be caused by chronic conditions such as kidney failure (uremia), Myelodysplastic syndrome (MDS), Leukemias (chronic myeloid leukemia or CML; acute myeloid leukemia or AML).
Some acquired platelet disorders are temporary because of the decreased function of platelets due to anti-platelet medications, non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, antihistamines and some antibiotics. The platelet function testing is transitioned from diagnostics for heritable diseases to a functional one for platelet functional therapies. The rapid usage of anti-platelet therapy, mainly dual anti-platelet therapy has changed the focus of platelet function testing from diagnostics to therapeutics.
Request For Sample Copy @ https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-sample
The market is driven by few notable factors such as the recent surge in infectious diseases (COVID-19) requiring rapid serological tests, innovations in platelet aggregation mechanisms, systems and consumables, and worldwide rise in chronic ailments. Specialized tests based on platelet aggregation include light transmission platelet aggregometry on platelet-rich plasma (LTA), impedance whole blood aggregometry (WBA), Lumi-aggregometry and flow cytometry.
Automated haematology analyzers can be used to obtain platelet counts over a wide range of values using optical counting methods like light scatter or fluorescence. Screening tests such as prothrombin time (PT) or activated partial thromboplastin time (aPTT) are more standardized and fully automated.
Number of reagents are available in the market to carry out the platelet function tests. These reagents include collagen, thrombin, ADP, vasopressin, epinephrine and ristocetin. Collagen, ADP were used in routine platelet aggregation studies for the evaluation of qualitative platelet function disorders.
Market participants such as F. Hoffmann La-Roche Ltd., Drucker Diagnostics, Haemonetics Corporation, Sysmex Corporation, Siemens Healthineers, Chrono-log Corporation, Instrumentation Laboratory, Accriva Diagnostics, Matis Medical, Helena Laboratories Corporation, Sienco, Inc., Bio/Data Corporation, Tem Group, WerfenLife, S.A., Laboratory Corporation of America Holdings, Sentinel CH. S.p.A., and Aggredyne, Inc. are some of the key players operating in the concerned market.
To get Incredible Discounts on this Premium Report, Click At: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-discount-pricing
Polaris Market research has segmented the vascular access devices market report on the basis of product, application, end-use and region
Platelet Aggregation Devices Type Outlook (Revenue – USD Million, 2016 – 2027)
Systems
Reagents
Consumables and Accessories
Platelet Aggregation Devices Application Outlook (Revenue – USD Million, 2016 – 2027)
Research Applications
Clinical Applications
Others
Platelet Aggregation Devices End-Use Outlook (Revenue – USD Million, 2016 – 2027)
Standalone Hospitals
Diagnostic Laboratories
Research and Academic Institutes
Blood Banks
Other End Users
Have Any Query or Specific Requirement? Request for customization: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-customization
About Polaris Market Research
Polaris Market Research is a global market research and consulting company. The company specializes in providing exceptional market intelligence and in-depth business research services for our clientele spread across different enterprises.
Contact Us:
Polaris Market Research
Phone: 1–646–568–9980
Email: [email protected]
Web: http://www.polarismarketresearch.com
0 notes
Text
Platelet Aggregation Devices Market 2021 Global Industry Analysis by Trends, Size, Share, Company Overview
The Global Platelet Aggregation Devices Market Size Is Expected To Reach USD 1,556.8 Million by 2027 according to a new study by Polaris Market Research. Platelet aggregation is the biological process where the platelet cells are employed in a process to prevent bleeding through vaso-constriction for rapid clot formation. The whole process is mediated via platelet aggregating factor (PAF). The quantitative and qualitative defects of platelets lead to increased bleeding. The high reactivity of platelets in the patients having anti-platelet therapy results in thromboembolic complications.
Platelet function related disorders can be either inherited or acquired. The inherited platelet function disorders include Von Willebrand disease, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Storage pool disease. The acquired platelet dysfunction may be caused by chronic conditions such as kidney failure (uremia), Myelodysplastic syndrome (MDS), Leukemias (chronic myeloid leukemia or CML; acute myeloid leukemia or AML).
Request A Sample Report at : https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-sample
Some acquired platelet disorders are temporary because of the decreased function of platelets due to anti-platelet medications, non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, antihistamines and some antibiotics. The platelet function testing is transitioned from diagnostics for heritable diseases to a functional one for platelet functional therapies. The rapid usage of anti-platelet therapy, mainly dual anti-platelet therapy has changed the focus of platelet function testing from diagnostics to therapeutics.
The market is driven by few notable factors such as the recent surge in infectious diseases (COVID-19) requiring rapid serological tests, innovations in platelet aggregation mechanisms, systems and consumables, and worldwide rise in chronic ailments. Specialized tests based on platelet aggregation include light transmission platelet aggregometry on platelet-rich plasma (LTA), impedance whole blood aggregometry (WBA), Lumi-aggregometry and flow cytometry.
Automated haematology analyzers can be used to obtain platelet counts over a wide range of values using optical counting methods like light scatter or fluorescence. Screening tests such as prothrombin time (PT) or activated partial thromboplastin time (aPTT) are more standardized and fully automated.
Request for Discount Pricing with Your Specific Research Needs At : https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-discount-pricing
Number of reagents are available in the market to carry out the platelet function tests. These reagents include collagen, thrombin, ADP, vasopressin, epinephrine and ristocetin. Collagen, ADP were used in routine platelet aggregation studies for the evaluation of qualitative platelet function disorders.
Market participants such as F. Hoffmann La-Roche Ltd., Drucker Diagnostics, Haemonetics Corporation, Sysmex Corporation, Siemens Healthineers, Chrono-log Corporation, Instrumentation Laboratory, Accriva Diagnostics, Matis Medical, Helena Laboratories Corporation, Sienco, Inc., Bio/Data Corporation, Tem Group, WerfenLife, S.A., Laboratory Corporation of America Holdings, Sentinel CH. S.p.A., and Aggredyne, Inc. are some of the key players operating in the concerned market.
Have Questions? Or make an Inquiry before buying this report Speak to Our Industry Expert: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/speak-to-analyst
#Platelet Aggregation Devices Market#Platelet Aggregation Devices Market size#Platelet Aggregation Devices Market share
0 notes
Link
The global platelet aggregation devices market size is expected to reach USD 1,556.8 million by 2027 according to a new study by Polaris Market Research. The report “Platelet Aggregation Devices Market Share, Size, Trends, Industry Analysis Report, By Product (Systems, Reagents, Consumables and Accessories); By Application (Research Applications, Clinical Applications, Others); By End Use (Standalone Hospitals, Diagnostic Laboratories, Research and Academic Institutes, Blood Banks, and Other End Users); By Regions; Segment Forecast, 2020 –2027” gives a detailed insight into current market dynamics and provides analysis on future market growth.
Platelet aggregation is the biological process where the platelet cells are employed in a process to prevent bleeding through vaso-constriction for rapid clot formation. The whole process is mediated via platelet aggregating factor (PAF). The quantitative and qualitative defects of platelets lead to increased bleeding. The high reactivity of platelets in the patients having anti-platelet therapy results in thromboembolic complications.
Get Sample Copy of report: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-sample
Platelet function related disorders can be either inherited or acquired. The inherited platelet function disorders include Von Willebrand disease, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Storage pool disease. The acquired platelet dysfunction may be caused by chronic conditions such as kidney failure (uremia), Myelodysplastic syndrome (MDS), Leukemias (chronic myeloid leukemia or CML; acute myeloid leukemia or AML).
Some acquired platelet disorders are temporary because of the decreased function of platelets due to anti-platelet medications, non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, antihistamines and some antibiotics. The platelet function testing is transitioned from diagnostics for heritable diseases to a functional one for platelet functional therapies. The rapid usage of anti-platelet therapy, mainly dual anti-platelet therapy has changed the focus of platelet function testing from diagnostics to therapeutics.
Market participants such as F. Hoffmann La-Roche Ltd., Drucker Diagnostics, Haemonetics Corporation, Sysmex Corporation, Siemens Healthineers, Chrono-log Corporation, Instrumentation Laboratory, Accriva Diagnostics, Matis Medical, Helena Laboratories Corporation, Sienco, Inc., Bio/Data Corporation, Tem Group, WerfenLife, S.A., Laboratory Corporation of America Holdings, Sentinel CH. S.p.A., and Aggredyne, Inc. are some of the key players operating in the concerned market.
Request For Discount: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-discount-pricing
About Polaris Market Research
Polaris Market Research is a global market research and consulting company. The company specializes in providing exceptional market intelligence and in-depth business research services for our clientele spread across different enterprises. We at Polaris are obliged to serve our diverse customer base present across the industries of healthcare, technology, semi-conductors and chemicals among various other industries present around the world
Contact us
Polaris Market Research
Phone: 1-646-568-9980
Email: [email protected]
Web: www.polarismarketresearch.com
0 notes
Text
Bernard-Soulier syndrome is a deficit in GPIb. Without GPIb, platelets can't adhere to vWF. So platelet adhesion is disrupted.
1 note
·
View note
Link
0 notes
Text
ABIM: Hematology
ABIM syllabus can be found here
Let me know if you find any errors
Sources: UWorld, MKSAP 16/17, Rizk Review Course, Louisville Lectures, Knowmedge (free version)
Hypoproliferative anemia
Aplastic anemia:
- associated with autoimmune diseases, thymomas <-- need CT chest, Tx with resection
- Tx all patients with PPx anticoagulation + iron + folic acid; if <40yo: stem cell transplant
- associated with PNH: pancytopenia/hemolytic anemia with need for transfusions + Budd-Chiari/venous thrombosis/CVA/MI + morning hematuria/iron deficiency, associated with AML; Dx: flow cytometry shows lack of CD55, CD59; Tx: iron + Eculizumab to decrease need for transfusions (AE of Eculizumab is increased risk of meningococcal infections) +/- (if thrombus) warfarin; if <40yo: allogenic BMT
Iron deficiency anemia:
- decreased iron, ferritin, transferrin; increased TIBC, RDW
- associated with gastric surgery, restless leg syndrome
- colon cancer until proven otherwise
- also seen in:
(1) Celiac disease: IBS Sx with iron deficiency that is unresponsive to oral supplementation; Dx: tissue transglutaminase Ab --> if neg: small bowel biopsy
(2) Plummer-Vinson: esophageal webs, glossitis; associated with squamous cell esophageal carcinoma
(3) Osler-Weber-Rendu/Hereditary Hemorrhagic Telangiectasia: lip/oral telangiectasias + epistaxis + +FOBT associated with hemoptysis/brain bleed
- Tx iron deficiency: PO supplementation x6mo or IV iron gluconate (dextran is associated with anaphylaxis)
Sideroblastic anemia:
- ringed sideroblasts/basophilic stippling on PBS seen in EtOH, lead toxicity (Burton line on teeth, deposition in metaphysis, RTA type II (hypokalemia, glucosuria)), copper deficiency, and use of INH (from B6 deficiency), chloramphenicol, Linezolid
- Tx hereditary sideroblastic anemia with pyridoxine/B6
Megaloblastic anemia: MCV>100, hypersegmented PMNs, associated with EtOH use
(1) B12 deficiency: peripheral paresthesias; associated with strict vegetarians and Crohn’s disease (terminal ileum disease), elevated methylmalonic acid > homocysteine
(2) Pernicious anemia: anti-IF antibodies causing B12 deficiency; associated with autoimmune diseases and increased risk of gastric cancer
(3) folate deficiency: no paresthesias; associated with pregnancy, EtOH, and Bactrim use; elevated homocysteine only
Pure red cell aplasia: associated with AIDS + Parvovirus B19; Dx: flow cytometry shows monoclonal CD57+ T-cells; Tx: IVIg and check for thymoma with CT chest
Hemolytic anemia
- PBS shows schistocytes (vs. dacryocytes/tear drop cells with 2 line involvement in Myelodysplastic syndrome)
- appropriate reticulocyte response = >100,000/uL
- Tx chronic hemolytic anemia with folate
- Scleroderma renal crisis (HTN, AKI, MAHA): Tx with ACEi (Captopril) even iff pregnant
- MAHA in the setting of mechanical heart valve needs emergent TEE to check for leak/regurg
Glucose-6-phosphate dehydrogenase deficiency:
- remember food: fava beans, bite cells, Heinz bodies (red spots in RBCs; looks kind of like a pink boob with 1 or more red nipples)
- associated with sulfa drugs, infection, and DKA --> hemolysis
- has decreased glutathione levels
Pyruvate kinase deficiency: Tx with PRN transfusions --> severe?: splenectomy
Autoimmune hemolytic anemia: Coomb’s/DAT positive
(1) warm immunoglobulins:
- IgG, DAT+ with spherocytosis
- associated with autoimmune (SLE, UC), HIV, CLL
- Tx steroids --> splenectomy --> refractory Tx: IVIg, AZT, cyclophosphamide, Rituximab
(2) cold:
- IgM (Mmm cold ice cream), occurs in cold temperatures
- associated with malignancies, mono, mycoplasma
- Tx: avoid the cold, Rituxan
Microangiopathic hemolytic anemia: Tx: plasma exchange +/- corticosteroids
- Sx: “FAT RN” (fever, anemia, thrombocytopenia, renal failure, neuro sx)
- Dx: normal coags, D-dimer, fibrinogen (vs. DIC = elevated coags and D-dimer; decreased fibrinogen, platelets)
*FYI: ITP, TTP/HUS, and HELLP all have normal coags
(1) TTP: primarily neurologic symptoms
- increased vWF multimers/decreased ADAMSTS13 (NOT needed for diagnosis)
- associated with tacrolimus, cyclosporine, plavix/ticlodipine, quinine
- Tx: plasmapheresis
*if >20 weeks pregnant, this is TTP and does NOT resolve with delivery
(2) HUS: primarily renal symptoms
- associated with E.coli/Shigella diarrhea and cyclosporine
- Tx: discontinue cyclosporine!, supportive, plasmapheresis
Hereditary spherocytosis:
- jaundice from unconj/indirect hyperbilirubinemia, pigmented gallstones, splenomegaly, leg ulcers
- PBS shows spherocytes and Howell-Jolly bodies (blue dot in RBC seen in splenectomy); DAT negative (vs. DAT+ in warm hemolytic anemia; see above)
- Dx: osmotic fragility test --> flow cytometry
- Tx: splenectomy
Wilson’s: young patient with hemolytic anemia + psychosis + transaminitis
Hemoglobinopathies and thalassemias
- present as microcytic anemias: MCV <80; target cells
Alpha thalassemia: has normal Hb electrophoresis
--, -x = HbH: hemolysis, splenomegaly, Heinz body
- --,-- = Barts / Hydrops fetalis (dies before birth)
Beta thalassemia: abnormal Hb electrophoresis
- minor: elevated HbA2 (alpha 2 gamma 2) and HbF
- intermedia: elevated HbA2 only; Tx: intermittent transfusion +/- iron chelation if Fe>1000
- Major: elevated HbF, decreased HbA; Tx: splenectomy and allogenic stem cell transplant
Hemoglobinopathy: severe disease requires stem cell transplant
Leukocyte disorders
(1) AML: t(15;17)
- associated with PCV, Fanconi’s, Down’s, Klinefelter’s, CML, XRT/chemo, benzenes, MDS
- presents acutely as sepsis (decreased PMNs, anemia, thrombocytopenia)
- pallor, gingival hypertrophy (M5), fatigue, easy spontaneous bleeding/purpura (due to thrombocytopenia), and NO hepatosplenomegaly or lymphadenopathy
- M3 (Auer rods) associated with DIC Tx: ATRA
*ATRA AE: after 1-3 weeks --> fever, leukocytosis, pulmonary infiltrates/hypoxemia; Tx: dexamethasone
*prevent TLS (hyperkalemic paresthesia/weakness, hypocalcemic tetany, bronchospasm, AKI) with Allopurinol BEFORE chemo --> Rasburicase
(2) CML: t(9;22)/BCR-ABL, decreased LAP
- asymptomatic splenomegaly with elevated WBC (symptomatic when >200) with increased Eosinophils and Basophils
- Tx: Imatinib/Gleevec (TKI)
(3) ALL: TdT, anterior mediastinal mass (thymoma <-- chest CT)/bulky mediastinal lymphadenopathy with bone pain and CNS involvement
- increased blasts (>30%)
- Tx: combo chemo (intrathecal if CNS involvement) +/- XRT if bulky disease --> stem cell
(4) CLL: B2microglobulin; CD5, CD23 B-cells; smudge cells
- asymptomatic, lymphadenopathy, hepatosplenomegaly, lymphocytosis, thrombocytopenia
- Tx: watchful waiting if asymptomatic; Bendamustine+Rituxan > Fludarabine + Bactrim PPx
*AE: Richter’s syndrome: transformation into aggressive large cell lymphoma
*Evan’s syndrome: AIHA + ITP
(5) Hairy cell: older patient with pancytopenia, splenomegaly, dry fibrotic bone marrow
- associated with PAN
- Dx: flow-cytometry: CD11c, CD103+; +TRAP
- Tx: Cladribine
Platelet disorders
*Rule of thumb: transfuse if Plt <10 or if ICH/pulm hemorrhage <40-50; 1 bag of platelets corrects by 25k
*give IVIg + steroids if pregnant with Plt <50
*Plt >50 = okay for surgery
Idiopathic thrombocytopenic purpura: diagnosis of exclusion
- Dx: PBS, DAT+ (don’t order anti-Plt antibodies)
- Tx (if symptomatic or Plt <15): steroids --> IVIg/Rhogam --> refractory: splenectomy, Rituxan
Heparin-induced thrombocytopenia (HIT):
- 4T’s: thrombocytopenia (2pts: >50%, 1pt: 30-50, 0pt: <30), timing (>5days, ?>5, <4), thrombosis (+, ?, -), no other cause (yes, maybe, no); score 6-8 = high, 0-3 low
- Dx: PF4, SRA
- Tx: stop Heparin (warfarin is NOT contraindicated!); switch to Argatroban
Essential thrombocythemia:
- “Jack et Vera are Buddies” (”et” in Latin is “and”): Jak2 mutations are associated with ET, polycythemia Vera, and Budd-Chiari”
- JAK2, CALR, BCR-ABL, NPL1
- Plt >600 --> livedo reticularis, erythromelagia (painful red hands/feet, Tx: ASA), headache, vision changes
- Tx: ASA + (if symptomatic) Hydroxyurea +/- (if TIA/CVA/MI/GIB) pheresis
Other platelet dysfunction: increased bleeding time; bleeding from small injuries, epistaxis, menorrhagia
(1) vWF: increased PTT/low-normal VIII corrected with mixing study; Dx: vWF Ag; Tx: pre-dental DDAVP or for active bleed, recombinant factor VIII
(2) Bernard-Soulier: X glycoprotein Ib --> thrombocytopenia
(3) Glanzmann (~Abciximab/Eptifibatide): X gpIIb-IIIa --> normal platelet counts
Coagulation factor disorders and thrombotic disorders
Rule of Thumb:
PeT PiTTbull
- PT extrinsic pathway (VII, X)
- PTT intrinsic pathway (VIII, IX, XI, XII)
*mixing studies correct = deficiency --> present as bleeding into muscle/joint; Tx with DDAVP for mild disease or missing factor for active bleed
*mixing studies don’t correct =
(1) if there is bleeding: presence of factor antibody: Tx with recombinant FVII
(2) if there is no bleeding: antiphospholipid Ab
Coagulation factor deficiencies:
- VII: elevated PT (it’s pretty much the only one that isn’t elevated PTT), presents as ICH, Tx: rfVII
- VIII/Hem A: elevated PTT, bleeding into muscles/joints, no excessive bleed after minor cuts; Tx: DDAVP before dental work, fVIII
- acquired VIII: elevated PTT that doesn’t correct, Tx: rFVII (<--yes, Tx is rf7, NOT 8)
- IX/Hem B: elevated PTT, bleeding into muscles/joints, no excessive bleeding after minor cuts; Tx: fIX
- XI/Rosenthal: elevated PTT in Ashkenazi Jews; Tx: FFP prior to major surgeries
- XII: asymptomatic and totally benign elevated PTT
- XIII: coags look normal, but has severe post-op bleed; Dx: urease clot dissolves; Tx: Qmonthly FFP
- acquired X/AL amyloid: elevated INR with postural hypotension, macroglossia, heart failure, and proteinuria/kidney failure; Dx: serum/urine electrophoresis, free light chain assay, BMB, fat pad aspirate
vs. vWF: increased bleeding time, normal/elevated PTT that corrects with mixing stud
- Dx: vWF Ag, vWF activy assay, VIII, level, subtype multimer study
- Sx: gingival/mucocutaneus bleed, menorrhagia, easy bruising
- Tx: DDAVP prior to dental work, active bleed: rfVIII
Thrombophilia: DVT/PE’s
(1) Antiphospholipid antibody syndrome: anti-beta2glycoprotein I Ab
- blood clots, miscarriage; associated with SLE
- apTT doesn’t correct with mixing study --> Dx: anticardiolipin IgG/IgM ELISA
(2) Factor V Leiden: most common
- Dx (check months after DVT): clotting assay (resistance to Protein C) --> genetic prothrombin G20210A mutation
Porphyria
-morning hematuria, blistering photosensitive rash, abdominal pain, nausea/vomiting, HTN, tachycardia, psychosis, seizures all exacerbated by EtOH, smoking, stress, sulfa drugs
- increased risk of HCC, lymphoma
- Dx: elevated urine uroporphyrinogen (urine turns purple in sunlight) --> check for Hep C and hemochromatosis
- Porphyria cutanea tarda: associated with HIV, Hep C; Tx: phlebotomy to decrease iron stores
Myeloproliferative disorders
Polychythemia vera and other erythrocytosis: JAK2V617F, associated with Budd-Chiari, facial plethora, pruritus with hot baths
- BMB is hypercellular, decreased EPO levels
- Tx: ASA and phlebotomy to Hct <45 +/- Hydrea
- also Tx hyperuricemia with allopurinol, pruritus with antihistamines
Essential thrombocythemia: JAK2, decreased EPO levels; associated with vWF disease (more info under Platelet Disorders above); Tx: ASA + Hydroxyurea +/- pheresis if TIA/CVA/MI/GIB
Agnogenic myeloid metaplasia and myelofibrosis:
- splenomegaly, dacryocytes, giant megakaryocytes/platelets, BM fibrosis
- portal HTN
- Tx: supportive (NOT splenectomy); if <60yo, stem cell transplant
Myelodysplastic syndrome
- cytopenia of 2 cell lines + tear drop cells + nucleated RBCs, elevated MVC
- r/o B12 deficiency (PBS macrocytosis)
- BMB shows ringed sideroblasts, Pseudo Pelger-Huetz cell (looks like 2-lobed PMN or cell wearing blue sunglasses)
- Tx: Azacitidine to keep Plt >100k, Epo, GCSF; if young: stem cell transplant
- 5q-subtype Tx (best prognosis): Thalidomide (AE: rash, peripheral neuropathy), Lenalidomide (AE: less neuropathy, but more decr PMN, thrombocytopenia)
Hematologic malignancies
Acute and chronic leukemias (see Leukocyte Disorders above)
Hodgkin’s disease: B-symptoms, non-tender contiguous nodes with Reed-Sternberg (owl-eye) B-cells, associated with EBV; Dx: full excision of lymph node + pan-CT + PET + BMB if Bsx or stage III/VI; Tx: ABVD + rads if same side of diaphragm --> screen for breast cancer 8 years after XRT or at 40yo
Non-Hodgkin’s lymphoma: multiple nodes with extranodal involvement, B>T cells, associated with autoimmune dz (Sjogrens: parotid MALT), HIV
(1) Indolent:
(a) Follicular: painless swelling in neck, armpit, groin; Tx: watchful waiting, but if symptomatic: XRT if limited, Bendamustine-Rituxan or R-CHOP if outside XRT field
(b) MALT: Tx H.pylori
(2) Aggressive:
(a) Diffuse large B-cell: B-symptoms; Dx: biopsy, Tx: CHOP --> R-CHOP --> XRT
(b) AIDs-associated lymphoma: EBV in CSF --> primary cerebral lymphoma
(c) Burkitt’s lymphoma: African jaw mass/U.S.A. abdominal mass, associated with EBV, increased LDH, starry sky
(3) Cutaneous T-cell (CD4): Sezary/Mycosis Fungoides: plaque --> nodular lesions with cerbriform nuclei (epidermis: Pautrier microabscess)
Plasma cell disorder / Multiple Myeloma:
- “CRAB” hypercalcemia, renal injury, anemia, lytic bone lesions
- >3gM protein, >10% plasma cells in BM, normal ALP, discrepancy between urine protein and urine dipstick (due to inability to detect light chains)
- Dx: BMB, XR>bone survey; serum and urine electrophoresis Q6 months
- Tx:
(1) <75yo: Lenalidomide/Thalidomide + Dexamethasone --> stem cell transplant --> Bortezomib
(2) can’t or >75yo: Melphalan + Prednisone
vs. Smoldering MM: MM without Sx
vs. Plasmacytoma: solitary lytic bone lesion; Dx: tissue Bx; Tx: follow
vs. MGUS: no CRAB, few clonal plasma cells, serum monoclonal protein <3g
*AE of Thalidomide = DVTs
Transfusion medicine
Indications for transfusion: Hb <7 or <10 for acute MI
Complications of transfusion:
(1) ABO/acute hemolytic transfusion: fever, flank pain, tachycardia, hypotension --> stop transfusion
(2) Delayed: elevated bili and LDH, decreased Hb and Haptoglobin, increased retic
(3) Post-transfusion purpura: within 1 week, anti-HPA-1a Ab; Tx: IVIg and watch for transfusion-induced thrombocytopenia with next transfusion
(4) TRALI (ARDs picture with hypotension after transfusion; Tx: vent/supportive fluids) vs TACO (hypertension; Tx: diuretics)
Other
Sickle Cell:
- may present as diffuse pulmonary infiltrates that mimic PE/PNA/appendicitis, but with >2g/dL Hb drop and elevated LDH/retic
- acute chest syndrome --> Tx: exchange transfusion if Hb <10
- associated with pulmonary HTN and increased risk for CVA (BUT DO NOT NEED PLAVIX; instead CVA PPx with monthly 2 unit transfusions)
- Dx: Hb electrophoresis
- chronic Tx with 2 pain crisis/year or h/o ACS: hydroxyurea (but CI in pregnancy and AKI)
*vs Fat embolus (long bone fx): fever, CP, thrombocytopenia, multiorgan failure; BAL shows fat bodies
*vs. Aplastic crisis (Parvovirus/B19): low retic count
Plasma exchange indications:
(1) Guillain Barre (symmetric ascending flaccid paralysis with reduced DTRs)
(2) Myasthenia gravis (ocular-->facial -->proximal muscle weakness that doesn’t fatigue)
(3) TTP (neurologic symptoms with hemolytic anemia and thrombocytopenia)
(4) Goodpasture (anti-GBM nephritis (hematuria, hypertension) with hemoptysis)
(5) Cryoglobulinemia (cold-induced nephritis, low complements, associated with HCV)
*AE of plasma exchange = hypocalcemia from citrate: perioral numbness, tingling, anxiety/vomit; Tx: calcium gluconate
6 notes
·
View notes
Text
Platelet Aggregation Devices Market Size, Growth Opportunities, Trends by Manufacturers, Regions, Application & Forecast to 2027
The global platelet aggregation devices market size is expected to reach USD 1,556.8 million by 2027 according to a new study by Polaris Market Research. The report “Platelet Aggregation Devices Market Share, Size, Trends, Industry Analysis Report, By Product (Systems, Reagents, Consumables and Accessories); By Application (Research Applications, Clinical Applications, Others); By End Use (Standalone Hospitals, Diagnostic Laboratories, Research and Academic Institutes, Blood Banks, and Other End Users); By Regions; Segment Forecast, 2020 –2027” gives a detailed insight into current market dynamics and provides analysis on future market growth.
Platelet aggregation is the biological process where the platelet cells are employed in a process to prevent bleeding through vaso-constriction for rapid clot formation. The whole process is mediated via platelet aggregating factor (PAF). The quantitative and qualitative defects of platelets lead to increased bleeding. The high reactivity of platelets in the patients having anti-platelet therapy results in thromboembolic complications.
Request for a sample copy of this research report @ https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-sample
Platelet function related disorders can be either inherited or acquired. The inherited platelet function disorders include Von Willebrand disease, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Storage pool disease. The acquired platelet dysfunction may be caused by chronic conditions such as kidney failure (uremia), Myelodysplastic syndrome (MDS), Leukemias (chronic myeloid leukemia or CML; acute myeloid leukemia or AML).
Some acquired platelet disorders are temporary because of the decreased function of platelets due to anti-platelet medications, non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, antihistamines and some antibiotics. The platelet function testing is transitioned from diagnostics for heritable diseases to a functional one for platelet functional therapies. The rapid usage of anti-platelet therapy, mainly dual anti-platelet therapy has changed the focus of platelet function testing from diagnostics to therapeutics.
The market is driven by few notable factors such as the recent surge in infectious diseases (COVID-19) requiring rapid serological tests, innovations in platelet aggregation mechanisms, systems and consumables, and worldwide rise in chronic ailments. Specialized tests based on platelet aggregation include light transmission platelet aggregometry on platelet-rich plasma (LTA), impedance whole blood aggregometry (WBA), Lumi-aggregometry and flow cytometry.
Complete Summary with TOC Available @ https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market
Automated haematology analyzers can be used to obtain platelet counts over a wide range of values using optical counting methods like light scatter or fluorescence. Screening tests such as prothrombin time (PT) or activated partial thromboplastin time (aPTT) are more standardized and fully automated.
Number of reagents are available in the market to carry out the platelet function tests. These reagents include collagen, thrombin, ADP, vasopressin, epinephrine and ristocetin. Collagen, ADP were used in routine platelet aggregation studies for the evaluation of qualitative platelet function disorders.
Market participants such as F. Hoffmann La-Roche Ltd., Drucker Diagnostics, Haemonetics Corporation, Sysmex Corporation, Siemens Healthineers, Chrono-log Corporation, Instrumentation Laboratory, Accriva Diagnostics, Matis Medical, Helena Laboratories Corporation, Sienco, Inc., Bio/Data Corporation, Tem Group, WerfenLife, S.A., Laboratory Corporation of America Holdings, Sentinel CH. S.p.A., and Aggredyne, Inc. are some of the key players operating in the concerned market.
Purchase This Report @: https://www.polarismarketresearch.com/checkouts/6581
Polaris Market research has segmented the vascular access devices market report on the basis of product, application, end-use and region
Platelet Aggregation Devices Type Outlook (Revenue – USD Million, 2016 – 2027)
Systems
Reagents
Consumables and Accessories
Platelet Aggregation Devices Application Outlook (Revenue – USD Million, 2016 – 2027)
Research Applications
Clinical Applications
Others
Platelet Aggregation Devices End-Use Outlook (Revenue – USD Million, 2016 – 2027)
Standalone Hospitals
Diagnostic Laboratories
Research and Academic Institutes
Blood Banks
Other End Users
Platelet Aggregation Devices Regional Outlook (Revenue – USD Million, 2016 – 2027)
U.S.
Canada
France
Germany
UK
Italy
Spain
Netherlands
Austria
China
India
Japan
Malaysia
South Korea
Indonesia
Mexico
Brazil
Argentina
UAE
Saudi Arabia
Israel
South Africa
Read More@ https://www.medgadget.com/2020/07/platelet-aggregation-devices-market-size-worth-1556-8-million-by-2027-cagr-20-1-exclusive-study-by-polaris-market-research.html
About Polaris Market Research
Polaris Market Research is a global market research and consulting company. The company specializes in providing exceptional market intelligence and in-depth business research services for our clientele spread across different enterprises.
Contact Us:
Polaris Market Research
Phone: 1–646–568–9980
Email: [email protected]
Web: www.polarismarketresearch.com
#Platelet Aggregation Devices Market#Platelet Aggregation Devices Market share#Platelet Aggregation Devices Market size
0 notes
Video
youtube
Bernard Soulier Syndrome (BSS) vs Glanzmann Thrombasthenia (GT)
0 notes
Link
Natural Cure For Bernard Soulier Syndrome With Herbal Remedies

#bernard soulier syndrome receptor.#bernard soulier syndrome#herbal remedies#ayurvedic doctor#article of the day
1 note
·
View note
Text
Platelet Aggregation Devices Market Size Historical Growth, Analysis, Opportunities and Forecast
The Global Platelet Aggregation Devices Market Size Is Expected To Reach USD 1,556.8 Million by 2027 according to a new study by Polaris Market Research. Platelet aggregation is the biological process where the platelet cells are employed in a process to prevent bleeding through vaso-constriction for rapid clot formation. The whole process is mediated via platelet aggregating factor (PAF). The quantitative and qualitative defects of platelets lead to increased bleeding. The high reactivity of platelets in the patients having anti-platelet therapy results in thromboembolic complications.
Platelet function related disorders can be either inherited or acquired. The inherited platelet function disorders include Von Willebrand disease, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Storage pool disease. The acquired platelet dysfunction may be caused by chronic conditions such as kidney failure (uremia), Myelodysplastic syndrome (MDS), Leukemias (chronic myeloid leukemia or CML; acute myeloid leukemia or AML).
Request A Sample Report at : https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-sample
Some acquired platelet disorders are temporary because of the decreased function of platelets due to anti-platelet medications, non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, antihistamines and some antibiotics. The platelet function testing is transitioned from diagnostics for heritable diseases to a functional one for platelet functional therapies. The rapid usage of anti-platelet therapy, mainly dual anti-platelet therapy has changed the focus of platelet function testing from diagnostics to therapeutics.
The market is driven by few notable factors such as the recent surge in infectious diseases (COVID-19) requiring rapid serological tests, innovations in platelet aggregation mechanisms, systems and consumables, and worldwide rise in chronic ailments. Specialized tests based on platelet aggregation include light transmission platelet aggregometry on platelet-rich plasma (LTA), impedance whole blood aggregometry (WBA), Lumi-aggregometry and flow cytometry.
Automated haematology analyzers can be used to obtain platelet counts over a wide range of values using optical counting methods like light scatter or fluorescence. Screening tests such as prothrombin time (PT) or activated partial thromboplastin time (aPTT) are more standardized and fully automated.
Request for Discount Pricing with Your Specific Research Needs At : https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-discount-pricing
Number of reagents are available in the market to carry out the platelet function tests. These reagents include collagen, thrombin, ADP, vasopressin, epinephrine and ristocetin. Collagen, ADP were used in routine platelet aggregation studies for the evaluation of qualitative platelet function disorders.
Market participants such as F. Hoffmann La-Roche Ltd., Drucker Diagnostics, Haemonetics Corporation, Sysmex Corporation, Siemens Healthineers, Chrono-log Corporation, Instrumentation Laboratory, Accriva Diagnostics, Matis Medical, Helena Laboratories Corporation, Sienco, Inc., Bio/Data Corporation, Tem Group, WerfenLife, S.A., Laboratory Corporation of America Holdings, Sentinel CH. S.p.A., and Aggredyne, Inc. are some of the key players operating in the concerned market.
Have Questions? Or make an Inquiry before buying this report Speak to Our Industry Expert: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/speak-to-analyst
0 notes
Link
The global platelet aggregation devices market size is expected to reach USD 1,556.8 million by 2027 according to a new study by Polaris Market Research. The report “Platelet Aggregation Devices Market Share, Size, Trends, Industry Analysis Report, By Product (Systems, Reagents, Consumables and Accessories); By Application (Research Applications, Clinical Applications, Others); By End Use (Standalone Hospitals, Diagnostic Laboratories, Research and Academic Institutes, Blood Banks, and Other End Users); By Regions; Segment Forecast, 2020 –2027” gives a detailed insight into current market dynamics and provides analysis on future market growth.
Platelet aggregation is the biological process where the platelet cells are employed in a process to prevent bleeding through vaso-constriction for rapid clot formation. The whole process is mediated via platelet aggregating factor (PAF). The quantitative and qualitative defects of platelets lead to increased bleeding. The high reactivity of platelets in the patients having anti-platelet therapy results in thromboembolic complications.
Get Sample Copy of report: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-sample
Platelet function related disorders can be either inherited or acquired. The inherited platelet function disorders include Von Willebrand disease, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Storage pool disease. The acquired platelet dysfunction may be caused by chronic conditions such as kidney failure (uremia), Myelodysplastic syndrome (MDS), Leukemias (chronic myeloid leukemia or CML; acute myeloid leukemia or AML).
Some acquired platelet disorders are temporary because of the decreased function of platelets due to anti-platelet medications, non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, antihistamines and some antibiotics. The platelet function testing is transitioned from diagnostics for heritable diseases to a functional one for platelet functional therapies. The rapid usage of anti-platelet therapy, mainly dual anti-platelet therapy has changed the focus of platelet function testing from diagnostics to therapeutics.
Market participants such as F. Hoffmann La-Roche Ltd., Drucker Diagnostics, Haemonetics Corporation, Sysmex Corporation, Siemens Healthineers, Chrono-log Corporation, Instrumentation Laboratory, Accriva Diagnostics, Matis Medical, Helena Laboratories Corporation, Sienco, Inc., Bio/Data Corporation, Tem Group, WerfenLife, S.A., Laboratory Corporation of America Holdings, Sentinel CH. S.p.A., and Aggredyne, Inc. are some of the key players operating in the concerned market.
Request For Discount: https://www.polarismarketresearch.com/industry-analysis/platelet-aggregation-devices-market/request-for-discount-pricing
About Polaris Market Research
Polaris Market Research is a global market research and consulting company. The company specializes in providing exceptional market intelligence and in-depth business research services for our clientele spread across different enterprises. We at Polaris are obliged to serve our diverse customer base present across the industries of healthcare, technology, semi-conductors and chemicals among various other industries present around the world
Contact us
Polaris Market Research
Phone: 1-646-568-9980
Email: [email protected]
Web: www.polarismarketresearch.com
0 notes