#COVID-19 Vaccines comparison
Text
This chart needs to be shared everywhere. It shows how truly dangerous the COVID shots are.
Drug Adverse Event Comparison (01/01/1996 - 12/29/23):
Ivermectin - 4,297
HCQ - 29,415
Flu Vaccine - 223,663
Dexamethasone - 113,686
Tylenol - 139,025
Remdesivir - 9,478
COVID Vaccines - 1,621,120
Naysayers will say this number is so high because billions of COVID-19 shots were administered. However, Senator Ron Johnson ran a calculation, and he found that the COVID shots were 55 times more lethal (25.1 vs 0.46 deaths per million doses) than the flu vaccines.
Related Stories on @Vigilant_News:
299 notes
·
View notes
Text
This chart needs to be shared everywhere. It shows how truly dangerous the COVID shots are.
Drug Adverse Event Comparison (01/01/1996 - 12/29/23):
Ivermectin - 4,297
HCQ - 29,415
Flu Vaccine - 223,663
Dexamethasone - 113,686
Tylenol - 139,025
Remdesivir - 9,478
COVID Vaccines - 1,621,120
Naysayers will say this number is so high because billions of COVID-19 shots were administered. However, Senator Ron Johnson ran a calculation, and he found that the COVID shots were 55 times more lethal (25.1 vs 0.46 deaths per million doses) than the flu vaccines.
Related Stories on @Vigilant_News
15 notes
·
View notes
Text
United Conservative Leader Danielle Smith apologized Monday after a 2021 video surfaced of her saying she wouldn’t wear a Remembrance Day poppy while comparing those who got the COVID-19 vaccine to followers of Adolf Hitler in Nazi Germany.
Alberta’s election is set for May 29.
“I’ve always remained a friend to the Jewish community, to Israel and to our veterans,” Smith told reporters Monday, deferring further comment to a statement from her campaign office.
In the statement, Smith said while the comment was made during her previous career as a radio host and pundit, any comparisons involving the horrors of the Nazi regime are offside. [...]
Continue Reading.
Note from poster @el-shab-hussein: Why do we Palestinians have to keep catching strays like this had nothing to do with us and now it does lmao. From colonial entity to colonial entity I guess.
Tagging: @politicsofcanada, @abpoli
#cdnpoli#alt right#Alberta#Danielle Smith#reactionary politics#far right#United Conservative Party#Conservatives#coronapolitics#coronavirus vaccine#nazism tw
53 notes
·
View notes
Text
"It has been more than four months since Health Canada approved the first COVID-19 vaccine for children under five, but national uptake has been low.
The latest numbers from the Public Health Agency of Canada show, as of Oct. 9, 6.5 per cent of kids under five have received one dose of vaccine, while one per cent have received two doses.
By comparison, 86.9 per cent of Canadians five and older have received one dose, while 84.2 per cent have received two doses.
"Coverage for COVID vaccination for kids under five is quite strikingly low," said Shannon MacDonald, a nursing professor at the University of Alberta who leads the university's applied immunization research team."
Full article
tagging: @allthecanadianpolitics
90 notes
·
View notes
Text
It is a small study, but a very disturbing one.
We keep being told that injury to the heart from the COVID vaccine is very rare, but a study done in Basel Switzerland indicates that the rate of subclinical myocarditis after the COVID vaccine is hardly rare at all.
In fact, in a study with only 777 participants with a median age of 37--all medical professionals getting the COVID vaccine–the incidence of elevated cardiac enzymes 3 days after injection was pretty substantial, at almost 3%.
The CDC did a study and from that, they claimed the rate was 0.001%, or one out of 100,000.
2.8% is a lot higher than 0.001%. Another 0.3% had “probable myocarditis,” putting the total at over 3%. That is 3000 times higher than the US government claimed.
In this small study, nobody had serious complications, but with a myocarditis complication rate of 3%, you would have to expect that giving out hundreds of millions of doses is a pretty risky proposition.
I think we all knew that already, but this study seems to put the nail in the coffin of “vaccine injuries are super rare” from COVID-19 shots.
Oops. Who could have guessed?
One oddity was that the rate of myocarditis among the participants was heavily weighted toward women, not men. That could be an artifact of the sample, or it could indicate that women are more likely to get a complication, but the complications are more likely to be serious among men.
One reason the researchers posit for the vast difference between their results–which are based upon blood tests looking for cardiac enzymes in all participants–and the commonly asserted claim that vaccine-induced myocarditis is rare is that the only cases that are diagnosed without looking specifically for it are severe.
In other words, most people don’t go to the doctor until there is a serious problem, so many people suffer from myocarditis without ever getting diagnosed.
This suggests that there is a very large group of people who were afflicted but never treated. This in most cases would not be a huge problem, as the inflammation resolves on its own, but in some cases, actual damage to the heart was done without it ever being caught.
Another variable, not mentioned, is that myocarditis complications are more common in young men, and this study skewed both female and middle-aged professionals. Given the cohort studied, one would expect them to be not entirely representative of the population as a whole. They are likely wealthier, healthier, and moderately older than the population as a whole.
In any case, this study sheds quite a light on just how deceptive the CDC, the FDA, and NIAID have been about vaccine safety. And also how intentionally ignorant they have chosen to be. This was not a complicated study to do. The researchers chose a cohort easy to recruit, tested them both before and after vaccination to create a baseline and comparison, and analyzed the data.
Easy peasy. Not even that costly. If you wanted to know the actual numbers of people with heart damage post-vaccine, this was an easy-to-construct and interpret study, and you can get results very quickly.
Why didn’t our public health officials do it then? Why did it take a hospital in Switzerland to come up with the idea and execute it? In 2023, no less.
Being off by a factor of 3000 is more than an oops. It is a very big deal.
11 notes
·
View notes
Text
Known COVID-19 Health Complications
Last Updated September 8, 2023
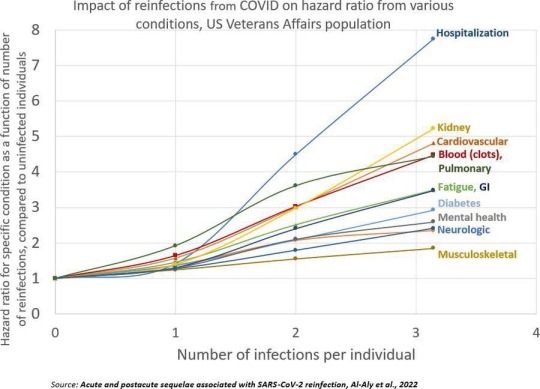
Repeat Infections
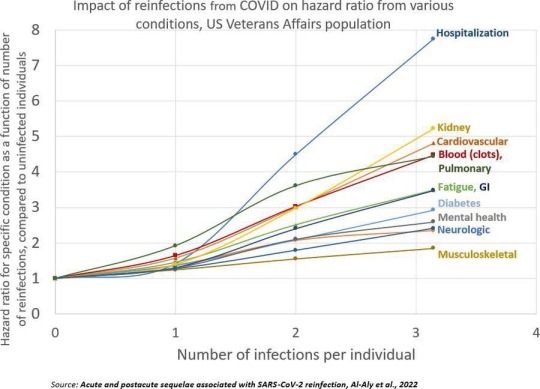
Summary: Repeat infections, even if mild during the acute phase, cause cumulative damage to the body and increase your risk of developing health complications or Long COVID. You should aim to limit the number of times you are infected as much as possible, even if you are not currently high risk (Note: Health complications post-COVID-19 infection can make you high risk) and have been vaccinated.
Published Research
Acute and postacute sequelae associated with SARS-CoV-2 reinfection | Nature Medicine
Bowe, B., Xie, Y, & Al-Aly, Z. (2022).
Articles & Reports
Repeat COVID-19 infections increase risk of organ failure, death – Washington University School of Medicine in St. Louis (wustl.edu)
Sauerwein, K. (2022).
Why Getting COVID-19 Multiple Times Is Risky For Your Health | Time
Park, A. (2022).
Heart & Cardiovascular Damage
Summary: COVID-19 increases your risk of heart failure, heart attacks, strokes, pulmonary embolism, palpitations, arrhythmia, myocarditis, blood clots (thrombosis), etc. post-infection. Inflammation during the acute phase of a COVID-19 infection can damage the heart and blood vessels.
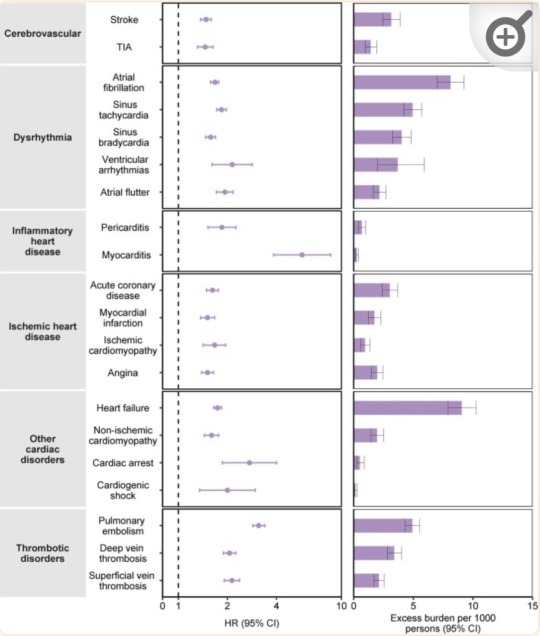
“Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes in participants without any history of cardiovascular outcomes prior to COVID-19 exposure compared to the contemporary control cohort.” (Xie et al., 2022)
Published Research
Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts | Science Translational Medicine
Guarnieri, J. W., Dybas, J. M., ... Wallace, D. C. (2023).
Long-term cardiovascular outcomes of COVID-19 - PMC (nih.gov)
Xie, Y., Xu, E., Bowe, B., & Al-Aly, Z. (2022).
Articles & Reports
Blood Clotting Proteins Might Help Predict Long COVID Brain Fog - Scientific American
Reardon, S. (2023, September 1).
SARS-CoV-2 can damage mitochondrion in heart, other organs, study finds | CIDRAP (umn.edu)
Van Beusekom, M. (2023, August 9).
Your vascular system and COVID | Heart and Stroke Foundation
Heart and Stroke Foundation. (2023).
COVID, heart disease and stroke | Heart and Stroke Foundation
Heart and Stroke Foundation. (2023, April 17).
How does coronavirus affect your heart? - BHF
British Heart Foundation. (2023, March 21).
COVID-19 and Heart Damage: What You Should Know (clevelandclinic.org)
Cleveland Clinic. (2022, May 10).
Heart Problems after COVID-19 | Johns Hopkins Medicine
Post, W. S., & Gilotra, N. A. (2022).
COVID and the Heart: It Spares No One | Johns Hopkins | Bloomberg School of Public Health (jhu.edu)
Desmon, S., & Al-Aly, Z. (2022, March 14).
COVID-19 takes serious toll on heart health—a full year after recovery | Science | AAAS
Wadman, M. (2022, February 9).
Brain & Neurological Damage
Summary: COVID-19 infection increases your risk of developing cognitive impairments, mental health issues, poor memory, early onset dementia, and permanent loss of smell due to brain damage and the atrophy of brain matter. "Brain fog" and problems concentrating are common complaints post-infection that have also been linked to brain damage. Damage to blood vessels due to inflammation during the infection may be responsible for this by restricting oxygen flow to the brain. COVID-19 may also directly infect the brain.
Published Research
Biology | Free Full-Text | Vascular Dysfunctions Contribute to the Long-Term Cognitive Deficits Following COVID-19 (mdpi.com)
Shabani, Z., Liu, J., & Su, H. (2023).
Frontiers | COVCOG 2: Cognitive and Memory Deficits in Long COVID: A Second Publication From the COVID and Cognition Study (frontiersin.org)
Guo, P., Ballesteros, B. A., Yeung, S. P., Liu, R., Saha, A., Curtis, L., Kaser, M., Haggard, M. P., & Cheke, L. G. (2022).
COVID-19 and cognitive impairment: neuroinvasive and blood‒brain barrier dysfunction - PMC (nih.gov)
Chen, Y., Yang, W., Chen, F., & Cui, L. (2022).
Comparison of post-COVID depression and major depressive disorder | medRxiv
Perlis, R. H., Santillana, M., Ognyanova, K., Green, J., Druckman, J., Lazer, D., & Baum, M. A. (2021).
Articles & Reports
Long COVID May Impair Memory, Cognition for Months (healthline.com)
Rossiaky, D. (2022).
COVID Variants Can Affect the Brain in Different Ways - Neuroscience News
(2023).
The hidden long-term cognitive effects of COVID-19 - Harvard Health
Budson, A. E. (2021). Harvard Medical School.
Long Covid: Even mild Covid is linked to damage to the brain months after infection (nbcnews.com)
Ryan, B. (2022). NBC News.
COVID-19 Can Affect the Brain Even Long After an Infection | Time
Ducharme, J. (2023). Time.
Lung Damage
Summary: COVID-19 infections can cause lung damage or scarring, and can trigger pneumonia, bronchitis, ARDS, and sepsis. Additionally, some people experience shortness of breath (dyspnea) and difficulty exercising as a post-acute sequela after infection, or multiple infections.
Published Research
At a crossroads: COVID-19 recovery and the risk of pulmonary vascular disease - PMC (nih.gov)
Cascino, T. M., Desai, A. A., & Kanthi, Y. (2021).
[Pulmonary manifestations in long COVID] - PubMed (nih.gov)
Sommer, N., & Schmeck, B. (2022).
Residual Lung Abnormalities after COVID-19 Hospitalization: Interim Analysis of the UKILD Post-COVID-19 Study - PubMed (nih.gov)
Stewart, I., Jacob, J., George, P. M., Molyneaux, P. L., Porter, J. C., Allen, R. J., Aslani, S., Baillie, J. K., Barratt, S. L., Beirne, P., Bianchi, S. M., Blaikley, J. F., ...Jenkins, G. R. (2023).
Articles & Reports
Even mild cases of COVID-19 may cause long-term lung damage - UPI.com
HealthDay News. (2022). United Press International.
COVID-19 Lung Damage | Johns Hopkins Medicine
Galiatsatos, P. (2022).
Immune System & Autoimmune Diseases
Summary: COVID-19 infection can impair the functioning of your immune system. This means that those who have previously been infected are potentially immunocompromised (higher risk). For some people, the way COVID-19 impairs their immune system results in the onset of autoimmune diseases.
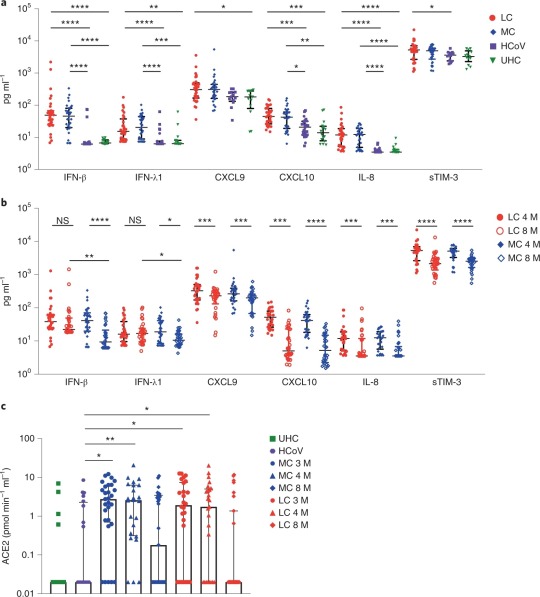
“Elevated levels of proinflammatory cytokines that persist more than 8 months following convalescence.” (Phetsouphanh et al., 2022)
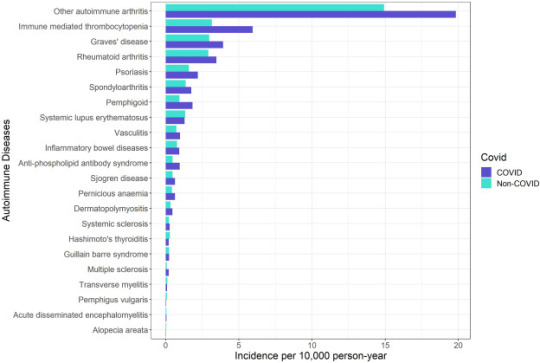
“Crude incidence of each autoimmune disease by COVID-19 and non-COVID groups.” (Peng et al., 2023)
Published Research
Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection | Nature Immunology
Phetsouphanh, C., Darley, D. R., Wilson, D. B., Howe, A., Munier, M. L., Patel, S. K., Juno, J. A., Burrell, L. M., Kent, S. J., Dore, G. J., ... & Matthews, G. V. (2022).
Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection | BMC Medicine | Full Text (biomedcentral.com)
Ryan, F. J., Hope, C. M., Masavuli, M. G., Lynn, M. A., Mekonnen, Z. A., Yeow, A. E. L., Garcia-Valtanen, P., Al-Delfi, Z., Gummow, J., Furguson, C., ... Lynn, D. J. (2022).
Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study - eClinicalMedicine (thelancet.com)
Peng, K., Li, X., Yang, D., Chan, S. C. W., Zhou, J., & Wan, E. Y. F. (2023).
Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection | BMC Medicine | Full Text (biomedcentral.com)
Winheim, E., Rinke, L., Lutz, K., Reischer, A., Leutbecher, A., Wolfram, L., Rausch, L., Kranich, J., Wratil, P. R., Huber, J. E., Baumjohann, D., ... Krug, A. B. (2021).
Articles & Reports
How COVID-19 Changes the Immune System | Time
Park, A. (2023, August 18).
How COVID-19 alters the immune system -- ScienceDaily
ScienceDaily. (2021, October 28).
Impacts of COVID on the immune system (medicalxpress.com)
Herrero, L. (2022, September 19).
COVID-19's impact on the immune system, and how this may affect subsequent infections - ABC News
Smith, B. (2022, December 1).
COVID-19 can derange immune system; survivors have autoimmune diseases (usatoday.com)
Szabo, L. (2021, March 2).
Long COVID & PASC
Summary: Long COVID is an umbrella term that refers to the onset of disabling symptoms/conditions resulting from any of the previously mentioned organ, immune system, and vascular damage sustained during infection. These conditions are also referred to as "post-acute sequelae of COVID-19" (PASC). Vaccination can reduce the damage experienced by decreasing inflammation during an infection, but Long COVID/PASC can affect anyone. This is especially true in the case of multiple infections. Your risk of developing Long COVID, or worse/new symptoms, increases with each additional infection.
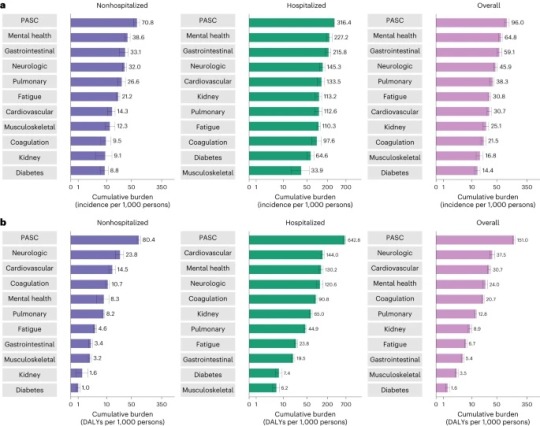
“Cumulative incidence and DALYs of postacute sequelae overall and by organ system at 2 years after infection.” (Bowe et al., 2023)
Published Research
T cell apoptosis characterizes severe Covid-19 disease - PubMed (nih.gov)
André, S., Picard, M., Cezar, R., Roux-Dalvai, F., Alleaume-Butaux, A., Soundaramourty, C., Cruz, A. S., Mendes-Frias, A., Gotti, C., … Estaquier, J. (2022).
SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC) | Nature Immunology
Proal, A. D., VanElzakker, M. B., Aleman, S., Bach, K., Boribong, B. P., Buggert, M., Cherry, S., Chertow, D. S., Davies, H. E., Dupont, C. L., ... Wherry, E. J. (2023).
The immunology of long COVID | Nature Reviews Immunology
Altmann, D. M., Whettlock, E. M., Liu, S., Arachchillage, D. J., & Boyton, R. J. (2023).
Long COVID: major findings, mechanisms and recommendations | Nature Reviews Microbiology
Davis, H. E., McCorkell, L., Vogel, J. M., & Topol, E. J. (2023).
Long COVID prevalence and impact on quality of life 2 years after acute COVID-19 | Scientific Reports (nature.com)
Kim, Y., Bae, S., Chang, H., & Kim, S. (2023).
Postacute sequelae of COVID-19 at 2 years | Nature Medicine
Bowe, B., Xie, Y., & Al-Aly, Z. (2023).
Articles & Reports
Long COVID | NIH COVID-19 Research
National Institutes of Health. (2023, June 8).
Long COVID or Post-COVID Conditions | CDC
Centers for Disease Control and Prevention. (2023, July 20).
The Most Important Question About Long COVID | Harvard Medical School
Pesheva, K. (2023, August 9).
Nearly One in Five American Adults Who Have Had COVID-19 Still Have "Long COVID" (cdc.gov)
Centers for Disease Control and Prevention. (2022, June 22).
2 notes
·
View notes
Link
3 notes
·
View notes