#Different types of Telehealth systems
Text
4 Different Types of Telehealth Services in India | Apollo Telehealth
Apollo Telehealth, one of the prominent telehealth companies in India, offers a range of innovative telemedicine services. These 4 different types of telehealth services are transforming the healthcare landscape, providing convenient and accessible care to patients across the nation.Tele Healthcare
Live Video-Conferencing: Through this telehealth service, patients can connect with healthcare professionals in real-time, enabling virtual consultations, diagnoses, and treatment recommendations, all from the comfort of their homes.
Asynchronous Video (AKA Store-and-Forward): This service allows patients to record their medical history, symptoms, or images and securely share them with healthcare providers. Doctors can review the information at a convenient time, providing accurate diagnoses and appropriate treatment plans.
Remote Patient Monitoring (RPM): Apollo Telehealth employs advanced technologies to monitor patients' vital signs, such as blood pressure, heart rate, and glucose levels, remotely. This continuous monitoring enables timely interventions and proactive management of chronic conditions.
Mobile Health (mHealth): Leveraging the power of mobile devices, this service enables patients to access healthcare resources, receive reminders for medications, track their health parameters, and access educational materials through user-friendly applications.
Conclusion:
By embracing these diverse telehealth services, Apollo Telehealth is at the forefront of revolutionizing telemedicine in India. They empower patients with greater access to quality healthcare, irrespective of their geographical location, thereby enhancing the overall healthcare experience for all.
#tele healthcare#telehealth companies in india#What are the best Telehealth Platforms?#Different types of Telehealth systems#Telemedicine in India#Live Video-Conferencing#Asynchronous Video#Remote Patient Monitoring#Mobile Health
0 notes
Text
State of the UC Union
Unified Communication and Collaboration (UC&C) is a combination of various communication methods and collaboration tools such as virtual whiteboards, real-time audio and video conferencing and enhanced call control capabilities to improve efficiency in the workplace. It provides a collection of easy-to-use solutions that can be implemented in various organizations to ensure that the end user receives a nearly real-time collaboration experience that works efficiently, smoothly and securely.
Video collaboration has been evolved from hardware-based codecs of traditional Polycom and Cisco Systems to more software driven solution of Microsoft Teams, Zooms, Google Meets, WebEx, post the pandemic. A lot of the solutions have now been replaced with simpler easier to deploy solutions for small meeting rooms, mid-size meeting rooms as well as larger boardrooms, meeting rooms, training rooms and large venue spaces such as Auditoriums and event spaces. However, the challenges of designing, executing and implementing the technologies and the user experience still remain. The intend of this whitepaper is to ensuring the reader to make the right decision based on today’s available technology. Video conferencing has become an increasingly important aspect of today’s world, as many organizations are transitioning to hybrid working environments. It has greatly aided in connecting people over a phone call where people can experience real-time video conferencing features while being located in different remote locations which would not be possible with Video conferencing platforms.

Types of Video Conferencing:
Telepresence Video Conferencing System
Integrated Video Conferencing System
Desktop Video Conferencing System
Video Collaboration Platforms:
Zooms
Microsoft Teams
Google Meets
Cisco
WebEX
What are Native and Non- Native Solutions. Why is it important in a Video Collaboration system?
Video conferencing is a live audio-visual connection between two or more remote parties over the internet that simulates a face-to-face meeting in real-time. In the business world, desktop video conferencing is a core component of Unified communications platforms that also include calling and messaging capabilities. Standalone on-premises and cloud-based video conferencing platforms are also available from numerous vendors who support desktop and room-based Video conferencing solutions with the ability to embed them into business applications, such as Telehealth, customer service and distance learning, etc.
The Primary difference between a Native and a Non-Native system is the user experience. Post Work from home and Back to office systems imply that the end users wants a user interface (IPAD, OEM’s touch panel, etc..) to have the same familiar look and feel that they are dialing/ joining directly from their laptop. Native user experiences also allow for a seamless connection to users within the enterprises in terms of a active directory integration as well. These native integrations have to be certified by the certified solution provides (Microsoft Team, Zooms, etc…) as a part of being through the ecosystem.
Though more expensive, native systems offer a more seamless experience to the management. Non-Native systems can be simply a Video collaboration bar in a room with a PC behind the display, essentially the PC is a desktop/ user laptop that allow content sharing as well as dialing/joining into the enterprise (As the main UC Engine). Non-native applications are easy to deploy, lower cost to maintenance as well.
Differences between Native and Non-Native Solutions
Hard Codec Running Native UC Platform Modes UC hardware often runs in “Native Mode,” meaning that the built-in Windows/Mac or Android computer is running a single UC Platform application such as Microsoft Teams or Zoom. The system is “locked in” to that platform. This is a great option if your business is already using a soft client version on employees’ laptops, as you essentially just extend this experience to the meeting room. Employees can then make a Zoom call from their laptops, or a Zoom call from a conference room’s dedicated “Native” platform. They are already familiar with the UI and so the transition to a hardware version feels seamless.
Soft codec Running Native UC Platform Modes
Soft codec systems are more commonly known as cloud or web-based video conferencing software. They’re “soft” as they don’t need codec hardware to work, and “codec” refers to devices or programs that compress and decompress data. It just needs a USB peripheral device such as USB camera, USB microphone and thin client PC in which all the software platforms can be loaded and they can initiate the call using wireless keyboard and mouse.
Unified Communication & Collaboration Tools for Native Interface
Zoom Rooms Zoom Rooms, the Modern Hybrid workspaces for Teams, brings HD video collaboration into any space – in the office, the classroom, or at home – and allows in[1]person and remote participants to interact in real-time. Zoom Rooms are the conference room experience you’ve always wanted, making it simple to start a meeting, book a room, and share content. Bring high-quality video, audio, and web conferencing to any sized room or workspace. Advanced features like Zoom Kiosks (virtual receptionist), voice commands & room controls on your mobile device. Enabling the hybrid workforce with features like Smart Gallery and Workspace Reservation. Google, Office 365 & Exchange calendar integrations support room booking, room status, upcoming meetings list, and more.
Workspace Reservation
Wireless sharing with proximity detection
Scheduling Displays
Digital Signage
Smart collaboration tools to keep projects moving Work from anywhere
Microsoft Teams
Microsoft Teams is an enterprise-ready unified communications (UC) platform. Teams connects people everywhere, on Windows MAC and other operating systems including mobile devices, as part of their everyday productivity experience. Microsoft Teams provides a consistent, single client experience for presence, instant messaging, voice, video and a great meeting experience. Microsoft Teams goes beyond communication. Easily find, share and edit files in real-time using apps like Word, PowerPoint and Excel inside Teams.
Chat: Share your opinion and your personality, send gifs, stickers and emojis in a group chat or in one-to-one messages.
Meet: Microsoft Teams offers real-time video conferencing. Host online meetings from 1:1, teams and live events up to 10,000 people.
Call: Make and receive calls with internal and external groups using Microsoft Teams Calling, Phone System, Calling Plan, or Direct Routing.
Collaborate: Store, share and edit files in real-time using apps like Word, PowerPoint and Excel in Microsoft Teams.
Digital whiteboard camera technology Kaptivo
Collaborate with remote team members with secure whiteboard/Interactive Display live sharing and video conference integrations.
Connect via Video Conference or Web Browser
Share Livestream of Whiteboard
Secure Whiteboard Image Capture
Save Snapshots and Track Changes
Kaptivo Cast
The Kaptivo Cast HDMI converter pairs with your Kaptivo to livestream vibrant, unobstructed whiteboard images to any HDMI capable input including traditional video codecs, displays, projectors, or lecture capture systems.
With the Kaptivo Cast, Kaptivo seamlessly integrates into meeting systems from all leading providers.
Quantum Leap Lite
The Leap Lite for Conference Room with Mounting Bracket is a step forward in conference cameras.
It features the camera and a display bracket mount that enables mounting your camera to the top or bottom of most display screens and monitors.
The lens of the leap lite with a 110-degree field of view that is suitable for most meeting or conference rooms.
No drivers are required to work on Linux, Windows, Android etc., the leap lite is also compatible with virtually all collaborative software platforms. And it connects your computer via USB, which makes it a simple plug[1]and-play video conference solution.
Quantum 4k PTZ camera with Condor Microphone
The advantages of Quantum camera is they provide stable product quality, 4k PTZ Camera from Value HD is the most cost-effective solution to provide effective communication.
With video in 4K Ultra HD and 82 degrees wide-angle lens, you can enjoy a superior resolution for all of your video conferences.
The 12X Optical Zoom is smooth and rapid and it delivers close-ups with superior resolution. With its patented 4K ISP solution, the lens of this PTZ camera can be controlled from a remote location. The software (Skype for business, Microsoft teams etc.) will be loaded in the thin client PC.
Display to be used to show Far end and Near end participants. During this mode Phoenix beamforming microphone with hemispheric pickup pattern in the room will get activated for audio pick up and reinforcement of far end audio shall be done via ceiling speakers.
The Phoenix Microphone is created with the vision of a clutter free conference table, the Condor sits above or below your monitor and with a pick-up range of up to 30 ft almost any conference room can use the Condor.
Conclusion
Enterprises today face a range of options, and we feel the top five takeaways are as follows:
Understand your vision for the Unified Collaboration rollout for your enterprise well in advance. (Spend time planning.)
Do trial runs with different manufacturers and end users to understand what works and what doesn’t across a range of budgets.
Deploy in small batches.
Understand the long-term value of the system as well as the compatibility with other systems that may come along the way that we may feel are going to be more software-driven.
Collect and analyze data around usage patterns using room schedulers, sensors on clouds, and analytics platforms to assist in improving the user experience as well as assisting with remote asset management and remote deployments.
To know more you can always contact Allwave AV on [email protected] or call us on 9372374450.
To view the complete document for State of the UC Union click here.

2 notes
·
View notes
Text
anyways, had therapy today and since there wasn’t a ton going on this week, we kinda went into a brief overview of the abuse i’ve experienced from my immediate family. my therapist was like “wow u really just dove in there” and i just said, well yeah, it’s my life. that was my normal for the longest time. it somewhat still is but thankfully less so.
i also talked about the emdr i’ve done in the past and the memories we focused on. she said it seemed like my previous therapist had just gone right in with me to the most prominent (most abusive) memories from the past. she told me there are generally 3 kinds of emdr; there’s EMD, EMDr, and EMDR. what i did sounds like EMDR, and she thinks EMD or EMDr might be more helpful for me rn.
not that the original emdr i did didn’t work at all but it definitely didn’t do all it could have done. especially with me having tried to hide just how dissociative i am from my previous therapist, and with not letting other parts that were not the host participate in the emdr cuz of a collection of not understanding/hiding system stuff.
so if my psychosis continues to stay under control as it did this week/i don’t have any hallucinations or delusions/paranoia in the next week or two, we’ll be able to talk about these types of emdr more and get started. i’m interested to also see the difference it’ll have doing emdr in person instead of only over telehealth like previously
6 notes
·
View notes
Text
Navigating the EHR Landscape: Choosing the Right Electronic Health Record Platform for Your Needs
Electronic health records (EHRs) have become an essential part of modern healthcare. They offer a secure and centralized platform for managing patient data, improving care coordination, and streamlining administrative tasks. However, with a multitude of electronic health record vendors and electronic health record systems available, selecting the right solution for your organization can be a daunting task.
We'll explore the benefits of EHRs, delve into the different types of EHR systems, and provide insights into selecting the best EHR vendor and electronic health record management strategies.
Benefits of Electronic Health Records
Implementing an electronic health record systems offers numerous advantages for both healthcare providers and patients. Here are some key benefits:
Improved Quality of Care: EHRs facilitate comprehensive patient records, allowing healthcare providers to access a complete medical history, allergies, medications, and treatment plans. This fosters informed decision-making and promotes continuity of care.
Enhanced Efficiency: Electronic health records automate administrative tasks like appointment scheduling, billing, and reporting. This frees up valuable time for providers to focus on patient care.
Streamlined Collaboration: EHRs enable secure sharing of patient information between healthcare providers, leading to improved care coordination and reduced duplication of services.
Heightened Patient Engagement: Patient portals within electronic health record systems allow patients to access their health information, communicate with providers, and manage appointments, promoting a more active role in their healthcare journey.
Types of Electronic Health Record Systems
There are two main categories of EHR systems:
Open EHR Systems: These systems utilize open-source software and offer greater flexibility in customization. However, they may require more IT expertise for setup and maintenance.
Proprietary EHR Systems: These systems are developed and maintained by specific vendors and offer a more user-friendly experience. However, customization options may be limited.
Choosing the Right EHR Vendor
Selecting the right electronic health record vendor is crucial for a successful electronic medical record implementation. Here are some key factors to consider:
Functionality: Ensure the EHR Platform caters to your specific needs. Consider features like appointment scheduling, e-prescribing, telehealth capabilities, and reporting tools.
Scalability: Choose a system that can adapt to your organization's growth and evolving needs.
Interoperability: Verify that the EHR system integrates seamlessly with existing practice management software and other healthcare information systems.
Implementation and Training: Evaluate the vendor's implementation support and training programs to ensure a smooth transition for your staff.
Security and Compliance: Select a vendor with robust security measures to protect sensitive patient data and ensure HIPAA compliance.
Effective EHR Management Strategies
Once you've chosen the right EHR platform, implementing effective management strategies is vital:
User Adoption: Invest in comprehensive training programs to ensure staff are comfortable using the new system.
Data Quality: Establish clear data entry protocols to maintain accurate and up-to-date patient information.
Regular Reviews: Conduct periodic reviews to assess system performance and identify areas for improvement.
How DrCloudEHR Can Help
DrCloudEHR is a comprehensive electronic health record platform designed specifically for behavioral health and integrated care organizations. DrCloudEHR addresses all the criteria outlined above to ensure a successful EHR implementation for your organization. Here's how:
Rich Functionality: DrCloudEHR offers a robust suite of features, including appointment scheduling, e-prescribing, telehealth capabilities, integrated billing, and customizable reporting tools to meet the unique needs of behavioral health providers.
Scalability and Flexibility: DrCloudEHR is a scalable solution that can adapt to the needs of practices of all sizes. Its open API allows for seamless integration with existing systems.
Interoperability: DrCloudEHR prioritizes interoperability and integrates seamlessly with various practice management software and healthcare information systems.
Implementation and Training: DrCloudEHR offers comprehensive implementation support and training programs to ensure a smooth transition for your staff.
Security and Compliance: DrCloudEHR is HIPAA-compliant and employs robust security measures to safeguard sensitive patient data.
Conclusion
Choosing the right electronic health record platform is an investment in your organization's future. By understanding the benefits of electronic healthcare record systems, the different system types, and key selection criteria, you can make an informed decision that enhances patient care, improves workflow efficiency, and fosters a data-driven approach to healthcare delivery. Remember, navigating the EHR landscape requires careful consideration, but the rewards of a well-implemented system, like DrCloudEHR, are significant.
0 notes
Text
Elevate Your Health Coverage: Exploring AARP UnitedHealthcare Medicare Advantage
Introduction:
Medicare Advantage plans have become increasingly popular among seniors seeking comprehensive and personalized healthcare coverage. These plans, offered by various insurers, including UnitedHealthcare, provide an alternative to traditional Medicare by combining hospital and medical coverage into a single plan. In this guide, we will explore the benefits and features of Medicare Advantage plans, with a focus on understanding how AARP UnitedHealthcare Medicare Advantage plans elevate the healthcare experience for seniors.

Understanding Medicare Advantage Plans:
Medicare Advantage plans, also known as Medicare Part C, are private health insurance plans offered by Medicare-approved insurers. These plans are designed to provide all the benefits of Original Medicare (Parts A and B) while often incorporating additional benefits, such as prescription drug coverage (Part D), dental, vision, and hearing benefits, wellness programs, and care management services. Medicare Advantage plans typically operate within provider networks and may require beneficiaries to use network providers for covered services.
Exploring the Benefits of AARP UnitedHealthcare Medicare Advantage:
AARP UnitedHealthcare Medicare Advantage plans offer several advantages that enhance the healthcare experience for seniors:
Comprehensive Coverage: One of the primary benefits of AARP UnitedHealthcare Medicare Advantage plans is their comprehensive coverage. These plans combine hospital, medical, and often prescription drug coverage into a single plan, simplifying the healthcare experience for beneficiaries. With coverage for hospital stays, doctor visits, preventive care, prescription drugs, and additional benefits like dental and vision, AARP UnitedHealthcare Medicare Advantage plans offer comprehensive protection against healthcare expenses.
Additional Benefits and Services: AARP UnitedHealthcare Medicare Advantage plans may include a wide range of additional benefits and services beyond what is covered by Original Medicare. These may include coverage for routine dental exams, cleanings, and dentures, vision exams and eyewear, hearing exams and hearing aids, fitness and wellness programs, telehealth services, and even transportation to medical appointments. By offering these extra benefits, AARP UnitedHealthcare Medicare Advantage plans help seniors maintain their overall health and well-being.
Cost Savings: Medicare Advantage plans often provide cost-saving opportunities for beneficiaries. Many AARP UnitedHealthcare Medicare Advantage plans have competitive premiums, copayments, and out-of-pocket maximums compared to Original Medicare with supplemental coverage. Additionally, by bundling medical and prescription drug coverage, beneficiaries may save money on premiums and out-of-pocket costs compared to purchasing separate Medicare Part D plans. Cost-saving opportunities contribute to the affordability and value of AARP UnitedHealthcare Medicare Advantage plans.
Care Coordination and Support: AARP UnitedHealthcare Medicare Advantage plans may offer care coordination and support services to help beneficiaries navigate the healthcare system and manage their health effectively. These services may include access to care managers or care coordinators who can assist with care transitions, chronic disease management, medication management, and coordination of care between different providers. By providing personalized support and guidance, AARP UnitedHealthcare Medicare Advantage plans help beneficiaries achieve better health outcomes and improve their overall quality of life.
Network Flexibility: While Medicare Advantage plans typically operate within provider networks, AARP UnitedHealthcare Medicare Advantage plans may offer flexibility in choosing healthcare providers. Depending on the plan type, beneficiaries may have the option to see providers both inside and outside the plan's network, although out-of-network services may be subject to higher costs. This network flexibility allows beneficiaries to continue seeing their current healthcare providers or access specialized care, ensuring continuity of care and satisfaction.
Conclusion:
AARP UnitedHealthcare aarp united healthcare medicare advantage offer seniors a comprehensive and personalized approach to healthcare coverage, with benefits and features designed to enhance the healthcare experience and improve overall well-being. With comprehensive coverage, additional benefits and services, cost-saving opportunities, care coordination and support, and network flexibility, AARP UnitedHealthcare Medicare Advantage plans provide seniors with peace of mind and confidence in their healthcare coverage.
In conclusion, understanding the benefits and features of AARP UnitedHealthcare Medicare Advantage plans can help seniors make informed decisions about their healthcare coverage. By choosing a plan that aligns with their individual needs and preferences, seniors can elevate their healthcare experience and enjoy greater health and well-being in their retirement years.
0 notes
Text
Precision Medicine and IoT: Advancements in Personalized Healthcare - Technology Org
New Post has been published on https://thedigitalinsider.com/precision-medicine-and-iot-advancements-in-personalized-healthcare-technology-org/
Precision Medicine and IoT: Advancements in Personalized Healthcare - Technology Org
Precision medicine and technology together have the potential to completely transform healthcare. Using precision medicine techniques, patterns are found in patients with uncommon treatment responses or distinct medical needs. Artificial intelligence and other cutting-edge technologies allow the system to think and learn, develop insights through complex computing and inference, and enhance clinician decision-making.
When combined with smart gadgets like Internet of Things (IoT) medical technology, this enables medical practitioners to individually customize a patient’s course of care. According to recent research, translating this technology integration into ongoing research will help tackle precision medicine’s most challenging problems, particularly those where unique medical issues, when paired with patient symptoms, clinical history, and lifestyle data, will enable personalized diagnosis and prognostication.
Internet of Things – artistic impression. Image credit: geralt via Pixabay, free license
IoT in Personalized Care
Advancements in medical technology have led to astounding developments in patient care. As little as two decades ago, patient treatment involved the sick person traveling to a physician’s office, undergoing rounds of tests and treatment at those locations, staying overnight in clinics to conduct rounds of lengthy testing, and a variety of other activities that were time-consuming and difficult for both the patient and the doctor. Now, thanks to IoT technology in healthcare, patients can undergo some testing, such as heart monitoring and sleep monitoring, at home with devices that connect to the Internet and send data in real-time to their physicians. Some ways in which the Internet of Things helps to personalize healthcare include:
Reducing waiting time by using telehealth and remote services connecting doctors and patients at their locations rather than require time to travel and wait in a doctor’s office.
At-home monitoring devices are now used for diagnosing disorders such as sleep apnea.
Using technology such as Near Field Communication (NFC) and Radio Frequency
Identification (RFID) technology to allow medical monitoring devices to interact with smartphones and mobile devices, sending alerts to the patient, such as a low blood sugar alert.
Cloud computing allows for apps such as MyChart, which allow patients to communicate via message with their doctors, view and share test results and medication lists with various providers.
Making use of IoT in healthcare through smart devices such as the Apple Watch for fall detection, medical alert monitoring, medication reminders, summoning emergency services, and heart rhythm monitoring.
IoT in Precision Medicine
Precision medicine, as defined by the Precision Medicine Initiative, is “an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person.” With this method, medical professionals and researchers will be able to more precisely forecast which preventative and treatment plans will be most effective for a certain disease in which populations in contrast to a one-size-fits-all approach ignores individual differences. Although it is a new term, it is not a new concept. For example, considering one of several personalized medicine examples, once medical providers realized that humans had several different blood types, treatment for blood transfusions was catered to the type of care a person with a particular blood type needed. Consider the following precision medicine examples:
Integrating artificial intelligence (A.I.) with machine learning models to aid in patient diagnosis, utilizing data from medical smart devices as it is collected.
Expand telemedicine, which enables patients to access timely healthcare remotely.
Wearable technology, such as smart watches with integrated health monitoring features that monitor chronic conditions and scan for any developing conditions, allows for early detection.
Improved patient care in medical facilities through IoT devices in hospitals and clinics that allow for easier and faster check-in, and assist in ongoing care.
Genetic Testing, Treatment and IoT
Genetic treatment, or cell-based therapy, has a wide variety of applications when paired with IoT-enabled hardware. With data collected from connected technological devices, physicians can monitor certain types of cancer developments, implement treatment through personalized application devices such as pumps or implants, or even enhance or suppress various bodily functions.
Genetic testing now allows medical providers to get a better idea of who might be most likely to develop certain chronic conditions, such as diabetes and high blood pressure, which then allows for precise and targeted monitoring of the individual through smart medical devices.
Remote Patient Monitoring
Medical monitoring is perhaps one of the most useful and powerful applications of IoT solutions for healthcare. As medical devices become smaller and more easily wearable, individuals can then make use of devices such as smartwatches to monitor their ongoing health and make note of any changes, many of which are often subtle and unnoticed in daily life, to determine worrisome patterns over time. Apps such as Apple’s Health app show trends over time collected by devices such as the Apple Watch, which continuously monitors heart rate, breathing, time spent sleeping, and a whole host of other useful features.
These insights give doctors much-needed information to tailor their treatment to the patient’s individual condition. In some cases, devices like the Apple Watch can take a single lead EKG reading to check for atrial fibrillation, which can be exported to a PDF and uploaded via MyChart to a cardiologist, who can then decide if a patient needs further testing and monitoring from dedicated medical devices.
To Recap
As we can see, the IoT has great potential in precision healthcare, as the data collected from these devices allows physicians to offer personalized healthcare solutions and greater flexibility for personalization in healthcare. As technology becomes more powerful, perhaps even utilizing A.I. in diagnostics, we can easily see a future in which, like in the television series Star Trek: Voyager, an A.I. holographic doctor who diagnoses and treats conditions (under the direction of a human doctor) gives patients the opportunity for more frequent and personalized medical care at a moment’s notice.
#alerts#app#apple#Apple Watch#applications#approach#apps#artificial#Artificial Intelligence#atrial fibrillation#blood#blood pressure#blood sugar#blood type#Cancer#cell#Cloud#cloud computing#communication#computing#course#cutting#data#detection#Developments#devices#diabetes#diagnostics#direction#Disease
0 notes
Text
Types of Healthcare Software creating a difference in 2024
The emergence of digital transformation technologies has caused a significant impact on various industries worldwide, leading to a nationwide change. The healthcare industry is one of the sectors that has been affected by this change. Interestingly, digital transformation has not only disrupted but also provided a significant impetus to the healthcare sector, positively influencing the different types of healthcare software and the medical software industry. This surge is reflected in the projection that the global Healthcare IT market size is expected to reach USD 662 billion by 2026.
Furthermore, the obstacles that hindered the acceptance of digital solutions, such as skepticism towards digital technologies, are currently decreasing. This shift in perspective creates a foundation for exploring the profound impact of software solutions for healthcare, revealing its capacity to take medical businesses to unprecedented levels.
15 Popular Types Of Healthcare Software On The Rise
A multitude of healthcare management software has been created with the explicit goal of refining specific processes within the healthcare sector. These software used in healthcare industry address various requirements, encircling solutions oriented toward patients, clinical management, prognostics, and research initiatives.
In this section, we will intricately explore the top 15 types of software solutions for healthcare, shedding light on their potential benefits and contributions to the industry.
EHR Software
Medical Database Software
Telemedicine Software
Telehealth Software
Medical Equipment Management Software
Hospital Management Software
Medical Diagnosis Software
Health Tracking Apps
Medical Imaging Software
Personal Health Record Software
Healthcare Billing Software
E-prescribing Software
Remote Patient Monitoring Software
Medical Research Software
Booking Software (For Scheduling Appointments)
1. EHR Software
EHR software stands out as one of the predominant, if not the singularly most popular, types of software extensively utilized by hospitals and clinics. Its functionality bears resemblance to a CRM system, albeit tailored to the intricacies of the medical industry.
Moreover, as per the studies, the global electronic health records market size was found at USD 28.1 billion in 2022 and is estimated to grow at a CAGR of 4.1% from 2023 to 2030.
Functioning as an information repository, EHR software compiles a comprehensive record of patients, encompassing details such as prescribed medications, physicians' recommendations, and the historical record of procedures they have undergone. Additionally, a distinct portal is often integrated for patients, granting them access to their consultation history, medical records, and prescription details.
The EHR software encompasses two prominent types:
Electronic Patient Record software (EPR): Internally employed by hospitals, EPR software serves as a repository for storing and managing patient information.
Electronic Medical Record software (EMR): Specifically tailored for recording data such as medication types and dosages, details of past and planned medical procedures, and information concerning the patient's recovery trajectory.
2. Medical Database Software
In contrast to Electronic Health Record (EHR) software, medical database software focuses on organizing information based on diseases rather than individual patient profiles. This specialized software serves a dual purpose for healthcare professionals, particularly doctors, in two crucial aspects:
Enhancing Treatment Decision-Making: By cross-referencing a patient's case with similar instances stored in the database, doctors can make more informed treatment decisions.
Facilitating Continuous Medical Education: Medical database software allows practitioners to expand their knowledge by delving into the clinical cases associated with a specific disease.
All in all, this tailored healthcare management software provides a valuable resource for medical professionals, fostering better-informed treatment strategies and supporting continuous learning within their respective specialties.
3. Telemedicine Software
The growth of the telemedicine market is estimated that the number will reach an astonishing $455.3 billion by 2030. But why is such exponential growth expected?
Well, the success of this platform is rooted in its unparalleled convenience for both doctors and patients.
By transforming healthcare delivery, telemedicine software enables seamless online consultations for healthcare professionals and patients, accessible through web browsers or mobile apps. Some platforms go beyond video conferencing, integrating features like e-prescriptions and a comprehensive billing module to enhance the overall telehealth experience.
4. Telehealth Software
The telehealth sector is projected to reach a value of $155.1 billion by 2027, experiencing an annual growth rate of 15.1%.
Through the use of communication technology, telehealth software enables healthcare professionals to provide medical services, guidance, mentoring, and health information remotely. Unlike telemedicine software, which primarily focuses on clinical services, telehealth software encompasses a wider range of medical support.
Healthcare practitioners can employ this type of medical software to observe a patient's recovery after hospital discharge, engage and counsel patients online regarding preventive care topics, or deliver virtual training sessions to medical staff.
5. Medical Equipment Management Software
The Medical Equipment Management Software market is anticipated to grow at a CAGR of 9.9% by 2028. Undoubtedly, it is driven by increasing demand for efficient equipment maintenance, regulatory compliance requirements, and the integration of advanced technologies in healthcare facilities.
The primary objective of this software is to streamline the maintenance of medical equipment. It allows healthcare professionals to automate tedious manual tasks, such as tracking inventory of various expendable items, thereby freeing up their time to focus on more critical tasks.
Additionally, this software for healthcare ensures proper scheduling of routine maintenance, which is crucial for the smooth functioning of hospital infrastructure. Typically, medical equipment management software is a component of comprehensive hospital management software packages.
6. Hospital Management Software
Hospital management software plays an important role in streamlining the daily operations of healthcare facilities. These types of software used by hospitals are designed to automate various aspects, including accounting, medical billing, claims processing, outpatient management, inventory control, and more.
In addition to these functionalities, hospital management software for healthcare often seamlessly integrates with Electronic Health Record (EHR) systems. This integration enhances the efficiency of healthcare administration by facilitating the concurrent management of patient records.
The collaborative synergy between hospital management software and EHR systems contributes to a comprehensive and cohesive approach to optimizing healthcare processes within the hospital environment.
7. Medical Diagnosis Software
The term ‘medical diagnosis software’ encompasses applications designed for both patients and physicians, proving to be invaluable.
Physician-oriented medical diagnosis software facilitates collaborative diagnosis efforts among doctors by enabling the sharing of anonymized patient records. In certain instances, artificial intelligence aids this process by collecting data and proposing potential diagnoses.
On the patient side, medical diagnosis apps help individuals input their symptoms, providing insights into whether medical action, such as scheduling a healthcare professional appointment, is necessary. This has proven instrumental in alleviating the workload of healthcare workers amidst the challenges posed by the pandemic.
8. Health Tracking Apps
The Global Health Tracking Apps market is projected to reach US$ 77,489.3 million by the end of 2033.
While still not classified as ‘professional’ medical software, these applications serve as a supplementary repository of health-related information. Healthcare apps commonly fall into three main categories: fitness, diet, and overall well-being, often combining features from each.
Backed by wearable technology, these apps can gather more precise health data, including metrics such as pulse rate, sleep quality, and even function as thermometers or glucometers.
9. Medical Imaging Software
Medical imaging software in healthcare industry has emerged as a revolutionary tool, facilitating the visualization and interpretation of medical images to aid in diagnosis, treatment planning, and monitoring of patients. From radiology information systems (RIS) to picture archiving and communication systems (PACS), and advanced 3D imaging tools, this medical software includes a diverse range of applications.
As of the latest statistics, the global medical imaging software market is thriving, with a significant growth trajectory. According to a report by Allied Market Research, the medical imaging software market was valued at USD 3.94 billion in 2020 and is projected to reach $68.8 Billion by 2030.
This robust growth underscores the increasing demand for innovative medical imaging solutions to enhance diagnostic accuracy and improve patient care.
10. Personal Health Record Software
In contrast to health tracking applications geared towards promoting a healthy lifestyle, Personal Health Record (PHR) software in healthcare industry serves a unique purpose by concentrating on disease monitoring. Operating as digital medical diaries, PHR software can be stored on the patient's device or seamlessly integrated into the healthcare provider's software.
Anticipated to witness substantial growth, the market size of Personal Health Records (PHR) Software is projected to increase from USD 9.25 million in 2023 to USD 14.71 million by 2028.
The expected expansion of this type of software used by hospitals is indicative of the rising demand for digital health solutions and the increasing recognition of the importance of comprehensive health records.
These applications not only document health data but also play a crucial role in aiding patients throughout their recovery process. Additionally, they function as an alert system, promptly notifying medical staff of emerging symptoms that may indicate a deteriorating health condition.
11. Healthcare Billing Software
Often referred to as medical billing software, this application automates the billing procedures within the healthcare industry. Its primary function is streamlining the billing process for patients, their insurance providers, and other relevant stakeholders.
Through the utilization of billing software, medical expenses for all patients can be promptly accessed and efficiently organized, contributing to enhanced financial management within the healthcare facility.
Notably, the global Hospital Billing Software market size, valued at USD 454.82 million in 2022, is expected to witness significant growth at a CAGR of 11.86% during the forecast period. Projections indicate that it will reach USD 891.26 million by 2028, underscoring the increasing importance and adoption of such hospital software systems.
While these systems are now commonly integrated into broader hospital and practice management systems, they still maintain their relevance as standalone solutions. Therefore, this technology not only improves overall efficiency but also plays a vital role in maintaining the fiscal health of healthcare institutions.
12. E-prescribing Software
Gradually and consistently, the shift from traditional paper prescriptions to digital formats is gaining momentum. The primary driver behind this transition is the convenience offered in modifying or extending prescriptions with just a few clicks.
E-prescriptions deliver benefits to both patients and doctors, as e-prescribing software significantly streamlines the prescription process. This type of medical business software enables quick and efficient granting, renewal, or suspension of prescriptions, reducing the time spent on administrative tasks.
With the efficiency and convenience it provides, the day is not distant when e-prescribing will likely become the standard across the global healthcare sector. As of the most recent data, the E-prescribing Market size is projected to witness substantial growth, with expectations to rise from USD 2.73 billion in 2023 to a remarkable USD 8.07 billion by 2028. This statistic highlights the increasing adoption and significance of e-prescribing in modern healthcare practices.
13. Remote Patient Monitoring Software
Remote Patient Monitoring (RPM) has transformed the healthcare landscape by enabling the collection of patient data beyond the confines of conventional healthcare settings like clinics and hospitals. These state-of-the-art hospital software systems not only enrich the depth of available patient health information but also facilitate remote diagnoses based on the collected data.
The spectrum of RPM technology comprises various devices, including heart rate and blood pressure monitors, wearable ECG monitors, and meters for measuring glucose and blood oxygen levels. With its capability for real-time monitoring and alerting healthcare professionals or clinics to any detected abnormalities, remote patient monitoring software is delivering high-quality healthcare.
According to Alltheresearch, the global remote patient monitoring market was valued at $975.0 million in 2020, and it is expected to reach $3,244.9 million by 2027, highlighting the considerable growth and significance of RPM in reshaping healthcare practices worldwide.
14. Medical Research Software
Each healthcare institution continually accumulates distinctive medical experiences rooted in unprecedented cases, recognizing the uniqueness of each patient, even when symptoms may seem similar. The purpose of medical research software is to disseminate such valuable experiences. Similar to other applied sciences, healthcare perpetually engages in research to educate medical students and elevate the qualifications of doctors.
Despite being among the most specialized programming products in the digital era, the significance of medical research software cannot be emphasized
enough. In numerous instances, precise diagnosis and, consequently, suitable patient treatment hinge on the functionality of medical research software.
15. Booking Software (For Scheduling Appointments)
Booking software is essential for hospitals, clinics, and medical practices to efficiently handle their appointment systems online. Typically, this software includes a patient panel, allowing individuals to easily schedule appointments through an app or website.
Moreover, it often comes equipped with an email notification system and automatic reminders. These features enhance communication between doctors and patients by ensuring both parties receive timely updates about upcoming appointments, contributing to a smoother healthcare experience.
As the demand for effective appointment management rises, the global appointment scheduling software market is expected to reach a substantial $546.31 million by 2026, highlighting the growing importance of such software in optimizing healthcare appointment processes globally.
How can GML Soft Labs help you build custom medical software solutions?
In the healthcare sector, time holds paramount importance. Each day, healthcare professionals, including doctors, grapple with the necessity of promptly addressing illnesses and emergency cases, recognizing the critical nature of swift and effective responses.
However, you can witness the future of the healthcare industry through the comprehensive healthcare software development services offered by GML Soft Labs, a leading provider of tailored projects on healthcare software.
As adept medical software providers, we stand ready to create customized healthcare software solutions, whether it involves developing applications of varying complexities or advancing existing healthcare platforms. Our proficient team is dedicated to delivering top-notch healthcare management software, empowering our clients to establish market leadership, elevate healthcare standards, improve patient satisfaction, and streamline internal workflows.
Key Takeaways
Global Healthcare IT Market Growth: Projections indicate that the global Healthcare IT market is expected to grow to USD 662 billion by 2026, reflecting the industry's increasing reliance on digital solutions.
Digital Acceptance: Skepticism towards digital technologies in healthcare is on the decline, creating a foundation for the profound impact of software solutions and their capacity to elevate medical businesses.
Top 15 Healthcare Software Types: Navigating through various types of healthcare software, including EHR, Medical Database, Telemedicine, Telehealth, Medical Equipment Management, Hospital Management, Medical Diagnosis, Health Tracking, Medical Imaging, Personal Health Record, Healthcare Billing, E-prescribing, Remote Patient Monitoring, and Medical Research Software.
Market Growth Statistics: Keep abreast of market growth statistics, such as the global electronic health records market size reaching USD 28.1 billion in 2022, the telemedicine market projected to reach $455.3 billion by 2030, and the medical imaging software market expected to reach $68.8 billion by 2030.
Rising Importance of EHR: Electronic Health Record (EHR) software, valued at USD 28.1 billion in 2022, plays a crucial role in compiling comprehensive patient records and improving healthcare efficiency.
Digital Transformation Benefits: Healthcare software is driving a digital transformation, leading to more efficient information management, enhanced patient care coordination, improved accessibility, data-driven decision-making, streamlined administrative processes, remote healthcare access, proactive health management, increased patient engagement, and operational excellence.
Future Trends: Anticipate future trends in healthcare software adoption, including the continued growth of EHR, telehealth, medical imaging, and emerging technologies contributing to the industry's digital evolution.
Conclusion
GML Soft Labs stands out as the top healthcare software development company in Chennai, thanks to its unwavering commitment to innovation, quality, and customer satisfaction. By leveraging cutting-edge technologies and industry best practices, GML Soft Labs continues to redefine the standards of excellence in healthcare software development, empowering organizations to deliver superior patient care and achieve operational excellence.
FAQs
What are the key benefits of using healthcare software? Healthcare software offers numerous benefits, including improved patient care, enhanced efficiency, streamlined workflows, and better decision-making through data analytics.
How can healthcare organizations overcome implementation challenges? Healthcare organizations can overcome implementation challenges by investing in robust training programs, fostering a culture of change management, and partnering with experienced vendors for support.
What role does data security play in healthcare software? Data security is critical in healthcare software to protect patient privacy, prevent unauthorized access, and comply with regulatory requirements such as HIPAA.
How are emerging technologies like AI and blockchain transforming healthcare software? Emerging technologies like AI and blockchain are revolutionizing healthcare software by enabling predictive analytics, enhancing interoperability, and ensuring the integrity and security of healthcare data.
What can we expect from the future of healthcare software? The future of healthcare software is expected to be characterized by increased personalization, interoperability, and accessibility, driven by advancements in AI, IoT, telemedicine, and other cutting-edge technologies.
#Software Development company in Chennai#Software development Company in India#Healthcare software development#Healthcare software development in Chennai#Software development company in India#Medical database software Development#EHR Software development
0 notes
Text
Precision Healthcare: The Promise of Advanced Medical Devices
Advancements in Medical Device Technology
One of the most dramatic changes in modern medicine has been the advancement of medical device technology. What were once highly invasive procedures requiring long hospital stays can now be done on an outpatient basis or even in a doctor's office. This is due to innovations in areas like minimally invasive surgery, implantable devices, digital health and more. Minimally invasive procedures allow doctors to perform surgeries through small incisions or natural openings instead of large incisions, resulting in less pain and scarring for patients. Implantable devices like pacemakers, defibrillators and implanted insulin pumps have given people more independence by monitoring conditions internally and delivering treatment when needed. The growth of digital health has connected patients to their care team remotely through technologies like remote patient monitoring devices and telehealth appointments. These advancements are improving patient outcomes and quality of life. In this article, we will explore the various types of medical devices, their applications and the growing medical devices market worldwide.
Impact of Medical Devices on Various Therapeutic Areas
Medical devices are making a difference across many therapeutic areas. In cardiology, devices like stents, catheters and valve replacements are revolutionizing treatments for conditions like heart attacks and heart valve diseases. Orthopedic devices like joint replacements, plates and screws are allowing millions to regain mobility by repairing injuries or alleviating pain from arthritis. Diagnostic imaging equipment like MRI and CT machines provide clearer views of internal structures that help physicians detect diseases earlier. In neurology, devices are helping restore movement disorders through deep brain stimulation and repairing injuries to the brain and spinal cord. Other areas benefiting include oncology with radiation therapy machines, urology with lithotripsy devices, and general surgery with surgical tools and endoscopes. The development of innovative devices is a major factor driving improvements in patient care for many conditions.
Challenges in Medical Device Design and Development
While medical devices offer life-changing benefits, their design and development also present unique technical and regulatory challenges. Safety is the top priority, as these technologies are used for invasive procedures or implanted in the body. Extensive testing and clinical trials are required to confirm a device will function as intended without serious adverse effects. Materials must be biocompatible for implants that will remain in the body long-term. Miniaturization allows for less invasive procedures but increases engineering complexity. Regulatory oversight from the Food and Drug Administration ensures strict standards are met before a device can be marketed in the U.S.
The Role of Startups and Collaboration
While large medical device companies have robust research programs, smaller startups are helping push innovation forward through novel ideas and business models. With lower overhead than established firms, startups can take more risks on disruptive concepts in areas like regenerative medicine, digital biomarkers and 3D printing of implants. This entrepreneurial activity is supported through public and private funding sources dedicated to medical technology development.
Impact on Healthcare Systems and Economics
As device technologies improve clinical outcomes and expand treatment options, they in turn impact healthcare economics and delivery models. More procedures can be done inoutpatient settings at lower cost compared to surgery requiring long hospital stays. Remote monitoring devices help manage chronic diseases better to reduce hospitalizations. Targeted interventions deliver therapy precisely as needed to minimize unnecessary treatment. These efficiencies help control rising costs while enhancing patient-centered care. Systems are shifting reimbursement to reward this value-driven approach rather than purely volume of services. Telehealth is expanding access to specialty care for rural populations through connected devices. While upfront investment is high for innovative devices, they offer the potential for long-term savings through healthcare delivery transformation. Ongoing progress in this field has massive benefits not only for individuals but also for the sustainability of whole healthcare systems globally.
Market Outlook
The global medical devices market is large and growing steadily driven by aging populations, rising incomes, increased access to healthcare and technological advancements. North America currently leads as the largest regional market owing to supportive regulatory framework, high healthcare spending and presence of major players. However, the emerging markets of Asia Pacific and Latin America are witnessing the fastest growth spurred by growing investments, awareness and demand for quality care. While the COVID-19 pandemic caused disruptions in 2020, the long term outlook remains positive as medical devices address both communicable and chronic diseases worldwide. Continuous R&D will fuel new product development and keep driving the industry towards improved outcomes.
0 notes
Text
Behavioral Health Software Market in Industry : Technology, Applications, Growth and Status 2023 – 2030

The global behavioral health software market is on the cusp of a transformative era, projected to reach USD 10.13 billion by 2030. This signifies a significant leap from its 2022 valuation of USD 2.60 billion, with a robust Compound Annual Growth Rate (CAGR) of 18.5% anticipated over the forecast period (2023-2030), according to a recent market analysis.
Driving Forces Behind the Behavioral Health Software Boom:
Several key factors are propelling the behavioral health software market to new heights:
Rising Demand for Mental Health Services: Mental health awareness and the growing number of individuals seeking help are driving the demand for efficient and accessible mental healthcare solutions.
Improved Efficiency and Streamlined Workflows: Behavioral health software streamlines administrative tasks, appointment scheduling, clinical documentation, and communication, allowing providers to dedicate more time to patient care.
Enhanced Patient Engagement and Care Coordination: Software solutions can facilitate patient engagement through self-assessment tools, medication reminders, and secure communication channels. Additionally, they can improve care coordination between providers and other healthcare professionals.
Data-Driven Insights for Better Outcomes: Behavioral health software allows for data collection and analysis, enabling providers to track patient progress and make data-driven decisions for improved treatment outcomes.
Get Free PDF Sample Copy of Report @ https://www.snsinsider.com/sample-request/1827
A Deep Dive into the Market Landscape:
The press release can be enhanced by incorporating a section on market segmentation, providing a more comprehensive picture:
Functionality Type: The market is segmented by the specific functionalities offered by the software, including:
Clinical Functionality: Tools for diagnosis, treatment planning, progress notes, and outcome tracking.
Administrative Functionality: Features for patient scheduling, appointment reminders, billing, and claims management.
Financial Functionality: Solutions for revenue cycle management, insurance verification, and reporting.
Delivery Method: Software solutions can be delivered through different models:
Subscription Model: Provides access to the software for a recurring fee.
Ownership Model: Involves a one-time purchase of the software license.
Software Type: Behavioral health software can be:
Standalone: Designed for specific functionalities (e.g., electronic health records for behavioral health).
Integrated: Works seamlessly with existing healthcare IT systems.
End Users: Several stakeholders benefit from behavioral health software solutions:
Payers (Insurance Companies): Utilize software for claims processing, fraud detection, and care management programs.
Providers (Therapists, Counselors, Psychiatrists): Leverage software to improve clinical workflows and patient care delivery.
Patients: Can utilize patient portals for appointment scheduling, medication management, and communication with providers.
A Global Phenomenon:
A section on the geographic landscape can be included to highlight regional trends:
The report explores the behavioral health software market across different regions, providing insights for geographically focused strategies.
Looking Ahead:
The future of the behavioral health software market is promising, with continued growth anticipated. Increasing government initiatives promoting mental health awareness, rising adoption of telehealth for behavioral health services, and continuous software advancements will further accelerate market expansion.
#Behavioral Health Software Market#Global Behavioral Health Software Market#Behavioral Health Software Market Size#Behavioral Health Software Market Share#Behavioral Health Software Market Trends#Behavioral Health Software Market Growth#Behavioral Health Software Market Demand#Behavioral Health Software Market Segmentation#Behavioral Health Software Market Analysis#Behavioral Health Software Industry Analysis
0 notes
Photo
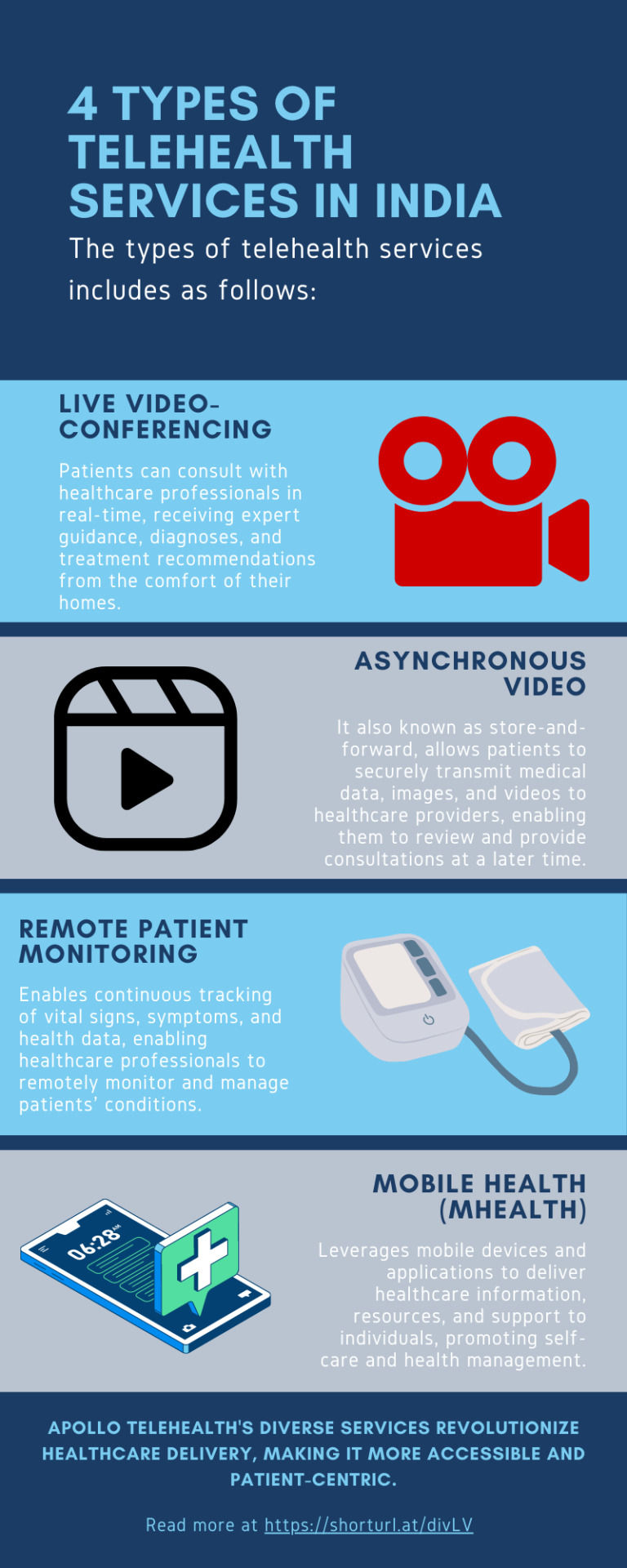
4 Types of Telehealth Services in India
Apollo Telehealth in India offers a range of innovative telehealth services to enhance healthcare accessibility and convenience. The types of telehealth services includes:
1. Live Video-Conferencing: Patients can consult with healthcare professionals in real-time, receiving expert guidance, diagnoses, and treatment recommendations from the comfort of their homes.
2. Asynchronous Video: It also known as store-and-forward, allows patients to securely transmit medical data, images, and videos to healthcare providers, enabling them to review and provide consultations at a later time.
3. Remote Patient Monitoring: Enables continuous tracking of vital signs, symptoms, and health data, enabling healthcare professionals to remotely monitor and manage patients' conditions.
4. Mobile Health (mHealth): Leverages mobile devices and applications to deliver healthcare information, resources, and support to individuals, promoting self-care and health management.
Apollo Telehealth's diverse services revolutionize healthcare delivery, making it more accessible and patient-centric.
#tele healthcare#telehealth services#telehealth companies in india#telehealth in india#telehealth services in india#remote patient monitoring#mobile health#remote healthcare#different types of telehealth systems#what are the best telehealth platforms#types of telehealth platforms#different types of telehealth services#what is remote patient monitoring
0 notes
Text
Telescribing Explained

Telemedicine has revolutionized the healthcare industry by providing convenient and accessible medical care to patients remotely. However, delivering care through telemedicine can still present challenges for healthcare providers, including documentation and medical charting. This is where telescribing comes in. Telescribing, or remote medical scribing, allows healthcare providers to receive real-time documentation support from a trained medical scribe located off-site. This blog will explore telescribing and how it can benefit healthcare providers and their patients.
What Is Telescribing?
Telescribing, also known as remote scribing, is a new healthcare innovation changing how doctors document patient encounters. Telescribing involves a remote medical scribe who listens on a telehealth call or video visit and documents the physician's notes in real-time. The remote scribe is typically located offsite, working from a secure location and using a secure internet connection to access the electronic medical record (EMR) system. This new way of documentation is becoming increasingly popular as healthcare providers look for ways to improve efficiency, reduce the documentation burden on physicians, and improve patient care. In this article, we will dive deeper into the world of telescribing and explore its benefits, challenges, and potential for the future.
Telescribing vs. Traditional Scribing
Telescribing is a form of medical scribing that takes place remotely. While traditional scribes work directly with physicians in-person, telescribing is done through telecommunication technology, allowing scribes to work remotely while still interacting with the physician in real time. In this section, we will discuss some of the key differences between telescribing and traditional scribing.
Location: The most obvious difference between telescribing and traditional scribing is the location of the scribe. Traditional scribes are physically present in the physician's office or at the patient's bedside, while telescribes work remotely. Telescribing allows scribes to work from anywhere, which can be particularly useful for practices in rural areas or have difficulty recruiting local talent.
Technology: Telescribing relies heavily on technology to facilitate communication between the scribe and the physician. The scribe and physician may use teleconferencing software, chat platforms, or other collaboration tools to communicate during the patient encounter. Traditional scribes, on the other hand, rely on face-to-face communication and often take notes on paper.
Training: Traditional and telescribing require training, but the nature of the training may differ. Traditional scribes typically receive on-the-job training, working directly with physicians to learn the skills necessary for the job. Telescribes, on the other hand, may receive more structured training that focuses on telecommunication technology and remote work.
Patient Interaction: In traditional scribing, the scribe may interact with the patient directly by taking the patient's medical history or explaining procedures. In telescribing, the scribe typically does not interact directly with the patient but instead focuses on documenting the encounter and assisting the physician as needed.
Workflow: The workflow for traditional scribing and telescribing may differ due to the location of the scribe. For example, a traditional scribe may be responsible for rooming the patient and taking vital signs before the physician enters the room. At the same time, a telescribe may join the encounter remotely after the physician has already started the visit.
While there are some differences between telescribing and traditional scribing, both can be effective ways to improve physician productivity and patient care. Practices must evaluate their specific needs and determine which type of scribing would work best for them.
Benefits Of Telescribing
Telescribing is a relatively new concept that has gained significant traction recently. It is a form of telemedicine that enables healthcare providers to capture and document patient encounters using audio-visual communication technology remotely. Telescribing has emerged as an effective solution for physicians overwhelmed with administrative tasks and patient documentation.Compared to traditional scribing, where scribes are physically present with physicians to document patient encounters, telescribing offers several benefits that can significantly enhance the efficiency of healthcare practices. Some of the key benefits of telescribing are:
Improved Productivity: Telescribing enables physicians to delegate documentation tasks to dedicated scribes, allowing them to focus on patient care and increasing productivity.
Increased Patient Engagement: By reducing the time physicians spend on documentation tasks, telescribing allows physicians to engage with their patients more effectively and provide personalized care.
Cost-Effective: Telescribing can significantly reduce the cost of hiring and managing in-house scribes, as it eliminates the need for physical office space and reduces administrative overhead.
Enhanced Accuracy: With telescribing, physicians can ensure that their patient's medical records are accurate and complete, minimizing the risk of errors and enhancing the quality of patient care.
Improved Work-Life Balance: By reducing the administrative burden on physicians, telescribing can help improve their work-life balance, enabling them to spend more time with their families and pursue other interests.
In summary, telescribing offers several benefits that can significantly improve the efficiency and quality of healthcare practices, making it an essential tool for physicians looking to streamline their workflow and provide better patient care.
Recommended Reading : What Is A Medical Scribe? And How They Are Boosting Patient Care?
The Future Of Telescribing
The practice of medicine has evolved significantly over the years. The healthcare field has undergone tremendous transformation, from the development of life-saving drugs and medical devices to the rise of telemedicine. One such innovation in healthcare delivery is the use of telescribing. Telescribing, or remote scribing, is documenting patient encounters in real time through a secure virtual platform. This allows for creating accurate and detailed medical records while enabling physicians to focus on their patients without the burden of documentation.As healthcare evolves, it becomes increasingly clear that traditional medical scribing methods are no longer sustainable. The shortage of qualified scribes, rising healthcare costs, and the need for more efficient documentation processes have led to the adoption of telescribing. Telescribing is gaining popularity in the healthcare industry, and its future looks promising. With technological advancements, the adoption of telescribing is likely to increase in the coming years. As healthcare continues to evolve, it is essential to embrace new and innovative solutions that can enhance the quality of patient care while improving efficiency and reducing costs.
Integration With Emerging Technologies
Telescribing has revolutionized the healthcare industry by providing a cost-effective and efficient solution for medical documentation. As technology evolves, there is an increasing demand for more advanced and sophisticated solutions to enhance medical documentation accuracy, speed, and quality. One such solution is integrating telescribing with emerging technologies like artificial intelligence (AI) and natural language processing (NLP).S10.AI Robot Medical Scribe is a prime example of the integration of telescribing with AI and NLP. It is a cutting-edge virtual assistant that uses advanced machine-learning algorithms to automate medical documentation. It can transcribe medical conversations and create comprehensive clinical notes in real time, significantly reducing the time and effort required for documentation.
S10.AI Robot Medical Scribe is designed to be highly adaptable and customizable, allowing physicians to tailor it to their specific needs. It can be integrated seamlessly with existing electronic health records (EHR) systems, making it easy to access patient information and update records in real time. This reduces the risk of errors and helps physicians make more informed decisions about patient care.Moreover, S10.AI Robot Medical Scribe has advanced security features to ensure patient data privacy and compliance with industry regulations. It is ISO 27001 certified, compliant with HIPAA, GDPR, and PIPEDA regulations, and uses 256-bit encryption to protect sensitive information.In addition to improving efficiency and accuracy, the integration of telescribing with emerging technologies like S10.AI Robot Medical Scribe has the potential to enhance patient care and outcomes. By automating mundane and repetitive documentation tasks, physicians can focus more on patient interaction and care, leading to better patient engagement and satisfaction.In conclusion, integrating telescribing with emerging technologies like S10.AI Robot Medical Scribe is a promising solution for the future of medical documentation. It offers significant advantages over traditional methods, including increased efficiency, accuracy, and patient privacy, while also enabling physicians to focus more on patient care.
Expansion Of Telescribing Services
Telescribing has been rapidly expanding in recent years and its popularity is only expected to grow. With the many benefits it offers, more and more healthcare organizations are realizing the potential of telescribing and incorporating it into their practices.One major advantage of telescribing is that it can be easily integrated into telemedicine, allowing physicians to access patient charts and receive real-time documentation assistance remotely. This integration with telemedicine has become even more critical in the wake of the COVID-19 pandemic, as more patients opt for virtual visits rather than in-person appointments.
Using artificial intelligence (AI) and machine learning (ML) technologies has paved the way for even more advanced telescribing services. S10.AI Robot Medical Scribe, for example, uses natural language processing (NLP) and ML algorithms to transcribe and document patient encounters accurately. Integrating AI and ML technologies not only improve the accuracy of telescribing, but also allows for more efficient and streamlined documentation processes.As telescribing continues to grow and expand, we will likely see even more advanced and innovative telescribing services being developed. The potential benefits for physicians and patients are clear, making it a promising technology for healthcare documentation.
Evolution Of Healthcare Delivery
The healthcare industry is continually evolving to adapt to new technology and patient needs. With the COVID-19 pandemic, there has been a significant shift towards telemedicine and remote healthcare services. As part of this evolution, telescribing has become an essential tool for healthcare providers to improve patient care while increasing efficiency and productivity.Telescribing, the practice of medical scribes working remotely with physicians, has been gaining popularity in recent years. With the increasing adoption of telemedicine, it has become even more crucial to have a reliable telescribing service to support physicians during virtual patient visits.Telescribing enables physicians to focus on patient care and reduces their administrative workload, resulting in more accurate documentation of patient encounters. This practice also ensures that physicians have more time to spend with patients, improving the quality of care.In addition to improving patient care, telescribing has been shown to reduce healthcare costs. With telescribing, physicians can see more patients daily, increasing revenue and decreased healthcare expenses. Furthermore, telescribing services often offer flexible pricing models, making it accessible to small practices and individual physicians.
With the increasing demand for telemedicine services, the telescribing industry is expected to grow significantly in the coming years. As new technologies, such as artificial intelligence and machine learning, are integrated into the telescribing process, the efficiency and accuracy of medical documentation will continue to improve.Overall, the evolution of healthcare delivery has brought about significant changes in the industry, and telescribing is one of the most important. As technology continues to advance and healthcare providers strive to improve patient care, the use of telescribing is expected to become even more prevalent in the years to come.
Conclusion
In conclusion, telescribing is a promising technology transforming the healthcare industry. It offers many benefits, such as increased efficiency, improved accuracy, and reduced costs. As the healthcare industry evolves, the need for telescribing services will only increase. With the integration of emerging technologies like the S10.AI Robot Medical Scribe, the future of telescribing is bright. It is an exciting time for the healthcare industry, and we expect to see more innovative solutions like telescribing that will continue to revolutionize how healthcare is delivered.
0 notes
Text
James Donaldson on Mental Health - Record suicides ‘a wake-up call’ to challenge current approach to mental health care

Key takeaways:
- The rise in suicide rates underscores the failure of the current mental health care approach.
- Collaboration and empathy are two key solutions to address challenges within the system.
A recently released report from the CDC revealed a grim milestone in mental health — a record-breaking 50,000 suicides in 2022.
This is a 3% increase from the previous year, serving as haunting proof that our current approach to mental health care is failing those who need it most. While the numbers are alarming, it is more concerning to ignore them.
It’s imperative to dissect the existing mental health care continuum in the U.S., acknowledging the stark realities and gaps that contribute to this alarming rise in suicides. The statistics, such as those provided by the CDC, are not just numbers but represent lives lost and a system in dire need of reevaluation.
A critical examination of the mental health care system reveals significant gaps, hindering effective care. Addressing the mental health crisis requires a multifaceted approach, centered on accessibility, the patient and provider relationship, and personalized care.
Accessibility through technological advancements
Accessibility to mental health services remains a hurdle, with more than one-third of the U.S. population facing a shortage of mental health care providers, according to an editorial in Nature Mental Health. In addition, some areas in the system are ill-equipped to address the diverse and complex needs of our population, leaving many feeling overlooked and neglected. As we navigate these challenges, it becomes crucial to highlight potential solutions that can pave the way for a more effective and compassionate mental health care system.
Moreover, embracing innovative technologies can enhance accessibility to mental health services, reaching those who might otherwise be left without support. Telehealth platforms, mental health apps and other digital solutions can democratize mental health care, ensuring that geographical barriers and resource constraints do not impede someone’s journey to healing.
By leveraging technology and telehealth capabilities, patients can communicate directly with their care team between sessions, ensuring consistent, quality care and access to resources at their convenience. When the person on the other end of the communication is familiar with the patient and their history, the interaction is comprehensive and individualized to best support specific therapeutic approaches, interventions or coping strategies.
Empathy at every level of care
As a patient heals, they may need different types of care during the journey. This often means a new provider, which brings up uncertainty as they have to begin the entire process of getting to know and trust someone all over again, in addition to feeling that they will need to once again get someone up to speed on their background. Having the same provider be with the patient during every step of their journey allows for the same level of understanding throughout the care continuum. Patients no longer feel handed off, but instead constantly supported at every level of care.
A strong patient and provider relationship is critical to improving mental health, and many times a provider only has “one shot” during the initial visit to make a connection. This is why having a mental health provider who exhibits empathy from the start is nonnegotiable. Mental health facilities must assess personalities upfront to ensure the patient and provider will be a strong match, and that the provider can adapt approaches that can lead to more positive outcomes.
Today, there are assessments available that can help determine the strength of the therapeutic alliance. This creates a new standard of care for organizations, empowering them to predict who’s likely to be successful and stay for the long term, a benefit to both the patient and the system alike.
#James Donaldson notes:Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticleFind out more about the work I do on my 501c3 non-profit foundationwebsite www.yourgiftoflife.org Order your copy of James Donaldson's latest book,#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
www.celebratingyourgiftoflife.com
Link for 40 Habits Signupbit.ly/40HabitsofMentalHealth
If you'd like to follow and receive my daily blog in to your inbox, just click on it with Follow It. Here's the link https://follow.it/james-donaldson-s-standing-above-the-crowd-s-blog-a-view-from-above-on-things-that-make-the-world-go-round?action=followPub
Personalizing therapy
Mental health is deeply personal, and the approach to care should be, too, tailored to align with an individual’s specific experiences, circumstances and preferences. Personalized mental health care promotes a more empathetic and deep understanding that can not only increase positive experiences but also foster a stronger connection of trust between the patient and provider.
There is no “one right way” to achieve mental well-being. By combining evidence-based therapies and a compassionate personal touch, patients can have a stronger chance to recover, grow and experience an improved quality of life.
While these changes won’t happen overnight, it is incumbent upon us to begin shifting the narrative surrounding how mental health care is addressed. The record number of suicides in 2022 serves as a wake-up call, an urgent plea for change. The path forward will not be forged by a single organization but rather through a collaborative endeavor of voices, hands and hearts.
Read the full article
0 notes
Text
Diabetes Care Knows No Boundaries: A Guide to Monitoring Parents' Glucose Abroad"
Introduction:
In a world that's becoming increasingly interconnected, families often find themselves spread across different corners of the globe. While distance may separate loved ones physically, the desire to ensure the well-being of family members remains a constant. For those with parents living abroad and managing diabetes, the challenges of overseeing their health from a distance can be daunting. However, with the advent of Continuous Glucose Monitoring (CGM) devices, technology is providing a solution that bridges the gap, offering a comprehensive guide to monitoring parents' glucose levels from afar.
The Global Landscape of Diabetes Management:
Diabetes is a pervasive health condition affecting millions worldwide. Whether managing Type 1 or Type 2 diabetes, staying vigilant about glucose levels is crucial for effective care. For families with parents residing in different countries, the global landscape of diabetes management takes on a unique complexity. Factors such as time zone differences, cultural variations in healthcare, and access to medical resources can significantly impact the ability to ensure proper diabetes care.
The Rise of Continuous Glucose Monitoring (CGM) Technology:
Continuous Glucose Monitoring (CGM) technology has revolutionized diabetes management by providing real-time data on blood sugar levels. This technology involves a small sensor placed under the skin that continuously measures glucose levels and transmits the data to a monitoring device or smartphone. The ability to receive instant updates on glucose levels enhances not only the accuracy of diabetes management but also the speed at which necessary adjustments can be made.
Overcoming the Distance Barrier with CGM Devices:
One of the primary challenges faced by individuals managing their parents' diabetes from abroad is the physical distance that separates them. CGM devices serve as a crucial tool in overcoming this barrier, offering a virtual connection to their parents' health. The real-time data provided by the CGM system allows for prompt responses to fluctuating glucose levels, irrespective of the geographical distance.
Choosing the Right CGM Device:
Selecting the most suitable CGM device is a critical step in effective long-distance diabetes management. Factors such as sensor accuracy, ease of use, data accessibility, and integration with other health platforms should be considered. It's essential to conduct thorough research, consult healthcare professionals, and explore user reviews to make an informed decision.
Remote Monitoring Apps and Platforms:
In addition to the CGM device itself, utilizing remote monitoring apps and platforms enhances the ability to keep track of parents' glucose levels. Many CGM systems offer dedicated applications that provide comprehensive insights, trend analysis, and customizable alerts. These apps facilitate seamless communication between caregivers and healthcare providers, ensuring a collaborative approach to diabetes care.
Establishing Communication Protocols:
Clear and effective communication is the cornerstone of successful long-distance diabetes management. Establishing protocols for sharing CGM data, discussing medication adjustments, and coordinating with healthcare professionals helps create a streamlined process. Regular virtual meetings or telehealth appointments can also be scheduled to ensure ongoing support and address any concerns.
Collaborating with Local Healthcare Professionals:
While technology plays a pivotal role in remote glucose monitoring, collaborating with local healthcare professionals in the country where parents reside is equally important. Establishing connections with local doctors and diabetes specialists ensures that there is a support system in place for emergencies, medication adjustments, and routine check-ups.
Navigating Time Zone Challenges:
Time zone differences can pose a unique challenge in managing parents' glucose levels from abroad. Developing a schedule that accommodates both the caregiver's location and the parents' local time is crucial for timely interventions. Utilizing technology to set reminders and alerts based on the parents' daily routines helps maintain consistency in diabetes care.
Conclusion:
In the era of advanced healthcare technology, diabetes care truly knows no boundaries. Continuous Glucose Monitoring devices have become invaluable tools for individuals overseeing their parents' health from abroad, offering real-time data, connectivity, and peace of mind. By embracing these technologies, establishing clear communication channels, and collaborating with local healthcare professionals, caregivers can navigate the challenges of long-distance diabetes management with confidence and efficiency. The journey towards ensuring the well-being of loved ones becomes a shared experience, transcending geographical limitations and reinforcing the notion that, indeed, diabetes care knows no boundaries.

0 notes
Text
A Manual To Selecting The Right Holistic Wellness Clinic

Choosing the right holistic health clinic is actually an important step towards achieving overall wellness. Holistic health and wellness concentrates on the interconnectedness of the mind, body system, and character, focusing on the importance of dealing with the whole individual as opposed to just taking care of certain signs.
To Assist You Opt For A Holistic Wellness Clinic, Listed Here Is Actually An Overview:
Study and also Credentials
Begin through looking into potential holistic wellness clinics in your place. Search for clinics along with knowledgeable and competent experts. Inspect their qualifications, qualifications, as well as licenses. Guarantee that the professionals are proficiented in different holistic techniques including homeopathy, chiropractic care, naturopathy, as well as a lot more.
Companies Offered
Analyze the range of solutions delivered due to the clinic. An extensive holistic health clinic needs to give a range of procedures to take care of various facets of your health. This may consist of acupuncture, herbal medication, dietary counseling, massage therapy, yoga exercise, and also other alternate therapies. The more unique the companies, the better the clinic may adapt a holistic approach to your specific requirements.
Treatment Philosophy
Understand the clinic's treatment theory. Holistic wellness is actually based on the concept that the body system has the capability to heal itself when given the ideal support. Guarantee that the clinic's ideology lines up with your ideas as well as tastes. Some clinics might concentrate on preventative care, while others might provide services for dealing with existing health and wellness concerns.
Practitioner-Patient Relationship
Keep an eye on the practitioner-patient partnership. Holistic wellness professionals often invest more opportunity with individuals compared to conventional doctor. A sturdy, open, and also trusting relationship along with your specialist is important for the effectiveness of holistic procedures. Consider scheduling an assessment to get a sense for the clinic's setting and also the professionals' method.
Customer reviews and Testimonials
Try to find reviews and also recommendations coming from previous individuals. On-line testimonials can easily supply understandings in to the knowledge of others that have found care at the clinic. Keep an eye on both positive as well as negative feedback to get a well-shaped understanding of the clinic's assets as well as potential weak spots.
Ease of access
Take into consideration the clinic's location, hours of operation, and also total availability. A holistic health clinic that is actually conveniently positioned and also possesses pliable hours can make it much easier for you to integrate holistic treatments in to your way of life. Furthermore, ask about the accessibility of digital or even telehealth appointments.
Holistic Approach to Health
Make certain that the clinic accepts a genuinely holistic approach to wellness. This suggests dealing with certainly not only bodily indicators yet additionally looking at psychological as well as emotional well-being. Holistic experts must consider your wellness in a complete fashion, bearing in mind way of living, diet, worry degrees, and also various other variables.
Communication and Education
A great holistic health London clinic must prioritize client learning. The professionals ought to agree to clarify the numerous procedures as well as their perks, empowering you to definitely take part in your wellness quest. Clear communication regarding procedure strategies as well as expected outcomes is important.
Follow-up and Continued Support
Inquire concerning the clinic's method to follow-up care and recurring help. Holistic wellness is actually often an adventure, and also continuous support is essential for long-term welfare. Ask regarding follow-up consultations, check-ins, and any type of sources or devices provided for self-care.
Choosing the best holistic health and wellness clinic includes cautious factor to consider of different elements. By making the effort to study, inquire inquiries, and also analyze the clinic's offerings, you may discover a holistic health provider that straightens with your values and sustains your adventure towards optimal health.
NŪŪTRO
58 South Molton Street, Mayfair, W1K 5SL London
+447392227735
0 notes
Text
Navigating the Complex Landscape of Billing for Behavioral Health Services
In the consistently developing field of healthcare, billing for behavioral health services and mental health services presents extraordinary difficulties that require a nuanced comprehension of both clinical practices and repayment structures. As experts endeavor to give fundamental mental health care, the complexities of billing can sometimes become an obstruction. This article means to reveal insight into the critical parts of billing for behavioral health and mental health services, offering bits of knowledge to specialists, heads, and healthcare experts.
Grasping the Scene: Behavioral Health Services
Billing for behavioral health services incorporates a wide range of care, going from treatment and directing to additional concentrated medications for people confronting mental health challenges. Behavioral health services frequently address conditions, for example, uneasiness, sadness, substance misuse, and other mental problems. While exploring the billing system, specialists should know about the particular codes and guidelines related to these services.
The Role of Legitimate Documentation in Billing for Mental Health Services
A basic part of fruitful billing for mental health services lies in exhaustive and exact documentation. Mental health experts should fastidiously record patient evaluations, treatment plans, and progress notes to legitimize the need for the offered types of assistance. Legitimate documentation guarantees adherence to moral norms as well as lays out a strong starting point for billing purposes.
Coding and Repayment
In the domain of billing for mental health services, exact coding is vital. Mental health experts utilize different Current Procedural Terminology (CPT) codes to address the particular services delivered during a meeting. It is urgent to keep up to date with updates to coding frameworks to try not to charge disparities. Furthermore, understanding the subtleties of repayment, including insurance contracts and charge plans, is fundamental for boosting income while giving quality consideration.
Exploring Insurance Challenges in Billing for Behavioral Health Services
Protection assumes a critical part in the repayment cycle for behavioral health services. Numerous mental health experts experience difficulties connected with pre-approvals, inclusion restrictions, and guarantee dissents. Effective billing for behavioral health services includes proactive correspondence with protection suppliers, confirmation of inclusion, and support for fundamental services to guarantee fair repayment.
Integrating Telehealth into Billing for Behavioral Health Services
The ascent of telehealth has transformed the conveyance of mental health services, giving more noteworthy openness to patients. Nonetheless, billing for telehealth services presents its arrangement of contemplations. Specialists should find out more about unambiguous telehealth CPT codes and comply with guidelines administering virtual help repayment. Exploring the crossing point of innovation and mental health billing is vital to adjusting to the developing scene of healthcare.
Difficulties and Opportunities in Billing for Mental Health Services
While presents difficulties, it likewise makes the way for open doors for development. Cooperative efforts inside the local healthcare area, continuous instruction on billing practices, and support for strategy changes are fundamental parts of tending to these difficulties. As the scene keeps on developing, experts should adjust and effectively take part in conversations that add to more straightforward and productive billing processes.
To Sum It Up
All in all, billing for behavioral health services and mental health services requires a diverse methodology that consolidates clinical skills with an exhaustive comprehension of billing guidelines. By focusing on legitimate documentation, remaining informed about coding and repayment changes, and embracing mechanical arrangements, mental health experts can explore the intricacies of billing while at the same time guaranteeing the conveyance of fundamental consideration to those out of luck.
0 notes
Text
Choosing the Best: A Review of Post Surgical Care Services in Mysore

Choosing the Best: A Review of Post Surgical Care Services in Mysore
Introduction
In the realm of healthcare, post-surgical care plays a pivotal role in the recovery journey of individuals who have undergone various medical procedures. Navigating through the myriad of services available in Mysore can be a daunting task, making it crucial for individuals and their families to choose the best post-surgical care. This article aims to provide a comprehensive review of post-surgical care services in Mysore, offering insights into key factors to consider when making this crucial decision.
Understanding Post-Surgical Care
Post-surgical care involves the specialized attention and support provided to patients after undergoing surgical procedures. This phase is critical as it contributes significantly to the overall success of the surgery and the patient's well-being. There are different types of post-surgical care, ranging from simple outpatient follow-ups to extensive inpatient rehabilitation programs.
Key Factors in Choosing Post-Surgical Care Services
Selecting the right Post Surgical Care Services in Mysore involves a careful evaluation of various factors. The professional expertise of the care giving team, the amenities offered by the facility, and the experiences shared by other patients through testimonials are crucial aspects to consider. Choosing a service that aligns with individual needs ensures a smoother and more effective recovery process.
Availability of Specialized Care
One size does not fit all when it comes to post-surgical care. The article delves into the importance of specialized care services tailored to specific surgical procedures. Providers offering customized care plans for different surgeries ensure that patients receive the precise attention required for their recovery.
Technological Advancements in Post-Surgical Care
The integration of technology in post-surgical care services has revolutionized the way patients experience recovery. From advanced monitoring systems to telehealth options, technology plays a vital role in enhancing the overall patient experience and improving recovery outcomes.
Comparison of Top Post-Surgical Care Services in Mysore
Post Surgical Care Services in Mysore boasts several post-surgical care services, each with its unique offerings. This section of the article compares the top services in the region, shedding light on what sets them apart and helping readers make informed decisions.
Patient-Centric Approach
The human touch is irreplaceable in healthcare. The article explores the significance of a patient-centric approach in post-surgical care, emphasizing the importance of personalized care plans that consider the individual needs and preferences of each patient.
Affordability and Insurance Coverage
Cost considerations and insurance coverage are often key determinants in choosing post-surgical care services. This section provides insights into understanding the financial aspects and navigating insurance options to ensure a smooth and financially viable recovery process.
Post-Operative Rehabilitation Services
Physical therapy and rehabilitation programs are integral components of post-surgical care. The article explores the role of these services in enhancing recovery and getting patients back to their normal lives.
Community Engagement and Support
Community involvement and support can significantly contribute to the overall well-being of individuals undergoing post-surgical care. From local support groups to community resources, this section highlights the importance of a robust support system.
Choosing the Right Facility for Your Needs
Selecting the right facility involves a thorough evaluation process. The article provides readers with a checklist and practical tips to aid in choosing the post-surgical care service that best suits their needs.
Common Challenges in Post-Surgical Care
No system is without challenges, and post-surgical care is no exception. This section addresses common issues that may arise during the recovery process and how top-notch services overcome these challenges.
Ensuring Quality and Safety
Quality and safety are paramount in healthcare. The article discusses the importance of accreditation, certifications, and adherence to safety standards in ensuring the delivery of high-quality post-surgical care services.
Future Trends in Post-Surgical Care Services
The healthcare landscape is ever-evolving. The article explores emerging technologies and anticipated advancements in post-surgical care services, giving readers a glimpse into the future of healthcare.
Conclusion
In conclusion, choosing the best post-surgical care services in Mysore involves a thoughtful consideration of various factors. From the expertise of the caregiving team to the support of the community, each element plays a crucial role in the overall recovery journey. By prioritizing personalized care, affordability, and safety, individuals can make informed decisions that positively impact their post-surgical experience.
0 notes