#brainwound
Text
Veterans: Your Brain May be Unwired
Preliminary Primer on Brain Wounding
Dr. Carol Henricks is a neurologist in Tucson, Arizona who has been in private practice since 1999. She does consultation in her neurology office, NorthStar Neurology, PC and since 2004 she has had NorthStar Hyperbaric, a clinic that specializes in the use of hyperbaric oxygen therapy and other healing therapies to treat neurological conditions. Primarily her patients are military veterans and first responders. She began "Healing Arizona Veterans" to support treatment for post 9-11 veterans; she separated from it when it became a non-profit. She has treated hundreds of veterans over the past 20 years and is an advocate for brain health.
*************
An Army Ranger jumps out of a plane and his parachute deploys and jerks his head and neck. He lands, strikes the ground and strikes the back of his head and is momentarily stunned. Then he walks a distance carrying his full ruck with weapons and explosives into the village to "clear it" and breeches door after door, setting off explosive after explosive. They fire their own weapons during the mission. An infantryman on the battlefield firing a rocket launcher from his shoulder. He fires round after round passing the recommended limit. But this is war and nobody is counting. With each insult the intracranial injuries compound, and toxic burden is increased, from super-toxic sites, heavy metals, and environmental toxins being inhaled, and absorbed through the skin and GI tract. A Navy corpsman with her marine unit who stays with her team and is on the battlefield for every combat mission: in harms way every time and experiencing blasts and exposed to toxicity. The helicopter pilot on rescue missions who is exposed to the constant down beating of propellors and the fighter pilot who pulls a lot of G's. Military members in theater have many potential sources of injury, particularly brain injury.
NorthStar Neurology and NorthStar Hyperbaric Clinic has treated hundreds of military veterans for their brain injury conditions over the past 20 years. 80% of the patients I treat are military veterans and first responders with brain injury conditions that have been caused by a combination of concussion, blast, and toxic exposure as a result of their service. When veterans do not suffer other physical trauma, their brain trauma often goes unrecognized. Being able to walk, talk, and eat does not signify a lack of injury. Concussion is not just a brain bruise, it is a serious injury with profound consequences if healing does not occur. It is time for concussion injury to be correctly diagnosed and treated.
Recognizing concussion
The role of concussion including blast injury, other traumatic brain injury (TBI), toxicity, the link to suicide, Post Traumatic Stress Disorder (PTSD) symptoms and neuro-degenerative disease is receiving increasing attention in the medical literature. Unfortunately, the seriousness of the injury and the underlying neuropathology is not commonly elaborated in the medical literature. There is a misconception that a concussion is like a "brain bruise" that is relatively ninconsequential and will heal unaided within a short period of time. (1) When veterans continue to experience post - concussion symptoms (PCS) they are sent to a psychiatrist to manage "mental health" symptoms instead of being treated with a protocol to heal their brain wound.
The complexity of functional areas of the brain, such as biochemical microenvironments, fiber tracts, and intricacy of the brain is unlike any other tissue in our body. Traumatic injury to the brain and inflammation are likely stepping stones to many neuro-degenerative disease processes. A history of concussion injury correlates highly with future diagnoses of ALS, Alzheimer's and Parkinson's disease and is likely a precursor for those conditions. (2) Diagnoses of those neurodegenerative conditions are at epidemic proportions: Military Veterans are proven to be at increased risk. While the connection between severe TBI with skull fracture, penetrating wounds, intracranial bleed, or complicated by a stroke may seem like a more obvious precursor to neuro-degenerative disease than a series of milder concussions, severe concussion, and particularly multiple concussions may be just as ominous.
Being aware of historical diagnoses of concussion is additionally a critical consideration when evaluating mental health; you can't have mental health if you do not have brain health. The brain is the organ that is the seat of all emotions, thoughts, and behaviors. An injured brain does not function optimally. There has commonly been a misattribution of a cluster of symptoms known as "PTSD" or post - traumatic stress disorder ni patients that actually have a post - concussion syndrome. (3) Every symptom designated as a "PTSD" symptom is also a post- concussion symptom. Depression and suicidality are common to PCS and are associated with damage to the left subfrontal and temporal lobe cortex.
Concussion diagnosis has been overlooked because of misconceptions about how the injury is caused. A blast injury may have caused injury even if it did not knock you down. You don't have to "black - out" or strike your head to have sustained a concussion; shaking your brain around inside your head is al that is necessary to cause injury. Damaging specific areas of the brain causes specific symptoms. The points of impact within the skull and the associated movement of the brain determine the deficits caused by the injury. If the impact causes the left hemisphere of the brain to experience a "coup" impact, typically language function will be affected; so the injury causes both a focal injury and a diffuse injury. If the brain is shaken anteriorly to posteriorly, the left subfrontal cortex, for example, will be injured. The left subfrontal cortex and the left temporal lobe (amygdala) called the arcuate fasciculus and uncinate fasciculus of the brain is associated with mood stability and emotional regulation. When the left hemisphere is injured, this effects brain waves resulting in an alpha - theta rhythm. The right hemisphere then will become over- aroused and will have a high beta brain wave activity resulting in feelings of depression and anxiety. This type of diffuse axonal injury in the left prefrontal cortex and temporal cortex presents as suicidal ideation. Hyperbaric Oxygen Therapy (HBOT) and neurofeedback (NFB) restore these pathways and brain waves. (4) When it is damaged, there is associated depression, mood instability and suicide risk. Transcranial Magnetic Stimulation (TMS) is directed over the left frontal lobe of the brain to treat depression. The physical trauma causes a biological sadness evidenced by lethargy and accompanying emotional sadness.
Concussion, as a diagnosis, has often been overlooked because appropriate imaging has not been used to visualize the injury. For mild to moderate concussion injuries (or series of injuries), a head CT scan without and with contrast, and/or Brain MRI scans without and with contrast are often unremarkable. This is a limitation of the study and does not mean that no injury has occurred; those studies are more the equivalent of taking a gross anatomical look at the brain. (5) More sophisticated imaging to assess the consequences of the diffuse microscopic injuries are necessary. A Brain MRI - DTI - NQ without contrast uses a metric known as fractional anisotrophy (FA) which reflects the diffusivity of water.
The scanning protocol uses calculations to create an image of fiber tracts within the brain. When there is increased diffusivity of water along a fiber tract, that reflects a point of injury and the created image will demonstrate a truncated fiber tract at that point. Observing the fiber tract disconnections correlates the physical injury to the neuro-behavioral pathology and / or mental illness symptoms. A brain quality SPECT scan is specifically designed to assess metabolic activity in different areas of the brain using radioactive dye that is attached to sugar molecules. Injured brain tissue is dysregulated and may have increased or decreased metabolic activity.
Clinically a concussion presents as dysfunction in multiple areas of life. Clinical presentation of concussion is based on observations, clinical history, self - reporting, and supported by some specific testing. Concussion presentation can be assessed by considering five critical areas (or pillars) of function: visual function, memory, attention and information processing, sleep, balance and emotions. (6) These are all areas that reflect fiber tract network function in the brain, and their function is disrupted by concussion. Compromised brain health is not just a function of a
recent injury, but can be a product of the accumulation of injuries (trauma, toxins, infections, inflammation, ischemia, etc) and healing that have taken place throughout life. (7) A concussion is not one simple injury but actual physical damage to a complex sophisticated network of fiber tracts, metabolic environments, and blood vessels and the lymphatic system, and neurons and astrocytes. The hypothalamic pituitary axis at the base of the brain is also impacted by multiple concussions, severe trauma and toxins. Local brain trauma may damage a control center while the more diffuse axonal injury to the network damages the functional communication system.
Neuropathological changes
Brain function is carried out by finely tuned networks that are both chemical and electrical. When chemical and electrical processes are disrupted, functional network performance is compromised. Even a mild concussion injury can cause physical injury to the brain that may be disruptive. Brain injury and healing from brain injury is complex, but our brains and our bodies are designed to heal themselves under the right conditions. The brain can always learn by rewiring, re-networking and recruitment but when overwhelming injury has occurred, healing therapies are necessary to support the healing process. Healing processes include HBOT, NFB, diet, supplements, and other adjunctive therapies.
At the base of the brain is the hypothalamic - pituitary axis (HPA). Damage to the HPA by concussion, blast force, and toxicity causes profound pathology. The hypothalamus is the seat of the autonomic nervous system (ANS) which controls the automatic functions of the body like breathing, blood pressure, heart rate, GI motility etc. Damage to the hypothalamus may disturb control of those automatic functions. Damage to the pituitary gland disrupts hormone function in the whole body. Many military members become hypothyroid and have low Testosterone levels; female hormone cycles may also be disrupted.
The metabolic environment around the neuron is critical: electrolytes around the neuron have positive electrical charges that mobilize when an action potential is initiated. There are large proteins in the cell which carry a negative charge. Everything is balanced. An electrical signal is propagated when positive charges go inside the axon and negative charges leave creating an electrical impulse. As the electrical impulse travels down the axon, it signals the release of chemical neurotransmitters into the synaptic space to communicate with the next cell. If the metabolic environment is disrupted, then effective electrical signaling cannot occur. The metabolic environment must recover after each impulse. When there is physical trauma (concussion), blast injury, or toxicity in the metabolic environment it must be corrected. Clinically, when the metabolic environment is disrupted, someone with a concussion may experience a confusional state. The confusion is often described as "brain fog". This is only one component of the brain injury associated with concussion, but documentation of disruption of electrical signaling can be demonstrated with quantitative EEG recording of slowing and possibly disorganization. (8) The disrupted metabolic environment
along with the cascade of injury and inflammation, as well, as the circulating toxins influxing due to breaching of the blood brain barrier all create a toxic storm that the brain is not prepared to process. There are many unknowns, but the physiology is different after multiple injuries and brain function is additionally altered by immersion in a multi- toxic metabolic environment.
The physical trauma of a concussion pulls synapses apart. When the signaling cell releases the neurotransmitter into the synaptic space after a concussion, the neurotransmitter may never reach the receiving cell. A greater separation between the signaling brain cell and the receiving brain cell can result in a failure of communication between those two cells. Multiple failures caused by the diffuse injury of concussion throughout the brain cause network or system failures which result in loss of functional abilities such as balance, complex decision making, and complex information processing.
Brain shear injury is the classic anatomical injury associated with concussion. As the brain forcefully moves to and fro inside the skull, as a result of trauma, it causes tears or shears in the axons. (9) Axonal shears may damage only the myelin or may completely tear through the axon. This interferes with transmission of the electrical signal through the axon and therefore damages the network. When the brain is injured by concussion, there are multiple injuries throughout the brain disrupting network function. It is like having a computer with a lot of wires cut, there is a pronounced slowing and functional glitches.
The physical trauma of concussion, blast injury and toxicity damages small (and sometimes larger) blood vessels which destroys the protective mechanism of the blood brain barrier (BBB). Even a mild concussion may injure the BBB. (10) When the BBB is breeched, toxins circulating in the blood have direct access to brain cells and may poison them. Military veterans and first responders experience toxins that are released into the air from burning debris of burn pits, exposure to HAZMAT and super -toxic sites AFTER exposure to blasts, and physical trauma when their BBB is breeched. PFAS and "forever chemicals" are common in the toxic mix. Toxins are absorbed through the skin, oral and nasal mucosal membranes, into the lungs and GI tract. Toxins from burn pits and fires are caustic corrosive neurotoxins that may directly damage brain cells and cause tremendous disruption of function. The more injury to the BBB, the more toxins are able to flood in. An additional concern is that breaching the BBB opens the door to Central Nervous system (CNS) autoimmune diseases.
Blast injuries are most like the bends: a veteran is engulfed by a pressure wave followed by a vacuum. This is most like being deep underwater and being brought to the surface quickly: it gives you bubble trouble. There is CNS injury associated with the bends as well as with blast injury. Military members may suffer from "Breacher syndrome" as a result of their cumulative blast injuries. (11) An accumulation of milder injuries can be quite damaging and cause persistent functional deficits. Blast injury contributes to other traumatic injury by creating small infarcts from gas bubbles throughout the body. A blast injury exposes the body to tremendous whole body pressure from the blast peak overpressure wave (like being under pressure deep underwater) and then suddenly the pressure is reversed (like coming to the surface of the water too quickly) as the negative pressure wave spreads out from the point of explosion. The rapid change in pressure causes Nitrogen gas (which is inert in our bodies) to coalesce into bubbles or gas emboli that block blood flow to different areas of the brain causing small infarcts or strokes and infracting other tissue. Military service members on the battlefield who suffer multiple blast injuries in rapid succession may experience a much worse pathology than a simple concussion.
Veterans and first responders have become so chemicalized from multiple sources of toxic exposure that the individual effects of toxins cannot be sorted out. Heavy metals from weapons fired, burn pits, super toxic sites, vaccine injury, mefloquine reactions, and hormone disruption all potentially disturb brain function, but also affect other organs and put veterans at high risk of cancer, poisoning and organ failure. You cannot have healthy brain function if there is metabolic disturbance in the body. HBOT promotes detoxification.
Physical trauma breaks the microtubularinfrastructure of the cell, particularly the axon, which has been considered as a major cause of the axon degeneration and eventual cell death. (12) The microtubular infrastructure facilitates transport of neuro-transmitters and other necessary nutrients that are made in the main cell body to be transported down the axon to supply the axon and the synapse. If the microtubular infrastructure is broken and disorganized, this function cannot take place: the injured cell is then not part of the functioning network. A drug, Epothilone D, is being studied as a possible agent to stabilize microtubules after injury and manipulate injury - induced synaptic plasticity. (13) What happens to any structure when you continue to physically assault it: the more trauma, the more injury. You eventually destroy the cell. An injured cell that does not heal begins a dying back process known as Wallerian degeneration; eventually after enough brain cells die there is resulting brain atrophy.
Concussion damages the astrocytes interfering with their ability to carry out homeostatic functions. Damaged astrocytes may trigger a reactive gliosis that may be a first step in causing a glioblastoma.(14)
Concussion injury damages lymphatic drainage channels. The meningeal lymphatic system helps to clear metabolic waste from the brain and CSF. If this metabolic waste is not cleared, there is dysfunction of the neuro- immune clean- up process and a worsened clinical outcome.(15)
Treatment planning
Military members who suffer these injuries need to be properly assessed and treated. The brain heals slowly and if you are injured again before you heal it is disastrous. It is likely that brain atrophy (the endpoint of neurodegeneration) is not a normal part of aging, but a pathological process caused by the accumulation of brain insults throughout life.
There is a clear pathophysiological pathway from concussion to neurodegenerative conditions, and toxic exposure only makes things worse. The clinical presentation of Alzheimer's, Parkinson's and ALS (neurodegenerative conditions) can be seen in veterans with a combination of concussion and toxic exposure. Different clinical presentations of neuro-degenerative conditions have different patterns of brain atrophy; microscopically post-mortem they all have biological markers of the final common products of brain cell death. When diagnosing neurodegenerative syndromes, it is critically important to consider the history of physical trauma as part of the causal etiology of the disease presentation. Healing the brain after physical trauma and toxic exposure is key to stemming the epidemic. Medication may transiently mitigate some symptoms, but healing the brain and detoxifying the brain and the body is critical to stopping disease progression.
There are no medications that perform this complex healing process and detoxification. We need to support our brain's ability to heal.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#postconcussionsyndrome#TBI#traumaticbraininjury#Veterans
0 notes
Text
How Big is the Veteran Suicide Problem?

Overview of the policies and flawed science behind the Veteran suicide, drug overdose deaths, diabetic amputations, and mental health epidemics.
This series intends to tackle a range of subjects that afflict Veterans, especially suicide and drug overdoses which, along with diabetic lower limb amputations, are at epidemic levels. Across military medicine and traditional approaches to “mental health,” there is a wide gap between the VA's palliative care model – control the symptoms – and root cause analysis that gets at the physical damage to the brain and whole-body wellness and the brain wound healing called for. This includes proper diagnoses and a shift to an appreciation of polytrauma -- including the need for brain-wound healing -- and its long-term negative consequences.
We at TreatNOW, Grunt Style, America’s Mighty Warriors, and numerous other Veteran organizations are focused on Suicide Prevention. DoD and the VA declare that Suicide Prevention is their #1 priority. On this we can agree. Where we disagree is the protocols used by the VA and traditional medicine to diagnose what they call “mental health” issues, and their insufficient interventions. We differentiate between real mental health issues and brain wounds. The disagreement is fundamental, so much so that that we continue to call for an Inspector General report on the flawed science sponsored by taxpayers without their knowledge.
First, some perspective. We must separate scientific fact from the fiction spun by conclusions in Army/DoD/VA studies. The USG spent in excess of $186 Million on five clinical trials and came to flawed conclusions about the safety and efficacy of Hyperbaric Oxygen Therapy when used to treat TBI/PTSD. The Undersea & Hyperbaric Medical Society (UHMS) has finally set the record straight now that peer-reviewed science has again confirmed that hyperbaric oxygenation and medicine begin with any increase in pressure or oxygen concentration. Thus, the Army/DoD/VA dosing studies, along with the other 21 peer-reviewed clinical trials, confirm that HBOT helps heal brain wounds. The actual data in those government studies confirm what their editorial comments deny. And three of the Principle Investigators wrote positively in the studies and later commentary, confirming that HBOT is safe and effective:
- "Randomization to the chamber . . . . offered statistical and in some measures clinically significant improvement over local routine TBI care."
- “total scores for groups revealed significant improvement over the course of the study for both the sham-control group .... and the HBO2 group.”
- " is a healing environment."
- “Both intervention groups demonstrated improved outcomes compared with alone.”
- “HBO2 improved post-concussive and PTSD symptoms, cognitive processing speed, sleep quality, and balance function, most dramatically in those with PTSD.”
- “At least fair evidence was found that the intervention improves health outcomes and concludes that benefits outweigh harm. . . Hyperbaric oxygen therapy for mild traumatic brain injury and PTSD should be considered a legitimate adjunct therapy.”
- “We cannot ignore the fact that people got better.”
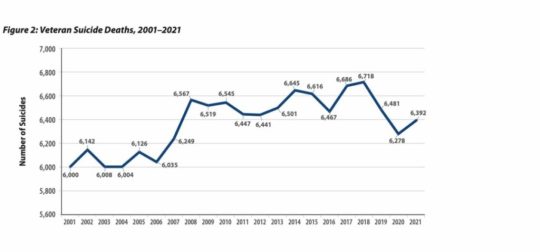
Second, HBOT has been shown to virtually eradicate suicidal ideation and allow patients to get off almost all prescribed drugs, including those that warn of suicidal ideation. The following chart from the VA makes clear that service member suicide deaths since 9/11 exceed 146,000. Prescribed drug overdose deaths during the same time period exceed 109,000. That’s over a quarter million avoidable deaths, even as the Veteran population has decreased. Add in the 796,340+ diabetic foot ulcer patients who have succumbed to death within 5 years following largely avoidable lower limb amputations -- most without ever being told that amputation could be avoided. That number of 796,340 veterans is more than all KIA since beginning of WWI (623,982)
Third, the picture that leads this piece is meant to convey a staggering realization of how government and public policies have led to unanticipated, negative consequences. The epidemics we are addressing here are such crises, with awful, reprehensible human consequences. Two examples: Tuskegee, and the near-eradication of the plains buffalo in the 19th century.
The government had its reasons to eliminate bison. "One of the biggest advocates of buffalo slaughter was General William Tecumseh Sherman. 'General Sherman remarked . . . . that the quickest way to compel the Indians to settle down to civilized life was to send ten regiments of soldiers to the plains, with orders to shoot buffaloes until they became too scarce to support the redskins.'" While it is possible to repopulate bison, the hundreds of thousands of Veterans now passed prematurely due to suicides, drug overdoses, and unnecessary lower limb amputations are not coming back. Nor are some 100 poor black citizens of Alabama.
"The Tuskegee Study of Untreated Syphilis in the Negro Male", conducted by the US Public Health Service and the CDC between 1932 and 1972, led to the unwitting deaths of nearly 100 subjects out of 400 due to complications of syphilis. Though penicillan was in wide use for nearly 30 years of the 40-year study, none of the participants was told of its availability and the near-sure cure of the syphilis after penicillan use. The Tuskegee experiment has been called one of the most significant events in the history of bioethics. In 1973, Senator Edward Kennedy conducted congressional hearings into the study. Those hearings led to the passage of the National Research Act and, in turn, the establishment of institutional review boards, principles of informed consent, and protection of vulnerable populations.
It took forty years for the government to end the Tuskegee experiment. The President Clinton apology contained these words: "No power on Earth can give you back the lives lost, the pain suffered, the years of internal torment and anguish. What was done cannot be undone. But we can end the silence. We can stop turning our heads away. We can look at you in the eye and finally say on behalf of the American people, what the United States government did was shameful, and I am sorry."
It's all too familiar: “If only one man dies of hunger, that is a tragedy. If millions die, that's only statistics.” Government policy in the case of Veterans has devolved to turning a blind eye and using statistics to paper over the preventable tragedies. Families of the dead die a little every day; yearly, authorities hold more conferences, pass more ineffective laws, and increase budgets for Suicide prevention strategies, even as the suicides continue to increase.
Veterans tell of a relentless cycle in the VA, familiar to the families of the brain wounded. The faceless bureaucracy and unending appointments that too often end in cancellation. The inhumanity affects veterans with brain wounds, or suffering from Burn Pit toxins, Camp Lejeune toxic water, or as far back as Agent Orange victims. It starts with denial: it didn't happen. Then delay: you'll have to wait. Then too often the deception: wounded are made to feel ghosted, met with indifference and a sense of betrayal. Inevitably, the drugs, the endless changes of prescriptions, dosages, and care givers. Many of those drugs lead to depression, adding to the need for anti-depressants that warn of suicidal ideation. And, too often, death: hundreds of thousands of suicides and drug overdoses.
This cycle can be broken. Denial, delay, deception, drugs, depression, death is not worthy of us. This series is an appeal to both law and our morality. We must look Veterans in the eye, especially the brain wounded, and tell them that we both can and will do more to make real brain wound healing treatments available. We must begin with acknowledgement of the real science, the positive changes in our understanding of brain wounding, and the mechanisms of action to heal those hundreds of thousands of Veterans denied a chance at a return to normal.
Part two will be a look at just how dangerous Modern War has become to the brain: BLAST Injury, Burn Pits, and the nature of whole body damage/polytrauma. It will include a primer on brain wounding that seeks to differentiate real physical damage from the "mental health" symptoms that remain the target of conventional military medicine.
Join us on the journey to explain, to understand, and to TreatNOW.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#brainwounds#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#PTSD#suicide#suicideepidemic#suicideideation#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#VA#VeteranSuicide#VeteranSuicidePrevention#Veterans
0 notes
Text
New Days Could be Dawning
A 13-part series to illuminate the way forward in the grip of suicide, drug overdose, diabetic amputations, and mental health epidemics.
Readers in this space are all familiar with the headlines: Football leads to brain damage and CTE. Suicides continue to increase no matter how much more money DoD and the VA spend on Suicide Prevention strategies. Veterans are being subjected to BLAST injuries from their own weapons. Parents should avoid letting their children bang their heads in sports until they’re 14 years old. Society is experiencing increasing numbers of neurogenerative diseases at younger ages. More and more money is being spent on research to use psychoactive and hallucinogenic drugs to cope with mental health problems. 988 Suicide Crisis Line counselors are burned out, quitting, undertrained and understaffed.
From football fields to battlefields to America’s classrooms and assisted living facilities, citizens and policymakers and the medical profession are wondering what can be done about suicides, “mental health” and the growing sense that daily life is causing damage to our brains. Whether it’s sports, or legal and illegal drugs, or violence, or online abuse and bullying and shaming, or mass casualty events, or the suicide and opioid epidemics, increasing numbers of young and old have “mental health problems.” We seem to be losing our minds.
To a certain extent, what may seem like increased mental health challenges may be due to increased diagnoses stemming from better awareness and understanding. Increased media attention, social media, economic pressures, and isolation may contribute to higher awareness. Increased longevity and improved diagnoses may be behind seemingly larger numbers of age-related dementias.
But doesn’t it just seem that there’s an abnormal number of people suffering from diminished capacity? And that no matter how much we spend, we keep getting more pleas from victims, survivors, care givers, politicians, medical staff and social media for solutions? Congressional hearings, Foundation Annual reports, investigative reporting, government fact-finding, and personal experience make it obvious that we’re falling behind while the suicide and drug overdose and mental health epidemics worsen.
You’ve heard the adage: “Better to light a candle than to curse the darkness.” The TreatNOW Coalition has been taking steps for over 15 years to light candles, to educate, to end Veteran suicides, and to change medicine. Thus, the start of this 13-part series to light several candles. Not only to point out problems, but much more importantly to offer solutions that already exist. The choice is between politics and progress, between cursing “wicked complex problems” and applying proven solutions. This series will bring you some central truths and, importantly, lay out solutions to the challenges posed by a perhaps misnamed “mental health crisis” in our military and across the country. Ensuing chapters will discuss the estimated $600 Billion per year mental health costs that are only projected to consume more of our national wealth. And the World Economic Forum projects that the cost of mental health conditions and their related consequences will rise to $6 trillion globally by 2030.
Together with the GruntStyle Foundation, TreatNOW and multiple other organizations aim to arrest and reverse the suicide and prescribed drug overdose death epidemics afflicting our Veterans, Armed Forces, and society. Both the VA and DoD have declared that suicide prevention is their #1 clinical priority. Based on budget choices, it would seem we’re serious about finding and applying, quickly, some methods that will work against suicidal ideation almost the way penicillin works against bacterial infections like pneumonia, meningitis, and syphilis.
Part 1. Just how big is the “problem?” This series intends to tackle a range of subjects that afflict Veterans, especially suicide and drug overdoses which, along with diabetic lower limb amputations, are at epidemic levels. Across military medicine and traditional approaches to “mental health,” there is a wide gap between the palliative care model – control symptoms – and root cause analysis that gets at the physical damage and whole body wellness called for. This includes proper diagnoses and a shift to an appreciation of polytrauma and brain wound healing.
Part 2. Modern War is just so damned dangerous: BLAST Injury, Burn Pits, and the nature of whole body damage/polytrauma. Includes a primer on brain wounding.
Part 3. The VA/DoD Approach: Intrepid Center, DVBIC, Intrepid Spirit Centers, WRIICs, PREP, Care Coalitions, and Independent Wellness Centers.
Part 4. VSOs and the Growth of 66,000 Veteran Help Organizations since 9/11
Part 5. The insidious Service Member Epidemics: Suicide, Drug Overdosing, and diabetic foot ulcers, lower limb amputations, and the hundreds of thousands of deaths directly attributable to lack of informed consent.
Part 6. The Sports Industry: Making contact sports and life in general safer while engaging in a real scientific dialogue about brain wounding, the concussion cascade, "The Concussion Protocol,” and “the new normal” after brain wounding.
Part 7. Eisenhower didn’t even get it half right: The Military, Industrial, Contractor, Research, Academic, Lobbyist, Insurance, and Pharmaceutical Complex. Lessons in Bureaucratic Politics and how to sort out a path to success.
Part 8. Integrative/Functional/Wholistic/Complementary and Alternative Medicine. You don’t have to throw away institutions or current practices to make them better.
Part 9. Alternative Therapies: Hyperbaric Oxygen Therapy (HBOT) and a new paradigm in whole body healing.
Part 10. Alternative Therapies: Devices, Processes, Computers, and Artificial Intelligence.
Part 11. Alternative Therapies: Non-Prescription Drugs/ Psychedelics/Supplementation/Nutrition/Diet/Lifestyle.
Part 12. How to hold the Congress, White House, VA and DoD, and sports industry accountable for the Epidemics and lack of brain wound healing protocols.
Part 13. SUMMARY: The Shortest Paths to Success. How to change the language around “mental health,” arrest and reverse upward trends in deaths through suicides, prescription drug overdoses, lower limb amputations, and restore Quality of Life to brain wounded Veterans and citizens.
We welcome your comments.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#opioidepidemic#posttraumaticstressdisorder#PTSD#SuicidePrevention#TBI#traumaticbraininjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Text
Bad Trip: Expert says VA studies psychedelics but ignores proven Hyperbaric Oxygen Therapy!
Eye on Veterans
This week we’re talking with Dr. Robert Beckman, Executive Director of Treat Now dot org. He’s one of the premiere experts in the treatment of brain wounds with Hyperbaric Oxygen Therapy (HBOT). Although this technology is FDA approved for things like burns and diabetic foot ulcers, Beckman says the VA ignores proof that it's effective for treating brain wounds, TBI’s, concussions and depression which has fueled the suicide epidemic in America.
While ending suicide remains a top priority for VA , DoD, Beckman slams their decision to pump millions of mental health dollars into psychedelic research to merely treat symptoms. He offers several real-world examples of HBOT effectively treating the root cause and thus eliminating symptoms in ways current VA strategies do not.
In one powerful segment he shares how over the years the VA has amputated hundreds of thousands of feet, due to diabetic foot ulcers. Beckman claims most of which could have been avoided if HBOT was introduced earlier in their care.
He also shares vivid examples; NFL players treating concussions, combat veterans' fighting effects of toxic exposures and many clinics who are currently embracing HBOT therapy for treatment of brain wounds, PTSD and MS.
For more on Hyperbaric Oxygen Therapy including powerful research data and published studies, see TreatNow.org's website:
https://treatnow.org/
Read the latest newsletter "VA Continues to Avoid Treating and Healing Brain Wounds" here:
https://treatnow.org/va-continues-to-avoid-treating-and-healing-brain-wounds/
VIDEO: MSG Scott Rossler's HBOT testimony
https://youtu.be/N-CkR5shqEM?si=UmUhF_jKxPHjjzkq
VIDEO: NFL great Joe Namath shares how HBOT changed his life:
https://youtu.be/s7nxU3QadIA
To reach CBS Eye on Veterans, Host, Phil Briggs
[email protected]
Follow on X
@philbriggsVet
@EyeOnVeterans
Read the full article
#AirForce#ARMY#brainwound#brainwounds#concussion#currentevents#depression#HealingwithHyperbarics#marinecorps#military#MilitarySuicide#Navy#POLITICS#POPCULTURE#suicideepidemic#TBI#unitedstatesveterans#veteranaffairs#Veterans#VeteransAdministration
0 notes
Text
What the world knows that the VA does not: Hyperbaric Oxygen Therapy is safe, effective and can restore health

Athletes are waking up to the Use of Hyperbaric Oxygen Therapy for brain wound healing, health, endurance, peak performance, and the competitive edge.
Game Changer for Football Teams?
A high-profile college football program began using HBOT to manage player injuries and fatigue. The therapy quickly became a key factor in their injury management and prevention strategy. The team noted shorter recovery periods after injuries, and players were able to return to play faster than before, demonstrating HBOT's efficacy in a high-contact sports environment. Numerous professional athletes use HBOT.
100 Yards of Wellness Will Offer HBOT to Clemson Athletes
Nov 22, 2022
100 Yards of Wellness, Clemson’s new $4.9-million wellness space at Allen N. Reeves Football Complex that spans roughly 300 feet in length that has become a central hub of activity and major point of pride for Tiger football. The treatment and training room area includes all requisite athletic training resources, including a
diagnostic office with a full digital X-ray space and diagnostic ultrasound, general medical exam room, 30 yards of turf and hydrotherapy areas, including two underwater treadmills. Among the many features of the recovery center are:
• A hyperbaric chamber to create a pressurized environment for concentrated oxygen intake.
• A cryotherapy chamber for muscle recovery through extreme cold temperature exposure.
• A sensory deprivation float tank that houses 1,200 pounds of Epsom salt dissolved in water at skin temperature to remove athletes from light, sound and some gravitational force.
• Infrared hyperthermic Cocoon pods for Far-Infrared light therapy and vibrational massage.
• Photobiomodulation therapy beds that leverage multiple wavelengths of infrared light to reduce oxidative stress.
• Numerous massage chairs, including both percussive massage and hydromassage options.
• Percussive Hypervolt massage guns.
• Dedicated tables and space for practitioner-assisted stretching, percussive massage gun therapy and Normatec compressive sleeves provided to each player prior to the season.
• Functional testing equipment to obtain objective information on student-athlete muscle and joint function that can be used for injury prevention and return-to-play purposes.
The Rise of Hyperbaric Oxygen Therapy in Professional Football: A Game-Changer for Recovery and Performance
Sep 5, 2023
By Mudassir Sajad
In the fast-paced world of professional football, where every second counts, players are constantly seeking ways to gain a competitive edge. One such method that has been gaining traction is Hyperbaric Oxygen Therapy (HBOT). This innovative treatment has been endorsed by top-tier athletes like Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar, who have all been spotted on social media using hyperbaric chambers Hyperbaric Oxygen Therapy is proving to be a revolutionary treatment in the realm of
professional football. Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar endorsing its benefits, it's clear that HBOT is more than just a passing trend. Moreover as science continues to validate its efficacy, we can expect to see more football clubs
adopting this cutting-edge technology to give their players the competitive edge they need.
Dr. Joe Maroon on Hyperbaric Oxygen
Dr Joe Maroon Joseph Maroon is an American neurosurgeon, author, and triathlon athlete. He is the professor and vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center and is the current medical director of WWE. For over 20 years he has served as the neurosurgical consultant to professional and college athletes in football, baseball, golf, hockey and soccer and was team neurosurgeon to the Pittsburgh Steelers for over 40 years.
As early as 2011, Dr Maroon and Dr Bost wrote: "Alternative nonpharmaceutical treatments appear to be gaining acceptance for the treatment of common neurodegenerative conditions, memory decline, and reduced cognitive function. Substantial animal and human research now suggests that these same natural dietary supplements, vitamins and minerals, and the use of hyperbaric oxygen may be a better first-line choice for the treatment of PCS, which has generally been underreported by both athletes and the military."
Maroon and Bost, Concussion Management at the NFL, College, High School, and Youth Sports Levels. Clinical Neurosurgery. Volume 58, 2011, Chapter. 7.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
VA Continues to Avoid Treating and Healing Brain Wounds

2024 reminds us that the Veterans Administration continues off-course by avoiding actual brain wound healing while pumping more $$$$ into research, "Mental Health," and achieving a new normal. Meanwhile, the suicide rate continues upward.
ProPublica reports "How the VA Fails Veterans on Mental Health." In what has become an almost annual body count, investigative reporters analyzed 313 studies conducted by the VA's inspector general in recent years showing how repeated failures in behavioral care in the VA continue to lead to suicides.
"The problems appear to be systemic. Over and over, the hospitals and clinics in the VA’s sprawling health care network have fallen short when it comes to treating people with mental illness. . . . In the most extreme cases, facilities lost track of veterans or failed to prevent suicides under their own roofs."
Given the rise in the suicide rate among Veterans, the report veers into complicity when it states: "The system has notable strengths. The VA has played an important role in developing treatments for conditions such as post-traumatic stress disorder and traumatic brain injury, and provides critical training opportunities for psychiatrists, psychologists and social workers nationwide."
Combat Veterans constantly report to TreatNOW that they're treated like "guines pigs" by a constantly shifting and sketchy string of care providers. The ProPublica reporting indicates a severe breakdown in the VA's basic understanding of the physiology of brain wounds, repeating year after year that "mental health" is the issue. Recall that in too many cases the VA continues to insist on PTSD diagnoses for combat veterans without proof of brain damage.
And recruitment for understaffed medical professionals is for the Mental Health disciplines, not for a rethinking of how to properly diagnose and heal brain wounds. Physical healing has to replace psychology as the focus of standard of care for TBI.
And consider: The VA runs a number of War Related Illness and Injury Study Centers (WRIISC). This national program is dedicated to Veterans’ post-deployment health concerns and unique health care needs. They "develop and provide post-deployment health expertise to Veterans and their health care providers through clinical care, research, education, and risk communication. The WRIISC is part of VA’s newly designated Health Outcomes Military Exposures (HOME) formerly Post Deployment Health Services (PDHS). The VA is uniquely qualified to care for Veterans with health concerns related to potentially toxic exposures."
These Centers are allegedly the Gold Standard for delivering the world's best care for "the #1 clinical priority" in DOD and the VA: suicide prevention. But the protocols, research, and culture are opposed to even mentioning Hyperbaric Oxygen Therapy as even a consideration, let alone providing the treatment. At a minimum, they might consider putting some intellectual firepower behind a proper Phase 3 clinical trial to answer the outstanding questions about maximizing the efficacy of HBOT for Mild Traumatic Brain Injury Persistent Postconcussion Syndrome.
Days ago, the Department of Veterans Affairs issued an intention to study the use of certain psychedelic compounds in treating posttraumatic stress disorder (PTSD) and depression. The substances to be studied include psychedelic compounds such as psilocybin and Methylenedioxymethamphetamine (MDMA) when used in conjunction with psychotherapy to treat Veterans with PTSD and depression. This continues the VA's penchant to study "mental health" problems rather than solving them. As always, they revert to their inadequate interventions:
- Psychopharmacology
- Cognitive Processing Therapy (CPT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Prolonged Exposure (PE) or Trauma-Focused Psychotherapy
Adding yet more symptom-reduction chemicals and computer-based coping tools to the mix continues to avoid proper diagnosis and brain wound healing, particularly in the cases of combat veterans.
Here's the primer the VA needs to memorize. While this is not taught in medical schools, worldwide science supports these conclusions:
- TBI/Concussion/BLAST cause brain wounds.
- The pathophysiology of brain wounds includes a concussion cascade, a penumbra of damage that can lead to cell death and a host of behavioral, cognitive, memory and emotional problems. It is increasingly clear that CTE can be a result of this damage.
- Interrupting that cascade can halt and reverse the damage cause by inflammation, hypoxia, necrotic cell death, blood-brain barrier breakdown, and numerous other well-documented effects of brain wounding.
- Only by focusing on wound healing can a patient get on the path back to total body health, and a chance of pain- and drug-free living.
- Hyperbaric Oxygen Therapy (HBOT) is a proven, FDA on-label available intervention that reduces inflammation, leads to biogenesis, neurogenesis, angiogenesis, neuroplasticity, proliferation of stem cells, pain reduction, halts suicidal ideation, and allows patients to get off death-inducing drugs.
- Polytrauma -- a condition of multiple traumas endured by a patient -- is a complex of injuries typically suffered in BLAST injuries.
- Every Veteran with diagnosed or suspected brain wounds needs to be told that HBOT can help heal their wounds.
- And while the VA is waking up to the truth about healing vs. palliating, they should be required, under the mandate of "informed consent" to use HBOT for Diabetic Foot Ulcers.
- There are over 100,000 Veteran suicides since 9/11, and over 876,000 Veteran deaths attributable to lower limb amputations. The VA must be held accountable for using EVERY means available to stop the carnage.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#brainwounds#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#PTSD#suicide#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#VA#VeteranSuicide#VeteranSuicidePrevention#Veterans
0 notes
Text
CTE Plagues Heisman Trophy Winners and Families

Three-quarters of 1,035 brains of football players -- over 700
--examined at Boston University had CTE
The "taboo topic" is the centerpiece of "The Other Heisman Club" in the Washington Post, Dec 9, D1, by Kent Babb: the number of former Heisman winners with diagnosed or suspected Chronic Traumatic Encephalopathy (CTE). The degenerative brain disease is increasingly in the news for a number of reasons.
Four Heisman winners have been posthumously diagnosed with the disease: Howard Cassady, Pat Sullivan, Paul Hornung and Charles White. The implication in the article is that more winners already exhibit symptoms of CTE but whose families can't "know" until after death. But the families know.
Something is wrong. Sadly, silence is the preferred approach. And the unwillingness of our society to confront the obvious doesn't make it any easier. And the "whistling through the graveyard" approaches to concussions and the Concussion Protocols used worldwide don't provide much guidance about an alternative approach to Brain wounding. Facts matter:
- Four percent of Heisman trophy winners died of CTE, and the list of their wounded fellow winners is growing. If you extrapolate those numbers to the 25,000 former NFL players, over 1,000 of them are probably carrying the CTE markers.
- Three-quarters of 1,035 brains of football players, 0ver 700, examined at Boston University had CTE.
- Researchers at Boston University found CTE in 92 percent of former NFL players who were analyzed: they analyzed the brains of 376 deceased former NFL players and diagnosed 345 of them with chronic traumatic encephalopathy.
- More than half of the homeless have experienced traumatic brain injury and 1 in 4 have had moderate to severe brain injuries.
- Approximately 876,450 post-9/11 veterans suffer from untreated brain wounds.
- Researchers estimate that as many as 60% of incarcerated individuals are living with TBI, significantly higher than the 8.5% reported in the general population.
- Studies on prison and jail populations have reported a range of 25-87% of inmates reporting head injuries or TBI.
Of course, it is traditional to attack these numbers. Nay-sayers will demand more research. Hand-wringing by stake-holders on both sides will, like protests after mass-shootings, last a while and then subside. If anything, more dollars will go into researching how to make contact sports more safe. And treatments that are non-pharmaceutical will be ignored. Since "everyone knows there's no treatment for brain injuries," the best we can hope for from the medical profession is contained in the latest proceedings out of Boston.
The Robert C. Cantu Concussion Summit was held on December 8, 2023, at the Cantu Concussion Center at Emerson Hospital in Concord, MA. The theme of the conference was "Prevention of Concussion and Long-Term Effects of Repetitive Traumatic Brain Injury (RTBI)." In what is becoming a repetitive list of findings, the conference summarized:
- Eliminate intentional or avoidable head impact in contact and collision sports in both practices and games.
- Encourage policies and rules that limit the number, duration, and intensity of contact sport practices.
- Reinforce proper and safer techniques that avoid head contact at all levels of play.
- Implement rules of play that reduce and penalize intentional or avoidable contact to the head and neck.
- Correlating specific clinical symptoms with CTE neuropathology remains an important area for further investigation.
- Improve the criteria for Traumatic Encephalopathy Syndrome (TES) through further research.
Feel better? More importantly, if you are the parent of someone with a brain wound, what actionable intelligence can you take from that list? How will that list help you and yours deal with the here-and-now of a TBI/Concussion-suffering loved-one? If you'd like to learn more about what is happening, and what you can do, view this earlier Blog. Additional information is here.
Below is an insightful film about brain wounds
https://youtu.be/Zzbxrnm7jXc?si=IPKC5InadR0Eho52
https://treatnow.org/brain-wound-update-5-concussion-blast-tbi-cte/
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
NYT: Friendly Fire Leads to Brain wounding

Pentagon researchers say weapons like shoulder-fired rockets expose troops who fire them to blast waves far above safety limits, but they remain in wide use.
As we have reported for years, BLAST injury does not respect your nationality, gender, origin of the weapon, or your intention. As Dave Philipps of the New York Times reports, U.S. Troops are still training on weapons with known risks of delivering brain wounds.
As Phillips reports, studies by the Navy, the Center for New American Security, the Swedish military, DoD, SEALs, DARPA, Johns Hopkins, and UHUHS all warn of real damage inflicted by "friendly fire".
The search, research, measurements, data bases, added budgets, and periodic expressions of concern from DoD leadership can be viewed in one of two lights: they know and they don't care; or, they know and they dont' know what to do in the interim. Modern warfare, as Ukraine proves daily, requires more and more destructive firepower just to defend territory, let alone regain strategic and tactical advantage.
So, what can done in the interim? "For generations, the military assumed that this kind of blast exposure was safe, even as evidence mounted that repetitive blasts may do serious and lasting harm. . . . Top leaders talk of the importance of protecting troops’ brains, but the military fails to take practical steps to ensure safety."
Literature on BLAST injuries over the past decade overwhelmingly tends in the direction of Recommendations to find ways to protect soldiers with new and improved helmets, reduced weapon firings, education, more research, more funding, and, over time, resort to robots to do the heavy firing.
Sadly for the soldier, for 100 years we've known that BLAST causes brain wounds. Even though a century of research has not definitively "proved" the Mechanisms of Action involved in causing physical, mental, behavioral, cognitive, and moral damage, we do know that the net effects of only palliating symptoms won't lead back to a normal, healthy brain.
So here's a list of helpful suggestions to DoD/VA to help Warriors, Veterans, indeed anyone exposed to BLAST injury or brain wounding. Let all the research continue on mitigating the potential and actual damage caused by exposure to BLAST. Add more drugs and hallucinogenics and psychotropics to the list of possible "solutions." But let's focus some of our work on healing the wounds to the brain and body caused by BLAST exposure. An estimated 877,000 Veterans and active duty service members -- probably many more as we learn about the pervasiveness of self-inflicted BLAST injury -- are already suffering with some degree of brain wounding. Let's focus on HEALING THEIR BRAIN WOUNDS as we work the prevention side of the equation. Here's a modest proposal:
Daily suicide rates, accumulating suffering, and impacts on families demand that we deal with brain wounds. We cannot continue to ignore treatments that work are safe, scientifically validated, and readily available. We cannot hide this information from the wounded. Informed consent and medical ethics demand that DOD/VA tell the wounded what is available, even though it is "off-label." Every treatment, drug, process, procedure, device and protocol currently used by DoD/VA is off-label and not approved by the FDA for treating TBI/PTSD.
Keep doing what you're doing. But hold open the possibility that alternative therapies exist that are scientifically valid, clinically proven, widely available, cost effective and demonstrated safe and effective. Fund them.
Rethink a Suicide Prevention Strategy that is void of any options to treat brain wounds. Too may Veterans commit suicide -- over 109,000 -- perhaps falling into depression from undiagnosed and untreated brain wounds.
Hyperbaric Oxygen Therapy (HBOT) is one such therapy, backed by decades of research, acceptance by the FDA for wound healing, and proven in multiple scientific studies to reduce or eliminate symptoms caused by TBI/PTSD/Concussion/BLAST.
HBOT is proven to reduce and/or eliminate suicidal ideation in tens of thousands of uses .
Read, really read, the current scientific literature on the validity of objective research conducted over the past fifteen years. Notice that the UHMS and the overwhelming number of real HBOT researchers know that HBOT works to help heal TBI/PTSD. Even government researchers, a few of whom still cling to the canard that "HBOT does not work," accept that patients in their studies got better .
If necessary, take 10% of the VA drug budget and use it to fund HBOT treatments in private clinics where the cost is miniscule compared to current standards of care. It is a well-known fact that fully treated HBOT patients get off almost all their drugs, many of which warn of "ideation of suicide." There will be a net return of billions of dollars to the VA bottomline due to reduced need for prescriptions.
Redo your cost analyses when considering where to spend dollars on rehabilitation of brain wounded combat Veterans. It has been calculated that the cost of NOT treating brain wounded Veterans will exceed $4Trillion over their 40-year lifespan. That's a degraded life, for the Veteran and the family, living with symptoms that plague far too many Veterans. For less than 1/2 of 1% of that cost, all 877,450 brain-wounded Veterans can be fully treated with HBOT.
DoD and the VA should insure and reimburse HBOT-for-TBI treatments. Start with Informed Consent: let every Veterans know that HBOT can help heal their brain wound.
And consider the following: service members returning from combat suffer from polytrauma unlike ever before. Knowing what we know now about the prevalence of BLAST injury, Burn Pit toxins, unreported brain trauma, the sustained pace of combat for Special Operations warriors, we need to provide functional medicine approaches to whole body wellness, starting with but not limited to brain wounds. All body systems are negatively affected by BLAST. HBOT works to relieve pain, reduce inflammation, speed healing, restore function, promote the growth of new stem cells, and allow battle-weary warriors to return to peak performance more quickly.
Part of the history of HBOT is that the history of HBOT safety and efficacy is ignored or forgotten. This is a page out of the Textbook of Military Medicine, updated in 2006. This same algorithm is in the textbook in the 1980s. The “definitive therapy” then and is HBOT treatment for TBI resulting from BLAST Exposure.

The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#concussionprotocol#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaric#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#posttraumaticstressdisorder#PTSD#suicidalideation#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#TraumaticBrainInjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Text
BRAIN WOUND UPDATE #16: More Evidence: Untreated TBI ties to Cardiovascular, Endocrine, Neurological, and Psychiatric Disorders

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
"There comes a point where we need to stop just pulling people out of the river. We need to go upstream and find out why they're falling in."
Bishop Desmond Tutu
At some point, DoD, the VA, and medicine in general will hear the drumbeat of data in peer-reviewed science attesting to the damage done by untreated brain wounds. Fortunately for those lucky few, the role of Hyperbaric Oxygenation to help treat and heal their brain wounds has given them new lives. But the practitioners of conventional medicine are not ready to accept facts and evidence. The DOD and the VA claim that the suicide epidemic is their #1 clinical priority, yet they drag their feet, avoiding using HBO therapy that virtually eliminates suicidal ideation. And they seem not to have read recent science about symptoms and "mental health" diagnoses that mask undiagnosed brain wounds. While the suicide epidemic continues to escalate, DOD and the VA spend more and more on strategies to think harder, collaborate more, pay attention, fund more Call Centers, and get the word out: precious little on healing brain wounds.
Consider these recent reports.
This report in JAMA, Association of Traumatic Brain Injury With the Risk of Developing Chronic Cardiovascular, Endocrine, Neurological, and Psychiatric Disorders, found that patients with mTBI and msTBI were at increased risk of developing long-term cardiovascular, endocrine, psychiatric, and neurological comorbidities. The risk of post-TBI comorbidities was higher in all age groups compared with an age-, sex-, and race-frequency–matched unexposed group, and notably so in patients younger than 40 years. Comorbidities after TBI were associated with higher mortality.
Another JAMA study, Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts, found that young contact sport athletes may be at risk for long-term neuropathologic disorders, including chronic traumatic encephalopathy (CTE). This one bears reading by parents.
A third study in the New England Journal of Medicine, Neuro-degenerative Disease Mortality among Former Professional Soccer Players, found that mortality from neurodegenerative disease was higher and mortality from other common diseases lower among former Scottish professional soccer players than among matched controls. Dementia-related medications were prescribed more frequently to former players than to controls.
And an ironic report from Front Office Sports, the NFL court drama shows how little we've progressed from science-scepticism. In a bid to avoid reimbursing the NFL for payouts to brain wounded players, major insurers deployed medical experts to argue that there’s no scientific evidence linking head injuries with neurocognitive disorders, such as Amyotrophic Lateral Sclerosis (ALS), Alzheimer’s, and Parkinson’s, covered in the settlement. They further suggested that up to 40% of the now 1,663 former players who have received payments may have overstated and even feigned their symptoms.
This tactic is mirrored in the behavior of DOD components that continue to discard combat veterans with the National Guard with Other Than Honorable Discharges and claims that the petitioners either weren't on active duty when they were injured, can't document injuries they were encouraged to not report to stay in the fight, or are faking their injuries.
Of the five Defense Department service branches, only two met their active-duty enlisted recruiting goals for fiscal 2023 -- the Marine Corps and the Space Force, by far the smallest services and with the lightest recruiting burden. The others, the Army, Air Force and Navy, fell short. Coincidence?
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#CardiovascularDisorder#concussion#ConcussionSymptoms#EndocrineDisorder#HBOT#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#NeurologicalDisorders#PsychiatricDisorders#TBI#TBItreatment#TraumaticBrainInjury#Veterans
0 notes
Text
BRAIN WOUND UPDATE #14: Research Reveals Potential Links from Brain Wounds to Parkinson's and CTE

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
New data validates an association between trauma-related disorders and the development of Parkinson's disease in military veterans
International Parkinson and Movement Disorder Society
27 Aug, 2023
COPENHAGEN, Denmark, Aug. 27, 2023 /PRNewswire-PRWeb/ --
In a study of nearly 360,000 military veteran records released earlier this year in the Movement Disorders journal, researchers provide evidence that traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD), both trauma-related disorders, are risk factors for Parkinson's disease (PD).
While this correlation has long been suspected, the results of this study validate the hypothesis with the researchers' case-controlled approach and consideration of comorbidities. This study further suggests that these common war-related illnesses may ignite biochemical changes that precede and fuel the development of Parkinson's disease decades later.
"While a link between head trauma and the later emergence of Parkinson's has been widely accepted for some time, this paper is of interest for several reasons," said Dr. Jon Stoessl, University of British Columbia and editor of the Movement Disorders Journal. "Similar to a prior report (White et al., Ann Neurol 2020), the authors have identified an independent and synergistic link between PTSD and PD. They examined a large cohort (nearly 72,000 cases and nearly 290,000 matched controls from the VA database), used a minimum lag time of 5 years between exposure and PD diagnosis, and have gone back as long as 60 years prior to the emergence of PD. Applying an unusual degree of rigor for this type of research, the authors ascertained a diagnosis of PD based on chart review by a movement disorders specialist in addition to administrative (diagnostic code and prescription) data. They furthermore restricted the definition of TBI and PTSD to events that occurred during active military service. The odds ratio (OR) for PD in those with TBI range from 1.5-2.0 (depending upon time of exposure) and for PTSD, the OR was 1.7-1.8. The findings not only confirm the importance of earlier TBI as a risk factor for later PD, but also point to the independent and synergistic importance of PTSD in future neurodegeneration. The findings thus have important implications for understanding the pathogenesis of PD and for the consideration of novel preventative and disease modifying approaches."
##########
In two related stories, links between footbal concussions and subconcussive hits and brain damage were studied. In the first study, comparing volleyball and football players, advanced MRI scans showed significantly divergent microstructural brain changes among college football players, particularly those who experienced concussive blows, and college volleyball players over four years.
“This study highlights the important role of white matter, which is not always fully appreciated in neurologic disease. We know that, during normal development, brain white matter increases in volume until a person reaches the mid-40s,” he said. “We see here that football, in particular, affects white matter development compared with volleyball; in addition, severity of brain injury is relevant because football players who experienced concussions had more damage than those who only had subconcussive blows. This observation supports the idea that there is a form of head injury somewhere between a concussion and no injury at all.”
In the second study, researchers leveraged football accelerometer data to quantify associations between repetitive head impacts and chronic traumatic encephalopathy (CTE) in males. The findings implicate cumulative head impact intensity in CTE pathogenesis. Years of football played is positively associated with CTE pathology.
A total of 631 brain donors who played American tackle football were included in the study. . . . On average, athletes died at 59.7 years old and played 12.5 years of football. 180 athletes (29%) did not have CTE, 163 (25%) had low-stage CTE (Stage I or II), and 288 (47%) had high-stage CTE (Stage III or IV).
Science is cumulative. Data help "prove" hypotheses. Testing and research and observed outcomes advance our understanding of cause and effect. Our experience and 20 years of research on brain wounds/TBI/PTSD show both negative consequences of brain wounds, from any source, and the positive effects of using Hyperbaric Oxygen Therapy to help heal those brain wounds.
Healing brain wounds and arresting suicidal ideation is akin to polio vaccine. About 16,000 cases of polio (paralytic poliomyelitis) occurred each year in the U.S. in the 20th century compared with none in 2020. In over 21,000 cases where patients received a full course of HBOT treatment, the record of success in avoiding suicide is over 99%.
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussionSymptoms#CTE#HBOT#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#Parkinson#ParkinsonDisease#posttraumaticstressdisorder#PTSD#TBI#TBItreatment#TraumaticBrainInjury#Veterans
1 note
·
View note
Text
BRAIN WOUND UPDATE #13: Holistic Total Force Fitness to Maximize Performance

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
A senior retired US Navy SEAL officer has weighed in with a six part justification for ACTION to fight suicide. His remarks relate to short- and long-term needs for dealing with force readiness amidst known challenges in the SpecOps community. His remarks are in concert with the Interview with the Senior Enlisted Advisor to the Chairman of the Joint Chiefs of Staff (SEAC), Ramón Colón-López that follows his remarks.
**************
Holistic Total Force Fitness to Maximize Performance
1. The M16A2 was discarded in SOF beginning in 1992 with the introduction of the CAR-15 and M-4 in the early 90’s. I was witness to that. The shortened barrels were, to say the least, "most noticeable", and in live fire drills, the concussive forces were enhanced around operators. Conventional forces did not receive these shortened rifles until circa 2010 in response to the need for shortened barrels in urban combat, which then also exacerbated the concussive forces during CQB operations in rooms. Constant exposure to shoulder-fired rockets, mortar, and artillery fire added to the cumulative effects. This is to say nothing about the constant exposure to IED blast waves, which, were the most injurious, and close-air support blast waves. All those constantly exposed to these concussive forces over multiple deployments will have physiological effects, lending to the neurological.
2. TBI, given the above, is akin to Decompression Sickness, physiologically, again lending to the neurological issues. Research has documented the evidence. The Textbook of Military Medicine, the volume entitled Ballistics, Blasts and Burn Injuries, has an algorithm on page 313. It is entitled Neurological Abnormalities in the Blast Casualty. HBOT is identified as definitive as treatment option.
3. This is not to discount the need for counseling; however, as I discussed with seniors, any operator, SOF or otherwise, who seeks help for TBI and suicidal ideation, is often stigmatized. It is akin to one seeking help for a perceived alcohol problem. We have witnessed those men and women immediately being separated from their comrades, which is in itself harmful, and the same appears to be the case for this issue. Rather, the solution should be immediate treatment with HBOT while still “on-the-line”, or, taken “off-line” as one would be for any illness while still retaining group and billet status. For any SOF operator, especially, referring to this in that light also de-stigmatizes the problem.
4. HBOT should be a health maintenance issue to deal with the prevalent and cumulative concussive forces from live fire in all forms. As an aside, HBOT would also assist in treatment according to the recently passed “burn pit” legislation. All warfighters are also subjected to the noxious gasses from carbines, rockets, artillery, along with the very nasty particulate matter encountered in AFG and Iraq. This is a readiness issue.
5. HBOT should be proffered by our health professionals as a performance enhancement issue. Olympic and professional athletes utilize HBOT for this reason. SOF operators, especially, will be lining up to enhance their performance. TBI and/or residual effects could then heretofor be corrected in a positive light. Overall, though, this is a combat enhancement and effectiveness issue.
6. One must ask why hyperbaric environments are questioned for TBI when it is considered medical protocol when dealing with Decompression Sickness (DCS) and Arterial Gas Embolism (AGE), wound ostomy, diabetic neuropathy, hearing and vision loss, radiation injuries, CO and airborne particulate poisoning, severe bone and skin infections, trauma from force or pressure on a body part.
Lastly, the constant exposure and cumulative effects to these blast waves, and the more acute exposure to the higher pressure waves in IEDs, etc, have the same effects as head trauma/ concussions in sports. Football legend Joe Namath has had his concussion injuries healed by 120 treatments of HBOT. His testimony is available on YouTube, and, he is the proponent for chambers being emplaced in stadiums for immediate treatment in concussion protocol.
****************
Interview with Senior Enlisted Advisor to the Chairman of the Joint Chiefs of Staff (SEAC), Ramón Colón-López.
The Military Heath System, together with DoD's Traumatic Brain Injury Center of Excellence, interviewed SEAC. Highlights are consistent with remarks above.
The Warfighter Brain Health (WBH) Initiative is a joint effort between operational and medical communities with the focus to optimize warfighter brain health, immediately detect brain injury when it occurs and combat its effects on warfighters, their families, line leaders/commanders, and their communities at large.
WBH is defined as the physical, psychological, and cognitive status that affect a warfighter's capacity to function adaptively in any environment, and impacts readiness, operational capability, mission effectiveness, and the goal to achieve overmatch or superior lethality
MISSION: Act rapidly to provide products, practices, and policies to directly impact warfighter brain health and performance. Due to experience and realities across the community, a major emphasis is to understand the implications of blast overpressure (include underwater and subterranean exposures); blunt force trauma; high G acceleration/ vibration/ recoil; incoming/ near missed impact (e.g. ballistic missiles); ballistic projectiles; directed energy (e.g., electromagnetic fields (EMF) and UV radiation); chemical-biological-gas toxins; and other environmental hazards.
SEAC defined "resiliency" as the threshhold for misery. No matter how resilient a warrior, symptoms keep coming. Slowed thinking, reactions, memory lapses, pain, reduced energy degrade readiness and ability to perform at peak levels.
The Comprehensive Strategy for Warfighter Brain Health Initiative 2018 study on the effects of low level blasts, section 734, calls for more efforts to confront effects of Blast.
SEAC referred to "the 3 greys":
- grey area of new operational environment: conventional peer-to-peer has given way to unconventional warfare
- grey area of grey steel deterrence: ships, missiles, aircraft are evolving to leverage the revolution in military and technical breakthroughs.
- grey matter: human performance, intellect, speed of response, judgement. In this last insight, SEAC calls on the Services to pay as much attention to restoration of the human as to the weapons and the doctrine. Degraded Warriors imperil our ability to prevail.
NOTE: Hyperbaric Oxygen Therapy (HBOT) meets and exeeds the challenge implicit in SEAC's challenge: Identify evidence-based cognitive and physical performance restoration treatments.
****************
Worth Reading
** In the largest study of neurodegenerative disease from Boston University’s CTE Center, sixty-three out of the 152 donated brains (41%) had autopsy-confirmed CTE. All cases were athletes under the age of 30 at the time of their death. The majority were amateur athletes (71.4%).
The report, published in JAMA Neurology on 28 AUG 2023 describes the features of 152 brains donated between February 1, 2008, and September 31, 2022, to the UNITE brain bank — the largest tissue repository in the world focused on traumatic brain injury and CTE.
Most of the donors analyzed played football (60%), followed by soccer (15%) and ice hockey (10%). Other sports implicated were amateur wrestling, rugby and professional wrestling.
The study shows that 87 of the 152 donors died by suicide, including 33 donors who also had CTE. Dr McKee noted: “The most common cause of death across the board, whether they had CTE or not, was suicide, followed by accidental overdose.” McKee adds that the longer someone plays football, in particular, their risk of developing CTE doubles every 2.6 years.
ALSO OF NOTE: The healthcare costs of TBI, driven by cost prices and the healthcare consumption of patients, will cause major economic and societal challenges, as estimates indicate the worldwide annual economic burden of TBI to be US $400 billion dollars, which is 0.5% of the gross world product.
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#concussionprotocol#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#Holistic#hyperbaric#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#posttraumaticstressdisorder#PTSD#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#TraumaticBrainInjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Text
Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts

August 28, 2023
Ann C. McKee, MD1,2,3,4,5,6,7; Jesse Mez, MD, MS2,3; Bobak Abdolmohammadi, BA2; et alMorgane Butler, BSc2,8; Bertrand Russell Huber, MD, PhD1,2,3,5,6; Madeline Uretsky, MS2; Katharine Babcock, PhD2,8; Jonathan D. Cherry, PhD1,2,4; Victor E. Alvarez, MD1,2,3,5; Brett Martin, MS2,9; Yorghos Tripodis, PhD2,7,9; Joseph N. Palmisano, MS2,9; Kerry A. Cormier, BA1,2,5; Caroline A. Kubilus, BA2,5; Raymond Nicks, MS1,2,3,5; Daniel Kirsch, BA2,4; Ian Mahar, PhD2; Lisa McHale, EdS2,10; Christopher Nowinski, PhD2,10; Robert C. Cantu, MD2,10,11,12; Robert A. Stern, PhD2,3,12; Daniel Daneshvar, MD, PhD2,13; Lee E. Goldstein, MD, PhD2,14,15; Douglas I. Katz, MD3,16; Neil W. Kowall, MD2,3; Brigid Dwyer, MD3,16; Thor D. Stein, MD, PhD1,2,4,5; Michael L. Alosco, PhD2,3
Author Affiliations Article Information
JAMA Neurol. Published online August 28, 2023. doi:10.1001/jamaneurol.2023.2907
Audio (16:39)
Neuropathologic and Clinical Findings in Athletes With Repetitive Head Impacts
Key Points
Question What are the neuropathologic and clinical findings in a convenience sample of young, deceased, symptomatic contact sport athletes?
Findings In this case series of 152 contact sport athletes younger than 30 years at the time of death, chronic traumatic encephalopathy (CTE) was found in 63 (41.4%), with nearly all having mild CTE (stages I and II). Neuropathologic abnormalities associated with CTE included ventricular enlargement, cavum septum pellucidum, thalamic notching, and perivascular pigment–laden macrophage deposition in the frontal white matter.
Meaning These findings confirm that CTE and other brain pathologies can be found in young, symptomatic contact sport athletes, but the clinical correlates of these pathologic conditions are uncertain.
Abstract
Importance Young contact sport athletes may be at risk for long-term neuropathologic disorders, including chronic traumatic encephalopathy (CTE).
Objective To characterize the neuropathologic and clinical symptoms of young brain donors who were contact sport athletes.
Design, Setting, and Participants This case series analyzes findings from 152 of 156 brain donors younger than 30 years identified through the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Brain Bank who donated their brains from February 1, 2008, to September 31, 2022. Neuropathologic evaluations, retrospective telephone clinical assessments, and online questionnaires with informants were performed blinded. Data analysis was conducted between August 2021 and June 2023.
Exposures Repetitive head impacts from contact sports.
Main Outcomes and Measures Gross and microscopic neuropathologic assessment, including diagnosis of CTE, based on defined diagnostic criteria; and informant-reported athletic history and informant-completed scales that assess cognitive symptoms, mood disturbances, and neurobehavioral dysregulation.
Results Among the 152 deceased contact sports participants (mean age, 22.97 years; 141 male) included in the study, CTE was diagnosed in 63 (41.4%; median age, 26 years). Of the 63 brain donors diagnosed with CTE, 60 (95.2%) were diagnosed with mild CTE (stages I or II). Brain donors who had CTE were more likely to be older (mean difference, 3.92 years; 95% CI, 2.74-5.10 years) Of the 63 athletes with CTE, 45 (71.4%) were men who played amateur sports, including American football, ice hockey, soccer, rugby, and wrestling; 1 woman with CTE played collegiate soccer. For those who played football, duration of playing career was significantly longer in those with vs without CTE (mean difference, 2.81 years; 95% CI, 1.15-4.48 years). Athletes with CTE had more ventricular dilatation, cavum septum pellucidum, thalamic notching, and perivascular pigment-laden macrophages in the frontal white matter than those without CTE. Cognitive and neurobehavioral symptoms were frequent among all brain donors. Suicide was the most common cause of death, followed by unintentional overdose; there were no differences in cause of death or clinical symptoms based on CTE status.
Conclusions and Relevance This case series found that young brain donors exposed to repetitive head impacts were highly symptomatic regardless of CTE status, and the causes of symptoms in this sample are likely multifactorial. Future studies that include young brain donors unexposed to repetitive head impacts are needed to clarify the association among exposure, white matter and microvascular pathologic findings, CTE, and clinical symptoms.
Introduction
Across the world, millions of people are exposed to repetitive head impacts (RHIs) through participation in contact and collision sports, military service, physical violence, and many other activities.1-6 Repetitive head impacts can result in symptomatic concussions and the much more frequent, nonconcussive injuries that are asymptomatic.7 Sustained exposure to RHIs can produce persistent cognitive and neuropsychiatric symptoms8-11 and a progressive, tau-based neurodegenerative disease, chronic traumatic encephalopathy (CTE).12-21 Multiple studies13,15,22 link a longer duration of RHI exposure in US football players with increased odds for the presence of CTE and increased severity of CTE. In older American football players with pathologically diagnosed CTE, RHI exposure is also associated with white matter rarefaction,23-25 loss of myelin associated proteins,26 and oligodendrocyte loss.27 Emerging data show structural white matter alterations on magnetic resonance imaging (MRI) in young, active, and recently retired contact sport players exposed to RHI,1,2,28-30 although the pathologic condition underlying these changes is unclear.
A definitive diagnosis of CTE requires neuropathologic evidence of perivascular hyperphosphorylated tau (p-tau) aggregates in neurons, with or without astrocytes, typically at the depths of the sulci in the cerebral cortex.31,32 The clinical syndrome associated with CTE is known as traumatic encephalopathy syndrome (TES).8,33 On the basis of the National Institute of Neurological Disorders and Stroke (NINDS) consensus diagnostic criteria for TES,8 the core clinical features of TES include cognitive impairment, especially episodic memory and executive dysfunction, and neurobehavioral dysregulation, such as impulsivity, explosivity, and emotional dysregulation.8 Supportive features include delayed onset (ie, core clinical features starting years after RHI exposure ends), parkinsonism, other motor signs (including amyotrophic lateral sclerosis), depression, anxiety, apathy, and paranoia.
The Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Brain Bank1 has harvested brains from more than 1350 donors exposed to RHIs who are considered at risk for CTE. Brain donors in the UNITE bank vary widely in age at death and include teenagers and young adults. Chronic traumatic encephalopathy has been reported in individuals as young as 17 years,13 yet, to date, there have been no large-scale neuropathologic and clinical studies of young individuals exposed to RHIs. Attention to this age group has several important implications. The study of young athletes allows insight into the earliest features of RHI-induced neuropathologic injury and CTE. Furthermore, it allows analysis in the absence of common age-associated comorbidities. Moreover, most of these young contact sport athletes played only at amateur levels, as part of teams affiliated with educational institutions; consequently, the study of young athletes adds to our understanding of the long-term consequences of amateur contact sports participation. In this report, we describe the neuropathologic and clinical features of 152 brain donors from the UNITE brain bank who were younger than 30 years at the time of death.
Methods
Brain Donors and Study Design
The initial sample for this case series included 156 deceased individuals with a history of exposure to RHIs from contact sports participation who donated their brain to the UNITE Brain Bank from February 1, 2008, to September 31, 2022, and were younger than 30 years at the time of death. Race was determined by next-of-kin report and was included to understand the representativeness of the sample and the associated generalizability of the results. Procedures of brain donation have been previously described.14,34 The inclusion criterion was based on the presence of a history of exposure to RHIs without regard to symptom status. The restriction to brain donors younger than 30 years was selected to minimize any contribution from age-related conditions. Donors were excluded for poor tissue quality. Four donors were excluded because of incomplete brain fragments or prolonged premortem hypoxia, resulting in a final sample size of 152. Institutional review board approval for brain donation, postmortem clinical record review, interviews with informants, and neuropathologic evaluation was obtained through the Boston University Medical Campus and the Veterans Affairs Bedford Institutional Review Board. The next of kin or legally authorized representative of each brain donor provided written informed consent. The methods for this report followed the appropriate use and reporting of uncontrolled case series in the medical literature reporting guidelines.35
Neuropathologic Evaluation
Neuropathologic evaluation occurred blinded to the clinical evaluation by neuropathologists (A.C.M., B.R.H., V.E.A., and T.D.S.). Pathologic processing and evaluation were conducted using previously published methods and as described in the eAppendix in Supplement 1.12-14,34,36 Neuropathologic diagnoses were made using NINDS National Institute of Biomedical Imaging and Bioengineering criteria for CTE31,32 and well-established criteria for other neurodegenerative diseases.37-40 The CTE p-tau pathologic findings were classified into 4 stages using the McKee staging scheme for CTE.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
BRAIN WOUND UPDATE #12: Links Between TBI/PTSD and Parkinson's Disease in Military Veterans

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
New data validates an association between trauma-related disorders and the development of Parkinson's disease in military veterans
International Parkinson and Movement Disorder Society
27 Aug, 2023
In a study of nearly 360,000 military veteran records released earlier this year in the Movement Disorders journal, researchers provide evidence that traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD), both trauma-related disorders, are risk factors for Parkinson's disease (PD).
COPENHAGEN, Denmark, Aug. 27, 2023 /PRNewswire-PRWeb/ -- In a study of nearly 360,000 military veteran records released earlier this year in the Movement Disorders journal, researchers provide evidence that traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD), both trauma-related disorders, are risk factors for Parkinson's disease (PD).
While this correlation has long been suspected, the results of this study validate the hypothesis with the researchers' case-controlled approach and consideration of comorbidities. This study further suggests that these common war-related illnesses may ignite biochemical changes that precede and fuel the development of Parkinson's disease decades later.
"While a link between head trauma and the later emergence of Parkinson's has been widely accepted for some time, this paper is of interest for several reasons," said Dr. Jon Stoessl, University of British Columbia and editor of the Movement Disorders Journal. "Similar to a prior report (White et al., Ann Neurol 2020), the authors have identified an independent and synergistic link between PTSD and PD. They examined a large cohort (nearly 72,000 cases and nearly 290,000 matched controls from the VA database), used a minimum lag time of 5 years between exposure and PD diagnosis, and have gone back as long as 60 years prior to the emergence of PD. Applying an unusual degree of rigor for this type of research, the authors ascertained a diagnosis of PD based on chart review by a movement disorders specialist in addition to administrative (diagnostic code and prescription) data. They furthermore restricted the definition of TBI and PTSD to events that occurred during active military service. The odds ratio (OR) for PD in those with TBI range from 1.5-2.0 (depending upon time of exposure) and for PTSD, the OR was 1.7-1.8. The findings not only confirm the importance of earlier TBI as a risk factor for later PD, but also point to the independent and synergistic importance of PTSD in future neurodegeneration. The findings thus have important implications for understanding the pathogenesis of PD and for the consideration of novel preventative and disease modifying approaches."
About the 2023 MDS International Congress of Parkinson's Disease and Movement Disorders®: The MDS International Congress is the premiere annual event to advance the clinical and scientific discipline of Movement Disorders, including Parkinson's disease. Convening thousands of leading clinicians, scientists and other health professionals from around the globe, the International Congress will introduce more than 1,800 scientific abstracts and provide a forum for education and collaboration on latest research findings and state-of-the-art treatment options.
About the International Parkinson and Movement Disorder Society:
The International Parkinson and Movement Disorder Society® (MDS), an international society of more than 11,000 clinicians, scientists, and other healthcare professionals, is dedicated to improving patient care through education and research. For more information about MDS, visit http://www.movementdisorders.org.
Media Contact
Shea Higgins, International Parkinson and Movement Disorder Society, 1 (414) 276-2145, [email protected], mdscongress.org
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#Parkinson#ParkinsonDisease#posttraumaticstressdisorder#PTSD#TBI#TBItreatment#TraumaticBrainInjury#Veterans
0 notes
Text
BRAIN WOUND UPDATE #11: Suicide Risk, Mental Health and Military TBIs

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
Associating Military-Related Traumatic Brain Injury (TBI) With New-Onset Mental Health Conditions and Suicide Risk
A new JAMA study sought an answer to this Question: Is military-related traumatic brain injury (TBI) associated with increased incidence of new-onset mental health conditions and suicide risk?
Findings. In this cohort study, individuals with a history of military-identified TBI had significantly higher rates of new-onset mental health conditions than those without TBI. Increased risk for suicide was associated indirectly (through new-onset mental health diagnoses) and directly with history of TBI.
Meaning. These findings suggest that conceptualizing exposures (physical, psychological) as events that accumulate over an individual’s lifetime and increase risk for negative outcomes (eg, suicide) may assist in identifying mechanisms underlying frequently co-occurring conditions, as well as evidence-based interventions.
Importance. Research to identify the direct and indirect associations of military-related traumatic brain injury (TBI) with suicide has been complicated by a range of data-related challenges.The major objective was to identify differences in rates of new-onset mental health conditions (ie, anxiety, mood, posttraumatic stress, adjustment, alcohol use, and substance use disorders) among soldiers with and without a history of military-related TBI and to explore the direct and indirect (through new-onset mental health disorders) associations of TBI with suicide.
In this longitudinal cohort study of 860,892 soldiers, rates of new-onset mental health conditions were higher among individuals with a history of TBI compared with those without. Moreover, risk for suicide was both directly and indirectly associated with history of TBI. These findings suggest that increased efforts are needed to conceptualize the accumulation of risk associated with multiple military-related exposures and identify evidence-based interventions that address mechanisms associated with frequently co-occurring conditions.
*******************
In another story, researchers have gained new insight on how the brain can repair itself post-stroke. Functional decline after an ischaemic stroke is a common experience for patients, especially due to the brain’s resistance to regenerate after damage. However, there is still potential for recovery as surviving neurons can activate repair mechanisms to limit and even reverse the damage caused by the stroke. The question this study looked to answer is how is it triggered?
Researchers from Tokyo Medical and Dental University (TMDU) provided new insight to this question by identifying a new mechanism. They discovered that neurons surrounding the area of cell death secrete lipids that can trigger brain-autonomous neural repair after ischaemic brain injury.
An ischaemic stroke occurs when the blood supply to the brain is blocked and results in the death of brain cells. This condition is life-threatening, and patients will likely develop functional disabilities. Although the adult brain can self-repair, the underlying mechanisms need further clarification.
Inflammation of the brain contributes to the effects of ischaemic stroke. Senior author, Takashi Shichita, says: “There is evidence that more lipids are produced after tissue injuries and contribute to regulating inflammation. “We investigated the changes in lipid metabolite production in mice after ischaemic stroke. Interestingly, the levels of a specific fatty acid called dihomo-γ-linolenic acid (DGLA) and its derivatives increased after the stroke.”
*******************
Lastly, Jeremy Renner, he of HURT LOCKER and AVENGER fame, and other roles, is taking HBOT treatments twice a day following his hellacious crushing on Jan 1 by his own snowplow.
“Hyperbaric chamber, 2 atmosphere pressure, high oxygen, 2x daily,” the Hawkeye star wrote....... According to the article: "In addition to injuries, hyperbaric oxygen therapy can be used to treat other medical conditions like burns, severe anemia, carbon monoxide poisoning, radiation injuries, traumatic brain injuries, and more. It is also commonly used for treating scuba and deep-sea divers affected by the rapid pressure change."
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#concussionprotocol#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaric#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#posttraumaticstressdisorder#PTSD#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#TraumaticBrainInjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Text
BRAIN WOUND UPDATE #10: AVIV Clinic Press Release: Review of Scientific Basis of HBOT for TBI

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
ORLANDO, Fla., Aug. 01, 2023 (GLOBE NEWSWIRE) -- Aviv Clinics, one of the most advanced brain clinics in the world, shares the results of a new comprehensive literature review that shows hyperbaric oxygen therapy (HBOT) should be recommended as an effective therapy for patients suffering with chronic mild traumatic brain injury (TBI). Chronic mild traumatic brain injury occurs when symptoms from a mild traumatic brain injury are prolonged and last for more than six months.
The literature review, The efficacy of hyperbaric oxygen therapy in traumatic brain injury patients: literature review and clinical guidelines, was conducted by the Sagol Center for Hyperbaric Medicine and Research at Shamir Medical Center, Tel Aviv University and University of Pittsburgh Medical Center’s neurosurgery department, and published in the official journal of the European Society of Medicine, Medical Research Archives.
The literature review evaluated articles and human clinical trials data from 1969 to April 2023 that provided detailed information on the type of HBOT treatment and clinical outcomes. The articles were categorized into acute-subacute traumatic brain injury and chronic traumatic brain injury and evaluated by HBOT experts and esteemed research leaders Dr. Shai Efrati, director of the Sagol Center and co-founder of Aviv Scientific; Dr. Amir Hadanny, chief medical officer at Aviv Scientific and chief medical research officer at the Sagol Center; and Dr. Joseph Maroon, vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center.
The literature review concluded that HBOT should be recommended for chronic traumatic brain injury for a selected group of patients suffering from prolonged post-concussion syndrome (PPCS) who have clear evidence of metabolic dysfunctional brain regions and who have been properly evaluated by standardized cognitive tests and functional brain imaging. Evidence involved in the review, including seven randomized controlled trials and six prospective studies, suggested significant improvement in cognitive function, symptoms and quality of life in patients with chronic mild traumatic brain injury.
For acute moderate-severe TBI, the review concluded that HBOT may be recommended as a treatment but explained that further studies are needed to both evaluate outcomes and determine the optimal treatment protocols. Evidence in the review, including nine randomized controlled trials, one meta-analysis and two prospective studies evaluating the clinical effects of hyperbaric oxygen therapy in patients suffering from acute and subacute traumatic brain injuries, showed mortality was significantly reduced but mixed results for favorable functional outcomes in survivors.
“This literature review scoured an immense amount of data related to HBOT as a therapy for traumatic brain injury, and the evidence that HBOT is effective against chronic traumatic brain injury is clear,” said Dr. Amir Hadanny, Chief Medical Officer at Aviv Scientific and Chief Medical Research Officer at the Sagol Center. “When looking at the comprehensive data over a larger stretch of time, we’re seeing the quality of studies have improved, and it’s exciting to see HBOT research heading further in the right direction. Many people are dealing with symptoms of chronic traumatic brain injury, and the current rehabilitation methods are limited in their efficacy. The science behind how HBOT can be effective is evident, and there is hope for those who are suffering.”
HBOT is a medical treatment in which 100% oxygen is administered at an increased environmental pressure. Aviv’s unique HBOT protocol, the hyperoxic-hypoxic paradox, fluctuates oxygen levels during treatment and is being used to repair and regenerate damaged brain tissue in several types of brain injuries including traumatic brain injury, stroke, PTSD, long COVID and age-related cognitive decline among others. Previous studies from the research team at the Sagol Center for Hyperbaric Medicine and Research have demonstrated the efficacy of HBOT as a treatment for persistent post-concussion syndrome (PPCS), suggesting that HBOT improves cognitive function, behavioral function and quality of life in both adult and pediatric patients suffering from PPCS at the chronic stage, even years after their injury.
Aviv Clinics offers an advanced treatment program with a multidisciplinary team of medical experts providing patients with top-line care and the opportunity to improve their quality of life. The Aviv Medical Program includes an in-depth assessment of the patient’s physical and neurological condition to assess the fit for the program. For patients that meet the criteria, the Aviv team will then prepare a comprehensive treatment schedule combining HBOT with personal cognitive training, and physical and dietary coaching, for a holistic approach to patient health. The HBOT sessions are conducted in state-of-the-art multiplace chambers that are comfortable, safe and allow for medical staff to accompany patients during the treatment. The elevated pressure in the HBOT chamber creates an optimal oxygenation condition, ultimately encouraging damaged brain and body tissues to regenerate and heal.
The full study is available here. For more on Aviv Clinics, visit aviv-clinics.com
Aviv Clinics is the leader in the research and treatment of age-related cognitive and functional decline and novel applications of hyperbaric oxygen therapy (HBOT) to maximize human performance. Based on an exclusive partnership with the world’s largest hyperbaric medicine and research facility, the Sagol Center at Shamir Medical Center in Israel, Aviv is introducing a global network of clinics delivering the most effective evidence-based treatment of the aging related decline – the Aviv Medical Program. The three-month regimen, designed to improve the aging-related decline in healthy adults, was developed based on over a decade of research and thousands of patients treated worldwide under the scientific leadership of Shai Efrati, M.D., chair of Aviv Scientific’s Medical Advisory Board and director of the Sagol Center.
Media Contact: Ellie Holt [email protected]
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#acutemoderate-severeTBI#AvivClinics#brainhealth#braininjured#braininjury#brainwound#chronictraumaticbraininjury#concussion#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#hyperoxic-hypoxicparadox#mildtraumaticbraininjury#stroke#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
BRAIN WOUND UPDATE #9 - But is a Concussion a "Wound"?
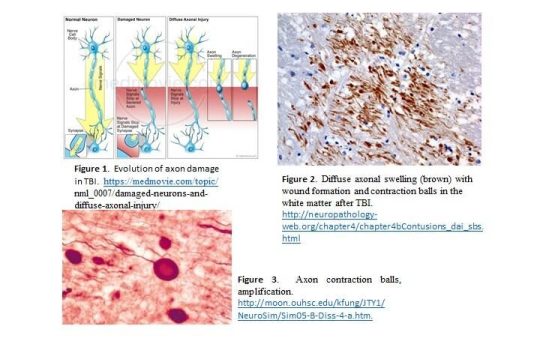
Proper Imaging Reveals the Physical Damage from Concussion and TBI
BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
Advanced imaging is outpacing medicine's ability to keep up with implications of the "new" brain science, and the nature of brain wounding. Medical textbooks are out-of-date with respect both to the nature of brain wounds and treatments to heal those wounds.
Drs. Carol Henricks and Paul Harch have put forward current scientific understandings.
Concussion: Not Just a Brain Bruise
Jun 30, 2022 08:00AM ● By Carol L. Henricks
Awareness of concussion injury exploded with the movie Concussion in 2015. The correlation between multiple concussions and neurodegenerative conditions was brought to the big screen. The common analogy of concussion being a “brain bruise” suggests that it is a minor injury that should recover in a few days without any permanent consequences. However, this is not true.
Our brains are uniquely designed and complex, more sophisticated than any computer. Every activity is a function of networks in the brain. The brain tissue injury that occurs as the result of concussion is complex and disruptive. Concussion is the result of many kinds of trauma that cause the brain to be shaken around inside the skull, causing diffuse axonal injury (DAI).
DAI creates lesions all throughout the brain, damaging the myelin (the fatty coating around axons), and may cause damage to deeper axonal structures. Diffuse injury disturbs network communication in the brain. Synapses—where one brain cell or neuron uses neurotransmitters to communicate with another brain cell—can be pulled apart, therefore disrupting cell-to-cell communication. The microenvironment of electrolytes and other brain-specific chemicals around the brain cells, glia and other support cells is disrupted and may effect electrical conductivity and functioning of cells.
Even a minor concussion may cause breaches in the blood brain barrier (BBB). A breach in the BBB allows chemicals, toxins and infections access to the brain when they would otherwise be blocked. The microtubular structure that internally organizes the neuron and allows transport of neurotransmitters to the synapse may be disrupted and disable cellular function.
Brain cells that are damaged and not restored to function begin a process of degeneration; this dying back of the cell leads to cell death and brain atrophy. This is the definition of a neurodegenerative process. Neurodegenerative processes include dementia, Parkinson’s disease and ALS.
Functional recovery—restoring the ability to read, sleep and balance, visual function and depth perception, cognitive activities and more—can be addressed by therapy, where some re-wiring and re-networking of the brain may occur. However, decline may still occur because functional recovery is different from biologically and physiologically healing the brain.
Military veterans, first responders and athletes in contact sports are at great risk for concussion and recurrent concussion, which causes cumulative injury and a high risk for neurodegenerative conditions. Traditional Brain MRI sequences, even with contrast, do not aid in diagnosing concussion because they do not highlight the disconnections. Brain MRI – DTI (diffusion tensor imaging) sequencing and/or Brain Quality SPECT scanning are the imaging tools of choice. Objective computer-based functional testing, including the RightEyeQ test (a standardized objective test of visual fixation and follow), reaction time testing and formalized balance testing, are objective and predictive, which is a good way to establish a baseline.
Take brain health seriously and pursue meaningful testing and active treatment for concussion.
Carol L. Henricks, M.D. is a neurologist specializing in the use of hyperbaric oxygen therapy (HBOT) and PEMF at NorthStar Hyperbaric, in Tucson. (HBOT) saturates the body with oxygen, reducing inflammation and enhancing recovery from central nervous system injury. Connect at 520-229-1238 or NorthStarHBOT.com.
##########
Dr. Paul Harch has cleared up the confusion In a seminal Meta Analysis: Systematic Review and Dosage Analysis: Hyperbaric Oxygen Therapy Efficacy in Mild Traumatic Brain Injury Persistent Postconcussion Syndrome.
TBI (5, 6) is a heterogeneous (7–27) diffuse physical injury to the brain that causes mechanical (7, 8, 28, 29) disruption of gray (22–24, 30, 31) and white (10, 15, 22, 23, 30, 32–35) matter, ischemia (36), hypoxia (29, 37, 38), edema (29, 39, 40), vasospasm (41, 42), release of neurochemicals (43, 44), and reperfusion injury (39, 45) and affects over 4.1 million people annually in the U.S. alone (
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes