Text
Legislative Update

First hyperlink is for the proposed Senate amendment to Title 10. Of note, on pg. 33 line 11, is "Special Operations Brain Health and Trauma Program". On pg.45 line 8, the formal language for TBI is now codified: "Definition of Traumatic Brain Injury".
https://www.kaine.senate.gov/imo/media/doc/blast_overpressure_safety_actpdf.pdf
Below is an article from Task & Purpose that embeds the attached Senate amendment to Title 10:
Blast overpressure getting attention from lawmakers
A new bill demands more oversight for troops injured from heavy weapon blasts, TBIs and the Army is developing a tool for troops to check their blast exposure risk.
And Rep Greg Murphy's Bill has moved on:
https://murphy.house.gov/media/press-releases/murphy-legislation-provide-hyperbaric-oxygen-therapy-veterans-passes-va-health
Murphy Legislation to Provide Hyperbaric Oxygen Therapy to Veterans Passes VA Health Subcommittee
April 16, 2024
Press Release
Washington, D.C. — Today, Congressman Greg Murphy, M.D.'s legislation, H.R. 3649, the Veterans National Traumatic Brain Injury Treatment Act, passed the House Veterans' Affairs Subcommittee on Health by voice vote. This bipartisan bill would establish a pilot program at the Department of Veterans Affairs to furnish hyperbaric oxygen therapy (HBOT) for veterans who have post-traumatic stress disorder (PTSD) or a traumatic brain injury (TBI).
"Since entering office, advocating for new treatment pathways for our veterans has been one of my top priorities," said Congressman Greg Murphy, M.D. "During my time in the North Carolina House of Representatives, I successfully led the effort to make hyperbaric oxygen therapy accessible to veterans in our state. I'm proud to announce that the U.S. House Veterans' Affairs Health Subcommittee has passed my Veterans National Traumatic Brain Injury Treatment Act which would enact similar reform at the national level. I'm grateful for the support of my colleagues and look forward to continuing my advocacy on behalf of this lifesaving treatment."
Cosponsors: Reps. Marilyn Strickland (D-WA), Jennifer Kiggans (R-VA), Don Davis (D-NC), Jeff Duncan (R-SC), William Timmons (R-SC), Chris Pappas (D-NH), Bill Huizenga (R-MI), and Del. James Moylan (R-GU).
Background
Hyperbaric oxygen therapy accelerates the brain’s healing process by providing the bloodstream with elevated oxygen to reach and repair damaged tissue and restore normal function.
Studies demonstrate that HBOT is an effective treatment for veterans suffering from PTSD and TBI. Authors of one such study described HBOT as having “one of the greatest reductions in PTSD symptoms in a four-week period with any reported treatment.”
Despite its proven efficacy and requests by Members of Congress, the Department of Veterans Affairs currently does not employ HBOT.
ACTION on the Bill thus far; date for full Comm vote TBD.
[Attached, please find our response to the VA Testimony at the hearing on 3.21.2024. All our testimony inserted into the Record can be found at: https://treatnow.org/knowledgebase_category/congress_house_veterans_affairs_2024/
Date
All Actions
04/16/2024
Forwarded by Subcommittee to Full Committee by Voice Vote.
Action By: House Veterans' Affairs Subcommittee on Health
04/16/2024
Subcommittee Consideration and Mark-up Session Held
Action By: House Veterans' Affairs Subcommittee on Health
03/21/2024
Subcommittee Hearings Held
Action By: House Veterans' Affairs Subcommittee on Health
06/20/2023
Referred to the Subcommittee on Health.
Action By: Committee on Veterans' Affairs
05/24/2023
Referred to the House Committee on Veterans' Affairs.
Action By: House of Representatives
05/24/2023
Introduced in House
Action By: House of Representatives
Read the full article
#blastinjury#brainhealth#braininjury#HBOT#headtrauma#hyperbaric#hyperbaricchamber#HyperbaricOxygentherapy#posttraumaticstressdisorder#PTSD#TBIdefinition#TBIVeterans#traumaticbraininjury#VAHealth#veteranaffairs#Veterans
0 notes
Text
Veterans: Your Brain May be Unwired
Preliminary Primer on Brain Wounding
Dr. Carol Henricks is a neurologist in Tucson, Arizona who has been in private practice since 1999. She does consultation in her neurology office, NorthStar Neurology, PC and since 2004 she has had NorthStar Hyperbaric, a clinic that specializes in the use of hyperbaric oxygen therapy and other healing therapies to treat neurological conditions. Primarily her patients are military veterans and first responders. She began "Healing Arizona Veterans" to support treatment for post 9-11 veterans; she separated from it when it became a non-profit. She has treated hundreds of veterans over the past 20 years and is an advocate for brain health.
*************
An Army Ranger jumps out of a plane and his parachute deploys and jerks his head and neck. He lands, strikes the ground and strikes the back of his head and is momentarily stunned. Then he walks a distance carrying his full ruck with weapons and explosives into the village to "clear it" and breeches door after door, setting off explosive after explosive. They fire their own weapons during the mission. An infantryman on the battlefield firing a rocket launcher from his shoulder. He fires round after round passing the recommended limit. But this is war and nobody is counting. With each insult the intracranial injuries compound, and toxic burden is increased, from super-toxic sites, heavy metals, and environmental toxins being inhaled, and absorbed through the skin and GI tract. A Navy corpsman with her marine unit who stays with her team and is on the battlefield for every combat mission: in harms way every time and experiencing blasts and exposed to toxicity. The helicopter pilot on rescue missions who is exposed to the constant down beating of propellors and the fighter pilot who pulls a lot of G's. Military members in theater have many potential sources of injury, particularly brain injury.
NorthStar Neurology and NorthStar Hyperbaric Clinic has treated hundreds of military veterans for their brain injury conditions over the past 20 years. 80% of the patients I treat are military veterans and first responders with brain injury conditions that have been caused by a combination of concussion, blast, and toxic exposure as a result of their service. When veterans do not suffer other physical trauma, their brain trauma often goes unrecognized. Being able to walk, talk, and eat does not signify a lack of injury. Concussion is not just a brain bruise, it is a serious injury with profound consequences if healing does not occur. It is time for concussion injury to be correctly diagnosed and treated.
Recognizing concussion
The role of concussion including blast injury, other traumatic brain injury (TBI), toxicity, the link to suicide, Post Traumatic Stress Disorder (PTSD) symptoms and neuro-degenerative disease is receiving increasing attention in the medical literature. Unfortunately, the seriousness of the injury and the underlying neuropathology is not commonly elaborated in the medical literature. There is a misconception that a concussion is like a "brain bruise" that is relatively ninconsequential and will heal unaided within a short period of time. (1) When veterans continue to experience post - concussion symptoms (PCS) they are sent to a psychiatrist to manage "mental health" symptoms instead of being treated with a protocol to heal their brain wound.
The complexity of functional areas of the brain, such as biochemical microenvironments, fiber tracts, and intricacy of the brain is unlike any other tissue in our body. Traumatic injury to the brain and inflammation are likely stepping stones to many neuro-degenerative disease processes. A history of concussion injury correlates highly with future diagnoses of ALS, Alzheimer's and Parkinson's disease and is likely a precursor for those conditions. (2) Diagnoses of those neurodegenerative conditions are at epidemic proportions: Military Veterans are proven to be at increased risk. While the connection between severe TBI with skull fracture, penetrating wounds, intracranial bleed, or complicated by a stroke may seem like a more obvious precursor to neuro-degenerative disease than a series of milder concussions, severe concussion, and particularly multiple concussions may be just as ominous.
Being aware of historical diagnoses of concussion is additionally a critical consideration when evaluating mental health; you can't have mental health if you do not have brain health. The brain is the organ that is the seat of all emotions, thoughts, and behaviors. An injured brain does not function optimally. There has commonly been a misattribution of a cluster of symptoms known as "PTSD" or post - traumatic stress disorder ni patients that actually have a post - concussion syndrome. (3) Every symptom designated as a "PTSD" symptom is also a post- concussion symptom. Depression and suicidality are common to PCS and are associated with damage to the left subfrontal and temporal lobe cortex.
Concussion diagnosis has been overlooked because of misconceptions about how the injury is caused. A blast injury may have caused injury even if it did not knock you down. You don't have to "black - out" or strike your head to have sustained a concussion; shaking your brain around inside your head is al that is necessary to cause injury. Damaging specific areas of the brain causes specific symptoms. The points of impact within the skull and the associated movement of the brain determine the deficits caused by the injury. If the impact causes the left hemisphere of the brain to experience a "coup" impact, typically language function will be affected; so the injury causes both a focal injury and a diffuse injury. If the brain is shaken anteriorly to posteriorly, the left subfrontal cortex, for example, will be injured. The left subfrontal cortex and the left temporal lobe (amygdala) called the arcuate fasciculus and uncinate fasciculus of the brain is associated with mood stability and emotional regulation. When the left hemisphere is injured, this effects brain waves resulting in an alpha - theta rhythm. The right hemisphere then will become over- aroused and will have a high beta brain wave activity resulting in feelings of depression and anxiety. This type of diffuse axonal injury in the left prefrontal cortex and temporal cortex presents as suicidal ideation. Hyperbaric Oxygen Therapy (HBOT) and neurofeedback (NFB) restore these pathways and brain waves. (4) When it is damaged, there is associated depression, mood instability and suicide risk. Transcranial Magnetic Stimulation (TMS) is directed over the left frontal lobe of the brain to treat depression. The physical trauma causes a biological sadness evidenced by lethargy and accompanying emotional sadness.
Concussion, as a diagnosis, has often been overlooked because appropriate imaging has not been used to visualize the injury. For mild to moderate concussion injuries (or series of injuries), a head CT scan without and with contrast, and/or Brain MRI scans without and with contrast are often unremarkable. This is a limitation of the study and does not mean that no injury has occurred; those studies are more the equivalent of taking a gross anatomical look at the brain. (5) More sophisticated imaging to assess the consequences of the diffuse microscopic injuries are necessary. A Brain MRI - DTI - NQ without contrast uses a metric known as fractional anisotrophy (FA) which reflects the diffusivity of water.
The scanning protocol uses calculations to create an image of fiber tracts within the brain. When there is increased diffusivity of water along a fiber tract, that reflects a point of injury and the created image will demonstrate a truncated fiber tract at that point. Observing the fiber tract disconnections correlates the physical injury to the neuro-behavioral pathology and / or mental illness symptoms. A brain quality SPECT scan is specifically designed to assess metabolic activity in different areas of the brain using radioactive dye that is attached to sugar molecules. Injured brain tissue is dysregulated and may have increased or decreased metabolic activity.
Clinically a concussion presents as dysfunction in multiple areas of life. Clinical presentation of concussion is based on observations, clinical history, self - reporting, and supported by some specific testing. Concussion presentation can be assessed by considering five critical areas (or pillars) of function: visual function, memory, attention and information processing, sleep, balance and emotions. (6) These are all areas that reflect fiber tract network function in the brain, and their function is disrupted by concussion. Compromised brain health is not just a function of a
recent injury, but can be a product of the accumulation of injuries (trauma, toxins, infections, inflammation, ischemia, etc) and healing that have taken place throughout life. (7) A concussion is not one simple injury but actual physical damage to a complex sophisticated network of fiber tracts, metabolic environments, and blood vessels and the lymphatic system, and neurons and astrocytes. The hypothalamic pituitary axis at the base of the brain is also impacted by multiple concussions, severe trauma and toxins. Local brain trauma may damage a control center while the more diffuse axonal injury to the network damages the functional communication system.
Neuropathological changes
Brain function is carried out by finely tuned networks that are both chemical and electrical. When chemical and electrical processes are disrupted, functional network performance is compromised. Even a mild concussion injury can cause physical injury to the brain that may be disruptive. Brain injury and healing from brain injury is complex, but our brains and our bodies are designed to heal themselves under the right conditions. The brain can always learn by rewiring, re-networking and recruitment but when overwhelming injury has occurred, healing therapies are necessary to support the healing process. Healing processes include HBOT, NFB, diet, supplements, and other adjunctive therapies.
At the base of the brain is the hypothalamic - pituitary axis (HPA). Damage to the HPA by concussion, blast force, and toxicity causes profound pathology. The hypothalamus is the seat of the autonomic nervous system (ANS) which controls the automatic functions of the body like breathing, blood pressure, heart rate, GI motility etc. Damage to the hypothalamus may disturb control of those automatic functions. Damage to the pituitary gland disrupts hormone function in the whole body. Many military members become hypothyroid and have low Testosterone levels; female hormone cycles may also be disrupted.
The metabolic environment around the neuron is critical: electrolytes around the neuron have positive electrical charges that mobilize when an action potential is initiated. There are large proteins in the cell which carry a negative charge. Everything is balanced. An electrical signal is propagated when positive charges go inside the axon and negative charges leave creating an electrical impulse. As the electrical impulse travels down the axon, it signals the release of chemical neurotransmitters into the synaptic space to communicate with the next cell. If the metabolic environment is disrupted, then effective electrical signaling cannot occur. The metabolic environment must recover after each impulse. When there is physical trauma (concussion), blast injury, or toxicity in the metabolic environment it must be corrected. Clinically, when the metabolic environment is disrupted, someone with a concussion may experience a confusional state. The confusion is often described as "brain fog". This is only one component of the brain injury associated with concussion, but documentation of disruption of electrical signaling can be demonstrated with quantitative EEG recording of slowing and possibly disorganization. (8) The disrupted metabolic environment
along with the cascade of injury and inflammation, as well, as the circulating toxins influxing due to breaching of the blood brain barrier all create a toxic storm that the brain is not prepared to process. There are many unknowns, but the physiology is different after multiple injuries and brain function is additionally altered by immersion in a multi- toxic metabolic environment.
The physical trauma of a concussion pulls synapses apart. When the signaling cell releases the neurotransmitter into the synaptic space after a concussion, the neurotransmitter may never reach the receiving cell. A greater separation between the signaling brain cell and the receiving brain cell can result in a failure of communication between those two cells. Multiple failures caused by the diffuse injury of concussion throughout the brain cause network or system failures which result in loss of functional abilities such as balance, complex decision making, and complex information processing.
Brain shear injury is the classic anatomical injury associated with concussion. As the brain forcefully moves to and fro inside the skull, as a result of trauma, it causes tears or shears in the axons. (9) Axonal shears may damage only the myelin or may completely tear through the axon. This interferes with transmission of the electrical signal through the axon and therefore damages the network. When the brain is injured by concussion, there are multiple injuries throughout the brain disrupting network function. It is like having a computer with a lot of wires cut, there is a pronounced slowing and functional glitches.
The physical trauma of concussion, blast injury and toxicity damages small (and sometimes larger) blood vessels which destroys the protective mechanism of the blood brain barrier (BBB). Even a mild concussion may injure the BBB. (10) When the BBB is breeched, toxins circulating in the blood have direct access to brain cells and may poison them. Military veterans and first responders experience toxins that are released into the air from burning debris of burn pits, exposure to HAZMAT and super -toxic sites AFTER exposure to blasts, and physical trauma when their BBB is breeched. PFAS and "forever chemicals" are common in the toxic mix. Toxins are absorbed through the skin, oral and nasal mucosal membranes, into the lungs and GI tract. Toxins from burn pits and fires are caustic corrosive neurotoxins that may directly damage brain cells and cause tremendous disruption of function. The more injury to the BBB, the more toxins are able to flood in. An additional concern is that breaching the BBB opens the door to Central Nervous system (CNS) autoimmune diseases.
Blast injuries are most like the bends: a veteran is engulfed by a pressure wave followed by a vacuum. This is most like being deep underwater and being brought to the surface quickly: it gives you bubble trouble. There is CNS injury associated with the bends as well as with blast injury. Military members may suffer from "Breacher syndrome" as a result of their cumulative blast injuries. (11) An accumulation of milder injuries can be quite damaging and cause persistent functional deficits. Blast injury contributes to other traumatic injury by creating small infarcts from gas bubbles throughout the body. A blast injury exposes the body to tremendous whole body pressure from the blast peak overpressure wave (like being under pressure deep underwater) and then suddenly the pressure is reversed (like coming to the surface of the water too quickly) as the negative pressure wave spreads out from the point of explosion. The rapid change in pressure causes Nitrogen gas (which is inert in our bodies) to coalesce into bubbles or gas emboli that block blood flow to different areas of the brain causing small infarcts or strokes and infracting other tissue. Military service members on the battlefield who suffer multiple blast injuries in rapid succession may experience a much worse pathology than a simple concussion.
Veterans and first responders have become so chemicalized from multiple sources of toxic exposure that the individual effects of toxins cannot be sorted out. Heavy metals from weapons fired, burn pits, super toxic sites, vaccine injury, mefloquine reactions, and hormone disruption all potentially disturb brain function, but also affect other organs and put veterans at high risk of cancer, poisoning and organ failure. You cannot have healthy brain function if there is metabolic disturbance in the body. HBOT promotes detoxification.
Physical trauma breaks the microtubularinfrastructure of the cell, particularly the axon, which has been considered as a major cause of the axon degeneration and eventual cell death. (12) The microtubular infrastructure facilitates transport of neuro-transmitters and other necessary nutrients that are made in the main cell body to be transported down the axon to supply the axon and the synapse. If the microtubular infrastructure is broken and disorganized, this function cannot take place: the injured cell is then not part of the functioning network. A drug, Epothilone D, is being studied as a possible agent to stabilize microtubules after injury and manipulate injury - induced synaptic plasticity. (13) What happens to any structure when you continue to physically assault it: the more trauma, the more injury. You eventually destroy the cell. An injured cell that does not heal begins a dying back process known as Wallerian degeneration; eventually after enough brain cells die there is resulting brain atrophy.
Concussion damages the astrocytes interfering with their ability to carry out homeostatic functions. Damaged astrocytes may trigger a reactive gliosis that may be a first step in causing a glioblastoma.(14)
Concussion injury damages lymphatic drainage channels. The meningeal lymphatic system helps to clear metabolic waste from the brain and CSF. If this metabolic waste is not cleared, there is dysfunction of the neuro- immune clean- up process and a worsened clinical outcome.(15)
Treatment planning
Military members who suffer these injuries need to be properly assessed and treated. The brain heals slowly and if you are injured again before you heal it is disastrous. It is likely that brain atrophy (the endpoint of neurodegeneration) is not a normal part of aging, but a pathological process caused by the accumulation of brain insults throughout life.
There is a clear pathophysiological pathway from concussion to neurodegenerative conditions, and toxic exposure only makes things worse. The clinical presentation of Alzheimer's, Parkinson's and ALS (neurodegenerative conditions) can be seen in veterans with a combination of concussion and toxic exposure. Different clinical presentations of neuro-degenerative conditions have different patterns of brain atrophy; microscopically post-mortem they all have biological markers of the final common products of brain cell death. When diagnosing neurodegenerative syndromes, it is critically important to consider the history of physical trauma as part of the causal etiology of the disease presentation. Healing the brain after physical trauma and toxic exposure is key to stemming the epidemic. Medication may transiently mitigate some symptoms, but healing the brain and detoxifying the brain and the body is critical to stopping disease progression.
There are no medications that perform this complex healing process and detoxification. We need to support our brain's ability to heal.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#postconcussionsyndrome#TBI#traumaticbraininjury#Veterans
0 notes
Text
Hyperbaric Oxygen Therapy May Be the First, Only Clinically Effective Treatment for Long COVID

February 26, 2024
Erin Hunter, Associate Editor
https://www.pharmacytimes.com/
“I’m better than I was before I had long COVID, and in so many ways,” said a patient in an interview with Pharmacy Times."
Key Takeaways
Hyperbaric Oxygen Therapy (HBOT) may be an effective treatment for long COVID, and it is the only therapy that has shown clinical effectiveness in a controlled clinical trial.
The benefits of HBOT are durable, as it triggers neuroplasticity in the brain and may reverse brain damage caused by COVID infection.
There are still many challenges in diagnosing and treating long COVID, as there are more than 200 symptoms associated with it (with most affecting the brain and nervous system), and many patients experience a delay in diagnosis or dismissal of symptoms.
After suddenly developing a series of severely debilitating neurological and physical disorders, Lynette Milakovich, a yoga teacher currently living in The Villages, Florida, spent almost 2 years and $20,000-plus on doctors’ appointments and failed therapies to treat her symptoms. It took nearly this duration of time before she learned the cause of her illness was long COVID-19 (long COVID), she told Pharmacy Times in a recent interview. It was not until receiving hyperbaric oxygen therapy (HBOT) treatment that she found lasting relief.
HBOT is currently the only treatment protocol that has been proven clinically effective in the treatment of long COVID in a controlled clinical trial, according to Shai Efrati, MD, the co-founder and chairman of the Medical Advisory Board to Aviv Scientific, and director of the Sagol Center for Hyperbaric Medicine & Research at Shamir Medical Center, in an interview with Pharmacy Times.
Additionally, there are findings from a new longitudinal study published in Scientific Reports —which evaluated patient outcomes after 1 year of finishing an HBOT intervention— that show that the benefits sustained from HBOT might be long-term. According to Efrati. HBOT can repair brain tissue damaged by COVID-19, and this can actually lead to permanent changes.1
“When we take care of the brain damage, it heals symptoms,” Efrati told Pharmacy Times.
What Is Long COVID?
There are estimates that more than 65 million people around the world have had long COVID, although this number is likely to be higher, according to investigators of a study published in Nature Reviews Microbiology.2 Long COVID (also referred to as post–COVID-19 condition) is a syndrome characterized by mild-to-severe symptoms of COVID-19 that can last for weeks, months, or years after overcoming initial COVID-19 infection.3
There are more than 200 symptoms associated with long COVID.3 Symptoms can be an extension of those experienced during acute infection, or they can appear as new symptoms altogether—and although symptoms can impact many different organ systems, they largely affect the brain and central nervous system (CNS).2,3
“We understand that COVID may penetrate the brain through blood vessels or the cribriform plate that is located above our nose and cause brain damage in the neurons,” Efrati said. “So, what we are dealing with is brain damage.”
Milakovich had suffered from many symptoms related to dysregulation of the brain and CNS: total body neuropathy, tinnitus, postural tachycardia syndrome (PoTS), tachycardia, high blood pressure, tremors, convulsions, insomnia, and severe mental symptoms (cognitive decline, depression, anxiety, suicidal ideations, apathy, and post-traumatic stress disorder).
Long-Term Impact of HBOT for Patients With Long COVID
The purpose of HBOT is to increase oxygen absorption into tissue, which can support brain injury recovery;1 it may be particularly effective for brain/CNS symptoms because it triggers brain neuroplasticity, or “the ability of the brain to repair itself,” Efrati explained. In essence, neuroplasticity enables the brain to reverse the damage and dysregulation caused by the virus.
Previous studies affirm these neuroplastic benefits in patients with stroke and traumatic brain injury who had improved cognitive and motor function and quality of life measures following HBOT. Findings from previous studies also show that HBOT creates positive microstructural changes in the brain.1
However, no studies had evaluated the long-term clinical benefits associated with HBOT for patients with long COVID.In the present longitudinal study, 31 patients—having originally completed 40 sessions of HBOT the year prior at Aviv Clinics—filled out a series of questionnaires about quality of life, quality of sleep, and psychiatric and pain symptoms.1
Patients were treated with hyperoxic-hypoxic paradox (HHP), an HBOT protocol that exposes the patient to elevated atmospheric pressure (compression/decompression rate of 1.0 m/min) and fluctuating oxygen levels (100% oxygen for 90 minutes with intermittent breaks of medical-grade air with normal 21% oxygen levels). 1
Based on the results, HBOT was found to be associated with persistent improvements in quality of life, quality of sleep, psychiatric and pain symptoms. There was a moderate magnitude of improvement in neuropsychiatric symptoms (ie, depression, anxiety) and sleep quality that lasted long term, along with a significant reduction in pain and significant increase in quality of life at the time of analysis.1
“ I still have a bit of tinnitus, the rest of the symptoms are gone,” says Milakovich. “I have full cognition and feeling back… no more tremors and convulsions, no more PoTS.”
Prior to HBOT, Milakovich used various pharmacologic agents to try and treat symptoms individually: low-dose naltrexone for nerve pain/neuropathy, a nitric-oxide supplement (Cardio Miracle ) for PoTs and tachyardia, and temazepam (Restoril; Mallinckrodt Pharmaceuticals) for insomnia. Milakovich also found anecdotal evidence supporting the use of other supplements like nattokinase (Cardiokinase; Plamed), curcumin, and bromelain for long COVID.
Efrati noted it may be worth trying different methods and treatments for long COVID, however, none offer evidence-based outcomes besides HBOT.
In time, Efrati believes that HBOT clinics will begin to create a multi-strategy treatment protocol to treat patients more effectively. Additionally, Efrati explained that going forward, there will need to be more research on the specific minimum number of sessions required for recovery. Currently, Efrati and other HBOT practitioners have made it a practice to calibrate the number of treatments needed for patients based on their response.
Long COVID and The Patient Perspective of Medical Gaslighting
It's worth noting that long COVID can have many possible symptoms, which makes it difficult to diagnose. Moreover, there are no laboratory tests that can technically prove an individual is suffering from long COVID.4
Given the myriad of symptoms, continued knowledge gaps, diagnostic difficulty, and other factors, there have been reports that long COVID is being improperly diagnosed; as a result, patients have reported that they feel like they are experiencing medical gaslighting, according to findings from a qualitative study that aimed to understand the experience of patients with long COVID in seeking care in the United States.5
Investigators observed that patients thought that their providers dismissed symptoms, met patients with a lack of empathy, and some providers were reported to have disqualified the patient experience and their ability to report symptoms. This can make the patient feel as though they must “prove” that their illness is real, and it can ultimately prolong the time it takes to receive adequate care.5
According to 1 study participant, it took over a year to prove that their symptoms were not psychosomatic.5 In Milakovitch’s case, it took nearly 2 years and countless providers before receiving a proper diagnosis, and she cautions pharmacists and providers to not “make the patient believe it is all in their head.”
“Patients need to be validated because long COVID is real,” Milakovich said.
Conclusion
Therapies like HBOT are an exciting innovation that can transform the treatment of long COVID. HBOT can provide long term improvements to neuroplasticity and reduce brain damage—it is the only therapy that has been proven safe and effective, improving psychological symptoms, pain symptoms, and quality of life in patients with long COVID.1
“I’m better than I was before I had long COVID,” Milakovich said. “And in so many ways, I have my life back!”
REFERENCES
Hadanny A, Zilberman-Itskovich S, Catalogna M, Elman-Shina K, et al. Long term outcomes of hyperbaric oxygen therapy in post covid condition: longitudinal follow-up of a randomized controlled trial. Sci Rep 14, 3604 (2024). doi:10.1038/s41598-024-53091-3
Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 21, 133–146 (2023). Doi:10.1038/s41579-022-00846-2
COVID-19 and the Nervous System. NIH. Article. Last reviewed on January 30, 2024. Accessed on February 18, 2024. https://www.ninds.nih.gov/current-research/coronavirus-and-ninds/covid-19-and-nervous-system#:~:text=SinceCOVID19canaffect,twitchingorjerking(myoclonus).
Katella K, What Happens When You Still Have Long COVID Symptoms? Yale Medicine. News Release. October 27, 2023. Accessed on February 26, 2024. https://www.yalemedicine.org/news/long-covid-symptoms
Au L, Capotescu C, Eyal G, Finestone G. SSM Qual Res Health. 2022 Dec; 2: 100167. Published online 2022 Sep 7. doi: 10.1016/j.ssmqr.2022.100167
Read the full article
0 notes
Text
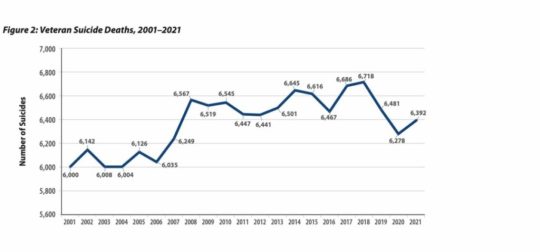
How Big is the Veteran Suicide Problem?

Overview of the policies and flawed science behind the Veteran suicide, drug overdose deaths, diabetic amputations, and mental health epidemics.
This series intends to tackle a range of subjects that afflict Veterans, especially suicide and drug overdoses which, along with diabetic lower limb amputations, are at epidemic levels. Across military medicine and traditional approaches to “mental health,” there is a wide gap between the VA's palliative care model – control the symptoms – and root cause analysis that gets at the physical damage to the brain and whole-body wellness and the brain wound healing called for. This includes proper diagnoses and a shift to an appreciation of polytrauma -- including the need for brain-wound healing -- and its long-term negative consequences.
We at TreatNOW, Grunt Style, America’s Mighty Warriors, and numerous other Veteran organizations are focused on Suicide Prevention. DoD and the VA declare that Suicide Prevention is their #1 priority. On this we can agree. Where we disagree is the protocols used by the VA and traditional medicine to diagnose what they call “mental health” issues, and their insufficient interventions. We differentiate between real mental health issues and brain wounds. The disagreement is fundamental, so much so that that we continue to call for an Inspector General report on the flawed science sponsored by taxpayers without their knowledge.
First, some perspective. We must separate scientific fact from the fiction spun by conclusions in Army/DoD/VA studies. The USG spent in excess of $186 Million on five clinical trials and came to flawed conclusions about the safety and efficacy of Hyperbaric Oxygen Therapy when used to treat TBI/PTSD. The Undersea & Hyperbaric Medical Society (UHMS) has finally set the record straight now that peer-reviewed science has again confirmed that hyperbaric oxygenation and medicine begin with any increase in pressure or oxygen concentration. Thus, the Army/DoD/VA dosing studies, along with the other 21 peer-reviewed clinical trials, confirm that HBOT helps heal brain wounds. The actual data in those government studies confirm what their editorial comments deny. And three of the Principle Investigators wrote positively in the studies and later commentary, confirming that HBOT is safe and effective:
- "Randomization to the chamber . . . . offered statistical and in some measures clinically significant improvement over local routine TBI care."
- “total scores for groups revealed significant improvement over the course of the study for both the sham-control group .... and the HBO2 group.”
- " is a healing environment."
- “Both intervention groups demonstrated improved outcomes compared with alone.”
- “HBO2 improved post-concussive and PTSD symptoms, cognitive processing speed, sleep quality, and balance function, most dramatically in those with PTSD.”
- “At least fair evidence was found that the intervention improves health outcomes and concludes that benefits outweigh harm. . . Hyperbaric oxygen therapy for mild traumatic brain injury and PTSD should be considered a legitimate adjunct therapy.”
- “We cannot ignore the fact that people got better.”
Second, HBOT has been shown to virtually eradicate suicidal ideation and allow patients to get off almost all prescribed drugs, including those that warn of suicidal ideation. The following chart from the VA makes clear that service member suicide deaths since 9/11 exceed 146,000. Prescribed drug overdose deaths during the same time period exceed 109,000. That’s over a quarter million avoidable deaths, even as the Veteran population has decreased. Add in the 796,340+ diabetic foot ulcer patients who have succumbed to death within 5 years following largely avoidable lower limb amputations -- most without ever being told that amputation could be avoided. That number of 796,340 veterans is more than all KIA since beginning of WWI (623,982)
Third, the picture that leads this piece is meant to convey a staggering realization of how government and public policies have led to unanticipated, negative consequences. The epidemics we are addressing here are such crises, with awful, reprehensible human consequences. Two examples: Tuskegee, and the near-eradication of the plains buffalo in the 19th century.
The government had its reasons to eliminate bison. "One of the biggest advocates of buffalo slaughter was General William Tecumseh Sherman. 'General Sherman remarked . . . . that the quickest way to compel the Indians to settle down to civilized life was to send ten regiments of soldiers to the plains, with orders to shoot buffaloes until they became too scarce to support the redskins.'" While it is possible to repopulate bison, the hundreds of thousands of Veterans now passed prematurely due to suicides, drug overdoses, and unnecessary lower limb amputations are not coming back. Nor are some 100 poor black citizens of Alabama.
"The Tuskegee Study of Untreated Syphilis in the Negro Male", conducted by the US Public Health Service and the CDC between 1932 and 1972, led to the unwitting deaths of nearly 100 subjects out of 400 due to complications of syphilis. Though penicillan was in wide use for nearly 30 years of the 40-year study, none of the participants was told of its availability and the near-sure cure of the syphilis after penicillan use. The Tuskegee experiment has been called one of the most significant events in the history of bioethics. In 1973, Senator Edward Kennedy conducted congressional hearings into the study. Those hearings led to the passage of the National Research Act and, in turn, the establishment of institutional review boards, principles of informed consent, and protection of vulnerable populations.
It took forty years for the government to end the Tuskegee experiment. The President Clinton apology contained these words: "No power on Earth can give you back the lives lost, the pain suffered, the years of internal torment and anguish. What was done cannot be undone. But we can end the silence. We can stop turning our heads away. We can look at you in the eye and finally say on behalf of the American people, what the United States government did was shameful, and I am sorry."
It's all too familiar: “If only one man dies of hunger, that is a tragedy. If millions die, that's only statistics.” Government policy in the case of Veterans has devolved to turning a blind eye and using statistics to paper over the preventable tragedies. Families of the dead die a little every day; yearly, authorities hold more conferences, pass more ineffective laws, and increase budgets for Suicide prevention strategies, even as the suicides continue to increase.
Veterans tell of a relentless cycle in the VA, familiar to the families of the brain wounded. The faceless bureaucracy and unending appointments that too often end in cancellation. The inhumanity affects veterans with brain wounds, or suffering from Burn Pit toxins, Camp Lejeune toxic water, or as far back as Agent Orange victims. It starts with denial: it didn't happen. Then delay: you'll have to wait. Then too often the deception: wounded are made to feel ghosted, met with indifference and a sense of betrayal. Inevitably, the drugs, the endless changes of prescriptions, dosages, and care givers. Many of those drugs lead to depression, adding to the need for anti-depressants that warn of suicidal ideation. And, too often, death: hundreds of thousands of suicides and drug overdoses.
This cycle can be broken. Denial, delay, deception, drugs, depression, death is not worthy of us. This series is an appeal to both law and our morality. We must look Veterans in the eye, especially the brain wounded, and tell them that we both can and will do more to make real brain wound healing treatments available. We must begin with acknowledgement of the real science, the positive changes in our understanding of brain wounding, and the mechanisms of action to heal those hundreds of thousands of Veterans denied a chance at a return to normal.
Part two will be a look at just how dangerous Modern War has become to the brain: BLAST Injury, Burn Pits, and the nature of whole body damage/polytrauma. It will include a primer on brain wounding that seeks to differentiate real physical damage from the "mental health" symptoms that remain the target of conventional military medicine.
Join us on the journey to explain, to understand, and to TreatNOW.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#brainwounds#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#PTSD#suicide#suicideepidemic#suicideideation#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#VA#VeteranSuicide#VeteranSuicidePrevention#Veterans
0 notes
Text
New Days Could be Dawning
A 13-part series to illuminate the way forward in the grip of suicide, drug overdose, diabetic amputations, and mental health epidemics.
Readers in this space are all familiar with the headlines: Football leads to brain damage and CTE. Suicides continue to increase no matter how much more money DoD and the VA spend on Suicide Prevention strategies. Veterans are being subjected to BLAST injuries from their own weapons. Parents should avoid letting their children bang their heads in sports until they’re 14 years old. Society is experiencing increasing numbers of neurogenerative diseases at younger ages. More and more money is being spent on research to use psychoactive and hallucinogenic drugs to cope with mental health problems. 988 Suicide Crisis Line counselors are burned out, quitting, undertrained and understaffed.
From football fields to battlefields to America’s classrooms and assisted living facilities, citizens and policymakers and the medical profession are wondering what can be done about suicides, “mental health” and the growing sense that daily life is causing damage to our brains. Whether it’s sports, or legal and illegal drugs, or violence, or online abuse and bullying and shaming, or mass casualty events, or the suicide and opioid epidemics, increasing numbers of young and old have “mental health problems.” We seem to be losing our minds.
To a certain extent, what may seem like increased mental health challenges may be due to increased diagnoses stemming from better awareness and understanding. Increased media attention, social media, economic pressures, and isolation may contribute to higher awareness. Increased longevity and improved diagnoses may be behind seemingly larger numbers of age-related dementias.
But doesn’t it just seem that there’s an abnormal number of people suffering from diminished capacity? And that no matter how much we spend, we keep getting more pleas from victims, survivors, care givers, politicians, medical staff and social media for solutions? Congressional hearings, Foundation Annual reports, investigative reporting, government fact-finding, and personal experience make it obvious that we’re falling behind while the suicide and drug overdose and mental health epidemics worsen.
You’ve heard the adage: “Better to light a candle than to curse the darkness.” The TreatNOW Coalition has been taking steps for over 15 years to light candles, to educate, to end Veteran suicides, and to change medicine. Thus, the start of this 13-part series to light several candles. Not only to point out problems, but much more importantly to offer solutions that already exist. The choice is between politics and progress, between cursing “wicked complex problems” and applying proven solutions. This series will bring you some central truths and, importantly, lay out solutions to the challenges posed by a perhaps misnamed “mental health crisis” in our military and across the country. Ensuing chapters will discuss the estimated $600 Billion per year mental health costs that are only projected to consume more of our national wealth. And the World Economic Forum projects that the cost of mental health conditions and their related consequences will rise to $6 trillion globally by 2030.
Together with the GruntStyle Foundation, TreatNOW and multiple other organizations aim to arrest and reverse the suicide and prescribed drug overdose death epidemics afflicting our Veterans, Armed Forces, and society. Both the VA and DoD have declared that suicide prevention is their #1 clinical priority. Based on budget choices, it would seem we’re serious about finding and applying, quickly, some methods that will work against suicidal ideation almost the way penicillin works against bacterial infections like pneumonia, meningitis, and syphilis.
Part 1. Just how big is the “problem?” This series intends to tackle a range of subjects that afflict Veterans, especially suicide and drug overdoses which, along with diabetic lower limb amputations, are at epidemic levels. Across military medicine and traditional approaches to “mental health,” there is a wide gap between the palliative care model – control symptoms – and root cause analysis that gets at the physical damage and whole body wellness called for. This includes proper diagnoses and a shift to an appreciation of polytrauma and brain wound healing.
Part 2. Modern War is just so damned dangerous: BLAST Injury, Burn Pits, and the nature of whole body damage/polytrauma. Includes a primer on brain wounding.
Part 3. The VA/DoD Approach: Intrepid Center, DVBIC, Intrepid Spirit Centers, WRIICs, PREP, Care Coalitions, and Independent Wellness Centers.
Part 4. VSOs and the Growth of 66,000 Veteran Help Organizations since 9/11
Part 5. The insidious Service Member Epidemics: Suicide, Drug Overdosing, and diabetic foot ulcers, lower limb amputations, and the hundreds of thousands of deaths directly attributable to lack of informed consent.
Part 6. The Sports Industry: Making contact sports and life in general safer while engaging in a real scientific dialogue about brain wounding, the concussion cascade, "The Concussion Protocol,” and “the new normal” after brain wounding.
Part 7. Eisenhower didn’t even get it half right: The Military, Industrial, Contractor, Research, Academic, Lobbyist, Insurance, and Pharmaceutical Complex. Lessons in Bureaucratic Politics and how to sort out a path to success.
Part 8. Integrative/Functional/Wholistic/Complementary and Alternative Medicine. You don’t have to throw away institutions or current practices to make them better.
Part 9. Alternative Therapies: Hyperbaric Oxygen Therapy (HBOT) and a new paradigm in whole body healing.
Part 10. Alternative Therapies: Devices, Processes, Computers, and Artificial Intelligence.
Part 11. Alternative Therapies: Non-Prescription Drugs/ Psychedelics/Supplementation/Nutrition/Diet/Lifestyle.
Part 12. How to hold the Congress, White House, VA and DoD, and sports industry accountable for the Epidemics and lack of brain wound healing protocols.
Part 13. SUMMARY: The Shortest Paths to Success. How to change the language around “mental health,” arrest and reverse upward trends in deaths through suicides, prescription drug overdoses, lower limb amputations, and restore Quality of Life to brain wounded Veterans and citizens.
We welcome your comments.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#opioidepidemic#posttraumaticstressdisorder#PTSD#SuicidePrevention#TBI#traumaticbraininjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Text
Bad Trip: Expert says VA studies psychedelics but ignores proven Hyperbaric Oxygen Therapy!
Eye on Veterans
This week we’re talking with Dr. Robert Beckman, Executive Director of Treat Now dot org. He’s one of the premiere experts in the treatment of brain wounds with Hyperbaric Oxygen Therapy (HBOT). Although this technology is FDA approved for things like burns and diabetic foot ulcers, Beckman says the VA ignores proof that it's effective for treating brain wounds, TBI’s, concussions and depression which has fueled the suicide epidemic in America.
While ending suicide remains a top priority for VA , DoD, Beckman slams their decision to pump millions of mental health dollars into psychedelic research to merely treat symptoms. He offers several real-world examples of HBOT effectively treating the root cause and thus eliminating symptoms in ways current VA strategies do not.
In one powerful segment he shares how over the years the VA has amputated hundreds of thousands of feet, due to diabetic foot ulcers. Beckman claims most of which could have been avoided if HBOT was introduced earlier in their care.
He also shares vivid examples; NFL players treating concussions, combat veterans' fighting effects of toxic exposures and many clinics who are currently embracing HBOT therapy for treatment of brain wounds, PTSD and MS.
For more on Hyperbaric Oxygen Therapy including powerful research data and published studies, see TreatNow.org's website:
https://treatnow.org/
Read the latest newsletter "VA Continues to Avoid Treating and Healing Brain Wounds" here:
https://treatnow.org/va-continues-to-avoid-treating-and-healing-brain-wounds/
VIDEO: MSG Scott Rossler's HBOT testimony
https://youtu.be/N-CkR5shqEM?si=UmUhF_jKxPHjjzkq
VIDEO: NFL great Joe Namath shares how HBOT changed his life:
https://youtu.be/s7nxU3QadIA
To reach CBS Eye on Veterans, Host, Phil Briggs
[email protected]
Follow on X
@philbriggsVet
@EyeOnVeterans
Read the full article
#AirForce#ARMY#brainwound#brainwounds#concussion#currentevents#depression#HealingwithHyperbarics#marinecorps#military#MilitarySuicide#Navy#POLITICS#POPCULTURE#suicideepidemic#TBI#unitedstatesveterans#veteranaffairs#Veterans#VeteransAdministration
0 notes
Text
What the world knows that the VA does not: Hyperbaric Oxygen Therapy is safe, effective and can restore health

Athletes are waking up to the Use of Hyperbaric Oxygen Therapy for brain wound healing, health, endurance, peak performance, and the competitive edge.
Game Changer for Football Teams?
A high-profile college football program began using HBOT to manage player injuries and fatigue. The therapy quickly became a key factor in their injury management and prevention strategy. The team noted shorter recovery periods after injuries, and players were able to return to play faster than before, demonstrating HBOT's efficacy in a high-contact sports environment. Numerous professional athletes use HBOT.
100 Yards of Wellness Will Offer HBOT to Clemson Athletes
Nov 22, 2022
100 Yards of Wellness, Clemson’s new $4.9-million wellness space at Allen N. Reeves Football Complex that spans roughly 300 feet in length that has become a central hub of activity and major point of pride for Tiger football. The treatment and training room area includes all requisite athletic training resources, including a
diagnostic office with a full digital X-ray space and diagnostic ultrasound, general medical exam room, 30 yards of turf and hydrotherapy areas, including two underwater treadmills. Among the many features of the recovery center are:
• A hyperbaric chamber to create a pressurized environment for concentrated oxygen intake.
• A cryotherapy chamber for muscle recovery through extreme cold temperature exposure.
• A sensory deprivation float tank that houses 1,200 pounds of Epsom salt dissolved in water at skin temperature to remove athletes from light, sound and some gravitational force.
• Infrared hyperthermic Cocoon pods for Far-Infrared light therapy and vibrational massage.
• Photobiomodulation therapy beds that leverage multiple wavelengths of infrared light to reduce oxidative stress.
• Numerous massage chairs, including both percussive massage and hydromassage options.
• Percussive Hypervolt massage guns.
• Dedicated tables and space for practitioner-assisted stretching, percussive massage gun therapy and Normatec compressive sleeves provided to each player prior to the season.
• Functional testing equipment to obtain objective information on student-athlete muscle and joint function that can be used for injury prevention and return-to-play purposes.
The Rise of Hyperbaric Oxygen Therapy in Professional Football: A Game-Changer for Recovery and Performance
Sep 5, 2023
By Mudassir Sajad
In the fast-paced world of professional football, where every second counts, players are constantly seeking ways to gain a competitive edge. One such method that has been gaining traction is Hyperbaric Oxygen Therapy (HBOT). This innovative treatment has been endorsed by top-tier athletes like Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar, who have all been spotted on social media using hyperbaric chambers Hyperbaric Oxygen Therapy is proving to be a revolutionary treatment in the realm of
professional football. Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar endorsing its benefits, it's clear that HBOT is more than just a passing trend. Moreover as science continues to validate its efficacy, we can expect to see more football clubs
adopting this cutting-edge technology to give their players the competitive edge they need.
Dr. Joe Maroon on Hyperbaric Oxygen
Dr Joe Maroon Joseph Maroon is an American neurosurgeon, author, and triathlon athlete. He is the professor and vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center and is the current medical director of WWE. For over 20 years he has served as the neurosurgical consultant to professional and college athletes in football, baseball, golf, hockey and soccer and was team neurosurgeon to the Pittsburgh Steelers for over 40 years.
As early as 2011, Dr Maroon and Dr Bost wrote: "Alternative nonpharmaceutical treatments appear to be gaining acceptance for the treatment of common neurodegenerative conditions, memory decline, and reduced cognitive function. Substantial animal and human research now suggests that these same natural dietary supplements, vitamins and minerals, and the use of hyperbaric oxygen may be a better first-line choice for the treatment of PCS, which has generally been underreported by both athletes and the military."
Maroon and Bost, Concussion Management at the NFL, College, High School, and Youth Sports Levels. Clinical Neurosurgery. Volume 58, 2011, Chapter. 7.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
VA Continues to Avoid Treating and Healing Brain Wounds

2024 reminds us that the Veterans Administration continues off-course by avoiding actual brain wound healing while pumping more $$$$ into research, "Mental Health," and achieving a new normal. Meanwhile, the suicide rate continues upward.
ProPublica reports "How the VA Fails Veterans on Mental Health." In what has become an almost annual body count, investigative reporters analyzed 313 studies conducted by the VA's inspector general in recent years showing how repeated failures in behavioral care in the VA continue to lead to suicides.
"The problems appear to be systemic. Over and over, the hospitals and clinics in the VA’s sprawling health care network have fallen short when it comes to treating people with mental illness. . . . In the most extreme cases, facilities lost track of veterans or failed to prevent suicides under their own roofs."
Given the rise in the suicide rate among Veterans, the report veers into complicity when it states: "The system has notable strengths. The VA has played an important role in developing treatments for conditions such as post-traumatic stress disorder and traumatic brain injury, and provides critical training opportunities for psychiatrists, psychologists and social workers nationwide."
Combat Veterans constantly report to TreatNOW that they're treated like "guines pigs" by a constantly shifting and sketchy string of care providers. The ProPublica reporting indicates a severe breakdown in the VA's basic understanding of the physiology of brain wounds, repeating year after year that "mental health" is the issue. Recall that in too many cases the VA continues to insist on PTSD diagnoses for combat veterans without proof of brain damage.
And recruitment for understaffed medical professionals is for the Mental Health disciplines, not for a rethinking of how to properly diagnose and heal brain wounds. Physical healing has to replace psychology as the focus of standard of care for TBI.
And consider: The VA runs a number of War Related Illness and Injury Study Centers (WRIISC). This national program is dedicated to Veterans’ post-deployment health concerns and unique health care needs. They "develop and provide post-deployment health expertise to Veterans and their health care providers through clinical care, research, education, and risk communication. The WRIISC is part of VA’s newly designated Health Outcomes Military Exposures (HOME) formerly Post Deployment Health Services (PDHS). The VA is uniquely qualified to care for Veterans with health concerns related to potentially toxic exposures."
These Centers are allegedly the Gold Standard for delivering the world's best care for "the #1 clinical priority" in DOD and the VA: suicide prevention. But the protocols, research, and culture are opposed to even mentioning Hyperbaric Oxygen Therapy as even a consideration, let alone providing the treatment. At a minimum, they might consider putting some intellectual firepower behind a proper Phase 3 clinical trial to answer the outstanding questions about maximizing the efficacy of HBOT for Mild Traumatic Brain Injury Persistent Postconcussion Syndrome.
Days ago, the Department of Veterans Affairs issued an intention to study the use of certain psychedelic compounds in treating posttraumatic stress disorder (PTSD) and depression. The substances to be studied include psychedelic compounds such as psilocybin and Methylenedioxymethamphetamine (MDMA) when used in conjunction with psychotherapy to treat Veterans with PTSD and depression. This continues the VA's penchant to study "mental health" problems rather than solving them. As always, they revert to their inadequate interventions:
- Psychopharmacology
- Cognitive Processing Therapy (CPT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Prolonged Exposure (PE) or Trauma-Focused Psychotherapy
Adding yet more symptom-reduction chemicals and computer-based coping tools to the mix continues to avoid proper diagnosis and brain wound healing, particularly in the cases of combat veterans.
Here's the primer the VA needs to memorize. While this is not taught in medical schools, worldwide science supports these conclusions:
- TBI/Concussion/BLAST cause brain wounds.
- The pathophysiology of brain wounds includes a concussion cascade, a penumbra of damage that can lead to cell death and a host of behavioral, cognitive, memory and emotional problems. It is increasingly clear that CTE can be a result of this damage.
- Interrupting that cascade can halt and reverse the damage cause by inflammation, hypoxia, necrotic cell death, blood-brain barrier breakdown, and numerous other well-documented effects of brain wounding.
- Only by focusing on wound healing can a patient get on the path back to total body health, and a chance of pain- and drug-free living.
- Hyperbaric Oxygen Therapy (HBOT) is a proven, FDA on-label available intervention that reduces inflammation, leads to biogenesis, neurogenesis, angiogenesis, neuroplasticity, proliferation of stem cells, pain reduction, halts suicidal ideation, and allows patients to get off death-inducing drugs.
- Polytrauma -- a condition of multiple traumas endured by a patient -- is a complex of injuries typically suffered in BLAST injuries.
- Every Veteran with diagnosed or suspected brain wounds needs to be told that HBOT can help heal their wounds.
- And while the VA is waking up to the truth about healing vs. palliating, they should be required, under the mandate of "informed consent" to use HBOT for Diabetic Foot Ulcers.
- There are over 100,000 Veteran suicides since 9/11, and over 876,000 Veteran deaths attributable to lower limb amputations. The VA must be held accountable for using EVERY means available to stop the carnage.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#brainwounds#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#PTSD#suicide#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#VA#VeteranSuicide#VeteranSuicidePrevention#Veterans
0 notes
Text
Phoenix clinic receives grant for hyperbaric oxygen therapy to help veterans

Valley nonprofits underwrite therapy for veterans that the VA & insurance still won’t cover
Original Story & Video link: A veteran is praising a Phoenix hyperbaric oxygen therapy clinic for helping him and now it's gotten a grant to help more veterans heal their minds.
By Nicole Crites
Published: Nov. 10, 2023 at 8:16 PM EST
PHOENIX (3TV/CBS 5) — Too many of our heroes who served and sacrificed in our military are suffering in silence with PTSD. Now, Hyperbaric Oxygen Therapy of Arizona, an alternative treatment clinic in north Phoenix, can help more of them, thanks to a grant from Southwest Veterans Foundation for specialized therapy that’s still not covered by insurance or the Veterans Affairs Department. Patients we talked with say it should be because it saved their lives.
Valley Marine combat veteran Travis Blow keeps a snapshot of his medicine cabinet on his cellphone three years ago as a reminder of how far he’s come. “As a society, we’re OK with giving a whole bunch of drugs to veterans that already have issues because of what they’ve done and seen and most of those prescriptions have side effects of suicidal thoughts. You get stuck in a hole and can’t dig yourself out,” he said.
The photo shows baskets and shelves of bottles and 53 prescription medications he was taking twice a day for PTSD and other combat injuries. “Pain medication, depression and anxiety, anything that could help. And then I would have to take pills to counteract some of the pills that I was taking,” Blow said. “It was a nightmare.”
Nothing was working. He did two tours in Fallujah, where his best friend died in his arms. “We really didn’t mourn that loss because we had missions to do. You have to bury it down and keep moving,” Blow said. He lost even more battle brothers to suicide after returning home and came close to doing the same himself.
Even with a wife and son, Blow couldn’t see a way out. “I had a plan. I knew where I was going to do it and I knew when I was going to do it,” he said. Then he got a phone call that changed everything.
Valley Gold Star Mom Debbie Lee, who started America’s Mighty Warriors to honor her son who was the first Navy SEAL killed In Iraq, paid to get Blow into hyperbaric oxygen therapy. “After the first 10 sessions, I was sleeping. I slept for probably 10 hours when before I was only sleeping three, maybe four hours,” he said.
Lori Klauber runs Hyperbaric Oxygen Therapy of Arizona and showed us how it works. The pressurized chamber looks like a submarine capsule. It pumps in 100% pure oxygen while you’re at the equivalent of being up to 66 feet below sea level. “The pressure dissolves the oxygen into the plasma, cerebral spinal fluid and all the clear liquids in the body. So, if the cells are functioning at a higher level, things are going to heal,” Klauber said.
It’s FDA-approved for more than a dozen ailments, from carbon monoxide poisoning to diabetic neuropathy. And while several studies have shown it can help with PTSD and TBI, it’s not covered by insurance or the VA. “I don’t understand why it’s not better accepted. But it should be,” Klauber said. “I see so many of these guys, that it makes such a difference in their life. And it’s just very rewarding.”
“I’m here today because it works,” said Blow. Blow managed to wean himself off all but two of those 53 prescriptions. It’s a point of pride he wears with a metal band stamped with the names of his fallen brothers on his wrist. “I’m just grateful to be alive. And now I can actually honor my brothers in the right way, by living the best life I can.”
Some states have set aside money specifically to cover this kind of treatment for veterans. Arizona lawmakers did as well, but Gov. Doug Ducey pulled the funding from that bipartisan effort in a line-item budget veto in August 2022. State house lawmakers are pushing to revive that effort and congressional lawmakers have a bipartisan measure working its way through D.C. right now to try and launch a pilot program with the VA to offer hyperbaric oxygen therapy treatments for PTSD.
Read the full article
#brainhealth#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#opioidepidemic#pharmaceuticals#posttraumaticstressdisorder#PTSD#TBI#TBItreatment#Veterans
0 notes
Text
CTE Plagues Heisman Trophy Winners and Families

Three-quarters of 1,035 brains of football players -- over 700
--examined at Boston University had CTE
The "taboo topic" is the centerpiece of "The Other Heisman Club" in the Washington Post, Dec 9, D1, by Kent Babb: the number of former Heisman winners with diagnosed or suspected Chronic Traumatic Encephalopathy (CTE). The degenerative brain disease is increasingly in the news for a number of reasons.
Four Heisman winners have been posthumously diagnosed with the disease: Howard Cassady, Pat Sullivan, Paul Hornung and Charles White. The implication in the article is that more winners already exhibit symptoms of CTE but whose families can't "know" until after death. But the families know.
Something is wrong. Sadly, silence is the preferred approach. And the unwillingness of our society to confront the obvious doesn't make it any easier. And the "whistling through the graveyard" approaches to concussions and the Concussion Protocols used worldwide don't provide much guidance about an alternative approach to Brain wounding. Facts matter:
- Four percent of Heisman trophy winners died of CTE, and the list of their wounded fellow winners is growing. If you extrapolate those numbers to the 25,000 former NFL players, over 1,000 of them are probably carrying the CTE markers.
- Three-quarters of 1,035 brains of football players, 0ver 700, examined at Boston University had CTE.
- Researchers at Boston University found CTE in 92 percent of former NFL players who were analyzed: they analyzed the brains of 376 deceased former NFL players and diagnosed 345 of them with chronic traumatic encephalopathy.
- More than half of the homeless have experienced traumatic brain injury and 1 in 4 have had moderate to severe brain injuries.
- Approximately 876,450 post-9/11 veterans suffer from untreated brain wounds.
- Researchers estimate that as many as 60% of incarcerated individuals are living with TBI, significantly higher than the 8.5% reported in the general population.
- Studies on prison and jail populations have reported a range of 25-87% of inmates reporting head injuries or TBI.
Of course, it is traditional to attack these numbers. Nay-sayers will demand more research. Hand-wringing by stake-holders on both sides will, like protests after mass-shootings, last a while and then subside. If anything, more dollars will go into researching how to make contact sports more safe. And treatments that are non-pharmaceutical will be ignored. Since "everyone knows there's no treatment for brain injuries," the best we can hope for from the medical profession is contained in the latest proceedings out of Boston.
The Robert C. Cantu Concussion Summit was held on December 8, 2023, at the Cantu Concussion Center at Emerson Hospital in Concord, MA. The theme of the conference was "Prevention of Concussion and Long-Term Effects of Repetitive Traumatic Brain Injury (RTBI)." In what is becoming a repetitive list of findings, the conference summarized:
- Eliminate intentional or avoidable head impact in contact and collision sports in both practices and games.
- Encourage policies and rules that limit the number, duration, and intensity of contact sport practices.
- Reinforce proper and safer techniques that avoid head contact at all levels of play.
- Implement rules of play that reduce and penalize intentional or avoidable contact to the head and neck.
- Correlating specific clinical symptoms with CTE neuropathology remains an important area for further investigation.
- Improve the criteria for Traumatic Encephalopathy Syndrome (TES) through further research.
Feel better? More importantly, if you are the parent of someone with a brain wound, what actionable intelligence can you take from that list? How will that list help you and yours deal with the here-and-now of a TBI/Concussion-suffering loved-one? If you'd like to learn more about what is happening, and what you can do, view this earlier Blog. Additional information is here.
Below is an insightful film about brain wounds
https://youtu.be/Zzbxrnm7jXc?si=IPKC5InadR0Eho52
https://treatnow.org/brain-wound-update-5-concussion-blast-tbi-cte/
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
NYT: Friendly Fire Leads to Brain wounding

Pentagon researchers say weapons like shoulder-fired rockets expose troops who fire them to blast waves far above safety limits, but they remain in wide use.
As we have reported for years, BLAST injury does not respect your nationality, gender, origin of the weapon, or your intention. As Dave Philipps of the New York Times reports, U.S. Troops are still training on weapons with known risks of delivering brain wounds.
As Phillips reports, studies by the Navy, the Center for New American Security, the Swedish military, DoD, SEALs, DARPA, Johns Hopkins, and UHUHS all warn of real damage inflicted by "friendly fire".
The search, research, measurements, data bases, added budgets, and periodic expressions of concern from DoD leadership can be viewed in one of two lights: they know and they don't care; or, they know and they dont' know what to do in the interim. Modern warfare, as Ukraine proves daily, requires more and more destructive firepower just to defend territory, let alone regain strategic and tactical advantage.
So, what can done in the interim? "For generations, the military assumed that this kind of blast exposure was safe, even as evidence mounted that repetitive blasts may do serious and lasting harm. . . . Top leaders talk of the importance of protecting troops’ brains, but the military fails to take practical steps to ensure safety."
Literature on BLAST injuries over the past decade overwhelmingly tends in the direction of Recommendations to find ways to protect soldiers with new and improved helmets, reduced weapon firings, education, more research, more funding, and, over time, resort to robots to do the heavy firing.
Sadly for the soldier, for 100 years we've known that BLAST causes brain wounds. Even though a century of research has not definitively "proved" the Mechanisms of Action involved in causing physical, mental, behavioral, cognitive, and moral damage, we do know that the net effects of only palliating symptoms won't lead back to a normal, healthy brain.
So here's a list of helpful suggestions to DoD/VA to help Warriors, Veterans, indeed anyone exposed to BLAST injury or brain wounding. Let all the research continue on mitigating the potential and actual damage caused by exposure to BLAST. Add more drugs and hallucinogenics and psychotropics to the list of possible "solutions." But let's focus some of our work on healing the wounds to the brain and body caused by BLAST exposure. An estimated 877,000 Veterans and active duty service members -- probably many more as we learn about the pervasiveness of self-inflicted BLAST injury -- are already suffering with some degree of brain wounding. Let's focus on HEALING THEIR BRAIN WOUNDS as we work the prevention side of the equation. Here's a modest proposal:
Daily suicide rates, accumulating suffering, and impacts on families demand that we deal with brain wounds. We cannot continue to ignore treatments that work are safe, scientifically validated, and readily available. We cannot hide this information from the wounded. Informed consent and medical ethics demand that DOD/VA tell the wounded what is available, even though it is "off-label." Every treatment, drug, process, procedure, device and protocol currently used by DoD/VA is off-label and not approved by the FDA for treating TBI/PTSD.
Keep doing what you're doing. But hold open the possibility that alternative therapies exist that are scientifically valid, clinically proven, widely available, cost effective and demonstrated safe and effective. Fund them.
Rethink a Suicide Prevention Strategy that is void of any options to treat brain wounds. Too may Veterans commit suicide -- over 109,000 -- perhaps falling into depression from undiagnosed and untreated brain wounds.
Hyperbaric Oxygen Therapy (HBOT) is one such therapy, backed by decades of research, acceptance by the FDA for wound healing, and proven in multiple scientific studies to reduce or eliminate symptoms caused by TBI/PTSD/Concussion/BLAST.
HBOT is proven to reduce and/or eliminate suicidal ideation in tens of thousands of uses .
Read, really read, the current scientific literature on the validity of objective research conducted over the past fifteen years. Notice that the UHMS and the overwhelming number of real HBOT researchers know that HBOT works to help heal TBI/PTSD. Even government researchers, a few of whom still cling to the canard that "HBOT does not work," accept that patients in their studies got better .
If necessary, take 10% of the VA drug budget and use it to fund HBOT treatments in private clinics where the cost is miniscule compared to current standards of care. It is a well-known fact that fully treated HBOT patients get off almost all their drugs, many of which warn of "ideation of suicide." There will be a net return of billions of dollars to the VA bottomline due to reduced need for prescriptions.
Redo your cost analyses when considering where to spend dollars on rehabilitation of brain wounded combat Veterans. It has been calculated that the cost of NOT treating brain wounded Veterans will exceed $4Trillion over their 40-year lifespan. That's a degraded life, for the Veteran and the family, living with symptoms that plague far too many Veterans. For less than 1/2 of 1% of that cost, all 877,450 brain-wounded Veterans can be fully treated with HBOT.
DoD and the VA should insure and reimburse HBOT-for-TBI treatments. Start with Informed Consent: let every Veterans know that HBOT can help heal their brain wound.
And consider the following: service members returning from combat suffer from polytrauma unlike ever before. Knowing what we know now about the prevalence of BLAST injury, Burn Pit toxins, unreported brain trauma, the sustained pace of combat for Special Operations warriors, we need to provide functional medicine approaches to whole body wellness, starting with but not limited to brain wounds. All body systems are negatively affected by BLAST. HBOT works to relieve pain, reduce inflammation, speed healing, restore function, promote the growth of new stem cells, and allow battle-weary warriors to return to peak performance more quickly.
Part of the history of HBOT is that the history of HBOT safety and efficacy is ignored or forgotten. This is a page out of the Textbook of Military Medicine, updated in 2006. This same algorithm is in the textbook in the 1980s. The “definitive therapy” then and is HBOT treatment for TBI resulting from BLAST Exposure.

The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#concussionprotocol#ConcussionSymptoms#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaric#hyperbaricoxygen#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#posttraumaticstressdisorder#PTSD#suicidalideation#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#TraumaticBrainInjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Text
Idaho Outdoor Fieldhouse & Summit Hyperbarics & Wellness

The J.A. and Kathryn Albertson Family Foundation is the vision and the support behind the IDAHO OUTDOOR FIELDHOUSE in Boise ID
Veterans Day weekend saw the ribbon-cutting at the Idaho Outdoor Fieldhouse (IOF) in Boise Idaho, along with the introduction of the companion Summit Hyperbarics and Wellness Center.
For over a decade, Idaho has been served by exceptionally veteran-friendly HBOT centers in Sun Valley and Pocatello, along with the Healing Centers in Boise, Malad City, Twin Falls, and Burley. Hundreds of Veterans have been helped to heal their brain wounds in Idaho, including many of the leaders behind IOF.
The vision of the Idaho Outdoor Fieldhouse is to provide opportunities to pursue well-being through outdoor activities and athletics, and to create collaborative experiences that strengthen a diverse community by supporting health, education, employment, and engagement in a uniquely inspirational setting. The focus is on challenged and adaptive athletes of all ages, veterans, and first responders, with outreach to the entire Idaho population.
The Fieldhouse is supported by the JAKA Family Foundation, Mission43, and the Challenged Athletes Foundation - Idaho. This partnership has come together on a seven acre complex near to downtown Boise on the Boise River. Started in 1966, the Board of the JAKA Family Foundation is committed to making Idaho an exemplary model for innovative learning, a destination for accessible world-class recreation, and the most desirable state for life after the military.
Mission43 provides servicemen, women, and military spouses opportunities to succeed in Idaho after the military through the pillars of EDUCATION, EMPLOYMENT, and ENGAGEMENT.
It is the mission of the Challenged Athletes Foundation (CAF) to provide opportunities and support to people with physical challenges, so they can pursue active lifestyles through physical fitness and competitive athletics. The Challenged Athletes Foundation and Mission43 believe that involvement in sports at any level increases self-esteem, encourages independence and enhances quality of life.
And now, with the installation of Summit Hyperbarics & Wellness, the combined history, focus, impetus, and Missions and Visions of the Idaho Outdoor Fieldhouse participants are joined with a world-class medical team practicing Hyperbaric Medicine. The Fieldhouse Consotium will help heal brain wounds and other physical, behavioral, emotional, psychological, spiritual, mental, cognitive, and moral injuries and obstacles of combat veterans and citizens of Idaho.
It is no coincidence that numerous members of Mission43 are recipients of Hyperbaric Oxygen Therapy and are living testaments to the healing power of Oxygen Under Pressure.
It is a tribute to the J.A. and Kathryn Albertson Family Foundation, and to the team they have assembled, that Idaho is doing the needed work to innovate in a space where its citizens can receive better-than-normal care, encouragement, and opportunity.
Roger Quarles, Executive Director of the J.A. & Kathryn Albertson Family Foundation, expressed his pride and enthusiasm, stating, "It's a campus designed to redefine boundaries, shatter barriers, and create a future where individuals, regardless of ability, can thrive in a world-class recreational environment."
And as the medical team at SUMMIT and the TreatNOW Coalition would add: "A healed and healthy brain is the best antidote to suicidal ideation and a path to restored life."
For more information, contact the Idaho Outdoor Fieldhouse at 877-574-7494 or Email [email protected]
**********
The information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#ChallengedAthletesFoundation#HBOTcenters#HBOTTreatment#HealingwithHyperbarics#hyperbaric#hyperbaricchamber#hyperbaricoxygen#HyperbaricOxygentherapy#IdahoOutdoorFieldhouse#JAKAFamilyFoundation#Mission43#suicidalideation
0 notes
Text
USJAG: Special Update

USJAG & CBS NEWS: National Guardsmen fight to get injury claims approved and disability benefits
CBS National News Story w/Catherine Herridge
A joint investigation by USJAG and Catherine Herridge, Senior Investigative Correspondent for CBS News, aired on Friday, November 10th, and revealed the following:
- National Guard Bureau is overturning at least 30% of “In the Line of Duty” Determinations without authority and evidence. This is used to deny Military Disability Retirement Benefits, thereby violating the Right to Due Process under the 5th Amendment to the Constitution of the United States of America.
- Injured Air National Guard and Air Force Reserve Service Members are denied active duty military status, pay, healthcare, and benefits in direct violation of Title 10 United States Code.
- The National Guard Bureau and U.S. Air Force weaponize the Line of Duty Determination process and Disability Retirement System to deny injured Service Members DOD retirement and VA Disability benefits.
- The Senior Leadership of the National Guard and the U.S. Air Force are aware of these injustices and refuse to correct them. The DOD & Air Force Inspectors General also refuse to conduct objective investigations, so no one is held accountable.
CBS MORNINGS
BY CATHERINE HERRIDGE, KERRY BREEN
November 10th, 2023
Nearly half a million Americans serve in the National Guard, with more than 40,000 engaged in missions around the world. But CBS News has uncovered cases where service members say they were injured in the line of duty face an uphill battle to get health benefits and pay.
According to the most recent data obtained by CBS News, about 30% of injury claims that are recommended by local commanders are determined not to qualify by the Air National Guard, raising questions among service members about whether correct policies and procedures are followed.
One of those veterans is Master Sergeant Jim Buckley, whose family has spent three generations serving in the military.
"It's infuriating," Buckley said. "You're shouting into the wind, and nobody's listening."
After tours in Iraq and Africa, Buckley says that he injured his shoulder during a physical fitness test in 2019. While he said he initially dismissed it as a "minor inconvenience," the shoulder wound up needing surgery a year later. Another physical turned up a sleep disorder, migraines and hypertension — all conditions that Buckley said he didn't have before his military service.
Unlike the active component of the military, the National Guard requires paperwork to determine that the injury happened or was aggravated while serving. While his shoulder injury was eventually approved, Buckley said he struggled to get his other medical issues recognized for benefits, or what's called a line-of-duty determination.
"If you don't have the line of duty, it's like the injury didn't happen," Buckley said. "You're on your own. You're taking care of the injury. You're footing the bill."
After Buckley was taken off military orders, he says his family lost his military health insurance and his monthly income of $4,000. It's been "a great hardship," he said.
Jeremy Sorenson also served in the Air National Guard as an F-16 and A-10 pilot. He now advocates for injured service members through the nonprofit USJAG.org. Sorenson told CBS News their team is already working with 15 similar Guard cases.
"Jim Buckley is representative of what we believe to be thousands of service members that are being mistreated," Sorenson said.
Buckley's paperwork indicates his Air Guard command in Mississippi backed up his injury claims, but the final call was made by the Air National Guard. He told CBS News that he has not seen any evidence to support the determination made by the Air National Guard.
In October, Buckley was in a dark place. Just minutes before midnight, he wrote the Air Force Secretary and National Guard senior leadership. He said in the email that he was "drowning" and "reaching out for your help," begging that the officials "not turn a deaf ear and a blind eye."
"It's coming from a place of pain in my heart," Buckley said. "The last thing I ever wanted to do was get injured. I would have served until I was 60."
A National Guard spokesperson told CBS News that Buckley was provided with evidence to back up the injury denials, adding that "a review of the medical records and application of accepted medical principles led the Air Reserve Board to conclude these conditions existed prior to service."
Buckley said the struggle to get his injuries covered has made him rethink his family's service. Now, he no longer wants his 16-year-old son, Matthew, to join the National Guard.
"Years ago, I would've had a much different answer. The furthest thing I can think of is him joining the military," Buckley said. "I'm so conflicted in saying that, because my grandfather, my father, myself (all served), and I'm very proud of the service, and love the military. But to think that he could be put through the wringer — all it takes is one injury."
CBS News has learned both the Defense Department and Air Force internal watchdogs have open cases into Buckley's allegations, which include abuse of authority and failing to provide evidence to back up the final determinations.
* * * * * * * * * * * *
The TreatNOW Coalition's pro bono Mission is to end service member suicides. The USMC reported this week that suicides are at an all-time high. TreatNOW HBOT Coalition clinics have demonstrated 100% safety and over 90% success in treating over 21,000 service members, Special Operators, first responders, athletes, and citizens with TBI/PTSD/Concussion. Brain Wounds like those described here can be successfully and safely treated and helped to heal with HBOT.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW.
The information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#braininjury#concussion#disabilitybenefits#HBOT#hyperbaric#HyperbaricOxygentherapy#MilitaryDisabilityRetirementBenefits#posttraumaticstressdisorder#PTSD#TBI#traumaticbraininjury#VA#VADisabilitybenefits#Veterans#VeteransAffairs
0 notes
Text
New York Times: USMC Blast Injury Update

Partial Explanation why Marines report Highest Suicide Rate since 2011, Navy since 2019
Dave Philipps, Pulitzer prize-winning and NYT reporter, has filed another report on continuing investigations into BLAST injury. He does it through a look at the US strategy of using firepower to destroy ISIS in Iraq and Syria. "A Secret War, Strange New Wounds, and Silence From the Pentagon" tells a sad tale but neglects a open secret: blast injury has been known for decades to cause brain wounds. "Strange New Wounds" have been known for fifteen years as "THE INVISIBLE WOUNDS OF WAR."
"An investigation by The New York Times found that many of the troops sent to bombard the Islamic State in 2016 and 2017 returned to the United States plagued by nightmares, panic attacks, depression and, in a few cases, hallucinations. Once-reliable Marines turned unpredictable and strange. Some are now homeless. A striking number eventually died by suicide, or tried to."
Too many of the wounded were forced out of the military without any medical help. The Epoch Times did a long two-part report on the same maladies caused by the deployment that led to tens of thousands of concussive friendly-fire BLAST waves hitting the artillerymen. The stories in the Epoch Times drew attention to the work of USJAG. Robert Alvarez, Nic Gray, and Jeremy "Weed" Sorenson are doing the heavy lifting exposing the unreported brain wounding and the downhill slide into Other Than Honorable discharges for too many of these wounded warriors. USJAG and a few intrepid reporters are uncovering the systemic flaws in our "mental health" approach to unrecognized physical damage wrought by war. And they are seeking redress of the further damage done by bureaucracies ignorant of the pain and suffering of the brain wounded.
The military and the VA continue in their willful ignorance about the reality of brain wounding and the scourge of TBI/PTSD injuries going unreported, undiagnosed, and untreated. Worse, lacking a service-wide education about the reality of brain wounding and its impact on behavior and performance and readiness of individuals, and the force more broadly, the wounded will continue to be mistreated by a medical community and command structure that has little sense of urgency about the need to treat brain wounds.
A curious and ineffective response has set in, reminiscent of the dilatory approach to Burn Pits and Agent Orange. "Paralysis through analysis" has taken hold once again. "We need to study the problem." "We just don't know enough yet." Meanwhile the suicide rate continues its upward trend and the researchers claim they need more time and money before they can even know what has happened. Time and again, the focus is on diagnosis, to the detriment of the wounded who continue to deteriorate, without even health insurance, disability payments, and an end to their careers. And treatments that have been proven safe, effective, and low-cost -- and which can be employed immediately -- are disdained as unproven, unsafe, too risky, too costly, and lacking in evidence. The simple fact is that medicine is willfully ignorant about hyperbaric medicine and likely to stay that way, despite overwhelming evidence, without intervention by Congress and the White House, as with Burn Pits.
Here are five take-aways from the NYT study:
** To defeat ISIS, the United States relied on artillery crews firing more intensively than any had in generations.
** Many members of the gun crews developed devastating and puzzling symptoms.
** When the troops started to act strangely, they were often treated ineffectively or punished.
** Studies are starting to reveal the risk posed by blast exposure, but progress is slow.
** The military says it now has safeguards to protect from blasts, but it is not clear that much has changed.
Here are five ALERTS to those who are still wondering if BLAST injuries exist. Brain wounding from friendly fire is not merely a Mental Health issue. Impaired performance is not the the victim's fault due to personal weakness, nor is it amenable to talk therapy and drugs that merely mask symptoms.
** The ground-breaking 2016 Lancet study sponsored by the Defense Health Program of the United States Department of Defense states: "scientific literature from the past 100 years shows that a substantial percentage of blast-exposed service members have persistent neurological or behavioral symptomatology."
** Breacher Syndrome and "Operator Syndrome" are real. Science and research will catch up to reality on the ground, facts which should be obvious to anyone paying attention.
** The modern Carl Gustav recoiless rifle, in operation since at least 1984, comes with warnings not to fire more than six rounds in a 24-hour period. The Danes seem to have understood BLAT damage four decades ago.
** Shoot rooms instructors and EOD personnel are well-known to suffer inordinately from recurring blasts and subconcussive impacts over years of exposure -- not unlike athletes subjected to repetitive head impacts.
** The "Invisible Wounds of War" are no longer "invisible" to anyone who cares about "root cause analysis". While brain wounds happen inside the head (and are frequently part of the polytrauma of combat), they can be "seen" via scans, functional and physiological outputs, symptom recognition, self-reporting, and careful diagnostics. Neglecting to diagnose and to treat brain wounds while waiting for more science in the face of a suicide epidemic is essentially medical malpractice. We KNOW, and we choose to shift the blame onto the victim or the "inadequacy" of scientific research.
Continuing malfeasance. US troops at two airbases in Iraq were injured during a Jan. 8, 2020 Iranian missile attack on Al Asad Air base. Once again, even years after Blast injury was finally recognized as a direct cause of brain wounds the US initially declared that no one was hurt in the attack. Dozens of diagnoses later, we now recognize BLAST injuries riddled those under the hail of missiles. (Just imagine the damage being done in Ukraine and the Middle East.)
One is reminded of the early military culture around Burn Pits: "nothing to see here; no damage." We know more now, and the VA, at least, presumes that proximity to Burn Pit toxic clouds causes physical damage and accepts responsibility to treat and help heal that damage. How long will it take the DoD and the VA to recognize that Blast damage is real, and can cause physical wounds to the brain and body? Further, how long before they link brain wounds to suicidal ideation? And that there is a treatment -- Hyperbaric Oxygen Therapy (HBOT) -- that virtually eliminates suicidal ideation and helps heal those brain wounds without drugs and other ineffective interventions?
The TreatNOW Coalition, alongside USJAG, has begun working with some of the casualties of the bombardments. USJAG are the pro bono advocates for those accused of Other Than Honorable behavior and subjected to fraudulent and penalizing discharges.
* * * * * * * * * * * *
The TreatNOW Coalition's pro bono Mission is to end service member suicides. The USMC reported this week that suicides are at an all-time high. TreatNOW HBOT Coalition clinics have demonstrated 100% safety and over 90% success in treating over 21,000 service members, Special Operators, first responders, athletes, and citizens with TBI/PTSD/Concussion. Brain Wounds like those described here can be successfully and safely treated and helped to heal with HBOT.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
The information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#blastinjury#braininjury#Brainwounding#concussion#HBOT#hyperbaric#HyperbaricOxygentherapy#Lestweforget#memorialday#mentalhealth#oxygen#posttraumaticstressdisorder#PTSD#suicideepidemic#SuicidePreventionFunding#TBI#traumaticbraininjury#VA#VeteranSuicide#Veterans#VeteransAffairs
0 notes
Text
Lest We Forget, 2023

NOV, 2023: Pentagon Reports Marines see Highest Suicide Rate since 2011, Navy since 2019
War Statistics, Military.com
Over 15,000 Americans are estimated to have died in wars since 9/11, with hundreds of thousands wounded in visible and invisible ways: 877,450 brain wounded veterans either misdiagnosed or undiagnosed, all untreated by the VA/DoD for their brain wounds.
Twenty-three years of war in Afghanistan, Iraq, Syria and Pakistan have cost American taxpayers over $6 trillion according to the Watson Institute of International and Public Affairs at Brown University. More than 800,000 people have died as a direct result of fighting. (Brown COW).
The HOW Foundation, GruntStyle, America's Mighty Warriors, the 22 Project, BurnPits360, the HUGS Project, KOTERRA, PFRPA, Stand for the Troops, over 145 clinics, and the TreatNOW Coalition remind us of other statistics that get lost too often.
16 - 44
Estimated Veteran Suicides Each Day
~109,000
Veteran deaths from SUICIDE since 9/11
642,000
Veterans dying every year
15,000+
US military, DoD civilians,
and US Contractors killed post-9/11 in Iraq,
Afghanistan, Pakistan & Syria
~109,000
Veteran deaths from prescribed drug overdoses
2.5 million+
Served in OEF, OIF, OND
30%+
Suffering From PTSD
877,450+
Suffering From Untreated TBI/Brain Wounds
80%
Combat Veteran Divorce Rate
Crisis Line 988
Since launch in July 2022 through May 2023, 988 has received almost 5 million contacts, of which nearly 1 million are from the Veteran's Crisis Line—a part of 988—with the rest consisting of 2.6 million calls, over 740,000 chats, and more than 600,000 texts
22%
Increased Likelihood of Suicide
Among Veterans vs. all others
Congress, the VA and DoD can and must do better. We can arrest the suicide rate among all Americans. The Opioid and Substance Abuse epidemics can likewise be reversed if and when we accept what science and research and clinical/evidence-based medicine are telling us, all over the world. The use of Hyperbaric Oxygenation (HBOT), together with Integrative Medicine and other safe and effective therapies, are in use and available today. (Evidence)
21,000+
Brain-Wounded Service Members given a
restored Quality of Life after HBOT treatment,
all through Donations and Pro Bono work
The information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#braininjury#concussion#HBOT#hyperbaric#HyperbaricOxygentherapy#Lestweforget#memorialday#mentalhealth#opioid#opioidepidemic#OUD#oxygen#pharmaceuticals#posttraumaticstressdisorder#PTSD#suicideepidemic#SuicidePreventionFunding#TBI#traumaticbraininjury#VA#VeteranSuicide#Veterans#VeteransAffairs
0 notes
Text
BRAIN WOUND UPDATE #17: Military Suicides: Rates gradually increased from 2011 to 2022

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
IMPROVE DELIVERY OF MENTAL HEALTH CARE:
"DoD aims to deliver the highest-quality clinical health care services."
Once again, we have to repeat: At some point, DoD, the VA, and medicine in general will hear the drumbeat of data in peer-reviewed science attesting to the advantages of treating and healing undiagnosed and untreated brain wounds. But "root cause analysis" as a prerequisite to understanding the physiological underpinnings of many suicides will have to await a more enlightened team of analysts, given the lack of a comprehensive and integrated attempt with this latest: ANNUAL REPORT ON SUICIDE IN THE MILITARY CALENDAR YEAR 2022.
The Report states that "Suicide is multifaceted, and suicide prevention needs a comprehensive and integrated approach. Thus, DoD aims to:
► Foster supportive environments.
► Address stigma as a barrier to care.
► Improve delivery of mental health care.
► Promote a culture of lethal means safety.
► Revise suicide prevention training"
Digging deeper on "Improve delivery of mental health care," the reader is left wondering how the Defense Suicide Prevention Office continues to assume that brain wounds are Mental Health issues amenable to non-FDA-approved interventions for brain wounds. Nothing the DOD Mental Health System of VA does for brain injuries is approved for Traumatic Brain Injuries (TBI). And TBI has been shown to be a direct contributor to suicidal ideation, amenable to healing with HBOT.
The shortcoming of NOT calling out brain wounds -- diagnosed or not -- as a contributor to suicidal ideation reminds this author of the case of COL Shawn "Norm" Pederson (USAF, ret). The former lead solo pilot in the Thunderbirds, a 23 year Veteran and recognized fast-burner, suffered a ruptured cerebral aneurysm just three weeks after retiring in 2014. Nine years later, the COL is a ward of his mother and brother, who, according to the terms of the US Suicide Prevention Office, is suffering from mental health problems.
To be sure, COL Pederson has mental health challenges, but his brain is damaged. He suffers from a physical wound to his brain. Yet after only a few years, the medical system declared there is no more they can do for him. He is deemed totally disabled and is in the care of his 85-year old mother, may the heavens smile upon her.
Leaving aside how we're going to intervene to help, his story is little different from active duty and Veteran service members who have been relegated to the inadequate standard of care available for chronic TBI/post concussive syndrome. It is failing. We continue to get requests for help from Veterans and active duty Special Operations . Yet thousands of success stories, positive peer-reviewed data, worldwide adoption, and clinical evidence are inadequate to break through at the official level.
A more thorough Suicide Prevention Strategy should report on efforts to properly diagnose and heal brain wounds, across the board. As we've reported, it was surprising to us that the Suicide Prevention and Response Independent Review Committee ignored our recommendations, and failed in a 16-page chapter on Treatment and Support Services to even mention better diagnoses and brain wound healing fundamentals.
After the hundreds of millions of dollars spent on Suicide Prevention strategies, research, outreach, 988 crisis lines, recruitment, and collaboration efforts, the 877,450 brain wounded Veterans deserve more than to be told that they have to get used to their new normal. Perhaps some of the billions of dollars allocated to Suicide Prevention could be usefully given over to healing brain wounds.
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made
Read the full article
#brainhealth#braininjured#braininjury#concussion#HyperbaricOxygentherapy#mentalhealth#oxygen#pharmaceuticals#posttraumaticstressdisorder#PTSD#suicide#suicideepidemic#suicideideation#SuicidePrevention#TBI#traumaticbraininjury#VA#VeteranSuicide#VeteranSuicidePrevention#Veterans#VeteransAffairs
0 notes
Text
BRAIN WOUND UPDATE #16: More Evidence: Untreated TBI ties to Cardiovascular, Endocrine, Neurological, and Psychiatric Disorders

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD
"There comes a point where we need to stop just pulling people out of the river. We need to go upstream and find out why they're falling in."
Bishop Desmond Tutu
At some point, DoD, the VA, and medicine in general will hear the drumbeat of data in peer-reviewed science attesting to the damage done by untreated brain wounds. Fortunately for those lucky few, the role of Hyperbaric Oxygenation to help treat and heal their brain wounds has given them new lives. But the practitioners of conventional medicine are not ready to accept facts and evidence. The DOD and the VA claim that the suicide epidemic is their #1 clinical priority, yet they drag their feet, avoiding using HBO therapy that virtually eliminates suicidal ideation. And they seem not to have read recent science about symptoms and "mental health" diagnoses that mask undiagnosed brain wounds. While the suicide epidemic continues to escalate, DOD and the VA spend more and more on strategies to think harder, collaborate more, pay attention, fund more Call Centers, and get the word out: precious little on healing brain wounds.
Consider these recent reports.
This report in JAMA, Association of Traumatic Brain Injury With the Risk of Developing Chronic Cardiovascular, Endocrine, Neurological, and Psychiatric Disorders, found that patients with mTBI and msTBI were at increased risk of developing long-term cardiovascular, endocrine, psychiatric, and neurological comorbidities. The risk of post-TBI comorbidities was higher in all age groups compared with an age-, sex-, and race-frequency–matched unexposed group, and notably so in patients younger than 40 years. Comorbidities after TBI were associated with higher mortality.
Another JAMA study, Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts, found that young contact sport athletes may be at risk for long-term neuropathologic disorders, including chronic traumatic encephalopathy (CTE). This one bears reading by parents.
A third study in the New England Journal of Medicine, Neuro-degenerative Disease Mortality among Former Professional Soccer Players, found that mortality from neurodegenerative disease was higher and mortality from other common diseases lower among former Scottish professional soccer players than among matched controls. Dementia-related medications were prescribed more frequently to former players than to controls.
And an ironic report from Front Office Sports, the NFL court drama shows how little we've progressed from science-scepticism. In a bid to avoid reimbursing the NFL for payouts to brain wounded players, major insurers deployed medical experts to argue that there’s no scientific evidence linking head injuries with neurocognitive disorders, such as Amyotrophic Lateral Sclerosis (ALS), Alzheimer’s, and Parkinson’s, covered in the settlement. They further suggested that up to 40% of the now 1,663 former players who have received payments may have overstated and even feigned their symptoms.
This tactic is mirrored in the behavior of DOD components that continue to discard combat veterans with the National Guard with Other Than Honorable Discharges and claims that the petitioners either weren't on active duty when they were injured, can't document injuries they were encouraged to not report to stay in the fight, or are faking their injuries.
Of the five Defense Department service branches, only two met their active-duty enlisted recruiting goals for fiscal 2023 -- the Marine Corps and the Space Force, by far the smallest services and with the lightest recruiting burden. The others, the Army, Air Force and Navy, fell short. Coincidence?
##########
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#CardiovascularDisorder#concussion#ConcussionSymptoms#EndocrineDisorder#HBOT#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#NeurologicalDisorders#PsychiatricDisorders#TBI#TBItreatment#TraumaticBrainInjury#Veterans
0 notes