Photo
New Post has been published on https://sydneyentclinic.com/richard-harvey/2023/02/21/what-is-the-snot22-questionaire-and-why-do-rhinologists-use-it/
What is the SNOT22 questionaire and why do rhinologists use it
Quality of life measures in sino nasal disease
Chronic rhinosinusitis (CRS) is a chronic inflammatory disease that affects the nasal and sinus cavities. To measure the quality of life (QoL) in patients with CRS, researchers typically use disease-specific QoL instruments that are designed to capture the impact of the disease on the patient’s physical, emotional, and social well-being.
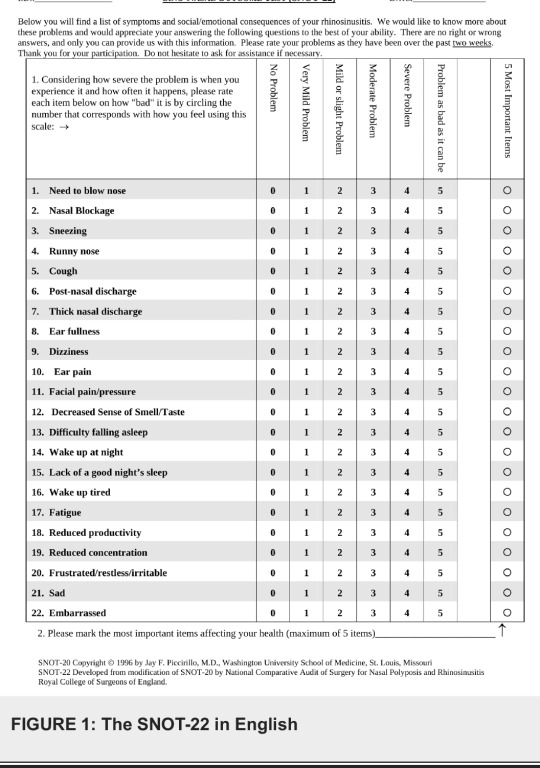
The most commonly used instrument for measuring QoL in patients with CRS is the Sino-Nasal Outcome Test (SNOT), which was developed by the Rhinology Research Society. The SNOT 22 questionaire is a validated instrument that asks patients to rate their symptoms, such as nasal obstruction, facial pain, and postnasal drip, on a scale from 0 (no problem) to 5 (problem as bad as it can be). The questionnaire also includes items that assess the impact of CRS on the patient’s daily activities and emotional well-being.
Other disease-specific QoL instruments that are used to measure the impact of CRS on QoL include the Rhinosinusitis Disability Index (RSDI), the Sinonasal Outcome Test-22 (SNOT-22), and the Chronic Sinusitis Survey (CSS). These instruments assess various aspects of QoL, including symptoms, functional limitations, emotional well-being, and social functioning.
In addition to disease-specific QoL instruments, researchers may also use generic QoL instruments to measure the impact of CRS on overall QoL. The most commonly used generic QoL instrument is the Short Form-36 (SF-36), which assesses overall QoL and includes domains such as physical functioning, social functioning, and emotional well-being.
Overall, the choice of QoL instrument used to measure the impact of CRS on QoL may depend on the specific research question, the patient population, and the clinical setting. However, the most commonly used instruments are disease-specific QoL instruments, such as the SNOT 22 questionnaire, which are designed to capture the unique impact of CRS on QoL. Currently, despite some limitations, the SNOT22 are the most widely accepted and researched quality of life tool in chronic rhinosinusitis. The questionaire has also been validated in other sino-nasal disorders. An example of the English version is featured below.
SNOT 22 questionaire translations are availiable for clinical practice and research
The Sino-Nasal Outcome Test (SNOT) is a widely used questionnaire for assessing the impact of chronic rhinosinusitis (CRS) on a patient’s quality of life. As the SNOT was developed in English, it has been translated into several other languages to facilitate its use in diverse populations.
To date, the SNOT 22 questionaire has been translated into more than 40 languages, including French, German, Spanish, Chinese, and Korean. These translations have been conducted using established translation and cross-cultural adaptation processes to ensure the validity and reliability of the translated instrument.
The German Translation of the SNOT22 by Prof Tobias Albrecht
Several of these translations have been validated in clinical studies, demonstrating their utility in assessing the impact of CRS on quality of life in different populations. The availability of these translated versions of the SNOT 22 questionaire has facilitated the use of this instrument in international clinical research, allowing for cross-cultural comparisons of CRS outcomes.
In summary, there are more than 40 translations of the Sino-Nasal Outcome Test, which have been validated and used to assess the impact of chronic rhinosinusitis on quality of life in diverse populations around the world.
Our links to the SNOT22 questionaire PDFs for download:
English
German
French
Korean
Chinese
1 note
·
View note
Photo

New Post has been published on https://sydneyentclinic.com/richard-harvey/2023/02/21/what-is-the-snot22-questionaire-and-why-do-rhinologists-use-it/
What is the SNOT22 questionaire and why do rhinologists use it
Quality of life measures in sino nasal disease
Chronic rhinosinusitis (CRS) is a chronic inflammatory disease that affects the nasal and sinus cavities. To measure the quality of life (QoL) in patients with CRS, researchers typically use disease-specific QoL instruments that are designed to capture the impact of the disease on the patient’s physical, emotional, and social well-being.
The most commonly used instrument for measuring QoL in patients with CRS is the Sino-Nasal Outcome Test (SNOT), which was developed by the Rhinology Research Society. The SNOT 22 questionaire is a validated instrument that asks patients to rate their symptoms, such as nasal obstruction, facial pain, and postnasal drip, on a scale from 0 (no problem) to 5 (problem as bad as it can be). The questionnaire also includes items that assess the impact of CRS on the patient’s daily activities and emotional well-being.
Other disease-specific QoL instruments that are used to measure the impact of CRS on QoL include the Rhinosinusitis Disability Index (RSDI), the Sinonasal Outcome Test-22 (SNOT-22), and the Chronic Sinusitis Survey (CSS). These instruments assess various aspects of QoL, including symptoms, functional limitations, emotional well-being, and social functioning.
In addition to disease-specific QoL instruments, researchers may also use generic QoL instruments to measure the impact of CRS on overall QoL. The most commonly used generic QoL instrument is the Short Form-36 (SF-36), which assesses overall QoL and includes domains such as physical functioning, social functioning, and emotional well-being.
Overall, the choice of QoL instrument used to measure the impact of CRS on QoL may depend on the specific research question, the patient population, and the clinical setting. However, the most commonly used instruments are disease-specific QoL instruments, such as the SNOT 22 questionnaire, which are designed to capture the unique impact of CRS on QoL. Currently, despite some limitations, the SNOT22 are the most widely accepted and researched quality of life tool in chronic rhinosinusitis. The questionaire has also been validated in other sino-nasal disorders. An example of the English version is featured below.
SNOT 22 questionaire translations are availiable for clinical practice and research
The Sino-Nasal Outcome Test (SNOT) is a widely used questionnaire for assessing the impact of chronic rhinosinusitis (CRS) on a patient’s quality of life. As the SNOT was developed in English, it has been translated into several other languages to facilitate its use in diverse populations.
To date, the SNOT 22 questionaire has been translated into more than 40 languages, including French, German, Spanish, Chinese, and Korean. These translations have been conducted using established translation and cross-cultural adaptation processes to ensure the validity and reliability of the translated instrument.
The German Translation of the SNOT22 by Prof Tobias Albrecht
Several of these translations have been validated in clinical studies, demonstrating their utility in assessing the impact of CRS on quality of life in different populations. The availability of these translated versions of the SNOT 22 questionaire has facilitated the use of this instrument in international clinical research, allowing for cross-cultural comparisons of CRS outcomes.
In summary, there are more than 40 translations of the Sino-Nasal Outcome Test, which have been validated and used to assess the impact of chronic rhinosinusitis on quality of life in diverse populations around the world.
Our links to the SNOT22 questionaire PDFs for download:
English
German
French
Korean
Chinese
0 notes
Photo

New Post has been published on https://sydneyentclinic.com/richard-harvey/2022/05/28/managing-nasal-obstruction-optimising-long-term-outcomes/
Managing nasal obstruction & optimising long-term outcomes
AIT as an essential surgeon’s tool –
Managing nasal obstruction & optimising long-term outcomes
Speaker: Professor Richard Harvey, Rhinologist UNSW and Macquarie University
Achieving long-term relief of nasal obstruction is a key goal for allergic rhinitis patients, particularly for those seeking surgical management. However, allergic rhinitis patients are at higher risk of disease relapse post-surgery due to the ongoing impact of their chronic allergic disease.
Prof. Harvey will explore why ‘disease modifying’ treatment with Allergen Immunotherapy (AIT) should be considered an essential surgeon’s ‘tool’. By targeting the underlying allergy, AIT has potential to provide lasting relief for allergic rhinitis patients. His presentation will cover the key drivers of allergy in Australia, practical aspects of allergy diagnosis and optimal approaches to AIT, informed by the latest evidence and evidence-based guidelines, including recent local studies of AIT in Australia.
Date: Tuesday 31 May 2022
Time: 6.30pm
Venue: Le Montage 38 Frazer Street Lilyfield NSW 2040 Tel: (02) 9555 6099
Parking: Available at the venue
RSVP:
To: Vanessa Dadley
t: 0421 744 587
0 notes
Photo

New Post has been published on https://sydneyentclinic.com/richard-harvey/2022/05/28/managing-nasal-obstruction-optimising-long-term-outcomes/
Managing nasal obstruction & optimising long-term outcomes
AIT as an essential surgeon’s tool –
Managing nasal obstruction & optimising long-term outcomes
Speaker: Professor Richard Harvey, Rhinologist UNSW and Macquarie University
Achieving long-term relief of nasal obstruction is a key goal for allergic rhinitis patients, particularly for those seeking surgical management. However, allergic rhinitis patients are at higher risk of disease relapse post-surgery due to the ongoing impact of their chronic allergic disease.
Prof. Harvey will explore why ‘disease modifying’ treatment with Allergen Immunotherapy (AIT) should be considered an essential surgeon’s ‘tool’. By targeting the underlying allergy, AIT has potential to provide lasting relief for allergic rhinitis patients. His presentation will cover the key drivers of allergy in Australia, practical aspects of allergy diagnosis and optimal approaches to AIT, informed by the latest evidence and evidence-based guidelines, including recent local studies of AIT in Australia.
Date: Tuesday 31 May 2022
Time: 6.30pm
Venue: Le Montage 38 Frazer Street Lilyfield NSW 2040 Tel: (02) 9555 6099
Parking: Available at the venue
RSVP:
To: Vanessa Dadley
t: 0421 744 587
0 notes
Photo
New Post has been published on https://sydneyentclinic.com/richard-harvey/2022/02/12/do-i-really-have-sinusitis-chronic-sinus-symptoms/
Do I really have sinusitis: matching imaging to "chronic sinus symptoms"?
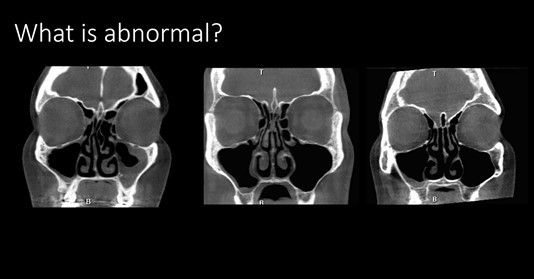
The non-medical concept of chronic sinus symptoms can really affect the true diagnosis. One of the most common clinical dilemmas is discussing incidental or insignificant radiologic findings with a patient that has a rhintis condition (allergy or otherwise) but has a radiology report that they have ‘sinusitis’. Chronic, episodic or recurrent sinonasal symptoms are often suspected as ‘sinus’ in origin. However, other conditions can produce these symptoms such as rhinitis and migraine.
However, there the concept of a perfect computed tomography ONLY equalling a normal state is false. Minor mucosal thickenings of the paranasal sinuses are part the ‘normal’ spectrum and incidental findings also include simple mucosal cysts (often incorrectly labelled as “nasal polyp’). A recent systematic review on the radiologic findings from a normal sinus cavity was publsihed this year. When patients have “chronic sinus symptoms” they are often describing chronic sino-nasal symptoms and the interpretation of the CT scan is essential to see if the symptoms really match the imaging.
This was the topic of recent ENT watch episode that you can watch here.
From this review of ‘normal’ or asymptomatic patients, a total of 950 articles were identified, of which 33 manuscripts met the inclusion criteria. The included studies involved 16,966 sinonasally asymptomatic subjects. The mean Lund-mackay (LM) score was 2.24 (95% CI, 1.61-2.87), and an LM score of ≥4 in 14.71% (95% CI, 6.86-24.82%) was present across all general asymptomatic population groups. Mucous retention cysts were noted in 13% (95% CI, 8.33-18.55%) and maxillary mucosal thickening of ≥2 mm in 17.73% (95% CI, 8.67-29.08%).
“Chronic sinus symptoms’ and a patient’s age
The other important factor is that the age of presentation is a significant distinguishing feature between persistent rhinitis and chronic rhinosinusitis. Symptom presentation among patients with persistent rhinitis (PR) and those with chronic rhinosinusitis (CRS) often overlaps. The sinonasal presentation of rhinorrhea, postnasal drip, nasal congestion, nasal itching, sneezing, facial pressure, facial pain, and headache are all common. Colloquially, many patients simply refer to any form of sinonasal symptoms as “sinus” or ”sinusitis,” but often patients simply have a rhinitis reaction. Otolaryngologists rely on both nasal endoscopy and computerized tomography (CT) to differentiate between PR and CRS. However in a recent study of n=651 patients presenting with chronic sino-nasal symptoms, younger age alone was an independant predictor of having a rhintiis condition rather than the diagnosis of chronic sinuitis.
When the data from this study is extracted the diagnostic characteristics for Age as a predictor of those patients presenting with sino-nasal symptoms and the final diagnosis of allergic rhinitis over sinus disease;
Age <25yro <30yro <35yro n= 25 52 82 Sensitivity (%) 17.8 40.0 56.7 Specificity (%) 96.0 93.0 86.3 PPV (%) 63.8 69.4 62.1 NPV (%) 74.7 79.6 83.4 LR+ 4.45 5.71 4.14 LR- 0.86 0.65 0.50 DOR 5.20 8.86 8.25
N: number of participants; PPV: positive predictive value; NPV: negative predictive value; LR+: positive likelihood ratio; LR-: negative likelihood ratio; DOR: diagnostic odds ratio.
Having a simple understanding of the age and the imaging of patient who presents with ‘chronic sinus symptoms’ is simple start to getting the diagnosis right.
1 note
·
View note
Photo

New Post has been published on https://sydneyentclinic.com/richard-harvey/2022/02/12/do-i-really-have-sinusitis-chronic-sinus-symptoms/
Do I really have sinusitis: matching imaging to "chronic sinus symptoms"?
The non-medical concept of chronic sinus symptoms can really affect the true diagnosis. One of the most common clinical dilemmas is discussing incidental or insignificant radiologic findings with a patient that has a rhintis condition (allergy or otherwise) but has a radiology report that they have ‘sinusitis’. Chronic, episodic or recurrent sinonasal symptoms are often suspected as ‘sinus’ in origin. However, other conditions can produce these symptoms such as rhinitis and migraine.
However, there the concept of a perfect computed tomography ONLY equalling a normal state is false. Minor mucosal thickenings of the paranasal sinuses are part the ‘normal’ spectrum and incidental findings also include simple mucosal cysts (often incorrectly labelled as “nasal polyp’). A recent systematic review on the radiologic findings from a normal sinus cavity was publsihed this year. When patients have “chronic sinus symptoms” they are often describing chronic sino-nasal symptoms and the interpretation of the CT scan is essential to see if the symptoms really match the imaging.
This was the topic of recent ENT watch episode that you can watch here.
From this review of ‘normal’ or asymptomatic patients, a total of 950 articles were identified, of which 33 manuscripts met the inclusion criteria. The included studies involved 16,966 sinonasally asymptomatic subjects. The mean Lund-mackay (LM) score was 2.24 (95% CI, 1.61-2.87), and an LM score of ≥4 in 14.71% (95% CI, 6.86-24.82%) was present across all general asymptomatic population groups. Mucous retention cysts were noted in 13% (95% CI, 8.33-18.55%) and maxillary mucosal thickening of ≥2 mm in 17.73% (95% CI, 8.67-29.08%).
“Chronic sinus symptoms’ and a patient’s age
The other important factor is that the age of presentation is a significant distinguishing feature between persistent rhinitis and chronic rhinosinusitis. Symptom presentation among patients with persistent rhinitis (PR) and those with chronic rhinosinusitis (CRS) often overlaps. The sinonasal presentation of rhinorrhea, postnasal drip, nasal congestion, nasal itching, sneezing, facial pressure, facial pain, and headache are all common. Colloquially, many patients simply refer to any form of sinonasal symptoms as “sinus” or ”sinusitis,” but often patients simply have a rhinitis reaction. Otolaryngologists rely on both nasal endoscopy and computerized tomography (CT) to differentiate between PR and CRS. However in a recent study of n=651 patients presenting with chronic sino-nasal symptoms, younger age alone was an independant predictor of having a rhintiis condition rather than the diagnosis of chronic sinuitis.
When the data from this study is extracted the diagnostic characteristics for Age as a predictor of those patients presenting with sino-nasal symptoms and the final diagnosis of allergic rhinitis over sinus disease;
Age <25yro <30yro <35yro n= 25 52 82 Sensitivity (%) 17.8 40.0 56.7 Specificity (%) 96.0 93.0 86.3 PPV (%) 63.8 69.4 62.1 NPV (%) 74.7 79.6 83.4 LR+ 4.45 5.71 4.14 LR- 0.86 0.65 0.50 DOR 5.20 8.86 8.25
N: number of participants; PPV: positive predictive value; NPV: negative predictive value; LR+: positive likelihood ratio; LR-: negative likelihood ratio; DOR: diagnostic odds ratio.
Having a simple understanding of the age and the imaging of patient who presents with ‘chronic sinus symptoms’ is simple start to getting the diagnosis right.
0 notes
Text
Patient selection, prognostic markers and outcomes in inflammatory airway disease
New Post has been published on https://sydneyentclinic.com/richard-harvey/2021/02/16/patient-selection-prognostic-markers-and-outcomes-in-inflammatory-airway-disease/
Patient selection, prognostic markers and outcomes in inflammatory airway disease
Patient selection, prognostic markers and outcomes in inflammatory airway disease
Created and Presented by: Rhinology And Skull Base Research Group, Continuing Medical Education Dinner Meeting
A live webinar and dinner educational event.
Agenda:
•
Prof Richard Harvey: Biologics – Responders and non-responders of the upper airway
•
A/Prof Janet Rimmer: Biologics – Responders and non-responders of the lower airway
•
Prof Constance Katelaris: Heterogeneity and similarities of action between biologics
Venue:
ZEST Waterfront – 21 Wunulla Road Point Piper 2027
(located at the Royal Motor Yacht club)
Date:
22.02.2021
Time:
Dinner meeting: 7:00pm – 9:30pm
Webinar session: 7:30pm – 9:30pm
PRIVACY STATEMENT:
Your personal information (“Information”) will be collected and used by AstraZeneca Pty Ltd (“AstraZeneca”) to register you for this event, for follow up purposes and for any other purpose described in AstraZeneca’s Privacy Policy. AstraZeneca may disclose your Information to our related entities or service providers (including IT support/service providers), some of which may be located overseas including in the US, European Union and Asia Pacific. If you do not provide your Information, AstraZeneca will not be able to register you for this event. Please refer to our Privacy Policy at http://www.astrazeneca.com.au/privacy-policy for more information about how your Information is handled and how you may seek to access or correct your Information, or submit a privacy complaint. AU-9861, February 2021.
For enquiries please contact:
Marie Urriste
For in-person meeting, register here:
For virtual meeting, register here:
#anosmia#can't smell#chronic sinusitis#eCRS#nasal polyps#nose#severe asthma and sinusitis#sinus#sinus surgery#sinus surgery cost
0 notes
Text
Patient selection, prognostic markers and outcomes in inflammatory airway disease
New Post has been published on https://sydneyentclinic.com/richard-harvey/2021/02/16/patient-selection-prognostic-markers-and-outcomes-in-inflammatory-airway-disease/
Patient selection, prognostic markers and outcomes in inflammatory airway disease
Patient selection, prognostic markers and outcomes in inflammatory airway disease
Created and Presented by: Rhinology And Skull Base Research Group, Continuing Medical Education Dinner Meeting
A live webinar and dinner educational event.
Agenda:
•
Prof Richard Harvey: Biologics – Responders and non-responders of the upper airway
•
A/Prof Janet Rimmer: Biologics – Responders and non-responders of the lower airway
•
Prof Constance Katelaris: Heterogeneity and similarities of action between biologics
Venue:
ZEST Waterfront – 21 Wunulla Road Point Piper 2027
(located at the Royal Motor Yacht club)
Date:
22.02.2021
Time:
Dinner meeting: 7:00pm – 9:30pm
Webinar session: 7:30pm – 9:30pm
PRIVACY STATEMENT:
Your personal information (“Information”) will be collected and used by AstraZeneca Pty Ltd (“AstraZeneca”) to register you for this event, for follow up purposes and for any other purpose described in AstraZeneca’s Privacy Policy. AstraZeneca may disclose your Information to our related entities or service providers (including IT support/service providers), some of which may be located overseas including in the US, European Union and Asia Pacific. If you do not provide your Information, AstraZeneca will not be able to register you for this event. Please refer to our Privacy Policy at http://www.astrazeneca.com.au/privacy-policy for more information about how your Information is handled and how you may seek to access or correct your Information, or submit a privacy complaint. AU-9861, February 2021.
For enquiries please contact:
Marie Urriste
For in-person meeting, register here:
For virtual meeting, register here:
#anosmia#can't smell#chronic sinusitis#eCRS#nasal polyps#nose#severe asthma and sinusitis#sinus#sinus surgery#sinus surgery cost
0 notes
Text
Sydney Sinus Surgery Course
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/08/05/sydney-sinus-surgery-course/
Sydney Sinus Surgery Course
************New date/Postponed due to covid. November 26-28th******* Any new enquiries please email Kate
The course focuses on the integrated medical and surgical management. Modern concepts of airway based approach will be discussed. Live surgery is planned on Friday morning. Lectures and discussions will prepare the participants for two afternoon sessions in the dissection laboratory.
Our invited speakers are:Dr Andrew Thamboo – is an Assistant Professor at the University of British Columbia (UBC) in Canada. He completed his medical degree and residency at University of British Columbia (UBC). During this time, he obtained another degree in Masters in Health Sciences concentrating on study design and epidemiology. He was awarded the Dr. I.B. Holubitsky Memorial Award for demonstrating the highest of surgical excellence at UBC. Dr. Thamboo then completed a two-year fellowship in Rhinology and Skull Base Fellowship at Stanford University. Dr. Thamboo medically and surgically manages chronic sinusitis and sinonasal tumors for a large part of Western Canada. He also has a basic science lab with an interest in the unified airway hypothesis and personalized medicine. Dr. Thamboo is recognized as a leader in the field in Canada, speaking at national and international meetings. He is also the chair of the Rhinology program for International Federation of Otolaryngology Society meeting happening in 2021.
Dr Jean Anderson Eloy is currently Professor and Vice Chair of Otolaryngology – Head and Neck Surgery at Rutgers New Jersey Medical School. He serves as the Director of Rhinology and Sinus Surgery, Director of Otolaryngology Research, and Co-Director of the Endoscopic Skull Base Surgery Program. Dr. Eloy also has joint appointments as Professor of Neurological Surgery and Professor of Ophthalmology and Visual Sciences at Rutgers New Jersey Medical School. He is currently the President of University Physician Associates of New Jersey, Inc., The Faculty Practice Plan of Rutgers New Jersey Medical School, the Vice President of the Doctor’s Center Management Corporation, the Vice President of the New Jersey Academy of Otolaryngology/New Jersey Academy of Facial Plastic Surgery, and the Chair and Chief of Service of the Department of Otolaryngology – Head and Neck Surgery at Saint Barnabas Medical Center. His clinical/surgical interests and area of expertise include medical and surgical management of refractory rhinosinusitis, endoscopic management of sinonasal neoplasia, cerebrospinal fluid rhinorrhea, ventral skull base lesions, endoscopic revision sinus surgery, and computer – aided sinus surgery. All members of the faculty have a wide experience in the management of sinus disease and endoscopic surgical techniques. They are joined by leading physicians involved in the management of upper airways disease, who all have academic appointments at major teaching facilities.
Dr Eri Mori, of Jekei University in Tokyo, demonstrating the finesse of olfactory cleft surgery in 2019
Local faculty: Prof Richard Harvey, A/Prof Raewyn Campbell, Prof Raymond Sacks, A/Prof Larry Kalish, A/Prof Janet Rimmer, Dr Geoff Wilcsek, A/Prof Nick Stow, A/Prof Yuresh Naidoo, Prof Pete Smith, Prof Stuart Mackay, Prof Connie Katelaris, Dr Justin Kong, Dr Harshita Pant, Dr Catherine Banks
0 notes
Text
Sydney Sinus Surgery Course
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/08/05/sydney-sinus-surgery-course/
Sydney Sinus Surgery Course
************New date/Postponed due to covid. November 28-30th******* Any new enquiries please email Kate The course focuses on the integrated medical and surgical management. Modern concepts of airway based approach will be discussed. Live surgery is planned on Friday morning. Lectures and discussions will prepare the participants for two afternoon sessions in the dissection laboratory. Our invited speakers are:Dr Andrew Thamboo – is an Assistant Professor at the University of British Columbia (UBC) in Canada. He completed his medical degree and residency at University of British Columbia (UBC). During this time, he obtained another degree in Masters in Health Sciences concentrating on study design and epidemiology. He was awarded the Dr. I.B. Holubitsky Memorial Award for demonstrating the highest of surgical excellence at UBC. Dr. Thamboo then completed a two-year fellowship in Rhinology and Skull Base Fellowship at Stanford University. Dr. Thamboo medically and surgically manages chronic sinusitis and sinonasal tumors for a large part of Western Canada. He also has a basic science lab with an interest in the unified airway hypothesis and personalized medicine. Dr. Thamboo is recognized as a leader in the field in Canada, speaking at national and international meetings. He is also the chair of the Rhinology program for International Federation of Otolaryngology Society meeting happening in 2021. Dr Jean Anderson Eloy is currently Professor and Vice Chair of Otolaryngology – Head and Neck Surgery at Rutgers New Jersey Medical School. He serves as the Director of Rhinology and Sinus Surgery, Director of Otolaryngology Research, and Co-Director of the Endoscopic Skull Base Surgery Program. Dr. Eloy also has joint appointments as Professor of Neurological Surgery and Professor of Ophthalmology and Visual Sciences at Rutgers New Jersey Medical School. He is currently the President of University Physician Associates of New Jersey, Inc., The Faculty Practice Plan of Rutgers New Jersey Medical School, the Vice President of the Doctor’s Center Management Corporation, the Vice President of the New Jersey Academy of Otolaryngology/New Jersey Academy of Facial Plastic Surgery, and the Chair and Chief of Service of the Department of Otolaryngology – Head and Neck Surgery at Saint Barnabas Medical Center. His clinical/surgical interests and area of expertise include medical and surgical management of refractory rhinosinusitis, endoscopic management of sinonasal neoplasia, cerebrospinal fluid rhinorrhea, ventral skull base lesions, endoscopic revision sinus surgery, and computer – aided sinus surgery. All members of the faculty have a wide experience in the management of sinus disease and endoscopic surgical techniques. They are joined by leading physicians involved in the management of upper airways disease, who all have academic appointments at major teaching facilities.
Dr Eri Mori, of Jekei University in Tokyo, demonstrating the finesse of olfactory cleft surgery in 2019
Local faculty: Prof Richard Harvey, A/Prof Raewyn Campbell, Prof Raymond Sacks, A/Prof Larry Kalish, A/Prof Janet Rimmer, Dr Geoff Wilcsek, A/Prof Nick Stow, A/Prof Yuresh Naidoo, Prof Pete Smith, Prof Stuart Mackay, Prof Connie Katelaris, Dr Justin Kong, Dr Harshita Pant, Dr Catherine Banks
1 note
·
View note
Text
Understanding Inflammatory sinusitis, nasal polyps and chronic sinusitis
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/07/11/understanding-inflammatory-sinusitis-nasal-polyps-and-chronic-sinusitis/
Understanding Inflammatory sinusitis, nasal polyps and chronic sinusitis
Most patients with ‘chronic’ sinus disease usually have disorders of sinus inflmmation or mechanical dysfunction (loss of mucus clearance). Chronic sinusitis is rarely an ‘infectious’ condition. Although bacteria take advantage of dysfunctional sinuses and create exacerbations, simplying taking antibiotics rarely solves this issues. In this lecture from our 2019 Sydney Sinus Surgery course, we review our current approach to ‘inflammatory’ sinus diseaes, the current phenotypes that we identify and how we approach the condition for patients.
youtube
Learn more by joining our youtube channel here.
Classic descriptions of chronic sinusits discuss simplistic origins of sinus ostia occulsion (thats the opening of the sinuses – there are 3 main openings on each side) and then secondary infection. While this type of sinus disease does occur, as below, it is very limited and usually unilateral, realtively uncommon and easily treated:
Examples of simple sinus disease that usually has very focal symptoms (ie not bilateral). Only 5-6 codes would typically describe the operation required to
Chronic sinusitis is more commonly bilateral diffuse and has inflammatory origins
Most patients with chronic symptoms will likely have diffuse changes and this is usually a marker of inflammatory disease. The lecture describes how we currently approach these patients:
These patients have extensive disease. The disease process here is diffuse and bilateral. This is not a simple ‘plumbing’ problem or anatomical obstruction. Complex sinus surgery is required here and up to 15 codes might describe such an intervention.
Subsequently, key research and clinical consensus groups have promoted that we better describe chronic sinusitis and have promoted a better understanding of the concept of ‘diffuse’ sinus disease that usually has inflammatory origins:
Primary CRS Classificiaton by EPOS2020
What are the features of differing types of inflammatory sinisitis?
Appreciating the underlying inflammatory subtype of sinus disease is critical to successful longterm control. Dr Jessica Grayson has published a terrific manuscript that summarises this process. The key table of clinical features are:
Journal of Otolaryngology – Head & Neck Surgery, 2019, doi:10.1186/s40463-019-0350-y
If you have chronic sinusitis, an abnormal CT scan of the sinuses, prior surgery or treatment that hasn’t worked then please contact us
0 notes
Text
Understanding Inflammatory sinusitis, nasal polyps and chronic sinusitis
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/07/11/understanding-inflammatory-sinusitis-nasal-polyps-and-chronic-sinusitis/
Understanding Inflammatory sinusitis, nasal polyps and chronic sinusitis
Most patients with ‘chronic’ sinus disease usually have disorders of sinus inflmmation or mechanical dysfunction (loss of mucus clearance). Chronic sinusitis is rarely an ‘infectious’ condition. Although bacteria take advantage of dysfunctional sinuses and create exacerbations, simplying taking antibiotics rarely solves this issues. In this lecture from our 2019 Sydney Sinus Surgery course, we review our current approach to ‘inflammatory’ sinus diseaes, the current phenotypes that we identify and how we approach the condition for patients.
youtube
Learn more by joining our youtube channel here.
Classic descriptions of chronic sinusits discuss simplistic origins of sinus ostia occulsion (thats the opening of the sinuses – there are 3 main openings on each side) and then secondary infection. While this type of sinus disease does occur, as below, it is very limited and usually unilateral, realtively uncommon and easily treated:
Examples of simple sinus disease that usually has very focal symptoms (ie not bilateral). Only 5-6 codes would typically describe the operation required to
Chronic sinusitis is more commonly bilateral diffuse and has inflammatory origins
Most patients with chronic symptoms will likely have diffuse changes and this is usually a marker of inflammatory disease. The lecture describes how we currently approach these patients:
These patients have extensive disease. The disease process here is diffuse and bilateral. This is not a simple ‘plumbing’ problem or anatomical obstruction. Complex sinus surgery is required here and up to 15 codes might describe such an intervention.
Subsequently, key research and clinical consensus groups have promoted that we better describe chronic sinusitis and have promoted a better understanding of the concept of ‘diffuse’ sinus disease that usually has inflammatory origins:
Primary CRS Classificiaton by EPOS2020
What are the features of differing types of inflammatory sinisitis?
Appreciating the underlying inflammatory subtype of sinus disease is critical to successful longterm control. Dr Jessica Grayson has published a terrific manuscript that summarises this process. The key table of clinical features are:
Journal of Otolaryngology – Head & Neck Surgery, 2019, doi:10.1186/s40463-019-0350-y
If you have chronic sinusitis, an abnormal CT scan of the sinuses, prior surgery or treatment that hasn’t worked then please contact us
0 notes
Text
Nose and sinuses 101: all the basics you need to know
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/06/30/nose-and-sinuses-101-all-the-basics-you-need-to-know/
Nose and sinuses 101: all the basics you need to know

Every year, we hold a 3 day educational course on Nose and sinus care with our combined Rhinoscopy and Sydney Sinus Surgery Courses.
Last year, in 2019, Medtronic kindly assisted in the recording of lectures as part of an ongoing effort to create a online archive of our teahcing activities.
I’m often asked about the basic anatomy and function of the nose and sinuses. It difficult to read a text book on rhinology without the clinical context and to understand what is really important.
For anyone wanting to join our courses, this a great pre-course lecture to familiarise yourself to the nose and sinus for beginners.
Nose and sinus basics 101 lecture:
youtube
Please don’t hesitate to send us questions or comments.
Learn more by joining our Youtube channel here
#chronic sinusitis#endoscopic#ESS#FESS#nasal polyps#nose#sinus#sinus infection#sinus surgery#sinusitis
0 notes
Text
Nose and sinuses 101: all the basics you need to know
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/06/30/nose-and-sinuses-101-all-the-basics-you-need-to-know/
Nose and sinuses 101: all the basics you need to know

Every year, we hold a 3 day educational course on Nose and sinus care with our combined Rhinoscopy and Sydney Sinus Surgery Courses.
Last year, in 2019, Medtronic kindly assisted in the recording of lectures as part of an ongoing effort to create a online archive of our teahcing activities.
I’m often asked about the basic anatomy and function of the nose and sinuses. It difficult to read a text book on rhinology without the clinical context and to understand what is really important.
For anyone wanting to join our courses, this a great pre-course lecture to familiarise yourself to the nose and sinus for beginners.
Nose and sinus basics 101 lecture:
youtube
Please don’t hesitate to send us questions or comments.
Learn more by joining our Youtube channel here
#chronic sinusitis#endoscopic#ESS#FESS#nasal polyps#nose#sinus#sinus infection#sinus surgery#sinusitis
0 notes
Text
Unexplained smell loss and CoVid: an increased risk of post-viral anosmia?
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/03/25/unexplained-smell-loss-and-covid-an-increased-risk-of-post-viral-anosmia/
Unexplained smell loss and CoVid: an increased risk of post-viral anosmia?
Smell loss or anosmia is a relatively common complication after viral upper respiratory infection but maybe be even more specific in Coronavirus-19.
Anosmia
Anosmia, also known as smell blindness, is the loss of the ability to detect one or more smells. Anosmia may be temporary or permanent. It differs from
There have been increasing reports of anosmia, or olfactory disturbance, in patients whom become infected with Coronavirus-19, regardless of the severity of other symptoms. As part of Covid symptoms reported, loss of smell appears to be more common than typical viral infections, ancedotally. As reported by the Australia Soceity of Otolaryngology, ansomia may be the only symptom reported by some patients with relatively asymptomatic infection.
Please see these interesting artilces about smell loss in CoVid infeciton:
New York times reported the link between smell loss and CoVid as unique feature of potential infection and repeated: Lost sense of smell may be peculiar clue to coronavirus infection (WRAL).
Washinton Post report the link between coronavirus-19 and disturbances in olfaction as part of the clinical presentation.
CNN has also published on ansomia and Covid:Doctors say loss of sense of smell might be Covid-19 symptom (CNN)
For many the perception of anosmia is the loss of ‘flavour of food’. While true taste is unlikley to be affected by coronavirus-19, the percetion of the flavour of food, is 80% contributed by retronasal smell. As we chew food, odourants from the food enter our smell cleft to contribute, with taste, to the perception of flavour.
Smell loss and CoVid infection impacts the senstation of taste/flavour: Retronasal passage of odourants contributes 80% to the perception of ‘flavour’ of food.
What to do if you’ve had suspected smell loss and CoVid.
if you have experienced recent disturbance of your olfactory system, please call us to discuss. There are interventions that can limit the injury to the olfactory system and also aid in recovery. By definition, you will likely be considered high risk of recent Coronavirus-19 infection. We offer telehealth services to discuss this with you:
Telehealth consultations are bulk billed, for eligible patients, but do not include an examination.
Call us to discuss 0293604811
Telehelth is conducted via Zoom
In the interim, pleaes remember there are other causes of anosmia, so CoVid infection is not the only issue. Practice hand hygiene and social distancing. If you have had smell loss then Coronavirus-19 screening maybe considered appropriate and strict social isolation, especially if meet the other high risk criteria:
Epidemiological criteria:
International travel in the 14 days before illness onset.
OR
Close contact in 14 days before illness onset with a confirmed case of COVID-19.
Clinical criteria:
Fever (≥38°C) or history of fever (e.g. night sweats, chills).
OR
Acute respiratory infection (e.g. shortness of breath, cough, sore throat) with or without fever.
In addition, if a patient has bilateral community-acquired pneumonia (critically ill) and no other cause is identified, with or without recent international travel, they are classified as a suspect case.
But do not hesitate to speak to a specialist if you have suspected smell loss and CoVid infection as simple interventions are availiable to help.
0 notes
Text
Unexplained smell loss and CoVid: an increased risk of post-viral anosmia?
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/03/25/unexplained-smell-loss-and-covid-an-increased-risk-of-post-viral-anosmia/
Unexplained smell loss and CoVid: an increased risk of post-viral anosmia?
Smell loss or anosmia is a relatively common complication after viral upper respiratory infection but maybe be even more specific in Coronavirus-19.
Anosmia
Anosmia, also known as smell blindness, is the loss of the ability to detect one or more smells. Anosmia may be temporary or permanent. It differs from
There have been increasing reports of anosmia, or olfactory disturbance, in patients whom become infected with Coronavirus-19, regardless of the severity of other symptoms. As part of Covid symptoms reported, loss of smell appears to be more common than typical viral infections, ancedotally. As reported by the Australia Soceity of Otolaryngology, ansomia may be the only symptom reported by some patients with relatively asymptomatic infection.
Please see these interesting artilces about smell loss in CoVid infeciton:
New York times reported the link between smell loss and CoVid as unique feature of potential infection and repeated: Lost sense of smell may be peculiar clue to coronavirus infection (WRAL).
Washinton Post report the link between coronavirus-19 and disturbances in olfaction as part of the clinical presentation.
CNN has also published on ansomia and Covid:Doctors say loss of sense of smell might be Covid-19 symptom (CNN)
For many the perception of anosmia is the loss of ‘flavour of food’. While true taste is unlikley to be affected by coronavirus-19, the percetion of the flavour of food, is 80% contributed by retronasal smell. As we chew food, odourants from the food enter our smell cleft to contribute, with taste, to the perception of flavour.
Smell loss and CoVid infection impacts the senstation of taste/flavour: Retronasal passage of odourants contributes 80% to the perception of ‘flavour’ of food.
What to do if you’ve had suspected smell loss and CoVid.
if you have experienced recent disturbance of your olfactory system, please call us to discuss. There are interventions that can limit the injury to the olfactory system and also aid in recovery. By definition, you will likely be considered high risk of recent Coronavirus-19 infection. We offer telehealth services to discuss this with you:
Telehealth consultations are bulk billed, for eligible patients, but do not include an examination.
Call us to discuss 0293604811
Telehelth is conducted via Zoom
In the interim, pleaes remember there are other causes of anosmia, so CoVid infection is not the only issue. Practice hand hygiene and social distancing. If you have had smell loss then Coronavirus-19 screening maybe considered appropriate and strict social isolation, especially if meet the other high risk criteria:
Epidemiological criteria:
International travel in the 14 days before illness onset.
OR
Close contact in 14 days before illness onset with a confirmed case of COVID-19.
Clinical criteria:
Fever (≥38°C) or history of fever (e.g. night sweats, chills).
OR
Acute respiratory infection (e.g. shortness of breath, cough, sore throat) with or without fever.
In addition, if a patient has bilateral community-acquired pneumonia (critically ill) and no other cause is identified, with or without recent international travel, they are classified as a suspect case.
But do not hesitate to speak to a specialist if you have suspected smell loss and CoVid infection as simple interventions are availiable to help.
0 notes
Text
Our clinic’s activities, services and procedures during the CoVid-19 pandemic
New Post has been published on https://sydneyentclinic.com/richard-harvey/2020/03/22/our-clinics-activities-services-and-procedures-during-the-covid-19-pandemic/
Our clinic’s activities, services and procedures during the CoVid-19 pandemic
Providing medical care in the CoVid-19 pandemic:
Unfortunately, there is still a need to provide care for patients with essential and important health issues throughout the period of time that will be occupied by the CoVid19 pandemic. Sydney Ear Nose & Throat Clinic remains open with additional precautions during the Covid-19 pandemic.
We are compliant with all directives and measures from the department of health:
We arre not seeing ‘at risk’ patients in the clinic
There are personal hygiene practices in place for patients and staff
Wait room has changed to be in line with these policies.
ENT surgeons are taking additional measure to protect themselves and patients.
Including aerosol/droplet protection such as P2 masks
The patient waiting room layout has been designed to minimise contact, promote social distancing and hand hygiene.
Telehealth services are availiable on request but:
Need to qualify under Medicare guidelines
New patients: must forward their referral so that it can be appropriately triaged to ensure they meet the criteria.
We may ask you to organise imaging/radiology prior to consult (at the clinic, or locally)
Telehealth consultations are bulk billed but do not include an examination.
Call us to discuss 0293604811
Telehelth is conducted via Zoom
The Australian Society of Otolaryngology/ Head & Neck Surgery (ASOHNS) have produced guidelines. to protect both healthcare professionals and patients.
All surgical patients, who are otherwise low risk of CoVid 19, having any surgery involving the airway (sinonasal, adenoids, tonsillectomy, oropharyngeal, laryngeal procedures) will be tested for COVID-19, where and when available, and be shown to be negative before proceeding:
We will provide this service on site.
72 hours prior to surgery
Post testing, patients should practice strict hand hygiene and social distancing prior to surgery.
We are thankful for all our patients efforts to contribute to the extra care and procedures during this period.
#anosmia#can't smell#covid#covid-19#ent#otolaryngology#sinus infection#sinus surgery#sinusitis#telehealth
0 notes