#HPV Cure Treatment
Text
Understanding Cervical Cancer Treatment in Hyderabad
Cervical cancer is a significant health issue for women in Hyderabad, India. However, with advancements in medical science, there are more treatment options available. Dr. Chinnababu, a renowned oncologist, is leading the way in providing effective treatments for cervical cancer patients in Hyderabad.
What is Cervical Cancer?
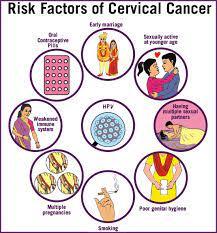
Cervical cancer starts in the cells of the cervix, the lower part of the uterus. It is usually caused by the human papillomavirus (HPV), but other factors like smoking and weakened immune systems can also contribute. Early detection is crucial for successful treatment.
Diagnosis
In Hyderabad, doctors use various tests to diagnose cervical cancer. These include Pap smears, HPV testing, colposcopy, and biopsy. These tests help doctors determine the stage and severity of the cancer, which guides treatment decisions.
Treatment Options
Treatment for cervical cancer depends on the stage of the disease and the patient's overall health. In Hyderabad, patients have access to several treatment options:
Surgery: Surgery may be recommended for early-stage cervical cancer. It can involve removing the cancerous tissue or the entire uterus. Dr. Chinnababu specializes in minimally invasive surgeries, which have shorter recovery times and fewer complications.
Radiation Therapy: Radiation therapy uses high-energy rays to kill cancer cells. It can be delivered externally or internally through brachytherapy. Hyderabad has advanced radiation therapy equipment to deliver precise treatment.
Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It can be given alone or in combination with other treatments. Dr. Chinnababu designs personalized chemotherapy plans for each patient.
Targeted Therapy: Targeted therapy targets specific molecules involved in cancer growth. It can be used for advanced or recurrent cervical cancer. Immunotherapy is a type of targeted therapy that boosts the body's immune system to fight cancer cells.
Conclusion
Cervical cancer treatment in Hyderabad offers hope for patients. Dr. Chinnababu and his team are dedicated to providing the best care possible. If you or someone you know is diagnosed with cervical cancer, don't hesitate to seek medical advice and explore treatment options available in Hyderabad. Early detection and personalized treatment plans can improve outcomes and quality of life for cervical cancer patients.
#cervical cancer#hpv vaccine#gardasil vaccine#pap smear#cervical cancer vaccine#cervical cancer causes#hpv vaccine price#hpv vaccine cost#pap smear price#papilloma vaccine#cure for cervical cancer#cervical#cervical vaccine#cervical cancer vaccine price#cervical cancer vaccine cost#pap exam#pap smear testing#papilloma virus vaccine#cervix#cervical cancer shot#pap screening#cervical vaccine cost#ca cervix treatment#ca cervix causes#ca cervix vaccine#p smear#pabst smear#papanicolaou smear#pap smear near me#hpv vaccine near me
0 notes
Text


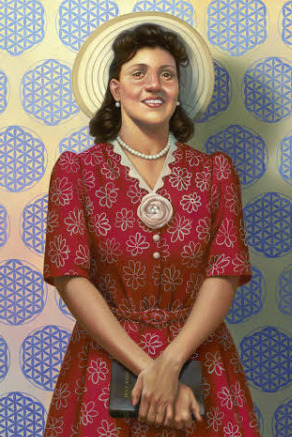

We at *BP family in the pass post a story of Mrs Henrietta Lacks story and how she and her family for generation were robbed by the scientific community for decades.
The most important information to take away is that a single BLACK WOMAN DNA has contributed to modern medical breakthroughs and cures, and is still ongoing.
There are a myriad of scientific developments due to Mrs Lacks -HELA CELLS as them called it. We are please to see that the family is getting restitution and reparations from yet again being robbed by them and covering up as them taken the credit and leaving the Black community/family in the dark and high and dry.
We will reblog the original post.
ONCE AGAIN A BLACK WOMEN IS THE MOTHER OF INVENTION
(The above is a *BP* commentary opinion)
BLACK PARAPHERNALIA DISCLAIMER - PLEASE READ
Family of Henrietta Lacks settles lawsuit with biotech giant, lawyer says

The family of Henrietta Lacks, a Black woman whose cancer cells were used without permission to form the basis of decades of scientific research, has reached a settlement with the biotech company Thermo Fisher Scientific.
The cells, known as HeLa cells, were taken from Lacks without her knowledge or consent in 1951 when she was seeking cervical cancer treatment at Johns Hopkins, in Baltimore. Doctors discovered that the cells doubled every 20 to 24 hours in the lab instead of dying. They were the first human cells that scientists successfully cloned, and they have been reproduced infinitely ever since.
Lacks herself died in 1951, but her cells continued to be used after her death in research that led to a series of medical advancements, including in the development of the polio vaccine and in treatments for cancer, HIV/AIDS, leukemia and Parkinson's disease. Lacks' family only found out about it decades later.
Lacks' story reached millions of Americans through the nonfiction bestseller "The Immortal Life of Henrietta Lacks," which was made into an HBO movie starring Oprah Winfrey as Lacks' daughter, Deborah.
In 2021, Lacks' estate filed a lawsuit against Thermo Fisher Scientific, alleging that the company was mass producing and selling tissue taken from Lacks even after it became well-known that the materials had been taken from her without her consent. The suit was filed exactly 70 years after Lacks' death.
"Thermo Fisher Scientific has known that HeLa cells were stolen from Ms. Lacks and chose to use her body for profit anyway," the lawsuit alleged. It has been previously reported that Thermo Fisher Scientific said they generate about $35 billion in annual revenue. In the lawsuit, Lacks' estate asked that the company "disgorge the full amount of its net profits obtained by commercializing the HeLa cell line to the Estate of Henrietta Lacks."
The suit also sought an order stopping the company from using the HeLa cells without the estate's permission. The terms of Tuesday's settlement were not made public, but Crump said in a news conference that both parties were "pleased" to have resolved the matter outside of court, CBS Baltimore reported. (except taken from KERRY BREEN CBS NEWS , 2023 )
INFORMATION OBTAIN FROM NATURE.COM FOR MORE READ CLICK HERE
SOME CONTRIBUTIONS OF THE HELA CELLS
-HeLa cells were first used to study the growth and spread of poliomyelitis virus, the cure of Polio
-HeLa cells have also been instrumental in the development of Human papilloma virus (HPV) vaccines.
-Over the years, HeLa cells have been infected with various types of viruses including HIV, Zika, herpes, and mumps
-HeLa cells have been used in a number of cancer studies, including those involving sex steroid hormones such as estradiol, estrogen, and estrogen proliferation.
-Hela cells contribute to scientists Joe Hin Tjio and Albert Levan to develop better techniques for staining and counting chromosomes.This was important for the study of developmental disorders such as down syndrome that involved the number of chromosomes.
-HeLa cells were sent on the first satellite and human space missions to determine the long term effects of space travel on living cells and tissue.
-HeLa cell line was derived for use in cancer research. and human papillomavirus 18 (HPV18) to human cervical cells created the HeLa genome, which is different from Henrietta Lacks’ genome in various ways,
-The complete genome of the HeLa cells was sequenced and published on 11 March 2013[46][47] without the Lacks family’s knowledge
-HeLa cells as a tool to uncover the machinery required and process used for invasion of human cells. Researchers have also investigated the stability of the virus’s genomic material in HeLa cells by comparing its genomic material with that of many other viruses. The use of HeLa cells in COVID-19 research has provided insights on the molecular mechanics of SARS-CoV-2019 and the components required for infection.
INFORMATION OBTAINED HERE
A LASTING CONTRIBUTION TO THE WORLD
When Henrietta Lacks and her cells alerted the world to the existence of immortal human cells, opportunities arose for research and medical treatment development.
Today, her cells continue to serve academic and industrial institutions. So much so that she has been described as the Mother of Modern Medicine in a painting by artist Kadir Nelson in 2017.
The use of HeLa cells in COVID-19 research is a testament to Henrietta Lacks’s lasting contribution to provide microscopic tools for scientific discoveries that billions have benefitted from thus far and will benefit from in the future to come.
INFORMATION OBTAIN FROM NATURE.COM FOR MORE READ CLICK HERE
SOME CONTRIBUTIONS OF THE HELA CELLS
-HeLa cells were first used to study the growth and spread of poliomyelitis virus, the cure of Polio
-HeLa cells have also been instrumental in the development of Human papilloma virus (HPV) vaccines.
-Over the years, HeLa cells have been infected with various types of viruses including HIV, Zika, herpes, and mumps
-HeLa cells have been used in a number of cancer studies, including those involving sex steroid hormones such as estradiol, estrogen, and estrogen proliferation.
-Hela cells contribute to scientists Joe Hin Tjio and Albert Levan to develop better techniques for staining and counting chromosomes.This was important for the study of developmental disorders such as down syndrome that involved the number of chromosomes.
-HeLa cells were sent on the first satellite and human space missions to determine the long term effects of space travel on living cells and tissue.
-HeLa cell line was derived for use in cancer research. and human papillomavirus 18 (HPV18) to human cervical cells created the HeLa genome, which is different from Henrietta Lacks’ genome in various ways,
-The complete genome of the HeLa cells was sequenced and published on 11 March 2013 without the Lacks family’s knowledge
-HeLa cells as a tool to uncover the machinery required and process used for invasion of human cells. Researchers have also investigated the stability of the virus’s gnomic material in HeLa cells by comparing its genomic material with that of many other viruses.
The use of HeLa cells in COVID-19 research has provided insights on the molecular mechanics of SARS-CoV-2019 and the components required for infection.
INFORMATION OBTAINED HERE
A LASTING CONTRIBUTION TO THE WORLD
When Henrietta Lacks and her cells alerted the world to the existence of immortal human cells, opportunities arose for research and medical treatment development.
Today, her cells continue to serve academic and industrial institutions. So much so that she has been described as the Mother of Modern Medicine in a painting by artist Kadir Nelson in 2017.
The use of HeLa cells in COVID-19 research is a testament to Henrietta Lacks’s lasting contribution to provide microscopic tools for scientific discoveries that billions have benefitted from thus far and will benefit from in the future to come.
13 notes
·
View notes
Text
“Revolutionize Your Health: The Ultimate Guide to Unlocking Comprehensive 360 degree Solutions and Cure Treatment Plans for “Cervical cancer” – Your Path to Lasting Wellness!” in 2023-2024
2 notes
·
View notes
Text
Cervical cancer Treatment in Jaipur - Dr. Chandrakanta Sulaniya
Cervical cancer remains a significant health concern for women worldwide, including in Jaipur. However, hope shines bright at Dr. Chandrakanta’s Gynae-Oncology Center, where expert care meets compassionate support. Let’s delve into the causes, prevention strategies, and treatment solutions for cervical cancer, and discover how Dr. Chandrakanta’s center stands at the forefront of combating this disease in Jaipur.
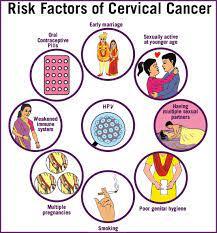
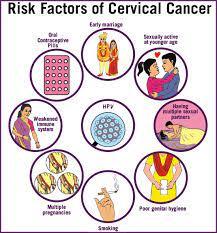
Causes of Cervical Cancer :
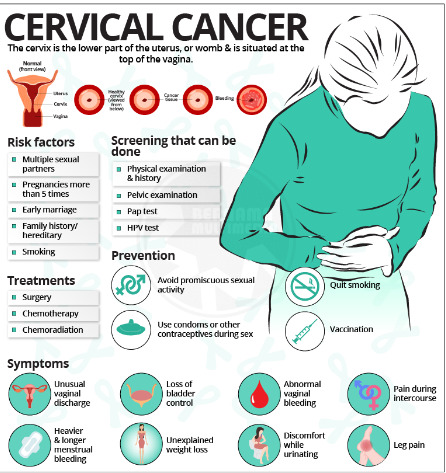
Cervical cancer typically develops due to persistent infection with high-risk strains of the human papillomavirus (HPV). Other factors such as smoking, weakened immune system, early onset of sexual activity, multiple sexual partners, and poor socio-economic status can also increase the risk. Cervical cancer Treatment in Jaipur.
Prevention Strategies :
Prevention is better than cure, and cervical cancer is largely preventable through vaccination and regular screening. HPV vaccination, typically administered during adolescence, protects against the most common cancer-causing strains of HPV. Additionally, routine cervical cancer screening, such as Pap smears and HPV tests, can detect precancerous changes early when treatment is most effective.
Treatment Solutions at Dr. Chandrakanta’s Gynae-Oncology :
1. Surgery : Surgical options may include cone biopsy, hysterectomy, or lymph node removal, depending on the stage and extent of cancer.
2.Chemotherapy : Powerful medications are used to destroy cancer cells or shrink tumors, either alone or in combination with other treatments.
3.Radiation Therapy : High-energy beams target and destroy cancer cells, often used in conjunction with surgery or chemotherapy.
4.Targeted Therapy : Drugs target specific molecules involved in cancer growth, offering a more precise and effective treatment approach.
5.Immunotherapy : Boosting the body’s immune system to recognize and attack cancer cells, revolutionizing cancer treatment.
Dr. Chandrakanta’s Approach :
At Dr. Chandrakanta’s Gynae-Oncology Center, a comprehensive approach to cervical cancer treatment is adopted, integrating the latest advancements in medical science with personalized care. Patients receive tailored treatment plans that consider their unique circumstances, ensuring the best possible outcomes.
Cervical cancer may pose challenges, but with the right approach, it is a battle that can be won. Through prevention, early detection, and advanced treatment options available at Dr. Chandrakanta’s Gynae-Oncology Center in Jaipur, women can confront cervical cancer with confidence and resilience. Don’t let cervical cancer hold you back — take charge of your health, and together, let’s defeat this disease with Dr .Chandrakanta Gynae Oncology in jaipur
#choriocarcinomatreatment in jaipur#dr chandrakanta gynae oncology in jaipur#cervical cancer treatment in jaipur#gynae oncologist in jaipur#endometrial cancer treatment in jaipur#gynae cancer doctor in jaipur#gynaecological cancer in jaipur#gynaecological surgeries in jaipur#gynaecological oncologist near me
0 notes
Text
Cervical Health Awareness: Preventing and Detecting Cervical Cancer

Cervical cancer is one of the most common types of cancer affecting women worldwide. According to the World Health Organization, it is estimated that every year, more than 500,000 women are diagnosed with cervical cancer and more than 300,000 die from the disease. However, with early detection and proper treatment, cervical cancer can be prevented and even cured. That is why it is crucial to raise awareness about cervical health and the importance of regular check-ups with the best gynaecologist in Indore.
What is Cervical Cancer?
Cervical cancer is a type of cancer that affects the cells of the cervix, the lower part of the uterus that connects to the vagina. It is mainly caused by the human papillomavirus (HPV), a common sexually transmitted infection. However, not all women who have HPV will develop cervical cancer, as it can take years for the virus to cause changes in the cells of the cervix.
Preventing Cervical Cancer
The most effective way to prevent cervical cancer is through regular screening tests and vaccination against HPV. The HPV vaccine is recommended for girls and boys between the ages of 9 and 14, as it provides the best protection when given before the onset of sexual activity. However, even if you have been vaccinated, it is still essential to get regular Pap tests to screen for any abnormal changes in the cells of the cervix.
Also Read: Test Tube Baby Centre in Indore
Pap tests, also known as Pap smears, are a simple and painless procedure that involves collecting cells from the cervix to be examined under a microscope. It is recommended for women to start getting Pap tests at the age of 21 and continue every three years until the age of 65. Women who are at a higher risk of developing cervical cancer, such as those with a weakened immune system or a history of abnormal Pap tests, may need to get tested more frequently.
Detecting Cervical Cancer
Early detection is crucial in the treatment of cervical cancer. In its early stages, cervical cancer may not cause any symptoms, which is why regular Pap tests are essential. However, as the cancer progresses, symptoms such as abnormal vaginal bleeding, pelvic pain, and pain during sexual intercourse may occur.
Also Read: IVF Centre in Indore
0 notes
Text
What you need to know about the HPV Vaccine
Globally, cervical cancer is the fourth most common cancer in women, with 6,04,000 new cases in 2020. Women living with HIV are 6 times more likely to develop cervical cancer, compared to the general population, and an estimated 5% of all cervical cancer cases are attributable to HIV. The contribution of HIV to cervical cancer disproportionately affects younger women, and as a result, 20% of children who lose their mother to cancer do so due to cervical cancer. If you have concerns about your cervical cancer, it’s best to consult with Dr. Kunaal Shine is offers Cervical Cancer Treatment in Pune and can assess your risk factors.
Understanding HPV:
HPV is a group of more than 200 related viruses, of which some can lead to cervical cancer. HPV is extremely common, with most sexually active individuals contracting it at some point in their lives. While most HPV infections clear up on their own without causing any harm, persistent infection with certain high-risk types can lead to cervical cancer and other cancers of the genital and oropharyngeal areas.
Benefits of the HPV Vaccine:
Immunizations are safe and effective and have successfully reduced the transmission of many deadly diseases. The CDC (Centers for Disease Control and Prevention) states the HPV vaccine protects against infections that can lead to HPV-related cancers and abnormal cells that can lead to cancer (precancers), as well as genital warts.
Symptoms of Cervical Cancer:
Dr. Kunaal Shinde states that early-stage cervical cancer is mostly asymptomatic. some of the early signs and symptoms include :
Abnormal vaginal bleeding during intercourse
Bleeding in between periods
Postmenstrual bleeding
Abnormal vaginal discharge which may or may not be foul smelling
What cancer does HPV cause?
HPV causes 1 in 20 cancers worldwide.
Almost all cervical cancers (99%) are caused by high-risk types of HPV infection.
The HPV virus also causes
5 out of 10 vulval cancers
7 out of 10 vaginal cancers
9 out of 10 HPV-related anal cancers
9 out of 10 incidences of genital warts
HPV also causes cancers of the mouth, anus, and penis.
Risk factors for Cervical Cancer:
Multiple sexual partners
Early sexual activity HPV infection
Other infection
Weakened immune system: increases chances of persistent HPV and thus chance of developing cervical cancer
Smoking
Prevention of Cervical Cancer:
Being vaccinated at age 9–14 years is a very effective way to prevent HPV infection, cervical cancer, and other HPV-related cancers.
Screening from the age of 30 (25 years in women living with HIV) can detect cervical disease, which when treated, also prevents cervical cancer.
At any age with symptoms or concerns, early detection followed by prompt quality treatment can cure cervical cancer.
How many doses to be given?
If vaccination is started before 15 years of age only 2 doses are recommended (0, 6-12 months). If vaccination is started after 15 years of age 3 doses (0, 1-2, 6 months) are recommended.
Side effects of the vaccine:
Mild problems include pain, redness, swelling, and itching at the injection site. Fainting has been reported among adolescents who receive the HPV vaccine (and other recommended vaccines as well). Dr. Kunaal Shinde recommended that the vaccine should be given in a sitting position and remain seated for 15–20 minutes after receiving the vaccine.
Early detection, diagnosis, and treatment of cervical cancer:
Cervical cancer can be cured if diagnosed and treated at an early stage of disease. Recognizing symptoms and seeking medical advice to address any concerns is a critical step. Women should see a Gyneac Cancer Specialist in Pune if they notice:
unusual bleeding between periods, after menopause, or after sexual intercourse
increased or foul-smelling vaginal discharge
symptoms like persistent pain in the back, legs, or pelvis
weight loss, fatigue, and loss of appetite
vaginal discomfort
swelling in the legs
What can you do to protect yourself from cervical cancer if you're not in the recommended vaccine age group?
As HPV spreads through sexual contact to protect yourself from HPV, use a condom every time you have sex. In addition, avoid smoking. Smoking raises the risk of cervical cancer. Additionally, screening can detect cervical cancer in the precancerous stage. so undergo regular screening after the age of 21 years.
The HPV vaccine is CANCER PREVENTION.
As a Gyneac Cancer Specialist in Pune, Dr. Shinde specializes in the diagnosis and treatment of gynecologic cancers, including cervical cancer. The more young people who get the HPV vaccine and women who get routinely screened for cervical cancers, the better we can control the spread of HPV infection. Protect your future – get the HPV vaccine.” Please contact Dr. Kunaal Shinde with any queries you may have regarding HPV vaccine or cervical cancer. HPV vaccination is our best defense in preventing HPV-related cancers.
#Gynecologist in Baner#Best Gynecologist in Baner#Laparoscopic Surgeon in Pune#Laparoscopic specialist in Pune#Gynaec Laparoscopic Surgeon in Pune#Best Gynaec Laparoscopic Surgeon in Pune#Laparoscopic surgeon & Robotic surgeon in Pune
0 notes
Text
Stg I am so happy the US media has not gotten a hold of STI treatment information
Like, I mean that while the results are promising, you just know that the US media is going to spin it into a horrible story like
'Anti-STI' miracle drug halted by lying women
When in reality, the drug focusing on preventing bacterial STI's by taking them the day after, Doxy-pep, has gotten great strides in clinical trials and is expected to be available to the US and worldwide soon. The problem being that within the trials, a number of women who were tested were found to have been lying about even taking the drug, for reasons still being looked into. This has given a statistical impact on the effectiveness of Doxy-pep based on gender, and currently it is recorded that Doxy-pep works best for "men who have sex with men or transgender women"
To reiterrate: The Drug Is Still Being Distributed. Everything is fine
This post is really just about how horrible the media is, and how much the average person *doesn't* look into things themselves for further information, blindly going by headlines and big bold text (if you are one of the few people who do look into things, thank you ever so much, I wish you all the sex you ever want in your lifetime)
Now, as one who personally loves rampant gay sex, I occasionally check up on the latest STI preventions, treatments and vaccinations. If you don't know what the STI scene currently looks like, the news is:
Syphalis - CURABLE
Gonorrhea - CURABLE
Chlamydia - CURABLE
Trichoniasis - CURABLE
Of course these are the four biggest bacterial STI's and can be treated with the right antibiotics. The real big scares are the viral STI's, like
Hepatitis B - NO CURE
HSV - NO CURE
HPV - NO CURE
HIV - NO CURE
These four are the big ones, the reasons why I can't get too drunk at my local bar. The biggest of those is obviously HIV, the others likely to get a boost in research once a HIV vaccine materializes
There is no HIV vaccine *yet* however there are over 20 ongoing trials, with a few seeing successful results. While things are currently in Phase 1 for the most part, it's possiple for Phase 2 to start soon, moving on through more rigourous testing and eventually making a HIV vaccine possible. Results will unfortunately take some time
0 notes
Text
Early detection of cancer is crucial for several reasons:
Increased Treatment Options: When cancer is detected early, there are often more treatment options available. Early-stage cancers may be more responsive to treatment and may require less aggressive therapies, resulting in better outcomes and fewer side effects.
Improved Survival Rates: Early detection generally leads to better survival rates. Cancers that are diagnosed at an early stage are more likely to be treated successfully, leading to higher chances of long-term survival and even cure.
Reduced Morbidity and Mortality: Early detection can help prevent cancer from spreading to other parts of the body, reducing the risk of complications and improving overall quality of life.
Lower Treatment Costs: Treating cancer in its early stages is often less costly than treating advanced-stage cancers. Early detection can help reduce the financial burden on individuals, families, and healthcare systems.
Easier Treatment: Early-stage cancers may require less aggressive treatments, such as surgery or localized therapies, which may be less physically and emotionally taxing on patients.
Overall, early detection plays a pivotal role in improving cancer outcomes, reducing mortality rates, and enhancing the effectiveness and tolerability of treatments. This underscores the importance of regular cancer screening and awareness of early signs and symptoms.
Several screening methods are available for various types of cancer. Here are some common ones:
Breast Cancer:
Mammography: X-ray imaging of the breast tissue to detect abnormalities.
Clinical Breast Exam: Physical examination of the breasts by a healthcare provider.
Cervical Cancer:
Pap Smear: Collection of cells from the cervix to detect abnormal changes.
HPV Testing: Screening for high-risk strains of human papillomavirus, which can cause cervical cancer.
Colorectal Cancer:
Colonoscopy: Visual examination of the colon and rectum using a flexible, lighted tube.
Fecal Occult Blood Test (FOBT): Tests for the presence of blood in stool samples.
Stool DNA Test: Detects DNA changes in stool samples that may indicate colorectal cancer.
Prostate Cancer:
Prostate-Specific Antigen (PSA) Test: Blood test measuring levels of PSA, a protein produced by the prostate gland.
Digital Rectal Exam (DRE): Physical examination of the prostate gland through the rectum.
Lung Cancer:
Low-Dose Computed Tomography (LDCT): X-ray imaging of the lungs to detect abnormalities in high-risk individuals, such as heavy smokers.
Skin Cancer:
Visual Inspection: Regular self-examination of the skin to detect changes in moles or other skin abnormalities.
Dermatologist Examination: Professional examination of the skin by a dermatologist.
Ovarian Cancer:
Transvaginal Ultrasound: Imaging test using sound waves to examine the ovaries for abnormalities.
CA-125 Blood Test: Measures levels of CA-125, a protein that may be elevated in ovarian cancer.
Choice of screening method may depend on factors such as age, sex, family history, and individual risk factors. Screening guidelines may also vary among different organizations and regions. Get the best treatment for cancer and a full body health checkup done at the best hospitals in India.
1 note
·
View note
Text
AHS Advocates for Regular Cervical Cancer Screening as a Vital Preventative Measure
Cervical cancer is a significant global health concern, but advancements in medical science have underscored the importance of early detection and prevention. Alberta Health Services (AHS) has emphasized the critical role of regular cervical cancer screening as a key tool in preventing the onset and progression of this potentially life-threatening disease. Through targeted awareness campaigns and educational initiatives, AHS aims to empower individuals to prioritize their health by incorporating routine screenings into their healthcare regimen.
The Importance of Cervical Cancer Screening:
Cervical cancer, primarily caused by certain strains of the human papillomavirus (HPV), is a preventable and treatable condition when detected early. Regular screenings, such as Pap smears and HPV tests, enable healthcare providers to identify abnormal changes in cervical cells before they develop into cancer. This proactive approach allows for timely intervention and significantly increases the likelihood of successful treatment and cure.
AHS Recommendations:
Alberta Health Services strongly recommends that individuals, particularly women, prioritize cervical cancer screenings as a routine aspect of their healthcare. The recommended frequency of screenings may vary based on individual risk factors, age, and previous screening results. AHS encourages women to engage in open and informed discussions with their healthcare providers to determine the most appropriate screening schedule tailored to their unique circumstances.
Access to Screening Services:
To further promote accessibility, AHS works towards ensuring that cervical cancer screening services are readily available across healthcare facilities in Alberta. Efforts are made to reduce barriers to screening, whether they be geographical, financial, or educational, to ensure that individuals from all walks of life can benefit from this preventative measure.
Public Awareness Campaigns:
AHS undertakes robust public awareness campaigns to educate the community about the importance of cervical cancer screening. These campaigns provide information on the benefits of early detection, debunk myths surrounding the screening process, and empower individuals to take control of their health through proactive measures.
Empowering Communities:
In addition to individual responsibility, AHS recognizes the role of communities in promoting preventative healthcare. Partnering with local organizations, educational institutions, and healthcare providers, AHS aims to create a supportive environment that encourages regular cervical cancer screenings. By fostering a culture of health-consciousness, AHS believes that the collective impact can significantly contribute to reducing the incidence and impact of cervical cancer in the region.
For More Information Visit US :
https://express004news.blogspot.com/2024/01/revolutionizing-legal-practices-sikaria.h
0 notes
Text
MIT researchers develop advanced machine learning models to detect pancreatic cancer

MIT researchers develop advanced machine learning models to detect pancreatic cancer.
MIT CSAIL researchers develop advanced machine-learning models that outperform current methods in detecting pancreatic ductal adenocarcinoma.
Prismatic perspectives pancreatic cancer
The path forward
The first documented case of pancreatic cancer dates from the 18th century. Since then, researchers have embarked on a long and difficult journey to better understand this elusive and deadly disease. To date, early intervention is the most effective cancer treatment. Unfortunately, due to its location deep within the abdomen, the pancreas is particularly difficult to detect early on.
Scientists from the MIT Computer Science and Artificial Intelligence Laboratory (CSAIL), as well as Limor Appelbaum, a staff scientist in the Department of Radiation Oncology at Beth Israel Deaconess Medical Center (BIDMC), wanted to better identify potential high-risk patients. They set out to create two machine-learning models for the early detection of pancreatic ductal adenocarcinoma (PDAC), the most common type of cancer.
To gain access to a large and diverse database, the team collaborated with a federated network company and used electronic health record data from multiple institutions across the United States. This vast data set contributed to the models' reliability and generalizability, making them applicable to a wide range of populations, geographical locations, and demographic groups.
The two models—the “PRISM” neural network and the logistic regression model (a statistical technique for probability)—outperformed current methods. The team’s comparison showed that while standard screening criteria identify about 10 percent of PDAC cases using a five-times higher relative risk threshold, Prism can detect 35 percent of PDAC cases at this same threshold.
Using AI to detect cancer risk is not a new phenomenon; algorithms analyze mammograms, CT scans for lung cancer, and assist in the analysis of Pap smear tests and HPV testing, to name a few applications.
“The PRISM models stand out for their development and validation on an extensive database of over 5 million patients, surpassing the scale of most prior research in the field,” says Kai Jia, an MIT PhD student in electrical engineering and computer science (EECS), MIT CSAIL affiliate, and first author on an open-access paper in eBioMedicine outlining the new work. “The model uses routine clinical and lab data to make its predictions, and the diversity of the U.S. population is a significant advancement over other PDAC models, which are usually confined to specific geographic regions, like a few health-care centers in the U.S. Additionally, using a unique regularization technique in the training process enhanced the models' generalizability and interpretability.”
“This report outlines a powerful approach to use big data and artificial intelligence algorithms to refine our approach to identifying risk profiles for cancer,” says David Avigan, a Harvard Medical School professor and the cancer center director and chief of hematology and hematologic malignancies at BIDMC, who was not involved in the study. “This approach may lead to novel strategies to identify patients with high risk for malignancy that may benefit from focused screening with the potential for early intervention.”
Prismatic perspectives pancreatic cancer
The journey toward the development of PRISM began over six years ago, fueled by firsthand experiences with the limitations of current diagnostic practices.
“Approximately 80-85 percent of pancreatic cancer patients are diagnosed at advanced stages, where cure is no longer an option,” says senior author Appelbaum, who is also a Harvard Medical School instructor as well as radiation oncologist. “This clinical frustration sparked the idea to delve into the wealth of data available in electronic health records (EHRs).”
The CSAIL group’s close collaboration with Appelbaum made it possible to understand the combined medical and machine learning aspects of the problem better, eventually leading to a much more accurate and transparent model. “The hypothesis was that these records contained hidden clues — subtle signs and symptoms that could act as early warning signals of pancreatic cancer,” she adds. “This guided our use of federated EHR networks in developing these models, for a scalable approach for deploying risk prediction tools in health care.”
Both PrismNN and PrismLR models analyze EHR data, including patient demographics, diagnoses, medications, and lab results, to assess PDAC risk. PrismNN uses artificial neural networks to detect intricate patterns in data features like age, medical history, and lab results, yielding a risk score for PDAC likelihood. PrismLR uses logistic regression for a simpler analysis, generating a probability score of PDAC based on these features. Together, the models offer a thorough evaluation of different approaches in predicting PDAC risk from the same EHR data.
One paramount point for gaining the trust of physicians, the team notes, is better understanding how the models work, known in the field as interpretability. The scientists pointed out that while logistic regression models are inherently easier to interpret, recent advancements have made deep neural networks somewhat more transparent. This helped the team to refine the thousands of potentially predictive features derived from EHR of a single patient to approximately 85 critical indicators. These indicators, which include patient age, diabetes diagnosis, and an increased frequency of visits to physicians, are automatically discovered by the model but match physicians' understanding of risk factors associated with pancreatic cancer.
The path forward
Despite the promise of the PRISM models, as with all research, some parts are still a work in progress. U.S. data alone are the current diet for the models, necessitating testing and adaptation for global use. The path forward, the team notes, includes expanding the model's applicability to international datasets and integrating additional biomarkers for more refined risk assessment.
“A subsequent aim for us is to facilitate the models' implementation in routine health care settings. The vision is to have these models function seamlessly in the background of health care systems, automatically analyzing patient data and alerting physicians to high-risk cases without adding to their workload,” says Jia. “A machine-learning model integrated with the EHR system could empower physicians with early alerts for high-risk patients, potentially enabling interventions well before symptoms manifest. We are eager to deploy our techniques in the real world to help all individuals enjoy longer, healthier lives.”
Jia wrote the paper alongside Applebaum and MIT EECS Professor and CSAIL Principal Investigator Martin Rinard, who are both senior authors of the paper. Researchers on the paper were supported during their time at MIT CSAIL, in part, by the Defense Advanced Research Projects Agency, Boeing, the National Science Foundation, and Aarno Labs. TriNetX provided resources for the project, and the Prevent Cancer Foundation also supported the team.
Source: MIT
Read the full article
0 notes
Text
New Hope for Early Pancreatic Cancer Intervention via AI-based Risk Prediction - Technology Org
New Post has been published on https://thedigitalinsider.com/new-hope-for-early-pancreatic-cancer-intervention-via-ai-based-risk-prediction-technology-org/
New Hope for Early Pancreatic Cancer Intervention via AI-based Risk Prediction - Technology Org
The first documented case of pancreatic cancer dates back to the 18th century. Since then, researchers have undertaken a protracted and challenging odyssey to understand the elusive and deadly disease. To date, there is no better cancer treatment than early intervention. Unfortunately, the pancreas, nestled deep within the abdomen, is particularly elusive for early detection.
Image credit: MIT CSAIL
MIT Computer Science and Artificial Intelligence Laboratory (CSAIL) scientists, alongside Limor Appelbaum, a staff scientist in the Department of Radiation Oncology at Beth Israel Deaconess Medical Center (BIDMC), were eager to better identify potential high-risk patients. They set out to develop two machine-learning models for early detection of pancreatic ductal adenocarcinoma (PDAC), the most common form of the cancer.
To access a broad and diverse database, the team synced up with a federated network company, using electronic health record data from various institutions across the United States. This vast pool of data helped ensure the models’ reliability and generalizability, making them applicable across a wide range of populations, geographical locations, and demographic groups.
The two models — the “PRISM” neural network, and the logistic regression model (a statistical technique for probability), outperformed current methods. The team’s comparison showed that while standard screening criteria identify about 10 percent of PDAC cases using a five-times higher relative risk threshold, Prism can detect 35 percent of PDAC cases at this same threshold.
Using AI to detect cancer risk is not a new phenomena — algorithms analyze mammograms, CT scans for lung cancer, and assist in the analysis of Pap smear tests and HPV testing, to name a few applications. “The PRISM models stand out for their development and validation on an extensive database of over 5 million patients, surpassing the scale of most prior research in the field,” says Kai Jia, an MIT PhD student in electrical engineering and computer science (EECS), MIT CSAIL affiliate, and first author on an open-access paper in eBioMedicine outlining the new work.
“The model uses routine clinical and lab data to make its predictions, and the diversity of the U.S. population is a significant advancement over other PDAC models, which are usually confined to specific geographic regions, like a few health-care centers in the U.S. Additionally, using a unique regularization technique in the training process enhanced the models’ generalizability and interpretability.”
“This report outlines a powerful approach to use big data and artificial intelligence algorithms to refine our approach to identifying risk profiles for cancer,” says David Avigan, a Harvard Medical School professor and the cancer center director and chief of hematology and hematologic malignancies at BIDMC, who was not involved in the study. “This approach may lead to novel strategies to identify patients with high risk for malignancy that may benefit from focused screening with the potential for early intervention.”
Prismatic perspectives
The journey toward the development of PRISM began over six years ago, fueled by firsthand experiences with the limitations of current diagnostic practices. “Approximately 80-85 percent of pancreatic cancer patients are diagnosed at advanced stages, where cure is no longer an option,” says senior author Appelbaum, who is also a Harvard Medical School instructor as well as radiation oncologist. “This clinical frustration sparked the idea to delve into the wealth of data available in electronic health records (EHRs).”
The CSAIL group’s close collaboration with Appelbaum made it possible to understand the combined medical and machine learning aspects of the problem better, eventually leading to a much more accurate and transparent model. “The hypothesis was that these records contained hidden clues — subtle signs and symptoms that could act as early warning signals of pancreatic cancer,” she adds. “This guided our use of federated EHR networks in developing these models, for a scalable approach for deploying risk prediction tools in health care.”
Both PrismNN and PrismLR models analyze EHR data, including patient demographics, diagnoses, medications, and lab results, to assess PDAC risk. PrismNN uses artificial neural networks to detect intricate patterns in data features like age, medical history, and lab results, yielding a risk score for PDAC likelihood. PrismLR uses logistic regression for a simpler analysis, generating a probability score of PDAC based on these features. Together, the models offer a thorough evaluation of different approaches in predicting PDAC risk from the same EHR data.
One paramount point for gaining the trust of physicians, the team notes, is better understanding how the models work, known in the field as interpretability. The scientists pointed out that while logistic regression models are inherently easier to interpret, recent advancements have made deep neural networks somewhat more transparent. This helped the team to refine the thousands of potentially predictive features derived from EHR of a single patient to approximately 85 critical indicators. These indicators, which include patient age, diabetes diagnosis, and an increased frequency of visits to physicians, are automatically discovered by the model but match physicians’ understanding of risk factors associated with pancreatic cancer.
The path forward
Despite the promise of the PRISM models, as with all research, some parts are still a work in progress. U.S. data alone are the current diet for the models, necessitating testing and adaptation for global use. The path forward, the team notes, includes expanding the model’s applicability to international datasets and integrating additional biomarkers for more refined risk assessment.
“A subsequent aim for us is to facilitate the models’ implementation in routine health care settings. The vision is to have these models function seamlessly in the background of health care systems, automatically analyzing patient data and alerting physicians to high-risk cases without adding to their workload,” says Jia. “A machine-learning model integrated with the EHR system could empower physicians with early alerts for high-risk patients, potentially enabling interventions well before symptoms manifest. We are eager to deploy our techniques in the real world to help all individuals enjoy longer, healthier lives.”
Written by Rachel Gordon
Source: Massachusetts Institute of Technology
You can offer your link to a page which is relevant to the topic of this post.
#A.I. & Neural Networks news#Adenocarcinoma#ai#alerts#Algorithms#Analysis#applications#approach#artificial#Artificial Intelligence#artificial intelligence (AI)#artificial neural networks#background#Beth Israel Deaconess Medical Center#Big Data#biomarkers#Biotechnology news#Cancer#cancer treatment#Collaboration#comparison#computer#Computer Science#data#Database#datasets#dates#detection#development#diabetes
0 notes
Text
“Revolutionize Your Health: The Ultimate Guide to Unlocking Comprehensive 360 degree Solutions and Cure Treatment Plans for “Cervical cancer” – Your Path to Lasting Wellness!” in 2023-2024
1 note
·
View note
Text
“Revolutionize Your Health: The Ultimate Guide to Unlocking Comprehensive 360 degree Solutions and Cure Treatment Plans for “Cervical cancer” – Your Path to Lasting Wellness!” in 2023-2024
0 notes
Text
Virtual Best Sexologist in Patna for STD Treatment | Dr. Sunil Dubey
When asked about the most common sexual diseases in women, world famous Ayurvedacharya Dr. Sunil Dubey says that there are three most common sexual diseases which always affect them. Their names are Human Papilloma Virus (HPV), Gonorrhea and Chlamydia. He said that these sexually transmitted infections can pass women in the vaginal fluid. That’s why; they can suffer from Sexual Pain Disorder like Pain during intercourse.
Dr. Sunil Dubey, the best sexologist doctor in Patna is one of the most experienced and Gold Medalist Ayurveda Specialist. He says that those women who realize the first stage of STDs in different ways.
The first sign of STD may include the following symptoms.
Abnormal discharge
Itching and soreness
Bleeding in the private area
Painful Sexual Intercourse
Bleeding after Sexual Intercourse
Pain or burning sensation when urinating
These above are some common factors those always indicate that a woman is under the influence of Sexually Transmitted Infections (STIs). In this condition, the female should not ignore it and directly consult the experienced Ayurveda and sexology medical science expert sexologist doctors.

About the treatment and medication of STDs:
Sexologist Dr. Sunil Dubey, honored with Bharat Gaurav, says that if sexual patients go to a real and experienced sexologist doctor in time, then treatment of STD is possible. If STD has affected a woman with infections like symphysis, gonorrhea, chlamydia and trichomoniasis; so these can be easily cured. These are the most common causes of sexually transmitted infections in women.
It can be easily cured in Ayurveda and Naturopathy without any side effects. Female sexual patients get relief from their problems after a few days of medicine. Dubey Clinic is India's most trusted and reputed Ayurveda and Sexology medical science clinic where male and female sex patients from all over India come to get their treatment and medicine. Don't waste your time and money; Just contact Dubey Clinic which is available over phone.
For more info:
Dubey Clinic, an ISO Certified Clinic in India
Dr. Sunil Dubey, Gold Medalist & Bharat Gaurav Awarded Sexologist
B.A.M.S (Ranchi), M.R.S.H (London), Ph.D. in Ayurveda (USA)
Helpline No: +91 98350 92586; +91 91555 55112
Venue: Dubey Market, Langar Toli Chauraha, Patna-04
Web info: https://ayurvedacharyadrsunildubey.com
Map Location: https://maps.app.goo.gl/SJX9u61BNbHh68HW8
#Sexologist#BestSexologist#FamousSexologist#SexologistInPatna#BestSexologistInPatna#DubeyClinic#DrSunilDubey#Patna#Bihar#India#Health#Clinic#Hospital#Naturopathy#GoldMedalist#Ayurveda#Ayurvdic#ErectileDysfunction#ErectionProblem#Healthcare#SexologistDoctors
0 notes
Text
Cervical Cancer – Symptoms, Diagnosis, Prevention for Indian Women - Dr Shweta Tahlan
Cervical Cancer (Cervix cancer) is the cancer originating in the lower part of uterus. Cervical Cancer is the second most common cancer affecting Indian women.
It is a highly preventable cancer and we have two strategies to save our women from this deadly disease.
HPV vaccination - It reduces the risk of developing precancer and cancer caused by HPV. As most cervical cancers are caused by high risk HPV, HPV vaccination is a strong tool in our fight against this disease. It is recommended to be given from 9 to 26 years, although 9-14 years is the ideal time to give the vaccine. Vaccines are safe, affordable, have been given to millions of women worldwide and are recommended by World Health Organisation. The vaccines are gender neutral, can be given to both girls and boys, as it prevents against all HPV related cancers.
Screening - All women over the age of 25 years are advised to undergo cervical screening at regular intervals even if they have no symptoms. Screening is done by Pap smear and HPV test. These tests are safe, painless and are done in OPD within minutes. The target of screening is to detect patients at precancer stage (when cancer has not yet developed) where patients can be cured altogether by simple surgical procedures.
Cervical Cancer Symptoms:
It's important to know the symptoms of this disease so that one can to go to the gynaecologist at earliest for checkup. Any vaginal bleeding or spotting after sexual intercourse (postcoital bleeding) or in between two periods (intermenstrual bleeding), after achieving menopause (post menopausal bleeding) needs to be checked. Other symptoms are irregular periods, persistent vaginal discharge, post menopausal vaginal discharge, pelvic pain, pain during sex.
Cervical Cancer Diagnosis:
The diagnosis is done by cervical biopsy. Colposcopy is done along with cervical biopsy to detect precancer lesions in women with abnormal screening tests or in those with suspicious clinical features by Oncologists in Mohali.
Cervical Cancer Treatment:
Cervical cancer is highly treatable with good survival outcomes in early stages by surgery. In advanced cases, we give radiotherapy and chemotherapy to treat the disease. Individualised treatment is given to every patient depending on clinical findings, biopsy report and imaging features.
Cervical Cancer Prevention:
Cervical cancer is a preventable, easily detectable and treatable cancer. HPV vaccination and regular screening are the key components in its prevention. Awareness about the symptoms and clinical examinations help in early detection which leads to better treatment outcomes.
0 notes
Text
HPV, most comprehensive understanding
Human Papillomavirus (HPV) is a group of related viruses that can infect the genital area, as well as the mouth and throat. There are over 200 different types of HPV, and some of them can cause various health problems, including genital warts and cancers.
Causes: HPV is primarily spread through intimate skin-to-skin contact, commonly through vaginal, anal, or oral sex. The virus can be transmitted even when an infected person does not show any signs or symptoms.
Types of Infection:
Low-Risk HPV: Can cause genital warts and mild cervical cell changes.
High-Risk HPV: Persistent infection with certain high-risk types can lead to the development of cancers, including cervical, anal, and oropharyngeal cancers.
Symptoms: Many people infected with HPV do not show any symptoms, and the infection often resolves on its own. However, when symptoms do occur, they may include genital warts, abnormal Pap test results, or, in the case of cancer, symptoms related to the specific cancer type.
Treatment: There is no cure for HPV, but most infections resolve on their own without causing any health problems. For conditions like genital warts or abnormal cell changes, treatments are available to manage symptoms and prevent complications.
Prevention:
Vaccination: HPV vaccines are highly effective in preventing infection with the most common types of the virus. Vaccination is recommended for both males and females before they become sexually active.
Safe Sex Practices: Consistent and correct use of condoms can reduce the risk of HPV transmission, but they do not provide complete protection as the virus can infect areas not covered by the condom.
Regular Screenings: Routine screenings, such as Pap tests and HPV tests, can help detect abnormal cell changes or infections early, allowing for timely intervention.
0 notes