#No Context Crow No. 317
Text
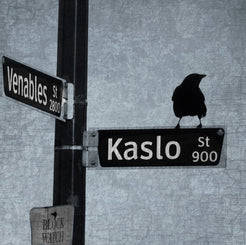
No Context Crow #317: Wayfinder Crow
Done by June Hunter!
#crows#corvids#corvidae#birds#animals#art#drawing#illustration#wayfinder#sign post#signs#street signs#metal signs#June Hunter#daily crows#crow queue#No Context Crow No. 317
49 notes
·
View notes
Text
Efficacy of Telehealth in Australia
Alexander, M. 1996. “Telemedicine in Australia. 1: The Health Communication Network.” Journal Of Telemedicine And Telecare 2. http://jtt.sagepub.com/content/1/4/187.full.pdf.
Alexander, M. 1996. “Telemedicine in Australia. 2: The Health Communication Network.” Journal Of Telemedicine And Telecare 1. https://www.ncbi.nlm.nih.gov/pubmed/9375035.
Anonymous. 2010. “The Potential of Telehealth in Australia.” PharmacoEconomics & Outcomes News (618): 10. http://trove.nla.gov.au/work/152879680?versionId=166613328.
Armfield, Nigel R., Sisira K. Edirippulige, Natalie Bradford, and Anthony C. Smith. 2014. “Telemedicine--Is the Cart Being Put before the Horse?” The Medical journal of Australia 200(9): 530–33. https://www.mja.com.au/journal/2014/200/9/telemedicine-cart-being-put-horse.
Benzion, Itay, and Eugene M. Helveston. 2007. “Use of Telemedicine to Assist Ophthalmologists in Developing Countries for the Diagnosis and Management of Four Categories of Ophthalmic Pathology.” Clinical ophthalmology (Auckland, N.Z.) 1(4): 489–95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2704545/.
Berkhof, Farida F., Jan W. K. Van Den Berg, Steven M. Uil, and Huib A. M. Kerstjens. 2015. “Telemedicine, the Effect of Nurse-Initiated Telephone Follow Up, on Health Status and Health-Care Utilization in COPD Patients: A Randomized Trial.” Respirology (Carlton, Vic.) 20(2): 279–85. http://onlinelibrary.wiley.com/doi/10.1111/resp.12437/pdf.
Boots, RJ, SJ Singh, and J Lipman. 2012. “The Tyranny of Distance: Telemedicine for the Critically Ill in Rural Australia.” Anaesthesia and Intensive Care 40(5): 871–74. https://www.ncbi.nlm.nih.gov/pubmed/22934873.
Bursell, Sven-Erik et al. 2013. “Telehealth in Australia: An Evolution in Health Care Services.” The Medical journal of Australia 199(1): 23–24. https://www.mja.com.au/journal/2013/199/1/telehealth-australia-evolution-health-care-services.
Bursell, SE, S Zang, AC Keech, and AJ Jenkins. 2016. “Evolving Telehealth Reimbursement in Australia.” Internal Medicine Journal 46(8). http://onlinelibrary.wiley.com.ezproxy.flinders.edu.au/doi/10.1111/imj.13150/abstract.
Celler, Bg, Nh Lovell, and Dky Chan. 1999. “The Potential Impact of Home Telecare on Clinical Practice.” 171(10): 518–21. https://www.mja.com.au/journal/1999/171/10/potential-impact-home-telecare-clinical-practice.
Chow, Josephine, and et al. 2016. “Beyond Dialysis - Telehealth Initiatives.” Renal Society of Australasia Journal12(1). http://www.renalsociety.org/public/6/files/documents/RSAJ/2016%2003/04%20chow.pdf.
Clark, R. A. et al. 1999. “A Growing Partnership in Telehealth.” https://core.ac.uk/display/10914950 (February 9, 2016).
Conlan, Lee, Judith Thompson, and Robyn Fary. 2016. “An Exploration of the Efficacy of Telehealth in the Assessment and Management of Stress Urinary Incontinence among Women in Rural Locations.” Australian and New Zealand Continence Journal, The 22(3).
Crowe, BL. 1997. “Telemedicine in Australia: Recent Developments.” Journal of Telemedicine and Telecare 3(1). https://www.ncbi.nlm.nih.gov/pubmed/9614732.
Crowe, B. L. 2001. “A Review of the Experience with Teleradiology in Australia.” Journal of Telemedicine and Telecare 7(suppl 2): 53–54. http://jtt.sagepub.com/content/7/suppl_2/53 (November 27, 2015).
Crowe, B., and P. Macisaac. 2006. “The Application of Qualitative Approaches to the Evaluation of Telehealth Systems in Australia.” Journal Of Telemedicine And Telecare 12: 33–35. http://jtt.sagepub.com/content/12/suppl_3/33.abstract.
D’Souza, R. 2000. “A Satisfaction Study of General Practitioners, and Community Mental Health Workers in Rural and Remote Areas with the Use of Telemedicine for Managing Their Psychiatric Patients.” Australian and New Zealand Journal of Psychiatry 34(s1): A20–A20. http://www.tandfonline.com/doi/abs/10.1080/000486700597.
Dattakumar, Ambica. 2013. “A Unified Approach for the Evaluation of Telehealth Implementations in Australia.” http://apo.org.au/research/unified-approach-evaluation-telehealth-implementations-australia (February 5, 2016).
David, L, R Reuben, and Jr McDaniel. 2016. “Facilitating Telemedicine Project Sustainability in Medically Underserved Areas: A Healthcare Provider Participant Perspective.” BMC Health Services Research 16. http://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-016-1401-y.
Della Mea, V. 1999. “Internet Electronic Mail: A Tool for Low-Cost Telemedicine.” Journal of telemedicine and telecare 5. http://jtt.sagepub.com/content/5/2/84.full.pdf.
Doolan, D. 2013. “A Telehealth Connection Service.” http://www.hisa.org.au/slides/wed/DavidDoolan.pdf.
Eley, Robert et al. 2008. “Nurses’ Confidence and Experience in Using Information Technology.” https://core.ac.uk/display/11037222 (February 7, 2016).
Eley, Robert et al. 2009. “Attitudes of Australian Nurses to Information Technology in the Workplace: A National Survey.” https://core.ac.uk/display/11036380 (February 9, 2016).
Ellis, I. 2004. “Is Telehealth the Right Tool for Remote Communities? Improving Health Status in Rural Australia.” Contemporary Nurse: A Journal for the Australian Nursing Profession 16(3): 163–68. https://www.ncbi.nlm.nih.gov/pubmed/15125098.
Fatehi, F, NR Armfield, M Dimitrijevic, and LC Gray. 2014. “Clinical Applications of Videoconferencing: A Scoping Review of the Literature for the Period 2002-2012.” Journal of Telemedicine and Telecare 20(7): 377–83. https://www.ncbi.nlm.nih.gov/pubmed/25399998.
Garrett, Cc et al. 2011. “Young Adults’ Views on Telemedicine Consultations for Sexual Health in Australia.” Sexually Transmitted Infections 87: A89–A89. http://sti.bmj.com/content/87/Suppl_1/A89.2.
Gool, K. van, M. R. Haas, and R. Viney. 2002. “From Flying Doctor to Virtual Doctor: An Economic Perspective on Australia’s Telemedicine Experience.” Journal of Telemedicine and Telecare 8(5): 249–54. http://jtt.sagepub.com/content/8/5/249 (November 27, 2015).
Haleh Ayatollahi, Mostafa Hasannezhad, Hedieh Saneei Fard, and Mehran Kamkar Haghighi. 2016. “Type 1 Diabetes Self-Management: Developing a Web-Based Telemedicine Application.” Health Information Management Journal 45(1). http://him.sagepub.com/content/45/1/16.
Helen Rienits, Greg Teuss, and Andrew Bonney. 2016. “Teaching Telehealth Consultation Skills.” The clinical teacher 13(2). http://onlinelibrary.wiley.com/doi/10.1111/tct.12378/abstract.
Hereward, Joanne. 2012. “Telehealth in General Practice: Providing Alternative Access Options for People in Regional, Rural and Remote Areas.” HIV Australia 10(2): 27–28. https://www.afao.org.au/library/hiv-australia/volume-10/vol.-10-number-2/telehealth-in-general-practice-providing-alternative-access-options#.V_Jx6vl97IU.
Jang-Jaccard, Julian, Surya Nepal, Leila Alem, and Jane Li. 2014. “Barriers for Delivering Telehealth in Rural Australia: A Review Based on Australian Trials and Studies.” Telemedicine Journal and E-Health: The Official Journal of the American Telemedicine Association 20(5): 496–504. https://www.ncbi.nlm.nih.gov/pubmed/24801522.
Jang-Jaccard, Julian, Surya Nepal, Branko Celler, and Bo Yan. 2016. “WebRTC-Based Video Conferencing Service for Telehealt.” Computing 98(1): 169. http://link.springer.com/article/10.1007/s00607-014-0429-2.
Jhaveri, D, S Larkins, and S Sabesan. 2015. “A Systematic Review to Analyse the Outcomes of Active Medical Therapies Delivered with Telemedicine Support to Rural and Remote Populations.” Internal Medicine Journal 45: 12–13. http://onlinelibrary.wiley.com/doi/10.1111/imj.12782_45/full.
Knight, Patricia et al. 2016. “Positive Clinical Outcomes Are Synergistic With Positive Educational Outcomes When Using Telehealth Consulting in General Practice: A Mixed-Methods Study.” Journal of Medical Internet Research18(2). http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4763112/ (August 17, 2016).
Knight, Patricia et al. 2016. “Positive Clinical Outcomes Are Synergistic With Positive Educational Outcomes When Using Telehealth Consulting in General Practice: A Mixed-Methods Study.” Journal of medical Internet research18(2). https://www.jmir.org/2016/2/e31/.
Kuipers, Willem (Pim) et al. 2008. “Primary Health Care Delivery Models in Rural and Remote Australia - a Systematic Review.” https://core.ac.uk/display/14936095 (February 9, 2016).
Kumar, Sajeesh K. R., Yogesan Kanagasingam, and Ian J. Constable. 2004. “Should Telemedicine in Eye Care Be Funded in Australia?” Medical Journal of Australia 181(10): 583. https://www.mja.com.au/journal/2004/181/10/should-telemedicine-eye-care-be-funded-australia.
Landgreen, Ian R. 2002. “‘Do No Harm’: A Comparative Analysis of Legal Barriers to Corporate Clinical Telemedicine Providers in the United States, Australia, and Canada.” Georgia Journal of International and Comparative Law30(2): 365–90. http://digitalcommons.law.uga.edu/cgi/viewcontent.cgi?article=1383&context=gjicl.
Lessing, K., and I Blignault. 2001. “Mental Health Telemedicine Programmes in Australia.” Journal of Telemedicine and Telecare 7(6): 317–23. http://jtt.sagepub.com/content/7/6/317.full.pdf.
Lugg, DJ. 2000. “Telemedicine: The Cornerstone of Australian Antarctic Medical Practice.” Informatics in Healthcare Australia 8(2): 61–64. http://search.informit.com.au/documentSummary;dn=923306084723965;res=IELHEA.
Magrabi, Farah. 2007. “Integrating Telemedicine.” Medical Journal of Australia 186(2): 95. https://www.mja.com.au/journal/2007/186/2/integrating-telemedicine.
Milstein, Robert D., and Robert D. Milstein. 1999. “Telehealth: Opportunities and Liabilities.” Medical Journal of Australia 171(10): 561–62. https://www.ncbi.nlm.nih.gov/pubmed/10816712.
Mitchell, J. G. 1999. “The Uneven Diffusion of Telemedicine Services in Australia.” Journal of telemedicine and telecare 5 Suppl 1: S45–47. https://www.ncbi.nlm.nih.gov/pubmed/10534838.
Moffatt, Jennifer J., and Diann S. Eley. 2011. “Barriers to the up-Take of Telemedicine in Australia--a View from Providers.” Rural and remote health 11(2): 1581. https://www.ncbi.nlm.nih.gov/pubmed/21385004.
Mohamed Estai, Estie Kruger, and Marc Tennant. 2016. “Role of Telemedicine and Mid-Level Dental Providers in Expanding Dental-Care Access: Potential Application in Rural Australia.” International Dental Journal 66(4). http://onlinelibrary.wiley.com/doi/10.1111/idj.12217/abstract;jsessionid=878A78BE1717F08039D5457D2B6D7EB6.f04t04.
Perkins, David. 2015. “Telehealth Will Supersede Face-to-Face Consultations in Rural Australia by 2025.” The Australian journal of rural health 23(5): 255–56. https://www.ncbi.nlm.nih.gov/pubmed/26425789.
Pickett, Steve M., George W. Van Der Heide, and Steve M. Pickett. 1999. “Medicolegal Risk in Telemedicine: Risk Control in Teleradiology.” Medical Journal of Australia 171(10): 563–65. https://www.ncbi.nlm.nih.gov/pubmed/10816713.
Sabesan, Sabe, and Jenny Kelly. 2015. “Implementing Telehealth as Core Business in Health Services.” The Medical Journal of Australia 202(5): 231–33. https://www.mja.com.au/journal/2015/202/5/implementing-telehealth-core-business-health-services.
Silberstein, M., and J. Hornstein. 1997. “Telemedicine: Here to Stay.” The Medical journal of Australia 166(11): 616. https://www.ncbi.nlm.nih.gov/pubmed/9076272.
Smith, Anthony C, and Leonard C Gray. 2009. “Telemedicine across the Ages.” Medical Journal of Australia 190(12): 719. https://www.mja.com.au/journal/2009/190/1/telemedicine-across-ages.
Smith, A. C., N. R. Armfield, J. Croll, and L. C. Gray. 2012. “A Review of Medicare Expenditure in Australia for Psychiatric Consultations Delivered in Person and via Videoconference.” J Telemed Telecare 18: 169–71. http://jtt.sagepub.com/content/18/3/169.full.pdf.
Walsh, M., and A. Chipperfield. 2000. “Australian National Telehealth Think Tank.” Journal of telemedicine and telecare 6(6): 353. http://jtt.sagepub.com/content/6/6/353.extract.
Wootton, Richard, Ilse Blignault, and Joanne Cignoli. 2003. “A National Survey of Telehealth Activity in Australian Hospitals.” Journal of Telemedicine and Telecare 9(suppl 2): 73–75. http://jtt.sagepub.com/content/9/suppl_2/73(November 27, 2015).
Wyatt, Stephanie N. et al. 2013. “Maternal Response to High?risk Obstetric Telemedicine Consults When Perinatal Prognosis Is Poor.” Australian and New Zealand Journal of Obstetrics and Gynaecology 53(5): 494–97. http://onlinelibrary.wiley.com/doi/10.1111/ajo.12094/abstract.
Yellowlees, Peter. 2001. “An Analysis of Why Telehealth Systems in Australia Have Not Always Succeeded.” Journal of Telemedicine and Telecare 7(suppl 2): 29–31. http://jtt.sagepub.com/content/7/suppl_2/29 (August 21, 2016).
Yellowlees, P., and W. T. Mccoy. 1993. “Telemedicine. A Health Care System to Help Australians.” The Medical journal of Australia 159(7): 437–38. https://www.ncbi.nlm.nih.gov/pubmed/8412912.
Yellowlees, P., M. Chapman, and K. Fielke. 2013. “Telehealth: Anywhere, Anytime, Achievements and Aspirations.” Australian And New Zealand Journal Of Psychiatry 47(S1): 19–20. http://anp.sagepub.com/content/47/1_suppl.toc.
Zilliacus, E, and B Meiser. 2010. “The Virtual Consultation: Practitioners’ Experiences of Genetic Counseling by Videoconferencing in Australia.” Telemedicine journal and e-health?: the official journal of the American Telemedicine Association 16(3): 350–57. https://www.ncbi.nlm.nih.gov/pubmed/20406122.
doctoroo
0 notes
Text
"The architectural world seems to be responding to Charlottesville with deafening silence"
When Neo-Nazis are marching in the streets, architects need to step up and confront the issues surrounding colonial monuments, argues Phineas Harper.
Baying Neo-Nazis grasping flaming torches on the steps of the University of Virginia's Rotunda, designed by president-turned-architect, Thomas Jefferson in the 1820s, was the chilling prelude to the events of Saturday 12 August 2017 in Charlottesville.
The fascists came from far afield in an organised display of white-supremacist hatred that left 19 injured, one murdered, two troopers dead in a helicopter crash and America reeling. At the heart of their stated mission was a local authority planning decision – the proposed removal (and sale) of a poorly executed bronze statue depicting a defeated Confederate general made 59 years after the end of the civil war.
The extraordinary events of Charlottesville have revealed the terrifying emboldenment of white supremacism under President Trump and show that the question of memorialisation in public space has become the most incendiary architectural debate of our time.
The demolition of monuments is as much a symbolic act as their erection and just as old. From the British destruction of Beijing's Gardens of Perfect Brightness amid the second Opium War to ISIS bombing the Great Mosque of al-Nuri in Mosul two months ago, monuments have been made and torn down to further political projects of all creeds.
The question of memorialisation in public space has become the most incendiary architectural debate of our time
Recent iconoclastic campaigns, however, are not set against a backdrop of imperial war. They are instead taking place domestically, as populations wrestle with the appropriate manner to reflect on the dark moments and contested figures of their past. My question is this: where on earth are architects in this discussion? The contemporary iconoclasm movement is no passing parochial fad, but marks a profound global shift in public agency over our streets. It wraps some of the most challenging discussions of colonialism, anti-racism and the built expression of public values into a fundamentally spatial problem. The design of the civic realm is at the absolute core of our expertise and yet the architectural world seems to be responding to this urgent conflict with deafening silence.
It cannot be to right to take a back seat, passively waiting for battles over public monuments to run their course, when acute suffering accompanies each struggle. How many neighbourhoods must endure mobs of Neo-Nazis marching past their homes? How many antifascist demonstrators will be hurt or killed in the counter demonstrations? This is not a situation that should be left to fumble along in bursts of violence. It calls for urgent creative attention and bold proposals. It calls on architects not to step back, but to step up.
In 1991, Hungarian architect Ákos Eleőd began work on an open-air museum several miles outside Budapest's city centre, to relocate the city's many Soviet statues erected over decades of occupation. With the fall of the USSR, central and eastern European nations had entered protracted periods of rediscovering their cultural identity. As the Red Army had crept west, they had become trigger-happy makers of monuments to idealised workers, soldiers and the grandfathers of communism. Often the new sculptures would deliberately replace existing ones, expunging the folk memories that once resonated in those districts and supplanting them with Russian propaganda.
This situation calls for urgent creative attention and bold proposals. It calls on architects not to step back, but to step up
After the Berlin Wall fell, Budapest, like other Eastern Bloc cities, had to look at redesigning its urban landscape, which was now littered with concrete Lenins. The USSR had effectively controlled Hungary for half a century, perpetuating violent suppression, forced labour and man-made famines that left millions dead. Yet it also constituted a huge chapter in their nationhood and was thought of nostalgically by many, especially older generations. The statues were a schizophrenic symbol of both abject suffering and paternalistic care. The challenge was to detoxify the stain of Sovietism but in a nuanced way – a way which could be more sympathetic that the USSR's top-down rewriting of local history.
Eleőd's Memento Park, completed in 1993, is a calm but surreal space in which the giant frozen figures are arranged along six circular gravel paths. A free-standing neo-byzantine brick portico forms a gatehouse accommodating cubist sculptures of Karl Marx and Friedrich Engels. But it feels deliberately thin – a nod, not an endorsement.
The rest of the park is grand in scale, but not opulent. The statues are treated with basic curatorial respect but are not venerated. Even charging of an entry fee rather than relying on public subsidies seems like a carefully considered decision to establish the appropriate tone for these equivocal monuments. Memento Park is not necessarily the perfect model to be rolled out across the world but it demonstrates how architecture can navigate extreme political differences to articulate bitter moral conflict more effectively than language can.
"Nelson's Column should be next" thundered the Guardian in a predictably clickbaity attempt to test the logical next step after Charlottesville. It was a provocative thought experiment but the bullish reduction hard moral questions to a churlish "keep it" vs "knock it down" binary that is typical of a media-led public debate will ultimately fail to provide meaningful restitution on any side.
Even universally lionised heroes of the past measure up abysmally to the ethical expectations of subsequent generations. The Suffragettes' links to early British fascists are well known – should Emmeline Pankhurst's memorial in Westminster therefore face the chop? Mahatma Gandhi is recored to have harboured racist thoughts about Africans – should his statue in Nelson Mandela Square be removed as a similar one was at the University of Ghana?
Or what of George Washington? At the time of his death, 317 people were enslaved at Washington's family home, 153 of whom he owned personally. What coherent moral argument can necessitate the removal of a Robert E Lee statue but spare the founding father? Surely if Lee must fall then so must Mount Rushmore and the one dollar bill.
Barack Obama remains an inspiration to many. But it's not hard to imagine iconoclasts of the future citing the tens of thousands who died in Iraq during his presidency, or the waves of drone bombings he authorised in support of an Obama Must Fall campaign.
It is not possible to simplistically set an ethical bar when weighing the actions of a supposed hero's right to a plinth
It is not possible to simplistically set an ethical bar when weighing the actions of a supposed hero's right to a plinth in public space. This conception of human morality is too narrow. Context is crucial. Winston Churchill's statue might be acceptable in London's Parliament Square, but it would be sick in Dresden.
Eric Foner, professor of history at Columbia University, argues that commissioning should be considered and that the symbolic authenticity of the confederate statues is disingenuous, adding to the case against them. Many were built long after the civil war. Their rushed construction, Foner argues, was not about mourning dead soldiers, but really triumphalist intimidation of black Americans suffering under the infamous Jim Crow laws.
Architects must not stand on the edge of this debate. Our leaders are failing to bring forward effective proposals to deal promptly with our tainted public spaces, while our media frames the struggle in unsatisfactory terms. We cannot sit aside, letting the struggle play out as a series of deadly skirmishes, handing Neo-Nazis easy opportunities to grab headlines and causing trauma to communities. Instead architects should pour creative energy into this issue, bring bold new ideas to the table and at the very least speak out against against those who turn our public spaces into platforms of hate.
Phineas Harper is a critic and designer. He is deputy director of the Architecture Foundation and former deputy editor of the Architectural Review. He is author of the Architecture Sketchbook (2015) and People's History of Woodcraft Folk (2016). In 2015 he co-created Turncoats, a design-based debating society which now has chapters in four continents.
Photograph shows the Robert E Lee statue in Charlottesville.
The post "The architectural world seems to be responding to Charlottesville with deafening silence" appeared first on Dezeen.
from ifttt-furniture https://www.dezeen.com/2017/08/29/phineas-harper-opinion-column-architects-respond-charlottesville-deafening-silence-monuments/
0 notes
Text
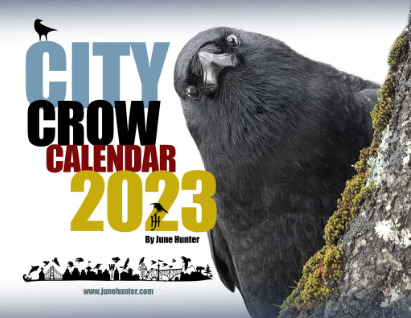
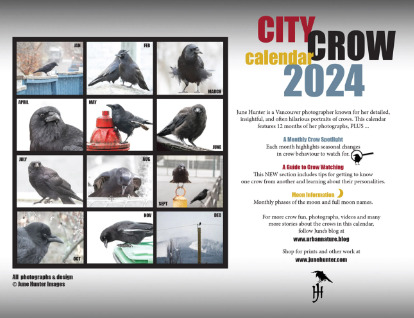
No Context Crow #317: Calendar of Crows
(for those of you enjoying this blog, you'll probably enjoy this too)
(click for better quality!)
#crows#corvids#corvidae#birds#animals#art#photography#calendar#city crow calendar#calendars#2024 calendar#daily crows#crow queue#No Context Crow No. 317
11 notes
·
View notes