#PULMONARY MALIGNANT MESOTHELIOMA
Link
#survival#malignant mesothelioma#PULMONARY MALIGNANT#PULMONARY MALIGNANT MESOTHELIOMA#survival rates
0 notes
Text
Mesothelioma | Causes, Symptoms, and Treatments
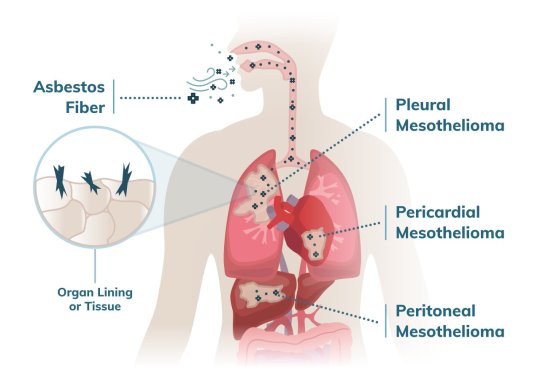
Mesothelioma is a rare and deadly cancer that originates from mesothelial cells of the pleura or serosal surfaces such as the peritoneum, pericardium, and tunica vaginalis.
It is most commonly observed in the pleura (65-70%), followed by the peritoneum (30%), pericardium, and tunica vaginalis (1-2%).
This type of tumor, which is associated with somatic and germline mutations, envelops and compresses organs and body cavities.
Asbestos exposure is the single most common cause (over 90% of mesotheliomas).
Common symptoms of malignant pleural mesothelioma include chest pain and dyspnea.
Dyspnea indicates the presence of pleural effusion.
There may also be general symptoms like unintentional weight loss, loss of appetite, cough, fatigue, and chest wall mass.
The only type of mesothelioma that can be staged is malignant pleural mesothelioma.
Early diagnosis is very difficult due to its silent progression and the long latent period.
A thorough history of occupational and environmental asbestos exposure is required for proper diagnosis.
CXR (or CT) shows:
Pleural effusion
Pleural mass or thickening ± free fluid.
Concomitant pleural plaques or pulmonary fibrosis (minority).
Local invasion of the chest wall, heart, or mediastinum.
Death is unavoidable within 4 to 6 months. Some patients may survive for 15 to 18 months with treatment.
Treatment depends on the stage of the tumor, with Stage III-IV malignant pleural mesothelioma being regarded as incurable and not susceptible to surgical resection.
The most common treatment options are surgical resection, chemotherapy, radiotherapy, and immunotherapy.
Read more at: Mesothelioma | Causes, Symptoms, and Treatments
0 notes
Text
Pleural Mesothelioma Treatment
In this article, we will discuss Pleural Mesothelioma Treatment (Management Overview). So, let’s get started.
Management
The NCCN Guidelines recommend that patients with MPM be managed by a multidisciplinary team with experience in MPM. Treatment options for patients with MPM include surgery, radiation therapy (RT), and/or chemotherapy. Select patients with medically operable disease are…
View On WordPress
#Malignant Pleural Mesothelioma#Medicine#Oncology#Physiotherapy#Pleural Mesothelioma#pulmonary medicine#Pulmonology
0 notes
Text
Reviewing questions:
Mesothelial cells are cells that line body cavities (including the peritoneum and pericardium, not just the pleura).
Mesothelial cells form a monolayer of specialised pavement-like cells that line the body's serous cavities and internal organs. The primary function of this layer, termed the mesothelium, is to provide a slippery, non-adhesive and protective surface. However, mesothelial cells play other pivotal roles involving transport of fluid and cells across the serosal cavities, antigen presentation, inflammation and tissue repair, coagulation and fibrinolysis and tumour cell adhesion. Injury to the mesothelium triggers events leading to the migration of mesothelial cells from the edge of the lesion towards the wound centre and desquamation of cells into the serosal fluid which attach and incorporate into the regenerating mesothelium. If healing is impaired, fibrous serosal adhesions form between organs and the body wall which impede vital intrathoracic and abdominal movement. Neoplastic transformation of mesothelial cells gives rise to malignant mesothelioma, an aggressive tumour predominantly of the pleura. Although closely associated with exposure to asbestos, recent studies have implicated other factors including simian virus 40 (SV40) in its pathogenesis.
Anyway, mesothelioma is cancer of the pleura associated with asbestos exposure. It can present with dyspnea, chest pain, cough, and hemorrhagic pleural effusion. If you look at the histology, there will be tumor cells with long microvilli and tonofilaments. CT scan will show pleural plaques.
CREST syndrome = Calcinosis, Raynaud phenomenon (vasospasm of fingers in response to cold), Esophageal dysmotility, Sclerodactyly (localized thickening and tightness of the skin of the fingers or toes), Telangiectasias (small dilated blood vessels that can occur near the surface of the skin or mucous membranes; spider veins). CREST syndrome is the limited cutaneous form of systemic sclerosis. Sysemic sclerosis can lead to pulmonary arterial hypertension due to remodeling of pulmonary arteries and arterioles. Activated T cells secrete TGF-beta, which causes fibroblast proliferation-> excess collagen deposition. There is also excess endothelin (vasoconstrictive) and TXA2 (enhances proliferation)-> vasoconstriction.
I didn't know fluid could go through the diaphragm. There are fenestrations in the diaphragm through which fluid from ascites can travel, causing pleural effusion. Specifically, the ascites in a pt with cirrhosis can cause hepatic hydrothorax, which is a transudative pleural effusion. The pleural effusion is usually on the right side. I don't think I've ever heard of hepatic hydrothorax.
Endothelin causes vasoconstriction. Thromboxane A2 (TXA2) causes proliferation of vascular smooth muscle. Nitric oxide causes vasodilation. Prostacyclin prevents proliferation of vascular smooth muscle. In Pulmonary Arterial Hypertension (PAH), there's increased endothelin and TXA2 and decreased NO and prostacyclin. This causes constriction of the pulmonary arterioles and arteries and proliferation of the vascular smooth muscle, which causes intimal thickening and thus a decreased lumen of the arterioles/arteries-> increased resistance-> loud P2 (pulmonic component of the S2 heart sound) due to increased pressure in the pulmonary artery, so when the valve closes, it closes forcefully. Endothelin comes from the endothelial cells, binds to the endothelin-1 receptor on vascular smooth muscle cells, and leads to vasoconstriction and proliferation of vascular smooth muscle cells. Endothelin-1 receptor antagonists (e.g. bosentan) prevent this. NO comes from L-arginine in the endothelium, enters vascular smooth muscle cells, increases cGMP-> vasodilation and decreased proliferation of vascular smooth muscle cells. Phosphodiesterase inhibitors (e.g. sildenafil) and nitrates (nitroglycerin) also work the same way (i.e., they increase cGMP-> vasodilation). Arachidonic acid from the endothelium becomes prostacyclin (aka prostaglandin I2), which increases cAMP in the vascular smooth muscle cells-> vasodilation and decreased proliferation of vascular smooth muscle cells. Prostacyclin analogs (epoprostanol) work the same way.
CHF-> pleural effusion because there's more blood in the heart, which isn't pumping well-> increased hydrostatic pressure in the pulmonary vasculature. Glucose in the pleural fluid will be decreased in pts with exudative pleural effusions. WBCs metabolize glucose; more inflammation means more WBCs and thus more glucose is being used up by the WBCs, so the glucose in the pleural fluid will be low. In transudative pleural effusions, there is no inflammation, so the glucose of the pleural fluid will be normal or high. The nucleated cell count of the pleural fluid will be low in a transudative pleural effusion (I'm assuming that's because there aren't a bunch of WBCs in the pleural fluid if it's transudative as compared to exudative, which would have more WBCs [nucleated cells] in the pleural fluid).
Carotid body chemoreceptors transmit information via the glossopharyngeal nerve (CN IX) to the medulla. Aortic arch baroreceptors and aortic body chemoreceptors transmit information via the vagus nerve (CN X) to the medulla. I need to think of a way to remember this: carotid body->CN IX-> medulla and aortic arch-> CN X-> medulla. I thought of a mnemonic: a perfect 10 (X) is like an A, so Aortic chemoreceptors transmit through CN X.
In normal pts, PaCO2 increases trigger increased respiratory rate. In COPD, the respiratory drive is driven by PaO2 instead of PCO2 because chronic retention of CO2 blunts the normal respiratory drive, which is driven by PaCO2. So I guess basically, if you always have high PaCO2, then the chemoreceptors don't pay as much attention to CO2; instead, they rely on low PO2 to cause enhanced respiration. Low O2 (hypoxemia) increases respiratory rate in pts with COPD. This is why giving too much O2 in these pts actually decreases their respiratory drive--you made it so there's high O2 instead of their normal baseline low O2. If the chemoreceptors sense high O2, then they think they don't have to trigger respiratory drive anymore, so the pt will breathe less and actually start retaining even more CO2 than normal. Peripheral chemoreceptors sense PaO2. The carotid and aortic bodies sense PaO2; they respond to low levels of O2 in blood. So if you increase O2 by giving supplemental O2, you prevent those peripheral chemoreceptors from responding. So ironically, COPD pts get oxygen-induced hypercapnia after you give them oxygen--they have high PCO2 if you give them roo much oxygen. But that's not the main mechanism that causes oxgen-induced hypercapnea in these pts--what mostly causes increased PCO2 after O2 administration in these pts is the fact that you've undone the hypoxic vasoconstriction when you give too much O2, therefore blood starts going to less-well ventilated alveoli, so you essentially increased their dead space. This means more blood is flowing to areas without ventilation, so they can't get rid of as much CO2 as they normally can-> hypercapnea.
In the anesthesia meeting this morning, they were talking about a pt who had high PCO2 (65+ mmHg) and who was thus kept intubated after surgery. When they looked at his bicarbonate, they saw that it was high (30 mEq/L) at baseline. That means his body is compensating for long-term CO2 retention. So he normally probably has a high PCO2 and thus his PCO2 (while it would be considered high for a normal person) was probably not high for him specifically. So he probably didn't need to be kept intubated. He already lives at a high PCO2. It's like what I learned in my last rotation about OHS/sleep apnea.
So oxygen doesn't normally regulate respiratory drive, CO2 does. Only when PO2 is less than ~65 mmHg do the peripheral chemoreceptors start responding to oxygen as their stimulus for regulating respiration. In pts with COPD, their chemoreceptors stop responding to PCO2. COPD pts can also be hypoxemic with PO2 less than 65 mmHg. So their chemoreceptors start relying on low PO2 to increase respiratory drive. The peripheral chemoreceptors in the carotid and aortic bodies respond to low PO2 to cause increased respiratory drive. Ironically, giving more O2 in pts with COPD causes even more CO2 retention than normal because the increased oxygen level decreases their respiratory drive. So they get O2 and they start breathing less. But apparently, that's not the major mechanism of oxygen-induced hypercapnia. The major mechanism of oxygen-induced hypercapnia is increased V/Q mismatch. If you give too much O2, the poorly ventilated areas vasodilate, leading to more blood flowing to areas that are not well-ventilated. That's what this question explanation says, but I'm confused. I'm not getting what causes the vasodilation. I guess giving O2 makes the less well ventilated areas better ventilated, but they are still not as well ventilated as the areas that at baseline were already better ventilated. So now blood is going away from the alveoli that were already better ventilated to areas that aren't as well ventilated even after you gave O2. It says this causes increased physiologic dead space, so increased V/Q mismatch.
#mesothelioma#asbestos#CREST syndrome#PAH#pleural effusion#hepatic hydrothorax#prostacyclin#TXA2#thromboxane#nitric oxide#oxygen induced hypercapnea
8 notes
·
View notes
Text
How to Identify Asbestos Insulation in a Building
Asbestos is a natural fibrous matter with very outstanding qualities: it can efficiently defend against heat, steam, and fire. These qualities make asbestos the just right material for insulation, which were utilized to line roofs, attics, and ceilings of both dwellings and buildings. This kind of insulation was extensively utilized in housing, public, and business-related buildings prior to the 1980's.
Construction material
Despite its outstanding qualities that made it the just right ingredient for building materials, asbestos is highly dangerous to both the wellbeing of humans and animals. Asbestos consists of quite a lot of silicate minerals that can be detached into fibres and particles straightforwardly. At what time inhaled and ingested, these fibres can lead to a multiplicity of pulmonary diseases, together with asbestos poisoning (a scar of the lung tissues caused via spiky asbestos fibres and will lead to chest tenderness, dumpiness of breath, and dehydrated coughing), mesothelioma (a malignancy exclusive to asbestos exposure-and an exceedingly deadly one), and a number of kinds of malignancy that will have an effect on the lungs, stomach, and the kidneys. In this situation, Commercial Asbestos Removal in New Jersey is greatly recommended.
Asbestos insulation is a quandary that plagues a great deal of homeowners and land owners. Action should be straight away taken i.e. Commercial Asbestos Abatement in NJ; owing to the risks of the ailments mentioned above will augment at what time exposure is prolonged. How will you know if your insulation uses asbestos? Here are some things to watch out for:
It is imperative for you to know the correct date at what time the house or building you are living in is built. If it was built prior to the 1960's, there is a high probability that the insulation material is lining the roofs and walls.
Make sure if the insulation utilized in your dwelling or building is of the wobbly or batted type. These kinds of insulation matter will look life downy, greyish clumps of fibres and they are time and again found amid the rafters.
If your dwelling has a lot of old pipes, make sure if they are covered by way of a blanket-like material in the jostle joints and valves - these are padding materials that include asbestos. There are also asbestos padding materials that look similar to cardboard coverings - and this was especially trendy in steam heating pipes.
Treatment
If you think that the insulation materials in your dwelling or construction contain asbestos, you should treat them as nevertheless they in reality contain asbestos. This denotes avoiding contact or contact to them, and straight away calling a professional remover for Commercial Asbestos Removal in New Jersey to examine them. Asbestos can only be undoubtedly identified by making use of polarizing light microscopy.
You should not make an effort to eliminate asbestos insulation by yourself, even if you wear a little over your nose to make available protection from gasping the fibres. Licensed professionals for Commercial Asbestos Abatement in NJ draw on special masks and gloves to hold the asbestos materials, and they hold the technological knowledge to safely remove these materials from your house.
0 notes
Text
300+ TOP ONCOLOGY Objective Questions and Answers
ONCOLOGY Multiple Choice Questions :-
1. Cytotoxic T cells (CTL) are capable of recognizing:
A. Peptide antigens associated with major histocompatibility complex (MHC) molecules.
B. Membrane-bound antigens.
C. Cytoplasmic antigens.
D. Nuclear antigens.
E. All of the above.
Answer: E
2. Adoptive immunotherapy with lymphokine activated killer cells (LAK) and tumor infiltrate (TIL) cells are characterized by:
A. Nonspecific stimulation of effector cells.
B. Expansion ex vivo of large numbers of lymphocytes.
C. Infusion with interleukin 2 (IL-2).
D. Significant toxicity at high doses.
E. All of the above.
Answer: E
3. Previous clinical studies with cancer vaccines have:
A. Clearly demonstrated induction of tumor-specific immune response.
B. Repeatedly demonstrated clinical response to large tumor burden.
C. Not clearly demonstrated induction of tumor-specific immune response.
D. Not been performed to date.
Answer: C
4. Which of the following statements is/are true of the epidemiology and etiology of melanoma?
A. Most patients are diagnosed after age 60 years.
B. Skin color has no association with risk of melanoma.
C. Sun exposure is the only risk factor for melanoma.
D. The per capita incidence of melanoma is highest in Australia.
Answer: D
5. Which of the following variables best predicts prognosis for patients with a recent diagnosis of cutaneous melanoma and no clinical evidence of metastatic disease?
A. Breslow thickness.
B. Clark's level.
C. Ulceration.
D. Gender.
E. Celtic complexion.
Answer: A
6. A 38-year-old man presents with a melanoma on the skin of the right calf measuring 5 mm. in thickness. Several large nodes are palpable in the right inguinal region. Which of the following statements about the appropriate management of this clinical problem is false?
A. In the absence of systemic disease, the primary melanoma of the right calf should be excised with at least a 2-cm. margin.
B. Complete right inguinal node dissection should be performed if there is no evidence of systemic metastasis.
C. If further work-up reveals multiple lung metastases of melanoma, they should be excised as soon as possible.
D. Chemotherapy for melanoma is primarily palliative; so surgical therapy is preferred if there is no evidence of metastatic disease beyond the inguinal region.
E. If the nodes do not contain metastatic disease but are simply reactive, the chance of 5-year survival is 50% or less.
Answer: C
7. A 42-year-old woman presents with an 8 cm. × 6 cm. × 4 cm. mass in the posterior thigh. Incisional biopsy reveals a high-grade liposarcoma. Her management should include:
A. High thigh amputation.
B. Extracompartment excision with negative margins.
C. Complete excision with negative margins.
D. Adjuvant radiation therapy.
E. Adjuvant chemotherapy.
Answer: CD
8. Biologic features of adult soft tissue sarcomas include the following:
A. Mutations of p53 in metastatic liposarcoma.
B. A low (less than 1%) risk of metastasis for small, low-grade lesions.
C. Recurrent disease in at least 33% of patients.
D. Lymph node metastasis in less than 3% of patients.
E. Mutations of p53 in Li-Fraumeni syndrome.
Answer: BCDE
9. Which of the following statements describes an ideal tumor marker?
A. The ideal tumor marker should be tumor specific; that is, in the normal population or patients with benign diseases, false-positive test results are rare.
B. The ideal marker must have a low false-negative rate; that means that all patients with a particular type of cancer should test positive.
C. The circulating level of an ideal tumor marker should correlate directly with the amount of viable tumor and be a measure of the response to therapy.
D. The ideal tumor marker should act as a prognostic indicator.
E. All of the above.
Answer: E
10. A marker for the diagnosis of pancreatic cancer is:
A. CA 15-3.
B. CA 19-9.
C. Alphafetoprotein (AFP).
D. Carcinoembryonic antigen (CEA).
E. CYFRA 21-1.
Answer: B

ONCOLOGY MCQs
11. Which of the following tumors may cause elevated CEA levels?
A. Breast cancer.
B. Colorectal cancer.
C. Gastric cancer.
D. Lung cancer.
E. All of the above.
Answer: E
12. The presence of which marker is a significant poor prognosis variable for patients with breast cancer:
A. CEA.
B. C-erb B-2.
C. AFP.
D. Human chorionic gonadotropin (hCG).
E. RB-1.
Answer: B
13. The most useful circulating marker for patients with hepatocellular carcinoma is:
A. CA 50.
B. Levels of vitamin B 12.
C. CEA.
D. AFP.
E. hCG.
Answer: D
14. In patients with colorectal cancer the serum CEA level is a clinically useful measure for all reasons except:
A. Prognosis.
B. Detection of recurrence.
C. Guiding second-look operations.
D. Following treatment response.
E. Early diagnosis.
Answer: E
15. Which serum markers are useful in the management of patients with testicular cancer?
A. hCG.
B. AFP.
C. CA 15-3.
D. Two of the above.
E. None of the above.
Answer: D
16. Which tumor marker is useful for the management of patients with breast cancer?
A. CA 125.
B. Inhibin.
C. CA 19-9.
D. CA 15-3.
E. CEA.
Answer: D
17. A new marker that has possible utility in the management of patients with non–small-cell lung cancer (NSCLC) is:
A. Calcitonin.
B. Neuron-specific enolase.
C. CYFRA 21-1.
D. Glucagon.
E. Chromogranin A.
Answer: C
18. A circulating marker that may be useful in the management of patients with any neuroendocrine tumor is:
A. Chromogranin A.
B. Neuron-specific enolase.
C. hCG.
D. Two of the above.
E. None of the above.
Answer: D
19. A 65-year-old man is seen two years following right hemicolectomy for a Duke’s B-2 carcinoma of the cecum. Although asymptomatic, the CEA level has risen four-fold from a value obtained six months previously. Computed tomography reveals a single, 3 cm lesion in the right hepatic lobe. There is no evidence of extra-hepatic metastatic disease and the patient undergoes right hepatic lobectomy. Which of the following correctly represents the chance of overall 5 year survival?
a. 15%
b. 33%
c. 50%
d. 66%
Answer: b
20. The most serious long-term side effect of bleomycin therapy is which of the following?
a. Pulmonary fibrosis
b. Cataract formation
c. Cardiomyopathy
d. Aplastic anemia
Answer: a
21. Which of the following malignancies have declined in incidence in the United States over the past two decades?
a. Breast carcinoma
b. Gastric carcinoma
c. Endometrial carcinoma
d. Prostate cancer
e. Carcinoma of the uterine cervix
Answer: b, c, e
22. Oncogenes have been implicated in the development of a number of human neoplasms. Oncogene activation is believed to be required for oncogenesis. Which of the following potential mechanisms are relevant to these processes?
a. Chromosome translocation
b. DNA point mutation
c. Amplification
d. Gene deletion
Answer: a, b, c
23. A 45-year-old woman undergoes excision of a 1 cm breast mass. Histologic examination reveals invasive ductal carcinoma. Flow cytometric analysis is also performed which determines that a fraction of the tumor cells are “aneuploid”. The patient asks for an explanation of this term. Which of the following is/are correct?
a. The cells have a DNA content 1 times the baseline content
b. The cells have hyperchromatic nuclei
c. The cells have a DNA content 2 times the baseline content
d. The cells have squamous morphology
e. The cells have a DNA content not an even multiple of baseline content
Answer: e
24. A 45-year-old man with long-standing gastroesophageal reflux undergoes upper endoscopy that reveals patchy areas of epithelium resembling gastric mucosa extending 5 cm proximal to the esophagogastric junction. Biopsies are obtained. The pathologic report describes “Barrett’s epithelium”. Which of the following processes does this finding represent?
a. Cellular hyperplasia
b. Cellular hypertrophy
c. Metaplasia
d. Carcinoma in situ
Answer: c
25. Which of the following statements regarding the inherited form of retinoblastoma is/are correct?
a. Retinoblastoma results from amplification of the H-ras oncogene
b. Clinical disease results after chromosomal loss in a retinal cell after birth
c. Retinoblastoma results from the loss of a tumor suppressor gene
d. Clinical disease results from chromosomal translocation
Answer: b, c
ONCOLOGY Objective type Questions with Answers
26. Analysis of metastatic tumor cells has revealed expression of factors promoting tissue invasion. Which of the following is/are among such factors?
a. Collagenase
b. Plasminogen activator
c. Fibroblast growth factor
d. Interleukin-2
Answer: a, b
27. The most common complication that requires alteration of planned chemotherapy regimens is which of the following?
a. Pulmonary fibrosis
b. Gastrointestinal ulceration
c. Hematologic suppression
d. Hepatotoxicity
Answer: c
28. Resistance of tumors to multiple chemotherapeutic agents is often due to the MDR gene. This gene encodes a protein that acts by which of the following mechanisms?
a. As a transmembrane efflux pump for chemotherapeutic agents
b. As a DNA repair molecule
c. As an isoform of superoxide dismutase
d. As a membrane stabilizer
Answer: a
29. The high incidence of hepatitis B infection in Africa and parts of Asia is thought to be causally associated with increased incidence of which of the following malignancies?
a. Hepatocellular carcinoma
b. Esophageal cancer
c. Burkitt’s lymphoma
d. Gastric carcinoma
Answer: a
30. Workers exposed to asbestos are at increased risk for which of the following tumors?
a. Thoracic mesothelioma
b. Bladder carcinoma
c. Laryngeal carcinoma
d. Testicular carcinoma
e. Non-Hodgkin’s lymphoma
Answer: a, b, c
31. The Lynch Syndrome is also known as hereditary non-polyposis colorectal cancer. Which of the following is/are features of this syndrome?
a. Left sided colon cancers
b. Autosomal dominant inheritance
c. Multiple polyps beginning in adolescence
d. Multiple cutaneous nevi
Answer: b
32. A number of clinical factors have been noted to decrease sensitivity of tumors to the effects of ionizing radiation. Which of the following is most important in this regard?
a. Increased tissue vascularity
b. High tumor mitotic rate
c. Tissue hypoxia
d. Subcutaneous tumor location
Answer: c
33. Brachytherapy involves the delivery of radiation therapy locally via specially designed catheters placed in direct apposition to the treated tissue. The most common radioisotope used in this application is which of the following?
a. 125I
b. 14C
c. 3H
d. 34P
Answer: a
34. Patients that have acquired immunodeficiency syndrome are at increased risk for which of the following neoplasms?
a. Colorectal cancer
b. Meningioma
c. Kaposi’s sarcoma
d. Hepatocellular carcinoma
e. Esophageal carcinoma
Answer: c
35. DNA viruses have been implicated as etiologic agents in several human tumors. Evidence for a causative role exists for which of the following neoplasms?
a. Burkitt’s lymphoma
b. Testicular carcinoma
c. Cervical carcinoma
d. Osteogenci sarcoma
e. Esophageal carcinoma
Answer: a, c
36. When a chemotherapeutic agent is stated to have caused a partial response this implies what degree of reduction in measurable tumor volume?
a. 0–9%
b. 10–29%
c. 30–49%
d. 50–99%
Answer: d
37. Which of the following represent obstacles to the use of retroviruses in therapeutic gene transfer?
a. Viral receptors may not be present on target cell membranes
b. For integration, the host cell must undergo mitosis
c. Virus particles are labile
d. Viral purification is difficult
Answer: a, b, c, d
38. Which of the following statements regarding alpha-1-antitrypsin deficiency is/are correct?
a. Alpha-1-antitrypsin is a plasma elastase inhibitor
b. Most homozygous patients develop chronic obstructive pulmonary disease
c. The spleen is the primary site of alpha-1-antitrypsin synthesis
d. Intracellular accumulation of abnormal protein occurs in hepatocytes
Answer: a, b, d
39. Which of the following statements regarding retroviruses is/are correct?
a. The genetic material contained within a retrovirus is RNA
b. Inside the host cell the viral RNA is converted to single-stranded DNA
c. Proviral DNA is integrated into the host chromosome
d. Retroviruses can be used to transfect both replicating and non-replicating cells
Answer: a, c
40. Which of the following statements relating to adenoviruses is/are correct?
a. Adenoviral infection is a common cause of upper respiratory tract infection
b. Adenoviral genetic material consists of double-stranded DNA
c. Adenovirus can be produced in large quantity and easily purified
d. Adenoviral infection requires host cell mitosis
Answer: a, b, c
41. Which of the following statement relating to cystic fibrosis is/are correct?
a. Cystic fibrosis is inherited as an X chromosome-linked recessive trait
b. Cystic fibrosis is caused by a defective chloride channel
c. Cystic fibrosis is caused by defective acetylcholine receptors
d. Cystic fibrosis is inherited as an autosomal recessive trait
Answer: b, d
42. Hemophilia B has been treated in a pre-clinical model by gene transfer for which deficient clotting factor?
a. Factor II
b. Factor VII
c. Factor IX
d. Factor X
Answer: c
43. Familial hypercholesterolemia has been proposed as a disease to be treated by gene therapy. The molecular basis of familial hypercholesterolemia is which of the following?
a. Absence of hepatic low density lipoprotein receptors
b. Overproduction of high density lipoprotein
c. Absence of lipoprotein lipase
d. Overproduction of hepatic ornithine transcarbamylase
Answer: a
44. Antisense oligodeoxynucleotides have been proposed as agents for cancer-directed gene therapy. When delivered intracellularly, antisense molecules act to block which of the following?
a. Transcription
b. Translation
c. Post-translational processing
d. Ribosylation
Answer: b
45. Which of the following viruses is/are considered to be neurotropic?
a. Adenovirus
b. Herpes simplex virus
c. Retrovirus
d. Adeno-associated virus
Answer: b
ONCOLOGY Questions and Answers pdf Download
Read the full article
0 notes
Text
Dosimetric Correlates of Pulmonary Toxicity in Patients with Malignant Pleural Mesothelioma Receiving Radiation Therapy to the Intact Lungs
Publication date: Available online 15 January 2019
Source: Practical Radiation Oncology
Author(s): Marcher R. Thompson, Vishruta A. Dumane, Stanislav A. Lazarev, Yaseen Zia, Kenneth E. Rosenzweig
Abstract
Introduction
We aimed to determine dose-volume constraints that correlate with severe (grade ≥3) radiation pneumonitis (RP) in patients diagnosed with malignant pleural mesothelioma (MPM), treated using volumetric modulated arc therapy (VMAT).
Methods
Data from 40 patients with MPM who underwent pleurectomy decortication (P/D) and adjuvant radiation therapy at our institution between December 2010 and October 2016 were retrospectively analyzed. Dosimetric variables for the absolute volume as well as percentage volume of the ipsilateral lung, contralateral lung and heart were recorded. Events of RP were assessed using the Common Terminology Criteria for Toxicity and Adverse Events v4.0. Statistical analysis with Wilcoxon rank-sum, Spearman rank correlation and Receiver operating characteristic curves was computed using MATLAB V9.1, RV3.4 and SAS V9.4.
Results
Of 40 patients, 26 patients were male (65%). The median age at diagnosis was 66.5 years (range 44-84). The median prescription dose was 45 Gy (30 Gy – 54 Gy). Five patients (12.5%) had grade ≥ 3 RP. Incidence of grade ≥ 3 RP showed significant correlation (P < 0.05) with the absolute volume and percentage volume of the ipsilateral lung spared of 20 Gy and higher (55cc; 7%) as well as spared of 30 Gy and higher (200cc; 23%). Dosimetric variables of the contralateral lung, total lung and heart did not show correlation with incidence of grade ≥ 3 RP.
Conclusions
In our cohort, sparing ipsilateral lung of at least 55cc of 20Gy and 200cc of 30Gy correlated with a reduced incidence of severe (grade ≥3) radiation pneumonitis.
http://bit.ly/2APeJHc
0 notes
Text
Symptoms of Pleural Mesothelioma
Symptoms of Pleural Mesothelioma
In this article, we will discuss the Symptoms of Pleural Mesothelioma (Malignant). So, let’s get started.
Symptoms
Symptoms of Malignant Pleural Mesothelioma are non-specific and may mimic other respiratory disease. Common symptoms includes breathlessness, chest pain, weight loss and fatigue.Symptoms or clinical features may be due to Ipsilateral Pleural Involvement (Parietal/Visceral),…
View On WordPress
#Malignant Pleural Mesothelioma#Medicine#Oncology#Physiotherapy#Pleural Mesothelioma#pulmonary medicine#Pulmonology
0 notes
Photo


Stuff I learned today in my pulmonology rotation:
The arrows in this CT scan show air bronchograms, which are areas where you can see the bronchioles clearly (black lines, which are the bronchioles that have air in them) because there is hyperdensity (white areas) around them. These are abnormal and indicate pneumonia or pulmonary edema. We have a pt today who had a spontaneous pneumothorax, which was treated with a pigtail and then a chest tube. He also has pneumonia.
From Wikipedia:
An air bronchogram is defined as a pattern of air-filled bronchi on a background of airless lung.
In pulmonary consolidations and infiltrates, air bronchograms are most commonly caused by pneumonia or pulmonary edema (especially with alveolar edema).
Other potential causes of consolidations or infiltrates with air bronchograms are:
Pulmonary edema
Non-obstructive atelectasis
Severe interstitial lung disease
Pulmonary infarct
Pulmonary hemorrhage
Normal expiration
Ground glass opacities on CT are less dense than the hyperdensities you see in pneumonia; may be due to atypical bacteria.
From Wikipedia:
In radiology, ground glass opacity (GGO) is a nonspecific finding on radiographs and computed tomography (CT) scans. It consists of a hazy opacity that does not obscure the underlying bronchial structures or pulmonary vessels, and that indicates a partial filling of air spaces in the lungs by exudate or transudate, as well as interstitial thickening or partial collapse of lung alveoli.
The differential diagnosis of the many causes of GGO includes pulmonary edema, infections (including severe acute respiratory syndrome coronavirus 2 (COVID-19),[2] cytomegalovirus and Pneumocystis jirovecii pneumonia), various noninfectious interstitial lung diseases (such as hypersensitivity pneumonitis, Hamman-Rich syndrome), diffuse alveolar hemorrhage, cryptogenic organizing pneumonia, and pulmonary contusion.
Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.
It is often a complication of an existing chronic inflammatory disease such as rheumatoid arthritis, dermatomyositis, or it can be a side effect of certain medications such as amiodarone. COP was first described by Gary Epler in 1985.
The clinical features and radiological imaging resemble infectious pneumonia. However, diagnosis is suspected after there is no response to multiple antibiotics, and blood and sputum cultures are negative for organisms.
Hamman-Rich Syndrome = acute interstitial pneumonitis. Acute interstitial pneumonitis is a rare, severe lung disease that usually affects otherwise healthy individuals. There is no known cause or cure.
Acute interstitial pneumonitis is often categorized as both an interstitial lung disease and a form of acute respiratory distress syndrome (ARDS) but it is distinguished from the chronic forms of interstitial pneumonia such as idiopathic pulmonary fibrosis.
The most common symptoms of acute interstitial pneumonitis are highly productive cough with expectoration of thick mucus, fever, and difficulties breathing. These often occur over a period of one to two weeks before medical attention is sought. The presence of fluid means the person experiences a feeling similar to 'drowning'. Difficulties breathing can quickly progress to an inability to breathe without support (respiratory failure).
Acute interstitial pneumonitis typically progresses rapidly, with hospitalization and mechanical ventilation often required only days to weeks after initial symptoms of cough, fever, and difficulties breathing develop.
Rapid progression from initial symptoms to respiratory failure is a key feature. An x-ray that shows ARDS is necessary for diagnosis (fluid in the small air sacs (alveoli) in both lungs). In addition, a biopsy of the lung that shows organizing diffuse alveolar damage is required for diagnosis. Other diagnostic tests are useful in excluding other similar conditions, but history, x-ray, and biopsy are essential. These other tests may include basic blood work, blood cultures, and bronchoalveolar lavage.
The clinical picture is similar to ARDS, but AIP differs from ARDS in that the cause for AIP is not known.
The chest tube is connected to a Pleur-evac. The first chamber will bubble if suction is on; it actively sucks air out of the pleural space. It tells you in centimeters of water how much suction is being applied. The pt I saw today had a little over 20 cm of H2O of suction. Normally, the visceral and parietal pleura have a small amount of fluid between them. In PTX, that space has air in it. The chest tube and Pleur-evac get air out of that space. The second chamber of the Pleur-evac will bubble as long as air is still in the pleural space. That's what happened with the pt from today. So he will need to keep the chest tube in until his PTX is better and no more air is coming into the pleural space.
I asked the attending to explain the pathophysiology of clubbing. I recall learning that it can be associated with heartor lung disease, but I don't know why it happens. She said that in chronic respiratory failure, hypoxia triggers fibroblasts that cause nail clubbing, but nobody really knows why. The second image shows clubbing. From Wikipedia:
Nail clubbing, also known as digital clubbing or clubbing, is a deformity of the finger or toe nails associated with a number of diseases, mostly of the heart and lungs. When it occurs together with joint effusions, joint pains, and abnormal skin and bone growth it is known as hypertrophic osteoarthropathy.
Clubbing is associated with lung cancer, lung infections, interstitial lung disease, cystic fibrosis, or cardiovascular disease. Clubbing may also run in families, and occur unassociated with other medical problems.
Clubbing is associated with Lung disease:
Lung cancer, mainly non-small-cell (54% of all cases), not seen frequently in small-cell lung cancer ( Heart disease:
Any disease featuring chronic hypoxia
Congenital cyanotic heart disease (most common cardiac cause)
Subacute bacterial endocarditis
Atrial myxoma (benign tumor)
Tetralogy of Fallot
It can apparently also occur in GI disease.
Gastrointestinal and hepatobiliary:
Malabsorption
Crohn's disease and ulcerative colitis
Cirrhosis, especially in primary biliary cirrhosis
Hepatopulmonary syndrome, a complication of cirrhosis
Others:
Graves' disease (autoimmune hyperthyroidism) – in this case it is known as thyroid acropachy
Familial and hereditary clubbing and "pseudoclubbing" (people of African descent often have what appears to be clubbing)
Vascular anomalies of the affected arm such as an axillary artery aneurysm (in unilateral clubbing)
Nail clubbing is not specific to chronic obstructive pulmonary disease (COPD). Therefore, in patients with COPD and significant degrees of clubbing, a search for signs of bronchogenic carcinoma (or other causes of clubbing) might still be indicated.
A congenital form has also been recognized.
The exact cause for sporadic clubbing is unknown. Theories as to its cause include:
Vasodilation (i.e., distended blood vessels).
Secretion of growth factors (e.g., platelet-derived growth factor and hepatocyte growth factor) from the lungs.
Overproduction of prostaglandin E2 by other tissues.
Increased entry of megakaryocytes into the systemic circulation. Under normal circumstances in healthy individuals, megakaryocytes that arise from the bone marrow are trapped in the pulmonary capillary bed and broken down before they enter the systemic circulation. It is thought that in disorders where there is right-to-left shunting or lung malignancy, the megakaryocytes can bypass the breakdown within the pulmonary circulation and enter the systemic circulation. They are then trapped within the capillary beds within the extremities, such as the digits, and release platelet-derived growth factor (PDGF) and vascular endothelial growth factor (VEGF). PDGF and VEGF have growth promoting properties and cause connective tissue hypertrophy and capillary permeability. This seems to be the theory the attending was explaining.
#air bronchograms#air bronchogram#bronchogram#CT#imaging#ground glass#ground glass opacity#pulmonology#chest tube#clubbing
4 notes
·
View notes
Text
The Mesothelioma
[ad_1]
What is Mesothelioma?
Mesothelioma is a rare form of cancer in which malignant cells are found in the sac lining of the chest or abdomen. Especially people who are diagnosed with malignant mesothelioma in this work that breathing asbestos.
Mesothelioma Diagnosis
For the diagnosis of this disease, a physical examination is performed, followed by x-rays and pulmonary function tests…
View On WordPress
#alcohol addiction therapy#diagnosed with mesothelioma#drug programs in schools#health#pharmacist jobs in chicago
0 notes
Text
Have you been disabled due to an asbestos exposure at work?
Asbestos is a naturally occurring mineral that is toxic to us humans. Believe it or not, you may be inhaling small quantities right now as it can be found soil and rock and in small doses, it isn’t harmful. The minerals the put off asbestos are in demand due to their properties in a wide array of manufacturing and construction applications.
Until regulations on the use of asbestos came into play in the 1970’s, asbestos was widely used in everything from floors and ceilings in buildings and ships to brake pads and heating systems in vehicles. The military also used asbestos in its bombers and fighter planes adding additional risk to our fighting forces and putting the long-term health of our warriors at risk.
When handled, asbestos effective sheds fibers into the air which end up getting inhaled by nearby workers. Over time, these fibers built up and lead to serious illnesses. People who worked in the industrial sector (Mining, Shipbuilding, Construction and some Manufacturing) have been at higher risk to asbestos exposure and the ailments it causes.
Unfortunately, even though regulations put a stop to the use of asbestos in the 70’s there are still installations and older building that may have this toxic material present. Also unfortunate, the impact of asbestos exposure may not be evident for decades as these small inhaled fibers slowly damage the soft tissue of the lungs and do not necessarily show up as symptoms until much time has passed. Symptoms can include difficulty breathing, chest pain and coughing. Some of the serious and debilitating diseases that asbestos can cause are:
Mesothelioma – You’ve almost seen commercials on the television about this form of cancer that impact the cardio-pulmonary system. Mesothelioma is aggressive and ultimately impacts the core of the human body with difficulty breathing, fatigue, and constipation.
Asbestosis – This is less known about than mesothelioma and is a chronic condition that can mean permanent lung damage with coughing and shortness of breath as leading symptoms. In some cases, the impacted person’s finger or toenails may look extra wide or round.
Pleural Plaques – This is a thickening of the lining of the lung fiber and often can exist without symptoms.
Lung Cancer – Is cancer or growth of malignant cells in the lungs that come with chest pain and shortness of breath. Sufferers may first notice respiratory infections before cancer is found.
If you worked in the industrial sector or served in the military and feel you may be disabled due to asbestos exposure, get us on your team to protect you and your family.
Disability is a serious issue that can substantively impact your life. Insurance policies don’t make this any easier and they often require a lawyer just to make sense of them. The disability lawyers of Edelstein Martin & Nelson, LLP represent clients who have become disabled and need a partner in their fight against insurance providers. Our practice is exclusively focused on this critical area and we are the trusted subject matter experts in disability insurance law. We will study your policy and situation so that we can advise you on your best options. We are located in Philadelphia and serve clients, throughout the state of Pennsylvania and across the United States.
To arrange a free initial consultation with an experienced disability attorney in Philadelphia, PA, call 215-858-8440, toll free 866-532-2504 or contact our Philadelphia disability insurance law firm online.
The post Have you been disabled due to an asbestos exposure at work? appeared first on Philadelphia Disability Insurance Lawyer.
Have you been disabled due to an asbestos exposure at work? published first on https://personalinjuryattorneyphiladelphiablog.wordpress.com/
0 notes
Text
Have you been disabled due to an asbestos exposure at work?
Asbestos is a naturally occurring mineral that is toxic to us humans. Believe it or not, you may be inhaling small quantities right now as it can be found soil and rock and in small doses, it isn’t harmful. The minerals the put off asbestos are in demand due to their properties in a wide array of manufacturing and construction applications.
Until regulations on the use of asbestos came into play in the 1970’s, asbestos was widely used in everything from floors and ceilings in buildings and ships to brake pads and heating systems in vehicles. The military also used asbestos in its bombers and fighter planes adding additional risk to our fighting forces and putting the long-term health of our warriors at risk.
When handled, asbestos effective sheds fibers into the air which end up getting inhaled by nearby workers. Over time, these fibers built up and lead to serious illnesses. People who worked in the industrial sector (Mining, Shipbuilding, Construction and some Manufacturing) have been at higher risk to asbestos exposure and the ailments it causes.
Unfortunately, even though regulations put a stop to the use of asbestos in the 70’s there are still installations and older building that may have this toxic material present. Also unfortunate, the impact of asbestos exposure may not be evident for decades as these small inhaled fibers slowly damage the soft tissue of the lungs and do not necessarily show up as symptoms until much time has passed. Symptoms can include difficulty breathing, chest pain and coughing. Some of the serious and debilitating diseases that asbestos can cause are:
Mesothelioma – You’ve almost seen commercials on the television about this form of cancer that impact the cardio-pulmonary system. Mesothelioma is aggressive and ultimately impacts the core of the human body with difficulty breathing, fatigue, and constipation.
Asbestosis – This is less known about than mesothelioma and is a chronic condition that can mean permanent lung damage with coughing and shortness of breath as leading symptoms. In some cases, the impacted person’s finger or toenails may look extra wide or round.
Pleural Plaques – This is a thickening of the lining of the lung fiber and often can exist without symptoms.
Lung Cancer – Is cancer or growth of malignant cells in the lungs that come with chest pain and shortness of breath. Sufferers may first notice respiratory infections before cancer is found.
If you worked in the industrial sector or served in the military and feel you may be disabled due to asbestos exposure, get us on your team to protect you and your family.
Disability is a serious issue that can substantively impact your life. Insurance policies don’t make this any easier and they often require a lawyer just to make sense of them. The disability lawyers of Edelstein Martin & Nelson, LLP represent clients who have become disabled and need a partner in their fight against insurance providers. Our practice is exclusively focused on this critical area and we are the trusted subject matter experts in disability insurance law. We will study your policy and situation so that we can advise you on your best options. We are located in Philadelphia and serve clients, throughout the state of Pennsylvania and across the United States.
To arrange a free initial consultation with an experienced disability attorney in Philadelphia, PA, call 215-858-8440, toll free 866-532-2504 or contact our Philadelphia disability insurance law firm online.
The post Have you been disabled due to an asbestos exposure at work? appeared first on Philadelphia Disability Insurance Lawyer.
Have you been disabled due to an asbestos exposure at work? published first on http://personalinjuryattorneyphiladelph.tumblr.com/
0 notes
Text
300+ TOP THORACIC SURGERY Objective Questions and Answers
THORACIC SURGERY Multiple Choice Questions :-
1. The bronchial circulation:
A. Is the blood supply to the conducting airways.
B. Drains into a peribronchial venous network that may expand considerably with conditions such as bronchiectasis and chronic obstructive pulmonary disease.
C. Is an especially important consideration in pulmonary transplantation.
D. All of the above.
Answer: D
2. Clearance of mucus produced in the tracheobronchial tree in chronic bronchitis secondary to smoking may:
A. Be hampered by the fact that the amount of mucus is increased by the number of mucus-producing cells at the expense of ciliated cells.
B. Be slowed if patients have decreased lung volume and are therefore unable to generate a vigorous cough that would cause an inflammatory process.
C. Cause a decrease in diffusion capacity and associated hypoxemia.
D. All of the above.
Answer: A
3. The pulmonary circulation:
A. Is the only vascular system in which the veins do not have the same course as the arteries.
B. Has a direct connection of vein to adjacent lung tissue by connective tissue fibers, making the diameter of the tissue fibers dependent upon lung volume.
C. Supplies the metabolic needs of the alveoli.
D. All of the above.
Answer: C
4. Which of the following screening tests are important for preoperative evaluation of pulmonary function?
A. History and physical examination.
B. Room air arterial blood gases.
C. Chest film.
D. Vital capacity and forced expiratory volume in 1 second (FEV 1).
E. Cardiopulmonary exercise testing.
Answer: ABCDE
5. Carbon monoxide diffusion capacity (DLCO) has been shown to correlate with:
A. The thickness of the alveolar lining membrane.
B. The permeability of the erythrocyte to carbon dioxide.
C. Pulmonary emboli.
D. Total alveolar-capillary capacity.
Answer: ABCD
6. The closing volume is:
A. The volume remaining in the lung at the end of expiration below which alveolar collapse begins to occur, resulting in physiologic shunting.
B. Higher in young persons.
C. Not changed during surgery.
D. Relative to the oxygen content of mixed venous blood.
Answer: AC
7. The effect of high positive end-expiratory pressures (PEEP) on cardiac output is:
A. None.
B. Increased cardiac output.
C. Decreased cardiac output because of increased afterload to the left ventricle.
D. Decreased cardiac output because of decreased effective preload to the left ventricle.
Answer: D
8. Weaning patients from maximum ventilator support usually involves:
A. Weaning PEEP first, tidal volume second, and the fraction of inspired oxygen (FIO 2) third.
B. Weaning FIO 2 first, ventilator rate second, and PEEP third.
C. Weaning FIO2 first, PEEP second, and tidal volume third.
D. Weaning FIO 2 first, PEEP second, and ventilator rate third.
Answer: D
9. Which of the following statements about bronchoscopy is false?
A. The morbidity and mortality are approximately 0.2% and 0.08%, respectively.
B. The most common complications of bronchoscopy are related to premedication of patients.
C. Adjunctive cancer therapy such as laser treatment and brachytherapy may be administered via this route.
D. A chronic cough and unilateral wheezing are accepted indications for bronchoscopy.
E. Early postoperative bronchoscopy for atelectasis is contraindicated following pulmonary resection.
Answer: E
10. Flexible bronchoscopy is preferred over rigid bronchoscopy for all of the following except:
A. Patients with cervical spine injuries requiring intubation.
B. The evaluation of a smoke inhalation injury.
C. Transcarinal needle aspiration of an enlarged subcarinal lymph node.
D. The removal of a bronchus intermedius foreign body from an infant.
E. A cost-effective evaluation of mild hemoptysis.
Answer: D

THORACIC SURGERY Objective Questions
11. Which of the following approaches is/are currently acceptable for the management of spontaneous pneumothorax?
A. Chest tube replacement alone for the patient with a first episode.
B. Operation on presentation for any patient with a first episode.
C. Video-assisted thoracic surgery (VATS) bleb excision and pleurodesis for recurrent pneumothorax on the same side.
D. Thoracotomy with bleb excision and pleurodesis for unilateral recurrent pneumothorax.
E. Operation after a first episode in an airline pilot.
Answer: ACDE
12. For which patient(s) with a pulmonary infiltrate of uncertain cause would you favor VATS over open wedge excision?
A. An AIDS patient with a diffuse infiltrate who is ambulatory but requires supplemental oxygen. Bronchoalveolar lavage is negative.
B. A 64-year-old previously healthy man with increasing shortness of breath, a diffuse infiltrate, and restrictive lung disease as shown by pulmonary function studies.
C. A 74-year-old diabetic woman with a rapidly progressing process throughout the right lung who is ventilator- and pressor-dependent.
D. A 44-year-old man with fever, left-sided infiltrate, and shortness of breath.
E. A 79-year-old man on a ventilator for right lower and middle lobe pneumonia which has been culture negative.
Answer: ABD
13. Which of the following statements about the cause and prevention of postintubation tracheal stenosis are correct?
A. Postintubation airway stenosis can largely be avoided by providing assisted ventilation via endotracheal tube rather than tracheostomy tube.
B. Postintubation tracheal stenosis at the cuff level results, more or less equally, from low blood pressure, advanced age, steroids, high intracuff pressure, sensitivity to tube materials, gas sterilization elution products, and systemic disease.
C. In women and smaller men large endotracheal tubes can produce lesions of the glottis and subglottis that can progress to stenosis.
D. Stomal stenosis is due principally to cicatricial closure of large stomas resulting from removal of a disk or segment of tracheal wall during tracheostomy.
E. A large-volume tracheostomy tube cuff such as that now used on most available tubes can become a high-pressure cuff if filled beyond its resting maximal volume.
Answer: CE
14. Which of the following statements about the treatment of postintubation airway stenosis are correct?
A. Emergency management of airway obstruction due to stenosis at the level of a prior tracheal stoma is best accomplished by establishing a new tracheostomy in normal tracheal tissue just below the scar of the old stoma.
B. Radial lasering and dilatation usually leads to permanent resolution of postintubation tracheal stenosis.
C. Splinting of a cervical trachea with a silicone T-tube for 6 to 8 months generally leads to permanent resolution of stricture.
D. Postintubation tracheal stenosis that extends into the subglottic larynx is treated by resection of a cylindrical sleeve of stenotic airway and end-to-end reconstruction.
E. Acquired tracheoesophageal fistula due to intubation injury is corrected by surgical closure of the fistula concurrent with resection and reconstruction of the damaged trachea.
Answer: E
15. Which of the following statements are true?
A. Pyogenic lung abscess occurs most frequently in the lower lobe of the left lung.
B. Anaerobic bacteria are commonly present in pyogenic lung abscess.
C. Operation is usually required to eradicate a pyogenic lung abscess.
D. Penicillin is the treatment of choice for lung abscess.
Answer: BD
16. Amphotericin B is effective for the following lung infections:
A. Histoplasmosis.
B. North American blastomycosis.
C. Aspergillosis.
D. Mucormycosis.
E. Sporotrichosis.
Answer: ABD
17. The following statements are true.
A. A distinguishing roentgenographic appearance of lung abscess, the air-fluid level can be seen only on roentgenograms obtained in the upright or lateral decubitus position.
B. The fungus ball characteristic of aspergillosis can be seen roentgenographically in either the upright or recumbent position.
C. Actinomycosis and nocardiosis are both fungal diseases of the lung that respond to treatment with the newer azole antifungal agents.
D. The commonest fungal lung infection in the United States is due to Histoplasma capsulatum.
Answer: ABD
18. Pneumocystis pneumonia is an opportunistic infection caused by Pneumocystis carinii. Which of the following statements are true?
A. P. carinii is a fungus.
B. Pneumocystis pneumonia is the most common opportunistic infection in patients with AIDS.
C. The diagnosis of Pneumocystis pneumonia depends on the demonstration of P. carinii organisms in lung tissue.
D. There is no effective treatment for Pneumocystis pneumonia.
Answer: BC
19. Which of the following statements are true?
A. The pleural space does not extend into the neck.
B. Positive intrapleural pressures as high as 40 cm. H 2O and negative pressures as low as -40 cm. H 2O are possible.
C. The pleural cavities cannot absorb more than 500 ml. of fluid per day.
D. All pleural effusions are of clinical significance and should be investigated.
Answer: BD
20. Which of the following statements are true?
A. Chylothorax, or chyle in the pleural cavity, usually is not a serious condition.
B. Chyle is easily identified by its milky appearance, which looks like no other kind of pleural effusion.
C. The commonest causes of chylothorax are trauma and tumor.
D. The thoracic duct can be ligated with impunity.
Answer: CD
21. Which of these statements about pleural tumors is/are true?
A. The commonest type of pleural tumor is primary pleural mesothelioma.
B. Exposure to asbestos dust is causally related to the development of malignant mesothelioma.
C. Localized benign mesotheliomas are asymptomatic.
D. Complete pleurectomy for malignant mesothelioma usually results in cure.
Answer: B
22. Which of the following correctly describe a patient with spontaneous pneumothorax?
A. The patient is almost always elderly and debilitated.
B. An unsuspected primary or metastatic lung tumor may be present.
C. The administration of supplemental oxygen is of little benefit to the patient.
D. The patient should always be treated with an intercostal tube and closed pleural drainage.
E. Video-assisted thoracic surgery (VATS) should be considered for persistent air leak in patients with secondary spontaneous pneumothorax.
Answer: BE
23. Which of the following statements about spontaneous pneumothorax (PSP) is/are correct?
A. The risk of recurrence after resolution of the first episode of PSP or secondary spontaneous pneumothorax (SSP) is 35% to 45%.
B. Patients with PSP are typically tall, thin, young adult males with a history of smoking.
C. Secondary spontaneous pneumothorax is associated with family history in 10% of cases.
D. For bleb resection and pleurodesis thoracoscopic thoracotomy and open thoracotomy provide similar cure rates for patients with primary spontaneous pneumothorax.
E. Causes of secondary pneumothorax include trauma and iatrogenic needle puncture.
Answer: ABD
24. Which of the following are relative contraindications for surgical management of emphysema?
A. Rapidly progressive dyspnea.
B. Bullae occupying less than one third of a hemithorax on plain chest radiography.
C. Elevated room air PCO 2.
D. “Pink puffer” patients.
E. FEV 1 less than 35% of predicted value.
Answer: BCE
25. Which of the following treatments would be appropriate therapy for symptoms that persist on medical therapy and bronchiectasis involving, in order of decreasing severity, the left lower lobe, the right middle lobe, and the left upper lobe?
A. Left pneumonectomy.
B. Wedge resection of the left lower lobe.
C. Left lower lobectomy.
D. Simultaneous left lower lobectomy and right middle lobectomy.
Answer: C
26. Which of the following would not be acceptable sequences of preoperative studies in a patient being prepared for lingulectomy for bronchiectasis?
A. CT alone.
B. CT, bronchoscopy, bronchography.
C. Bronchoscopy alone.
D. Bronchoscopy, bronchography.
Answer: C
27. Which of the following statements about pulmonary mycobacterial infection is/are correct?
A. Worldwide, tuberculosis no longer represents a significant public health problem.
B. Mycobacterium tuberculosis is responsible for the majority of cases of pulmonary mycobacterial disease.
C. Mycobacterium kansasii pulmonary infection almost always requires surgical treatment.
D. Atypical mycobacteria are never primary pulmonary pathogens in humans.
Answer: B
28. Which of the following chemotherapeutic regimens are currently recommended for the treatment of pulmonary infection caused by M. tuberculosis?
A. Isoniazid, rifampin, pyrazinamide, and streptomycin for 24 months.
B. Isoniazid for 9 months with ethambutol for the first 3 months.
C. Isoniazid and rifampin for 6 months with pyrazinamide added for the first two months.
D. Isoniazid alternating with rifampin at 3-month intervals for 12 months.
E. Isoniazid and rifampin for 9 months.
Answer: CE
29. Which of the following are appropriate indications for pulmonary resection for mycobacterial disease?
A. Localized pulmonary disease caused by M. avium-intracellulare.
B. Advanced lobar tuberculous pneumonia with massive hilar lymphadenopathy and bronchial obstruction in a young child.
D. An asymptomatic tuberculous cavity greater than 12 cm. in diameter.
E. Massive hemoptysis from a right upper lobe cavity occurring during an appropriate course of chemotherapy for pulmonary tuberculosis in a sputum-negative patient.
Answer: AE
30. Which statements about squamous papillomatosis of the trachea is/are correct?
A. It is the most common type of benign tracheal tumor in adults.
B. It is the most common type of benign tracheal tumor in children.
C. Most are treated with segmental tracheal resection.
D. There is no risk of malignant degeneration.
E. It is associated with a herpesvirus.
Answer: A
31. Which of the following statements about pulmonary hamartomas is/are true?
A. Hamartomas are benign chondromas.
B. Most are located in the conducting airways.
C. Wedge resection is curative.
D. A lobectomy is necessary to obtain draining hilar lymph nodes.
E. Hemoptysis is common.
Answer: C
32. Which of the following statements about typical carcinoid tumors are true?
A. They make up the majority of bronchial adenomas.
B. They frequently have lymph node metastases.
C. The carcinoid syndrome is observed in 33%.
D. Overall survival at 5 years is 90%.
E. Overall survival at 5 years is 50%.
Answer: AD
33. Which is/are true of adenoid cystic carcinoma?
A. It is a common type of salivary gland tumor.
B. Another name is cylindroma.
C. Most patients are completely resected for cure.
D. Different histological types have different prognoses.
E. Tissue invasion is rare.
Answer: ABCD
34. A solitary pulmonary nodule is discovered in an asymptomatic 55-year-old smoker with no evidence of extrathoracic dissemination. The most appropriate management would be to:
A. Obtain serial chest films every 3 months to determine the growth potential of the nodule.
B. Perform transthoracic needle aspiration (TTNA) before considering pulmonary resection to confirm malignancy.
C. Conduct an extensive systematic evaluation to exclude the possibility that the nodule represents a metastatic lesion.
D. Proceed with pulmonary resection after ascertaining that the patient would tolerate removal of the requisite amount of lung.
E. Obtain baseline serum levels of carcinoembryonic antigen and p53.
Answer: D
35. After thoracotomy, pulmonary resection, and mediastinal lymph node dissection, a patient is determined to have a squamous cell carcinoma 2 cm. in diameter, located 1 cm. from the carina along the right mainstem bronchus. Three peribronchial lymph nodes are positive for cancer, and all other lymph node stations are negative. The correct stage, according to the TNM system, is:
A. T1N0M0 Stage I.
B. T1N1M0 Stage II.
C. T2N1M0 Stage II.
D. T3N1M0 Stage IIIa.
E. T2N3M0 Stage IIIb.
Answer: C
36. After complete resection of Stage I non-small cell lung cancer (NSCLC), the role of adjuvant therapy is best summarized thus as:
A. Postoperative radiation therapy improves disease-free survival.
B. Postoperative radiation therapy improves overall survival.
C. Postoperative chemotherapy improves disease-free survival.
D. Postoperative chemotherapy improves overall survival.
E. Adjuvant therapy is not indicated after complete resection of Stage I NSCLC.
Answer: E
37. Compared to segmentectomy or wedge resection, lobectomy for NSCLC is associated with:
A. Similar operative morbidity but higher operative mortality.
B. Similar operative mortality but higher operative morbidity.
C. More severe postoperative pulmonary dysfunction.
D. Lower incidence of locoregional recurrence.
E. Equivalent locoregional recurrence.
Answer: D
38. In contrast to NSCLC, small cell lung cancer (SCLC) is characterized by:
A. Greater response rate to chemotherapy.
B. Inability to achieve surgical cure.
C. Less frequent association with paraneoplastic syndromes at the time of diagnosis.
D. Lower likelihood of metastases present at the time of diagnosis.
E. Slower growth.
Answer: A
39. Which of the following statements about the diagnosis and staging of mesothelioma is/are correct?
A. Fluid obtained by thoracentesis is usually adequate for accurate diagnosis.
B. Open biopsy or thoracoscopy should be performed to obtain tissue for diagnosis.
C. Immunohistochemistry should be performed in all cases of suspected mesothelioma.
D. Chest CT and/or magnetic resonance imaging (MRI) are useful in the staging of mesothelioma.
E. Head CT and bone scans are useful in the staging of mesothelioma.
Answer: BCD
40. Which of the following statements about therapy for malignant pleural mesothelioma is/are correct?
A. The role of surgery is confined to biopsy for diagnosis and pleurodesis for palliation of effusion.
B. Extrapleural pneumonectomy involves resection en bloc of the lung, visceral and parietal pleura, pericardium, and diaphragm.
C. If a lesion is unresectable by extrapleural pneumonectomy, pleurectomy/decortication is contraindicated.
D. Neither surgery, chemotherapy, nor radiation therapy as a single therapy improves survival.
E. Multimodality therapy, combining surgery, chemotherapy, and radiation therapy may improve survival in select patients.
Answer: BDE
41. All of the following may be acceptable operative approaches to management of the thoracic outlet syndrome except:
A. Scalenectomy.
B. Excision of a cervical rib.
C. Thoracoplasty.
D. First rib resection.
E. Division of anomalous fibromuscular bands.
Answer: C
42. Initial conservative (nonsurgical) management of the thoracic outlet syndrome may include all of the following except:
A. Weight reduction.
B. Improvement of posture.
C. Exercises to strengthen the muscles of the shoulder girdle.
D. Pentoxifylline.
E. Avoiding hyperabduction.
Answer: D
43. Which of the following statements about pectus excavatum are correct?
A. It is the most common congenital malformation of the chest wall.
B. The most frequent presenting complaint is the cosmetic deformity.
C. The manubrium and first and second costal cartilages typically are involved in the deformity.
D. It may be associated with cardiac defects and other skeletal defects such as scoliosis.
E. Restrictive alterations in chest wall mechanics and abnormalities in pulmonary function tests have been documented.
Answer: ABDE
44. Surgical correction of pectus excavatum is characterized by which of the following?
A. Significant cosmetic improvement initially but a high incidence of recurrence of the defect on late follow-up.
B. An increase in exercise tolerance and respiratory reserve postoperatively.
C. Improvement in FEV 1, vital capacity, and total lung capacity.
D. Improvement in maximal ventilatory volume, total progressive exercise time, and maximal exercise capacity.
E. Prevention of the development of “thoracogenic scoliosis.”
Answer: BDE
45. Which of the following statements about the diagnosis of chest wall tumors is/are correct?
A. Pain is a common presenting symptom.
B. Firmness and fixation to underlying bone and muscle are important to note in the physical examination as aids to diagnosis.
C. In general, chest wall tumors are slow growing and produce symptoms late in their course.
D. CT is the most useful imaging study for making the diagnosis and for planning surgical resection of chest wall tumors.
E. Angiography should be performed routinely.
Answer: BCD
THORACIC SURGERY Objective type Questions with Answers
46. Which of the following statements about chest wall resection and reconstruction is/are correct?
A. Most tumors of soft tissue and bone require 4-cm. margins to be adequately resected.
B. At least one normal rib above and below the primary tumor should be included in the resection.
C. Techniques of chest wall reconstruction are directed at the prevention of paradoxical chest wall movement with respiration.
D. Soft tissue defects are most conveniently addressed by stretching the existing skin over the defect under tension.
E. Chest wall defects that are covered by the scapula require no special reconstructive procedures, even if the defects are quite large.
Answer: ABCE
47. Prolonged extracorporeal membrane oxygenation (ECMO):
A. Is highly successful in the treatment of severe respiratory failure in newborn infants.
B. Is contraindicated in adult respiratory distress syndrome (ARDS).
C. Causes hemolysis and renal failure.
D. Requires total systemic heparinization (activated clotting time longer than 500 seconds).
E. Is identical to heart/lung bypass for cardiac surgery.
Answer: A
48. Indications for ECMO include:
A. Newborn infants with pulmonary hypoplasia secondary to congenital diaphragmatic hernia.
B. Meconium aspiration syndrome in full-term babies (at least 35 weeks).
C. Children with pulmonary infection after bone marrow transplantation.
D. Adults with acute viral pneumonia.
E. Adults requiring mechanical ventilation and 100% oxygen for 2 weeks or longer.
Answer: BD
49. Venovenous ECMO:
A. Avoids major arterial access.
B. Provides cardiac and pulmonary support.
C. Can be accomplished via cannulation at separate venous sites or at a single venous site using a double-lumen catheter.
D. Provides greater venous drainage than venoarterial ECMO.
E. Maintains the normal pulsatile blood flow to the systemic circulation.
Answer: ACE
50. As compared with venovenous ECMO, venoarterial ECMO:
A. Requires cannulation of a major artery and vein.
B. Provides both cardiac and respiratory support.
C. Can be performed with less anticoagulation.
D. Usually maintains a normal pulse pressure.
Answer: AB
51. A 24-year-old male has new onset of chest pain. Chest films demonstrate a large anterosuperior mass. Appropriate evaluation should include:
A. CT of the chest.
B. Measurement of serum alpha-fetoprotein and beta–human chorionic gonadotropin.
C. A barium swallow.
D. A myelogram.
Answer: AB
52. Systemic syndromes frequently associated with mediastinal tumors include:
A. Myasthenia gravis.
B. Hypercalcemia.
C. Malignant hypertension.
D. Carcinoid syndrome.
Answer: ABC
53. A 36-year-old female developed dyspnea on exertion that has progressed over 3 months. Chest film reveals a left anterior mediastinal mass with evidence of elevated left hemidiaphragm. CT indicates probable invasion of the pericardium. Paratracheal or subcarinal adenopathy is not identified. Appropriate intervention in this patient would include:
A. A median sternotomy with radical resection of the tumor, sacrificing the left phrenic nerve and excising the involved pericardium.
B. A mediastinoscopy with biopsy.
C. A left anterolateral thoracotomy or median sternotomy with generous biopsy of the tumor.
D. Observation with repeat chest radiography in 3 months.
Answer: C
54. An 18-year-old male presents with a history of increasing shortness of breath that worsens in the recumbent position. On physical examination, the neck veins are noted to be distended, with facial plethora that is accentuated by lying the patient down. A 2.5-cm. left supraclavicular lymph node is palpable. Chest film reveals an extensive right anterosuperior mediastinal mass. Appropriate intervention may include:
A. An urgent biopsy of the mediastinal mass under general anesthesia with subsequent initiation of therapy.
B. CT.
C. Pulmonary function testing in the sitting and supine positions.
D. A biopsy of the right supraclavicular lymph node under general anesthesia.
E. A biopsy of the supraclavicular lymph node under local anesthesia.
Answer: BCE
55. A 42-year-old male who is scheduled to undergo elective knee surgery has a preoperative chest film that demonstrates a 5-cm. posterior mediastinal mass. The patient denies any neurologic symptoms and physical examination fails to elucidate any neurologic deficit. CT confirms the presence of a 5-cm. mediastinal mass in the left costovertebral gutter with minimal enlargement of the seventh thoracic foramen. Appropriate intervention includes:
A. Resection of the posterior mediastinal mass using a standard posterolateral incision.
B. A CT with myelography or magnetic resonance (MR) imaging.
C. Two-stage removal of the tumor, performing the resection of the thoracic component first with subsequent removal of the spinal column component at a later date.
D. One-stage removal of the dumb-bell tumor, excising the intraspinal component prior to resection of the thoracic component.
Answer: BD
56. True statements regarding patients with a mediastinal mass include:
A. Asymptomatic patients have a benign mass in over 75% of cases.
B. Symptomatic patients are more likely to have a malignant lesion than a benign lesion.
C. In a patient with a chest film demonstrating a mediastinal mass, a Tru-cut needle biopsy is a safe procedure.
D. Seminomas usually produce alpha-fetoprotein.
Answer: AB
57. Which of the following would be the least appropriate in the management of acute suppurative mediastinitis?
A. Wide débridement.
B. Irrigation under pressure.
C. Topical antibacterials.
D. Long-term systemic antibacterials.
E. Closure with muscle flaps.
Answer: D
58. Each of the following is appropriate for managing acute suppurative mediastinitis except:
A. Alloplastic material and skin flaps.
B. Rectus abdominis muscle flaps.
C. Omentum.
D. Pectoralis major muscle flaps.
E. Rigid internal fixation.
Answer: A
59. Clinical features suggestive of myasthenia gravis include all of the following except:
A. Proximal muscle weakness.
B. Diplopia.
C. Sensory deficits of the extremities.
D. Dysphagia.
Answer: C
60. The diagnosis of myasthenia gravis can be confirmed most reliably using:
A. Anti–acetylcholine receptor antibody titers.
B. The Tensilon test.
C. Electromyography (EMG).
D. Single-fiber EMG.
E. Physical examination.
Answer: D
61. All of the following statements are true about the pathogenesis of myasthenia gravis except:
A. The number of functional acetylcholine receptors at the motor end plate is reduced.
B. An autoimmune mechanism involving antibodies to the acetylcholine receptor has been proposed.
C. Complement system involvement has been demonstrated.
D. A nonspecific “thymitis” may initiate the autoimmune response.
E. Clinical improvement following thymectomy is correlated with decreased acetylcholine receptor antibody titers.
Answer: E
62. Which of the following statements about the relationship of the thymus and myasthenia gravis is/are true?
A. Thymic abnormalities are present in up to 80% of patients with myasthenia gravis.
B. Thymoma is present in up to 20% of patients with myasthenia gravis.
C. Myasthenia gravis will occur in up to 60% of patients with thymomas.
D. Myasthenia patients with thymoma respond more favorably to thymectomy.
E. Thymoma is the most common abnormality of the thymus in patients with myasthenia gravis.
Answer: ABC
63. Which of the following statements about the results of thymectomy for myasthenia gravis are true?
A. Patients with ocular symptoms experience clinical improvement in 90% of cases.
B. Clinical remission can be expected in 90% of cases.
C. The response rate to thymectomy for patients with generalized symptoms is 90%.
D. Patients with thymoma experience improvement in 75%.
E. Continued medical therapy is required in 75%.
Answer: C
64. All of the following are true of the treatment of myasthenia gravis except:
A. The transcervical approach to surgical thymectomy is less likely to benefit the patient with myasthenia gravis.
B. Corticosteroids result in improvement in 80% of patients.
C. Plasma exchange is associated with improvement in up to 90% of patients.
D. Medical therapy with Mestinon (pyridostigmine) is associated with remission in approximately 10% of patients.
E. Surgical thymectomy, regardless of the approach, is associated with improved remission and response rates as compared with medical therapy.
Answer: A
65. Which of the following is/are acceptable alternatives in the management of malignant pericardial effusion?
A. Pericardiocentesis.
B. Subxiphoid pericardiotomy (“pericardial window”).
C. Thoracotomy with pericardiectomy.
D. Instillation of tetracycline or bleomycin into the pericardial space.
E. Treatment of the underlying malignancy.
Answer: ABCDE
66. Which of the following statements about cardiac tamponade is/are correct?
A. At least 500 ml. of fluid must be present in the pericardium of an adult to cause symptoms of tamponade.
B. A drop in systemic blood pressure of greater than 20 mm. Hg during inspiration (pulsus paradoxus) is a finding specific to cardiac tamponade.
C. The vast majority of patients with cardiac tamponade demonstrate a low QRS voltage, nonspecific ST T-wave abnormalities, and electrical alternans (alternation of QRS amplitude) on the electrocardiogram.
D. In trauma victims with cardiac tamponade, the three components of “Beck's triad” (hypotension, elevated jugular venous pressure (JVP), and muffled heart sounds) are almost always present.
E. When the diagnosis is made, treatment must be instituted rapidly and may include pericardiocentesis, creation of a pericardial window, and identification and treatment of the underlying cause.
Answer: E
67. Which of the following statements about constrictive pericarditis is/are correct?
A. Most patients who develop constrictive pericarditis after cardiac operation present with symptoms within 6 months of the procedure.
B. Results of pericardiectomy for constrictive pericarditis are worse in patients who develop constriction after mediastinal irradiation.
C. Drainage of asymptomatic pericardial effusions arising from acute pericarditis is advised to prevent development of constrictive pericarditis.
D. If surgical treatment is planned for constrictive pericarditis it should involve total or complete pericardiectomy.
E. Echocardiography can usually make the diagnosis by imaging a thickened pericardium.
Answer: BD
68. The relationship between small-cell and non-small cell lung cancers can be described by the following:
a. They differ by histology, clinical behavior and cell of origin
b. Of all lung cancers, approximately 80% are non-small cell and 20% are small cell
c. Both cell types are predictably responsive to chemotherapy
d. The International Staging System can be applied to both tumor types
e. The majority of non-small cell cancer patients vs. the minority of small cell cancer patients are candidates for pulmonary resection
Answer: b
69. A 62-year-old male smoker presents with right anterior chest pain. There is a 3 cm mass attached to the chest wall with radiographic evidence of rib erosion and positive cytology for non-small cell carcinoma. Which of the follow is/are true:
a. The patient is inoperable due to tumor size and chest wall involvement
b. Radiation therapy is the preferred initial treatment
c. Operative resection should be performed with en bloc removal of the tumor and adjacent chest wall as well as a mediastinal lymph node resection
d. Positive mediastinal nodes will have little effect on survival
e. The patient would be classified Stage IIIa
Answer: c, e
70. For the patient in the pervious question to become an operative candidate which of the following must be met?
a. Extrathoracic metastases must be able to be controlled by another modality, e.g. radiotherapy
b. Tumor doubling time must exceed 40 days
c. If there is recurrence at the primary site, it must be treated before the metastatic disease
d. Even if effective systemic therapy is available, resection of metastases is preferred
e. If pulmonary reserve is marginal, resection of the maximal number of metastatic foci should be performed
Answer: c
71. Biopsy of the lesion in the previous question is reported as “bronchial carcinoid with no signs of atypia.” Which of the follow is/are true?
a. Sleeve resection of the bronchus would be appropriate
b. Lymph node biopsy at time of resection is unnecessary
c. Associated carcinoid syndrome is very unlikely
d. If carcinoid syndrome were found in a tumor this size, hepatic metastases would be likely
e. When bronchial carcinoid syndrome occurs, right-sided cardiac valves are affected
Answer: a, c, d
72. In the evaluation and preparation of a 55-year-old smoker for resection of a 3 cm pulmonary adenocarcinoma, the following is/are true:
a. Preoperative cessation of smoking does not reduce postoperative pulmonary complications
b. Resting PaCO2 is of more value than PaO2
c. FEV1 is of more value than measured vital capacity
d. Diffusion capacity should be measured routinely
e. V/Q lung scan is useful when pulmonary reserve is marginal
Answer: b, c, e
73. Following resection of a T1N1 squamous cell cancer in a 47-year-old male, the following is/are true:
a. There is a higher risk of local recurrence than with any other histologic type of non-small cell cancer
b. The greatest risk to the patient is a distant metastasis
c. Of all metastatic sites, liver is most likely
d. If the patient survives five years, there is a greater risk of a new lung cancer than recurrence
e. To improve survival, the patient should be considered for adjuvant chemotherapy
Answer: a, b, d
74. A 42-year-old woman with hemoptysis is seen to have a 2 cm mulberry appearing polypoid lesion in the left mainstem bronchus suspicious for bronchial adenoma. The differential diagnosis includes which of the following:
a. Mucoepidermoid carcinoma
b. Plasma cell granuloma
c. Carcinoid tumor
d. Adenoid cystic carcinoma
e. Mucous gland adenoma
Answer: all of the above
75. A 42-year-old man has a solitary “coin lesion” 2 cm in diameter in the area of the right upper lobe on a routine chest radiograph. Which of the following is/are true?
a. A previous radiograph from five years prior showing the lesion to be 1.2 cm in diameter indicates malignancy
b. If a CT scan shows mediastinal adenopathy, mediastinoscopy is preferable to thoracotomy
c. In the absence of previous radiographs, the lesion should be followed by serial films at 6 month intervals
d. Calcification in a concentric or “popcorn” configuration denotes a benign lesion
e. Needle aspiration showing “chronic inflammatory cells” denotes a benign lesion
Answer: b, d
76. A 2 cm peripheral squamous cell carcinoma in the lung of a 60-year-old male with a pleural effusion positive for malignant cells would be classified as:
a. T1N0M1
b. T3N0M0
c. T3N0M1
d. T4N0M0
e. T4N0M1
Answer: d, e
77. A 53-year-old woman who had a malignant tumor removed 2 years ago presents with a solitary lung nodule 1.5 cm in diameter. The following is/are true:
a. If the primary tumor originated in the breast, the lesion is most likely to represent a new primary lung cancer.
b. If the primary tumor was melanoma, the lesion is most likely to be metastatic
c. If the remainder of the lung fields are clear, a CT scan is unnecessary
d. If the primary tumor was in the GI tract, there is very little chance that the lesion is a new primary lung cancer
e. Fine needle aspiration should always be performed prior to resection of the lung lesion
Answer: a, b
78. A 61-year-old male presents with a painful mass 3.5 cm in diameter below the clavicle and attached to the chest wall. The following is/are true:
a. A CT scan is the best study to determine rib destruction
b. The lesion should be removed enbloc without biopsy to minimize the chances for local recurrence
c. The chances are approximately 40% that the lesion is metastatic
d. If it is metastatic, the most likely primary tumor is in the lung or pancreas
e. Fortunately, less than 50% of chest wall tumors are malignant
Answer: c
79. Concerning the sternum, the following is/are true:
a. The xiphoid process is the anterior border of the thoracic outlet
b. Gladiolus is the body of the sternum
c. The angle of Louis is at the level of the 2nd costal cartilage
d. The 11th rib is attached via costal cartilage to the xiphoid
e. The sterno-manubrial junction is at the level of T4 posteriorly
Answer: a, b, c, e
80. A 22-year-old woman recovering from a traumatic head injury is noted to have bright red bleeding when her tracheostomy is suctioned. The following is/are true statement(s):
a. Antibiotics should be administered to treat the bronchitis
b. Deflation of the tracheal tube cuff is a useful diagnostic maneuver
c. If massive bleeding occurs, a finger should be used to compress the innominate artery against the sternum
d. Operative treatment of a tracheoinnominate fistula includes resection and prosthetic replacement of the innominate artery
e. Tracheal resection is usually required for a tracheoinnominate fistula to prevent recurrence
Answer: b, c
81. A 52-year-old alcoholic with fever and a cough productive of purulent sputum is found to have the opacity on chest film as shown (Fig. 62-15). The following is/are true statement(s):
a. The findings suggest a parapneumonic empyema
b. If pus is found on aspiration of the pleural space, a chest tube should be placed
c. If pus is found on aspiration, bronchoscopy is a necessary part of the patient’s evaluation
d. In this situation, rib resection for drainage is preferred to a large-bore chest tube
e. Decortication of the lung should be considered if the lung fails to expand within 4 weeks
Answer: a, b, c
82. The lesion shown (Fig. 62-6) was found on a 32-year-old male on a routine chest film required for his employment. Which of the following is/are true?
a. The stippled calcification and intact cortex of the rib are characteristic of osteochondroma
b. The stippled calcification is characteristic of osteogenic sarcoma
c. If the lesion is osteogenic sarcoma, the optimal treatment is resection and radiation therapy
d. If the lesion is an osteochondroma, it need not be resected in this age group
e. The radiographic picture is typical for Ewing sarcoma
Answer: a
83. To resect a chondrosarcoma of the chest wall in a 42-year-old man, ribs 2–4 were removed, leaving a defect 8 x 8 cm. For reconstruction, the following is/are true:
a. If this were to be posterior, beneath the scapula, reconstruction would not be required
b. If this defect is anterior, the primary benefit of reconstruction is an improved cosmetic result
c. Whenever chest wall reconstruction is considered, it should be delayed 6–12 months to allow detection of recurrent tumor
d. If Marlex is used for reconstruction, no wound drainage tube is necessary
e. If PTFE is used for reconstruction, both pleural and wound tubes should be used
Answer: a, d, e
84. An upright chest film of a cachectic, homeless 47-year-old woman shows blunting of the right costophrenic angle. The following is/are true:
a. A lateral decubitus film should be obtained to confirm the presence of fluid rather than a CT scan
b. Tuberculous effusion can readily be identified by stain and culture of aspirated fluid
c. A pleural fluid glucose level lower than in the serum is diagnostic of empyema
d. Bloody pleural effusion in this patient is diagnostic of an underlying malignancy
e. Pleural fluid cytology report of lumphoma should be viewed with skepticism
Answer: a, e
85. The pectoralis major muscle is available and innervated by the medial and lateral pectoral nerves so named because it describes their relationship to the pectoralis minor
a. The serratus anterior muscle is available since its absence has no functional significance
b. There is no serratus posterior muscle
c. The latissimus dorsi muscle is available and supplied by the thoracodorsal artery
d. The latissimus dorsi is innervated by the thoracodorsal nerve with fibers from C6, C7 and C8
Answer: d, e
86. A 38-year-old man presents with facial and upper extremity edema, venous distention in the neck and arms and a cyanotic appearance. The following is/are true statement(s):
a. The most likely cause of the problem is mediastinal granulomatous disease
b. A venogram should be obtained to confirm the diagnosis
c. Mediastinoscopy for diagnosis is contraindicated
d. If a malignancy is identified, resection is indicated for palliation
e. If the etiology is benign disease, gradual improvement without operation is to be expected
Answer: e
87. A 39-year-old woman with hypertension and radicular chest wall pain was found to have the lesion seen on chest radiograph (Fig. 63-23). The following is/are true statement(s):
a. The location of the lesion suggests a teratoma
b. High urinary vanillylmandelic acid levels would indicate that the lesion is a paraganglioma
c. If the lesion was seen on a film 5 years earlier, resection would not be indicated
d. A neurosurgical consultation should be obtained
e. Vasoactive intestinal polypeptide level elevation suggests a ganglioneuroma
Answer: d, e
THORACIC SURGERY Questions and Answers pdf Download
Read the full article
0 notes
Text
Have you been disabled due to an asbestos exposure at work?
Asbestos is a naturally occurring mineral that is toxic to us humans. Believe it or not, you may be inhaling small quantities right now as it can be found soil and rock and in small doses, it isn’t harmful. The minerals the put off asbestos are in demand due to their properties in a wide array of manufacturing and construction applications.
Until regulations on the use of asbestos came into play in the 1970’s, asbestos was widely used in everything from floors and ceilings in buildings and ships to brake pads and heating systems in vehicles. The military also used asbestos in its bombers and fighter planes adding additional risk to our fighting forces and putting the long-term health of our warriors at risk.
When handled, asbestos effective sheds fibers into the air which end up getting inhaled by nearby workers. Over time, these fibers built up and lead to serious illnesses. People who worked in the industrial sector (Mining, Shipbuilding, Construction and some Manufacturing) have been at higher risk to asbestos exposure and the ailments it causes.
Unfortunately, even though regulations put a stop to the use of asbestos in the 70’s there are still installations and older building that may have this toxic material present. Also unfortunate, the impact of asbestos exposure may not be evident for decades as these small inhaled fibers slowly damage the soft tissue of the lungs and do not necessarily show up as symptoms until much time has passed. Symptoms can include difficulty breathing, chest pain and coughing. Some of the serious and debilitating diseases that asbestos can cause are:
Mesothelioma – You’ve almost seen commercials on the television about this form of cancer that impact the cardio-pulmonary system. Mesothelioma is aggressive and ultimately impacts the core of the human body with difficulty breathing, fatigue, and constipation.
Asbestosis – This is less known about than mesothelioma and is a chronic condition that can mean permanent lung damage with coughing and shortness of breath as leading symptoms. In some cases, the impacted person’s finger or toenails may look extra wide or round.
Pleural Plaques – This is a thickening of the lining of the lung fiber and often can exist without symptoms.
Lung Cancer – Is cancer or growth of malignant cells in the lungs that come with chest pain and shortness of breath. Sufferers may first notice respiratory infections before cancer is found.
If you worked in the industrial sector or served in the military and feel you may be disabled due to asbestos exposure, get us on your team to protect you and your family.
Disability is a serious issue that can substantively impact your life. Insurance policies don’t make this any easier and they often require a lawyer just to make sense of them. The disability lawyers of Edelstein Martin & Nelson, LLP represent clients who have become disabled and need a partner in their fight against insurance providers. Our practice is exclusively focused on this critical area and we are the trusted subject matter experts in disability insurance law. We will study your policy and situation so that we can advise you on your best options. We are located in Philadelphia and serve clients, throughout the state of Pennsylvania and across the United States.
To arrange a free initial consultation with an experienced disability attorney in Philadelphia, PA, call 215-858-8440, toll free 866-532-2504 or contact our Philadelphia disability insurance law firm online.
The post Have you been disabled due to an asbestos exposure at work? appeared first on Philadelphia Disability Insurance Lawyer.
0 notes
Photo

Social Security Disability Expedites Compassionate Allowances Conditions
http://socialsecuritydisabilityandyou.com/blog/
Released on Tuesday, September 5, 2017
Social Security Disability expedites Compassionate Allowances with a claims. But you must have one of the Compassionate Allowances Conditions below. Also, I have medical documents and test results to prove you one of the Compassionate Allowances Conditions.
However, if you have an attorney, inform him or her about the Compassionate Allowances Conditions. Yet, show you attorney or representative the article and list of Compassionate Allowances.
Compassionate Allowances Conditions
CAL Conditions (A – B)
Acute Leukemia
Adrenal Cancer - with distant metastases or inoperable, unresectable or recurrent
Adult Non-Hodgkin Lymphoma
Adult Onset Huntington Disease
Aicardi-Goutieres Syndrome
Alexander Disease (ALX) - Neonatal and Infantile
Allan-Herndon-Dudley Syndrome
Alobar Holoprosencephaly
Alpers Disease
Alpha Mannosidosis - Type II and III
ALS/Parkinsonism Dementia Complex
Alstrom Syndrome
Alveolar Soft Part Sarcoma
Amegakaryocytic Thrombocytopenia
Amyotrophic Lateral Sclerosis (ALS)
Anaplastic Adrenal Cancer - Adult with distant metastases or inoperable, unresectable or recurrent
Angelman Syndrome
Angiosarcoma
Aortic Atresia
Aplastic Anemia
Astrocytoma - Grade III and IV
Ataxia Telangiectasia
Atypical Teratoid/Rhabdoid Tumor
Batten Disease
Beta Thalassemia Major
Bilateral Optic Atrophy- Infantile
Bilateral Retinoblastoma
Bladder Cancer - with distant metastases or inoperable or unresectable
Breast Cancer - with distant metastases or inoperable or unresectable
CAL Conditions (C – D)
Canavan Disease (CD)
CACH--Vanishing White Matter Disease-Infantile and Childhood Onset Forms (Effective 9/16/2017)
Carcinoma of Unknown Primary Site
Cardiac Amyloidosis- AL Type
Caudal Regression Syndrome - Types III and IV
Cerebro Oculo Facio Skeletal (COFS) Syndrome
Cerebrotendinous Xanthomatosis
Child Lymphoblastic Lymphoma
Child Lymphoma
Child Neuroblastoma - with distant metastases or recurrent
Chondrosarcoma - with multimodal therapy
Chronic Idiopathic Intestinal Pseudo Obstruction
Chronic Myelogenous Leukemia (CML) - Blast Phase
Coffin-Lowry Syndrome Congenital Lymphedema
Congenital Myotonic Dystrophy (Effective 9/16/2017)
Cornelia de Lange Syndrome - Classic Form
Corticobasal Degeneration
Creutzfeldt-Jakob Disease (CJD) – Adult
Cri du Chat Syndrome
Degos Disease - Systemic
DeSanctis Cacchione Syndrome
Dravet Syndrome
CAL Conditions (E – H)
Early-Onset Alzheimer’s Disease
Edwards Syndrome (Trisomy 18)
Eisenmenger Syndrome
Endometrial Stromal Sarcoma
Endomyocardial Fibrosis
Ependymoblastoma (Child Brain Cancer)
Erdheim Chester Disease
Esophageal Cancer
Esthesioneuroblastoma
Ewing Sarcoma
Farber Disease (FD) – Infantile
Fatal Familial Insomnia
Fibrodysplasia Ossificans Progressiva
Follicular Dendritic Cell Sarcoma - metastatic or recurrent
Friedreichs Ataxia (FRDA)
Frontotemporal Dementia (FTD), Picks Disease -Type A – Adult
Fryns Syndrome
Fucosidosis - Type 1
Fukuyama Congenital Muscular Dystrophy
Fulminant Giant Cell Myocarditis
Galactosialidosis - Early and Late Infantile Types
Gallbladder Cancer
Gaucher Disease (GD) - Type 2
Giant Axonal Neuropathy
Glioblastoma Multiforme (Brain Cancer)
Glioma Grade III and IV
Glutaric Acidemia - Type II
Head and Neck Cancers - with distant metastasis or inoperable or unresectable
Heart Transplant Graft Failure
Heart Transplant Wait List - 1A/1B
Hemophagocytic Lymphohistiocytosis (HLH) - Familial Type
Hepatoblastoma
Hepatopulmonary Syndrome
Hepatorenal Syndrome
Histiocytosis Syndromes
Hoyeaal-Hreidarsson Syndrome
Hutchinson-Gilford Progeria Syndrome
Hydranencephaly
Hypocomplementemic Urticarial Vasculitis Syndrome
Hypophosphatasia Perinatal (Lethal) and Infantile Onset Types
Hypoplastic Left Heart Syndrome
CAL Conditions (I – M)
I Cell Disease
Idiopathic Pulmonary Fibrosis
Infantile Free Sialic Acid Storage Disease
Infantile Neuroaxonal Dystrophy (INAD)
Infantile Neuronal Ceroid Lipofuscinoses
Inflammatory Breast Cancer (IBC)
Intracranial Hemangiopericytoma
Jervell and Lange-Nielsen Syndrome
Joubert Syndrome
Junctional Epidermolysis Bullosa - Lethal Type
Juvenile Onset Huntington Disease
Kidney Cancer - inoperable or unresectable
Kleefstra Syndrome (Effective 9/16/2017)
Krabbe Disease (KD) – Infantile
Kufs Disease - Type A and B
Large Intestine Cancer - with distant metastasis or inoperable, unresectable or recurrent>
Late Infantile Neuronal Ceroid Lipofuscinoses
Leigh’s Disease
Leiomyosarcoma
Leptomeningeal Carcinomatosis
Lesch-Nyhan Syndrome (LNS)
Lewy Body Dementia
Liposarcoma - metastatic or recurrent
Lissencephaly
Liver Cancer
Lowe Syndrome
Lymphomatoid Granulomatosis - Grade III
Malignant Brain Stem Gliomas – Childhood
Malignant Ectomesenchymoma
Malignant Gastrointestinal Stromal Tumor
Malignant Germ Cell Tumor
Malignant Multiple Sclerosis
Malignant Renal Rhabdoid Tumor
Mantle Cell Lymphoma (MCL)
Maple Syrup Urine Disease
Marshall-Smith Syndrome
Mastocytosis - Type IV
MECP2 Duplication Syndrome
Medulloblastoma - with metastases
Menkes Disease - Classic or Infantile Onset Form
Merkel Cell Carcinoma - with metastases
Merosin Deficient Congenital Muscular Dystrophy
Metachromatic Leukodystrophy (MLD) - Late Infantile
Mitral Valve Atresia
Mixed Dementias
MPS I, formerly known as Hurler Syndrome
MPS II, formerly known as Hunter Syndrome
MPS III, formerly known as Sanfilippo Syndrome
Mucosal Malignant Melanoma
Multicentric Castleman Disease
Multiple System Atrophy
Myoclonic Epilepsy with Ragged Red Fibers Syndrome
CAL Conditions (N – R
Neonatal Adrenoleukodystrophy
Nephrogenic Systemic Fibrosis
Neurodegeneration with Brain Iron Accumulation - Types 1 and 2
NFU-1 Mitochondrial Disease
Niemann-Pick Disease (NPD) - Type A
Niemann-Pick Disease-Type C
Nonketotic Hyperglycinemia
Non-Small Cell Lung Cancer
Obliterative Bronchiolitis
Ohtahara Syndrome
Oligodendroglioma Brain Cancer- Grade III
Ornithine Transcarbamylase (OTC) Deficiency
Orthochromatic Leukodystrophy with Pigmented Glia
Osteogenesis Imperfecta (OI) - Type II
Osteosarcoma, formerly known as Bone Cancer - with distant metastases or inoperable or unresectable
Ovarian Cancer – with distant metastases or inoperable or unresectable
Pallister-Killian Syndrome
Pancreatic Cancer
Paraneoplastic Pemphigus
Patau Syndrome (Trisomy 13)
Pearson Syndrome
Pelizaeus-Merzbacher Disease-Classic Form
Pelizaeus-Merzbacher Disease-Connatal Form
Peripheral Nerve Cancer - metastatic or recurrent
Peritoneal Mesothelioma
Peritoneal Mucinous Carcinomatosis
Perry Syndrome
Phelan-McDermid Syndrome
Pleural Mesothelioma
Pompe Disease – Infantile
Primary Central Nervous System Lymphoma
Primary Effusion Lymphoma
Primary Progressive Aphasia
Progressive Bulbar Palsy
Progressive Multifocal Leukoencephalopathy
Progressive Supranuclear Palsy
Prostate Cancer - Hormone Refractory Disease – or with visceral metastases
Pulmonary Atresia
Pulmonary Kaposi Sarcoma
Retinopathy of Prematurity - Stage V
Rett (RTT) Syndrome
Revesz Syndrome
Rhabdomyosarcoma
Rhizomelic Chondrodysplasia Punctata
Roberts Syndrome
CAL Conditions (S – Z)
Salivary Cancers
Sandhoff Disease
Schindler Disease - Type 1
Seckel Syndrome
Severe Combined Immunodeficiency - Childhood
Single Ventricle
Sinonasal Cancer
Sjogren-Larsson Syndrome
Skin Malignant Melanoma with Metastases
Small Cell Cancer (Large Intestine, Prostate or Thymus)
Small Cell Cancer of the Female Genital Tract
Small Cell Lung Cancer
Small Intestine Cancer - with distant metastases or inoperable, unresectable or recurrent
Smith Lemli Opitz Syndrome
Soft Tissue Sarcoma - with distant metastases or recurrent
Spinal Muscular Atrophy (SMA) - Types 0 and 1
Spinal Nerve Root Cancer-metastatic or recurrent
Spinocerebellar Ataxia
Stiff Person Syndrome
Stomach Cancer - with distant metastases or inoperable, unresectable or recurrent
Subacute Sclerosing Panencephalitis
Tabes Dorsalis
Tay Sachs Disease - Infantile Type
Thanatophoric Dysplasia - Type 1
Thyroid Cancer
Transplant Coronary Artery Vasculopathy
Tricuspid Atresia
Ullrich Congenital Muscular Dystrophy
Ureter Cancer - with distant metastases or inoperable, unresectable or recurrent
Usher Syndrome - Type I
Ventricular Assist Device Recipient - Left, Right, or Biventricular
Walker Warburg Syndrome
Wolf-Hirschhorn Syndrome
Wolman Disease
X-Linked Lymphoproliferative Disease
X-Linked Myotubular Myopathy
Xerodema Pigmentosum
Zellweger Syndrome
“The Practical Guide to Social Security Disability Benefits”
Is your Social Security Disability case at standstill? Do you want your Social Security Disability case to start moving again? Then my self-help digital eBook “The Practical Guide to Social Security Disability Benefits” for $6.99 can help you. Go to http://socialsecuritydisabilityandyou.com/ and buy the book today.
After you purchase the book, you will get 1 free hour of Social Security Disability Consultation. Please contact me at http://socialsecuritydisabilityandyou.com/contact/
Or on Facebook at https://www.facebook.com/SSDandYou/
#ssdandyou,#disabilityhelp,#ssdiappeal,#supplementalsecurityincome,#socialsecuritydisability,#socialsecuritydisabilitybenefits,
/
0 notes