#developed a chronic illness including brain problems a heart condition and asthma
Text
Infectious Diseases That Are Emerging
New infectious illnesses are brought about by a variety of circumstances, including changes in the social and environmental milieu. Climate change, globalization, and rural-to-urban migration are a few examples of these shifts.
Most frequently, these modifications are linked to infections from the animal kingdom, some of which have evolved to infect people. In other cases, a microbial genome mutation or genetic reassortment produces a new agent that may infect humans.
A respiratory disease called influenza, which can be mild or severe, might get worse for people who already have certain medical issues. Infants, expectant mothers, and adults who have asthma or other chronic medical conditions are particularly at risk.
When someone coughs, sneezes, or chats, tiny droplets of the virus are released into the air and readily pass from one person to another. People close may subsequently receive these droplets in their mouths, noses, or eyes. The ciliated epithelial cells that border the nose, throat, and lungs are invaded by influenza viruses after they have entered the body. After that, they target these cells, inflaming and harming them.
The virus that causes chikungunya is transmitted by the bite of an infected mosquito. Joint discomfort and a high temperature are typical symptoms. In certain persons, it might result in severe and incapacitating symptoms. The female Aedes aegypti and Aedes albopictus mosquitoes are the carriers of the virus. The tropical and subtropical areas of Africa, Asia, Europe, and the Pacific Islands are where it is most prevalent.
Serious problems are rare, and the symptoms often go better within a few days or weeks. However, some patients develop a chronic (long-lasting) version of the illness, which can cause persistent joint discomfort. This chronic type is worse for babies, elderly individuals, and persons with heart problems or diabetes.
Ebola is an uncommon, serious illness with a high mortality rate. Although HIV is a major source of death in Africa, it can be managed and perhaps eradicated with better medical care and vaccinations. It is passed on by diseased wild animals such fruit bats, chimps, gorillas, monkeys, and forest antelope. Blood, saliva, and other body fluids from diseased animals can also infect humans.
Rehydration and early intervention increase survival. Patients must be treated in isolation from the general population while being housed in a hospital. Protective gear and measures must be used by healthcare professionals who are infected or who work with patients who have been exposed to the disease.
Zika is a virus spread by mosquitoes that can result in a low-grade fever, rash (most commonly maculopapular), and other symptoms. Usually, two to seven days after a mosquito bite, symptoms appear. For babies whose mothers contracted the virus while they were pregnant, Zika can result in serious brain issues including microcephaly. Women who get the infection early in their pregnancies experience these issues more frequently.
Avoiding mosquito bites is the basic method of illness prevention. Several repellents might potentially lessen the quantity of mosquito bites you get and protect you from them while having sex. Use barrier defenses against sex as well, such as condoms or dental dams. These help prevent STIs and are used to stop sperm from getting to the egg.
0 notes
Text
Immunotherapy Shown To Be Risk-free In Individuals With Kind 1.
Healthy Proteins & Peptides.
Content
Unique Problem On Bioactive Peptides In Metabolic Syndrome.
Supplied For Research Functions Only.
Chemical Culture Testimonials.
Medik8 Fluid Peptides (30ml).

Peptides are made up of chains of amino acids. When peptides are produced by the body, these chains are broken down into peptides, which then travel through the bloodstream to target tumors. However, in some cases, the peptides skip across the blood-clotting system. This causes the peptide to bind to the side of the clotting system and cause it to collapse, reducing or stopping its function. While this sounds dangerous, this side effect is generally harmless and does not affect the body's overall health.
Peptides also provide many benefits to the brain. Peptides have been shown to fight depression and anxiety in both animals and humans. Peptides can also help the body's metabolism, increasing energy levels and helping the body to tolerate and handle stress. Peptides also help the body produce its own antibodies, which can help protect the body against viruses and infections.
Special Issue On Bioactive Peptides In Metabolic Disorder.
It is important to note, though, that peptides do have side effects. In particular, peptides linked to chemotherapy drugs have been known to cause vomiting, diarrhea, and constipation. These side effects occur because the drug needs to break down the larger molecules in peptides in order for them to be able to perform their functions. However, there have been no reports linking these side effects with the health benefits of peptides.
One of the main health benefits of peptides is their ability to activate a defense mechanism in your body. Peptides can help slow the progression of many autoimmune diseases and help repair damage to your organs. information BPC157 Norway can boost your energy, prevent or treat irritable bowel, promote weight loss and can treat an array of mental conditions including anxiety, depression and bipolar disorder.
Provided For Research Study Purposes Only.
Peptides are protein molecules that have multiple actions in the body. Peptides can activate, inhibit or destroy enzymes and can help with the breakdown of many proteins. They also can interact with receptors in the blood or tissues to stimulate or inhibit responses.
youtube
Achieve Weight Loss - Peptides can increase your metabolic rate. This means that it helps your body burn more calories. You can achieve weight loss with the aid of peptides, especially if you combine them with protein. The combination of amino acids stimulates the burn of fat and calories. It also regulates appetite, promotes digestion and boosts energy levels to fight weight gain.
Chemical Society Testimonials.
Peptides are extremely important to the body. They are the building blocks of many essential proteins that are required for the health of the immune system. Without peptides, many aspects of the immune system would be unable to work properly. Some of the common benefits of peptides include: improving the body's ability to fight off diseases; reducing swelling and pain; improving kidney functions and protecting the body from kidney disease; reducing the risk of cancer; and more.
The Best Peptide Skincare Products to Help Build Collagen and Elastin - Coveteur
The Best Peptide Skincare Products to Help Build Collagen and Elastin.
Posted: Wed, 23 Dec 2020 08:00:00 GMT [source]
Peptides can be used to treat a variety of diseases and ailments including allergies, cancer, inflammation, arthritis, asthma, psoriasis, depression, fever, food allergies, chronic fatigue, menopause, wound healing, osteoarthritis, autoimmune disorders, multiple sclerosis and even Parkinson's disease. Peptides can also prevent many degenerative diseases including Alzheimer's and dementia. Peptides are essential for immunity and can be made by our bodies naturally. However, in our modern day environment, many pollutants in the air and water can attack the stomach lining and other internal organs. This can weaken the inner lining of our organs and makes us more prone to disease. Our diets also do not contain enough nutrients for optimal health.
Medik8 Fluid Peptides (30ml).
Peptides are also valuable in relieving the symptoms of rheumatoid arthritis. They can provide relief from the stiffness and pain that come with this disease. Peptides can enhance your body's ability to fight infection and heal from wounds and trauma. It can also help boost your immune system, which can help ward off colds and other illness.
The major issue associated with the dissolution of a peptide is the development of aggregated secondary frameworks.
If the peptide does not dissolve with the above organic solvent, it may need TFA or formic acid 1.
This slide collection is ideal as an introduction to the topic of peptide ligands.
High concentration of chaotropic salts aids to dissolve the peptide by breaking up the additional structures.
Propanol as well as acetonitrile can dissolve some medium-sized peptides.
If the peptide is to be infused onto a column, the quantity of natural solvent, especially propanol, should be maintained little, or retention time will certainly be considerably affected.
Maintain peptides in an oxygen-free setting as peptides containing cysteine, methionine, tryptophan, glutamine and also asparagine are susceptible to oxidation and have limited life span.
Peptides are made up of amino acids that are arranged in linear pairs. These are essential to every living thing, however, they do not have any form of protein. Peptides assist the body with the production of proteins. The body needs a steady supply of proteins, and these can be provided through the digestive system. Here, BPC157 USA will be introducing a few of the most common Peptides Types.
Peptides are also very effective in the treatment of cancer, especially when administered through chemotherapy. Chemotherapy drugs sometimes fail to deliver on their promises. Peptides have been shown to be very effective in stimulating the immune system, which helps fight tumors and keep them from growing. They also increase the body's detoxification capabilities and allow it to eliminate waste products that might interfere with chemotherapy drugs. Peptides can provide a major benefit to patients who suffer from cancer as they increase the chances of survival.
Will peptides make me bigger?
Supplement companies often tout peptides to boost muscle growth, promote fat loss, or improve workout performance and recovery. However, strong research does not back many of these claims. Very little evidence is available on the effects of peptides in well-trained individuals like bodybuilders.
Glutamic acids are a medium sized group of amino acids. They are produced by the breakdown of carbohydrates. Glutamic acids also contain an amino acid called glutamine. This amino acid functions as a low rate antioxidant. Glutamic acids are highly recommended for those suffering from conditions such as heart disease and stroke.
To help build up our immune system and defend the body from disease, peptides are a powerful natural supplement. Peptides have a wide range of beneficial uses in the body. They can improve your mood, boost your energy, stabilize your cholesterol level, regulate your digestive system, fight off infectious agents and even reduce the risk of a number of cancers. Peptides can also increase your fertility. Peptides are an important part of a healthy diet, because they work to improve digestion and absorption of nutrients in the body, they also help the body absorb nutrients and rid it of waste.
Peptides serve a variety of purposes in the body. They help to balance the levels of the chemicals that create inflammation and the chemicals that protect the immune system. They can also help to regulate blood pressure and cholesterol levels as well as regulate the secretion of important hormones. These benefits make peptides an essential part of a healthy diet and lifestyle.
#BPC157 EU#BPC157 Europe#information BPC157 EU#information BPC157 Europe#EU BPC157 how does it work#Europe BPC157 how does it work
1 note
·
View note
Text
Pneumonia
The lungs are made up of small sacs called alveoli, which fill with air when a healthy person breathes. Pneumonia is an infection of the lungs that may be caused by bacteria, viruses, or fungi. The infection causes the alveoli to become inflamed and fill up with fluid or pus. That can make it hard for the oxygen you breathe in to get into your bloodstream. The symptoms of pneumonia can range from mild to severe, and include cough, fever, chills, and trouble breathing.
Many factors affect how serious a case of pneumonia is, such as the type of germ causing the lung infection, the person’s age, and their overall health. The people most at risk are infants and young children, adults 65 or older, and people who have other health problems. Pneumonia is a leading cause of hospitalization in both children and adults. Most cases can be treated successfully, although it can take weeks to fully recover. Tens of thousands of people in the U.S. die from pneumonia every year, most of them adults over the age of 65. And is the single largest infectious cause of death in children worldwide. Pneumonia killed 808 694 children under the age of 5 in 2017, accounting for 15% of all deaths of children under five years old. Pneumonia affects children and families everywhere, but is most prevalent in South Asia and sub-Saharan Africa. Children can be protected from pneumonia, it can be prevented with simple interventions, and treated with low-cost, low-tech medication and care.
Causes:
Many germs can cause pneumonia. The most common are bacteria and viruses in the air we breathe. Your body usually prevents these germs from infecting your lungs. But sometimes these germs can overpower your immune system, even if your health is generally good. Most germs that cause pneumonia are contagious. This means they can spread from person to person. Pneumonia is classified according to the types of germs that cause it and where you got the infection.
Both viral and bacterial pneumonia can spread to others through inhalation of airborne droplets from a sneeze or cough. You can also get these types of pneumonia by coming into contact with surfaces or objects that are contaminated with pneumonia-causing bacteria or viruses.
Community-acquired pneumonia
The most common type of pneumonia. It occurs outside of hospitals or other health care facilities. It may be caused by:
Bacteria. The most common cause of bacterial pneumonia in the U.S. is Streptococcus pneumonia. Other type of bacteria that cause pneumonia can be Mycoplasma pneumonia, Haemophilus influenza, Staphylococcus aureus, Legionella pneumophila and Viral pneumonia. This type of pneumonia can occur on its own or after you've had a cold or the flu. It may affect one part (lobe) of the lung, a condition called lobar pneumonia.
Bacteria-like organisms. Mycoplasma pneumoniae also can cause pneumonia. It typically produces milder symptoms than do other types of pneumonia. Walking pneumonia is an informal name given to this type of pneumonia, which typically isn't severe enough to require bed rest.
Fungi. This type of pneumonia is most common in people with chronic health problems or weakened immune systems, and in people who have inhaled large doses of the organisms. The fungi that cause it can be found in soil or bird droppings and vary depending upon geographic location. Some of them being Pneumocystis jirovecii, Cryptococcus species, Coccidioidomycosis, Histoplasmosis, Cryptococcus, and Histoplasmosis species. However, it doesn’t spread from person to person. (in infants infected with HIV, Pneumocystis jiroveci is one of the most common causes of pneumonia, responsible for at least one quarter of all pneumonia deaths in HIV-infected infants.)
Viruses. Some of the viruses that cause colds and the flu can cause pneumonia. Most commonly caused by the respiratory syncytial virus (RSV) and sometimes influenza type A or B. Viruses are the most common cause of pneumonia in children younger than 5 years. Viral pneumonia is usually mild. But in some cases it can become very serious.
Hospital-acquired pneumonia
Some people catch pneumonia during a hospital stay for another illness. Hospital-acquired pneumonia can be serious because the bacteria causing it may be more resistant to antibiotics and because the people who get it are already sick. People who are on breathing machines (ventilators), often used in intensive care units, are particularly at risk of developing ventilator-associated pneumonia
Health care-acquired pneumonia
Health care-acquired pneumonia is a bacterial infection that occurs in people who live in long-term care facilities or who receive care in outpatient clinics, including kidney dialysis centers. Like hospital-acquired pneumonia, health care-acquired pneumonia can be caused by bacteria that are more resistant to antibiotics.
Aspiration pneumonia
Aspiration pneumonia occurs when you inhale vomit, a foreign object, such as a peanut, or a harmful substance, such as smoke or a chemical into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcohol or drugs.
Some types of bacteria cause what is known as "atypical" pneumonia, including:
Mycoplasma pneumoniae, a tiny wide-spread bacterium that usually infects people younger than 40 years old, especially those living and working in crowded conditions. The illness is often mild enough to go undetected and is sometimes referred to as walking pneumonia.
Chlamydophila pneumoniae, which commonly causes upper respiratory infections year-round, but can also result in a mild form of pneumonia.
Legionella pneumophila, which causes a dangerous form of pneumonia called Legionnaire's disease. Unlike other bacterial pneumonias, Legionella is not passed from person to person. Outbreaks of the disease have been linked to exposure to contaminated water from cooling towers, whirlpool spas, and outdoor fountains.
These bacteria are referred to as "atypical" because pneumonia caused by these organisms might have slightly different symptoms, appear different on a chest X-ray, or respond to different antibiotics than the typical bacteria that cause pneumonia. Even though these infections are called "atypical," they are not uncommon.
Symptoms:
The signs and symptoms of pneumonia vary from mild to severe, depending on factors such as the type of germ causing the infection, and your age and overall health. Mild signs and symptoms often are similar to those of a cold or flu, but they last longer.
Signs and symptoms of pneumonia may include:
Sharp or stabbing chest pain that gets worse when you breathe deeply or cough
Confusion or changes in mental awareness (in adults age 65 and older)
cough – which may be dry, or produce thick yellow, green, brown or blood-stained mucus (phlegm)
difficulty breathing – your breathing may be rapid and shallow, and you may feel breathless, even when resting
Fatigue
feeling generally unwell
Fever, sweating and shaking chills
loss of appetite
Lower than normal body temperature (in adults older than age 65 and people with weak immune systems)
Nausea, vomiting or diarrhea
rapid heartbeat
Shortness of breath
Less common symptoms include:
coughing up blood (haemoptysis)
headaches
fatigue
feeling sick or being sick
wheezing
joint and muscle pain
feeling confused and disorientated, particularly in elderly people
Newborns and infants may not show any sign of the infection. Or they may vomit, have a fever and cough, appear restless or tired and without energy, or have difficulty breathing and eating.
When to see a doctor
See your doctor if you have difficulty breathing, chest pain, persistent fever of 102 F (39 C) or higher, or persistent cough, especially if you're coughing up pus. It's especially important that people in these high-risk groups see a doctor:
Adults older than age 65
Children younger than age 2 with signs and symptoms
People with an underlying health condition or weakened immune system
People receiving chemotherapy or taking medication that suppresses the immune system
For some older adults and people with heart failure or chronic lung problems, pneumonia can quickly become a life-threatening condition.
Diagnosis:
Pneumonia can be difficult to diagnose because it shares many symptoms with other conditions, such as the common cold, bronchitis and asthma. To diagnose pneumonia, and to try to identify the germ that is causing the illness, your doctor will ask questions about your medical history, do a physical exam, and run some tests.
Medical history
Your doctor will ask you questions about your signs and symptoms, and how and when they began. To help figure out if your infection is caused by bacteria, viruses or fungi, you may be asked some questions about possible exposures, such as:
Any recent travel
Your occupation
Contact with animals
Exposure to other sick people at home, work or school
Whether you have recently had another illness
Physical exam
Your doctor will listen to your lungs with a stethoscope. If you have pneumonia, your lungs may make crackling, bubbling, and rumbling sounds when you inhale.
Diagnostic Tests
They’ll then give you a physical exam. This will include listening to your lungs with a stethoscope for any abnormal sounds, such as crackling. Depending on the severity of your symptoms and your risk for complications, your doctor may also order one or more of these tests
If your doctor suspects you may have pneumonia, they will probably recommend some tests to confirm the diagnosis and learn more about your infection. These may include:
Blood culture: This test uses a blood sample to confirm an infection. Culturing can also help identify what may be causing your condition.
Chest X-ray: An X-ray helps your doctor look for signs of inflammation in your chest. If inflammation is present, the X-ray can also inform your doctor about its location and extent.
Fluid sample: If your doctor suspects there’s fluid in the pleural space of your chest, they may take a fluid sample using a needle placed between your ribs. This test can help identify the cause of your infection.
Pulse oximetry: A pulse oximetry measures the amount of oxygen in your blood. A sensor placed on one of your fingers can indicate whether your lungs are moving enough oxygen through your bloodstream.
Sputum culture: During a sputum culture, a sample of mucus is collected after you’ve coughed deeply. It’s then sent to a lab to be analyzed to identify the cause of the infection.
If you are considered a high-risk patient because of your age and overall health, or if you are hospitalized, the doctors may want to do some additional tests, including:
CT scan of the chest to get a better view of the lungs and look for abscesses or other complications.
Arterial blood gas test, to measure the amount of oxygen in a blood sample taken from an artery, usually in your wrist. This is more accurate than the simpler pulse oximetry.
Pleural fluid culture, which removes a small amount of fluid from around tissues that surround the lung, to analyze and identify bacteria causing the pneumonia.
Bronchoscopy, a procedure used to look into the lungs' airways. If you are hospitalized and your treatment is not working well, doctors may want to see whether something else is affecting your airways, such as a blockage. They may also take fluid samples or a biopsy of lung tissue. Your doctor will start by taking your medical history. They’ll ask you questions about when your symptoms first appeared and your health in general.
Treatment:
Specific treatments depend on the type and severity of your pneumonia, your age and your overall health. The options include:
Antibiotics. These medicines are used to treat bacterial pneumonia. It may take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms don't improve, your doctor may recommend a different antibiotic.
Cough medicine. This medicine may be used to calm your cough so that you can rest. Because coughing helps loosen and move fluid from your lungs, it's a good idea not to eliminate your cough completely. In addition, you should know that very few studies have looked at whether over-the-counter cough medicines lessen coughing caused by pneumonia. If you want to try a cough suppressant, use the lowest dose that helps you rest.
Fever reducers/pain relievers. You may take these as needed for fever and discomfort. These include drugs such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
Your doctor may prescribe a medication to help treat your pneumonia. What you’re prescribed will depend on the specific cause of your pneumonia.
Oral antibiotics can treat most cases of bacterial pneumonia. Always take your entire course of antibiotics, even if you begin to feel better. Not doing so can prevent the infection from clearing, and it may be harder to treat in the future.
Antibiotic medications don’t work on viruses. In some cases, your doctor may prescribe an antiviral. However, many cases of viral pneumonia clear on their own with at-home care.
Antifungal medications are used to fight fungal pneumonia. You may have to take this medication for several weeks to clear the infection.
Hospitalization
You may need to be hospitalized if:
You are older than age 65
You are confused about time, people or places
Your kidney function has declined
Your systolic blood pressure is below 90 millimeters of mercury (mm Hg) or your diastolic blood pressure is 60 mm Hg or below
Your breathing is rapid (30 breaths or more a minute)
You need breathing assistance
Your temperature is below normal
Your heart rate is below 50 or above 100
You may be admitted to the intensive care unit if you need to be placed on a breathing machine (ventilator) or if your symptoms are severe.
Children may be hospitalized if:
They are younger than age 2 months
They are lethargic or excessively sleepy
They have trouble breathing
They have low blood oxygen levels
They appear dehydrated
Hospital treatment may include:
intravenous antibiotics injected into a vein
respiratory therapy, which involves delivering specific medications directly into the lungs or teaching you to perform breathing exercises to maximize your oxygenation
oxygen therapy to maintain oxygen levels in your bloodstream (received through a nasal tube, face mask, or ventilator, depending on severity)
Mild pneumonia can usually be treated at home by:
getting plenty of rest
taking antibiotics
drinking plenty of fluids
Your doctor may also recommend over-the-counter (OTC) medication to relieve your pain and fever, as needed. These may include:
aspirin
ibuprofen (Advil, Motrin)
acetaminophen (Tylenol)
If you do not have any other health problems, you should respond well to treatment and soon recover, although your cough may last for some time. It's usually safe for someone with pneumonia to be around others, including family members. But people with a weakened immune system are less able to fight off infections, so it's best they avoid close contact with a person with pneumonia.
For at-risk groups, pneumonia can be severe and may need to be treated in hospital. This is because it can lead to serious complications, which in some cases can be fatal, depending on a person's health and age. Your treatment will depend on the type of pneumonia you have, how severe it is, and your general health.
Take any medications as prescribed by your doctor. If your pneumonia is caused by bacteria, you will be given an antibiotic. It is important to take all the antibiotic until it is gone, even though you will probably start to feel better in a couple of days. If you stop, you risk having the infection come back, and you increase the chances that the germs will be resistant to treatment in the future. Typical antibiotics do not work against viruses. If you have viral pneumonia, your doctor may prescribe an antiviral medication to treat it. Sometimes, though, symptom management and rest are all that is needed.
Sources: x x x x x
5 notes
·
View notes
Text
Nicotine Dependence: Symptoms and Causes

Nicotine dependence occurs when you need nicotine and can't stop using it. Nicotine is the chemical in tobacco that makes it hard to quit. Nicotine produces pleasing effects in your brain, but these effects are temporary. So you reach for another cigarette.
The more you smoke, the more nicotine you need to feel good. When you try to stop, you experience unpleasant mental and physical changes. These are symptoms of nicotine withdrawal.
Regardless of how long you've smoked, stopping can improve your health. It isn't easy but you can break your dependence on nicotine. Many effective treatments are available. Ask your doctor for help.
Symptoms
For some people, using any amount of tobacco can quickly lead to nicotine dependence. Signs that you may be addicted include:
1. You can't stop smoking. You've made one or more serious, but unsuccessful, attempts to stop.
2. You have withdrawal symptoms when you try to stop. Your attempts at stopping have caused physical and mood-related symptoms, such as strong cravings, anxiety, irritability, restlessness, difficulty concentrating, depressed mood, frustration, anger, increased hunger, insomnia, constipation or diarrhea.
3. You keep smoking despite health problems. Even though you've developed health problems with your lungs or your heart, you haven't been able to stop.
4. You give up social activities. You may stop going to smoke-free restaurants or stop socializing with family or friends because you can't smoke in these situations.
When to See a Doctor
-- You're not alone if you've tried to stop smoking but haven't been able to stop for good. Most smokers make many attempts to stop smoking before they achieve stable, long-term abstinence from smoking.
-- You're more likely to stop for good if you follow a treatment plan that addresses both the physical and the behavioral aspects of nicotine dependence. Using medications and working with a counselor specially trained to help people stop smoking (a tobacco treatment specialist) will significantly boost your chances of success.
-- Ask your health care team to help you develop a treatment plan that works for you or to advise you on where to get help to stop smoking.
Nicotine is the chemical in tobacco that keeps you smoking. Nicotine reaches the brain within seconds of taking a puff. In the brain, nicotine increases the release of brain chemicals called neurotransmitters, which help regulate mood and behavior.
Dopamine, one of these neurotransmitters, is released in the reward center of the brain and causes feelings of pleasure and improved mood. The more you smoke, the more nicotine you need to feel good. Nicotine quickly becomes part of your daily routine and intertwined with your habits and feelings.
Common Situations That Trigger the Urge to Smoke Include:
a. Drinking coffee or taking breaks at work
b. Talking on the phone
c. Drinking alcohol
d. Driving your car
e. Spending time with friends
To overcome your nicotine dependence, you need to become aware of your triggers and make a plan for dealing with them.
Risk Factors
Anyone who smokes or uses other forms of tobacco is at risk of becoming dependent. Factors that influence who will use tobacco include:
1. Age. Most people begin smoking during childhood or the teen years. The younger you are when you begin smoking, the greater the chance that you'll become addicted.
2. Genetics. The likelihood that you will start smoking and keep smoking may be partly inherited. Genetic factors may influence how receptors on the surface of your brain's nerve cells respond to high doses of nicotine delivered by cigarettes.
3. Parents and peers. Children who grow up with parents who smoke are more likely to become smokers. Children with friends who smoke are also more likely to try it.
4. Depression or other mental illness. Many studies show an association between depression and smoking. People who have depression, schizophrenia, post-traumatic stress disorder or other forms of mental illness are more likely to be smokers.
5. Substance use. People who abuse alcohol and illegal drugs are more likely to be smokers.
Complications
Tobacco smoke contains more than 60 known cancer-causing chemicals and thousands of other harmful substances. Even "all natural" or herbal cigarettes have harmful chemicals.
You already know that people who smoke cigarettes are much more likely to develop and die of certain diseases than people who don't smoke. But you may not realize just how many different health problems smoking causes:
A. Lung cancer and lung disease. Smoking is the leading cause of lung cancer deaths. In addition, smoking causes lung diseases, such as emphysema and chronic bronchitis. Smoking also makes asthma worse.
B. Other cancers. Smoking increases the risk of many types of cancer, including cancer of the mouth, throat (pharynx), esophagus, larynx, bladder, pancreas, kidney, cervix and some types of leukemia. Overall, smoking causes 30% of all cancer deaths.
C. Heart and circulatory system problems. Smoking increases your risk of dying of heart and blood vessel (cardiovascular) disease, including heart attacks and strokes. If you have heart or blood vessel disease, such as heart failure, smoking worsens your condition.
D. Diabetes. Smoking increases insulin resistance, which can set the stage for type 2 diabetes. If you have diabetes, smoking can speed the progress of complications, such as kidney disease and eye problems.
E. Eye problems. Smoking can increase your risk of serious eye problems such as cataracts and loss of eyesight from macular degeneration.
F. Infertility and impotence. Smoking increases the risk of reduced fertility in women and the risk of impotence in men.
G. Complications during pregnancy. Mothers who smoke while pregnant face a higher risk of preterm delivery and giving birth to lower birth weight babies.
H. Cold, flu and other illnesses. Smokers are more prone to respiratory infections, such as colds, the flu and bronchitis.
I. Tooth and gum disease. Smoking is associated with an increased risk of developing inflammation of the gum and a serious gum infection that can destroy the support system for teeth (periodontitis).
J. Smoking also poses health risks to those around you. Nonsmoking spouses and partners of smokers have a higher risk of lung cancer and heart disease compared with people who don't live with a smoker. Children whose parents smoke are more prone to worsening asthma, ear infections and colds.
Prevention
The best way to prevent nicotine dependence is to not use tobacco in the first place. The best way to keep children from smoking is to not smoke yourself. Research has shown that children whose parents do not smoke or who successfully quit smoking are much less likely to take up smoking.
Diagnosis
Your doctor may ask you questions or have you fill out a questionnaire to see how dependent you are on nicotine. Knowing your degree of dependence will help your doctor determine the right treatment plan for you. The more cigarettes you smoke each day and the sooner you smoke after awakening, the more dependent you are.
Treatment
Like most smokers, you've probably made at least one serious attempt to stop. But it's rare to stop smoking on your first attempt — especially if you try to do it without help. You're much more likely to be able to stop smoking if you use medications and counseling, which have both been proved effective, especially in combination.
Medications
Some quit-smoking products are known as nicotine replacement therapy because they contain varying amounts of nicotine. Some of these nicotine replacement therapies require a prescription, but others don't. There are two approved quit-smoking medications that don't contain nicotine, and both are available only by prescription.
Any of these products can help reduce nicotine cravings and withdrawal symptoms — making it more likely that you'll stop smoking for good. Using more than one may help you get better results. Although you can buy some quit-smoking products without a prescription, it's a good idea to talk to your doctor first. Together you can explore which products might be right for you, when to start taking them and possible side effects.
Counseling
Medications help you cope by reducing withdrawal symptoms and cravings, while behavioral treatments help you develop the skills you need to give up tobacco for good. The more time you spend with a counselor, the better your treatment results will be.
During individual or group counseling, you learn techniques you can use to help you stop smoking. Many hospitals, health care plans, health care providers and employers offer treatment programs. Some medical centers provide residential treatment programs — the most intensive treatment available.
Methods to Avoid
Electronic cigarettes (e-cigarettes) have not proved to be safe nor are they more effective in helping people stop smoking than nicotine replacement medications. In fact, many people who use e-cigarettes to stop smoking find themselves using both products rather than quitting.
It's not a good idea to substitute another type of tobacco use for smoking. Tobacco in any form is not safe. Steer clear of these products:
- Dissolvable tobacco products
- Smokeless tobacco
- Nicotine lollipops and balms
- Cigars and pipes
- Hookahs
Coping and Support
Social support is key to achieving a stable and solid, smoke-free life. Ask your family, friends and co-workers for support and encouragement. Be direct and let them know what would help you most.
Also Consider Trying These Resources:
1. Support groups. Often available at little or no cost, support groups offer coaching and mutual support from others attempting to quit. Nicotine Anonymous groups are available in many locations.
2. Telephone counseling. Quit lines offer convenient access to trained counselors. In the U.S., call 800-QUIT-NOW (800-784-8669) to connect directly to your state's quit line.
3. Text messaging and mobile apps. A number of services are available to get reminders and tips delivered to your mobile phone.
4. Web-based programs. Sites such as BecomeAnEX provide free personalized support, interactive guides and tools, and discussion groups to help you quit.
Preparing for Your Appointment
You're likely to start by seeing your primary care doctor. Here's some information to help you get ready, and what to expect from your doctor.
What You Can Do To Get Ready for Your Appointment:
a. Consider your smoking triggers. List the circumstances when you're most likely to reach for a cigarette. In what situations has smoking become a ritual?
b. Make note of any symptoms that may be related to smoking. Include the length of time you've had each one.
c. Make a list of your medications. Include any vitamins, herbs or other supplements.
d. Invite a family member or friend along. Sometimes it can be difficult to soak up all the information provided during an appointment.
What to Expect From Your Doctor
Being ready to answer questions your doctor may ask reserves time to go over any points you want to spend more time on. Some questions your doctor may ask include:
1. How many cigarettes do you smoke each day? How soon after waking do you smoke?
2. Have you previously tried to stop smoking? If so, what happened? What worked? What didn't work?
3. What is motivating you to stop smoking now?
4. Do you have any physical health problems, such as heart disease or diabetes, which you suspect are related to smoking?
5. Has smoking caused any problems at work or in your relationships?
SOLIAIR™ is a company that specializes in alternative medicine and natural drug development that is privately owned. The SOLIAIR™ Food supplements are patented and are regularly used by doctors, pharmacists and patients in the U.S and around the world! - Please contact us for an advice and a professional treatment!
Best Regards,
Solomon J.
(Naturopath/Alternative Therapist)
#####
youtube
#stop smoking#Quit Smoking#heavy smoker#Light Smoker#lung cancer#Addiction Ash#chain smoker#cigarette butt#nicotine addiction#nicotine#nicotine carvings#smoking#cigarette#cancer#lung rehabilitation#smoking addiction#addiction#copd#lung disease#lung infections#respiratory diseases#respiratory symptoms#respiratory syndrome#respiratory infection#bronchitis#breathing#breathing disorders#breathing problem#breathing difficulties#asthma
1 note
·
View note
Text
Chronic Diseases Driven by Metabolic Dysfunction
New model suggests natural healing cycle becomes blocked by cellular miscommunication, allowing conditions like cancer, diabetes and some neurological disorders to persist; a small but dramatic autism trial offers evidence
Much of modern Western medicine is based upon the treatment of acute, immediate harm, from physical injury to infections, from broken bones and the common cold to heart and asthma attacks.
But progress in treating chronic illness, where the cause of the problem is often unknown—and, in fact, may no longer even be present — has lagged. Chronic conditions like cancer, diabetes and cardiovascular disease defy easy explanation, let alone remedy. The Centers for Disease Control and Prevention estimate that more than half of adults and one-third of children and teens in the United States live with at least one chronic illness. Chronic medical conditions, according to the National Institutes of Health, cause more than half of all deaths worldwide.
In a new paper, available online in Mitochondrion in advance of publication, Robert K. Naviaux, MD, PhD, professor of medicine, pediatrics and pathology at University of California San Diego School of Medicine, posits that chronic disease is essentially the consequence of the natural healing cycle becoming blocked, specifically by disruptions at the metabolic and cellular levels.
“The healing process is a dynamic circle that starts with injury and ends with recovery. The molecular features of this process are universal,” said Naviaux, who also directs the Mitochondrial and Metabolic Disease Center at UC San Diego. “Emerging evidence shows that most chronic illnesses are caused by the biological reaction to an injury, not the initial injury or the agent of the injury. The illness occurs because the body is unable to complete the healing process.”
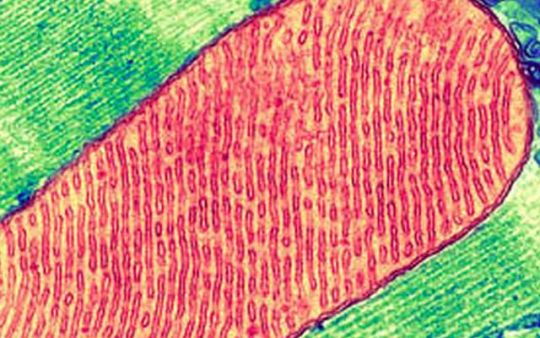
False-color transmission electron micrograph of a mitochondrion inside a cell. Photo credit: Thomas Deerinck, National Center for Microscopy and Imaging Research, UC San Diego
For example, said Naviaux, melanoma — the deadliest form of skin cancer — can be caused by sun exposure that occurred decades earlier, damaging DNA that was never repaired. Post-traumatic stress disorder can flare months or years after the original head injury has healed. A concussion sustained before an earlier concussion has completely resolved typically results in more severe symptoms and prolonged recovery, even if the second impact is less than the first.
“Progressive dysfunction with recurrent injury after incomplete healing occurs in all organ systems, not just the brain,” said Naviaux. “Chronic disease results when cells are caught in a repeating loop of incomplete recovery and re-injury, unable to fully heal. This biology is at the root of virtually every chronic illness known, including susceptibility to recurrent infections, autoimmune diseases like rheumatoid arthritis, diabetic heart and kidney disease, asthma, chronic obstructive pulmonary disease, Alzheimer’s dementia, cancer and autism spectrum disorder.”
For more than a decade, Naviaux and colleagues have been investigating and developing a theory based on cell danger response (CDR), a natural and universal cellular reaction to injury or stress. In the new paper, Naviaux describes the metabolic features of the three stages of CDR that comprise the healing cycle.
“The purpose of CDR is to help protect the cell and jump-start the healing process,” said Naviaux, by essentially causing the cell to harden its membranes, cease interaction with neighbors and withdraw within itself until the danger has passed.
Chronic Diseases Driven by Metabolic Dysfunction
39 notes
·
View notes
Text
Gluten Intolerance, Wheat Allergies, and Celiac Disease - It's More Complicated Than You Think
Is “gluten free” a fad? No, it’s going to be a thing for as long as we are producing wheat and bread the way we’re doing it. A lot has changed in the bread industry – it’s not just one thing.
People often comment about how bread didn’t cause problems with our health before GMOs and Roundup were prevalent in our food supply. Our farming practices have changed, and fairly recently, wheat has started being sprayed with Roundup. The newest speculation is that wheat is not the problem – that the problem is glyphosate, the active ingredient in Roundup. People also often suspect that wheat has been genetically modified. And, of course, there are those who believe the whole gluten-elimination thing is ridiculous and that most people are jumping on the gluten-free bandwagon because it’s trendy.
Related: How to Eliminate IBS, IBD, Leaky Gut
In my experience, if one suffers from a chronic illness of any kind, they must remove gluten from their diet in order to get well. I have yet to see an exception. So what’s the problem? Is it the glyphosate or the wheat or something else? The truth is it’s not just one thing. Everyone would already know this if most humans weren’t so bad at thinking in terms of systems. We tend to think linearly and look for singular cause and effects, but rarely if ever are complex problems solved by such simplistic thinking. There are multiple reasons one gets sick, with a cold or a chronic disease, just like there are multiple reasons why our planet’s ecosystem is changing. This is why you can’t blame the rise of autism on just glyphosate, or GMOs, or increased vaccinations, or diminishing food quality, or environmental degradation – they all correlate, it’s all of the above.
Related: Best Supplements To Kill Candida and Everything Else You Ever Wanted To Know About Fungal Infections
There is a very complex system that is causing the decline of American health, and it’s not just the bread. And yes, our health is in decline. If you doubt that…here, google it and take your pick. Our lifespan is actually decreasing.
What’s the difference between Gluten Intolerance, Wheat Allergies, and Celiac Disease
Conventional medicine states that celiac disease and non-celiac gluten sensitivity have a lot of symptoms in common but identifies a key difference. Non-celiac gluten sensitivity is not a genetic disease and does not cause an autoimmune reaction, and celiac disease is a genetic autoimmune disease. A wheat allergy is an allergic reaction to any of the hundreds of proteins in wheat. Gluten intolerance used to be a catch-all phrase for any problem with eating gluten, but now it’s being relegated to mean Non-celiac gluten sensitivity.
Non-celiac Gluten Sensitivity
Non-celiac gluten sensitivity is believed to be the most prevalent of the gluten-related disorders, but it’s not as well defined as the other two. It’s not an autoimmune reaction nor is it an allergic reaction. There are no tests or biomarkers to identify this disorder. Other components of gluten-grains may be causing symptoms. In order for non-celiac gluten sensitivity to be diagnosed, a doctor will rule out celiac disease and wheat allergies or other possible causes of the symptoms first.
Common Symptoms for Non-celiac Gluten Sensitivity
Fatigue
Mental fatigue, aka “brain fog”
Headaches
Migraines
Bone or joint pain
Gastrointestinal distress
Gas
Bloating
Cramping
Indigestion
Abdominal pain
Diarrhea
Constipation
It’s said that individuals with gluten sensitivity do not experience damage to the small intestine or develop tissue transglutaminase antibodies like they do with celiac disease. Non-celiac gluten sensitivity has been linked to a variety of health problems including, diabetes, allergies, autism spectrum disorders, and much more.
Related: How to Avoid GMOs in 2018 – And Everything Else You Should Know About Genetic Engineering
Gastroenterologists looking for celiac disease typically test for a few specific antibodies, and if found, they do an intestinal biopsy to determine if tissue damage is present. Chris Kresser addresses the issue with this kind of testing in 3 Reasons Gluten Intolerance May Be More Serious Than Celiac Disease, which I highly recommend reading. He states:
According to some estimates, for every diagnosed case of celiac disease (CD), there are 6.4 undiagnosed cases that remain undiagnosed—the majority of which are atypical or “silent” forms with no damage to the gut. (1) This silent form of CD is far from harmless; it is associated with a nearly fourfold increase in the risk of death. (2)
I believe that patients with NCGS are even more likely than patients with CD to go undiagnosed. Most gastroenterologists today know how to screen for celiac disease. They will typically test for antibodies to antibodies to alpha gliadin, transglutaminase-2, deamidated gliadin, and endomysium, and if positive do a biopsy to determine if tissue damage is present.
However, we now know that people can (and do) react to several other components of wheat above and beyond alpha gliadin, the component that is implicated in CD. These include other epitopes of gliadin (beta, gamma, omega), glutenin, wheat germ agglutinin (WGA), gluteomorphin, and deamidated gliadin. What’s more, people can react to other types of tissue transglutaminase, including type 3—primarily found in the skin—and type 6—primarily found in the brain. (3, 4, 5, 6, 7, 8)
Celiac Disease
Celiac disease is considered a genetic, autoimmune disorder. Ninety-eight percent of people with celiac disease carry one or both of two very specific genes, HLA DQ2 and DQ8. On the other hand, so does up to 25-30% of the general population. Carrying one or both of these genes does not mean you have celiac disease nor does it mean you will develop it. Doctors often use gene testing to rule out celiac disease, but there are some cases where people who do not have either of the genes still tested out to have celiac disease.
Though celiac disease is said to be genetic, genes cause predispositions and our diet and environment adjust our genes. Environment can alter gene activity without changing the DNA sequence. This is called gene expression. I also believe that the environment and diet can actually alter the DNA sequence, but from what I’m seeing, current science doesn’t agree with me on this. Regardless, how your genes affect you is altered by our diet and our environment, and those traits can be passed down to our offspring as well. In other words, a predisposition to celiac disease may be hereditary, but whether or not we have celiac disease could depend on our genetic health, which depends on our overall health, which depends on our lifestyle. And this can all be traced to gut health – you cannot have a healthy gut without a healthy lifestyle, and our gut health is something most of us have complete control over.
Related: Gluten, Candida, Leaky Gut Syndrome, and Autoimmune Diseases
Common Symptoms of Celiac Disease
Fatigue
Mental fatigue, aka “brain fog”
Headaches
Migraines
Bone or joint pain
Gastrointestinal distress
Gas
Bloating
Cramping
Indigestion
Abdominal pain
Diarrhea
Constipation
Arthritis
Dermatitis
Eczema
Osteoporosis
Liver disorders
Depression or anxiety
Peripheral neuropathy
Seizures
Migraines
Irregular menstruation
Miscarriages
Canker sores
Doctors believe that in order to develop the disease, a person needs to have the genetic predisposition while they are consuming gluten and to subsequently have the disease activated. Activation triggers are said to potentially be stress, trauma, and viral infections. I contend that vaccines and antibiotics are the two most common triggers for the disease. Damaging the gut is what leads to problems with wheat, but we’ll get more into that below.
Wheat Allergies
Celiac disease and non-celiac gluten sensitivity have many symptoms in common, but wheat allergies are often much more distinctive. Symptoms include itching, hives, or anaphylaxis which is a life-threatening reaction. A wheat allergy is an immune reaction to any of the hundreds of proteins in wheat. It is possible for a person to be allergic to wheat and to have non-celiac gluten sensitivity or celiac disease at the same time.
What About Roundup?
Monsanto introduced glyphosate under the trade name Roundup in 1974 shortly after DDT was banned. It wasn’t used very much until the late 1990s when Monsanto genetically engineered seeds to withstand high doses of Roundup, and the product took off. Eager to sell more of its flagship herbicide, Monsanto has encouraged farmers to use their glyphosate as a desiccant. Wheat can be harvested quicker and easier if you dry it all out ahead of time with Roundup. It’s also used in this way on wheat, barley, oats, canola, flax, peas, lentils, soybeans, dry beans, and sugar cane.
Studies have concluded that chronically ill people have higher levels of glyphosate in their bodies. Glyphosate has been attributed to an increased prevalence of most of our common chronic conditions including, but not limited to ADHD, Alzheimer’s, birth defects, autism, cancer, kidney disorder, irritable bowel syndrome, Parkinson’s disease, depression, diabetes, heart disease, thyroid disorders, liver disorders, multiple sclerosis, reproductive issues, adrenal failure, obesity, asthma, and of course, celiac disease.
It’s not hard to understand why. Glyphosate is poison and so are the other ingredients in Roundup. People have to wear protective gear to apply the product. It is designed to kill. It kills plants by preventing them from making certain proteins. Just imagine what that does to one’s gut ecology.
How Wheat Has Changed
The wheat we have now is very different from what our ancestors consumed. Modern dwarf wheat is hybridized. That isn’t a GMO, but the genes of our wheat plant have certainly been modified to grow faster, and to be more resilient. We used to eat wheat called einkorn, which was actually one of the very first grains we humans cultivated more than 10,000 years ago. When you read in the Bible about how we should eat bread, this is the wheat it refers to.
There is a lot more gluten in modern wheat than there is in einkorn, and the gluten that einkorn wheat does contain is different. Einkorn also has 15 percent less starch and 30 percent more protein. Modern wheat has a lower nutrient content and a different protein structure. In fact, many with celiac and gluten intolerance report being able to eat einkorn without issue.
Also, that blood sugar spike experienced after eating bread does not happen with einkorn.
So I conducted a simple experiment on myself. On an empty stomach, I ate 4 oz of einkorn bread. On another occasion I ate 4 oz of bread that dietitian, Margaret Pfeiffer, made with whole wheat flour bought at the grocery store. Both flours were finely ground and nothing was added beyond water, yeast, olive oil, and a touch of salt.” – Einkorn and blood sugar
“Ancient wheat diets caused a downregulation of key regulatory genes involved in glucose and fat metabolism, equivalent to a prevention or delay of diabetes development. Spelt and rye induced a low acute glycemic response compared to wheat.” – NCBI
How Bread Making Has Changed
Most commercial bread contains bromides, added starches, refined sugars, added gluten (vital wheat gluten), preservatives, artificial flavorings, leveling agents, and stabilizers. Potassium bromate is an additive used in commercial bread and baked goods that make the products lighter and fluffier. Bromines are part of the halide family, a group of elements that includes fluorine, chlorine, and iodine, which are all endocrine disruptors that cause digestive issues and a host of other health problems.
Related: Sugar Leads to Depression – World’s First Trial Proves Gut and Brain are Linked (Protocol Included)
Baking Soda, baking powder, and cream of tartar are often used in place of yeast or in addition to rapid rise yeast to make the bread rise quickly and more uniformly. Modern bread rises for a couple of hours or less, whereas homemade bread traditionally takes at least 12 hours to rise. I got curious about the difference between baking soda and baking powder, and I thought you might be as well, hence the video below.
youtube
Traditional bread recipes typically utilized a few common ingredients including flour, yeast, salt, water, a sweetener, and some spices or herbs.
Related: Holistic Guide to Healing the Endocrine System and Balancing Our Hormones
Refined flours started to be widely used around 1880 which caused worldwide epidemics of pellagra and beriberi. Refining the flours removes bran and germ which increases shelf life. It also removed the B vitamins. Previous iterations of bread did use bolted or sifted flour which did refine the wheat somewhat, but it didn’t remove all of the bran, germ, and endosperm, and that flour was never bleached.
Bread with Whole Grains that are gently stone ground just before mixing the dough and then allowed to ferment slowly and naturally, in other words — authentic sourdough. That’s how the Egyptians made it 6,000 years ago.”
Bread was fundamentally redesigned. Refined flours, large quantities of commercial yeast, and a combination of additives and intense energy created the modern industrial bread. Fast mixing, fast rise, fast baking. Industrial bread is made far too fast.” – Mario Repetto
How Our Gut Biology Has Changed
We keep eating more and more sugar. In the early 1700s, the average sugar consumption was about 4 pounds a year. By 1800 we were at 18 pounds a year. By 1900 we were up to 60 pounds of sugar a year. Today the average American consumes between 130 and 150 pounds of sugar every year.
Sugar feeds pathogens. Our healthiest gut bacteria like the healthiest foods: vegetables and herbs. Nature wouldn’t work any other way; how could it? You’re probably thinking, “What about fruit?” We don’t eat the fruit we used to eat. Like wheat, our fruit has been radically altered through hybridization. But that’s another article (I’m working on it). For now, just Google “wild banana” or “what watermelon used to look like“.
We get way more sugar than our ancestors got even if we cut out refined foods. This causes an abundance of Candida. I believe Candida is prevalent in every single person with chronic illness. Everyone has yeast but when yeast is left unchecked they turn into pathogenic fungi. Tests for Candida aren’t accurate. Candida, when in it’s in the virulent fungal form, will make the gut more permeable. When this happens food proteins are absorbed into the body before they are digested. This causes allergies. This is one of the main causes of allergies, but there are others at play as well. In my experience, every single person who has cut refined sugar out of their lives and decreased their body’s Candida was able to rid themselves of seasonal, environmental, and food allergies. Every single time!
In addition to that, a study published in The Lancet showed that the candida protein HWP-1 is similar in structure to gluten.
A candida infection in the gut can cause an immune system reaction to HWP-1, which then stimulates an allergic reaction to the gluten in wheat and other grains and may trigger celiac disease in genetically susceptible people.” – Leyla Muedin, RD
Wheat proteins can also cause an immune response against the thyroid.
An obvious explanation is that the initial attack on the thyroid by anti-tTG autoantibodies of celiac leads to thyroid inflammation and presentation of TPO, with a second round of autoantibodies produced to TPO resulting in Hashimoto’s Thyroiditis.” – Dr. Art Ayers
Celiac disease and hypothyroidism beget more chronic autoimmune issues. Allergies lead to autoimmune disease. Allergies lead to chronic health issues. Medical science has established this. Medical science is just starting to understand the fact that a permeable gut causes allergies. Science also has established that an abundance of Candida causes a permeable gut. What they haven’t figured out yet is just how prevalent the permeable gut issue really is. But the bottom line is that our poor diet leads to allergies and almost all that commonly ails us.
Suggestions
If you have a healthy gut, make your own sourdough bread using heirloom wheat and the old-school practices. If you have any chronic illness, then you do not have a healthy gut. Here’s how you fix it. If you’re not well, wait until you get well before consuming any kind of bread. And don’t think of old-fashioned bread as healthy. Vegetables are healthy. Bread is at its best a neutral food with some health benefits and easy calories that can help sustain life like brown rice and millet. Vegetables and herbs heal the body.
Obviously, stay the heck away from poisons! Glyphosate is a cocktail of poisons. Science has firmly established this. And avoid GMOs as well. They weren’t designed with our health in mind, they were designed for profit, and in most cases, to sell more Roundup.
The hard truth is that letting companies cook your food for you leads to poor health. People often ask me, “If you can cure cancer why aren’t you rich?” If I could cure cancer and figure out how to do it while still eating refined, prepackaged, and processed foods that we humans have grown accustomed to, I would be rich. But people would rather die for convenience food than give it up. Obviously. We see this everywhere.
Being well long-term means preparing all your own food yourself the right way, or being rich and hiring someone else to do it. There is no shortcut. Certainly not with bread.
Sources:
Your Ancestors Didn’t Eat The Same Type Of Wheat That You Do (And They Were Healthier) – Off The Grid News
4 Ways Modern Bread is Different From Traditional Bread – Our Heritage of Health
The Real Problem With Bread (It’s Probably Not Gluten) – Mother Jones
Problems Linked to Monsanto’s RoundUp – EcoWatch
15 Health Problems Linked to Monsanto’s Roundup – EcoWatch
Consumption of Sugar – Sugar and Sweetener Guide
Gluten Intolerance, Wheat Allergies, and Celiac Disease – It’s More Complicated Than You Think was originally published on Organic Lifestyle Magazine
3 notes
·
View notes
Text
How Physiotherapists In Lusaka Can Easily Solve Your Pain
Physiotherapists in Lusaka/physiatrists in Lusaka play a vital part in the health care of persons of all ages who have lost movement or capacity as a result of an accident or disease, assisting them in returning to an active and independent life as quickly as possible. Their research focuses on the prevention, treatment, and relief of a variety of illnesses. Gross motor development, postural management, hydrotherapy, orthotic assessment and monitoring, sensory integration, respiratory disorders, orthopedic concerns, and horseback riding for people with special needs are all areas where physiotherapists operate. Physical therapists, sometimes known as a physiatrist, assist wounded or ill persons in regaining mobility and managing pain. Patients with chronic ailments, illnesses, or injuries commonly rely on these professionals for rehabilitation, treatment, and prevention. Physiotherapists operate as part of a multi-disciplinary team with health care organizations. Evaluate and investigate the impact of sickness, disability, injury, and inactivity on functional ability. Exercising, moving, electrotherapy, and mobilization are all used to treat patients. Patients and caregivers should be educated and advised.

Physical Therapists' Responsibilities:
Physical therapists help patients of all ages who are suffering from back and neck injuries, sprains, strains, fractures, arthritis, amputations, neurological diseases including stroke or cerebral palsy, work and sports-related injuries, and other conditions. Physical therapists are trained to treat their patients using a range of approaches. Exercises, functional movement training, which may include the use of equipment such as canes, crutches, wheelchairs, and walkers, particular movements of joints, muscles, and other soft tissue to enhance movement and reduce discomfort are some of the approaches used.
Physiotherapists in Lusaka commonly perform the following tasks:
· Examine the patient's medical history, any referral notes from doctors, surgeons, or other healthcare professionals.
· Develop tailored patient care plans that outline the patients' goals and the plans' predicted outcomes.
· Create tailored patient care plans that include the patients' goals as well as the plans' predicted outcomes.
· To relieve pain, promote mobility, prevent further pain or injury, and facilitate health and wellness, use exercises, stretching motions, hands-on therapy, and equipment.
· Evaluate and record a patient's progress, adjusting a treatment plan as needed, and experimenting with novel treatments.
· Use exercises, stretching motions, hands-on therapy, and equipment to reduce pain, enhance mobility, prevent further pain or injury, and facilitate health and wellness.
Physical therapists' tasks differ depending on the patient. A patient healing from a stroke, for example, requires different treatment than a patient recovering from a sports injury. Some physical therapists specialize in a specific area of care such as orthopedics or geriatrics, for example. Many physical therapists also assist patients in maintaining or improving mobility by establishing fitness and wellness programs that encourage patients to live healthier and more active lives. Physical therapists supervise the work of physical therapist assistants and aides and confer with physicians, surgeons, and other experts as part of a healthcare team.
What problems do physiotherapists treat?
Physiotherapists concentrate on prevention as well as rehabilitation. Injuries, diseases, and disabilities can all result in treatment. Some instances are as follows:
· Neck and back discomfort is caused by muscle and bone abnormalities.
· Arthritis and the after-effects of amputation are examples of problems in the bones, joints, muscles, and ligaments.
· Asthma and other lung diseases
· As a result of heart difficulties, you've been disabled.
· Childbirth-related pelvic concerns, such as bladder and bowel problems
· Mobility loss is a result of brain or spine injuries or disorders like Parkinson's disease and multiple sclerosis.
· Fatigue, discomfort, edema, stiffness, and loss of muscle strength are common side effects of cancer treatment and palliative care.
Benefits of Physical Therapy:
Physical therapy helps people of all ages who have medical issues, disabilities, or accidents that make it difficult for them to travel and function on a daily basis. A customized physical therapy program can help people regain their prior level of function while also facilitating habits and lifestyle changes that can help them avoid further injury and enhance their overall health and well-being. Physical therapy is also a classic technique to issue management that primary care physicians send patients to at the first sign of a problem.
Reduce or eliminate pain:
Joint and soft tissue mobilization, therapies like ultrasound, taping, or electrical stimulation, may assist relieve discomfort and restore muscle and joint function to reduce pain. Such treatments may also help to prevent the recurrence of discomfort.
Avoid taking a certain activity:
If physical therapy helps you get rid of pain or heal from an accident, surgery may not be necessary. Even if surgery is required, you can benefit from physical therapy before surgery. In certain circumstances, going into surgery healthier and in better shape will help you heal faster afterward. Often, avoiding surgery lowers healthcare expenses.
Increasing adaptability:
If you have trouble standing, walking, driving, physical therapy can assist, regardless of your age. Stretching and strengthening exercises might help you restore your mobility. Physical therapists can properly fit clients with a cane, crutches, or other assistive equipment, as well as do orthotic medication testing. By developing an individual care plan, any activity that is crucial to a person's life can be practiced and modified to provide maximum efficiency and protection.
Getting back on your feet after a stroke:
It's typical to lose some function and motion after a stroke. Physical therapy aids in the stabilization of weaker body components, the improvement of gait and balance. Physical therapists can also help stroke patients, improve their ability to walk and move around in bed, allowing them to be more self-sufficient at home.
Stop or recover from a sports injury:
Physical therapists are aware of how participating in several sports might increase the risk of certain ailments. They can design appropriate rehabilitation or prevention exercise regimens for you to ensure a healthy return to your sport.
0 notes
Link
Many people who have suffered from the effects of this disease might now be at risk of long-term impairment which is unknown yet, but a rehabilitation program for the covid-19 patient is to reduce the impact of COVID-19 on the health and function of people.
The rehabilitation program includes:
Pulmonary rehabilitation
Cognitive rehabilitation
Mental health support
Complications of COVID-19
COVID-19 can affect the body in a variety of ways. While 81% of people experience mild to moderate symptoms and recover without treatment, 14% develop severe symptoms that can last several weeks or months.
Lung damage
Heart damage or inflammation, such as myocarditis or pericarditis
Cognitive impairments that affect memory or concentration
Conditions that affect the blood vessels, such as clotting
Lasting effects from complications, such as heart attacks, stroke, or pulmonary embolism
The mental effects such as anxiety, depression, or trauma
Muscle or joint pain
Chronic fatigue in the body
Pulmonary rehabilitation:
The very 1st symptom of COVID-19 is decreased Oxygen level, shortness of breath, these can have long-term effects on lung function. Chronic illness can affect the lungs, such as chronic obstructive pulmonary disease.
Pulmonary rehabilitation through respiratory yoga therapy and respiratory physiotherapy helps in
Reducing shortness of breath
Improving lung capacity
Managing any respiratory complications
Reducing the impact of respiratory symptoms on mental health
Specific interventions through Yoga can ease symptoms such as coughing, wheezing, and shortness of breath. Breathing exercises (Pranayama) include
Training to adjust someone’s breathing rhythm
Techniques to strengthen the breathing muscles
Expectoration training, which helps someone clear mucus from the airways
Treatments through Naturopathy and Ayurveda:
Hydrotherapy – Asthma bath, Hot Foot and Arm Bath
Acupuncture
Uro Vasti
Cognitive rehabilitation:
COVID-19 can also impact the nervous system, including the brain.
Symptoms:
Memory problems
Trouble concentrating
Brain fog
Dramatic mood changes
A loss of taste or smell
People with severe COVID-19 may also experience cognitive changes. Up to 80% of people who receive ventilation can experience delirium, which can include hallucinations. For critically ill patients who do not need ventilation, the condition affects 20–40%.
Cognitive rehabilitation therapy (CRT) can help manage or potentially recover hallucinations.
CRT helps to strengthen cognitive abilities. This may include:
Memory training
Speech therapy
Mental exercises
Psychological support for people who feel confused or disoriented
Yogic intervention in Cognitive Rehabilitation:
Treatments:
Deep Relaxation Techniques
Yoga Nidra
AUM-kara Meditation
AUM-kara Chanting
Simhasana
Bhramari Pranayam
Bhasthrika
Kapalbhati
Mental health support:
Patients who spent long days in the hospital are prone to psychological trauma. Trauma may cause anxiety, depression, or disassociation, which refers to a feeling of disconnection from a person’s thoughts, feelings, or experiences also.
It is important to accept that it will take time to recover physically and psychologically. It can be useful to set small realistic goals to help you see your progress and feel better about yourself.
Natural Therapy Treatments:
Psychological Counseling
Hypnotherapy
Raga therapy
Energy Healing
Activities that ease stress and anxiety, such as yoga or mindfulness
0 notes
Text
Epigenetics Drugs and Diagnostic Technologies Market 2020-2025| Comprehensive Study COVID19 Impact
Epigenetics Drugs and Diagnostic Technologies Market is valued at USD 7.71 Billion in 2018 and expected to reach USD 27.13 Billion by 2025 with the CAGR of 19.68% over the forecast period.
Growing prevalence of oncological and non-oncological conditions like respiratory diseases, alzheimer disease and growing R & D investments in the healthcare industries promotes the growth of global epigenetics drugs and diagnostic technologies market.
Epigenetics is a study of heritable variations in gene expression; it is a trait change without genotype alteration. Epigenetic change is a normal and natural phenomenon but can also be affected by a variety of factors like age, environment or lifestyle and disease state. New and ongoing work continues to uncover the role of epigenetics in a variety of human disorders and fatal diseases. Many diseases are affected by epigenetic processes, including cancer, heart disease, diabetes and mental illnesses. Epigenetic therapy provides a potential way to directly influence those pathways. Epigenetic drugs and diagnostics are used in early stage cancer screening, as well as other pathological modifications in skin cells, liver cells, brain cells and others. Epigenetic test kits are used to diagnose diseases due to early-stage epigenetic changes and during therapy to verify the therapeutic efficacy. They work by involving modification-specific monoclonal antibodies, based on immunoprecipitation. Epigenetic drugs belong to a group of medications which are used to treat different cancers and other diseases like respiratory diseases, alzheimer disease. Those drugs fall into two groups which are methylation inhibitors of DNA and inhibitors of histone deacetylase. There are seven cancer care drugs have been licensed by the FDA. Also epigenetic drugs used in sensitization of chemotherapy, radiotherapy, and modulation of immune system.
The global epigenetics drugs and diagnostic technologies market is segmented on the basis of product, type of therapy, technology, application and region and country level. On the basis of product, the global epigenetics drugs and diagnostic technologies market is segmented into reagents, kits, instruments, enzymes and services. Based on type of therapy, the epigenetics drugs and diagnostic technologies market is classified into histone deacetylase (HDAC) inhibitors and DNA methyltransferase (DNMT) inhibitors. On the basis of technology, the global epigenetics drugs and diagnostic technologies market is segmented into DNA methylation, histone methylation, histone acetylation, large non-coding RNA, microRNA modification and chromatin structures. On the basis of application, the global epigenetics drugs and diagnostic technologies market is segmented into oncology and non-oncology.
The regions covered in global Epigenetics Drugs and Diagnostic Technologies Market report are North America, Europe, Asia-Pacific and Rest of the World. On the basis of country level, global Epigenetics Drugs and Diagnostic Technologies Market sub divided in U.S., Mexico, Canada, U.K., France, Germany, Italy, China, Japan, India, South East Asia, GCC, Africa, etc.
Epigenetics Drugs and Diagnostic Technologies Companies
Global Epigenetics Drugs and Diagnostic Technologies Market reports cover prominent players,
Zymo research
CellCentric Ltd
Thermo Fisher Scientific
Abcam, Eisai Co. Ltd
Diagenode
Merck
Elli Lilly
Syndax Pharmaceuticals, Inc.
Qiagen
Chroma Therapeutics Ltd
Novartis International AG
Oncolys Biopharma Inc
Sigma-Aldrich Corporation
Valirx Plc
others.
Global Epigenetics Drugs and Diagnostic Technologies Market Dynamics –
The key factor responsible for the growth of the epigenetics drugs and diagnostic technologies market is growing prevalence of oncological and non-oncological conditions like respiratory diseases, alzheimer’s disease. Cancer is a leading cause of death for children and adolescents worldwide and about 300,000 children aged 0 to 19 are diagnosed with cancer every year. More than 80 % of children with cancer are cured in high-income countries but only around 20 % are cured in many low- and middle-income countries. Cancer is the world's second leading cause of death, and is responsible for estimated deaths of 9.6 million in 2018. Overall, cancer causes about 1 in 6 deaths. In low- and middle-income countries, approximately 70 % of cancer deaths occur. Tobacco use is the most important risk factor for cancer, and is responsible for about 22% of deaths from cancer. According to WHO more than 3 million people die each year from COPD, an estimated 6% of all deaths worldwide.
Another factor which drives the epigenetics drugs and diagnostic technologies market is growing R & D investments in the healthcare industries. Pharmaceutical industries spent nearly USD 179.55 Billion on research and development. While spending on marketing in healthcare industry in 2016 was around USD 31 Billon. Nonetheless, Quality-related problems and lack of knowledge are likely to restrain the epigenetics drugs and diagnostic technologies market to certain extent. Introduction of technologically advanced products will create new opportunities for epigenetics drugs and diagnostic technologies market over the forecast period.
Epigenetics Drugs and Diagnostic Technologies Market Regional Analysis –
North America dominates the global market owing to factors such as high prevalence of cancer, increased support for R&D. In 2019, the United States was spent around 581 billion U.S. dollars into research and development according to Statisca. More than 25 million people have asthma in the United States, About 14.8 million adults have been diagnosed with COPD and about 12 million people have not yet been diagnosed with COPD in 2019.
The Asia Pacific is the expected to emerge as the fastest-growing epigenetics drugs and diagnostic technologies market due to significant number of cancer, diabetes and other chronic diseases with related unmet medical needs. In 2016, there were around 3.8 million new cases of and 2.3 million deaths caused by malignant tumors. That is, 7 people were diagnosed with cancer on average while 4 people died from cancer every minute in China.
Key Benefits for Epigenetics Drugs and Diagnostic Technologies Market reports –
Global Epigenetics Drugs and Diagnostic Technologies Market report covers in depth historical and forecast analysis.
Global Epigenetics Drugs and Diagnostic Technologies Market research report provides detail information about Market Introduction, Market Summary, Global market Revenue (Revenue USD), Market Drivers, Market Restraints, Market opportunities, Competitive Analysis, Regional and Country Level.
Global Epigenetics Drugs and Diagnostic Technologies Market report helps to identify opportunities in market place.
Global Epigenetics Drugs and Diagnostic Technologies Market report covers extensive analysis of emerging trends and competitive landscape.
Epigenetics Drugs and Diagnostic Technologies Market Segmentation –
By Product: Reagents, Kits, Instruments, Enzymes, Services
By Type of Therapy: Histone Deacetylase (HDAC) Inhibitors, DNA Methyltransferase (DNMT) Inhibitors
By Technology: DNA Methylation, Histone Methylation, Histone Acetylation, Large Non-Coding RNA, MicroRNA Modification, Chromatin Structures
By Application: Oncology, Non-Oncology
Regional & Country Analysis
North America, U.S., Mexico, Canada , Europe, UK, France, Germany, Italy , Asia Pacific, China, Japan, India, Southeast Asia, South America, Brazil, Argentina, Columbia, The Middle East and Africa, GCC, Africa, Rest of Middle East and Africa
About Us:
Brandessence Market Research and Consulting Pvt. ltd.
Brandessence market research publishes market research reports & business insights produced by highly qualified and experienced industry analysts. Our research reports are available in a wide range of industry verticals including aviation, food & beverage, healthcare, ICT, Construction, Chemicals and lot more. Brand Essence Market Research report will be best fit for senior executives, business development managers, marketing managers, consultants, CEOs, CIOs, COOs, and Directors, governments, agencies, organizations and Ph.D. Students. We have a delivery center in Pune, India and our sales office is in London.
Contact us at: +44-2038074155 or mail us at [email protected]
0 notes
Text
How does Mental Health Affect Physical health
The link between mental state and physical health is usually misunderstood. They’re often considered as separate entities, but the two goes hand in hand. World Health Organization defines health as a state of complete physical, mental and social well-being.
The perceived disconnect between “mind” and “body” creates the misunderstanding that mental disease isn't a physical disease. Actually, mental state has a direct impact on your physical health. So it is advised to visit Best Clinical Psychologist in Mumbai.
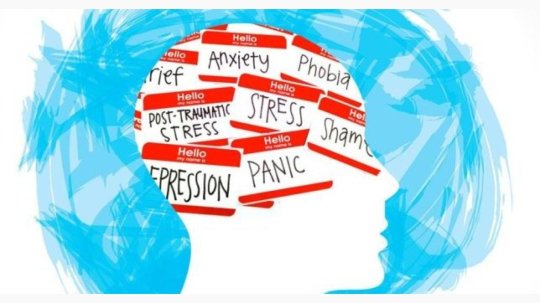
UNDERSTANDING Mental Health
Contrary to popular belief, mental disease isn't rare. Almost one in five adults has a mental disease in any given year. Mental disease ranges widely in issue and severity, from anxiety and depression to eating disorders and schizophrenia.
Any given mental disease can affect your body’s ability to function properly and should even reduce anticipation. A 2014 study from Oxford University found that several mental illnesses can reduce anticipation by up to twenty years, the equivalent of heavy smoking. If you are going through breakup issue, it also effects the mental health and your physical health. So it’s better to take Breakup Counselling.
While mental disease is taken into account a significant issue today, Mental state is usually overlooked among other physical health issues.
Many folks aren't conscious of how common mental disease is. Mental disease is quite just being depressed. It covers a good range of problems, spanning from ones that affect mood to people who affect thinking or behavior. Examples include:
Depression
Anxiety disorders
Schizophrenia
Eating disorders
Bipolar depression
Addictive behaviors
CONNECTING THE MIND AND BODY
So, you would possibly be wondering, exactly how does my mental state affect my physical health? Well, poor mental state can affect your ability to form healthy decisions and repel chronic diseases.
Neglecting your mental state can cause more serious health complications such as:
Heart disease
High vital sign
Weakened system
Asthma
Obesity
Gastronomical problems
Premature death
Depression alone can cause chronic fatigue, insomnia and increased sensitivity to aches and pains thanks to abnormal function of neurotransmitters within the brain. So it’s better to take counselling. Nowadays you can even take Online Breakup Counseling.
TIPS TO HELP YOU CREATE A HEALTHY BODY AND MIND
Just taking care of your mind isn’t the simplest thanks to maintain or improve your mental state . Here are some ways you'll improve your mental and physical health
Exercise regularly. Exercise can release feel-good brain chemicals like endorphins and serotonin which will ease depression and anxiety. Choose a program or sort of exercise that works for you. this might be cardio-intense interval training or a more mindful and intention-driven yoga practice or something in between. What’s key's that you simply stick with it.
Eat a healthy diet. Diets loaded with processed, high-calorie and low-nutrient foods are linked with increased depression and anxiety. Avoid skipping meals, which may cause fatigue and unhealthy snacking. attempt to include fruits, vegetables, nuts, whole grains, fish and healthy fats, like avocados, into your meals. this may be helpful for increased brain function.
Maintain a traditional sleep schedule. Not getting enough sleep has been linked with depression, anxiety and stress. the advice for adults is seven or more hours of sleep per night. If you’re having trouble falling and staying asleep, try one among the following:
Relaxing before bed,
Lowering your caffeine intake
Setting a stricter schedule for bedtime
Get support. If you are going through relationship problems,you should take Online Couples Counselling. Your social circle is additionally an important aspect to preventing a decline in mental state. But mental state is often a difficult topic to debate with peers. This often prevents people from seeking help. Don’t be afraid to succeed in bent friends and family for support.
DON’T WAIT TO GET HELP
In many cases, people go to a mental health expert only after a crisis has occurred. Getting help earlier can prevent mental state conditions, like depression and anxiety, from developing.
If you're experiencing symptoms of any mental state condition, it's important to contact a medical professional who can assist you . Eating right and exercising can help some people improve their mental state. However, others may have medication or counselling to ascertain changes. By talking to a doctor, you'll be better ready to determine what’s right for you.
If you are looking for counselling online like Breakup Counselling Online, or even if you prefer going physically for counselling, you should visit The Thoughts CO.
#Breakup Counselling Online#Online Breakup Counseling#Online Couples Counselling#Breakup Counselling#Best Clinical Psychologist in Mumbai
0 notes
Text
IMPACT OF MENTAL HEALTH AT PHYSICAL HEALTH
Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. It also helps determine how we handle stress, relate to others, and make choices. Mental health is important at every stage of life, from childhood and adolescence through adulthood.
Mental health and physical health are closely connected. Mental health plays a major role in people’s ability to maintain good physical health. Mental illnesses, such as depression and anxiety, affect people’s ability to participate in health-promoting behaviors. In turn, problems with physical health, such as chronic diseases, can have a serious impact on mental health and decrease a person’s ability to participate in treatment and recovery.
Connecting the mind and body
So, you might be wondering, exactly how does my mental health affect my physical health? Well, poor mental health can affect your ability to make healthy decisions and fight off chronic diseases.
What’s more, neglecting your mental health can lead to more serious health complications such as:
Heart disease
High blood pressure
Weakened immune system
Asthma
Obesity
Gastronomical problems
Premature death
Depression alone can cause chronic fatigue, insomnia and increased sensitivity to aches and pains due to abnormal function of neurotransmitters in the brain.
Buy medicines and healthcare products online at a reasonable cost.
How mental health affects physical health
There are various ways in which poor mental health has been shown to be detrimental to physical health.
People with the highest levels of self-rated distress (compared to lowest rates of distress) were 32% more likely to have died from cancer.1,2 Depression has been found to be associated with an increased risk of coronary heart disease3
Schizophrenia is associated with:
double the risk of death from heart disease
three times the risk of death from respiratory disease.
This is because people with mental health conditions are less likely to receive the physical healthcare they're entitled to. Mental health service users are statistically less likely to receive the routine checks (like blood pressure, weight and cholesterol) that might detect symptoms of these physical health conditions earlier. They are also not as likely to be offered help to give up smoking, reduce alcohol consumption and make positive adjustments to their diet.
Lifestyle Factors
These lifestyle factors can influence the state of both your physical and mental health.
Exercise
Physical activity in any form is a great way to keep you physically healthy as well as improving your mental wellbeing. Research shows that doing exercise influences the release and uptake of feel-good chemicals called endorphins in the brain. Even a short burst of 10 minutes brisk walking increases our mental alertness, energy and positive mood. Read the Let's Get Physical report for more on the positive health benefits of physical activity.
Physical activity means any movement of your body that uses your muscles and expends energy. From tending your garden to running a marathon, even gentle forms of exercise can significantly improve your quality of life.

Diet
Good nutrition is a crucial factor in influencing the way we feel. A healthy balanced diet is one that includes healthy amounts of proteins, essential fats, complex carbohydrates, vitamins, minerals and water. The food we eat can influence the development, management and prevention of numerous mental health conditions including depression and Alzheimer's. Read about the ways in which you can ensure you are getting a balanced diet.

Smoking
Smoking has a negative impact on both mental and physical health. Many people with mental health problems believe that smoking relieves their symptoms, but these effects are only short-term.
People with depression are twice as likely to smoke as other people.
People with schizophrenia are three times as likely to smoke as other people.
Nicotine in cigarettes interferes with the chemicals in our brains. Dopamine is a chemical which influences positive feelings, and is often found to be lower in people with depression. Nicotine temporarily increases the levels of dopamine, but also switches off the brain's natural mechanism for making the chemical. In the long term, this can make a person feel as though they need more and more nicotine in order to repeat this positive sensation.

Long-term health conditions and mental health
The promotion of positive mental health can often be overlooked when treating a physical condition. Psoriasis is one such condition in which the effects go beyond the visual signs and symptoms, impacting psychological wellbeing and quality of life.
#Psoriasis:
Psoriasis is a condition which is commonly characterized by red flaky sores on the surface of the skin, but its effects go beyond the visual signs and symptoms.
Psoriasis is an auto-immune condition commonly triggered by stress. It affects 1.8 million people in the UK and can impact on emotional as well as physical wellbeing.
Up to 85% feel annoyance with their psoriasis
Approximately one third experience anxiety and depression
1 in 10 admit to contemplating suicide
1 in 3 experience feelings of humiliation about their condition
1 in 5 report being rejected (and stigmatized) as a result of their condition
1/3 experience problems with loved ones.
Yet, a recent report from the British Association of Dermatologists (BAD) highlighted that only 4% of Dermatology Units have access to a counsellor.
3MEDS is a online medicine app in Delhi, which delivers medicines 24x7 at your doorstep.
The physical and psychological impacts can be cyclically linked: the condition can cause emotional distress which can trigger a psoriasis flare and, as a result, cause further distress.
Some people with psoriasis can feel that their GP regards psoriasis as a minor skin complaint and are dismissive of the emotional aspects, leaving many to continue unaided on the isolating and emotional journey associated with psoriasis.
Conclusion:
The physical health of mentally ill patients should be part of the field of action of psychiatric practitioners. Health consists of physical, mental, and social aspects, consideration of all three aspects is very essential; change in one aspect will lead to distortion of health.
0 notes
Text
Biomed Grid | The Impact of Stress, Anxiety, Fear and Depression in The Cause of Cancer in Humans
IntroductionDepression, Anxiety, Stress and Fear
Depression is a state of low mood and aversion to activity that can affect a person’s thoughts, behavior, feelings, and sense of well-being. A depressed mood is a normal temporary reaction to life events such as loss of a loved one. It is also a symptom of some physical diseases and a side effect of some drugs and medical treatments. Depressed mood is also a symptom of some mood disorders such as major depressive disorder or dysthymia [1].
Anxiety is an emotion characterized by an unpleasant state of inner turmoil, often accompanied by nervous behavior, such as pacing back and forth, somatic complaints, and rumination [2]. It is the subjectively unpleasant feelings of dread over anticipated events, such as the feeling of imminent death [3]. Anxiety is not the same as fear, which is a response to a real or perceived immediate threat, whereas anxiety is the expectation of future threat [4]. Anxiety is a feeling of uneasiness and worry, usually generalized and unfocused as an overreaction to a situation that is only subjectively seen as menacing. It is often accompanied by muscular tension, restlessness, fatigue and problems in concentration. Anxiety can be appro priate, but when experienced regularly the individual may suffer from an anxiety disorder [5].
In psychology, stress is a feeling of strain and pressure. Also, this is one type of psychological pain [6]. Small amounts of stress may be desired, beneficial, and even healthy. Positive stress helps improve athletic performance. It also plays a factor in motivation, adaptation, and reaction to the environment. Excessive amounts of stress, however, may lead to bodily harm. Stress can increase the risk of strokes, heart attacks, ulcers, dwarfism, and mental illnesses such as depression [7].
Fear is a feeling induced by perceived danger or threat that occurs in certain types of organisms, which causes a change in metabolic and organ functions and ultimately a change in behavior, such as fleeing, hiding, or freezing from perceived traumatic events. Fear in human beings may occur in response to a specific stimulus occurring in the present, or in anticipation or expectation of a future threat perceived as a risk to body or life. The fear response arises from the perception of danger leading to confrontation with or escape from/avoiding the threat (also known as the fight-or-flight response), which in extreme cases of fear (horror and terror) can be a freeze response or paralysis [8].
In humans and animals, fear is modulated by the process of cognition and learning. Thus fear is judged as rational or appropriate and irrational or inappropriate. An irrational fear is called a phobia. Psychologists such as John B. Watson, Robert Plutchik, and Paul Ekman have suggested that there is only a small set of basic or innate emotions and that fear is one of them. This hypothesized set includes such emotions as acute stress reaction, anger, angst, anxiety, fright, horror, joy, panic, and sadness. Fear is closely related to, but should be distinguished from, the emotion anxiety, which occurs as the result of threats that are perceived to be uncontrollable or unavoidable. The fear response serves survival by generating appropriate behavioral responses, so it has been preserved throughout evolution [9].
Cortisol and Epinephrine
Cortisol is a steroid hormone, in the glucocorticoid class of hormones. It is produced in humans by the zona fasciculata of the adrenal cortex within the adrenal gland [10]. It is released in response to stress and low blood-glucose concentration. It functions to increase blood sugar through gluconeogenesis, to suppress the immune system, and to aid in the metabolism of fat, protein, and carbohydrates [11].
Epinephrine, also known as adrenalin or adrenaline, is a hormone, neurotransmitter, and medication [12,13]. Epinephrine is normally produced by both the adrenal glands and certain neurons. It plays an important role in the fight-or-flight response by increasing blood flow to muscles, output of the heart, pupil dilation, and blood sugar [14,15]. It does this by binding to alpha and beta receptors. It is found in many animals and some single cell organisms [16,17].
The Immune System, Cytokines, and Inflammation
mounting a rapid innate immune system and inflammatory response to a specific trigger and then down regulating the response once a pathogen has been cleared are critical for resolving infection, repairing tissue damage, and returning the body to a state of homeostasis. Recently, however, evidence has accumulated showing that when activation of the inflammatory response is altered or prolonged, it can actually cause more damage to a host than the pathogen itself. Indeed, it is now widely recognized that chronic inflammation plays a role in several major diseases including asthma, arthritis, diabetes, obesity, atherosclerosis, certain cancers, and Alzheimer’s disease. One factor that can alter adaptive innate immune system responding and prolong inflammation is stress. In this review, therefore, we consider how stress influences the regulation of inflammation in a way that may be relevant for depression.
The immune system plays a critical role in keeping the body biologically healthy, especially during times of physical injury, wounding, and infection. A key component of this system is the inflammatory response, which is mediated by pro-and anti-inflammatory cytokines that identify, neutralize, and eliminate foreign pathogens such as bacteria and viruses. Inflammation is regulated most proximally by the expression of immune response genes including IL1B, IL6, and TNF. When activated, these genes promote the secretion of pro-inflammatory cytokines that mediate systemic inflammation. Inflammation is also regulated more distally by processes occurring in the brain, which detects social-environmental cues indicating possible danger. This neuro-inflammatory link is highly adaptive insofar as it can activate the CTRA before a physical injury or bacterial infection takes place. A downside of central regulation of systemic inflammation, however, is that it gives social, symbolic, and anticipated threats—including those that have not yet happened or that may never actually occur—the ability to activate the CTRA in the absence of actual physical threat. Under normal conditions, the SNS up-regulates CTRA-related inflammatory activity via stimulation of β-adrenergic receptors, and the HPA axis downregulates CTRA-related inflammatory activity via the production of cortisol. However, under conditions of prolonged actual or perceived threat, or possibly during acute stressors indicating social threat or physical danger, glucocorticoid resistance can develop, leading to excessive inflammation that increases a person’s risk for several disorders including depression, especially if activation of these pathways is prolonged.
Materials and Methods
Cortisol can weaken the activity of the immune system. It prevents proliferation of T-cells by rendering the interleukin-2 producer T-cells unresponsive to interleukin-1 (IL-1), and unable to produce the T-cell growth factor (IL-2). Cortisol also has a negative- feedback effect on interleukin-1 [18].
Though IL-1 is useful in combating some diseases, endotoxic bacteria have gained an advantage by forcing the hypothalamus to increase cortisol levels (forcing the secretion of corticotropin-releasing hormone, thus antagonizing IL-1). The suppressor cells are not affected by glucosteroid response-modifying factor [19], so the effective setpoint for the immune cells may be even higher than the setpoint for physiological processes (reflecting leukocyte redistribution to lymph nodes, bone marrow, and skin). Rapid administration of corticosterone (the endogenous type I and type II receptor agonist) or RU28362 (a specific type II receptor agonist) to adrenalectomized animals induced changes in leukocyte distribution. Natural killer cells are affected by cortisol [20].
Cortisol stimulates many copper enzymes (often to 50% of their total potential), probably to increase copper availability for immune purposes. This includes lysyl oxidase, an enzyme that cross-links collagen, and elastin. Especially valuable for immune response is cortisol’s stimulation of the superoxide dismutase, [21] since this copper enzyme is almost certainly used by the body to permit superoxides to poison bacteria.
Cortisol counteracts insulin, contributes to hyperglycemia-causing hepatic gluconeogenesis [22] and inhibits the peripheral use of glucose (insulin resistance) by decreasing the translocation of glucose transporters (especially GLUT4) to the cell membrane [23]. However, cortisol increases glycogen synthesis (glycogenesis) in the liver [24]. The permissive effect of cortisol on insulin action in liver glycogenesis is observed in hepatocyte culture in the laboratory, although the mechanism for this is unknown [25,26].
As a hormone, epinephrine acts on nearly all body tissues. Its actions vary by tissue type and tissue expression of adrenergic receptors. For example, high levels of epinephrine causes smooth muscle relaxation in the airways but causes contraction of the smooth muscle that lines most arterioles.
Epinephrine acts by binding to a variety of adrenergic receptors. Epinephrine is a nonselective agonist of all adrenergic receptors, including the major subtypes α1, α2, β1, β2, and β3 [27]. Epinephrine’s binding to these receptors triggers a number of metabolic changes. Binding to α-adrenergic receptors inhibits insulin secretion by the pancreas, stimulates glycogenolysis in the liver and muscle [28], and stimulates glycolysis and inhibits insulin-mediated glycogenesis in muscle [29,30]. β adrenergic receptor binding triggers glucagon secretion in the pancreas, increased adrenocorticotropic hormone (ACTH) secretion by the pituitary gland, and increased lipolysis by adipose tissue. Together, these effects lead to increased blood glucose and fatty acids, providing substrates for energy production within cells throughout the body [31].
Its actions are to increase peripheral resistance via α1 receptor- dependent vasoconstriction and to increase cardiac output via its binding to β1 receptors. The goal of reducing peripheral circulation is to increase coronary and cerebral perfusion pressures and therefore increase oxygen exchange at the cellular level. While epinephrine does increase aortic, cerebral, and carotid circulation pressure, it lowers carotid blood flow and end-tidal CO2 or ETCO2 levels. It appears that epinephrine may be improving macrocirculation at the expense of the capillary beds where actual perfusion is taking place [32].
George M. Slavich and Michael R. Irwin in 2014 concluded that we know a lot about the adverse social-environmental conditions that typically precipitate depression and about cognitive and emotional processes that mediate these effects. With the advent of new neuroimaging, immunological, and genome-wide profiling techniques, we are now poised to go one step deeper and elucidate the full set of biological mechanisms that link stress with depression. Inflammation is undoubtedly a key player in this link. As we have discussed, two general phenomena are consistent with the hypothesis that stress-related increases in inflammation are involved in depression. First, a large number of naturalistic and laboratory- based experimental studies have shown that stress is a potent activator of inflammation, and second, it is now well known that vaccinations and immunological challenges that up-regulate inflammatory activity evoke depressive-like behaviors in rodents and clinically significant episodes of depression in at least some people. In addition, these challenges have been shown to up-regulate peripheral and central cytokine production and to alter metabolic and neural activity in brain regions that have been implicated in depression. Many questions remain unanswered regarding these effects, including whether inflammation is necessary or sufficient for all cases of MDD.
Nonetheless, based on existing data, we conclude that stress likely increases risk for depression in a substantial number of people by up-regulating inflammatory activity and by altering social, cognitive, and affective processes that are known to promote this disorder. These insights are important because they can help update contemporary theories of depression with information about biological mechanisms that are involved in the pathogenesis of MDD. For the potential of these insights to be fully realized, they will need to be translated into new strategies for modifying processes that promote depression (Sanislow et al., 2010). At a very general level, such processes include neurocognitive mechanisms like negative cognitive appraisals and neural sensitivity to social threat, which have been associated with inflammation and depression; immunological processes such as preclinical levels of inflammation, which could presage the development of chronic inflammation and disease; and psychosocial factors such as parental behaviors, which have been found to influence the effects of social-environmental adversity on proinflammatory signaling. The hope is that by targeting these and other dynamics, we may one day be able to reduce the prevalence of depression and the substantial financial burden and personal suffering associated with this common and costly disorder [33].
Sheldon Cohen et al. [34] did a research about stress and disease promotion. In Cohen’s first study, after completing an intensive stress interview, 276 healthy adults were exposed to a virus that causes the common cold and monitored in quarantine for five days for signs of infection and illness. Here, Cohen found that experiencing a prolonged stressful event was associated with the inability of immune cells to respond to hormonal signals that normally regulate inflammation. In turn, those with the inability to regulate the inflammatory response were more likely to develop colds when exposed to the virus. In the second study, 79 healthy participants were assessed for their ability to regulate the inflammatory response and then exposed to a cold virus and monitored for the production of pro-inflammatory cytokines, the chemical messengers that trigger inflammation. He found that those who were less able to regulate the inflammatory response as assessed before being exposed to the virus produced more of these inflammation-inducing chemical messengers when they were infected. The immune system’s ability to regulate inflammation predicts who will develop a cold, but more importantly it provides an explanation of how stress can promote disease, when under stress, cells of the immune system are unable to respond to hormonal control, and consequently, produce levels of inflammation that promote disease. Because inflammation plays a role in many diseases such as cardiovascular, asthma and autoimmune disorders, this model suggests why stress impacts them as well [34].
Michopoulos V. et al. [35] concluded that the study of inflammation in fear- and anxiety-based disorders has gained interest as growing literature indicates that pro-inflammatory markers can directly modulate affective behavior. Indeed, heightened concentrations of inflammatory signals, including cytokines and C-reactive protein, have been described in posttraumatic stress disorder (PTSD), generalized anxiety disorder (GAD), panic disorder (PD), and phobias (agoraphobia, social phobia, etc.). However, not all reports indicate a positive association between inflammation and fear- and anxiety-based symptoms, suggesting that other factors are important in future assessments of inflammation’s role in the maintenance of these disorders (i.e., sex, co-morbid conditions, types of trauma exposure, and behavioral sources of inflammation).
The most parsimonious explanation of increased inflammation in PTSD, GAD, PD, and phobias is via the activation of the stress response and central and peripheral immune cells to release cytokines. Dysregulation of the stress axis in the face of increased sympathetic tone and decreased parasympathetic activity characteristic of anxiety disorders could further augment inflammation and contribute to increased symptoms by having direct effects on brain regions critical for the regulation of fear and anxiety (such as the prefrontal cortex, insula, amygdala, and hippocampus). Taken together, the available data suggest that targeting inflammation may serve as a potential therapeutic target for treating these fear- and anxiety-based disorders in the future. However, the field must continue to characterize the specific role pro-inflammatory signaling in the maintenance of these unique psychiatric conditions [35].
Based on evidence that psychological stress may induce a chronic inflammatory process, we hypothesized that the stress caused by chronic fear of terror may be associated with low-grade inflammation. This hypothesis was examined in employed men and women with the presence of low-grade inflammation measured by high sensitivity C-reactive protein (CRP). Apparently healthy employed adults (N = 1153) undergoing periodic health check-ups in a tertiary hospital in Israel completed a questionnaire. Fear of terror (scored 1-5) was assessed by three items measuring the extent to which respondents have deep concern for personal safety, elevated tension in crowded places, and fear of terror strikes causing harm to one’s self or one’s family members. The main outcome measure was the presence or absence of an elevated CRP level (>3.0 mg/L). Women scored significantly higher on fear of terror compared with men (M = 2.16 vs. M = 1.68, respectively; p <.0001). Most of the study participants who scored high (4 or 5) on fear of terror, reported having experienced this feeling for 1 year or more. In women only, there was a positive association between fear of terror and risk of elevated CRP level (adjusted OR = 1.7, 95% CI 1.2-2.4) in a multivariate model adjusting for generalized anxiety, depressive symptoms, and potentially confounding demographic and biomedical variables. Chronic fear of terror in women, but not in men, is associated with elevated CRP levels, which suggests the presence of low-grade inflammation and a potential risk of cardiovascular disease [36].
Vignes M. et al. & Bouayed J, et al. [37,38] summarized the data to support a link between oxidative stress and anxiety. While all of the data demonstrate that there is a link between oxidative stress and high-anxiety-related behavior, a cause-effect relationship has yet to be completely established. Some of these studies suggest that oxidative stress causes anxiety-related behaviors but do not explain the underlying mechanisms. While there are some limits in the approach to establish the anxiogenic effect of oxidative stress, the available data are consistent this causal relationship. The potential causal role of oxidative stress on anxiety may generate interest in antioxidants. Masood et al. were able to show that oxidative stress-related anxiety can be reversed in mice upon inhibition of NADPH oxidase or phosphodiesterase-2, enzyme that is indirectly implicated in oxidative stress mechanisms. Surprisingly, they found that diazepam, which is a well-known anxiolytic, does not fully reverse the oxidative stress-related anxiety. These results point to a possible use for antioxidants in the prevention or reduction of high anxiety. Recent work has shown that some dietary polyphenols have both anxiolytic and antioxidant effects, which may be beneficial to anxious subjects [37,38].
It is well known that low/moderate concentrations of reactive oxygen species (ROS) affect a great number of physiological functions [39]. However, when ROS concentration exceeds the anti-oxidative capacity of an organism, animal cells enter a state termed oxidative stress, in which the excess ROS induces oxidative damage on cellular components [40]. As a result, oxidative stress has been implicated in a large range of diseases, including cancer [41,42].
The brain is highly vulnerable to oxidative stress due to its high O2 consumption, its modest antioxidant defenses and its lipid-rich constitution [43,44]. Human brain utilizes 20% of oxygen consumed by the body even though this organ constitutes only about 2% of the body weight [45]. When the production of oxygen-derived metabolites prevails over the brain defence systems, however, oxidative damage to nucleic acids, proteins and neuronal membrane lipids, which are rich in highly polyunsaturated fatty acids, can occur [46]. In presence of oxidative stress, the lipid-rich constitution of brain favors lipid peroxidation that results in decrease in membrane fluidity and damage in membrane proteins inactivating receptors, enzymes and ion channels. As a result, oxidative stress can alter neurotransmission, neuronal function and overall brain activity [47]. Oxidative stress has been associated with several diseases which are specific for nervous system impairment including neurodegenerative diseases and neuropsychiatric diseases, such as schizophrenia and major depressive disorder [42,44]. The intrinsic oxidative vulnerability of the brain has led some authors to suggest that oxidative damage may be a plausible pathogenic factor for certain neurological diseases including neuropsychiatric disorders [40-46].
Stress and Illness including cancer
There is likely a connection between stress and illness. Theories of the stress–illness link suggest that both acute and chronic stress can cause illness, and several studies found such a link [48]. According to these theories, both kinds of stress can lead to changes in behaviour and in physiology. Behavioural changes can be smoking and eating habits and physical activity. Physiological changes can be changes in sympathetic activation or hypothalamic pituitary adrenocorticoid activation, and immunological function [49]. However, there is much variability in the link between stress and illness [50].
Stress can make the individual more susceptible to physical illnesses like the common cold [51]. Stressful events, such as job changes, may result in insomnia, impaired sleeping, and health complaints [52]. Research indicates the type of stressor (whether it’s acute or chronic) and individual characteristics such as age and physical well-being before the onset of the stressor can combine to determine the effect of stress on an individual. An individual’s personality characteristics (such as level of neuroticism) [53], genetics, and childhood experiences with major stressors and traumas [54] may also dictate their response to stressors.
Chronic stress and a lack of coping resources available or used by an individual can often lead to the development of psychological issues such as depression and anxiety [55]. This is particularly true regarding chronic stressors. These are stressors that may not be as intense as an acute stressor like a natural disaster or a major accident, but they persist over longer periods of time. These types of stressors tend to have a more negative impact on health because they are sustained and thus require the body’s physiological response to occur daily. This depletes the body’s energy more quickly and usually occurs over long periods of time, especially when these microstressors cannot be avoided (i.e. stress of living in a dangerous neighborhood). See allostatic load for further discussion of the biological process by which chronic stress may affect the body. For example, studies have found that caregivers, particularly those of dementia patients, have higher levels of depression and slightly worse physical health than noncaregivers [56].
Studies have also shown that perceived chronic stress and the hostility associated with Type A personalities are often associated with much higher risks of cardiovascular disease. This occurs because of the compromised immune system as well as the high levels of arousal in the sympathetic nervous system that occur as part of the body’s physiological response to stressful events [58]. However, it is possible for individuals to exhibit hardiness – a term referring to the ability to be both chronically stressed and healthy. [58]. Many psychologists are currently interested in studying the factors that allow hardy individuals to cope with stress and evade most health and illness problems associated with high levels of stress. Stress can be associated with psychological disorders such as delusions [59], general anxiety disorder, depression, and post-traumatic stress disorder. However, everyone experiences some level of stress, and diagnosis of stress disorders can only be performed by a licensed practitioner. According to a 2016 review article, pathological anxiety and chronic stress lead to structural degeneration and impaired functioning of the hippocampus [60].
It has long been believed that negative affective states, such as feelings of anxiety and depression, could influence the pathogenesis of physical disease, which in turn, have direct effects on biological process that could result in increased risk of disease in the end. However, studies done by the University of Wisconsin- Madison and other places have shown this to be partly untrue; although stress seems to increase the risk of reported poor health, the perception that stress is harmful increases the risk even further [61,62]. For example, when humans are under chronic stress, permanent changes in their physiological, emotional, and behavioral responses are most likely to occur [63]. Such changes could lead to disease. Chronic stress results from stressful events that persist over a relatively long period of time, such as caring for a spouse with dementia, or results from brief focal events that continue to be experienced as overwhelming even long after they are over, such as experiencing a sexual assault.
Experiments show that when healthy human individuals are exposed to acute laboratory stressors, they show an adaptive enhancement of some markers of natural immunity but a general suppression of functions of specific immunity. By comparison, when healthy human individuals are exposed to real-life chronic stress, this stress is associated with a biphasic immune response where partial suppression of cellular and humoral function coincides with low-grade, nonspecific inflammation.
Even though psychological stress is often connected with illness or disease, most healthy individuals can still remain disease-free after confronting chronic stressful events. Also, people who do not believe that stress will affect their health do not have an increased risk of illness, disease, or death. This suggests that there are individual differences in vulnerability to the potential pathogenic effects of stress; individual differences in vulnerability arise due to both genetic and psychological factors. In addition, the age at which the stress is experienced can dictate its effect on health. Research suggests chronic stress at a young age can have lifelong impacts on the biological, psychological, and behavioural responses to stress later in life [64].
As stress has a physical effect on the body, some individuals may not distinguish this from other more serious illnesses. Individuals experiencing stress are less likely to see medical care for a symptom if the symptom is ambiguous (e.g. headache) and they are currently experiencing stress. If the symptom is unambiguous however (e.g. a breast lump), and the onset of the stressor is recent, individuals are motivated to seek care as usual [65].
In animals, stress contributes to the initiation, growth, and metastasis of select tumors, but studies that try to link stress and cancer incidence in humans have had mixed results. This can be due to practical difficulties in designing and implementing adequate studies [66].
Discussion
Fear hormones are secreted by the adrenal gland, an endocrine gland located on top of the kidneys [67]. The fear hormones circulate through the bloodstream to all cells of the body [68]. The effect of adrenaline is similar to the effect of the sympathetic nerve action [69]. Adrenaline increases heart rate, increases breathing rate, dilates blood vessels to the lungs and muscles [70]. Adrenaline also decreases blood flow to the brain and decreases digestion. Cortisol increases blood sugar level by converting stored glycogen and fats into blood sugar. Cortisol also suppresses the immune response and inflammation. Fear hormones result in a longer lasting and more widespread fight‐or‐flight response than the effects of the nervous system [71-73]. Fear hormone action explains why one may feel the fight‐or‐flight response even after he/she realize there really is no danger. Daily life can involve many stimuli that are perceived as threatening [74-76]. Problems at work or at school, money or social problems, and medical problems can trigger a chronic (long term) fight‐or‐flight response. Even anticipating or worrying about things that might happen in the future can trigger the same response as actually experiencing it. Chronic stress occurs when the fight‐orflight response does not shut down to allow for the proper balance between fear and relaxation. Stress can increase a person’s risk of health problems [77-80].
The fight‐or‐flight response uses calories so the urge to eat makes sense after running. But, eating in response to daily stresses can lead to weight gain and obesity. In addition, stress increases cortisol levels causing elevated blood sugar levels that can lead to both weight gain and diabetes. When the fight‐or‐flight response causes blood pressure and heart rate to remain high, it puts extra strain on blood vessel walls. As a result, the linings of blood vessels can become damaged and the amounts of oxygen in blood can become lesser than normal [81,82]. An interruption of blood flow to the heart can lead to a heart attack. Blood vessels in the brain can also be blocked, resulting in brain‐damaging strokes. People suffering from stress secrete cortisol at much higher rates than normal people. There is evidence that abnormally high cortisol levels may actually be the initial trigger for depression in some individuals. High cortisol levels also result in sleep deprivation. Stress also affects the function of the immune system, the body’s natural means of fighting off infection. Stressed individuals produce lower levels of antibodies when exposed to pathogens. They also produce higher levels of cytokines, inflammation triggering chemicals secreted when fighting infections. Excessive inflammation is thought to increase the risks for heart disease, diabetes, and cancer. Feeling stressed mentally and physically may have serious health consequences [83,84].
A large literature exists demonstrating that major life events, especially those involving interpersonal loss and social rejection, are a key proximal risk factor for MDD. As it turns out, these stressors have been implicated not just in the development of depression but in the onset, exacerbation, or progression of a variety of health problems. These conditions include several that, like depression, are thought (or known) to be mediated at least in part by inflammation, such as asthma, rheumatoid arthritis, cardiovascular disease, chronic pain, and certain cancers. As a result, we turn now to the question of whether stress is associated with inflammation.
Acknowledgements
We would like to thank Professor Thomas N. Seyfried at Boston University, Professor Stephanie Seneff the Senior Research Scientist at Massachusetts Institute of Technology (MIT) and Specially Professor Sir John Gurdon at Gurdon Institute for their informative and support. We also would like to thank the Weston A Price Foundation in Washington for their Support
Conclusion
Inflammation is partly regulated by the hormone cortisol and when cortisol is not allowed to serve this function, inflammation can get out of control. chronic stress may hamper a naturally occurring anti-inflammatory response in the body. Ordinarily, white blood cells will concentrate in the area of injury or infection where they release chemicals called cytokines to fend off the invaders, a process generally known as inflammation. While inflammation can help fight infection, too much inflammation occurring over time can actually be damaging. Under normal circumstances, the inflammation process is naturally stopped in the body when levels of a stress hormone, cortisol, begin to rise. It is harmful to the body when the inflammation process does not stop as it should. The researchers found that the white blood cells of stressed parents were less responsive to the cortisol hormone, and less likely to shut down an inflammatory response, than the less stressed parents. Their cells kept producing more cytokines. The findings highlight the fact that stress may interfere with the body’s ability to shut down its own immune response after it gets started.
Therefore, the bodies of those people suffering from stress may be less likely to regulate their normal defense mechanisms. In conclusion, chronic anxiety, fear and stress results in increasing the hormone cortisol which leads to diabetes, decreasing immune response and increasing inflammation in the tissues which leads to increasing the possibility of cancer incidence. Chronic fear and anxiety increase the hormone adrenaline which decreases the blood flow to the brain and in the long time leads to hypoxia. Therefore; chronic stress, chronic fear and anxiety increase the possibility of cancer incidence basically in the brain. These three chronic disorder cause hypocapnia as well which leads to the hypoxia in body tissues through the Bohr Effect and increases the possibility of cancer incidence in the whole body tissues. In cancer patients, stress, fear, anxiety and depression worsen the disease. Depression alone has not been linked as a factor in causing any types of cancer.

Read More About this Article: https://biomedgrid.com/fulltext/volume3/the-impact-of-stress-anxiety-fear-and-depression-in-the-cause-of-cancer-in-humans.000696.php
For more about: Journals on Biomedical Science :Biomed Grid
#biomedgrid#American Journal of Biomedical Science & Research#Journals on Cancer medicine#Journals on Medical Microbiology#Open access clinical and medical journal#Journals on Medical Casereports
0 notes
Text
Does CBD help with stress and anxiety?
Going on a first date, making a speech to a broad audience or having a job interview – there are too many stressful situations in everyday life. The good thing is that the circumstances that cause sweaty palms and heart-pounding tend to pass quickly.
However, prolonged family problems or challenges at work may lead to chronic anxiety and require medical care. Besides medicaments, there are more natural ways of therapy, such as CBD consumption.
Nowadays, cannabis is promoted by the media as an alternative to traditional medicines and a natural cure to help prevent or even cure many illnesses. Numerous studies prove that CBD may be helpful with everything from anxiety and bad sleep, to Parkinson’s disease and chronic pain management. Let’s discuss how CBD can be helpful in coping with mental health problems.
How cannabinoids interact with your body?
There are two types of cannabinoids. Phytocannabinoids come from the cannabis plant, while endocannabinoids are made within the body.
Cannabinoids help to keep the homeostasis of the physiological functions such as sleep, mood, appetite, or immune functions. For example, if your body lacks water, it will send thirst signals, or if you’re stressed, it will help regulate the heart rate.
The body keeps the balance with the help of our endocannabinoid system, a sensitive network of cannabinoid receptors, which are found mainly in nervous and the immune systems. A receptor is a protein molecule on the surface of cells, which can receive chemical signals and help to produce the corresponding cellular or tissue response to the outer changes. Cannabinoid receptors can easily be activated by the endocannabinoids naturally made in the body or external cannabinoids, such as CBD and THC. Therefore, by consuming these plant compounds, you can keep the endocannabinoid system regulated.
Are you anxious or stressed?
Usually, the terms stress and anxiety are used interchangeably. Even though both stress and anxiety share many similar symptoms, they are two different health conditions. It may be a challenge to see the differences between the two. However, you must identify which one you are struggling with and treat it accordingly.
Stress is the body’s reaction in response to a real or alleged threatening situation or discomfort.
Some of the psychological and physiological signs of stress include:
Headaches
Upset stomach, including diarrhoea and constipation
Nausea
Aches, pains, and tense muscles
Pain in chest and rapid heartbeat
Frequent colds and infections
Lack of sex drive
Anger
Irritability
Feeling tired, unmotivated, or unfocused
Sleeping too much or too little
Racing thoughts or constant worry
Memory or concentration problems
Anxiety, on the other hand, is a reaction to stress. It is an emotion accompanied by the following symptoms:
Excessive worrying
Feeling nervous, restless, agitated or tense
A sense of impending danger or doom
Increased heart rate
Breathing rapidly
Sweating
Trembling
Fatigue
Tense Muscles
Panic Attacks
Trouble concentrating
Feeling anxious or fearful of social situations
Various factors that may trigger anxiety disorders:
Genetic predisposition. The latest studies suggest that such disorders may be partly genetic. A 2016 review demonstrated that social anxiety disorder, generalised anxiety disorder and panic disorder, are provoked by specific genes. A 2017 review of studies proved that generalised anxiety disorder could be inherited.
Environment. Studies suggested that environmental factors could also influence anxiety. Socialising with people at school or work, surrounding and lifestyle may potentially lead to anxiety.
Traumatic life experiences. The National Institute of Mental Health claims that an individual is more likely to develop an anxiety disorder due to lousy family relationships, abuse in childhood, neglect, and poverty.
Smoking, alcohol and drugs use. Consumption of various medications and drugs, including alcohol, caffeine, and benzodiazepines, may play a role in anxiety development.
Health conditions. Some physical conditions such as thyroid disorders may be linked to anxiety.
Stress. Chronic stress trains the brain to feel anxious, so you can anticipate and avoid more stress and tension in the future. However, it can make you more resilient or more vulnerable to potential mental distress.
Unfortunately, anxiety may develop into further more damaging forms:
Generalised anxiety disorder (GAD) is excessive worrying for no logical reason. Such a condition is considered a GAD if it lasts more than six months. In a mild case, it allows you to manage everyday activities and doesn’t affect your performance. On the contrary, more severe GAD can significantly change your lifestyle.
Social anxiety disorder (SAD) implies a paralysing fear of social situations, the worry of being judged or humiliated by other people. Those who experience social anxiety disorder often feel alone and embarrassed.
Post-traumatic stress disorder (PTSD). Traumatic experiences such as natural disasters, military action or physical attack can lead to PTSD. The impact is usually immediate and may last for years.
Obsessive-compulsive disorder (OCD). People suffering from OCD may experience intrusive and unwanted thoughts that become a real obsession. Common compulsions are hand washing, counting of things, or checking if a door is locked.
Phobia is a persistent urge to avoid a frightening object or situation. These can include the fear of enclosed places (claustrophobia), fear of heights (Acrophobia), fear of the dark (Achluophobia), and many others.
Panic disorder leads to panic attacks, spontaneous feelings of anxiety, or fear. Physical symptoms may occur anytime and include heart palpitations, pain in the chest, and shortness of breath.
How does anxiety affect your body?
Small bursts of stress hormones make the body to prepare for “fight or flight”. Unfortunately, human bodies weren’t designed to manage a constant state of panic. High levels of chronic stress hormones, especially cortisol, may wreak havoc everywhere. Here are the main effects that anxiety may cause to the body:
The central nervous system (CNS)
Regular panic attacks make your brain release stress hormones and lead to persistent headaches, lightheadedness, and depression. The brain releases adrenaline and cortisol in the nervous system, helping the body to respond accordingly to the threat. Prolonged exposure may negatively affect the body. For example, a high level of cortisol may cause weight gain over time.
Cardiovascular system
Anxiety may cause heart palpitations, chest pain, high blood pressure, and cardiovascular diseases. For those who already suffer from heart disorders, anxiety raises the chance of coronary events.
Digestive systems
Anxiety can cause digestive disorders, such as stomach aches, nausea, and diarrhoea. Anxiety disorders may also lead to loss of appetite.
Immune system
Constant feelings of anxiety and stress, and high levels of chemicals and hormones, such as adrenaline, weaken the immune system. This increases the risk of viral diseases and illnesses. Moreover, regular vaccines may not provide the desired result in this case.
Respiratory system
Rapid breathing, caused by anxiety disorders, may worsen respiratory functions for people with asthma. Furthermore, patients with chronic obstructive pulmonary disease may also suffer from anxiety complications.
Other effects:
Muscle tension
Weight gain
Insomnia
Depression
Social isolation
Once you’ve determined which disorder you have, if not both, it is time to start the treatment. CBD may be helpful for both stress and anxiety. However, some anxiety disorders require additional medications or therapy.
How may CBD alleviate stress?

Regular stress can be harmful for social life, mental and physical health. In this case, CBD products such as oil or tincture act as a natural way to lower the daily stress that stops you from living your best life.
If you experience chronic stress, the hypothalamus becomes less sensitive to cortisol, the main stress hormone. It means that you need more cortisol to obtain the same response. Lowered sensitivity causes us to remain stressed for a long time. CBD may increase the hypothalamus’ ability to sense cortisol and prevent stress from lasting for too long.
Stress causes an increase in blood sugar and metabolic activity, which in turn causes a buildup of free radical products and oxidative damage. CBD products such as oil are high in antioxidants that help neutralize free radicals and protects the body from damaging influence.
Animal and human studies indicate that cannabidiol has anxiolytic properties. A study conducted in 2010 showed that CBD can help reduce anxiety in people with social anxiety disorder, or SAD. It was found that CBD could affect limbic and paralimbic brain areas, help to minimise current anxiety and change the initial brain reaction to anxiety disorders. Similarly, a 2011 study demonstrated that CBD might significantly reduce anxiety, cognitive impairment and discomfort induced by public speaking, and significantly increase alertness.
In 2015, the research results suggested that CBD had considerable potential as a treatment for multiple anxiety disorders, including panic disorder, obsessive-compulsive disorder, social anxiety disorder, generalised anxiety disorder, and post-traumatic stress disorder.
Anxiety and sleep disorders may be the result of posttraumatic stress disorder. The 2016 research with a trial of cannabidiol oil resulted in a decrease in anxiety and an improvement in the quality of the young patient’s sleep.
How does CBD facilitates fighting anxiety?
Due to the different therapeutic properties of cannabidiol, it is difficult to know exactly what body part it may activate. According to the studies, CBD can reduce anxiety by stimulating neural regeneration and neurotransmitter systems.
CBD can bind to the specific receptor of the neurotransmitter serotonin, which is thought to play the most substantial role in anxiety disorders. This bind causes anti-anxiety effects.
CBD may prevent overstimulation of CB1 receptors and trigger the production of endocannabinoids, which helps to restore balance in the endocannabinoid system. Usually, the body produces cannabinoids on its own. However, the system can become dysregulated under chronic stress. The experiments on rodents show that CBD may relieve Obsessive Compulsive Disorder and other anxiety disorders by affecting the endocannabinoid system, which is important for the processing and forgetting the fears.
CBD may encourage neural regeneration, particularly in the hippocampus. Even though chronic stress can damage neurons and shrink the brain, some areas of the brain are still able to regenerate. CBD may boost the formation of new neurons and, therefore, compensate for the brain damage caused by chronic stress. Its ability to reduce anxiety and help to form new neurons was successfully tested on mice with chronic stress.
Compatibility of CBD and medications
If you choose to take a CBD product, it will work best as part of comprehensive anxiety treatment. The best way is to speak with a trusted medical professional first and discuss your plans, especially if you are currently taking prescription medications. CBD may interfere with your body’s ability to metabolise drugs. A doctor can also help you manage other health issues.
References:
https://www.ncbi.nlm.nih.gov/pubmed/26575296
https://journals.sagepub.com/doi/abs/10.1177/0269881110379283
https://link.springer.com/article/10.1007/s13311-015-0387-1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4543605/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938896/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573560/
https://www.nature.com/articles/npp20116?foxtrotcallback=true
https://www.ncbi.nlm.nih.gov/pubmed/20695034
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5101100/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3775646/
https://www.sciencedirect.com/science/article/pii/0014299982902643
https://www.pnas.org/content/95/14/8268.short
from Hemp Frontiers https://hempfrontiers.com/does-cbd-help-stress-anxiety/
0 notes
Text
GIVE YOUR BODY THE BOOST IT NEEDS WITH VITAMIN THERAPY!

With all the vitamin and also hydration treatment selections available available, Nore Women's Wellness can aid you take the guesswork out of the equation!
In the grocery store vitamin aisle, there are many options, brands, and also eye-catching labels intending to catch your eye. There are Med-spas advertising walk-in IV hydration and also vitamin therapy. Internet-site pop-ups declare to have the ideal treatment to all your troubles. Having numerous alternatives is frightening and the quick solution is alluring.
Stronger nails as well as shinier hair? Of course! More energy, much less pains and also pains, much better rest, and a healthier body immune system? Sounds excellent! More powerful bones? Absolutely! Improved state of mind? Yes, please.
All of us intend to really feel much better and also less exhausted, increase our immune system, protect against illness, and also have actually balanced nourishment. However exactly how do we set about doing this?
There are so many inquiries:
Do I require vitamin therapy?
How do I find out what, especially, my body demands?
How do I recognize if I have a dietary deficiency or if something else is taking place?
How do I figure out which vitamin options to make-- do I require to take oral vitamins, simply re-hydrate or are there other methods to stabilize my nourishment and really feel much better?
The length of time do I need therapy for?
Who should I trust to encourage me regarding this?
The answers to these inquiries can be overwhelming. You are not alone. Your trusted Nore companies are here to aid simplify the choice!
Do I need Vitamin Therapy and also how can it help?
Lots of people do not satisfy their everyday nutritional requirements with diet alone, even if they eat vitamin strengthened food as well as take a daily multi-vitamin. The risk of this boosts when the body is stressed, fatigued, and exposed to contaminants and bacteria triggering pressure on the body immune system. Nutritional equilibrium plays a vital duty in ideal wellness, body immune system feature, chronic disease avoidance as well as taking care of the aging procedure.
Replenishing your deficiencies can assist with:
Exhaustion
Dehydration
Headaches/migraines
State of mind
Sleep problems
Athletic performance
Bone wellness
Immune system feature
Nerve/muscle function
Skin/hair/nail look
Some evidence also shows it can help with persistent illnesses such as bronchial asthma, seasonal allergies, autoimmune problems, chronic discomfort, as well as even cognitive decrease.
How do I identify what my nourishment requirements are?
Everyone's nutrition requirements are special. Possibly your lifestyle or food choices have developed particular vitamin deficiencies. You may have simply run a fifty percent marathon as well as are feeling dried out and also weak. Perhaps a disease or chronic concern has you feeling diminished. You may prefer to increase your immune system before the beginning of influenza period or prior to beginning a brand-new Bootcamp.
At Nore, we provide nutrition consults, screening as well as therapy options to fulfill your needs as well as obtain you feeling Your Most once more. Relying on your age, personal health and wellness history, and signs, our carriers may advise blood work to check your nourishment standing, hormonal agent condition, including the thyroid as well as adrenal hormone degrees, and also feasible other tests to eliminate specific persistent problems.
If you just need a quick boost for your immune system during influenza period or for athletic improvement as well as are not ready for a detailed workup, your Nore supplier additionally has options for you and can aid.
Just how will my nutrition status be analyzed?
At Nore, we offer SpectraCell's Trace element Examination. This examination is one of the most comprehensive dietary analysis offered. It gauges levels of choose vitamins, minerals, antioxidants, and various other crucial trace elements within your leukocyte over a longer period than traditional lotion screening.
What Vitamin Therapy choices are readily available?
Vitamin IV Mixtures Vitamin Booster Injections. Dental Vitamin Supplements.
Depending upon your specific needs, symptoms, and/or specific screening outcomes, your Nore supplier will certainly provide therapy suggestions and also go over possible negative effects with each treatment choice. Therapy recommendations are typically based upon whether a broad or particular deficiency is established as well as if there is a need for temporary or long-term therapy.
Vitamin IV Mixtures.
Customized combined vitamins, minerals, amino acids and antioxidants are supplied directly right into your circulatory system via an IV placed in your arm under straight medical guidance in a comfortable, loosened up environment.
IV infusions are fantastic for instant requirement hydration, broad nutritional shortages, and body immune system recovery and also boosting. They can also assist if you deal with persistent discomfort, an auto-immune disorder, and also various other usual wellness issues such as bronchial asthma and seasonal allergic reactions. Most of the times results are really felt within hours. To get the optimum results from IV mixture, many patients will take advantage of 4 once a week treatments. At Nore, we perform the mixtures gradually to lessen negative effects.
" Vitamin IV Mixture is effective due to the fact that it bypasses the challenges of the stomach, liver, as well as intestinal tract, which can have difficulty taking in the nutrients properly," stated Julie Morin, WHNP-BC, one of Nore's Vitamin Therapy providers.
If you have a particular or chronic shortage, your Nore supplier will likely advise extra long-lasting supplements as well.
Vitamin Boosters
Custom mixed vitamin boosters are delivered into the body swiftly as well as successfully via intramuscular shot. Vitamin booster are suggested choices for details vitamin deficiencies. 2 of the most usual vitamin shortages are Vitamin D and also Vitamin B12. Your body requires these important vitamins to operate ideally.
Vitamin D is a nutrient required by the body for the upkeep of strong bones, immune system feature, neuromuscular function, boosting state of mind guideline, safeguarding the brain against toxic chemicals, and also possibly lowering discomfort.
Vitamin B12 is a nutrient that helps keep the body's nerve as well as blood cells healthy and balanced and assists make DNA, the genetic material in all cells. It additionally helps stop a type of anemia called megaloblastic anemia that makes individuals exhausted and also weak.
After treatment with a Vitamin booster, it is usually advised to proceed with oral supplementation to prevent the deficiency from returning.
Vitamin Supplements
Oral nutritional therapy is recommended when particular deficiencies take place in your vitamin, mineral, antioxidant and/or other vital micronutrient levels.
Nore provides a vast option of supplements from Layouts for Health ®. They manufacture nutritional supplements as well as vitamins based upon scientific study and clinical responses. They provide risk-free as well as efficient quality products, assisting you achieve complete health and wellness as well as wellness.
Vitamin Therapy for Your Health and wellness
Offer your body the boost it needs and attain optimal health.
The post “ GIVE YOUR BODY THE BOOST IT NEEDS WITH VITAMIN THERAPY! “ was published first on NORE Women’s Health
Boost your immune system with IV vitamin therapy at Dr. Amauri Wellness Centre located in the heart of Yorkville, Toronto.
0 notes
Text
Anxiety: It’s More Extensive Than It Seems

I’m sure everyone knows the term ‘anxiety’ and can decipher what it means in their own way. When people first hear this word being used, they usually automatically assume that the person using said word is either nervous, worried, or tense about something. However, that’s the extent that most people can understand about anxiety. Many people are uneducated on this topic and either aren’t knowledgeable or understanding of the severity and impact it can bring amongst others. It’s extremely important that this type of information gets put into society, so that this issue of “not knowing” becomes less of an issue or none at all.
Before you can even begin to think of a solution for a problem like this, you have to consider why it even is a problem in the first place. Anxiety is a normal sensation of life. Anyone can feel anxious at any point throughout their day. However, increasing constant anxiety that affects daily routines and lifestyle is not normal. The issue here lies with people not knowing or understanding when anxiety is no longer just anxiety. This oblivion can lead to further issues as well including denial that something is actually wrong or that someone is exaggerating/making it up. It’s crucial that we tackle this issue as a society so that people who suffer from anxiety disorders can feel supported and valued.
Knowing what causes anxiety disorders is one of the keys to understanding the impacts it can have on someone. Things like environmental factors, genetics, medical factors, brain chemistry, and substance abuse can all trigger the disorder to appear within a person according to Medical News Today. You might be wondering how any of these factors is connected with an anxiety disorder. Stress stemming from school, work, personal relationships, or financial issues can be the starting point for someone’s anxiety. Kids who are born into families with past experiences dealing with this disorder can later develop it themselves. Specific medical conditions and medications also go hand in hand with anxiety. Traumatic experiences that one has faced in the past can definitely trigger the beginning of this disorder. In fact, “psychologists and neurologists define many anxiety and mood disorders as disruptions to hormones and electrical signals in the brain”. This is evidence showcasing how anxiety disorders can be brought upon somebody in several, unique ways.
Understanding why anxiety exists in a person’s life is important in discovering what type of anxiety disorder a certain person is dealing with if they even are. When someone is battling with an anxiety disorder, it causes them to be constantly stressed, which makes is difficult for them to continue living their life the way they want to. According to Your Health In Mind, those with a disorder are constantly worried about things that are not likely to cause issues, feeling panicked, finding it difficult to concentrate, avoiding certain places, and having trouble breathing. These are only some of the many symptoms one may face when suffering from an anxiety disorder. Applying these signs to a specific disorder is the next step is understanding the depth and severity of this issue.
There are many types of anxiety disorders that all contain aspects different from one another. For instance, generalized anxiety disorder (GAD), social anxiety disorder, panic disorder, agoraphobia, and specific phobia all belong to the main focus of anxiety disorders. According to Your Health In Mind, “people with GAD, worry much of the time about all sorts of everyday things – to do with work, finances, health, or family. They worry something terrible might happen, even if there’s no real reason to think so”. In other words, this is most general form of an anxiety disorder that ties into the feeling that something is wrong and that there is a constant need for worry. Someone with a social anxiety disorder “worries about other people noticing their anxiety and thinking less of them because of it”. This can lead to avoiding meeting new people, going to parties or gatherings, using public transportation, or being watched while eating. It shows within itself how big of a dilemma it is for those who have it. Panic disorder can be described as “someone who has repeated panic attacks, which seem to happen for no particular reason, and then they worry a lot about having more panic attacks”. Having a panic attack is a terrifying feeling. I would know because I get them occasionally. It’s very important to comprehend what a panic attack looks and feels like. It differs for everyone, but the difficult breathing, chest tightening, and loss of self-awareness is a common theme. Agoraphobia connects to panic disorder because it is simply the fear of certain places or situations because they are afraid that they will have a panic attack. This disorder is seen on a deeper level and can affect people drastically. Lastly, specific phobia is a disorder in which someone is afraid of a certain thing or situation. For example, spiders, shots, airplanes, or heights. It’s more severe than a regular phobia because it affects the way a person will live their life. Everyone should be aware of these disorders, so that they can apply it to their own life when dealing with a loved one or themselves.
Now that the concept of anxiety and its disorders are clear, I’d like to discuss the effects that it can have on the human body. Chronic anxiety can interfere with the quality of someone’s life, meaning it can have drastic effects on their body. We need to know and understand this in order to help understand someone who is going through this instead of making them feel like it’s all an exaggeration. According to Healthline, “an excessive or persistent state of anxiety can have a devastating effect on your physical and mental health”. We can see these effects through the central nervous system. Medically speaking, “when you feel anxious and stressed, your brain floods your nervous system with hormones and chemicals designed to help you respond to a threat”. The cardiovascular system is also affected due to the fact that anxiety causes rapid heart rate, palpitations, and chest pain. Excretory and digestive systems can be impacted by the nausea, stomachaches, diarrhea, irritable bowel syndrome and loss of appetite that anxiety brings. Immune systems can be weakened by the constant fight or flight response your body is producing, which can expand your risk for more illnesses. Lastly, the respiratory system is affected by rapid and shallow breathing. It can make those with asthma have heavily severe symptoms. It is clear how much the human body is impacted by anxiety disorders. To those who have never understood the depth of anxiety, it will most likely frighten you to think of these things actually occurring because of anxiety. However, it’s better to be knowledgeable on the subject, rather than ignorant.
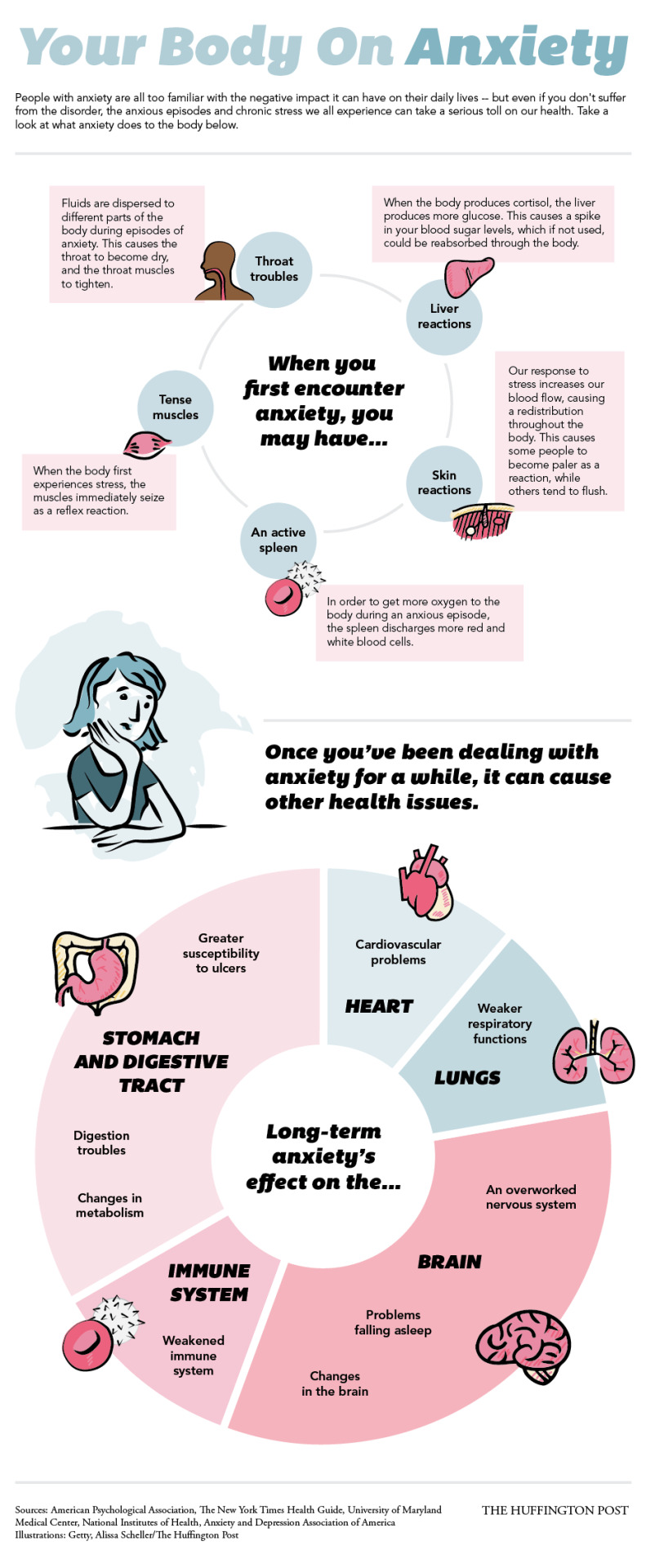
This photo visually showcases the effects anxiety has on the body, like I was discussing previously.
Maybe some people aren’t too sure or are unable to tell whether someone they know is dealing with chronic anxiety. That is why it’s beneficial to also understand the hidden signals of anxiety. According to 6 Hidden Signs of Teen Anxiety, “given that teens experience a wide variety of physical and emotional changes as they grow, an anxiety disorder can be difficult to spot. Many red flags may seem like usual teens struggles or be chalked up to hormones”. This quote specifically shows how it’s not uncommon for anxiety symptoms to be hidden, but that it’s crucial we discover them so we can act upon the problem. For example, things like emotional changes, social changes, physical changes, sleep disturbance, poor school performance, and panic attacks can be hidden easier than other symptoms. Finding these “hidden signals” is another key in aiding those who are unaware become more aware.
Being educated on coping mechanisms is just as important as being educated on anxiety as a whole. Cognitive behavioral therapy (CBT) is the most common and most frequently used therapy for those suffering with chronic anxiety. According to Psych Central, “CBT is a short-term, goal-oriented psychotherapy treatment that takes a hands-on, practical approach to problem-solving”. It focuses mostly on the relationship between our problems, our behavior, and our thoughts. CBT was actually created in the 1960’s by Aaron Beck, who created the idea of “automatic thoughts”, which are the emotion-filled thoughts that appear in the back of ones’ mind. This type of therapy was continued and carried out into today’s society. It remains effective and it can truly help turn someone’s life around for the better.
It’s one thing to be fully aware and understanding of anxiety and the long-term effects it can bring to the table. But, it’s another to set forth action and have something be done about it. The solution I am proposing is not for all of us to become psychologists and therapists in order to heal those who are suffering. I am proposing that passing on this information to someone who is uneducated on the topic whether it be by talking to a friend about it, giving a speech about it at your school/job, posting about it on social media, or even sharing this article with others, will help put an end to the issue of ignorance. It takes something as small as this to truly make a difference.
This photo is displaying the argument of anxiety disorder stigma and why it should not be treated lesser than other health predicaments.
0 notes
Text
Understanding Sleep Deprivation

Sleep is one constant in your daily life. It is as natural as breathing, eating, and drinking. However, a lot of people try to skimp on sleep. There is plenty of debate floating around on why sleep is required and if sleep is required and ways in which to sleepless. The popular belief being that sleep is just hours lost, which you could be utilizing in something more productive. This article will clarify the importance of sleep and how this seemingly useless activity can have serious consequences for your health.
Lack of Sleep and Lack of Health
Breaking it down for your lack of sleep translates directly to a lack of health. There is no way that you can or even should attempt to bypass sleep. Sleep is a natural biological function that requires no efforts on your part and provides the much-needed rest to your body. It is recommended that an average adult clock in 7 to 9 hours of sleep daily to function properly. Remember, a healthy mind, body, and soul start with a night of healthy sleep.
The importance of sleep can be gauged by the study that established that sleep leads to early mortality rate. The other ways in which sleep deprivation or lack of sleep compromises the various body organ functions are enumerated below to turn even the most vicious sleep skeptic into a sleep fan:
Central Nervous System (CNS)
The CNS consists of your brain and the spinal cord. It is responsible for controlling and regulating the functions of both your mind and body. The brain is the central control of most of your bodily functions, including awareness, sensations, thoughts, actions, speech, and movements. Anything that hampers your CNS has serious consequences on your health. Sleep deprivation disrupts the way information is sent from the brain to other parts of the body, thereby disrupting body synchronization. This results in behavioral and cognitive impairments like:
Impulsive behavior
Hallucinations
Depression
Paranoia
Microsleep
Immune System
The immune system is your first line of defense against any invasion or threat to the body. While you sleep, your body produces “cytokines,” which help the immune system identify and fight the foreign particles effectively. Sleep deprivation not only causes low levels of cytokine production but also trigger stress, which in turn further compromises your immunity. Also, sleeplessness puts pressure on your immune system without allowing adequate rest to repair itself. Low immunity caused by sleep deprivation causes:
Frequent catching of common illnesses like cough and cold
More sick days as your body will take longer to heal
Unresponsiveness to medical treatment
Lower insulin resistance leading to diabetes
Heart diseases due to the body’s lower resistance to irritants and other triggers
Respiratory System
Sleep and respiratory system relationships go both ways. Obstructive Sleep Apnea (OSA) is a nighttime breathing disorder that affects the respiratory system and makes it difficult to sleep or stay asleep. This sleep deprivation, in turn, makes your respiratory system more prone to common infections like cold and flu. It can also make any existing lung conditions like asthma to worsen.
Digestive System
Sleep deprivation puts you at risk for:
Weight gain and Obesity: Sleep helps regulating and proper functioning of the two hormones responsible for appetite and hunger, namely:
Leptin
Ghrelin
These two hormones are responsible for signaling your brain to stop eating. When they don’t function properly, you tend to develop poor eating habits like emotional eating and also overeating, which over time, causes obesity. Sleep also increases fatigue, which in turn reduces your motivation for exercising. This lack of exercise, along with overeating, is the perfect recipe for weight gain and obesity.
Diabetes: Sleep deprivation reduces your body’s tolerance for insulin and compromises the way glucose is processed. This increases your risk of developing Type 2 diabetes.
Further sleep deprivation upsets the microbiology of your gut. This causes problems in digestion, including upset stomach, bloating, belching, etc.
Cardiovascular System
The cardiovascular system is also known as the circulatory system or the vascular system. It refers to:
Heart
Blood vessels
Blood
This system is responsible for the circulation of blood and the transportation of nutrients to different parts of the body. Sleep deprivation affects the processes that are responsible for keeping these blood vessels and heart-healthy like blood sugar, blood pressure, inflammation levels, and blood clotting. These compromise your heart functions and results in:
Heart Attack
Stroke
Endocrine System
Sleep deprivation affects the endocrine system by affecting the process of hormone production. The endocrine system is a set of glands that regulate hormone production in your body. Hormones are responsible for:
Regulating metabolism
Growth and development
Sexual function
Reproduction
Tissue function
Sleep deprivation results in shorter slow-wave sleep (SWS). This increases the pro-inflammatory cytokines in the body and hence low-grade inflammation. Sleep deprivation also causes significant hormonal changes affecting the hypothalamic-pituitary-adrenal axis activity. These result in:
Lower sex drive
Decreased fertility
Growth and development especially in children
Tips to Recover from Sleep Deprivation
Now that you know the profound effect that sleep has on your health, you must be wondering how to overcome sleep deprivation. The good news is that sleep deprivation is very easily reversible. All it takes is to get some added sleep.
It is also easy to discharge the effect of sleep deprivation on health but only in the short term. Chronic sleep deprivation is harder to challenge. Hence you must make an effort to rid yourself of sleep deprivation as quickly as possible. Some tips to help you with this are:
Avoid stimulants like caffeine and nicotine at least an hour before sleeping.
Keep the bedroom temperature cool. Research shows that it is easier for the body to sleep in cooler temperatures.
Minimize all light, sounds, and disturbances when going to bed
Avoid all sorts of technology for an hour before bedtime
Maintain a regular sleep-wake schedule
Exercise daily for at least 15 to 20 minutes
Indulge in stress-relieving activities like yoga and meditation
Take an afternoon nap
Sleep Deprivation FAQ Corner
What is sleep debt?
Sleep debt is calculated as the difference between the number of hours you should be sleeping and the number of hours you sleep. This difference in the number of sleep hours keeps getting stacked up over a period increasing your sleep debt and reducing your chances of successfully making up to the lost sleep hours.
How do you reduce your sleep debt?
The good thing about sleep deprivation is that it is easily reversible in the short run. You can make up for last night’s sleep the next day. Or even catch up on the weekends. However, the problem arises when you rack up over 20 hours of sleep debt. This pushes your body into the chronic sleep deprivation mode, affecting your regular bodily functions permanently. Research suggests that it takes you four days to recover from an hour of lost sleep in the long run.
Are sleep debt and sleep deprivation two separate things?
Sleep deprivation is different from sleep debt. Sleep deprivation is simply a term used for lack of sleep. Sleep debt, on the other hand, is the number of missed sleep hours that you have lost because of sleeplessness.
Can you die from sleep deprivation?
There is no conclusive study on humans that links certain death with sleep deprivation. However, research has shown that sleep deprivation can lead to a reduced life span.
Conclusion
Everyone suffers from sleep deprivation at one point or another. The trick is to nip it in the bud and not let your sleep debt accumulate into large numbers. Remember, the higher and more prolonged your sleep deprivation, the harder it is for your body to bounce back, and the worse the effects on your health.
0 notes