#amyotrophie spinale
Text
RÉAPPARAÎTRE AVEC PANACHE
Bonsoir à tou.x.t.e.s !
Le dernier article publié sur ce blog date du 25 mai 2022... Je ne suis qu'une larve. (J'espère que vous avez la ref)
Voici une liste non-exhaustive de ce qu'il s'est passé dans ma vie depuis cette date :
Roadtrip de 10 000 km jusqu'à Trømso
Victime de mobbing
Concert de Lady Gaga à Paris
Fêter mes 30 et 31 ans (oh gosh)
Concert de Juliette Armanet
Nouveau petit chat qui s'appelle Catniss
Demission pour cause de mobbing
6 mois de chômage
12 mois de dépression
Beaucoup d'anti-dépresseurs
Voyage à Marrakech
Roadtrip de 2 000 km jusqu'à Amsterdam
Concert de Beyoncé à Paris
Voyage à New York
Concerts de Mylène Farmer à Genève et Nice
Paléo Festival pour Pomme, Rosalia, Pierre de Maere, Aya Naka-jauraisvouluquelleannule-mura
Commencer un nouveau job (omg yay)
5 injections de Spinraza
Ça va faire beaucoup à écrire. Non je ne vais pas TOUT écrire. Mais tout de même !
Oui, en effet, comme ça, visuellement, ça fait énormément de chouettes expériences sur un peu plus d'un an et demi... mais ne vous voilez pas la face car 80% de mon énergie a été utilisée pour garder tout juste une narine hors de l'eau lors de ma dépression.
But let's keep it light. I'm back bitches !
Gésiers et fluorescence !

3 notes
·
View notes
Text
Mechanisms of nerve injury – The major mechanisms of upper extremity peripheral nerve injury are compression, transection, ischemia, inflammation, neuronal degeneration, and radiation exposure.
●Diagnostic testing
•Electromyography and nerve conduction studies are useful for identifying and classifying peripheral nerve disorders affecting the upper extremity.
•Magnetic resonance imaging of the cervical spine is useful to identify disc herniation or degeneration and the degree of nerve root compression as well as to exclude the possibility of a mass lesion.
•Neuromuscular ultrasound can be helpful in assessing individual peripheral nerves in patients who present with an unusual upper extremity mononeuropathy.
•Laboratory testing and cerebrospinal fluid analysis are generally reserved for patients with conditions associated with an inflammatory, infectious, or endocrine source.
●Median neuropathies
•Carpal tunnel syndrome is the most common upper extremity mononeuropathy. Typical symptoms include pain or paresthesia in a distribution that includes the median nerve territory, with involvement of the lateral portion of the hand. The symptoms are typically worse at night and characteristically awaken affected individuals from sleep.
•Less common median nerve syndromes include entrapment where the median nerve passes through the pronator teres muscle and injury to the anterior interosseous nerve that branches at the elbow.
●Ulnar neuropathy – Ulnar neuropathy at the elbow is the second most common compression neuropathy affecting the upper extremities. Symptoms include sensory loss and paresthesias over digits 4 and 5 and weakness of the interosseous muscles of the hand in severe cases.
●Radial nerve syndromes – With compression of the radial nerve at the spiral groove, the triceps retains full strength, but there is weakness of the wrist extensors (ie, wrist drop), finger extensors, and brachioradialis. Sensory loss is present over the dorsum of the hand and may extend up the posterior forearm. With posterior interosseous neuropathy, forearm pain and weakness of finger dorsiflexion is typical.
●Proximal neuropathies – Several uncommon proximal focal neuropathies of the upper extremity typically present with pain and sensorimotor impairment. These include suprascapular neuropathy, long thoracic neuropathy, axillary neuropathy, spinal accessory neuropathy, and musculocutaneous neuropathy.
●Brachial plexopathy – The brachial plexus is vulnerable to trauma and may be affected secondarily by disorders involving adjacent structures. Most brachial plexus disorders show a regional involvement rather than involvement of the entire brachial plexus.
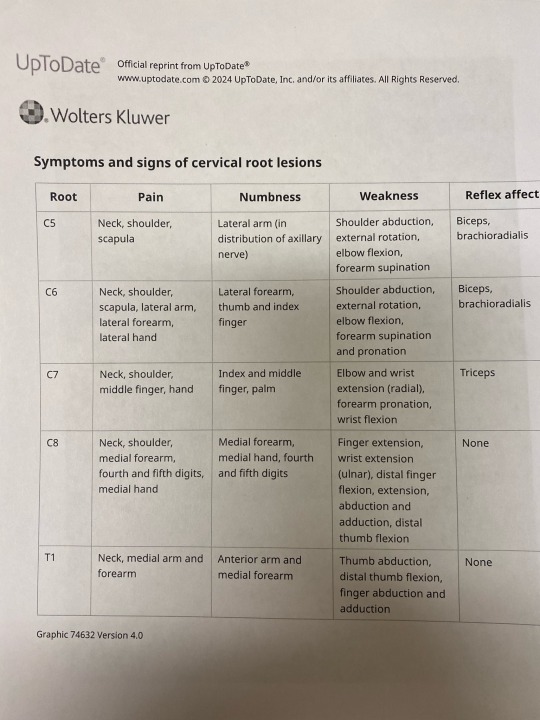
●Cervical radiculopathy – Cervical radiculopathy is a common cause of both acute and chronic neck pain. Most radiculopathies arise from nerve root compression due to cervical spondylosis and/or disc herniation. Lower cervical roots, particularly C7, are more frequently affected by compression.
●Other syndromes – Additional uncommon peripheral nerve syndromes affecting the upper extremities include focal amyotrophy, mononeuropathy multiplex, multifocal motor neuropathy (MMN), and zoster radiculoganglionitis.
4 notes
·
View notes
Text

🇫🇷 La missionnaire Ana Clara Schindler a témoigné par sa propre vie de la grandeur de la grâce de Dieu. À l'âge de six mois, on lui a diagnostiqué une amyotrophie spinale, une maladie dégénérative rare qui provoque une faiblesse et une paralysie musculaire progressive.
Elle s'est convertie à 14 ans grâce à un chrétien qu'elle a rencontré sur Internet. Des années après sa conversion, elle s'est davantage consacrée à sa relation avec le Seigneur et à l'étude de la Bible. Son intérêt pour les missions est né grâce au missionnaire Luca Martini, lorsqu'elle a regardé une vidéo dans laquelle il priait pour un homme qui avait des difficultés motrices, et l'homme a été guéri.
Dès lors, Ana Clara a été motivée pour s'inscrire dans une école missionnaire du Mouvement Dunamis appelée "Projet 21". Au cours de ces trois années de mission, Ana Clara a effectué cinq voyages missionnaires et est en route pour le sixième, qui sera au Japon. « Je me déplace par la voix de Dieu. Chaque fois qu'il donne la direction, je vais », a déclaré le missionnaire.
"Jésus est venu et a accompli son ministère même s'il savait qu'il allait mourir sur une croix. Alors, il semble que je ne remplirai pas ma vocation à cause des difficultés rencontrées en cours de route. Je crois en un Dieu qui a séparé la mer Rouge, donc même si je ne vois pas la rampe, elle est déjà là », a déclaré Ana Clara | Source : Guiame.
« Qu'ils sont beaux les pieds de celui qui apporte de bonnes nouvelles » Esaïe 52:7 🔥
#adoration #louange #worship #gospel #evangile #bible #chrétien #covergospel #medley #gospelmusic #jesuschrist #louvor #adoracao #praise #cristo #amém #jesuscristo #musique #Actualité #Afrique #música #Africa #brasil #evangelho #novidades #clipe #novidade #viral #news #gospelnews
0 notes
Text
Motor Neuron Disease.
Motor Neuron Disease.
Guillain Barre syndrome.
Hirayama disease.
Oblique amyotrophy.
Muscular atrophy.
Spinal muscular atrophy.
Brachial plexus injury.
Polio.
Leprosy.
Stroke.
Paralytic condition.
The disease is considered to be affection of the brain and the spinal cord or nervous system .There can be varied presentations.
One or more muscles may not work optimally. This causes inability to move one or more joints of the finger or wrist.
Conventional neurology teaches muscle strengthening as the treatment. This may be of frustratingly of limited usefulness.
We aim to significantly improve the function of the affected hand through surgery.
For example, the person may not be able to lift up(extend) the finger. Or he may not be able to lift up(extend) the thumb.
It may not be possible to surgically manage the brain in this condition. But a more straight forward approach is to reshuffle the muscles of the hand in such a way that the weak muscles are augmented using certain sparable muscles.
An analogy is if in an organization 10 people are working and 3 go on leave.
The organization is not shut down but the available manpower is reshuffled to carry on the routine business.
Similarly in a hand, if a certain more necessary muscle has become inactive, a sparable muscle is utilized to best restore the function.
This forms the basis of surgery in a weak hand or a paralyzed hand.
The general principle of treatment remains the same in all these conditions.
The more required functions are restored and augmented by transferring sparable muscles. Nature has provided numerous sparable muscles.
Like a person has two kidneys but can live life normally with only one.
Once the disease has stopped progressing and the weakness is not worsening, the patient is evaluated for remedial measures.
The remedy is to restore the function of the finger and the hand by surgery on the forearm or wrist and fingers.
The spine or the brain is not surgically treated.
0 notes
Text
What is brachial neuritis?

Brachial neuritis is a kind of peripheral neuropathy that affects the nerves that run from the chest to the shoulder, arm, and hand. Peripheral neuropathy is a condition that causes discomfort or loss of function in the nerves that transmit information from the brain and spinal cord (the central nervous system) to other regions of the body. Brachial neuritis is a rather uncommon disorder.
Brachial neuritis is also known as brachial neuropathy or damage to the brachial plexus. The injury to the brachial nerves happens quickly and unexpectedly in acute brachial neuritis. It isn't related to any other injury or health condition. This condition is also known as Parsonage-Turner syndrome or neuralgic amyotrophy.
Brachial neuritis mostly affects the lower brachial plexus nerves in the arm and hand. The brachial plexus is a network of nerves that connects the spinal cord to the chest, shoulder, arms, and hands. Typically, this illness affects just one side of the body. However, it may also affect other nerves and regions of the body.
If you are facing any signs of brain injury, Call Dr. Amit Shah one of the best Neurologist in Mumbai.
0 notes
Text
Is There A Neck-Shoulder Syndrome?| Lupine Publishers

Lupine Publishers| Anesthesia and pain medicine Journal
Abstract
Concomitant presentation of neck and shoulder pain is a common clinical scenario which can present a significant diagnostic and therapeutic dilemma. Neck and shoulder pain presentations can be separated into four different categories: Primary neck pathology with referred pain to the shoulder, primary shoulder pathology with referred pain to the neck, primary neck and primary shoulder pathology, and primary neck pathology resulting in secondary shoulder pathology. Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible but not proven. Authors are proposing this scenario to be described as “neck-shoulder syndrome.” For instance, C5 and/or C6 cervical radiculopathy can result in rotator cuff, deltoid, biceps and scapular muscle weakness as these nerve roots innervate the shoulder girdle musculature which in turn could produce shoulder/scapular muscle imbalance resulting in shoulder impingement signs. A patient may present with features of both cervical radiculopathy and shoulder impingement syndrome in this scenario. At this time there are no agreed clinical criteria for a diagnosis of “neck-shoulder syndrome.” As with any other syndrome, management differences can only be well studied once the entity has been properly defined. In this article, authors set out to summarize how to best approach patients presenting with both neck and shoulder pain while describing features of proposed “neck-shoulder syndrome.” It is paramount to take a comprehensive and holistic approach towards patients presenting with concomitant neck and shoulder pain as the symptoms may not always represent isolated entities.
Keywords: Neck and shoulder pain; Neck-shoulder syndrome; Pain treatment; Differential diagnosis of neck and shoulder pain
Introduction
Co-existent neck and shoulder pain has been described in limited fashion in the literature as a unique diagnosis, but the concomitant presentation of neck and shoulder pain is a common scenario in primary care and orthopedic offices [1,2]. Gorski et al described “shoulder impingement syndrome” where patients presented with neck pain secondary to rotator cuff tendinopathy [1]. Compere et al described a “neck, shoulder, and arm syndrome” which primarily referred to neuropathic pain in the neck, shoulder and arm resulting from a brachial plexus lesion [2]. When patients present with both neck and shoulder pain, it can present a significant diagnostic dilemma[3]. “Hip spine syndrome” has recently been described, and “neck-shoulder syndrome” likely represents an analogous entity involving the cervical spine and upper limb [4]. It is estimated that among primary care office visits, neck pain accounts for approximately 20-30% and shoulder pain for 10-20% of musculoskeletal complaints. From this population, combined neck and shoulder problems account for approximately 6-10% [3,5,6,7].
Discussion
Concomitant neck and shoulder pain presentations can be separated into four different categories: Primary neck pathology with referred pain to the shoulder, primary shoulder pathology with referred pain to the neck, primary neck and primary shoulder pathology, and primary neck pathology resulting in secondary shoulder pathology
Primary neck pathology with referred pain to the shoulder
An isolated C5 and/or C6 radiculopathy without shoulder pathology could certainly present with neck and shoulder pain due to C5 and C6 dermatomal symptoms corresponding to the shoulder region. C5 or C6 myotomal pain can cause pain in the deltoid, scapula and biceps, and can mimic shoulder pathology [8,9]. This scenario is typically straightforward as the physical examination will be absent of shoulder impingement signs. Classically, cervical radiculopathy examination can demonstrate positive cervical root impingement signs (Spurling’s maneuver), myotomal weakness, dermatomal sensory abnormalities and blunted reflexes in a specific root distribution. Several neuropathies involving brachial plexus and its proximal branches will also refer pain to neck and shoulder simultaneously.
Primary shoulder pathology with referred pain to the neck
Primary shoulder pathology should not directly lead to neck pathology, and such cases are not well described in the literature. Nevertheless, patients with shoulder pathology may develop pain and tightness in the trapezius muscle on the ipsilateral side and referred pain in the cervical area. Restricted motion at the glenohumeral joint may also lead to overuse and pain in the scapulothoracic musculature. A general concern in musculoskeletal medicine is that symptomatic pathology in a joint may refer pain to a joint below and/or above.
Primary neck and primary shoulder pathology
Degenerative arthritis can affect multiple joints. Thus, many patients may have both glenohumeral arthritis and cervical spondylosis. The radiographic incidence of glenohumeral arthritis is reported as 32.8% in people over 60 years of age [10]. Radiographic evidence of cervical spondylosis is present in 50% of people over 50 years of age and 75% of individuals over 65 years of age [11]. As both conditions are common, both can present as “pain generators.”
Primary neck pathology resulting in secondary shoulder pathology
Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible although not proven. For instance, C5 and/or C6 cervical radiculopathy can result in rotator cuff, deltoid, biceps and scapular muscle weakness as these nerve roots innervate the shoulder girdle musculature. This could produce muscle imbalance and poor shoulder/scapular mechanics. A patient may present with features of both cervical radiculopathy and shoulder impingement syndrome in this scenario. In clinical practice, it is not uncommon to see a patient with chronic neck pain presenting with insidious onset of shoulder pain later in the course. Authors are proposing this unique presentation be referred to as “neck-shoulder syndrome.” Although most clinicians would treat this as separate neck and shoulder pain, they may be related diagnoses.
Literature Search
We conducted a comprehensive search in the PubMed database in order to identify relevant studies on “neck-shoulder syndrome.” Based on the review of the available literature, there are no agreed upon clinical criteria for a diagnosis of “neck-shoulder syndrome” despite its common clinical presentation nor is there a well described “neck-shoulder syndrome.” As with any other syndrome, management differences cannot actually be studied until the entity has been appropriately defined. This article will concentrate on how to best approach patients presenting with both neck and shoulder pain while describing features of proposed “neckshoulder syndrome.”
Presentation
In patients presenting with neck and shoulder pain, a thorough history is paramount in identifying the etiology of the patient’s pain.
Location: Patients with primary neck pathology can experience pain extending beyond the neck based on the etiology. Disorders that affect the lower cervical nerve roots will often result in pain distal to the shoulder which can be characterized by radiation into the arm in a clear dermatomal or myotomal distribution [12]. In addition, Dwyer et al described reproducible pain patterns that can refer into the shoulder, trapezius and occiput from cervical zygapophyseal joint pathology [13-15]. Pain from a primary shoulder problem can also refer pain to the neck, periscapular region and distally into the arm although not typically extending below the elbow [16]. Associated paresthesias are not classically associated with a primary shoulder problem.
Onset: Onset of symptoms is also a key component of the history. Degenerative cervical pathology can have insidious onset although acute disc herniations can have a sudden onset that may be precipitated by trauma. Whiplash injuries are known to precipitate neck pain which can be of myofascial and/or cervical facet in origin. Shoulder disorders can also be of insidious (overuse injuries) or acute onset (trauma). Sudden onset of shoulder pain with restricted motion can be associated with acute calcific tendinitis or adhesive capsulitis. Neuralgic amyotrophy (Parsonage Turner syndrome/ brachial neuritis) has a unique presentation where patients usually experience severe, acute pain following exercise, recent illness, immunization, surgery or trauma [17]. As the initial severe pain starts to resolve, neurological deficits will become apparent, which is in contrast to most presentations of cervical radiculopathy where pain will continue with associated neurological symptoms. Onset of symptoms plays a key role in proper identification of proposed “neck-shoulder syndrome.” Development of shoulder pain (especially in the absence of injury) after onset of neck/radicular pain can be considered primary neck pathology with secondary shoulder pathology and can be referred to as “neck-shoulder syndrome.” Shoulder pain in this scenario is likely secondary to rotator cuff and periscapular muscle weakness/imbalance caused by C5 and/or C6 cervical radiculopathy. This clinical scenario is not well studied in the literature, hence prevalence and incidence is not known. Among patients with cervical radiculopathy, studies report a frequency of C5 nerve root involvement at 5-10%, C6 at 20-25%, and C7 at 45-60% [12,18].
Exacerbating factors: Pain with overhead arm movements generally suggests primary shoulder pathology. However same pattern can also be present in peripheral neuropathies like thoracic outlet syndrome and spinal accessory, suprascapular, or axillary neuropathy. Shoulder pain with side lying on the affected upper limb tends to be associated with shoulder impingement and acromioclavicular joint arthropathy.
Features of systemic diseases: In patients who present with neck and shoulder pain in the absence of trauma, the history will need to include an assessment for widespread involvement that may suggest systemic disease processes like fibromyalgia, polymyalgia rheumatica, myofascial pain syndrome and myopathy.
Red flags: The history should also include an evaluation for findings to suggest a disease process that requires more urgent evaluation. Red-flag symptoms to assess for include gait imbalance, hand clumsiness, bowel/bladder dysfunction (cervical myelopathy), pain after high impact trauma (fractures), unintentional weight loss (Pancoast tumor), chest pain (cardiac ischemia), blurry vision, nausea/vomiting and vertigo (vertebral artery dissection/ insufficiency).
Physical Examination
In addition to a detailed history, a thorough physical examination is key for proper diagnosis and identification of the pain generator(s). A thorough neurological exam plays an essential role in distinguishing neck from shoulder pathology. Sensory, motor and reflex changes in a specific nerve root distribution are characteristic of cervical radiculopathy. C5 and C6 cervical radiculopathies may result in periscapular and shoulder/rotator cuff muscle weakness while C7 radiculopathy is unlikely to cause shoulder weakness. Rotator cuff pathology may result in shoulder weakness with preserved elbow flexion while a C5 radiculopathy can result in weakness of both. Testing deltoid strength with the arms at the sides instead of in shoulder abduction can aid in differentiating pain inhibition versus true weakness.
Provocative Testing
Provocative testing can assist in the diagnosis of cervical and shoulder disorders [9, 19]. Among them, provocative tests for shoulder impingement may help distinguish primary versus secondary shoulder pathology in proposed “neck-shoulder syndrome”(Table 1) [18-30].
In patients with neck and shoulder pain, one test by itself may not have enough sensitivity and specificity to make a diagnosis and most physical exam maneuvers are not pathognomonic. A combination of multiple exam components and a thorough history are necessary to accurately identify the etiology of symptoms.
Table 1: Provocative tests for common cervical and shoulder problems and reported validity.

Diagnostic Testing
When presented with both neck and shoulder pain, history and physical exam should dictate appropriate use of diagnostic tests. Although imaging studies such as radiography, CT and MRI can reveal many pathologies, further testing should be done to identify the true pain generator. When suspecting pain mediated by a cervical zygapophyseal joint, cervical diagnostic medial branch blocks can be considered. A shoulder injection of lidocaine with or without corticosteroid can be done for diagnostic and perhaps therapeutic reasons. In cases of secondary shoulder pathology, this may give the patient partial benefit, but a primary cervical pathology should still be investigated [9]. Electrodiagnostic testing with electromyography (EMG) and nerve conduction studies (NCS) can be employed when suspecting myopathy, brachial plexopathy, peripheral neuropathy or radiculopathy. When evaluating neck and shoulder pain, scientific evidence suggests using a combination of history, physical examination, imaging modalities, diagnostic injections and electrodiagnostic study to make the appropriate diagnosis.
Treatment
Success of any proposed treatment algorithms will depend on an accurate diagnosis. There is scant evidence on how to approach the concomitant presentation of neck and shoulder pain. Treatment should be geared toward the primary site of pathology whether it be the cervical spine or the shoulder [3]. Lack of current literature evidence underscores the importance of describing a “neckshoulder syndrome,” as it can lead to studies looking at management differences. It can be hypothesized that in patients with cervical radiculopathy with secondary rotator cuff impingement, treatment of the primary lesion will likely yield eventual improvement at the secondary site although no studies have been done on this topic.
Conclusion
The concomitant presentation of shoulder and neck pain is a common scenario in primary care and orthopedic offices and can present a diagnostic and therapeutic dilemma. A careful history and thorough physical examination along with ancillary studies can often yield the correct diagnosis and successful treatment. Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible but not proven. Authors are proposing this scenario to be described as “neck-shoulder syndrome.” Appropriately describing a “neck-shoulder syndrome” can lead to further studies looking at management differences. A prospective study looking at incidence of shoulder impingement signs in chronic C5 and/or C6 radiculopathy patients could be helpful in delineating diagnostic criteria for “neck-shoulder syndrome.” Above all, it is paramount to take a comprehensive and holistic approach towards patients presenting with concomitant neck and shoulder pain as the symptoms may not always represent isolated entities.
Acknowledgements
The authors would like to thank Dr. David Janerich for his help with the development of the article.
For more Lupine Publishers Open Access Journals Please visit our website:
https://lupinepublishers.us/
For more Global Journal of Anesthesia & Pain Medicine articles Please Click Here:
https://lupinepublishers.com/anesthesia-pain-medicine-journal/index.php
To Know More About Open Access Publishers Click on Lupine Publishers: https://lupinepublishers.com/
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
#Lupine Publishers#Lupine Publishers Group#Open Access Journals#Anesthesia Jounal#Pain medicine#pain management#general anesthesia#local anesthesia#surgery#post operative#critical care
3 notes
·
View notes
Text
Neuropathy Types of Neuropathy:
Fringe Neuropathy
Fringe diabetic neuropathy passes by different names: fringe diabetic nerve torment and distal polyneuropathy. In this Patient Guide, we'll allude to it as fringe diabetic neuropathy, or just fringe neuropathy .
Fringe neuropathy is the most widely recognized type of neuropathy brought about by diabetes. It influences nerves prompting your furthest points—to your feet, legs, hands, and arms. The nerves setting off to your feet are the longest in your body: after they branch off the spinal rope in the lumbar district (low back), they need to go right down your legs and into the feet—a significant separation for more information see Neurorehabilitation .
Since the nerves prompting your feet are so long, it's frequently these nerves that are harmed; there's a greater amount of them to be harmed. This nerve harm can prompt the foot issues regularly connected with diabetes, including foot disfigurements, diseases, ulcers, and removals.
The article on diabetic neuropathy side effects will assist you with getting familiar with the particular manifestations related with fringe diabetic neuropathy.
Proximal Neuropathy:
Proximal neuropathy can likewise be called diabetic amyotrophy. That myo in the word implies muscle, so this is a type of neuropathy that can cause muscle shortcoming. It explicitly influences the muscles in the upper piece of your leg(s), hindquarters, and hips.
Now and again, proximal neuropathy can likewise include nerve torment, particularly torment that shoots from the low back and down the leg. The specialized restorative term for that is radiculopathy, albeit the vast majority allude to it as sciatica. On the off chance that there's additionally shooting nerve torment included, this type of neuropathy can likewise be called polyradiculopathy-diabetic amyotrophy.
Proximal neuropathy is the second most normal sort of diabetic neuropathy (second just to fringe diabetic neuropathy). It for the most part influences older individuals with diabetes; instead of fringe neuropathy, it typically settle with time or treatment.
Autonomic Neuropathy:
Autonomic nerves should keep your body running as it should. There are numerous capacities that occur in your body without you contemplating them: your heart siphons, you inhale, and your stomach digests nourishment. Those activities are constrained by the autonomic sensory system; it's likewise here and there called the programmed sensory system.
The autonomic sensory system ought to keep up your body's homeostasis, which is its typical, adjusted state. In the event that the autonomic nerves are harmed by the impacts of diabetes—autonomic diabetic neuropathy—at that point your body may experience difficulty looking after homeostasis.
Autonomic neuropathy can appear to be overwhelming on the grounds that it can influence such huge numbers of your body's frameworks, from your stomach related tract to how well you can see. Be that as it may, recollect that your side effects rely upon what explicit nerves in the autonomic sensory system are harmed.

Central Neuropathy
The entirety of the kinds of diabetic neuropathy above—fringe, autonomic, and proximal—are instances of polyneuropathy. Poly implies that they influence numerous nerves. Central neuropathy, on the other hand, influences one explicit nerve; it's engaged neuropathy. It can likewise be called mononeuropathy.
Central neuropathy, which goes ahead all of a sudden, regularly influences nerves in the head (particularly ones that go to the eyes). It can likewise influence the middle and legs.
At the point when central neuropathy influences the legs, it has unexpected manifestations in comparison to proximal neuropathy, which can likewise influence the legs. Proximal neuropathy, as you can peruse above, causes muscle shortcoming in the legs, and it might likewise cause shooting torment down the leg. Central neuropathy, in any case, causes torment in unmistakable areas on the legs, which you can peruse progressively about in the indications article.
1 note
·
View note
Link
Les traitements disponibles ne concernent encore qu’une poignée de maladies. L’enjeu est celui de la bioproduction.

Il y a trente ans avait lieu le premier essai de thérapie génique. Deux enfants atteints d’un s déficit immunitaire combiné sévère (DICS par déficit enzymatique), plus communément appelé«bébés bulle», sortaient de leur environnement stérile confiné. Les résultats furent mitigés mais suffisamment encourageants pour stimuler la recherche. À cette époque, la thérapie génique visait essentiellement à remplacer les gènes originaux déficients de personnes atteintes de maladies monogéniques (liées à un seul gène déficient ou manquant). Depuis, la cible s’est élargie aux cancers.
» LIRE AUSSI - Maladies rares: les secrets de fabrication des thérapies géniques
«Comme ce fut le cas avec les greffes ou les anticorps monoclonaux, on s’est dit que cela allait révolutionner la médecine», explique Serge Braun, directeur scientifique de l’AFM-Téléthon. «Et puis en 1999, Jesse Gelsinger meurt à 18 ans, quatre jours après l’injection d’une thérapie génique» , se souvient Serge Braun. D’une défaillance multiviscérale (des organes vitaux) attribuée à la trop forte dose d’adénovirus reçue. Car déjà à cette époque, le vecteur privilégié pour transporter la thérapie génique au cœur des cellules est un adénovirus, virus du rhume bien connu des chercheurs. La mort de Jesse Gelsinger vient brutalement doucher l’enthousiasme initial.
Au total, une douzaine de médicaments innovants de thérapie génique ont été approuvés
Heureusement, les résultats d’un autre essai clinique déjà engagé en France (avec des doses d’adénovirus plus de 100 fois inférieures) vont en quelque sorte «repêcher» cette approche thérapeutique. «On doit à la France la preuve du concept de la thérapie génique», souligne Serge Braun. Le 28 avril 2000, Le Figaro titre sur le véritable «Premier succès de la thérapie génique», obtenu par l’équipe du Pr Alain Fischer (Inserm, APHP) à l’hôpital Necker à Paris, avec cinq enfants atteints du DCIS. «Aujourd’hui, pas moins de huit produits issus de Généthon sont en cours d’expérimentation clinique et trois autres devraient y entrer dans les deux années qui viennent», rappelait son directeur général, Frédéric Revah, il y a quelques mois.
Au total, une douzaine de médicaments innovants de thérapie génique ont été approuvés: Strimvelis (déficit immunitaire combiné sévère), Zalmoxis (contre le rejet de greffe de moelle osseuse), Luxturna (dystrophie rétinienne), Zolgensma (amyotrophie spinale), Zynteglo (bêta-thalassémie), Glybera (retiré du marché), Gencidine, Oncorine, Imlygic, Kymriah et Yescarta (en oncologie).
» LIRE AUSSI - Thérapie génique: un espoir majeur pour une myopathie de l’enfant
Néanmoins, au regard de l’enthousiasme médiatique que suscite la thérapie génique, on aurait pu s’attendre à davantage de médicaments disponibles. La réalité est malheureusement plus laborieuse, et les traitements commercialisés, ou en passe de l’être, ne concernent encore qu’une poignée de maladies rares.
Karen Aiach, mère d’une patiente atteinte du syndrome de Sanfilippo, a fondé et dirige Lysogene, à la recherche de solutions thérapeutiques. Elle craint paradoxalement que l’enthousiasme actuel des industriels pour la thérapie génique ne bénéficie pas tant que cela aux maladies rares. «J’ose espérer que les maladies rares ne soient pas juste un prétexte pour développer de nouvelles technologies», expliquait-elle le 20 juin dernier lors d’un colloque organisé par la revue spécialisée Pharmaceutiques.
L’inquiétude du Dr Geraldine Honnet, directrice du développement clinique de Généthon, porte sur la bioproduction. Elle se demande si la France sera capable de produire suffisamment de vecteurs viraux pour les thérapies géniques qui s’annoncent. «Il en faut des doses énormes, explique-t-elle. À tel point qu’un industriel a de lui-même décidé de limiter les indications de son traitement, Zolgensma, à des enfants de moins de 2 ans. Cela montre bien que les enjeux de la bioproduction sont énormes.»
2 notes
·
View notes
Text
If you haven’t heard of Hirayama’s Disease before, you’re not alone. Hirayama’s Disease is a neurological condition that primarily affects the lower cervical cord in young males, and is classed as a rare disease. Little is known about how it works, but the good news is that it’s not as serious as it may sound. Here, we offer a brief introduction to what Hirayama’s Disease looks like.
Understanding Hirayama’s Disease
Hirayama’s Disease is a rare neurological condition that causes gradually progressive atrophy of the muscles in the arms and forearms. Also known as monomeric amyotrophy (MMA), it primarily impacts young males in their late teens and early twenties. It was first defined by Keizo Hiramaya in Japan in 1959 as juvenile muscular atrophy. Hirayama’s Disease primarily affects young males in countries like India, Sri Lanka, Japan, Taiwan, and Singapore, although there have been cases in non-Asian countries too. The disease typically progresses the fastest in the first few years before stabilizing by itself.
Symptoms for Hirayama’s Disease
Typically, Hirayama’s Disease will manifest as a sudden weakness in one or both arms, leading to difficulty performing daily activities like writing or playing games. The classic symptoms for Hirayama’s Disease include:
Weakness in the hands and/or forearms
A ‘wasted’ appearance of the hands
Tremors in the hands
Unilateral / asymmetrically bilateral muscular atrophy
Excessive sweating of the palms
Impaired palmar grasp (the reflex by which one instinctively grasps something placed in the hand)
Hypertonia (in some cases)
Mild worsening of symptoms when exposed to the cold
Slow progression in the initial years followed by spontaneous stabilization
It is the disease’s tendency to stabilize it on its own, that separates it from motor neuron disease, which it is often mistaken for. There is also no sensory impairment in the hands.
Diagnosing Hirayama’s Disease
Patients who have been exhibiting symptoms for Hirayama’s Disease should visit the clinic right away. The doctor will examine the patient’s medical history and take notes on any family history of neurological conditions, before running multiple tests including blood, stool, thyroid, and urine. The diagnosis of Hirayama’s Disease is typically by exclusion, once the doctor has ruled out other possible culprits such as motor neuron disease, brachial plexopathy, multifocal motor neuropathy, and spinal cord tumours. An MRI can also detect signs like asymmetric Spinal Cord Atrophy, upper motor neuron lesions, and forward displacement of the posterior subdural sac upon neck flexion.
Treatment for Hirayama’s Disease
Hirayama’s Disease is a self-limiting condition, as the progression stabilizes on its own after some years. In addition, regular physiotherapy can help to restore strength in the arm and hand muscles and avoid secondary problems like joint stiffness or immobility.
In short, while it may be alarming to suddenly feel your hands and arms become weaker, Hirayama’s Disease is among the least serious forms of atrophy and will in fact cease progressing on its own. With early detection and intervention, you can keep the symptoms well under control and enjoy all the activities you love.
0 notes
Text
Téléthon 2021 : "C'est grâce aux dons que je peux encore faire quelques pas aujourd'hui"
A l'occasion du lancement de la 35ème édition du Téléthon, France Bleu Saint-Étienne Loire recevait ce vendredi Colette Espigolé, coordinatrice de l'AMF Téléthon Loire Sud et Abdel Makhlouf, parrain ligérien de l'événement depuis 2015.
Un seul numéro à retenir ce week-end : le 36-37. La 35ème édition du Téléthon commence ce vendredi dans toute la France. Dans la Loire, environ 90 événements sont organisés pour récolter des fonds et financer la recherche sur les maladies génétiques. L'an dernier, le Téléthon avait permis de récolter plus de 77 millions d'euros. "On espère faire aussi bien et même plus cette année", confie Colette Espignolé, la coordinatrice de l'AMF Sud Loire, qui était notre invitée ce matin, en compagnie d'Abdel Makhlouf, parrain ligérien du Téléthon depuis 2015.
Chaque euro compte
"La recherche, ça coûte des dizaines de millions d'euros", confie le trentenaire, atteint d'une amyotrophie spinale de type 3 qui empêche ses muscles de fonctionner correctement. "Mais elle permet vraiment d'améliorer le quotidien des malades. Dans mon cas, des chercheurs parisiens ont développer un médicament à prendre tous les 4 mois qui retarde le développement de ma maladie. Aujourd'hui, je suis encore capable de faire quelques pas à la maison, ce ne serait pas le cas sans ce médicament. Tout ça, c'est grâce au Téléthon. Il n'y a pas de petit don, même un euro ça sert."
L'AMF Téléthon aide aussi les malades dans l'achat de matériel, quand les mutuelles et la sécurité sociale ne remboursent pas tout. Enfin, l'argent récolté via les dons permet aussi de faire progresser la recherche sur la génétique en générale. "Pendant des années je n'ai pas voulu d'enfant, par crainte de transmettre ma maladie, mais aujourd'hui grâce à la recherche, je suis papa de deux petites filles", explique Abdel Makhlouf. "Je suis très content." Sexy Gaming
0 notes
Text
Société : Le handicap s’expose
En septembre dernier, à l’occasion de la rentrée des classes, la marque Kiabi lançait une campagne de publicité qui a fait parler d’elle. La raison ? Parmi les enfants souriants et portant des tenues colorées se trouvait un petit garçon en fauteuil roulant : Loukas, 5 ans, atteint d’une amyotrophie spinale, maladie d’origine génétique l’empêchant de marcher. Quelques mois auparavant, la marque américaine d’alimentation infantile Gerber annonçait que l’heureux gagnant de son concours du plus beau poupon de l’année était remporté par Lucas Warren, petit garçon de 18 mois atteint de trisomie 21. Pour la première fois, la filiale du géant Nestlé qui, chaque année, choisit un « ambassadeur » parmi le public, sélectionnait un enfant porteur de handicap sur les 140 000 candidatures reçues. Que deux marques qui s’adressent à un très large public décident de communiquer avec un enfant « hors norme » a de quoi interroger. Cherchent-elles simplement à faire le buzz ? Ou faut-il y voir le signe d’une société plus inclusive ?
Se différencier et être plus proche de la réalité
« Pour les marques, choisir des égéries “hors norme” est l’occasion de se démarquer », analyse Nathalie Fleck, professeur en marketing à Le Mans Université, spécialiste de la communication des marques. « En mettant en avant des personnes au physique étonnant ou avec une particularité comme un handicap, elles souhaitent créer un effet de surprise. L’objectif est d’émerger et de faire parler d’elles auprès des consommateurs et dans les médias. » Un coup marketing pour se différencier de leurs concurrents ? Pas seulement. « Il y a une réelle prise de conscience du décalage trop important entre les photographies de publicité et la réalité, assure Nathalie Fleck. Il a été prouvé que l’image que l’on construit de soi dépend de celles vues dans les publicités, sur les défilés ou dans les médias. Les marques savent qu’elles ont une responsabilité et ne veulent pas être blâmées pour cela : elles cherchent désormais à être plus proches de la réalité dans leur communication. » Pour les annonceurs, choisir une égérie inattendue atteinte d’un handicap ou d ’une maladie, c’est aussi l’occasion de se positionner comme une marque tolérante. « Les entreprises d’aujourd’hui cherchent à communiquer sur leur image, à montrer qu’elles sont insérées dans la société, et qu’elles ne cherchent pas le profit avant tout, avance Nathalie Fleck. Cela passe par le choix des égéries, mais aussi par le sponsoring, le mécénat… Des actions qui leur permettent de se positionner comme altruistes, humanistes mais aussi comme des entreprises qui prônent la diversité, la tolérance, l’inclusion. » Des valeurs positives et dans l’air du temps.
Communiquer sur l’inclusion doit avoir du sens
Pour Kiabi, le choix d’un petit garçon en fauteuil roulant n’a pas été fait au hasard. Depuis 2017, avec Les Loups bleus – première marque de vêtements adaptés aux enfants, adolescents et adultes porteurs de handicap ou en situation de motricité réduite –, l’enseigne propose en effet des collections spécifiques, avec, par exemple, davantage de pressions pour être enfilées facilement. « Nous voulons rendre visible la pluralité au travers d’une communication plus inclusive illustrant toutes les morphologies, l’intergénérationnel et les personnes en situation de handicap, indique Elisabeth Fauvarque, responsable de la communication chez Kiabi. Il ne s’agit pas d’un effet de communication ni d’une tendance, nous pensons que cela répond à nos valeurs et à notre mission qui est d’offrir au monde du bonheur à porter. » Parfois, la présence d’un enfant différent sur une photo publicitaire s’explique par une histoire plus personnelle. Aux États-Unis, si la marque Napaani, connue pour ses vêtements composés de matières 100 % naturelles et bio, a ainsi fait poser pour les visuels de ses collections de ravissantes petites filles trisomiques, c’est parce que sa créatrice est particulièrement sensible à ce sujet. « Je suis la maman d’une enfant, aujourd’hui adulte, qui a cette différence, explique María Teresa Larrondo. Si nous incluons des enfants avec des particularités dans nos photos de communication, c’est parce que nous souhaitons leur intégration dans la société. Nous voulons dire au monde entier qu’ils n’ont pas de handicap mais simplement des besoins particuliers. »
Être irréprochable sur la question du handicap
Les marques qui exposent des enfants différents pour promouvoir l’inclusion ont intérêt à être vigilantes : elles ne doivent pas être attaquables sur la question du handicap. « Le choix d’une égérie ou d’un mannequin, ce n’est pas qu’une image, rappelle Nathalie Fleck. Elles doivent être irréprochables sur ce thème : embauchent-elles réellement des personnes handicapées ? Aménagent-elles leurs locaux pour recevoir ce type de public ? Existe-t-il des actions fortes sur ce thème ou n’est-ce qu’un discours ? Si ce n’est pas le cas, et que cela vient à se savoir, la situation peut tourner au fiasco… »
Des parents actifs sur les réseaux sociaux
Sur Instagram et sur Facebook, les enfants porteurs de handicap, atteints d’une maladie rare ou de troubles autistiques sévères, sont aussi davantage visibles. Sur des comptes dédiés en accès libre, leurs parents y dévoilent leur quotidien. Avec les dizaines de milliers de personnes qui les suivent, ils partagent leurs difficultés, leurs joies, parfois le combat contre la maladie ou les ennuis avec l’administration, les relations avec le corps médical, avec la famille, l’école… C’est le cas de la page Louise and Co. (facebook.com/extralouise), où les parents d’une petite fille trisomique de 5 ans racontent une partie de sa vie à 36 000 followers, grâce à des photos et des vidéos. « En 2005, sur mon compte Facebook, j’ai publié un message pour appeler à changer de regard sur la trisomie et faire prendre conscience de la maladresse face au handicap, raconte Caroline Boudet, sa maman. Repris par les médias, il a fait le tour du monde et a été “liké” plus d’un million de fois ! Avec son père, nous avons donc décidé d’ouvrir une page dédiée à notre fille pour continuer à lutter contre les idées reçues sur sa maladie. »
Changer de regard sur la différence
En montrant Louise qui aime danser, qui est heureuse d’aller à l’école, ou qui réalise des progrès, ses parents cherchent à démystifier la maladie et à montrer à quel point son existence et celle de sa famille ressemblent à celles des autres. Ses followers, depuis sa naissance, se sont attachés à elle et à son histoire, comme en témoignent les nombreux messages qu’elle reçoit et même les cadeaux qui lui sont parfois envoyés. « Notre page nous sert également à dénoncer les difficultés rencontrées, comme la scolarisation, pour laquelle il faut vraiment se battre, s’emporte Caroline Boudet qui vient de sortir un livre sur le sujet (L’Effet Louise, Stock, 2020). Nous échangeons entre parents d’enfants porteurs de trisomie confrontés aux mêmes situations, cela nous permet de nous soutenir, de partager des informations. Mais nous répondons aussi aux messages de nombreux couples qui viennent d’apprendre le diagnostic et qui sont totalement désemparés… » Si les parents de Louise sont actifs, c’est qu’ils pensent qu’il y a encore un grand manque de pédagogie vis-à-vis des personnes porteuses de ce handicap et que cela nuit à leur bonne intégration. Les montrer, les raconter, les rendre visibles est pour eux une forme de militantisme. « Je pensais connaître la trisomie 21 mais j’avais un a priori très négatif, sombre, avant d’avoir ma fille, reconnaît Caroline Boudet. Si j’avais côtoyé des personnes dans cette situation, si j’avais eu plus de connaissance sur la trisomie, j’aurais été moins perdue lorsque l’on m’a annoncé à sa naissance que mon bébé avait un chromosome en plus. »
Davantage de personnes en situation de handicap dans les médias
Voilà pourquoi les parents de Louise, comme de nombreux autres, se réjouissent que les médias accordent de plus en plus de place au handicap : dans les téléfilms, les émissions de divertissement comme « Danse avec les stars » qui a été remporté par un champion handisport, les séries comme Vestiaires sur France 2, dont les deux personnages principaux sont des nageurs en situation de handicap, ou encore Plus belle la vie, qui a intégré à son casting un acteur atteint de trisomie 21. « La visibilité est essentielle, car c’est signifier que les personnes malades ou porteuses d’un handicap existent, assure Sonia Ahehehinnou, porte parole de l’Unapei (Union nationale des associations de parents, de personnes handicapées mentales et de leurs amis). C’est un moyen de changer le regard du grand public, en faisant de la pédagogie. »
Si, auparavant, lorsque des inconnus étaient confrontés à un enfant avec un comportement atypique, ils pouvaient le qualifier de fou, de marginal ou de mal élevé, aujourd’hui ils savent qu’il peut s’agir d’un trouble du spectre autistique, ou d’un autre handicap. Cette médiatisation permet à ceux qui n’y sont pas confrontés de réaliser les difficultés que rencontrent les personnes différentes et leurs proches, mais aussi les grands points communs avec le reste de la population. « Cela participe à la déstigmatisation de la différence, se réjouit Sonia Ahehehinnou. Moi qui suis maman d’une jeune fille handicapée de 14 ans, j’observe que les regards ont commencé à changer : il y a moins de méchanceté, d’incompréhension, de remarques désagréables… Beaucoup reste à faire, bien sûr, mais les améliorations sont notables. » Pour que cela continue, nous avons tous un rôle à jouer en adoptant le bon regard et en expliquant à nos enfants que les particularités, les différences ne sont pas des tabous ni des défauts. Comme on peut le lire sur la page Facebook du petit Marcel, 4 ans, porteur de trisomie 21 (facebook.com/ lextraordinairemarcel), « si nous étions tous pareils, le monde serait bien ennuyant… »
Source link
The post Société : Le handicap s’expose appeared first on Trends Dress.
from Trends Dress https://trendsdress.com/societe-le-handicap-sexpose/
0 notes
Text
What is brachial neuritis? | Neurologist in Mumbai | Dr. Amit Shah

Brachial neuritis is a kind of peripheral neuropathy that affects the nerves that run from the chest to the shoulder, arm, and hand. Peripheral neuropathy is a condition that causes discomfort or loss of function in the nerves that transmit information from the brain and spinal cord (the central nervous system) to other regions of the body. Brachial neuritis is a rather uncommon disorder.
Brachial neuritis is also known as brachial neuropathy or damage to the brachial plexus. The injury to the brachial nerves happens quickly and unexpectedly in acute brachial neuritis. It isn't related to any other injury or health condition. This condition is also known as Parsonage-Turner syndrome or neuralgic amyotrophy.
Brachial neuritis mostly affects the lower brachial plexus nerves in the arm and hand. The brachial plexus is a network of nerves that connects the spinal cord to the chest, shoulder, arms, and hands. Typically, this illness affects just one side of the body. However, it may also affect other nerves and regions of the body.
Call Dr. Amit Shah | Neurologist in Mumbai - 9819561456
0 notes
Photo

This is Thomas, he has spinal amyotrophy but he is the toughest and kindest little boy I know and he puts a smile on my face everyday. I want him to have the spotlight for a bit and if you guys could help him it'd be awesome :) via /r/MadeMeSmile http://ift.tt/2xdzpZf
#MadeMeSmile This is Thomas#he has spinal amyotrophy but he is the toughest and kindest little boy I
0 notes
Text
what is a muscle?
01.10.2020
Definition: what is a muscle?
Muscles are contractile tissues that allow the performance of different gestures and in particular to animate certain parts of the body. The shape of the muscles can be elongated, flat, or circular depending on their position in their body and their function. All the muscles of the body represent 30 to 40% of the total body weight. They are mainly made up of water (80%), but also contain proteins (17%), glycogen (1%), lipids (1%), and mineral salts (1%).
List of main muscles
The muscles are divided into muscle groups according to their anatomical location and their common function:
The muscles of the head controlling the movements of the eyes and the face to show expressions but also to allow chewing for example. We mainly find the masseter, zygomatic, occipitofrontal, or orbital muscle of the lips or the corrugator (around the eyes).
The muscles of the neck which allow the head to be oriented in all directions and the shoulders to be raised. We mainly find the scalene muscles, the sternocleidomastoid muscle, or the trapezius muscles.
The muscles of the trunk are only involved in breathing and movement of the spine. The diaphragm muscle is one of the most important, but we also find the pectoralis major, the deltoids, the latissimus dorsi, the intercostal muscles, the square muscle of the lower back or the erector muscles of the spine.
The muscles of the upper limbs such as the biceps, triceps, forearm flexors, or forearm extensors and muscles of the fingers, which are used to pick up objects, lift, throw or throw raise your arms.
The muscles of the lower limbs such as the glutes, abductors, adductors, hamstrings, quadriceps, twins, or t muss of the feet that allow walking, running, sitting, g, or jumping.
Smooth muscles, such as those found in the stomach, on without voluntary stimulus (i.e. withoualannl).
The striated heart muscle (the myocardium) which is a muscle different from others, in particular, because it is subject to the influence of hormones, and contracts involuntarily.
The skeletal striated muscles which are linked to the bones and allow movement. They are controlled by the will.
Examples of muscle diseases
The muscle can be the seat of various pathologies:
Myoma, a benign tumor of muscle tissue, which can affect any smooth muscle tissue or, more rarely, striated muscle fibers such as the myocardium and skeletal muscles.
Myopathies, muscle diseases that cause muscle weakness or exercise intolerance with pain, cramps, and a feeling of exhaustion. They can go as far as episodes of muscle destruction (rhabdomyolysis) caused by exercise. They are mostly genetic and for the moment difficult to treat.
Neuromuscular diseases that affect the nerve cells that control muscles. They often cause muscle atrophy, ie loss of volume and function. This is the case, for example, with spinal amyotrophies, amyotrophic lateral sclerosis, peripheral neuropathies, or myasthenia gravis.
Trauma (especially in athletes), which can appear suddenly or chronically. They usually cause pain during or after exercise with functional impairment. They range from simple contracture or stiffness to elongate even tearing (straining).
My advice
To prevent muscle problems during physical activity, remember to warm-up well before exercise, to drink during exercise, and to stretch afterward. In case of pain or discomfort, it is advisable to stop all activity and consult your doctor.
from Blogger http://goodhealthtipsideas.blogspot.com/2020/09/what-is-muscle_5.html
0 notes