#drops started out as a bed app but eventually became one of my daily routine apps
Text
inspiring myself to go to bed by saying that i get to play my fun and gamified korean learning apps
#trying to make duolingo one of these it’s been a good app for bed in the week i’ve been using it so far#i finally gained enough of an intuitive grasp of the language after four months of serious study that i can use it again lmaooooo#it’s great for vocab!! i like the wacky scenario aspect of it for that#drops started out as a bed app but eventually became one of my daily routine apps#was not quite gamified enough for Fun#memrise and lingodeer are my other two daily apps and i love them both so very much#my sejong class has been on a break week for the comeback and i’ve been missing it so dearly#not only has it seriously elevated my comprehension but it kept my sleep schedule reasonable bc it’s a 9 AM class twice a week hfhfngnfn#and i finally started doing HTSK……… i’m only on the first lesson but i just KNOW it’s gonna be a game changer for me#especially bc quite thorough notes are required for the club assignments#hahaha#i can play my fun and gamified apps#or i can write an essay in the tags about my daily korean routine#OH i also write a journal entry every day#usually only one or two sentences but it’s the repetition that matters not the quantity#ok i’m really going to bed now lmao#korean langblr#bangtan academy#welcome to textas
6 notes
·
View notes
Link
Freshman Bailey Cabrera never imagined a pandemic would force her to begin her first year of college at the University of Redlands from her Bakersfield bedroom.
But when the university opened its dorms in January for spring semester, she jumped at the chance to move on campus.
“I wanted to get as much of a college experience that I could, no matter how modified,” said Cabrera, 18. “… Now, living on campus, I feel more like an adult, with higher expectations and responsibilities.”
But with Inland Empire universities mostly shuttered for in-person classes, students like Cabrera who live on campus are having to adjust to a lonelier, socially distant, “ghost town” college experience.
Many Inland universities — including UC Riverside, the University of Redlands, Cal Poly Pomona and Cal State San Bernardino — have scaled back their dorms and residence halls to less than half capacity in hopes of curbing the spread of COVID-19. Gone is the tradition of a college roommate, as students now live alone to minimize their exposure. Students take classes from laptops in their rooms. Wearing masks, they eat together spaced out in quads. And some schools have added a new ritual for students — regular coronavirus tests.
UC Riverside first-year students Luis Sandoval, 18, left, Marjorie Serrano, 18, middle, and Miezue Primo, 18, finger paint as they interact with their resident adviser via Zoom at Pentland Hills Residence Hall on Oct. 12, 2020. (Photo courtesy of Stan Lim, UC Riverside)
Rajbeer Sahi, a registered nurse for UC Riverside’s Student Health Services, looks to make sure a coronavirus test is done properly by student Christian Arguelles on Sept. 28, 2020, at the Pentland Bear Cave. The test requires the subject to extract saliva and place it into a tube. (Photo courtesy of Stan Lim, UC Riverside)
Sound
The gallery will resume inseconds
Resident adviser Thomas Valenzuela, checks in with first-year student Prabhnoor “Noor” Kaur on Zoom from his room at Pentland Hills Residence Hall on Oct. 12, 2020. Resident advisers such as Valenzuela are finding ways to interact with students safely during the pandemic. (Photo courtesy of Stan Lim, UC Riverside)
UC Riverside student Christian Arguelles takes a COVID-19 test Sept. 28, 2020, at the Pentland Bear Cave. (Photo courtesy of Stan Lim, UC Riverside)
First-year students line up to receive paint supplies from their resident adviser Thomas Valenzuela at Pentland Hills Residence Hall on Oct. 12, 2020. Valenzuela did a finger-painting activity with his students through Zoom as a way to interact with them safely. (Photo courtesy of Stan Lim, UC Riverside)
UC Riverside student Killian Andrews, 18, interacts with resident adviser Thomas Valenzuela and other students through Zoom from his room at Pentland Hills Residence Hall on Oct. 12, 2020. (Photo courtesy of Stan Lim, UC Riverside)
Show Caption
of
Expand
The few who live on Inland campuses are a diverse group, but include athletes, those whose homes are far away, students with campus jobs, and those with specific needs or who have learning issues at home.
After mostly switching to online courses when the pandemic struck in March, some colleges, including UC Riverside and the Cal State universities, began to slowly reopen some facilities as the 2020-21 school year started.
At Redlands, campus residents are down from 1,600 in a typical year to about 600 now, according to university spokeswoman Jennifer Dobbs.
UC Riverside has nearly 2,000 students in three residence halls this quarter — far fewer than the more than 7,000 students living in campus residence halls, apartments and family housing during a normal school year, according to housing staff.
Cal State San Bernardino has about 200 students in two apartment villages, down from the usual 1,700 residents. And Cal Poly Pomona, which typically houses 4,000 students, has about 270 undergraduates in suites and apartments this semester, staff said.

Bailey Cabrera, 18, is a freshman at the University of Redlands and a vocal music education major. While living alone on campus during the coronavirus pandemic, she enjoys singing and playing music in her makeshift dorm room studio. (Photo courtesy of Bailey Cabrera)
For Cabrera, in addition to her seven classes on Zoom, the vocal music education major practices trumpet and piano from a makeshift “recording studio” — the extra bed in her dorm room. She and friends in the ensemble choir sometimes meet off campus to practice, socially distant, while wearing masks.
Music, she says, keeps her motivated while in solitude. She also enjoys caring for her room’s growing plant collection.
“It’s different for sure, but (it) brings a different kind of joy in the lockdown,” Cabrera said.
At Cal Poly, Hazar Eldick, a junior liberal studies major from Irvine, still remembers having to move out of her school’s new residence halls when classes went fully online.
“The energy was kind of sad,” she said.
Eldick, 21, was excited to move back on campus in fall as a resident adviser. She takes classes and stays virtually involved with her sorority. Such community, she said, has given her a sense of normalcy that “most students don’t have now.”
“Things stopped and it was like, wow, I have so much time with myself,” she said. “I had to learn to be OK with that, find ways to stay connected, take care of myself and fulfill my social needs. But it’s hard because going to class can sometimes be your only social fix.”
Inland students follow similar rules, including a no-visitor policy, wearing masks when outside their rooms, no eating in dining halls, and staying 6 feet apart when dining outside in the quad and campus common areas.
Coronavirus testing can be campus routine
The pandemic has also added an extra step to housing procedures: coronavirus screening and testing.
Inland universities have their own versions of online daily health surveys, in which students living on campus must check in — via their school’s website or through an app — and report symptoms. Health officials monitor the responses for possible COVID-19 symptoms, and anyone who tests positive must follow procedures, including contact tracing or possible quarantine.
Related Articles
UCLA creates new department to focus on languages and cultures of Europe
UC Riverside launching Latino and Latin American research center
La Sierra University plans in-person classes for fall 2021
Justice Dept. drops Yale admissions discrimination lawsuit
UC Riverside’s 44th annual Writers Week goes virtual
The University of Redlands requires weekly tests. It partners with the San Bernardino County Department of Public Health to offer COVID-19 nasal swab testing on campus. In addition to daily health assessments through a smartphone app, students are supposed to report up to three “close contacts,” with whom they don’t need to wear masks while in their residence hall.
Neither Inland Cal State school has testing requirements, but students are encouraged to get tested regularly and must complete daily online health assessments to enter campus. Of the Inland Cal States, only Cal Poly Pomona offers on-site testing, administered by school staff.
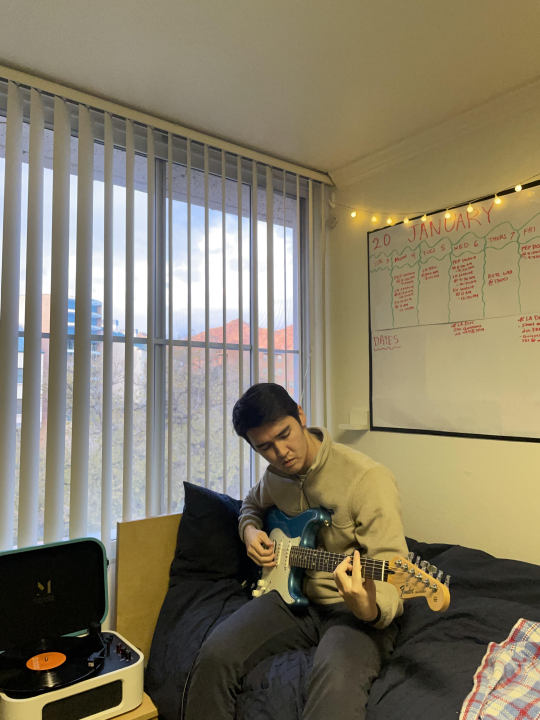
Nick Leiva, 21, a fourth-year political science major at UC Riverside, is a campus resident adviser in the East Lothian hall. He says playing music and working out in his dorm room helps make campus life feel as normal as possible, even in a pandemic. (Photo courtesy of Nick Leiva)
UC Riverside has the strictest policies. Students test twice a week at “spit-and-go” stations, where they spit into a plastic pipette tube and give it to a staff member. The process, including check-in, takes one minute. Students can get results, processed at the campus COVID-19 laboratory, the same day. Lab staff can process up to 900 saliva samples a day.
“It’s the easiest and most efficient way,” Senior Administrative Director William Rall said. “If you did nasal tests twice a week, just think about the scars.”
UCR senior Nick Leiva, 21, agreed that spit-and-go testing is “a lot less uncomfortable,” and is something to which he and other students eventually became accustomed.
Leiva, who works as a resident adviser at the Lothian residence hall, said enforcing the rules — which include making sure people wear masks, stay socially distant and hold no private gatherings or parties in dorm rooms — comes easier when residents understand the implications of living on campus during a global pandemic.
“I know that when I first started college, I wanted to live in the dorms so bad,” said Leiva. “The fact that these students are choosing to do that during these times really speaks to the desire for adulthood and a feel for college life… I see it as my job to make them feel welcome and safe here.”
Students find community on campus
Though day-to-day campus life looks different these days, students say prioritizing “self-care” hobbies — such as meditation and exercise — and finding community keeps them going, even while pent up indoors. They’ve joined virtual club meetings and events, found friends to grab lunch with outside between classes and gradually established a routine in the quiet.

Hazar Eldick, a 21-year-old junior liberal studies major at Cal Poly Pomona, has lived on campus all three years. She wanted the full college experience, even during the coronavirus pandemic. (Photo courtesy of Hazar Eldick)
Jon Merchant, interim director for housing and residential education at Cal State San Bernardino, said it’s important to give students a “normal experience” as best as they can — knowing that nothing about the past year has been normal.
Reyes Luna, interim executive director and director of residence life and university housing services at Cal Poly Pomona, agreed that campuses are doing their best “to build engagement in a virtual world.”
Eldick, the Cal Poly student, said that living on a typically bustling campus with less than 300 others for the past few months has allowed students to get to know each other much faster, and to “get creative with how we spend time together.”
Related links
California college classes go online only in counties where coronavirus not under control
UC Riverside classes to stay online for spring quarter
Parents, students rally to resume youth sports competitions
Keep calm and play on: Students chart a new music course during COVID-19
Norco prison inmates earning bachelor’s degrees through Pitzer College
UC schools more popular than ever for college hopefuls
She likes to skateboard with friends and hike to hideaway spots — such as the school’s iconic hilltop “Cal Poly Pomona letters” — around campus.
“Our campus is usually so crowded and busy, but I’ve been noticing more of its natural beauty when it’s empty,” Eldick said. “It’s very peaceful.”
Leiva said that, between a rigorous class and work schedule, he finds ways to exercise through his ROTC program. He said it’s all about “making the best out of the situation,” especially with the lack of social or extracurricular events. As a resident assistant, he enjoys hosting virtual programs with students, such as watching movies or teaching arts-and-crafts through Zoom.
“I’ve still been able to make good connections, even if it’s all virtual,” he said. “That’s what makes it all worth it.”
-on February 10, 2021 at 04:58AM by Allyson Escobar
0 notes
Text
Body image. A topic that I find, like many of you, difficult to talk about sometimes. Let me start by saying this: my body is nowhere near “perfect” and it never will be. What is perfection anyways? Being slender? Being curvy? Slim thicc? Everyone is attracted to different traits, body types, hair colors, etc. It’s all about preference. I’ve battled with myself for far too long about body image and it’s taken me years to try to be body positive. I’m still not happy with where I am, but I’m amazed with how far I’ve come.
I’ve never been “skinny.” I was a chubby baby and it didn’t stop there. My brother called me fat on a daily basis when I was growing up. My grandpa told me if I kept eating as much as I was, I was going to look like my mother one day. My grandmother told my mom I had large thighs. One of my childhood friends told me I had cellulite (well, we didn’t know what cellulite was back then. She referred to it as “dimples”). Classmates made snide comments about my weight and/or my appearance during the years that I craved acceptance the most. Once all of these flaws were brought to my attention, it was hard for me to ignore them.
In some ways, I had a normal childhood like everyone else. I grew up in a nice neighborhood, I always had kids my own age to play with, and I did well in school. I didn’t have many hobbies outside of having play dates, spending time outside, and writing in a diary before I went to bed at night...but I still felt happy and fulfilled. My parents stayed married and kept any kind of problems they may have had private. I had a brother I could always play video games or watch tv with. I had a great group of friends. Life truly was as easy and loving as it could have been for me. Until my brother got sick.
I don’t want to draw too much attention to it or get to personal with these stories, because I don’t want people to look at me any differently. But my brother used to hit me...a lot. And over the smallest things. He seemed very much unlike himself. His demeanor would change like the flip of a switch and he could go from being perfectly content to aggressively angry. Most of the time, he took his anger out on me. I was the closest person in proximity to him, so I was, unfortunately, an easy target. I’m also three years younger than him.
I distinctly remember one of my friends coming over to the house when my parents weren’t home, and my brother was on the computer. We asked him if we could use it--I wanted to show her how to create a new AIM screen name (holy throwback!). He repeatedly told me no. I threatened to call our mom (wasn’t that how you got your siblings to do anything when you were kids?). He rose from the chair and started wailing on me until I fell to the ground. He hovered over me and continued to hit me, despite how much I was crying out in pain. My friend jumped on the couch and started yelling at him, saying she was going to call the police if he didn’t stop. We were both hysterical--my friend hysterical with fear, and I was hysterically in pain. I don’t remember anything after that, honestly. I probably tried to block in out from my memory.
He used to threaten me not to tell my parents. I listened to him because I didn’t want to be in pain again. I had tried telling my parents before...I don’t know if they were in denial, or if they just thought it was normal sibling behavior. Eventually, my parents started witnessing more of the pent up anger he had and took him to see a child counselor. He seemed to be handling his anger better but things took a turn for the worse. His health seemed to be declining. My parents had to keep an extra set of clothes at school for him because he had suddenly lost his ability to tell when he had to go to the bathroom. He was late to school one day and when my dad and I went to drop him off, we watched him hook his arm through one of the straps, and when he went to do the second one, he just completely fell over. We went to our doctor and she was watching him walk in a straight line. “Pick up your foot!” I had said to him. There was one foot that seemed to be dragging behind the other.
I don’t remember all of the details, but it turned out that he did have a serious medical problem. He had a cyst that hung off of his spinal cord that was affecting his balance, and he had a brain tumor. The next year or two were hard. He had to have emergency surgery that left me to be shuffled between different friends and family’s houses. I had to have out-of-state family members stay with me so he could see specialists in New York. He was in the hospital and a rehabilitation center for a long time, and eventually had to move in with my grandpa because his spinal surgery caused him to have to relearn how to walk again. Our grandpa’s house was a rancher-style and the only steps were to get into the basement.
You’re probably wondering why I’m telling you this. During the years that this was happening, my brother and I were both at ages where our brains were actively growing. It was the time when our perception of who we were as people began to form. I felt abandoned at that time--by my family for leaving me behind and keeping me out of the loop. I felt like they cared more about him than they did me, (Of course, I realize now that the problems were bigger than me--they almost lost him and needed to tend to him. Putting me with friends and other family members was the best avenue they could’ve taken, without having to pull me from school.) My life seemed chaotic. I was being teased by classmates about his medical problems and how I probably had them, too.
Everything seemed to normalize once my brother moved back home, but he was never the same. The loving relationship we had before his medical problems began to surface had completely disintegrated. He was bitter that I had a normal life and wasn’t plagued by the same hardships he faced. It created a resentment that was almost palpable. He still let anger consume him and he’d make me his punching bag. While it wasn’t necessarily physical anymore, he still made an effort to hurt me with his words. He made me feel worthless by calling me fat and ugly.
I carried the weight of my childhood and turned to eating as a source of comfort. Food was something that I could always rely on. So, when my brother or my classmates made me feel bad, I ate. And ate. And probably ate some more. This certainly didn’t help me with my self-esteem or my body image. I was definitely chubby, but I wouldn’t say I was ever “fat.” I think the most I ever weighed was 170, which is embarrassing to admit now. But guys didn’t like me. They thought I was nerdy and couldn’t be bothered to get to know me because of my appearance. Looking back, I think I attribute my relationship with my brother to my fear of men. I was uncomfortable being around them one on one to the point where I’d get physically sick. I guess that explains my nonexistent dating life in high school and college...Here’s a super personal fact about me: I was so afraid of guys and the idea of being physically intimate with someone, I didn’t kiss anyone until I was twenty-one. Yes, you heard that correctly. Thank goodness for that one guy I allowed myself to take a chance on and who was super patient with me.
Those years were hard. Both emotionally and mentally draining. Once I graduated college, I made an active effort to eat better and to shed some of that weight. I wanted to grow into a confident, happy version of myself who wasn’t afraid of male attention. I wanted to like what I saw in the mirror. Being out of school absolutely helped me make better food choices--I wasn’t constantly surrounded by french fries, burgers, milkshakes, etc. I started feeling mentally healthier once I became more physically active. Now, mind you, my weight still fluctuates to this day. But I am proud to say that I am thirty pounds lighter than I was at my heaviest, and I’ve grown to be more body positive. I don’t shy away from clothing that hugs my body anymore. I used to be petrified to wear shorts in public because I have cellulite on my legs, but I started showing more of my body off two years ago and I’ve realized that I am my own worst critic. I know that the cellulite is there, so I assume that everyone else is staring at it as heavily as I was, but they’re not. Can they see the little dimples on my legs when I wear shorts or dresses? Sure. Is it the most appealing thing to look at? No. But, I’m fucking human. I have cellulite, who the fuck cares?
I used to let it RUN my life. I would only go “so far” with a guy because I didn’t want him to see me entirely naked. I was afraid that if a guy saw that I had cellulite on my legs (and butt, let’s be honest), that it would somehow make me less attractive or less lovable in his eyes. I constantly told myself I wasn’t good enough for someone who was very physically fit because I’m not toned and have those little dimples. I criticized myself to the point where I felt ugly. I still have that cellulite. My legs still jiggle every time I walk, but you know what? I don’t care as much. I truly believe that I suffered from that ugly duckling syndrome. I finally became the swan when I began taking care of myself. I’m on my feet for at least five hours a day at my job. I was exercising multiple times a week before my back started hurting, so that is something that I slowly want to bring back into my routine. I gave up Dunkin Donuts, bread, and pizza for lent, and I feel so much better. I haven’t quite seen the weight loss that I’ve been looking for, but I feel more energized. I enjoy making healthier food choices. I enjoy curling my hair, wearing makeup, and wearing a dress that shows off my very imperfect body. I’m tired of trying to attain perfection or feeling bad about myself when I scroll through my social media apps and realize that my body is painfully average. I’m still a damn queen, even with a couple extra dimples. It’s about time I start acting like it!
0 notes
Text
Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway)
One of the most common complaints people have as they age is poor quality sleep. They get less sleep than younger people, and, despite what you may have heard, their sleep requirements do not decline with age. A 70-year-old should still be getting 7-8 hours of sleep a night. The problem is that, for many different reasons, older people usually have issues getting the amount of sleep they need.
The popular approach is to accept poor sleep as an inevitable part of aging and find workarounds, ideally workarounds that require a lifelong prescription to a name-brand pharmaceutical. That’s not my way. I accept that the conventional approach may be warranted in certain cases, but it should be a last resort. A person should exhaust the diet, lifestyle, and exercise options before turning to the prescription pad.
What about that central position of the conventional wisdom: Declining sleep quality is a necessary function of age. Is that actually true?
Why Do We Equate Getting Older With Sleeping Poorly?
Age is a predictor of poor quality sleep, but it’s not a foregone conclusion. Not every older adult suffers from poor sleep, which means the passage of time alone cannot explain the loss of sleep quality. In fact, when you drill down deeper, you find that there are many health and lifestyle-related predictors of poor quality sleep among older adults.
Such as:
In older Taiwanese adults living in a retirement community, 42% reported sleep disturbances. The best predictors for low quality sleep were being sedentary, suffering from nighttime urination, using anti-hypertensive drugs, and having poor mental health.
In older Korean adults, 60% reported sleep issues. The best predictors for low quality sleep in this group were depression, pain, and poor self-rated health scores.
In older women, menopause can make getting good sleep harder. The night sweats and body temperature fluctuations (the body tends to drop its temperature in preparation for sleep, and heat flashes can interfere with this) are notorious sleep disruptors.
These are all modifiable risk factors. Even menopause. Menopause will happen, but the symptoms can be addressed and mitigated (though admittedly not easily). I actually wrote a post about this.
There is one specific cluster of neurons called the ventrolateral preoptic nucleus that acts as a “sleep switch”—releasing GABA and other inhibitory neurotransmitters that inhibit wakefulness. The ventrolateral preoptic nucleus has been shown to degrade with age, actually getting smaller over time; further research shows that the size of a person’s VPN correlates closely with their sleep quality. But there’s no indication that this is an inevitable consequence of aging. After all, the rate of VPN decline varies between individuals. Maybe some of that rate variation is genetic. Maybe some is environmental—based on how you live and eat and exercise. We do know that light and sun exposure during the day boosts serotonin levels, and serotonin is one of the precursors for VPN sleep activity. What if a lifetime of inadequate sun and daylight exposure causes the VPN to “atrophy”? There are many unanswered questions, but even if the VPN turns out to follow a strictly chronological decline, there are improvements to be made.
Other “inevitabilities” of aging are often a function of accruing compound interest on one’s failure to lead a healthy lifestyle. If we’ve neglected our health and wellness for our entire lives—often because we were following bad advice from the “experts” who were supposed to know better—that’s going to come to a head the older we get. The older we are, the worse our body will work. The more negative interest we’ll have accrued.
Okay, Sisson, that’s all well and good, but what if I’m already an older adult, I’ve already accrued a lifetime of suboptimal health, and my sleep is bad? What can I do?
5 Easy Ways To Improve Your Sleep (At ANY Age)
You can start addressing the issues right now, right today.
1. You can lift heavy things.
Resistance training has been shown to improve sleep quality in older adults. Three times a week, older adults lifted weights for 30 minutes in the morning and saw their sleep quality improve by 38%. It also works in older adults with poor sleep and depression.
2. You can walk.
A three-time weekly walking program for four weeks helped older Nepalese adults improve their sleep quality.
3. You can reduce your alcohol intake.
A few years ago, I noticed that my nightly glass or two of wine was messing with my sleep, so I gave it up and my sleep improved immediately. I’ve since re-introduced Dry Farm natural wine—lower in alcohol and sulfites, higher in antioxidants and complexity—and have no issues. If you drink on a regular basis and have trouble with sleep, try giving up alcohol for a month. It’s a potentially very easy fix.
4. You can avoid artificial light after dark.
This doesn’t just work in younger people. There is strong evidence that exposure to artificial light after dark is linked to insomnia in older adults. Wearing blue-blocking goggles or simply not using electronic devices after dark are easy fixes.
5. You can get more natural light in the morning and daytime.
In older adults, getting more natural light in the daytime hours has a direct effect of improving sleep quality.
Hey, it’s almost like everything in our lives is connected. Some people find this overwhelming and depressing—”how can I possibly fix everything?” I find it empowering. It fills me with optimism because addressing one piece of the chain can get everything else moving in the right direction. Just look at the study with depressed older adults who had trouble sleeping. All they had to do was start lifting heavy things a few times a week and all their major issues began resolving, or at least improving. That’s powerful.
Now imagine if you tried everything. Imagine if you started lifting weights, walking, reduced your alcohol intake. Imagine the changes you could see. Now imagine if you did this from early adulthood and never stopped. Imagine how you’d sleep. Oh, and don’t neglect the power of a consistent routine.
What I Do (and One Thing That’s Made the Biggest Difference)
Last year, I released a video of my nighttime routine. Now that I’m in Miami, the setup has changed but I still do the same basic stuff.
I live in a condo now that has a great spa. I do “fire and ice” before dinner almost every night”—usually 7-10 minutes sauna, 3-4 minutes cold plunge at 50 degrees, repeat a few times. So, no longer right before bed. But it has the effect of making me relaxed and sleep-ready a few hours after a light dinner.
But there’s one tool I began using a couple years ago that has probably made the most difference of any particular strategy: controlling the temperature of my bed.
Ambient temperature matters for sleep quality. My chiliPAD has become indispensable. (Disclosure: I became such a fan that I eventually invested in the company.) Carrie uses one, too. We have different ideal temperature ranges. Mine cools to 65 at bedtime, but with the app I can set it to rise to 68 at 3:00 A.M. (otherwise I get a little too much heat loss), 70 at 5:00 A.M. and then 75 at 6:45 to help me wake up. It makes a huge difference and has real evolutionary antecedence; humans spent many millennia sleeping on a cold surface (the ground) covered with animal skins. It’s what our genes still expect from us.
How’s your sleep, older (or not) readers? What’s worked, what hasn’t? If you have any questions about sleep, drop them down below and I’ll follow up!
Now For the Giveaway…
Whenever I find a product I truly love, I want to share it. Today it’s for two lucky winners.
The great folks at ChiliTechnology have offered two of their cooling systems for MDA readers (the two Carrie and I use): a chiliPAD system and their new OOLER system. Both offer the same fully programmable cooling technology to help you manufacture your best night’s sleep. Plus, I’m throwing in a Primal Essentials Kit (Damage Control, Primal Omegas, Primal Sun, Primal Probiotics and Adaptogenic Calm) because good health and great sleep go hand-in-hand.
One winner will nab the chiliPAD, plus Primal supplements package.
The second winner will enjoy the OOLER system, plus Primal supplements package.
To enter to win:
1. Follow @marksdailyapple + @chilisleep + @primalblueprint
2. Tag two friends in the comments from this giveaway post.
Open to US only. The winner will be announced and contacted via Instagram direct message on Thursday, May 30th.
Good luck, everybody!
(function($) { $("#dfoybto").load("https://www.marksdailyapple.com/wp-admin/admin-ajax.php?action=dfads_ajax_load_ads&groups=674&limit=1&orderby=random&order=ASC&container_id=&container_html=none&container_class=&ad_html=div&ad_class=&callback_function=&return_javascript=0&_block_id=dfoybto" ); })( jQuery );
window.onload=function(){ga('send', { hitType: 'event', eventCategory: 'Ad Impression', eventAction: '84166' });}
References:
Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. Int J Nurs Pract. 2013;19(2):116-23.
Ferris LT, Williams JS, Shen CL, O’keefe KA, Hale KB. Resistance training improves sleep quality in older adults a pilot study. J Sports Sci Med. 2005;4(3):354-60.
Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of the effect of exercise on sleep. Sleep. 1997;20(2):95-101.
The post Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway) appeared first on Mark's Daily Apple.
Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway) published first on https://drugaddictionsrehab.tumblr.com/
0 notes
Text
Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway)
One of the most common complaints people have as they age is poor quality sleep. They get less sleep than younger people, and, despite what you may have heard, their sleep requirements do not decline with age. A 70-year-old should still be getting 7-8 hours of sleep a night. The problem is that, for many different reasons, older people usually have issues getting the amount of sleep they need.
The popular approach is to accept poor sleep as an inevitable part of aging and find workarounds, ideally workarounds that require a lifelong prescription to a name-brand pharmaceutical. That’s not my way. I accept that the conventional approach may be warranted in certain cases, but it should be a last resort. A person should exhaust the diet, lifestyle, and exercise options before turning to the prescription pad.
What about that central position of the conventional wisdom: Declining sleep quality is a necessary function of age. Is that actually true?
Why Do We Equate Getting Older With Sleeping Poorly?
Age is a predictor of poor quality sleep, but it’s not a foregone conclusion. Not every older adult suffers from poor sleep, which means the passage of time alone cannot explain the loss of sleep quality. In fact, when you drill down deeper, you find that there are many health and lifestyle-related predictors of poor quality sleep among older adults.
Such as:
In older Taiwanese adults living in a retirement community, 42% reported sleep disturbances. The best predictors for low quality sleep were being sedentary, suffering from nighttime urination, using anti-hypertensive drugs, and having poor mental health.
In older Korean adults, 60% reported sleep issues. The best predictors for low quality sleep in this group were depression, pain, and poor self-rated health scores.
In older women, menopause can make getting good sleep harder. The night sweats and body temperature fluctuations (the body tends to drop its temperature in preparation for sleep, and heat flashes can interfere with this) are notorious sleep disruptors.
These are all modifiable risk factors. Even menopause. Menopause will happen, but the symptoms can be addressed and mitigated (though admittedly not easily). I actually wrote a post about this.
There is one specific cluster of neurons called the ventrolateral preoptic nucleus that acts as a “sleep switch”—releasing GABA and other inhibitory neurotransmitters that inhibit wakefulness. The ventrolateral preoptic nucleus has been shown to degrade with age, actually getting smaller over time; further research shows that the size of a person’s VPN correlates closely with their sleep quality. But there’s no indication that this is an inevitable consequence of aging. After all, the rate of VPN decline varies between individuals. Maybe some of that rate variation is genetic. Maybe some is environmental—based on how you live and eat and exercise. We do know that light and sun exposure during the day boosts serotonin levels, and serotonin is one of the precursors for VPN sleep activity. What if a lifetime of inadequate sun and daylight exposure causes the VPN to “atrophy”? There are many unanswered questions, but even if the VPN turns out to follow a strictly chronological decline, there are improvements to be made.
Other “inevitabilities” of aging are often a function of accruing compound interest on one’s failure to lead a healthy lifestyle. If we’ve neglected our health and wellness for our entire lives—often because we were following bad advice from the “experts” who were supposed to know better—that’s going to come to a head the older we get. The older we are, the worse our body will work. The more negative interest we’ll have accrued.
Okay, Sisson, that’s all well and good, but what if I’m already an older adult, I’ve already accrued a lifetime of suboptimal health, and my sleep is bad? What can I do?
5 Easy Ways To Improve Your Sleep (At ANY Age)
You can start addressing the issues right now, right today.
1. You can lift heavy things.
Resistance training has been shown to improve sleep quality in older adults. Three times a week, older adults lifted weights for 30 minutes in the morning and saw their sleep quality improve by 38%. It also works in older adults with poor sleep and depression.
2. You can walk.
A three-time weekly walking program for four weeks helped older Nepalese adults improve their sleep quality.
3. You can reduce your alcohol intake.
A few years ago, I noticed that my nightly glass or two of wine was messing with my sleep, so I gave it up and my sleep improved immediately. I’ve since re-introduced Dry Farm natural wine—lower in alcohol and sulfites, higher in antioxidants and complexity—and have no issues. If you drink on a regular basis and have trouble with sleep, try giving up alcohol for a month. It’s a potentially very easy fix.
4. You can avoid artificial light after dark.
This doesn’t just work in younger people. There is strong evidence that exposure to artificial light after dark is linked to insomnia in older adults. Wearing blue-blocking goggles or simply not using electronic devices after dark are easy fixes.
5. You can get more natural light in the morning and daytime.
In older adults, getting more natural light in the daytime hours has a direct effect of improving sleep quality.
Hey, it’s almost like everything in our lives is connected. Some people find this overwhelming and depressing—”how can I possibly fix everything?” I find it empowering. It fills me with optimism because addressing one piece of the chain can get everything else moving in the right direction. Just look at the study with depressed older adults who had trouble sleeping. All they had to do was start lifting heavy things a few times a week and all their major issues began resolving, or at least improving. That’s powerful.
Now imagine if you tried everything. Imagine if you started lifting weights, walking, reduced your alcohol intake. Imagine the changes you could see. Now imagine if you did this from early adulthood and never stopped. Imagine how you’d sleep. Oh, and don’t neglect the power of a consistent routine.
What I Do (and One Thing That’s Made the Biggest Difference)
Last year, I released a video of my nighttime routine. Now that I’m in Miami, the setup has changed but I still do the same basic stuff.
I live in a condo now that has a great spa. I do “fire and ice” before dinner almost every night”—usually 7-10 minutes sauna, 3-4 minutes cold plunge at 50 degrees, repeat a few times. So, no longer right before bed. But it has the effect of making me relaxed and sleep-ready a few hours after a light dinner.
But there’s one tool I began using a couple years ago that has probably made the most difference of any particular strategy: controlling the temperature of my bed.
Ambient temperature matters for sleep quality. My chiliPAD has become indispensable. (Disclosure: I became such a fan that I eventually invested in the company.) Carrie uses one, too. We have different ideal temperature ranges. Mine cools to 65 at bedtime, but with the app I can set it to rise to 68 at 3:00 A.M. (otherwise I get a little too much heat loss), 70 at 5:00 A.M. and then 75 at 6:45 to help me wake up. It makes a huge difference and has real evolutionary antecedence; humans spent many millennia sleeping on a cold surface (the ground) covered with animal skins. It’s what our genes still expect from us.
How’s your sleep, older (or not) readers? What’s worked, what hasn’t? If you have any questions about sleep, drop them down below and I’ll follow up!
Now For the Giveaway…
Whenever I find a product I truly love, I want to share it. Today it’s for two lucky winners.
The great folks at ChiliTechnology have offered two of their cooling systems for MDA readers (the two Carrie and I use): a chiliPAD system and their new OOLER system. Both offer the same fully programmable cooling technology to help you manufacture your best night’s sleep. Plus, I’m throwing in a Primal Essentials Kit (Damage Control, Primal Omegas, Primal Sun, Primal Probiotics and Adaptogenic Calm) because good health and great sleep go hand-in-hand.
One winner will nab the chiliPAD, plus Primal supplements package.
The second winner will enjoy the OOLER system, plus Primal supplements package.
To enter to win:
1. Follow @marksdailyapple + @chilisleep + @primalblueprint
2. Tag two friends in the comments from this giveaway post.
Open to US only. The winner will be announced and contacted via Instagram direct message on Thursday, May 30th.
Good luck, everybody!
(function($) { $("#df0wBDV").load("https://www.marksdailyapple.com/wp-admin/admin-ajax.php?action=dfads_ajax_load_ads&groups=674&limit=1&orderby=random&order=ASC&container_id=&container_html=none&container_class=&ad_html=div&ad_class=&callback_function=&return_javascript=0&_block_id=df0wBDV" ); })( jQuery );
window.onload=function(){ga('send', { hitType: 'event', eventCategory: 'Ad Impression', eventAction: '67622' });}
References:
Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. Int J Nurs Pract. 2013;19(2):116-23.
Ferris LT, Williams JS, Shen CL, O’keefe KA, Hale KB. Resistance training improves sleep quality in older adults a pilot study. J Sports Sci Med. 2005;4(3):354-60.
Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of the effect of exercise on sleep. Sleep. 1997;20(2):95-101.
The post Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway) appeared first on Mark's Daily Apple.
Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway) published first on https://venabeahan.tumblr.com
0 notes
Text
I'm W. Garth Callaghan, 'Napkin Notes Dad,' and This Is How I Parent
New Post has been published on http://funnythingshere.xyz/im-w-garth-callaghan-napkin-notes-dad-and-this-is-how-i-parent/
I'm W. Garth Callaghan, 'Napkin Notes Dad,' and This Is How I Parent
Photo: Napkin Notes Dad
Ever since his daughter Emma was in elementary school, W. Garth Callaghan would jot down inspirational quotes and bits of dad wisdom onto napkins and slip the notes into her lunchbox. It became their special thing, their way to connect. He wanted to make sure Emma could read a note from her father every single school day until graduation—even if was no longer around to write them.
Callaghan has been diagnosed with cancer five times since 2011. He believed that these napkin notes might eventually be the only thing Emma would have left of him. He wrote the memoir Napkin Notes: Make Lunch Meaningful, Life Will Follow, which Reese Witherspoon is adapting into a film. As he prepares to send Emma off to college this fall, Callaghan reflects on how he parents.
Advertisement
Name: W. Garth Callaghan
Location: Richmond, Virginia
Job: Napkin Notes Dad and author
Family: Wife Lissa and daughter Emma (18)
Tell us how Napkin Notes began.
When Emma was younger, I worked in a typical office setting, and missed eight to ten hours of her day. I wanted to connect with her more than my schedule allowed, so I started writing napkin notes and sticking them into her lunch when she was in kindergarten. Sometimes I’d pop in a cookie or a piece of candy to make her lunch special. I wasn’t sure what mattered to her, the note or the treat.
Advertisement
When Emma was in 2nd or 3rd grade, I was in the kitchen prepping her lunch while sipping my morning cup of coffee. I hadn’t yet written a note. Emma scooped up her lunch bag, peered in, stomped over to me, and asked, “Napkin note?” That’s when I knew it mattered to her, and I committed to putting a note into each lunch.
Photo: Napkin Notes Dad
I have been diagnosed with cancer five times. The first diagnosis came out of the blue and turned our world upside down. After my third diagnosis in 2013, I made a promise to write out all of the napkin notes Emma would need up until high school graduation.
Advertisement
I am by no means perfect, and there were days life just didn’t work in my favor. I have driven a note to school more than a few times. Do you know how embarrassing it is to have to ask the principal, “Can you please get this note into Emma’s lunch bag?”
Take us through your morning routine. What are your best tricks for getting out the door?
I have been taking daily chemo now for well over four years. My chemo brain is strong and I easily forget things. The key to any successful morning is planning, and that starts the night before. I review my schedule as well as the family schedule. I follow the same routine each day so that I am less likely to forget something.
Advertisement
Once everyone is set, I take a few minutes and write at least 800 words before starting work.
Photo: Courtesy of W. Garth Callaghan
How much outside help do you get as a parent? Who or what can’t you live without?
I’d like to think that we don’t need more help than any other typical family, but I know that my health impacts so much of our lives that it’s impossible to survive alone. Our friends and church family step up to help with carpooling, delivering egg drop soup when I am nauseated, fetching prescriptions or groceries, and even raking our yard. I am happy to say we don’t have to lean on everyone all of the time, but we couldn’t make it without this strong support circle.
Advertisement
What are the gadgets, apps, charts or tools you rely on?
I am a self-professed geek and love gadgets. I can’t remember everything I need to, so my Google Pixel is never out of my sight. I love the pictures this phone takes! I use Wunderlist for to-dos (chemo brain!) and Evernote for cataloging. I keep all of my medical records on Evernote so they are easily accessible for me at any time. I track health issues with PatientsLikeMe to help others with kidney cancer.
Has becoming a parent changed the way you work?
Being a parent has made me realize that work is important, but not nearly as important as raising the next generation. I work so that I can be the dad who never misses a softball game. There was a time when I traveled quite a bit for work, and I wrote out napkin notes before each trip so Emma always had a note in her lunch.
Advertisement
What does your evening routine like?
Fatigue is the biggest side effect from my treatment and I really need to wind down after 7 PM. During the school year, we’d often be at the ballfield until late evening and I’d spend my time doing my favorite thing: cheering Emma and her team on. Now that we’re in a permanent off-season, I am an avid reader and try to read a few chapters of something. I am in the middle of Mindset by Carol Dweck. Next up is Cryptonomicon by Neal Stephenson.
How do you decompress?
I love to play video games. I play any version of Halo on my XBOX One, and I play Star Wars Galaxies on my PC.
Advertisement
I’d like to say I am also an avid gym-goer, but I am not as good as I should be. My oncologist told me today that I should act as if I am training for a marathon and has motivated me to step up my game.
What’s been your proudest moment as a parent?
A single moment??? I can’t. I just can’t. I am tearing up even remembering all of the moments that I can easily list off. Like …
Advertisement
… the time when Emma was the incredibly kind and gentle coach playing Buddy Ball with the special needs team.
… the time when an impossible-to-stop hard grounder was hit to Emma at shortstop, and she caught it and effortlessly backhanded it to the third Baseman without even looking where the player was.
… the time when I asked her if it was okay to write a very personal book about our lives and she responded eagerly, “Oh Dad, I want you to write the book!”
Advertisement
I work so that I can be the dad who never misses a softball game.
What moment are you least proud of?
Emma was about 18 months old and was jumping on her bed. I told her to stop jumping there. Why did I do that? Did it really matter that she was jumping on her bed? I lost my cool and told her if she jumped on the bed, I’d spank her. She stopped, looked me straight in the eye, and jumped some more. What could I do? We sat together in her room, both of us crying and I swatted her bottom once with just enough force to crush my heart.
Advertisement
What do you want your kid to learn from your example?
I want Emma to know the value of trying and failing, then trying better and failing better.
What are your favorite funny/weird/special family rituals?
We have this weird thing for an overabundance of fall produce. We pick pumpkins at an “All You Can Carry” pumpkin patch and have perfected the art of carrying more pumpkins that we can remotely use, all for $10. (The trick is to load the first layer of pumpkins stem side down.) We also pick our own apples at an orchard in Charlottesville. We pick so many that I have to make two trips to the car! I think our family record was over 70 pounds.
Advertisement
One very funny, weird thing about us and our dear friends: We sing the diarrhea song together, but only when camping. I don’t think we’ve ever actually had bowel problems out there, but the song is funny to sing around a campfire.
Has anyone ever given you a piece of parenting advice that has really stuck with you?
Rachel Macy Stafford wrote a piece on the most important six words you can say to your child and I took that advice to heart. It changed my perspective immediately and I started to practice it at the very next softball game I attended.
Advertisement
The six words: “I love to watch you play.”
What’s the hardest part about being a parent?
Learning to fail well in front of your child.
What’s your favorite part of the day?
I know this will be corny, but every part of every day. I have metastatic kidney cancer and the likelihood to become cured is practically zero. Whenever someone asks me how I am doing, I always respond with, “Each day on this side of the grass is a good day” and genuinely mean it.
Advertisement
How can parents find ways to connect with their kids?
Find the small thing, the ritual, that’ll be just between you and your child. It could be anything! Try flying paper airplanes from the second story window, wearing the same T-shirt to the movies, memorizing a favorite story word-for-word, or learning how to dance in tandem like they do in the movie Big.
Any other wisdom you’d like to share?
Write a note on the napkin. You can use a sticky note or regular paper and put in somewhere safe if you don’t pack a lunch. Last year I wrote about 180 napkin notes for Emma. Five were super successful and were brought back home to be tacked onto the message board in the kitchen or placed on Emma’s dresser.
Advertisement
I had put this one on her car seat one random morning and it stayed on her dresser all year:
Photo: Napkin Notes Dad
Oh, and your kids absolutely know when you’re looking at your phone during their game/meet/performance. Don’t think you’re fooling them one bit.
Advertisement
Source: https://offspring.lifehacker.com/im-w-garth-callaghan-napkin-notes-dad-and-this-is-ho-1827618994
0 notes
Text
Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway)
One of the most common complaints people have as they age is poor quality sleep. They get less sleep than younger people, and, despite what you may have heard, their sleep requirements do not decline with age. A 70-year-old should still be getting 7-8 hours of sleep a night. The problem is that, for many different reasons, older people usually have issues getting the amount of sleep they need.
The popular approach is to accept poor sleep as an inevitable part of aging and find workarounds, ideally workarounds that require a lifelong prescription to a name-brand pharmaceutical. That’s not my way. I accept that the conventional approach may be warranted in certain cases, but it should be a last resort. A person should exhaust the diet, lifestyle, and exercise options before turning to the prescription pad.
What about that central position of the conventional wisdom: Declining sleep quality is a necessary function of age. Is that actually true?
Why Do We Equate Getting Older With Sleeping Poorly?
Age is a predictor of poor quality sleep, but it’s not a foregone conclusion. Not every older adult suffers from poor sleep, which means the passage of time alone cannot explain the loss of sleep quality. In fact, when you drill down deeper, you find that there are many health and lifestyle-related predictors of poor quality sleep among older adults.
Such as:
In older Taiwanese adults living in a retirement community, 42% reported sleep disturbances. The best predictors for low quality sleep were being sedentary, suffering from nighttime urination, using anti-hypertensive drugs, and having poor mental health.
In older Korean adults, 60% reported sleep issues. The best predictors for low quality sleep in this group were depression, pain, and poor self-rated health scores.
In older women, menopause can make getting good sleep harder. The night sweats and body temperature fluctuations (the body tends to drop its temperature in preparation for sleep, and heat flashes can interfere with this) are notorious sleep disruptors.
These are all modifiable risk factors. Even menopause. Menopause will happen, but the symptoms can be addressed and mitigated (though admittedly not easily). I actually wrote a post about this.
There is one specific cluster of neurons called the ventrolateral preoptic nucleus that acts as a “sleep switch”—releasing GABA and other inhibitory neurotransmitters that inhibit wakefulness. The ventrolateral preoptic nucleus has been shown to degrade with age, actually getting smaller over time; further research shows that the size of a person’s VPN correlates closely with their sleep quality. But there’s no indication that this is an inevitable consequence of aging. After all, the rate of VPN decline varies between individuals. Maybe some of that rate variation is genetic. Maybe some is environmental—based on how you live and eat and exercise. We do know that light and sun exposure during the day boosts serotonin levels, and serotonin is one of the precursors for VPN sleep activity. What if a lifetime of inadequate sun and daylight exposure causes the VPN to “atrophy”? There are many unanswered questions, but even if the VPN turns out to follow a strictly chronological decline, there are improvements to be made.
Other “inevitabilities” of aging are often a function of accruing compound interest on one’s failure to lead a healthy lifestyle. If we’ve neglected our health and wellness for our entire lives—often because we were following bad advice from the “experts” who were supposed to know better—that’s going to come to a head the older we get. The older we are, the worse our body will work. The more negative interest we’ll have accrued.
Okay, Sisson, that’s all well and good, but what if I’m already an older adult, I’ve already accrued a lifetime of suboptimal health, and my sleep is bad? What can I do?
5 Easy Ways To Improve Your Sleep (At ANY Age)
You can start addressing the issues right now, right today.
1. You can lift heavy things.
Resistance training has been shown to improve sleep quality in older adults. Three times a week, older adults lifted weights for 30 minutes in the morning and saw their sleep quality improve by 38%. It also works in older adults with poor sleep and depression.
2. You can walk.
A three-time weekly walking program for four weeks helped older Nepalese adults improve their sleep quality.
3. You can reduce your alcohol intake.
A few years ago, I noticed that my nightly glass or two of wine was messing with my sleep, so I gave it up and my sleep improved immediately. I’ve since re-introduced Dry Farm natural wine—lower in alcohol and sulfites, higher in antioxidants and complexity—and have no issues. If you drink on a regular basis and have trouble with sleep, try giving up alcohol for a month. It’s a potentially very easy fix.
4. You can avoid artificial light after dark.
This doesn’t just work in younger people. There is strong evidence that exposure to artificial light after dark is linked to insomnia in older adults. Wearing blue-blocking goggles or simply not using electronic devices after dark are easy fixes.
5. You can get more natural light in the morning and daytime.
In older adults, getting more natural light in the daytime hours has a direct effect of improving sleep quality.
Hey, it’s almost like everything in our lives is connected. Some people find this overwhelming and depressing—”how can I possibly fix everything?” I find it empowering. It fills me with optimism because addressing one piece of the chain can get everything else moving in the right direction. Just look at the study with depressed older adults who had trouble sleeping. All they had to do was start lifting heavy things a few times a week and all their major issues began resolving, or at least improving. That’s powerful.
Now imagine if you tried everything. Imagine if you started lifting weights, walking, reduced your alcohol intake. Imagine the changes you could see. Now imagine if you did this from early adulthood and never stopped. Imagine how you’d sleep. Oh, and don’t neglect the power of a consistent routine.
What I Do (and One Thing That’s Made the Biggest Difference)
Last year, I released a video of my nighttime routine. Now that I’m in Miami, the setup has changed but I still do the same basic stuff.
I live in a condo now that has a great spa. I do “fire and ice” before dinner almost every night”—usually 7-10 minutes sauna, 3-4 minutes cold plunge at 50 degrees, repeat a few times. So, no longer right before bed. But it has the effect of making me relaxed and sleep-ready a few hours after a light dinner.
But there’s one tool I began using a couple years ago that has probably made the most difference of any particular strategy: controlling the temperature of my bed.
Ambient temperature matters for sleep quality. My chiliPAD has become indispensable. (Disclosure: I became such a fan that I eventually invested in the company.) Carrie uses one, too. We have different ideal temperature ranges. Mine cools to 65 at bedtime, but with the app I can set it to rise to 68 at 3:00 A.M. (otherwise I get a little too much heat loss), 70 at 5:00 A.M. and then 75 at 6:45 to help me wake up. It makes a huge difference and has real evolutionary antecedence; humans spent many millennia sleeping on a cold surface (the ground) covered with animal skins. It’s what our genes still expect from us.
How’s your sleep, older (or not) readers? What’s worked, what hasn’t? If you have any questions about sleep, drop them down below and I’ll follow up!
Now For the Giveaway…
Whenever I find a product I truly love, I want to share it. Today it’s for two lucky winners.
The great folks at ChiliTechnology have offered two of their cooling systems for MDA readers (the two Carrie and I use): a chiliPAD system and their new OOLER system. Both offer the same fully programmable cooling technology to help you manufacture your best night’s sleep. Plus, I’m throwing in a Primal Essentials Kit (Damage Control, Primal Omegas, Primal Sun, Primal Probiotics and Adaptogenic Calm) because good health and great sleep go hand-in-hand.
One winner will nab the chiliPAD, plus Primal supplements package.
The second winner will enjoy the OOLER system, plus Primal supplements package.
To enter to win:
1. Follow @marksdailyapple + @chilisleep + @primalblueprint
2. Tag two friends in the comments from this giveaway post.
Open to US only. The winner will be announced and contacted via Instagram direct message on Thursday, May 30th.
Good luck, everybody!
(function($) { $("#dfBZVkE").load("https://www.marksdailyapple.com/wp-admin/admin-ajax.php?action=dfads_ajax_load_ads&groups=674&limit=1&orderby=random&order=ASC&container_id=&container_html=none&container_class=&ad_html=div&ad_class=&callback_function=&return_javascript=0&_block_id=dfBZVkE" ); })( jQuery );
window.onload=function(){ga('send', { hitType: 'event', eventCategory: 'Ad Impression', eventAction: '72277' });}
References:
Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. Int J Nurs Pract. 2013;19(2):116-23.
Ferris LT, Williams JS, Shen CL, O’keefe KA, Hale KB. Resistance training improves sleep quality in older adults a pilot study. J Sports Sci Med. 2005;4(3):354-60.
Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of the effect of exercise on sleep. Sleep. 1997;20(2):95-101.
The post Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway) appeared first on Mark's Daily Apple.
Does Sleep Quality Really Decline With Age? (Plus, What I Do & a Giveaway) published first on https://drugaddictionsrehab.tumblr.com/
0 notes